Does a fetus share blood with the mother
Baby's Cells Mix and Mingle with Pregnant Mom's
A pregnant woman's blood stream contains not only her own cells, but a small number of her child's, as well. (Image credit: <a href="http://www.shutterstock.com/gallery-58667p1.html"> Supri Suharjoto</a>, <a href="http://www.shutterstock.com/index-in.mhtml">Shutterstock</a>)During pregnancy, and even decades later, a baby's influence on mom runs deep — cell deep. While the fetus develops inside the womb, its cells mix and mingle with the mother's after traveling through the placenta, and can stay there for years.
In a new study, researchers discovered cells from the placenta and the fetus inside a pregnant mouse's lungs. They were even able to tell that some of the cells were immune cells, while others looked like undefined connective tissue.
"We and other people have shown they stay around for decades. They aren't the original cells so there must be some way they can give rise to daughter cells in the mother's body," study researcher Diana Bianchi of Tufts Medical Center, told LiveScience. "We strongly believe that there are implications for the future health of women who are or have previously been pregnant."
Pregnant mice
The researchers aren't sure how fetal cells get across the placenta into the mother, but it's possible that there are leaky spots (which get bigger as pregnancy reaches term) in the cells that form the barrier between the baby's blood and the mother's blood in the placenta.
They also don't know what the cells do in the mother's body, or what types of cells they are. So Bianchi and her colleagues studied pregnant mice to see what types of cells they could find in the mother's lungs. [8 Odd Changes That Happen During Pregnancy]
To track the fetal cells, Bianchi's graduate student, Stephanie Pritchard, mated a male mouse that had two copies of the green fluorescent protein gene with a normal female. This gene was present in every fetus he fertilized, so when these fetal cells made it into the mother's organs, the researchers were able to recognize the fluorescent signal and separate those cells from the mother's own cells.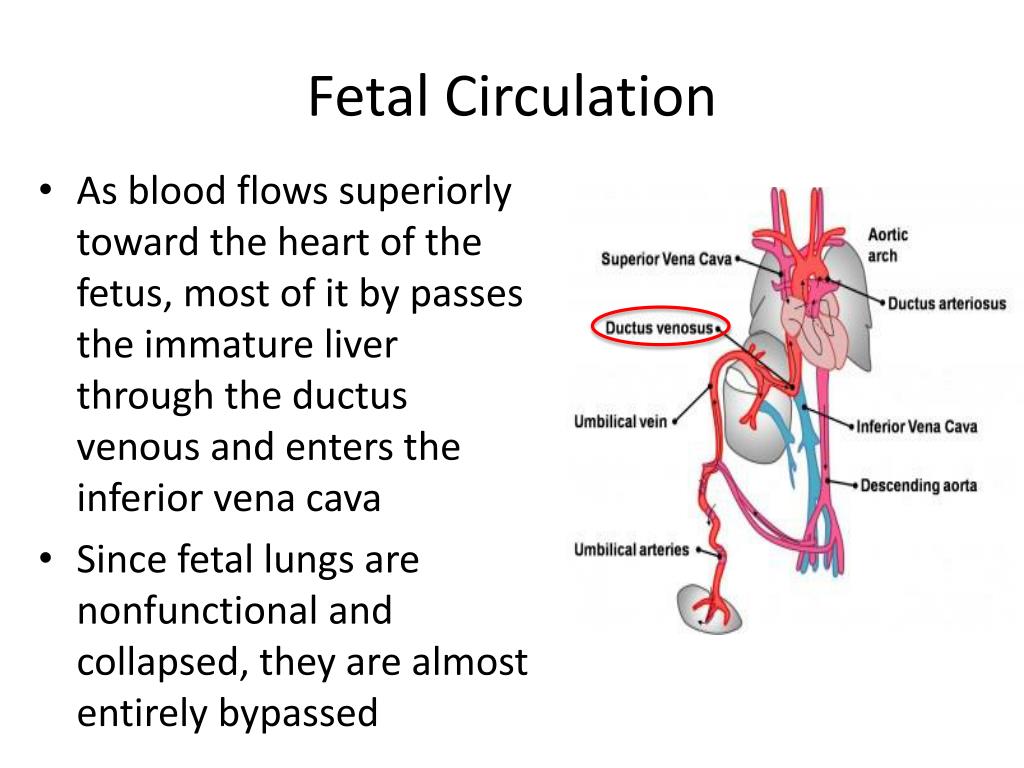
Next, they analyzed the genetics of these captured fetal cells to see which genes were turned on, comparing these "expressed" genes with data for the genes expressed by various cell types. They found the genetic signatures of cells matched those derived from the placenta, and from two types of fetal cells: immune cells and undifferentiated cells that make up the connective tissues, called mesenchymal cells.
