Does pregnancy cause migraines
Migraines & Headaches During Pregnancy: Causes and Treatment
Written by Rebecca Buffum Taylor
In this Article
- Causes of Migraine Headaches
- Tracking Triggers With a Migraine Diary
- Tests for Migraines
- Self-Care of Migraines
- Medications for Migraines
- Acute Migraine Treatment
- Preventive Migraine Treatment
If you're pregnant, you're no doubt experiencing new aches and pains. If you're also one of the millions of pregnant women who experience migraines, you might be glad to know that pregnancy eases migraine headache symptoms for many women. But even if it doesn't for you, the information in this article can help you cope.
Causes of Migraine Headaches
Exactly what causes migraine headaches isn't known. But migraines appear to involve changes in nerve pathways, neurochemicals, and blood flow in the brain.
Researchers believe that overly excited brain cells stimulate a release of chemicals. These chemicals irritate blood vessels on the brain's surface. That, in turn, causes blood vessels to swell and stimulate the pain response.
Estrogen is thought to play a role in migraines. That's why pregnancy, menstruation, and menopause often change a woman's pattern of migraine headaches.
The neurotransmitter serotonin also appears to have a key role in migraines.
Tracking Triggers With a Migraine Diary
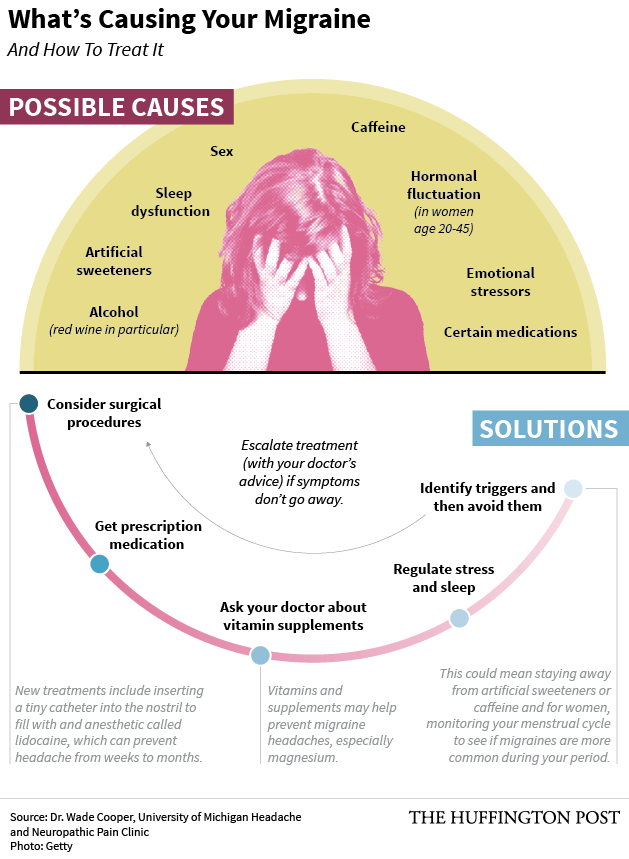
Hormone changes during pregnancy are not the only thing that can trigger migraine headaches. Most women have a combination of triggers. For instance, stress, skipped meals, and lack of sleep may all trigger a migraine. And something that triggers a migraine one day may not bother you at all the next.
Some migraines last a few hours. Others, if left untreated, could last a couple of days. Migraines are quite unpredictable. So while pregnancy may make them worse for one woman, they might completely disappear for another.
A headache diary can let you track your particular triggers.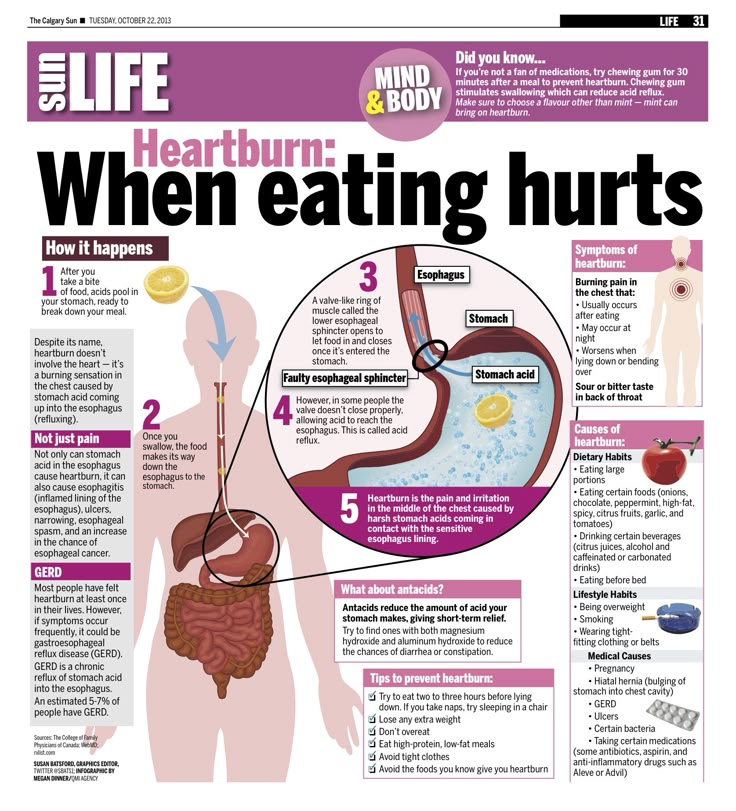 This will help your doctor decide on what treatment will work best to relieve your specific symptoms. It may also help you recognize a pattern that tells you which triggers to avoid while you're pregnant.
This will help your doctor decide on what treatment will work best to relieve your specific symptoms. It may also help you recognize a pattern that tells you which triggers to avoid while you're pregnant.
Each time you have a headache, write down:
- Your specific symptoms: where you feel the pain, what the pain feels like, and any other symptoms such as vomiting or sensitivity to noise, smells, or bright light
- The time your headache started and ended
- Food and beverages you had during the 24 hours before the migraine
- Any change in your environment, such as traveling to a new place, a change in weather, or trying new kinds of food
- Any treatment you tried, and whether it helped or made the headache worse
Common headache triggers include:
- Chocolate
- Caffeine
- Foods that contain the preservatives MSG (monosodium glutamate) and nitrates
- Aspartame, the sweetener in NutraSweet and Equal
Tests for Migraines
Headaches can be caused by a pregnancy complication called preeclampsia.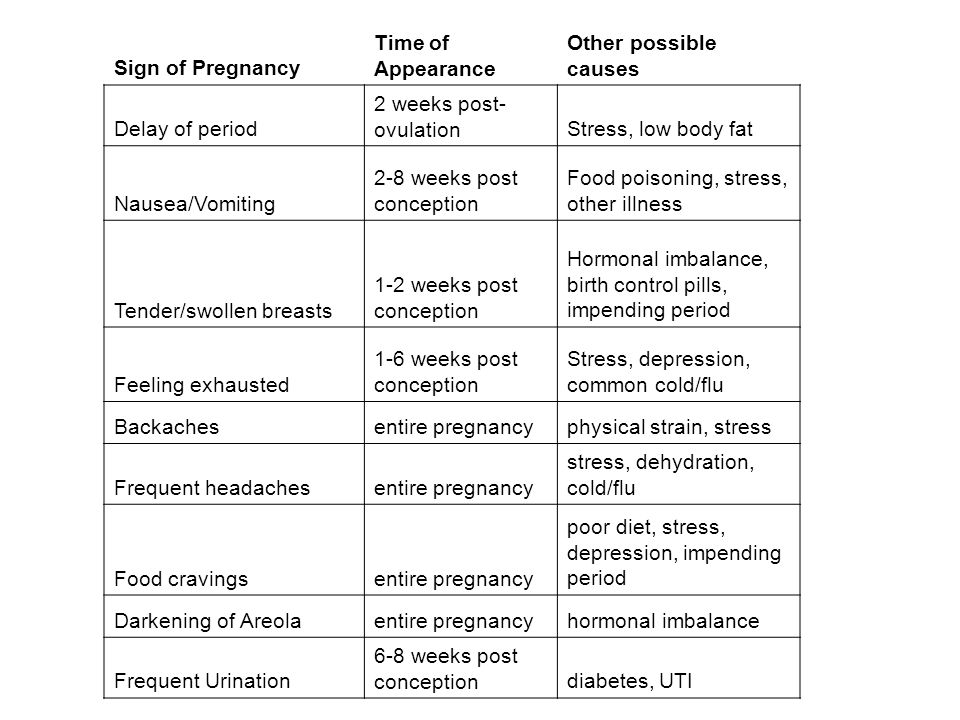 So your doctor may evaluate you for that condition before making a diagnosis of migraine. Be sure to tell your doctor about all the medications you're taking, including over-the-counter products and natural supplements. Also let your doctor know whether anyone in your family has had migraines.
