Effect of flu on pregnancy
Influenza (flu) and pregnancy | March of Dimes
It’s safe to get the flu shot. It protects you and your baby from serious health problems during and after pregnancy.
Pregnant women who get the flu are more likely than women who don’t get it to have problems, like preterm labor and premature birth.
If you think you have the flu, call your health care provider right away. Quick treatment can help prevent serious flu complications.
What is the flu?
Influenza (also called flu) is a virus that can cause serious illness. It’s more than just a runny nose and sore throat. The flu can make you very sick, and it can be especially harmful if you get it during or right after pregnancy.
How does the flu spread?
The flu spreads easily from person to person. When someone with the flu coughs, sneezes or speaks, the virus spreads through the air. You can get infected with the flu if you breathe it in or if you touch something (like a door handle or a phone) that has the flu virus on it and then touch your nose, eyes or mouth.
People with the flu may be able to infect others from 1 day before they get sick up to 5 to 7 days after. People who are very sick with the flu or young children may be able to spread the flu longer, especially if they still have symptoms.
How can the flu harm your pregnancy?
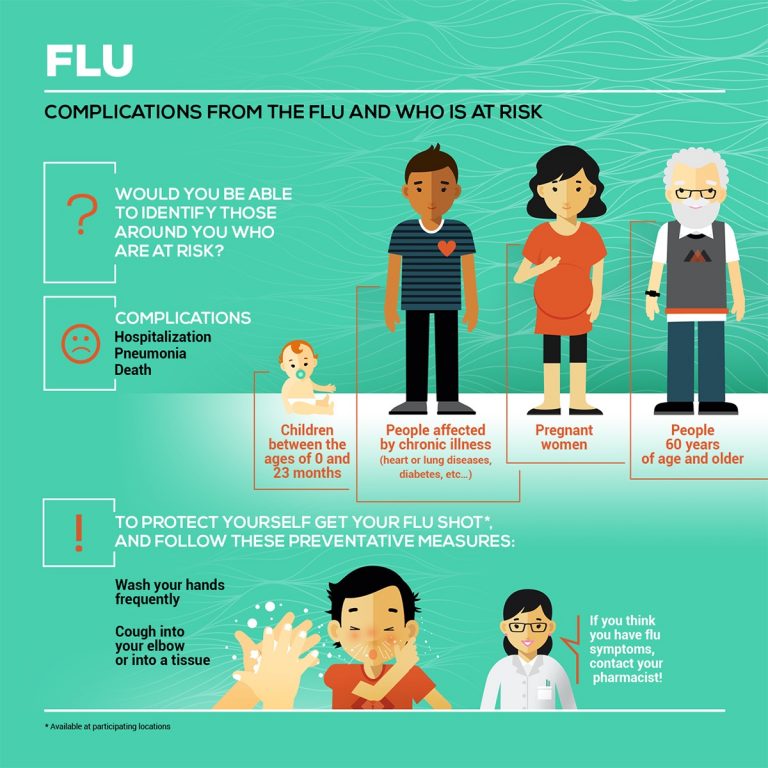
Health complications from the flu, like a lung infection called pneumonia, can be serious and even deadly, especially if you’re pregnant. If you get the flu during pregnancy, you’re more likely than other adults to have serious complications. It’s best to get a flu shot before you get pregnant. Getting a flu shot can help reduce your risk of getting the flu, having serious flu complications and needing treatment in a hospital.
Pregnant women who get the flu are more likely than women who don’t get it to have preterm labor (labor that happens before 37 weeks of pregnancy) and premature birth (birth that happens before 37 weeks of pregnancy. Fever from the flu may be linked to birth defects, like neural tube defects, and other problems in your baby. A birth defect is a health condition that is present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, how the body develops, or in how the body works. Neural tube defects are birth defects of the brain and spinal cord.
A birth defect is a health condition that is present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, how the body develops, or in how the body works. Neural tube defects are birth defects of the brain and spinal cord.
How does the flu shot help protect you from flu?
The flu shot contains a vaccine that helps prevent you from getting the flu. The flu shot can’t cause the flu. It’s safe to get a flu shot any time during pregnancy, but it’s best to get it before flu season (October through May). Even though you’re more likely to get the flu during flu season, you can get it any time of year.
There are many different flu viruses, and they’re always changing. Each year a new flu vaccine is made to protect against three or four flu viruses that are likely to make people sick during the upcoming flu season. Protection from a flu shot only lasts about a year, so it’s important to get a flu shot every year. You can get the shot from your health care provider, and many pharmacies and work places offer it each fall. Use the HealthMap Vaccine Finder to find out where you can get the flu vaccine.
You can get the shot from your health care provider, and many pharmacies and work places offer it each fall. Use the HealthMap Vaccine Finder to find out where you can get the flu vaccine.
Is it safe to get a flu shot during pregnancy?
It’s safe for most pregnant women to get the flu shot. Tell your health care provider if you have any severe allergies or if you’ve ever had a severe allergic reaction to a flu shot. Severe allergic reactions to flu shots are rare. If you’re worried about being allergic to the flu shot, talk to your provider to make sure it’s safe for you.
