Mammary constriction syndrome
Mammary Constriction Syndrome - Breastfeeding Support
Breastfeeding SupportCreated with Sketch.Evidence-based breastfeeding tips and resources
Editor in Chief Philippa Pearson-Glaze
- Home
- Articles
- Our Picks
- Find IBCLC
- About
- Contact
- Newsletter
- Terms & Privacy
- Log in
- Latching & Attaching
- Problems
Author
By Philippa Pearson-Glaze IBCLC
Last Revised
Mammary constriction syndrome (MCS) is a new explanation for deep breast pain during breastfeeding. It was first described by Edith Kernerman IBCLC and Eileen Park, IBCLC, ND. 1
Search Articles
Need to look something up?
A tightening of blood vessels
If there is a sudden tightening (i.e. narrowing or constriction) of blood vessels in an area of the body, it reduces blood flow and oxygen to that area. This sudden tightening of vessels is known as vasospasm. If a baby breastfeeds in an uncomfortable or shallow latch (has mostly nipple in their mouth without plenty of breast tissue) this can trigger a nipple vasospasm which can cause a burning or stabbing pain in the nipple(s). And when a constriction of blood vessels happens deeper in the breast, it can cause deep stabbing or shooting pains in the chest—this collection of symptoms is known as mammary constriction syndrome.
Causes of mammary constriction syndrome
Tension in a mother’s shoulders or chest can cause her pectoral muscles beneath the glandular tissue in the breast to press on the blood vessels that supply the breast and nipples. Tension may have several causes including the way a mother is sitting to breastfeed for long periods or the tensing of her shoulders in anticipation of a very painful latch. Edith Kernerman explains;
Tension may have several causes including the way a mother is sitting to breastfeed for long periods or the tensing of her shoulders in anticipation of a very painful latch. Edith Kernerman explains;
Excerpt from
Dr. Jack Newman’s Guide to Breastfeeding (updated edition) p146
Because of difficulties the mother may have had during pregnancy, labour, or after birth, she may have tightness in her shoulders and chest that causes her pectoral (chest) muscles to press on the blood vessels that lead to her breasts and nipples, causing a lack of blood flow and oxygen, leading to pain. This pain may be throbbing or constant, deep or superficial, itchy, tingling, aching or knife-like, burning or freezing, shooting, sharp or dull, or a combination of any of the above. Also, if a latch feels painful, the mother may tighten her shoulders, clench her teeth, etc., causing the cycle triggering pain to begin again.
Edith Kernerman recommends treating mammary constriction syndrome with a technique she calls pectoral muscle massage. This involves massage of the chest muscles to help ease the tension and trying gentle pectoral muscle stretching, just before a breastfeed. She also suggests a mother with this syndrome should try to keep her back supported rather than hunching forward over her baby and avoid carrying heavy items such as shopping bags or heavy car seats.
This involves massage of the chest muscles to help ease the tension and trying gentle pectoral muscle stretching, just before a breastfeed. She also suggests a mother with this syndrome should try to keep her back supported rather than hunching forward over her baby and avoid carrying heavy items such as shopping bags or heavy car seats.
Pectoral muscle massage
Jack Newman is a Canadian paediatrician and breastfeeding author. There is a useful post online about mammary constriction syndrome on Jack Newman’s Community Facebook page. Here he describes how most cases of breast pain—and/or nipple pain—in breastfeeding mothers are the result of a poor latch at the breast. A poor latch can lead to the secondary problem of vasospasm symptoms of the nipple and mammary constriction syndrome (often mistakenly diagnosed as thrush on nipples as the symptoms are very similar). In the excerpt below Dr Newman briefly describes the treatment technique of pectoral muscle massage;
Excerpt from
Mammary Constriction Syndrome, Dr Jack Newman’s Community Page on Facebook, Feb 2014
Photo courtesy Emily WalkerIt involves rubbing the chest muscles (not the breast) quite vigorously for about 45-60 seconds on the affected side.
There are four places to massage: 1) above the breast against the chest wall; 2) between her breasts just to the side of the breast bone; 3) under the breast against her rib cage; 4) on the side of her body, beside her breast, against the rib cage. One of these four areas is likely to be the ideal spot for her to relieve her pain.