So your doctor may evaluate you for that condition before making a diagnosis of migraine. Be sure to tell your doctor about all the medications you're taking, including over-the-counter products and natural supplements. Also let your doctor know whether anyone in your family has had migraines.
The doctor often can diagnose migraine from a headache diary and your medical history. CT scans and other radiology tests to rule out other causes of your headaches aren't usually advised in pregnancy. That's because of the potential risks to the fetus.
Self-Care of Migraines
Your first line of defense against migraine headaches is a healthy lifestyle and self-care. Here are some tips to help you manage migraines during pregnancy:
- Avoid your known triggers, such as specific foods, as much as possible.
- Keep a predictable schedule of meals and snacks.
- Drink plenty of water.
- Get plenty of rest.
- Consider taking a class in biofeedback or other relaxation techniques.
- When pain strikes, try ice packs, massage, and resting in a quiet, darkened room.
Medications for Migraines
If you're pregnant -- or planning to get pregnant soon -- your doctor will generally advise you to stay off medications unless they're absolutely needed. Together, you'll have to weigh the potential effects of a drug on your unborn baby. In some cases, a decision will need to be made based on scant or inconclusive research into a particular drug.
Many of the anti-migraine medications to treat or prevent migraine headache and its symptoms should be avoided during pregnancy. Some have been linked to birth defects in babies. Other medications are associated with pregnancy complications. For instance, some have been associated with bleeding, miscarriage, or intrauterine growth restriction (IUGR), a condition in which the uterus and fetus don't grow normally.
Acute Migraine Treatment
Acute treatment aims to stop a migraine attack after its first signs appear.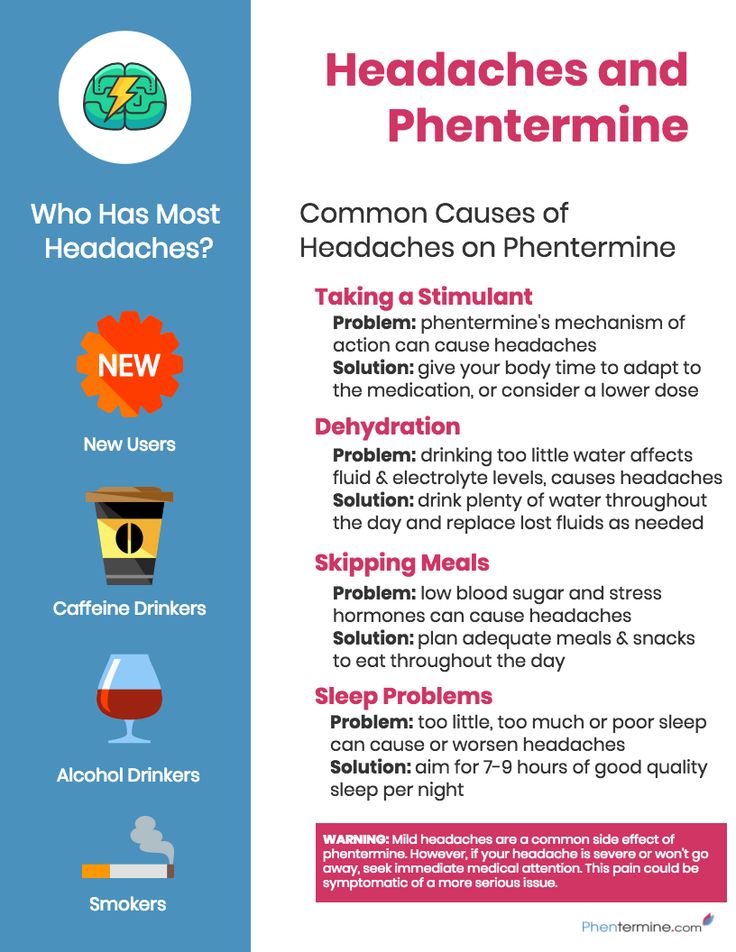
Pain relievers, also called analgesics, may help ease the intense pain of migraines. These general pain-relieving drugs, though, aren't specific to the migraine pain pathway:
- Acetaminophen is generally considered low-risk during pregnancy.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, may carry a risk of bleeding and miscarriage if taken in early pregnancy. There is also a possible risk of heart complications in the baby if they are taken in the third trimester. Aspirin taken near delivery may lead to excess blood loss in mothers during birth.
- Most NSAIDs, including ibuprofen -- sold over the counter under the brand names Advil and Motrin -- and naproxen -- sold as Aleve, Naprosyn and other brands -- don't have enough controlled human research studies to assess all their risks in pregnancy.
- Narcotic pain relievers should generally be avoided. There is a dual risk of addiction in both mothers and babies if they are used for prolonged periods of time.

Ergotamines work specifically for migraine pain. But doctors advise against taking these drugs during pregnancy. They carry a risk of birth defects, especially if taken in the first trimester. These drugs may also stimulate labor contractions and premature birth.
Triptans work specifically on the migraine pain pathway. Triptans aren't known to cause birth defects. But most research to date has focused on animals, not humans. Your doctor can help you decide is it is safe for you and your unborn baby.
Other medications may be prescribed for relief of specific symptoms of a migraine during pregnancy. For instance, antiemetics help soothe the vomiting and nausea that can accompany a migraine. But many of the drugs typically used for migraine haven't been adequately studied in pregnancy, so their safety or risk to the fetus has not been determined.