Some flu vaccines are made with eggs. Most women with egg allergies can get the flu shot. But if you have severe egg allergies, get the shot in a medical setting (like a doctor’s office, hospital or clinic) from a provider who knows how to treat severe allergies and allergic reactions.
Pregnant women should not get the flu nasal spray. This is a spray that’s put in your nose.
What are signs and symptoms of the flu?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing.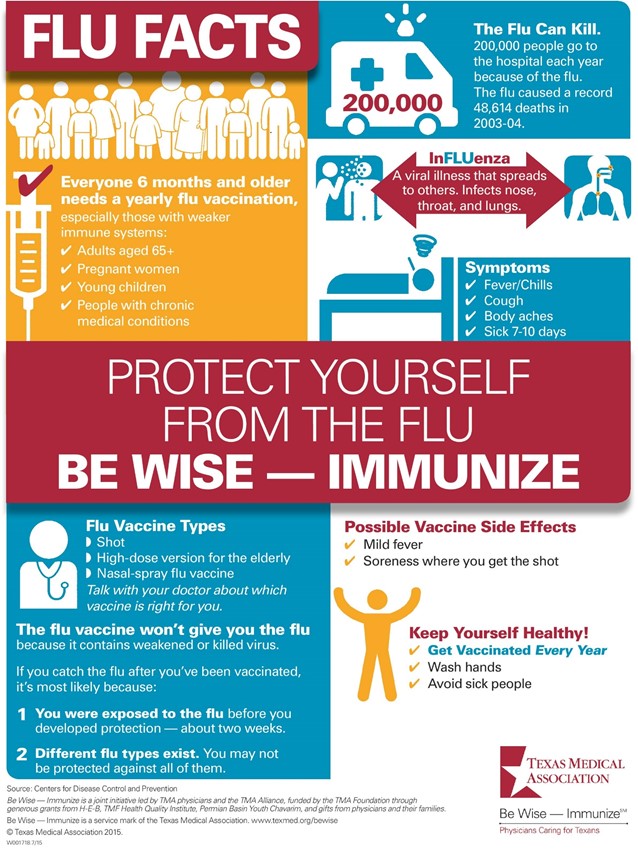 Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Common signs and symptoms of the flu include:
Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Common signs and symptoms of the flu include:
- Being very tired or sleepy (also called fatigue)
- Cough
- Fever (100 F or above), chills or body shakes. Not everyone who has the flu has a fever.
- Headache, or muscle or body aches
- Runny or stuffy nose
- Sore throat
- Vomiting (throwing up) or diarrhea (more common in children)
The flu often comes on quickly. Fever and most other symptoms can last a week or longer. But some people can be sick from the flu for a long time, including children, people older than 65, pregnant women and women who have recently had a baby.
Call 911 and get medical care right away if you have any of these signs or symptoms:
- Feeling your baby move less or not at all
- High fever that doesn’t go down after taking acetaminophen (Tylenol®). Don’t take any medicine without checking with your provider first.

- Pain or pressure in the chest or belly
- Sudden dizziness or confusion
- Trouble breathing or shortness of breath
- Vomiting that’s severe or doesn’t stop
- Flu signs or symptoms that get better but then come back with fever and a worse cough
How is the flu treated during pregnancy?
If you think you have the flu even if you’ve been vaccinated, call your health care provider right away. She may prescribe an antiviral medicine to help prevent or treat the flu. Antivirals kill infections caused by viruses. They can make your flu milder and help you feel better faster. Antivirals also can help prevent serious flu complications, like pneumonia. For flu, antivirals work best if you take them within 2 days of having symptoms. Quick treatment with antiviral medicine can help prevent serious flu complications.
If you’ve had close contact with someone who has the flu during your pregnancy or in the 2 weeks after giving birth, tell your health care provider. Even if you don’t have signs or symptoms of flu, your provider may want to treat you with an antiviral medicine to help prevent you from getting the flu and having serious complications.
Even if you don’t have signs or symptoms of flu, your provider may want to treat you with an antiviral medicine to help prevent you from getting the flu and having serious complications.
Three medicines are approved in the United States to prevent or treat the flu in pregnant women and women who recently had a baby. Talk to your provider about which one is right for you:
- Oseltamivir (brand name Tamiflu®).This medicine comes as a capsule or liquid.
- Zanamivir (brand name Relenza®). This medicine is a powder that you breathe in by mouth. It isn’t recommended for people with breathing problems, like asthma.
- Peramivir (Rapivab®). This medicine is given through a needle into a vein (also called IV) by a health care provider.
If you have a fever, call your provider as soon as possible and ask about taking acetaminophen. If you have the flu, get lots of rest and drink plenty of fluids. You may not want to eat much. Try eating small meals to help your body get better.
How can you stop the flu from spreading?
When you have the flu, you can spread it to others. Here’s what you can do to help prevent it from spreading:
- Stay home when you’re sick and limit contact with others.
- Don’t kiss anyone.
- Cough or sneeze into a tissue or into your arm. Throw used tissues in the trash.
- Try not to touch your eyes, nose or mouth.
- Wash your hands with soap and water before touching anyone. You also can use alcohol-based hand sanitizers. Use enough hand sanitizer so that it takes at least 15 seconds for your hands to dry.