Other causes of deep breast pain
Finding the causes of sore nipples or reasons for pain deep in the breast are not always straightforward—mammary constriction syndrome may only be part of the puzzle. Deep breast pain can be associated with engorgement with breast milk or mastitis and is sometimes confused with thrush. See our articles on Engorged Breasts, Mastitis Symptoms and Treatment and Thrush on Nipples for more information.
Seek skilled help
Contacting an International Board Certified Lactation Consultant (IBCLC) can help to find the most likely causes of pain and for more information see Causes of Sore Nipples and Why Does Breastfeeding Hurt?
Mammary constriction syndrome is a name given to symptoms of deep breast pain that can be caused by the constriction of blood vessels within the breast tissue. The pain is likely caused by a baby feeding in an uncomfortable latch and/or due to muscle tension either from the way a mother is sitting to breastfeed, or the tensing of muscles in anticipation of breastfeeding pain. Mammary constriction syndrome can be helped by a pectoral muscle massage and improving a baby’s positioning and attachment at the breast.
The pain is likely caused by a baby feeding in an uncomfortable latch and/or due to muscle tension either from the way a mother is sitting to breastfeed, or the tensing of muscles in anticipation of breastfeeding pain. Mammary constriction syndrome can be helped by a pectoral muscle massage and improving a baby’s positioning and attachment at the breast.
Footnotes & References
-
Kernerman and Park. Severe Breast Pain Resolved with Pectoral Muscle Massage. Journal of Human Lactation. 2014
Tags
Breast Pain, Deep Breast Pain, Mammary Constriction Syndrome, MCS, Pain, Pain Between Feeds, Painful Feeding, Pectoral Muscle Massage, Referred Pain, Sore Breast, Sore Nipples, Vasoconstriction, Vasospasm
Further Reading
- Severe Breast Pain Resolved with Pectoral Muscle MassageEdith Kernerman and Eileen Park, 2014
Important
This article should not be construed as medical advice. Information found online should always be discussed with your own IBCLC lactation consultant and doctor to ensure it is appropriate for you and your baby’s situation. Contact your doctor, paediatrician or health care provider with any concerns about your baby’s health and welfare.
Information found online should always be discussed with your own IBCLC lactation consultant and doctor to ensure it is appropriate for you and your baby’s situation. Contact your doctor, paediatrician or health care provider with any concerns about your baby’s health and welfare.
Find an IBCLC Read our full disclaimer
International BreastFeeding Centre | Vasospasm (Reynaud's phenomenon) of the nipples
Vasospasm describes a situation when blood vessels contract abnormally resulting in impaired blood flow to an area. People with Raynaud’s phenomenon (often associated with “auto-immune” illnesses such as lupus erythematosus and rheumatoid arthritis) may have vasospasm that will occur in the fingers when going outside from a warm house on a cool day. The fingers will turn white and the lack of blood getting to the tips of the fingers will cause pain.
Vasospasm of the nipples can occur occasionally during pregnancy and not infrequently with breastfeeding and can cause pain in the nipples and/or breasts. See also the information sheet “Sore Nipples”. Note, vasospasm pain in the breast is sometimes referred to as Mammary Constriction Syndrome (MCS), a related condition that is treated similarly.
See also the information sheet “Sore Nipples”. Note, vasospasm pain in the breast is sometimes referred to as Mammary Constriction Syndrome (MCS), a related condition that is treated similarly.
Symptoms of vasospasm in breastfeeding:
Burning, stabbing, throbbing, and/or “pins and needles” pain in the nipple and/or in the breast usually once the baby is off the breast.
- Pain may also occur when stepping out of a warm shower or when going outside on a cold day.
- There may or may not be pain during breastfeeding.
- Nipples may change colour (red, white, or purple) and go back and forth between colours (e.g. white to pink, back to white) for several minutes or even an hour or two.
-
- See this video of colour changes in the nipple.
-
- Note: colour changes on their own (without pain) are not a concern.
- Note: colour changes on their own (without pain) are not a concern.
- Because of a lack of blood flow to the nipple, healing of nipple damage/wounds may be delayed
Causes of vasospasm:
- Any cause of nipple pain, like a less than adequate latch or pulling at the breast (as in decreased milk flow), can be associated with vasospasm.