Preventive Migraine Treatment
If you have severe, recurring attacks, preventive treatment may stop future attacks or reduce their severity.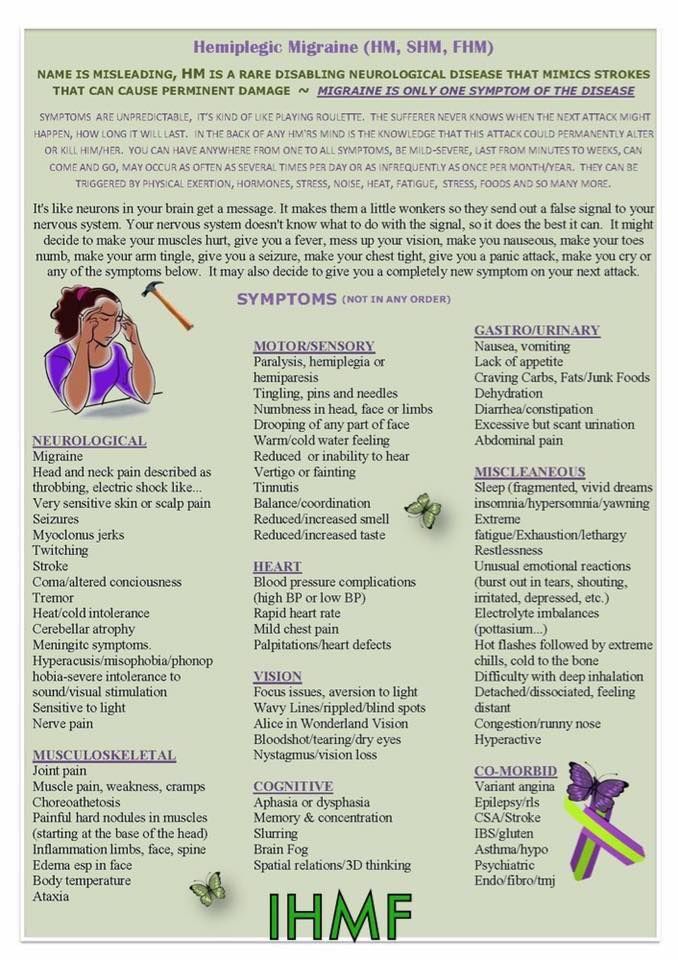 Many of the drugs used for prevention were originally used for other conditions, such as high blood pressure.
Many of the drugs used for prevention were originally used for other conditions, such as high blood pressure.
See a neurologist experienced with treating pregnant women. They'll prescribe a medicine in the lowest dose needed to help you and likely recommend some kind of talk therapy. Relatively safe medications for migraines include beta-blockers, such as metoprolol (Lopressor, Toprol XL) and propranolol (Inderal LA, Inderal XL, InnoPran XL)
When you're pregnant, always talk with your doctor before taking any drug, herbal product, or natural medicine.
If you can't take medications or wish not to, there are some devices which might be worth considering. Cefaly is a portable headband-like device that gives electrical impulses on the skin at the forehead. This stimulates a nerve associated with migraine headaches. Cefaly is used once a day for 20 minutes, and when it's on you'll feel a tingling or massaging sensation.
SpringTMS is a magnet placed on the back of the head at the first sign of a headache. It gives off a split-second magnetic pulse that stimulates part of the brain. It usually has no side effects. Also, gammaCore is a hand-held portable device which is a noninvasive vagus nerve stimulator (nVS). When placed over the vagus nerve in the neck, it releases a mild electrical stimulation to the nerve's fibers to relieve pain.
It gives off a split-second magnetic pulse that stimulates part of the brain. It usually has no side effects. Also, gammaCore is a hand-held portable device which is a noninvasive vagus nerve stimulator (nVS). When placed over the vagus nerve in the neck, it releases a mild electrical stimulation to the nerve's fibers to relieve pain.
If you're seeing a headache specialist, double-check with your obstetrician or certified midwife about the safety of any medications ordevices during pregnancy. While migraine pain may be excruciating, taking a risk with your baby's health could cause lifelong health problems for your child.
Causes, Treatments, When to Worry
Migraine and Pregnancy: Causes, Treatments, When to WorryMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
We’re gonna give it to you straight: Pregnancy can mess with your head. And we’re not just talking about brain fog and forgetfulness. We’re also talking about headaches — migraine attacks, in particular.
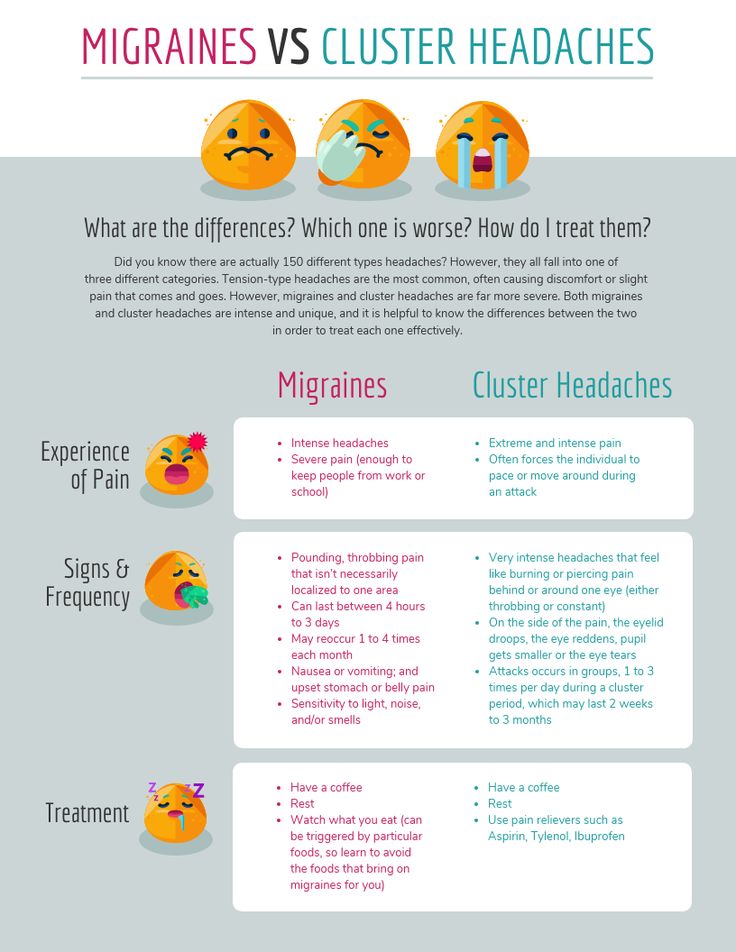
Migraine is a type of headache that can cause intense throbbing, usually on one side of the head. Imagine having a 3-year-old living behind your eye socket and relentlessly pounding a drum. Each beat sends waves of agony through your skull. The pain can make natural childbirth seem like a walk in the park.
Well, almost. Maybe we shouldn’t go that far — but migraine attacks can be very painful.
Migraine affects about 30 million Americans, 75 percent of whom are women. While many women (up to 80 percent) find that their migraine attacks improve with pregnancy, others struggle on.
In fact, about 15 to 20 percent of pregnant women experience migraine. Women who have migraine attacks with “aura” — a neurological event that accompanies or proceeds migraine and can manifest as flashing lights, wavy lines, vision loss, and tingling or numbness — generally don’t see their headaches improve during pregnancy, according to experts.
So what’s a mom-to-be to do when a migraine attack strikes? What’s safe to take and what’s not? Is migraine ever dangerous enough that you should seek emergency medical care?
Most headaches during pregnancy — including migraine — are nothing to worry about. But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
Here’s everything you need to know about migraine during pregnancy so you can tackle the pain — head on.