- Use hot, soapy water or a dishwasher to wash your dishes and utensils.
- Don’t share your dishes, glasses, utensils or toothbrush.
Why is the flu so harmful during pregnancy?
The flu can be dangerous during pregnancy because pregnancy affects your immune system, heart and lungs. Your immune system is your body’s way of protecting itself from illnesses and diseases. When your body senses something like a virus that can harm your health, your immune system works hard to fight the virus.
When your body senses something like a virus that can harm your health, your immune system works hard to fight the virus.
When you’re pregnant, your immune system isn’t as quick to respond to illnesses as it was before pregnancy. Your body knows that pregnancy is OK and that it shouldn’t reject your baby. So, your body naturally lowers the immune system’s ability to protect you and respond to illnesses so that it can welcome your growing baby. But a lowered immune system means you’re more likely get sick with viruses like the flu.
Another reason the flu can be harmful during pregnancy is that your lungs need more oxygen, especially in the second and third trimesters. Your growing belly puts pressure on your lungs, making them work harder in a smaller space. You may even find yourself feeling shortness of breath at times. Your heart is working hard, too. It’s busy supplying blood to you and your baby. All of this means your body is stressed during pregnancy. This stress on your body can make you more likely to get the flu. If you’re pregnant or had a baby within the last 2 weeks, you’re more likely than other women to have serious health problems from the flu.
If you’re pregnant or had a baby within the last 2 weeks, you’re more likely than other women to have serious health problems from the flu.
More information
Centers for Disease Control and Prevention Pregnant women & Influenza
Flu.gov
See also: Flu and your baby, Vaccinations and pregnancy
Last reviewed: September, 2019
Pregnancy and the flu: MedlinePlus Medical Encyclopedia
During pregnancy, it is harder for a woman's immune system to fight infections. This makes a pregnant woman more likely to get the flu and other diseases.
Pregnant women are more likely than nonpregnant women their age to become very ill if they get the flu. If you are pregnant, you need to take special steps to stay healthy during the flu season.
This article gives you information about the flu and pregnancy. It is not a substitute for medical advice from your health care provider. If you think you have the flu, you should contact your provider's office right away.
WHAT ARE THE SYMPTOMS OF FLU DURING PREGNANCY?
Flu symptoms are the same for everyone and include:
- Cough
- Sore throat
- Runny nose
- Fever of 100°F (37.8°C) or higher
Other symptoms may include:
- Body aches
- Headache
- Fatigue
- Vomiting, and diarrhea
SHOULD I GET THE FLU VACCINE IF I AM PREGNANT?
If you are pregnant or thinking about becoming pregnant, you should get the flu vaccine. The Centers for Disease Control and Prevention (CDC) considers pregnant women at a higher risk for getting the flu and developing flu-related complications.
Pregnant women who get the flu vaccine get sick less often. Getting a mild case of the flu is often not harmful. However, the flu vaccine can prevent the severe cases of the flu that can harm mother and baby.
Flu vaccines are available at most provider offices and health clinics. There are two types of flu vaccines: the flu shot and a nose-spray vaccine.
- The flu shot is recommended for pregnant women. It contains killed (inactive) viruses. You cannot get the flu from this vaccine.
- The nasal spray-type flu vaccine is not approved for pregnant women.
It is OK for a pregnant woman to be around somebody who has received the nasal flu vaccine.
WILL THE VACCINE HARM MY BABY?
A small amount of mercury (called thimerosal) is a common preservative in multidose vaccines. Despite some concerns, vaccines that contain this substance have NOT been shown to cause autism or attention deficit hyperactivity disorder.
If you have concerns about mercury, ask your provider about a preservative-free vaccine. All routine vaccines are also available without added thimerosal. The CDC says pregnant women may get flu vaccines either with or without thimerosal.
WHAT ABOUT SIDE EFFECTS OF THE VACCINE?
Common side effects of the flu vaccine are mild, but can include:
- Redness or tenderness where the shot was given
- Headache
- Muscle aches
- Fever
- Nausea and vomiting
If side effects occur, they most often begin soon after the shot. They may last as long as 1 to 2 days. If they last longer than 2 days, you should call your provider.
They may last as long as 1 to 2 days. If they last longer than 2 days, you should call your provider.
HOW DO I TREAT THE FLU IF I'M PREGNANT?
Experts recommend treating pregnant women with flu-like illness as soon as possible after they develop symptoms.
- Testing is not needed for most people. Providers should not wait for results of testing before treating pregnant women. Rapid tests are often available in urgent care clinics and provider's offices.
- It is best to start antiviral medicines within the first 48 hours of developing symptoms, but antivirals can also be used after this time period. A 75 mg capsule of oseltamivir (Tamiflu) twice per day for 5 days is the recommended first choice antiviral.
WILL ANTIVIRAL MEDICINES HARM MY BABY?
You may be worried about the medicines harming your baby. However, it is important to realize there are severe risks if you do not get treatment:
- In past flu outbreaks, pregnant women who were otherwise healthy were more likely than those who were not pregnant to become very sick or even die.

- This does not mean that all pregnant women will have a severe infection, but it is hard to predict who will become very ill. Women who become more ill with the flu will have mild symptoms at first.