Treatment of vasospasm:
Note: vasospasm is often diagnosed as a Candida infection (yeast, fungus) because some of the symptoms are said to be similar. We recommend trying the suggestions below before trying treatments for yeast. Candida infections of the nipples are over-diagnosed.
1. Improve the latch. Almost all nipple soreness is due to a less than adequate latch, or made worse by a less than adequate latch. See information sheet “Latching and Feeding Management”. Try the latch quiz.
2. Air-drying the nipples, often recommended for other causes of sore nipples, may actually increase vasospasm because of the cool air.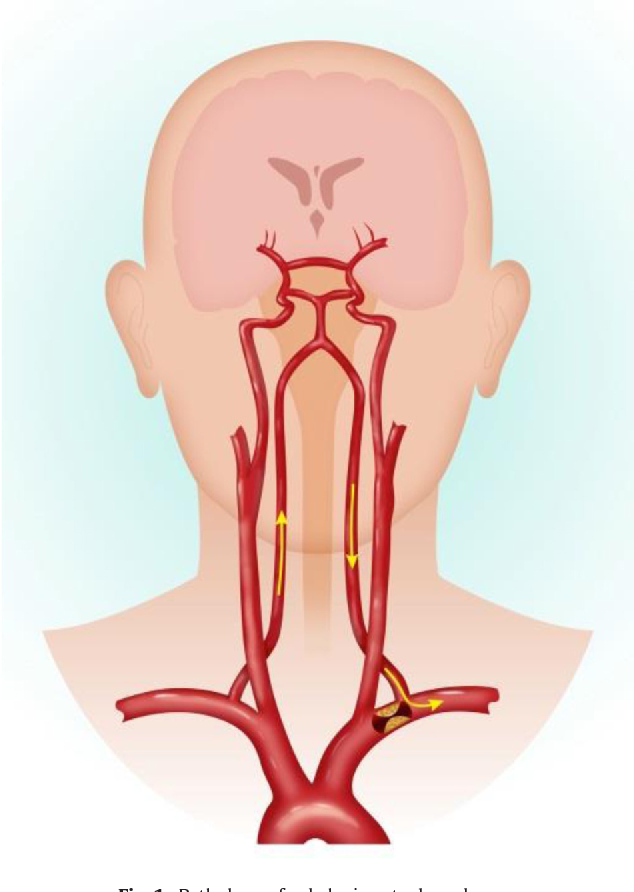 We see more cases of vasospasm in summer than in winter, presumably because of air conditioning.
We see more cases of vasospasm in summer than in winter, presumably because of air conditioning.
3. Keep your nipples/breasts warm. Exposing the nipple to cooler air after it has been inside the baby’s warm mouth often triggers vasospasm. When baby comes off the breast, immediately cover the nipple with your warm hand while you get your bra done up. After taking a shower, wrap a towel around your breasts before stepping out of the shower enclosure. Wool breast pads keep the nipples warmer than regular cotton or disposable pads. You can also apply dry heat to nipples/breasts by using a heating pad or hot water bottle over your clothes.
4. All Purpose Nipple Ointment or olive oil. If using the All Purpose Nipple Ointment, warm a small amount between your fingers, reach inside your bra and squeeze and massage the areola. The same can be done with plain olive oil as an alternative.
5. Pectoral muscle massage. Massage the chest muscles below the collarbone and above the breasts after the feedings or at the onset of nipple or breast pain. The massage should be very vigorous and firm and should be done for 60 seconds on each side. You can also massage under or between the breasts or in her armpits, but this massage should be done gently.
The massage should be very vigorous and firm and should be done for 60 seconds on each side. You can also massage under or between the breasts or in her armpits, but this massage should be done gently.
6. Stretching. If there is pain in the breast, stretching the muscles around the breast throughout the day can help keep blood flowing more easily. Lift one arm to shoulder height or slightly lower and press it back/behind you. Hold the stretch while taking a couple of deep breaths. Do the stretch twice with each arm – once with your palm facing forward and once with it facing back. Use the photos below as a guide.