Migraine headaches seem to have a genetic component, which means they tend to run in families. That said, there’s usually a triggering event that unleashes them. One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
Moms-to-be who get migraine attacks tend to experience them most often in the first trimester of pregnancy, when hormone levels, including estrogen, haven’t yet stabilized. (In fact, headaches in general are an early pregnancy sign for a lot of women.)
An increase in blood volume, which is also common in the first trimester, can be an additional factor. As blood vessels in the brain expand to accommodate extra blood flow, they can press against sensitive nerve endings, causing pain.
Other common migraine triggers, whether you’re pregnant or not, include:
- Not getting enough sleep. The American Academy of Family Physicians recommends 8–10 hours per night when you’re pregnant. Sorry, Jimmy Fallon — we’ll catch you on the flip side.
- Stress.
- Not staying hydrated. According to the American Migraine Foundation, one-third of those who get migraine headaches say dehydration is a trigger. Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom.
- Certain foods. These include chocolate, aged cheeses, wines (not that you should be drinking any of those), and foods containing monosodium glutamate (MSG).
- Exposure to bright, intense light. Light-related triggers include sunlight and florescent lighting.
- Exposure to strong smells.
 Examples include paints, perfumes, and your toddler’s explosive diaper.
Examples include paints, perfumes, and your toddler’s explosive diaper. - Weather changes.
A migraine attack while you’re pregnant will look a lot like a migraine attack when you’re not pregnant. You’re apt to experience:
- throbbing head pain; usually it’s one-sided — behind one eye, for example — but it can occur all over
- nausea
- sensitivity to light, smells, sounds, and movement
- vomiting
When you’re pregnant, you have to think twice about everything you put into your body. Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
At-home remedies
These should be your first line of defense to avoid and treat migraine:
- Know your triggers. Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack.
- Hot/cold compresses. Figure out what eases migraine pain for you. A cold pack (wrapped in a towel) placed over your head can numb the pain; a heating pad around your neck can ease tension in tight muscles.
- Stay in the dark. If you have the luxury, retreat to a dark, quiet room when a migraine attack hits. Light and noise can make your headache worse.
Medications
If you’re like a lot of pregnant women, you may loathe the idea of taking medication. Nevertheless, migraine attacks can be intense, and sometimes the only thing that’ll snuff out the pain is medication.
Safe to take
According to the American Academy of Family Physicians (AAFP), drugs safe to use for migraine in pregnancy are:
- Acetaminophen. This is the generic name of the drug in Tylenol. It’s also sold under many other brand names.
- Metoclopramide. This drug is often used to increase the speed of stomach emptying but also sometimes prescribed for migraine, especially when nausea is a side effect.

Possibly safe to take under certain circumstances
- Non-steroidal anti-inflammatory drugs (NSAIDS). These include ibuprofen (Advil) and naproxen (Aleve) and are only OK in the second trimester of pregnancy. Earlier than that there’s an increased chance of miscarriage; later than that there can be complications like bleeding.
- Triptans. These include Imitrex and Amerge. While their use during pregnancy is somewhat controversial — there’s not a lot of well-performed research proving their safety — many doctors think the benefits of their use outweigh any risks.
No-gos
- Full-dose aspirin. If you’re to kick it old school and pop some aspirin, don’t. Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine.
- Opioids. According to the Centers for Disease Control and Prevention (CDC), opioid use during pregnancy can lead to preterm birth, stillbirth, and certain birth defects.
 If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
According to a 2019 study, pregnant women with migraine attacks have an increased risk of certain complications, including:
- having high blood pressure while pregnant, which may progress to preeclampsia
- delivering a low birth weight baby
- having a cesarean delivery
Older research shows that pregnant women with migraine have a higher risk of stroke. But — take a deep breath — experts say that the risk is still very low.
That’s the bad news — and it’s important to keep it in perspective. The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
- you have a first-time headache during pregnancy
- you have a severe headache
- you have high blood pressure and a headache
- you have a headache that won’t go away
- you have a headache accompanied by changes in your vision, such as blurry vision or sensitivity to light
Thanks to a more constant supply of hormones, most women get a break from migraine attacks during pregnancy.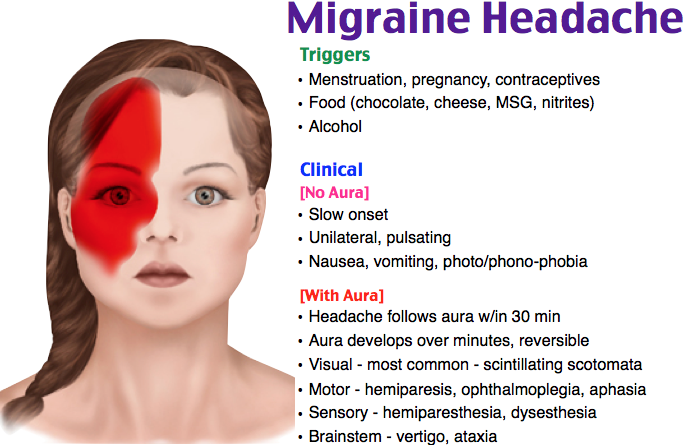 For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
Make a migraine management plan with your doctor early on in your pregnancy (and ideally, before), so you have tools at the ready.
Last medically reviewed on May 6, 2020
- Parenthood
- Pregnancy
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- About opioid use during pregnancy. (2020).
cdc.gov/pregnancy/opioids/basics.html - Bushnell CD, et al. (2009). Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study.
 DOI:
DOI:
10.1136/bmj.b664 - Experts comment on research suggesting links between migraine and stroke risk in pregnancy, as published in the BMJ. (2009).
sciencemediacentre.org/experts-comment-on-research-suggesting-links-between-migraine-and-stroke-risk-in-pregnancy-as-published-in-the-bmj-2/ - Mayans L, et al. (2018). Acute migraine headache: Treatment strategies.
aafp.org/afp/2018/0215/p243.html#sec-6 - Mayo Clinic Staff. (2017). Nutrition and healthy eating.
mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256 - Migraine. (2019).
womenshealth.gov/a-z-topics/migraine - Migraine and pregnancy: What moms-to-be need to know. (2017).
americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy-what-moms-to-be-need-to-know/ - Migraine headaches during pregnancy. (n.d.).
stanfordchildrens. org/en/topic/default?id=migraine-headache-90-P02476
org/en/topic/default?id=migraine-headache-90-P02476 - Migraine headaches during pregnancy. (n.d.).
chop.edu/conditions-diseases/migraine-headaches-during-pregnancy - Pregnancy and breastfeeding: Key issues for women who have migraine and become pregnant. (n.d.).
migrainetrust.org/living-with-migraine/coping-managing/pregnancy-breastfeeding/ - Skajaa N, et al. (2019). Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. DOI:
10.1111/head.13536 - Sleep and pregnancy. (2017).
familydoctor.org/getting-enough-sleep-pregnancy/ - Top 10 migraine triggers and how to deal with them. (2017).
americanmigrainefoundation.org/resource-library/top-10-migraine-triggers-and-how-to-deal-with-them/
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
related stories
5 Tips for Managing Pregnancy Challenges with Migraine
How Improving Sleep Can Prevent Migraine Attacks
Headache During Pregnancy: What You Need to Know
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
How Symptom Tracking Can Help You Find Relief from Migraine
Read this next
5 Tips for Managing Pregnancy Challenges with Migraine
Medically reviewed by Carolyn Kay, M.
 D.
D.Managing migraine throughout pregnancy can be a challenge, but there are options that can help limit attacks.