- Pregnant women can become very sick very fast, even if the symptoms are not bad at first.
- Women who develop a high fever or pneumonia are at higher risk for early labor or delivery and other harm.
DO I NEED AN ANTIVIRAL DRUG IF I HAVE BEEN AROUND SOMEONE WITH THE FLU?
You are more likely to get the flu if you have close contact with someone who already has it.
Close contact means:
- Eating or drinking with the same utensils
- Caring for children who are sick with the flu
- Being near the droplets or secretions from someone who sneezes, coughs, or has a runny nose
If you have been around someone who has the flu, ask your provider if you need an antiviral drug.
WHAT TYPES OF COLD MEDICINE CAN I TAKE FOR THE FLU IF I'M PREGNANT?
Many cold medicines contain more than one type of medicine. Some may be safer than others, but none are proven 100% safe. It is best to avoid cold medicines, if possible, especially during the first 3 to 4 months of pregnancy.
Some may be safer than others, but none are proven 100% safe. It is best to avoid cold medicines, if possible, especially during the first 3 to 4 months of pregnancy.
The best self-care steps for taking care of yourself when you have the flu include rest and drinking plenty of liquids, especially water. Tylenol is most often safe in standard doses to relieve pain or discomfort. It is best to talk to your provider before taking any cold medicines while you are pregnant.
WHAT ELSE CAN I DO TO PROTECT MYSELF AND MY BABY FROM THE FLU?
There are many things you can do to help protect yourself and your unborn child from the flu.
- You should avoid sharing food, utensils, or cups with others.
- Avoid touching your eyes, nose, and throat.
- Wash your hands often, using soap and warm water.
Carry hand sanitizer with you, and use it when you are unable to wash with soap and water.
Influenza and pregnancy. How to avoid disaster?
- Home |
- News |
- Influenza and pregnancy.
 How to avoid disaster?
How to avoid disaster?
09/14/2020 | Number of views: 5584
Influenza is an acute infectious disease of the respiratory tract caused by the influenza virus, which has a high epidemiological and clinical significance, with a high incidence of complications among people at high risk.
The ECDC (European Center for Disease Control and Prevention) guidelines emphasize: “Influenza vaccination is the main strategy for preventing severe and complicated influenza infection, even if the vaccination is less effective than expected.”
Vaccination of pregnant women against influenza with subunit and split vaccines has been routinely performed in Europe and America for more than 20 years, while its immunological efficiency reaches 70-85%. When vaccinating pregnant women against influenza, first of all, the goal is to eliminate or limit the possibility of infection in the event of an epidemic contact between a woman and a sick person. In the post-vaccination period, specific immunity is formed in women with its subsequent transfer to the fetus and newborn.
In the Russian Federation, the issue of influenza vaccination has always been relevant, but it arose especially acutely in connection with the events of the pandemic threat of 2009-2010. It was then that low-reactogenic domestic and foreign vaccines that did not contain live or killed viruses were first used, which largely made it possible to avoid the severe consequences of an influenza epidemic among pregnant women.
In Russia, as in other countries, the main burden of influenza A/h2N1/ fell on school-age children and young adults. According to official figures, out of 531 deaths from laboratory-confirmed influenza, 79.4% accounted for the age of 18-53 years, 4.5% - for children 0-17 years old and 3.0% - for persons 65 years of age and older. The number of deaths during the influenza A/h2N1/ epidemic was 50-100 times higher than the number of deaths in the epidemic of the last two decades. An analysis of cases of death from laboratory-confirmed influenza revealed that the most common aggravating circumstances were diseases of the endocrine system - 9. 2%, including obesity - 5.8%, immunodeficiency states, including HIV, blood diseases and neoplasms - 5.3 %, as well as diseases of the cardiovascular system - 6.4%, pregnancy - 4.5%, chronic lung diseases - 3.6%.
Pregnant women are at high risk for the adverse course of respiratory infections, among which influenza is the leading disease, often ending tragically for the pregnant woman herself and her unborn child.
Extremely severe forms of influenza in pregnant women with a high mortality rate observed during pandemics of the 20th century are described. The influenza A/h3N2/1957 pandemic in a number of cities in the United States of America killed more than 50% of women at different stages of pregnancy, which accounted for up to 10% of all deaths from this infection during the epidemic season.