If there is little or no improvement: (skip to point 9 below as we have generally stopped using the treatments in point 7 and 8). Though 7 and 8 do seem to work, we recommend these only if the mother cannot take nifedipine for some reason. Though nifedipine is often used for high blood pressure, having a normal blood pressure does not mean you cannot take it.
7. Vitamin B6 in a B vitamin complex. Vitamin B6 seems to work best for vasospasm when it is taken as part of a B complex of vitamins that includes niacin. Take 100 mg of B6, in the complex, twice a day. The amount of B6 in each capsule will be listed on the bottle’s label. So, for example, if the overall capsule is 125 mg of B complex and there is only 50 mg of B6 in that capsule, then you would need to take two capsules, two times a day. If there is no significant improvement within one week, stop the B complex. If the B complex decreases the pain, continue taking it until your pain has been stable (or you have been pain-free) for 2 weeks, and then stop.
8. Magnesium can help relax muscles and blood vessels. A magnesium supplement can be especially helpful if there is vasospasm pain in the breasts. Take 250 to 300 mg of magnesium, twice a day. There are different forms of magnesium available as supplements – look for magnesium bisglycinate or magnesium citrate, as they are better absorbed and less likely to cause loose stool than others. If there is no significant improvement within 3 to 4 weeks, stop the magnesium supplement. If the magnesium decreases the pain, continue taking it until your pain has been stable (or you have been pain-free) for 2 weeks, and then stop.
If there is no significant improvement within 3 to 4 weeks, stop the magnesium supplement. If the magnesium decreases the pain, continue taking it until your pain has been stable (or you have been pain-free) for 2 weeks, and then stop.
9. Nifedipine (or other medication which causes relaxation of blood vessels). Nifedipine is a prescription drug used for high blood pressure. One 30 mg tablet of the slow release formulation once a day often almost always takes away the pain of vasospasm completely. After two weeks, we recommend you stop the medication. If pain returns (about 10% of the time), start it again. After two more weeks, stop the medication. If pain returns (which is uncommon), start it again.
In resistant cases, we have prescribed nifedipine 30 mg of the slow release twice a day.
If necessary nifedipine can be used long term. Side effects are uncommon, but headache is not rare. The dose can be increased if 1 tablet is insufficient (contact us for more information).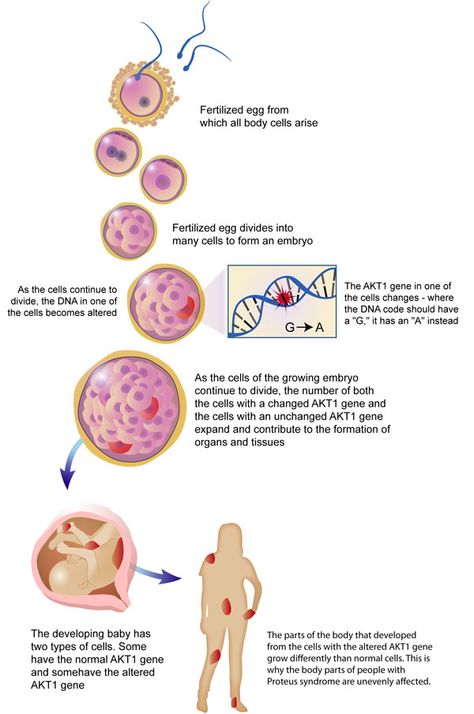 Nifedipine may be used in conjunction with all of the other treatments listed above.
Nifedipine may be used in conjunction with all of the other treatments listed above.
The information presented here is general and not a substitute for personalized treatment from an International Board Certified Lactation Consultant (IBCLC) or other qualified medical professionals.
This information sheet may be copied and distributed without further permission on the condition that it is not used in any context that violates the WHO International Code on the Marketing of Breastmilk Substitutes (1981) and subsequent World Health Assembly resolutions. If you don’t know what this means, please email us to ask!
©IBC, updated November 2016, 2021
Questions or concerns? Email Dr. Jack Newman (read the page carefully, and answer the listed questions).
Make an appointment at the Newman Breastfeeding Clinic.