READ MORE
How Improving Sleep Can Prevent Migraine Attacks
Medically reviewed by Seunggu Han, M.D.
A lack of rest can trigger migraine attacks. Here are eight ways you can improve the quality of your sleep for migraine relief.
READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
Medically reviewed by Deena Kuruvilla, MD
During a migraine attack, sometimes the only thing you can do is make yourself as comfortable as possible while you ride out the neurological storm.

READ MORE
How Symptom Tracking Can Help You Find Relief from Migraine
Medically reviewed by Deena Kuruvilla, MD
Symptom tracking can be a helpful tool to better understand and manage your migraine pain.
READ MORE
Antidepressants in Pregnancy Aren't Linked to Increased Neurological Issues in Children
A cohort study of antidepressant use in pregnancy found that the rate of neurological disorders in children born to those who took antidepressant…
READ MORE
These Guided Pregnancy Journals Will Help You Document All the Feels
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
The pregnancy and postpartum periods are full of emotions (rightfully so!), and these pregnancy journals are a great place to document it all.

READ MORE
What You Need to Know If You’re Having a High Risk Pregnancy
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A high risk pregnancy is any pregnancy that comes with increased health risks for either the pregnant parent, the fetus, or both.
READ MORE
What Are Conjoined Twins?
Conjoined twins are identical twins who are born connected and likely share one or more organs. We explain how they develop and when separation is…
READ MORE
The Acupressure Points for Inducing Labor
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Are you pregnant and past your due date? Help induce labor naturally by pressing on these acupressure points along the body.
READ MORE
Migraine during pregnancy - Juno
Migraine during pregnancy - Juno -->home
Articles
Migraine during pregnancy
How to recognize an attack and deal with it properly - read on.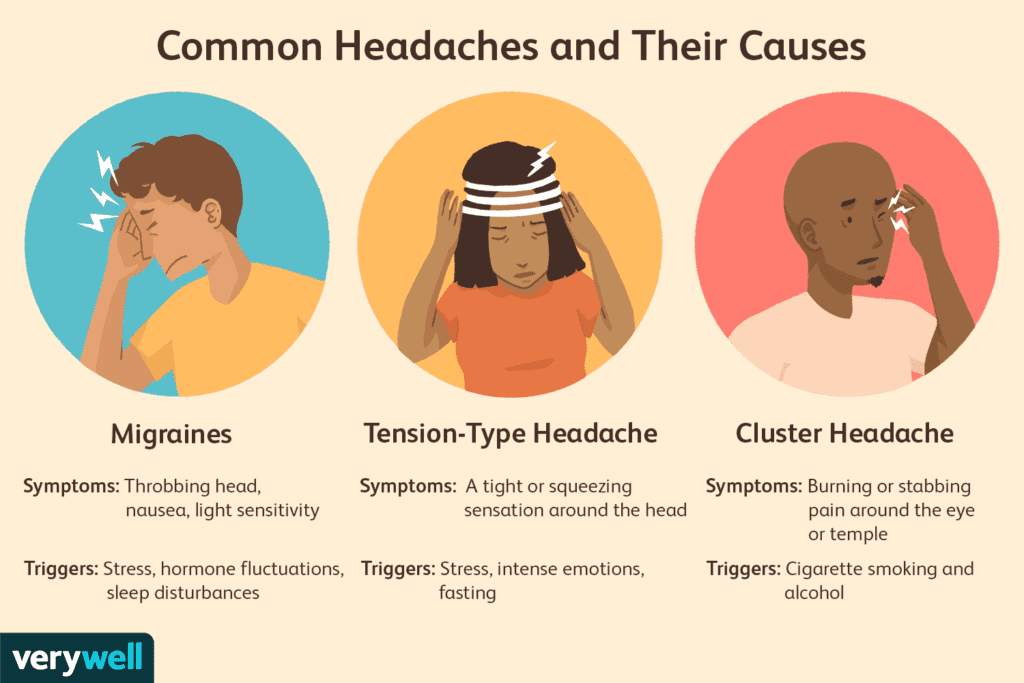 We will tell you how dangerous migraines are and how to get rid of them safely during pregnancy.
We will tell you how dangerous migraines are and how to get rid of them safely during pregnancy.
Contents of the article
Features and manifestations of migraine during pregnancy
If a woman was worried about migraines before pregnancy, then during the bearing of a child, the attacks are more likely to stop, or become milder and rarer. Improvements come from the 2nd trimester and are due to the fact that fluctuations in estrogen levels stop. In the early stages, the likelihood of migraine is higher. In the 1st trimester, ailments often occur, including headaches. But it's not always a migraine.
Migraine symptoms in pregnant women are similar to those that occur in other people. Approximately the picture looks like this:
- Harbingers. They are not characteristic for everyone and may be absent. They occur 1-3 days before an attack, manifest as irritability, depression, or, conversely, a surge of activity.
- Headache.
 Very intense, more often covers the temporal or frontal region, has a pulsating, bursting character. It can be localized in one half of the head, but sometimes it spreads to the entire head. The pain lasts from 2-3 hours to several days, it is difficult to remove.
Very intense, more often covers the temporal or frontal region, has a pulsating, bursting character. It can be localized in one half of the head, but sometimes it spreads to the entire head. The pain lasts from 2-3 hours to several days, it is difficult to remove. - Aura. It also doesn't happen to everyone. The phenomenon accompanies headache and lasts 10-40 minutes. Patients note flashes of light, spots, flies before the eyes, sometimes numbness of the extremities worries. With an aura, it is almost impossible to do something around the house or work.
Even after the pain passes, the expectant mother experiences depression, fatigue, irritability. Unpleasant sensations continue for about a day.
Why do pregnant women get migraines
The exact cause of the disease has not been established. However, experts single out hormonal changes in the body and an increased load on the body during pregnancy among the provoking factors.
General risk factors:
- sudden change of weather - especially for weather-sensitive women;
- stress and depression have a bad effect on blood vessels and the nervous system;
- violation of the diet - long intervals between meals, overeating, abuse of citrus fruits, smoked products and chocolate;
- overwork - physical fatigue at home and at work, sleep disturbances;
- irritants - unpleasant odors, stuffiness, excessive light or noise;
- fluid deficiency - dehydration due to insufficient water intake;
- concomitant pathologies, for example, hypertension.

The condition of pregnant women is adversely affected by weight gain, hypothermia and overheating. This can also provoke migraine attacks, especially if they have happened before.
Are seizures dangerous for the fetus
By itself, migraine during pregnancy is not critical. If the seizures are not caused by more serious problems - hypertension, eclampsia, then a woman is highly likely to give birth to a healthy child at term. Migraine does not increase the risk of preterm birth or developmental anomalies in the fetus.
But despite the safety for the baby, migraines are debilitating for a pregnant woman. This affects general well-being - worsens sleep, nutrition, causes stress, decreased activity. Therefore, too frequent seizures can result in problems with the nervous system, fetal hypoxia. It is important to help yourself in time.
Treatment of migraine during pregnancy
Tablets should be taken only as a last resort. In the early stages, strong drugs are prohibited. First, try to cope with non-drug methods:
In the early stages, strong drugs are prohibited. First, try to cope with non-drug methods:
- Drink sweet tea or cola. Caffeine in small doses is harmless and can help relieve headaches.
- Take a walk in the fresh air, do simple exercises. This contributes to the outflow of blood from the vessels of the brain and the elimination of pain.