Epidemiological observations of the incidence of influenza in highly developed countries over the past 20 years during peak seasons have shown more frequent hospitalizations of pregnant women compared to ordinary women.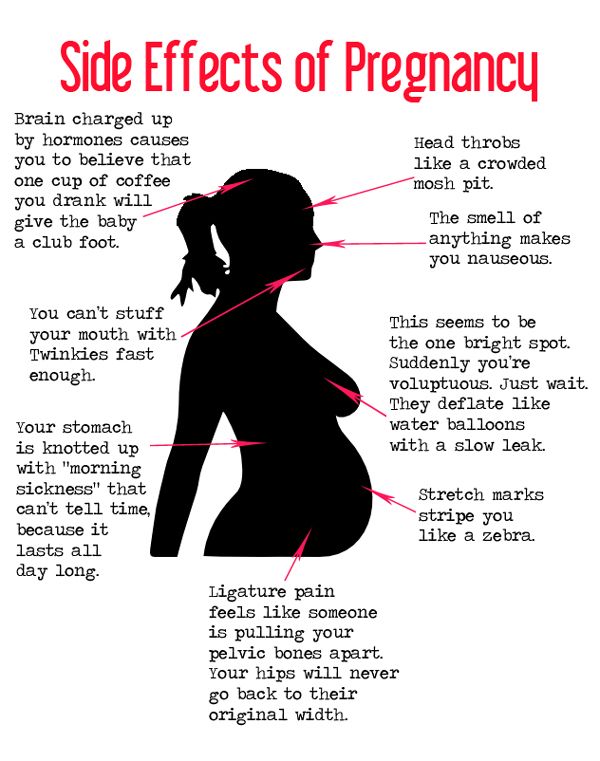 So, in Canada, up to 60% of pregnant women with influenza needed hospitalization due to the development of severe respiratory complications. Events caused by the latest influenza pandemic caused by the circulation of the A/California/7/2009(h2N1) virus showed that in Europe and North America the need for hospitalization of pregnant women ranged from 4.3% (Ireland) to 13% (USA) of all influenza-related hospitalizations in the population. About 60% of sick women needed intensive therapeutic measures. Most often, pregnant women were hospitalized in the second or third trimesters of pregnancy, and up to 51% of them had various aggravating concomitant diseases.
So, in Canada, up to 60% of pregnant women with influenza needed hospitalization due to the development of severe respiratory complications. Events caused by the latest influenza pandemic caused by the circulation of the A/California/7/2009(h2N1) virus showed that in Europe and North America the need for hospitalization of pregnant women ranged from 4.3% (Ireland) to 13% (USA) of all influenza-related hospitalizations in the population. About 60% of sick women needed intensive therapeutic measures. Most often, pregnant women were hospitalized in the second or third trimesters of pregnancy, and up to 51% of them had various aggravating concomitant diseases.
Mortality among pregnant women with severe influenza infection caused by the A/California/7/2009(h2N1) virus varied from 0.7% (Greece) to 6.9% (UK) in different countries. For the entire pandemic period in England, mortality among pregnant women was 90 per 100,000 clinical cases. In Australia and the United States, the proportion of pregnant women who died of all pandemic influenza deaths ranged from 1.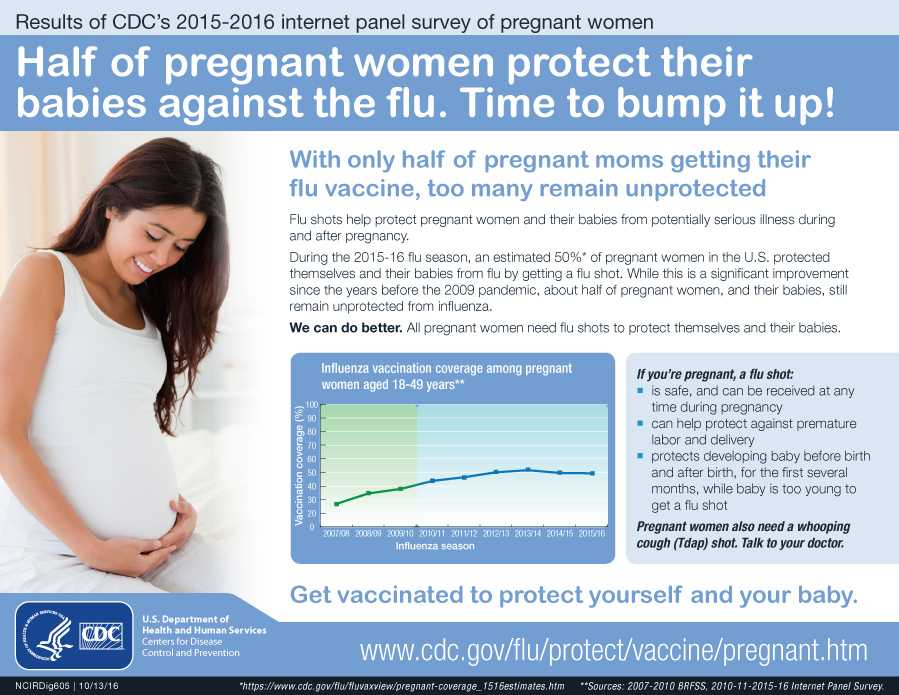 6% to 16%. In Russia, this figure was 0.22 - 0.3% of all pregnant women, increasing maternal mortality to 15.8%. Most deaths occur in the third trimester of pregnancy, as the most critical period of pregnancy for a woman in terms of the difficult to predict outcome of influenza.
6% to 16%. In Russia, this figure was 0.22 - 0.3% of all pregnant women, increasing maternal mortality to 15.8%. Most deaths occur in the third trimester of pregnancy, as the most critical period of pregnancy for a woman in terms of the difficult to predict outcome of influenza.
Pregnant women have a higher susceptibility to the influenza virus - the incidence is 3.78 per 1000 (according to 2015-2016), in non-pregnant women of childbearing age - 0.2 per 1000. 18 times higher!
All this increases the rate of hospitalization by 3-10 times compared with non-pregnant populations.