Breast deformity, nipple retraction - diagnosis of causes, treatment in a clinic in Moscow
Consult a mammologist
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Contents
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Specialists of the Clinical Hospital on Yauza carry out an accurate diagnosis of the causes of breast deformity and nipple retraction using mammography (digital X-ray, MRI), ductography, ultrasound, biopsy, and laboratory tests. We prescribe effective conservative and surgical treatment of the underlying disease according to individually designed schemes.
Breast deformity and nipple retraction can be both congenital features and indicate the development of a pathological process, including breast cancer.
Causes of breast deformity, nipple retraction
Breast fibroadenoma
Breast fibroadenoma is one of the most common benign breast tumors. This is a nodular formation of a rounded shape, limited from the surrounding tissues. Leaf-shaped fibroadenoma can lead to significant breast deformity. The tumor develops rapidly and reaches a large size - up to 20 cm in diameter, causing a change in skin color.
This is a nodular formation of a rounded shape, limited from the surrounding tissues. Leaf-shaped fibroadenoma can lead to significant breast deformity. The tumor develops rapidly and reaches a large size - up to 20 cm in diameter, causing a change in skin color.
Lipomas
Lipoma is a benign breast tumor of non-epithelial origin. These are soft, lobular formations, sometimes painful. Lipomas can be located above the gland or have deep localization, significantly deforming the breast.
Breast cancer
Breast cancer is the most common malignant disease in women. In the later stages, it is externally manifested by wrinkling of the skin over the tumor, discoloration of the skin, deformity of the mammary gland, retraction of the nipple. Men most often suffer from a scirrhous form of cancer (fibrous, dense, from stromal cells), which also leads to deformity of the breast.
Breast lesions
Bruises and burns are the most common traumatic injuries.
Contusions cause hematomas. Deeply located hematoma can cause the development of pseudocysts, suppuration, limited fat necrosis, lipogranuloma, scarring. Thus, there is a deformation of the mammary gland, retraction of the skin, and can even cause cancer.
Burns of the mammary glands - the cause of necrosis of glandular tissue, scarring and deformity of the breast.
Breast tuberculosis
Tuberculosis bacteria can enter the mammary glands through the milk ducts, through the lymphatic tract, or through the hematogenous route (through the blood). If, in tuberculosis, the development of connective tissue dominates in the mammary gland, there is a thickening and deformation of the breast, retraction of the nipple, fistulas, ulcerations may appear.
Breast actinomycosis
This is a rare fungal disease. Small nodules appear in the mammary gland, from which an infiltrate is formed, fistulas and ulcers are formed. At a late stage of the development of the disease, tissue sclerosis occurs, which leads to deformation of the mammary gland.
At a late stage of the development of the disease, tissue sclerosis occurs, which leads to deformation of the mammary gland.
Breast cysts
Breast cyst is a pathological cavity with liquid contents. If left untreated, the cyst can grow large. Large cysts lead to deformation of the mammary gland.
Congenital deformities of the mammary gland
Breast deformities can be congenital. You can call aplasia (absence of glandular tissue), hypoplasia (insufficient formation and development). In addition, congenital retraction of the nipple occurs.
Diagnosis of causes of breast deformity, nipple retraction
- Mammologist's consultation. A mammologist at the Yauza Clinical Hospital will conduct a visual examination of the mammary gland, palpation, ask the patient about symptoms, the history of the disease, etc., and decide whether it is necessary to consult other specialists of our clinic.

- 2. Instrumental tests:
- breast ultrasound;
- ductography;
- digital and MR mammography.
- Lab tests:
- biopsy of breast tissue with histological examination;
- cytological examination of a smear discharged from the chest;
- study of hormonal levels;
- genetic study (risk of developing breast cancer).
- 4. Drawing up an individual treatment program.
Treatment of breast deformity, nipple retraction
The treatment program depends on the cause of the detected breast deformity and nipple retraction. The main thing when pathological symptoms appear is to immediately contact a mammologist, who will conduct an examination, determine the examination scheme and subsequent treatment.
We have all the possibilities for early diagnosis and treatment of a wide range of breast diseases at the modern level.
Cost of services
Prices for services you can see in the price list or check by phone listed on the site.
Attention! Website prices may vary.
Please check the current cost with the administrators by phone.