- Apply a warm or cool compress to the head. It can be a towel moistened with water or a heating pad.
- Take a cool shower (but not too cold). The procedure is useful as a prevention of varicose veins and migraines.
- Relax and sleep in a quiet, dark room.
- Do not hold back the urge to vomit - it can relieve an attack of pain.
- Rub essential oils of lemon, orange, lemon balm into whiskey - a little is enough. Too much oil can make headaches worse. If you have previously noticed such a reaction of your body to odors, you should not apply this method now.
- Drink freshly squeezed juice or clean water.
 Replenishing fluids often helps get rid of a migraine.
Replenishing fluids often helps get rid of a migraine.
If the above measures do not help, and the seizures are disturbing enough, you need to consult a doctor. The specialist will prescribe treatment, for example, prescribe pills that will help to cope with pain. The safest drug is paracetamol. It can be taken on its own. The doctor may prescribe magnesium for treatment - it has a beneficial effect on blood vessels.
In some cases, ibuprofen and aspirin are acceptable (only in the 2nd trimester). Opioid analgesics and triptans are strictly prohibited. If a migraine is growing or has appeared for the first time, an aura has joined, pressure rises, you should definitely consult a doctor and in the near future.
Prophylaxis
Dealing with migraines during pregnancy is not always easy. It is better to follow some rules that will help reduce the risk of seizures:
- Keep a sleep and rest schedule.
- Control sweets and fatty foods.

- Try to walk every day, do light exercises.
- Massage or self-massage the head and collar area. Movements should be light: it is better if the specialist shows what they should be.
Even if an attack has already happened, try not to abruptly get involved in worries and affairs after it. Remember that you are responsible not only for yourself, but also for the child. Do not be shy to turn to your loved ones for help and do not be heroic. Be healthy!
Other articles
08/17/2022
Perinatal screening of the 1st trimester of pregnancy
Perinatal screening of the 1st trimester of pregnancy - what are the features? What is important for a future mother to know? We tell you all the important details in our article!
08/05/2022
Insomnia during pregnancy
The need for proper sleep is a natural desire of the body. For a pregnant woman, full sleep is not only a whim, but also an opportunity to replenish energy resources, recover and gain strength for a new day.
For a pregnant woman, full sleep is not only a whim, but also an opportunity to replenish energy resources, recover and gain strength for a new day.
08/03/2022
Management of pregnancy
The birth of a child is the most important event in a woman's life. It is necessary to prepare for this difficult event as a test, on the one hand, and as a joyful, unforgettable event in the life of parents, on the other hand. We will tell you everything about pregnancy management in our article!
Making an appointment?
Making an appointment?
Request a call
a particular example of the course of the disease uMEDp
Migraine is one of the most common forms of headache. There is evidence for the role of magnesium deficiency in the pathogenesis of migraine. The disease most often occurs in women of reproductive age.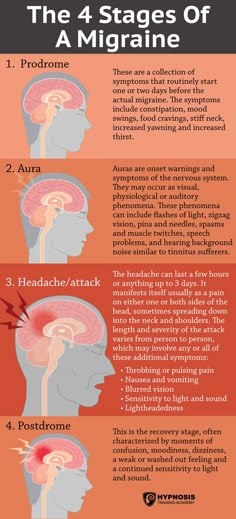 The frequency of migraine attacks during pregnancy tends to decrease. However, in cases where migraine attacks persist during pregnancy, difficulties arise in the selection of a drug. Magnesium preparations (Magnerot) are effective and safe drugs and can be recommended for prophylactic treatment of migraine in pregnant women.
The frequency of migraine attacks during pregnancy tends to decrease. However, in cases where migraine attacks persist during pregnancy, difficulties arise in the selection of a drug. Magnesium preparations (Magnerot) are effective and safe drugs and can be recommended for prophylactic treatment of migraine in pregnant women.
Migraine is the second most common form of primary headache after tension headache. Epidemiological studies have confirmed the high prevalence of migraine and its socio-economic significance, negative impact on the quality of life and performance [1].
Periodically recurring migraine headache attacks are pulsating, often unilateral in nature, accompanied by nausea, vomiting, photo and sound phobia. After an attack, drowsiness and lethargy are observed. Migraine is a chronic, heterogeneous disease. There are more than 15 subtypes of migraine, but in practice migraine with aura and without aura is usually distinguished [1]. The frequency, duration, and intensity of seizures vary greatly among patients.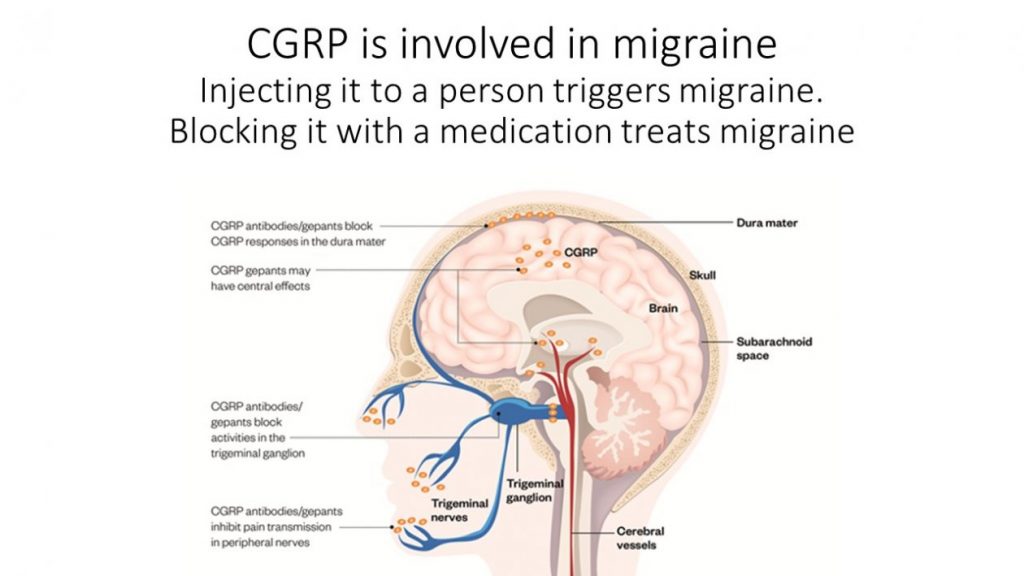 Each patient has their own specific precipitating factors. Young women suffer from migraine three times more often than men. A change in the hormonal status associated with menarche, pregnancy, lactation or menopause is accompanied by a change in the clinical course of the disease in them. Women note a clear relationship between headache attacks and the onset of menstruation [2]. During pregnancy, approximately 70% of women with migraine, mostly without aura, improve, the frequency of headache attacks decreases as the gestational age increases. However, in migraine with aura, the frequency and intensity of attacks persist throughout pregnancy [3]. In this case, it is necessary to exclude the secondary nature of migraine, in particular, an increase or decrease in blood pressure (BP), the development of venous vascular dyscirculation, intracranial hypertension, preeclampsia / eclampsia. It is also necessary to conduct a differential diagnosis of primary headaches according to international diagnostic criteria, to determine the subtype of migraine [1].