The number of hospitalized pregnant women with respiratory influenza-like illness increases with the duration of pregnancy (1.4% in the second trimester and 4.7% in the third trimester). Moreover, healthy women in the third trimester of pregnancy have the same risk of severe respiratory infection as non-pregnant women with chronic comorbidities.
Perinatal mortality is more common among infants born to influenza-infected women (39 per 1,000 births) compared to those of non-influenza-infected mothers (7 per 1,000 births). The risk of having a child with congenital malformations in pregnant women with influenza A (h2N1) 09 is 5.8 times greater than in those who did not have influenza.
The risk of having a child with congenital malformations in pregnant women with influenza A (h2N1) 09 is 5.8 times greater than in those who did not have influenza.
High perinatal mortality is due to an increase in the number of stillbirths, influenza complications in the pregnant woman and the fetus in late pregnancy, and premature births.
Women who had preterm labor were more likely to contract influenza in the third trimester of pregnancy, and had a more severe course of infection with a pneumonia clinic and the need for hospitalization in an intensive care unit. The course of influenza in the third trimester of pregnancy was more often an indication for delivery by caesarean section. Influenza in the second and third trimesters of pregnancy creates a high risk of severe disease and complications (acute cerebrovascular accident, pneumonia, myocarditis, postpartum hemorrhage).
Trivalent inactivated vaccines have been developed to prevent influenza and are recommended for women whose pregnancy coincides with influenza season.
In 2005 regulations, the World Health Organization (WHO) calls on all countries to vaccinate all pregnant women during the flu season.
To understand the feasibility and safety of influenza vaccination in pregnant women and children, a number of independent studies have been conducted among large groups of children of different ages and women at different stages of pregnancy. Based on the results obtained, reports were generated that formed the basis of the ECDC consensus document, created for the correct and informed decision on the regular vaccination of healthy children and pregnant women with the seasonal influenza vaccine.
Annual influenza vaccination of all pregnant women has no contraindications. Post-vaccination complications in pregnant women were not registered.
World Health Organization's case for vaccination:
vaccination can reduce influenza-related hospitalizations and deaths among pregnant women;
vaccination during pregnancy may potentially reduce the occurrence and severity of influenza in infants younger than six months of age for whom influenza vaccination and specific antiviral treatment are not available;
the use of antiviral therapy and vaccination against influenza in children under six months of age is not acceptable, so the lack of an alternative to effective protection against possible infection and severe consequences of the disease in infants makes vaccination of the expectant mother a priority;
Influenza vaccination may reduce a pregnant woman's need for antivirals, which are more dangerous than inactivated vaccines. In addition, antiviral drugs are expensive, while influenza vaccination is provided free of charge under the MHI policy;
In addition, antiviral drugs are expensive, while influenza vaccination is provided free of charge under the MHI policy;
the vaccine is effective enough to reduce the risk of influenza complications such as secondary bacterial infections. This situation is especially relevant today, when the resistance of bacteria to antibiotics is growing, as well as in women with intolerance to antibacterial drugs.
Currently, large-scale pre-season immunization of the population against influenza is being carried out in the Republic of Mordovia. As of mid-September 2020, about 151 thousand people have already been vaccinated, which is 31.8% of the planned or 19.1% of the population of the republic.
Preservative-free inactivated influenza vaccine (Sovigripp) is available in sufficient quantities to immunize pregnant women in the second and third trimesters. 199 pregnant women have already been vaccinated in the republic (over the previous season, about 300 pregnant women were vaccinated). However, this indicator is not sufficient and raises the medical community's concern for the life and health of pregnant women and newborns in the 2020-2021 influenza season.
However, this indicator is not sufficient and raises the medical community's concern for the life and health of pregnant women and newborns in the 2020-2021 influenza season.
To vaccinate a pregnant woman, it is enough to contact a local therapist at the clinic at the place of residence, get a vaccination permit and get a free flu shot, protecting herself and her unborn baby from the severe consequences of one of the most formidable infectious diseases of our time.
Chief Freelance Epidemiologist
Ministry of Health of the Republic of Mordovia
Chumakov Mikhail Eduardovich
Influenza and SARS in pregnant women
HomeFor PatientsInformation Influenza and SARS in pregnant women
Viral infections are now regarded as one of the main causes of reproductive losses. On the one hand, the infectious agent has a direct damaging effect on the fetus, and on the other hand, causing significant changes in the immune responses of the mother's body, leads to a complicated course of pregnancy. A special place among infectious diseases of pregnant women is occupied by influenza and other acute respiratory viral infections transmitted by airborne droplets.
A special place among infectious diseases of pregnant women is occupied by influenza and other acute respiratory viral infections transmitted by airborne droplets.
The urgency of the problem of acute respiratory diseases of a viral nature is determined by their prevalence, uncontrollability, high contagiousness, allergization and the development of secondary immunodeficiency states after an illness.
The environmental features of modern urbanization provide a real basis for the frequent encounter of women with various respiratory viruses during the entire period of pregnancy. In extragenital pathology of pregnant women, acute respiratory infections occupy the first place in terms of prevalence - more than 2/3 of the total incidence of acute infections. This is due to the high susceptibility of pregnant women to viral infections, the tendency to chronicity of pathological processes, which is due to the peculiarities of the immunity of pregnant women.