MAKE AN APPOINTMENT. WE WORK WITHOUT DAYS OFF
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Hospital shares
Stock
Oral hygiene for only 1500 rubles!
09/22/2022
Stock
30% discount for appointments after CT, MRI
08/09/2022
Stock
20% discount on endoscopic examination of the gastrointestinal tract!
09.08.2022
All shares
Our programs
Age-APA
Check-APs in areas of
“Endocrinologist Supplies
Clinics
more than 100
specialists
Over 35,000
satisfied clients
Inpatient facility
with 15 beds
Over 30
specialties
Breast contusion | Arktika-N LLC (Arktika-N Medical Center)
Created: July 9, 2018
Oncologist, surgeon at Arktika-N Medical Center Allahyarov Tengiz Chingizovich.
Bruising of the mammary glands is a closed traumatic injury to the tissues of the mammary gland. Most often, a bruise of the mammary glands occurs in everyday life during a fall, car accidents, bumps in transport and during sports games. A bruise of the mammary glands is accompanied by pain, the formation of a site of compaction and hematoma. Diagnosis of a bruise is based on the presence of a history of trauma, ultrasound of the mammary glands, mammography. Treatment of bruised mammary glands is often carried out conservatively; with a large hematoma, its puncture aspiration or removal (sectoral resection of the mammary gland) is performed.
Traumatic injuries of the mammary glands can be closed and open, isolated or combined. Closed injuries include bruises and hematomas of the mammary glands. Among the open injuries, there may be cut, stab, gunshot, bitten wounds. In mammology, bruises and other injuries of the breast, despite the superficial location of the organ, are rare and account for 1-2% of the entire pathology of the mammary glands. Injuries to the mammary glands can be combined with injuries of the chest - bruises of the ribs, fractures of the ribs and sternum, pneumothorax, hemothorax. Any injury to the mammary glands can be complicated by bleeding, suppuration, and also lead to the development of pain shock.
Injuries to the mammary glands can be combined with injuries of the chest - bruises of the ribs, fractures of the ribs and sternum, pneumothorax, hemothorax. Any injury to the mammary glands can be complicated by bleeding, suppuration, and also lead to the development of pain shock.
Causes of breast injuries
Bruises of the mammary glands are more likely to occur as a result of household injuries - falls on furniture, accidental blows in transport, while playing with children, on doorposts, on the steering wheel in car accidents, etc. Under the influence of a traumatic factor, the integrity of the vessels is violated, which leads to the outflow of blood into the tissues. With minor bruises of the mammary gland, bleeding usually stops spontaneously. Mammary gland tissues are resistant to direct injuries, however, due to the good innervation of the organ, bruises can be accompanied by traumatic shock, especially if the damage occurs in the paraareolar or nipple region.
Open wounds of the mammary glands are most often the result of violence (attempted murder, suicide) or the result of a careless injection or falling on a sharp object. A feature of stab and bitten wounds is their infection with microorganisms resistant to traditional antibacterial drugs, the presence of anaerobic infection, and pathogen polymorphism.
Symptoms of bruising of the mammary glands
As a rule, bruises of the mammary glands are accompanied by the formation of subcutaneous or deep hematoma - a limited accumulation of blood in the soft tissues of the breast. Over time, hematomas can resolve, but quite often, fatty necrosis of the mammary gland forms in their place. In addition, when infected with blood that has poured into the tissue, there is a high probability of suppuration and the formation of an abscess of the mammary gland.
As a result of a contusion of the mammary gland, the patient is concerned about pain and swelling in the chest area, which persist for a long time. Sometimes, when the milk ducts are injured, discharge from the nipple of a transparent nature or containing an admixture of blood may appear.
Sometimes, when the milk ducts are injured, discharge from the nipple of a transparent nature or containing an admixture of blood may appear.
At the site of a bruise of the mammary gland, there is usually an area of compaction that is not dangerous in terms of malignancy. On the other hand, trauma to the mammary glands can be a provoking factor in the growth of another tumor, which has not yet been identified. Many of the patients subsequently diagnosed with breast cancer had a history of breast trauma. Bruises of the mammary glands are especially dangerous when a woman has nodular mastopathy. Replacement of adipose tissue necrosis with scar tissue sometimes leads to skin retraction, breast deformity, which can also be mistaken for breast cancer.