Each patient has their own specific precipitating factors. Young women suffer from migraine three times more often than men. A change in the hormonal status associated with menarche, pregnancy, lactation or menopause is accompanied by a change in the clinical course of the disease in them. Women note a clear relationship between headache attacks and the onset of menstruation [2]. During pregnancy, approximately 70% of women with migraine, mostly without aura, improve, the frequency of headache attacks decreases as the gestational age increases. However, in migraine with aura, the frequency and intensity of attacks persist throughout pregnancy [3]. In this case, it is necessary to exclude the secondary nature of migraine, in particular, an increase or decrease in blood pressure (BP), the development of venous vascular dyscirculation, intracranial hypertension, preeclampsia / eclampsia. It is also necessary to conduct a differential diagnosis of primary headaches according to international diagnostic criteria, to determine the subtype of migraine [1].
Tactics of migraine therapy in pregnant women in most cases does not differ from the traditional one and includes two directions - relief of a headache attack and prophylactic therapy for frequent (more than 2-3 per month) attacks. For mild or moderately intense migraine attacks, the drugs of choice are simple analgesics (paracetamol, ibuprofen), as well as their combination with caffeine. Given that during migraine attacks, many patients have pronounced atony of the stomach or intestines, which makes it difficult for the absorption of oral drugs, antiemetics (metoclopramide or domperidone) are added to therapy. For more severe migraine attacks, specific triptan preparations are used that effectively eliminate headaches. The most studied is sumatriptan, which can be used in pregnant women.
As a preventive therapy for migraine in pregnant women, the use of low doses of beta-blockers, tricyclic antidepressants, non-steroidal anti-inflammatory drugs, and magnesium preparations is recommended [4]. Most drugs for the treatment of migraine are allowed to be used during pregnancy, however, before prescribing a particular drug, it is necessary to take into account factors such as the form of migraine, its intensity, gestational age, fetal condition, concomitant extragenital diseases, the benefit-risk ratio of the intended therapy.
On the example of a clinical case, let us consider the features of the course of migraine in a pregnant woman and the tactics of its management in case of a change in the nature of cephalalgia.
Patient management
Patient V., 36 years old. She was under the supervision of an obstetrician-gynecologist in the antenatal clinic from 10 weeks of pregnancy. Married. Works as a nurse.
Second birth, third pregnancy. The first birth at the age of 24, during pregnancy was observed due to the threat of termination, blood pressure during pregnancy did not increase. Term delivery, newborn boy, weight 3050 g,
height 51 cm.
From the age of 18, the patient has been suffering from attacks of unilateral throbbing headache lasting up to 24 hours with nausea and photophobia. The frequency of migraine attacks before pregnancy is 1-2 times a month. The patient was seen by a neurologist for headache. Diagnosis of migraine without aura. The secondary nature of the headache was excluded. The headache was stopped by simple analgesics or passed after rest, sleep.
History of aggravated heredity - arterial hypertension (AH) in the father, migraine in the mother.
Smoker, has not smoked for the last 10 years.
A year before the expected pregnancy, she underwent a clinical, laboratory and instrumental examination at the place of residence, including an electrocardiographic study, 24-hour blood pressure monitoring (ABPM), electroencephalography, and ultrasound duplex scanning of the vessels of the main parts of the head. AH, vascular disease of the head were not detected, there was no pathology of the kidneys.
First visit: 12 weeks pregnant
Objectively: the condition is satisfactory. Height 158 cm, weight 70.3 kg (weight before pregnancy 67 kg, body mass index 26.8 kg / m², overweight). BP 110/60 mm Hg. Art. Heart rate (HR) 88 beats / min. No changes were found according to clinical blood and urine tests. Biochemical blood test: total cholesterol 3.8 mmol/l, glucose
3.86 mmol/l, uric acid 172 µmol/l. Coagulogram without deviations from the reference values.
Urinalysis: specific gravity 1012, protein negative, leukocytes 8–10 per field of view.
Electrocardiogram (ECG) - sinus rhythm, heart rate 80 bpm, vertical position of the electrical axis of the heart.
ABPM: daily average BP 110/65 mm Hg. Art., standard deviation from the mean value of blood pressure (standard deviation - STD)
14/9 mm Hg. Art.; day - BP 116/66 mm Hg. Art., STD 10/9 mm Hg. Art.; night - 94/53 mm Hg. Art., STD 10/8 mm Hg. Art.; SI (daily BP index) 18/9%, VI (time index) 0/0%. Conclusion: normal average daily BP levels are recorded, the circadian rhythm of BP for diastolic BP is disturbed - non-dipper, BP variability is within the normal range.
Echocardiography (EchoCG): morphofunctional parameters within the normal range: interventricular septal thickness (IVSD) - 0.83 cm, thickness of the posterior wall of the left ventricle (PVSLV) - 0.83 cm, end diastolic size (EDD) of the left ventricle - 4, 4 cm, end systolic size (SSR) of the left ventricle - 2.23 cm, ejection fraction (EF) - 65%, myocardial mass index (IMM) of the left ventricle - 74.7 g / m³, total peripheral vascular resistance (OPVR) -
1212 dyne x s x cm-5.
Due to a history of headaches, the patient was referred for a consultation with a neurologist. No focal symptoms were found in the neurological status. Diagnosis: migraine without aura. Due to rare migraine attacks, prophylactic therapy is not indicated. Relief of seizures with paracetamol in combination with caffeine.
The patient is assigned to the high-risk group: age, complicated obstetric anamnesis, heredity burdened by hypertension, overweight, circadian rhythm disturbances in diastolic blood pressure.
Re-examination: pregnancy 20 weeks
No active complaints at the time of examination. He notes an increase in the frequency of headaches up to 2-3 times a week. The characteristic of cephalgia is the same.
Objectively: satisfactory condition, weight 73.1 kg, blood pressure 118/68 mm Hg. Art., heart rate 76 beats / min.
No abnormalities were found in general blood and urine tests. Biochemical blood test: total cholesterol 5.7 mmol/l, glucose 4.0 mmol/l, uric acid 256 µmol/l. The coagulogram corresponds to the reference values.
ECG - sinus rhythm, heart rate 80 bpm, vertical position of the electrical axis of the heart.
Echocardiography: TMZhP 0.8 cm, TLSLV 0.8 cm, EDR 4.8 cm, EFR 2.2 cm, EF 67%, IMM 79.1 g/m³, TPVR 1714 dyn × s × cm-5.
ABPM: daily average BP 111.7/66.5 mm Hg. Art., STD 15 / 9.6 mm Hg. Art.; day - BP 114.3 / 68.3 mm Hg. Art., STD 10.9 / 9.6 mm Hg. Art.; night - 103/62.1 mm Hg. Art., STD 11.3 / 9.1 mm Hg. Art.; SI 9.7/9.1%, CI 5/2%.
Conclusion: normal average daily BP levels are recorded, disturbed circadian rhythm of BP with a decrease in day/night pressure drop of less than 10% - non-dipper, systolic daily BP variability is increased. In comparison with the data of the previous study, there is an increase in the level of nocturnal blood pressure by 9/9 mmHg Art.
In neurological status without negative dynamics.
Despite the patient's satisfactory condition, the normal level of blood pressure, the absence of any laboratory markers of a complicated course of pregnancy, the trend towards an increase in TPVR and a change in the daily profile of blood pressure by the non-dipper type, an increase in the frequency of cephalalgia, is worrying.