The impact of viral infection on the course of pregnancy and the condition of the fetus is characterized by two main mechanisms. Firstly, the possible infection of the placenta, amniotic membranes, as well as the fetus itself, teratogenic (causing malformations) effect on the embryo and fetus, the development of local lesions of the fetus, as well as infection of the fetus with clinical manifestations in the postnatal period (after birth). Secondly, a possible indirect effect as a result of the development of a pregnant fever, a violation of homeostasis (balance, constancy) in the body, etc. , and the fetus.
Firstly, the possible infection of the placenta, amniotic membranes, as well as the fetus itself, teratogenic (causing malformations) effect on the embryo and fetus, the development of local lesions of the fetus, as well as infection of the fetus with clinical manifestations in the postnatal period (after birth). Secondly, a possible indirect effect as a result of the development of a pregnant fever, a violation of homeostasis (balance, constancy) in the body, etc. , and the fetus.
The main links in the pathogenesis of a viral infection in a pregnant woman, which determine the high risk of perinatal pathology, are:
Activation of the blood coagulation system by the toxic effect of the virus on the vascular wall;
Pathological changes in the immune system resulting from a viral infection;
Activation of chronic intrauterine infection.
The possibility of transmission of respiratory group viruses, which include viruses that cause ARVI, through the placenta from a sick mother to a fetus has been proven, which leads to the involvement of all three components of the "mother-placenta-fetus" system in the infectious process.
Modern researchers consider gestosis (toxicosis of the second half of pregnancy), including its severe forms, as a causal factor in placental insufficiency (PI), a direct relationship between the severity of late gestosis and the severity of PI has been proven. Recent studies have confirmed the assumption that the placenta serves as a kind of "reservoir" in the process of intrauterine infection, as it has been proven that under the influence of viruses, some structures of the placenta change, and viruses reproduce in them.
Specific prophylaxis of influenza does not eliminate the problem of respiratory viral infections, since the share of ARVI of non-influenza etiology is up to 75% even during influenza epidemic periods. In addition, the physiological changes in the immune system that occur in the body of pregnant women do not allow them to use vaccine preparations to prevent infectious diseases.
The risk group for ARVI infection includes women who had the incidence of these infections more than three times in the previous year of pregnancy. This sign is a classic confirmation of immunological deficiency in the patient. They are characterized by: a protracted, recurrent course of diseases (rhinitis, pharyngitis, laryngotracheitis, bronchitis), the presence of foci of chronic infection (chronic tonsillitis, sinusitis). In the pathological process in such patients, to one degree or another, other body systems are also involved, which ensure its protection when it encounters the external environment. The most common pathology of the digestive tract: from dysfunctions and dysbiosis to chronic colitis, enteritis, enterocolitis, pancreatitis and cholecystitis.
This sign is a classic confirmation of immunological deficiency in the patient. They are characterized by: a protracted, recurrent course of diseases (rhinitis, pharyngitis, laryngotracheitis, bronchitis), the presence of foci of chronic infection (chronic tonsillitis, sinusitis). In the pathological process in such patients, to one degree or another, other body systems are also involved, which ensure its protection when it encounters the external environment. The most common pathology of the digestive tract: from dysfunctions and dysbiosis to chronic colitis, enteritis, enterocolitis, pancreatitis and cholecystitis.
Features of the course of acute respiratory viral infections in pregnant women
Pregnant women are characterized by a protracted course of acute respiratory viral infections in the absence of severe clinical manifestations. This is due to the ability of respiratory group viruses to reproduce in the placenta, as well as the peculiarity of the immune system of the pregnant woman (a state of physiological immunodeficiency).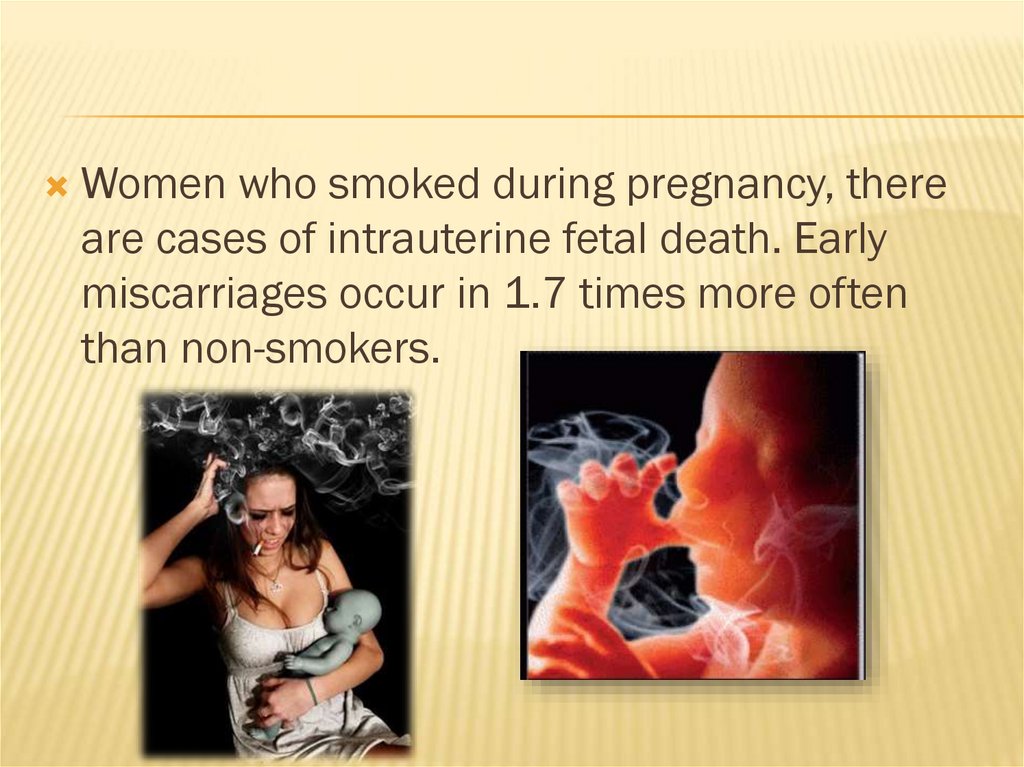
The main clinical symptoms of acute respiratory infections: symptoms of general intoxication (malaise, weakness, increased fatigue, etc.) against the background of subfebrile or normal temperature, symptoms of rhinitis or nasopharyngitis.