Therefore, any bruise of the mammary glands, hematoma, induration, changes in skin color is a reason to contact a mammologist and conduct a detailed mammological examination.
Diagnosis of breast contusion
After a bruise, it is recommended to conduct an independent examination and palpation of the breast for early detection of hematoma and induration. In the process of self-examination, it is necessary to carry out sequential palpation of each of the sectors of the mammary gland and armpits. Examination of the skin of the breast is best done in front of a mirror. If you detect a change in skin color, a venous pattern, retraction of the nipple or skin, visual or palpation determination of a seal, a nodule, you should immediately contact a specialist.
In the process of self-examination, it is necessary to carry out sequential palpation of each of the sectors of the mammary gland and armpits. Examination of the skin of the breast is best done in front of a mirror. If you detect a change in skin color, a venous pattern, retraction of the nipple or skin, visual or palpation determination of a seal, a nodule, you should immediately contact a specialist.
Intramammary hematoma formed during a bruise of the mammary gland leads to an increase in the volume of the breast and gives the skin a purple or bluish tint. Over time, the hematoma changes color and turns pale ("fades").
Quite often, it is possible to detect the consequences of a bruise of the mammary gland in the thickness of tissues only with the help of instrumental diagnostics. Therefore, a visit to a mammologist is necessary even in the absence of visible and palpable changes. With a bruise of the mammary gland, ultrasound, mammography is performed, in unclear situations - CT or MRI of the mammary glands.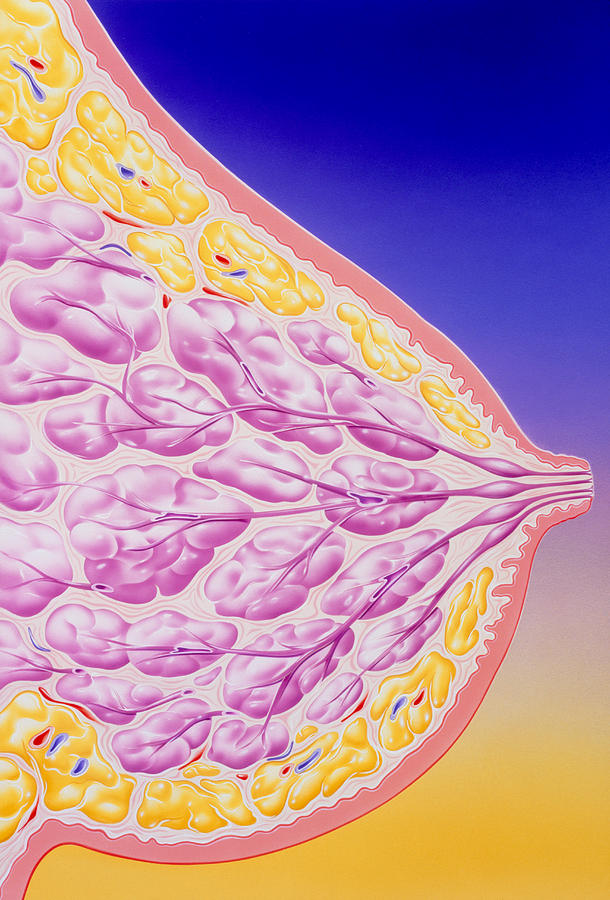
Ultrasound of the mammary glands reveals traumatic edema in the form of reduced tissue echogenicity. Fresh hematomas are initially defined as a homogeneous echo-negative structure, but soon echo-positive signals appear in them - small inclusions of fibrin. Resorption of the hematoma is accompanied by a decrease in its size and a decrease in echogenicity. With an organized hematoma, the formation of high echogenicity with clear boundaries is located.
Mammography for bruises of the mammary glands makes it possible to differentiate post-traumatic changes from neoplastic neoplasms. Radiothermometry with a bruise of the mammary glands allows you to identify the presence of an inflammatory component in the thickness of the tissues.
Treatment of breast contusion
In case of breast contusion, the injured breast is immobilized and fixed with a bandage in an elevated position. In order to stop the pain syndrome, retromammary blockades are performed.