It is recommended to continue monitoring, re-examinations every 14 days with an assessment of weight gain, measurement of blood pressure, urinalysis. Magnesium preparations are recommended for a long time. Over the next 6 weeks, the patient took Magnerot 500 mg 3 times a day, noted an improvement in well-being. During the first 2 weeks of therapy, one mild attack of headache was noted, in the future, headache attacks did not bother.
Pregnancy 32 weeks: hospitalization
At 32 weeks, during the next visit, the patient complained of a bilateral headache of a pressure-pulsating nature of the frontotemporal localization. The pain is most pronounced in the morning, decreases somewhat with the vertical position of the body, sleep is disturbed. Objectively: the condition is satisfactory, weight is 79.1 kg, blood pressure is 150/90 mm Hg. Art., heart rate 72 beats / min.
In the general analysis of urine: specific gravity 1014, traces of protein, leukocytes up to 10–12 per field of view. Complete blood count (30 weeks): hemoglobin 109g/l, hematocrit 34.1%, the number of erythrocytes, platelets are normal, there are no deviations in the leukocyte blood count, ESR 32 mm/h. Biochemical blood test: total cholesterol 7.2 mmol/l, glucose 3.8 mmol/l , uric acid 286 µmol/l.
ECG - sinus rhythm, heart rate 76 beats/min, ventricular extrasystole was registered.
Ultrasound of the fetus: dimensions correspond to a period of 30 weeks, no signs of disturbance of the uteroplacental and fetoplacental blood flow were detected, the threat of termination of pregnancy.
Examination by a neurologist revealed no focal symptoms. Headache is most likely due to the manifestation of hypertensive syndrome.
Diagnosis: 32 weeks pregnant. Gestational arterial hypertension. Preeclampsia (PE)? The threat of abortion. Anemia.
Immediate hospitalization to the maternity hospital is recommended to clarify the diagnosis and conduct intensive drug treatment. Later, the patient developed PE: an increase in blood pressure up to 150/9 was recorded.0 mmHg Art., was determined protein in the urine more than 0.3 g / day. Therapy was carried out with antihypertensive drugs - Dopegyt 1500 mg / day, as well as magnesium therapy. At 34 weeks, the patient had a premature birth, the newborn was a boy, weight 2600 g, height 49 cm with an Apgar score of 7.8 points at the 1st and 5th minutes, respectively.
Summary: the development of PE in a pregnant woman with a burdened somatic and neurological history, an increased risk of vascular complications was preceded by structural and functional changes in the cardiovascular system from the beginning of pregnancy; the use of magnesium preparations (Magnerot) improved the patient's condition at the 20-26th week of pregnancy due to a decrease in headache attacks; monitoring of blood pressure levels, its circadian rhythm and laboratory data contributed to the timely detection of gestational complications, timely hospitalization and adequate complex antihypertensive and magnesium therapy.
Cephalgic syndrome in women during pregnancy is observed quite often, accompanies hypertensive disorders, vegetative-vascular dystonia syndrome, depression and is considered the leading manifestation of migraine. Frequent and intense headaches reduce performance, significantly worsen the quality of life. Difficulties in differential diagnosis dictate the need to find effective and safe methods of preventive therapy for headache in pregnant women. In our patient, a migraine headache that preceded pregnancy recurred during pregnancy, which was the basis for prophylactic treatment. Certain difficulties were caused by the choice of the drug. We preferred magnesium preparations.
Migraine is a magnesium deficiency disease
Clinical and experimental data allow us to consider migraine as a magnesium deficiency disease [5]. Patients suffering from migraine, compared with healthy people, often have lower concentrations of magnesium in serum and blood cells, saliva and cerebrospinal fluid [6]. Magnesium is the second intracellular cation after potassium; it is involved as a cofactor in more than 300 metabolic reactions in the body, including protein synthesis, intracellular energy metabolism, DNA and RNA reproduction, and stabilization of mitochondrial membranes. Magnesium plays an important role in nerve impulse transmission, cardiac excitability, neuromuscular conduction, muscle contraction, vasomotor tone, and the regulation of glucose and insulin metabolism. Low levels of magnesium in the body are associated with the development of hypertension, type 2 diabetes, Alzheimer's disease, and migraines. It is suggested that one of the mechanisms for the development of migraine headache may be a violation of the intracellular interaction of magnesium and calcium. Altered activity of ion channels plays the role of a trigger in the development of spreading cortical depression [7].
Magnesium deficiency contributes to platelet hyperaggregation, negatively affects the function of serotonin receptors, the synthesis and release of various neurotransmitters, which causes the development of vascular spasm [8]. Magnesium is involved in modulating the level of nitric oxide in the cell [9], a decrease in which is noted in migraine, especially in women with migraine pain, potentially mediated by sex hormones [10].
Magnesium deficiency in migraine sufferers may be due to genetic causes of malabsorption or increased excretion [11].
Mitochondrial Theory of Migraine: Drugs
Recent studies have shown that several subtypes of migraine are associated with mitochondrial damage to neurons and astrocytes due to intracellular calcium accumulation, free radicals, and a deficiency in oxidative phosphorylation. Markers of these disorders are low superoxide dismutase activity, activation of cytochrome oxidase and nitric oxide, high levels of lactate and pyruvate, and a low ratio of phosphocreatine-inorganic phosphates and N-acetylaspartate-choline in patients with migraine. Mitochondrial dysfunctions are genetically determined; mitochondrial DNA polymorphisms have been described in migraine with vomiting in pediatric practice [12]. The therapeutic evidence of the mitochondrial theory of migraine can be recognized as the effectiveness of a number of drugs with a positive effect on mitochondrial metabolism. These drugs include primarily magnesium preparations, as well as riboflavin, coenzyme Q10, carnitine, topiramate, lipoic acid, niacin.
Empiric magnesium therapy seems reasonable in all patients with migraine, as half of them are magnesium deficient, and routine determination of blood magnesium levels does not reflect its real status. At the same time, magnesium preparations are available, safe and inexpensive [11]. The effectiveness of magnesium therapy in patients with migraine has been proven in a number of clinical studies [13].
For patients with episodic migraine (headache ≤ 14 days per month), recommendations for preventive therapy have been developed based on an analysis of the results of randomized trials and Cochrane reviews. Magnesium preparations along with some other drugs (topiramate, propranolol, nadolol, metoprolol, amitriptyline, gabapentin, candesartan, butterbur, riboflavin, coenzyme Q10) were found to be effective and recommended for migraine prevention [14].
Magnerot during pregnancy
During pregnancy, the administration of magnesium preparations allows achieving a satisfactory effect without fear of embryotoxic and teratogenic effects, unlike many drugs traditionally used to treat headache [15].
For our patient, we recommended taking Magnerot in medium therapeutic doses for a long time (at least 8 weeks). Correction of magnesium deficiency during pregnancy is necessary, since magnesium deficiency is associated with a wide range of complications of pregnancy and childbirth. As is known, a decrease in the content of magnesium leads to an increase in the tone of the myometrium and underlies preterm labor [16, 17]. A low level of intracellular magnesium contributes to the development of AH in pregnant women [18, 19]. Magnesium deficiency during pregnancy can lead to intrauterine growth retardation (IUGR) [20] and poor offspring survival [21]. At the same time, experimental data on the study of IUGR treatment methods in pregnant rats demonstrate the possibility of therapy with a magnesium-enriched diet, which reduced induced fetal growth retardation by 64%, and also reduced the level of pro-inflammatory cytokines in the amniotic fluid and placenta [22].