The most typical ARVI clinic for pregnant women is often the reason for insufficient attention to the very fact of the disease, both on the part of doctors and the woman herself, however, ARVI leads to a breakdown in physiological immune mechanisms and does not exclude the possibility of complications during pregnancy.
Features of pregnancy after SARS. Influence of ARVI in pregnant women on the health of their newborns
The most typical complications of pregnancy after ARVI are:
- more than double the incidence of placental insufficiency;
- increase in cases of early onset of preeclampsia;
- oligohydramnios - as a concomitant sign of placental insufficiency, as well as a manifestation of a viral lesion of the fetoplacental complex;
- the threat of premature termination of pregnancy is more common in the 2nd trimester, namely at 17-26 weeks, for pregnant women after ARVI, a constant course of the threat of termination of pregnancy is characteristic, insensitive to the ongoing standard therapy;
- intrauterine growth retardation and intrauterine fetal hypoxia;
- increase in neonatal morbidity:
- hypoxic damage to the central nervous system is most characteristic of acute respiratory viral infections in the 2nd trimester;
- chronic placental insufficiency (inflammatory and degenerative changes in the placenta, impaired differentiation of placental tissue, suppression of compensatory-adaptive vascular reactions of chorionic villi).
Characteristics of the state of the immune system of pregnant women after SARS
In the study of the state of systemic immunity in pregnant women who had ARVI, depending on the duration of pregnancy, in comparison with similar indicators in healthy pregnant women, the following patterns were revealed.
Past ARVI causes changes in the immune status, is characterized, as a rule, by changes in the content of leukocytes and lymphocytes and their populations. A characteristic sign of the immunogram of pregnant women who have had ARVI is lymphocytopenia (destruction of lymphocytes), while during the physiological development of pregnancy, an increase in the total number of leukocytes occurs. Lymphocytopenia can be explained by the direct damaging effect of respiratory viruses on lymphoid cells, its degree depends both on the virulent properties of the viral pathogen and on the adaptive capabilities of the organism.
The effect of viruses on immunological reactivity lies in the fact that in the course of infection, not one, but a series of indicators characterizing the immune response of the organism affected by the virus to foreign antigens changes. There is a disorder of immunological reactivity, caused by a violation of all the functions of immunocompetent cells as a result of the reproduction of the virus.
There is a disorder of immunological reactivity, caused by a violation of all the functions of immunocompetent cells as a result of the reproduction of the virus.
The occurrence of defects in immunological reactivity should be considered as an essential element of the pathogenesis of ARVI. The presence of these defects does not prevent the formation of specific immunity against the homologous virus.
Methods of prevention and treatment of acute respiratory viral infections in pregnant women
It is known that specific prevention of influenza and acute respiratory viral infections by vaccine preparations is contraindicated during pregnancy. Researchers both here and abroad pay attention to the search and implementation in practice of methods of non-specific protection of the population from respiratory viral infections. It should be noted that one of the most promising methods of viral infection tactics is immunocorrection. From this point of view, the use of modern immunobiological preparations, adaptogens and eubiotics, is promising.
Therapeutic measures with the use of immunotropic drugs are carried out after ARVI in the 2nd - 3rd trimesters of pregnancy, as well as 10-14 days before the expected date of delivery in the following groups of patients:
- diseases more than 3 times in the previous year of pregnancy;
- pregnant women who had ARVI with a complicated course of pregnancy;
- in the presence of a positive prognosis for the development of perinatal pathology.
Preventive measures
All pregnant women should refrain as much as possible from visiting public places with a large crowd of people in case of a threat and the emergence of an epidemic of influenza and SARS.
Pregnant women with acute respiratory infections three or more times in the year preceding pregnancy should be classified as a high risk group for the development of complications.
This group of patients, as well as all pregnant women with the threat and occurrence of an epidemic of influenza and ARVI, need to undergo a course of non-specific prophylaxis.