Special cells
The immune cells may help ensure that the mother's immune system doesn't "reject" the fetus (as it would a transplanted organ that isn't a genetic match), but the researchers don't really know what role the undifferentiated mesenchymal cells have.
These mesenchymal cells could play a role in regeneration or healing of the mother's tissues, the researchers speculate. For instance, these fetal cells have been found integrated into lung tissue, and researchers have seen them come to the rescue when maternal heart tissue is injured. They've also shown up at the site of tumors.
They've also shown up at the site of tumors.
"They are younger cells and they do appear to have different capabilities," Bianchi said. "That's an area for future research: to determine if an undifferentiated cell from the fetus has different regenerative capability than the mother's own stem cells."
The study was published today (June 6) in the journal Biology of Reproduction.
Follow Jennifer Welsh on Twitter @microbelover or LiveScience @livescience. We're also on Facebook & Google+.
Jennifer Welsh is a Connecticut-based science writer and editor and a regular contributor to Live Science. She also has several years of bench work in cancer research and anti-viral drug discovery under her belt. She has previously written for Science News, VerywellHealth, The Scientist, Discover Magazine, WIRED Science, and Business Insider.
Healthy Pregnancy: What's Blood Mixing?
There are an estimated 128,845,000 babies born each year at a rate of 350,000 per day, with the global population expected to reach 9.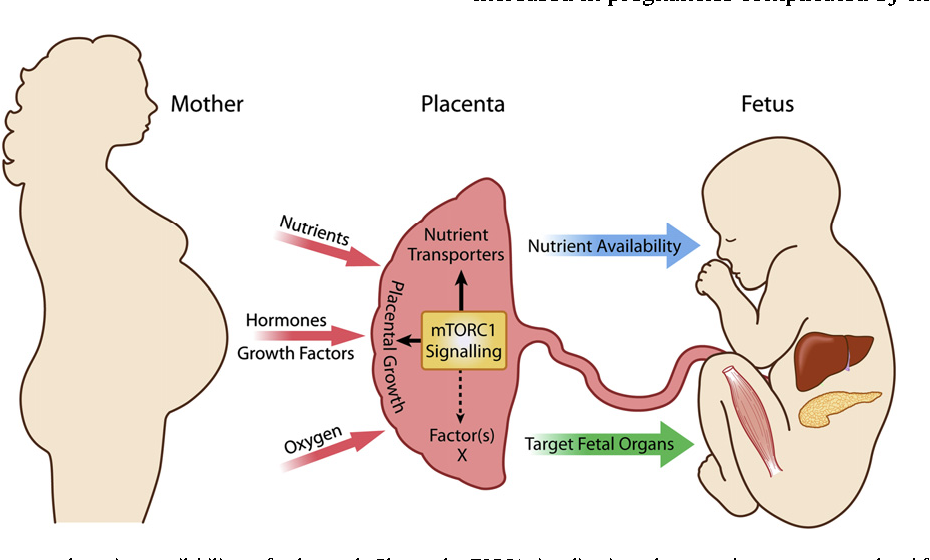 8 billion by the year 2050.
8 billion by the year 2050.
And while thankfully medicine has come a long way since the days when forceps were considered the apex of obstetric technology, sorting through the cacophony of information on potential pregnancy health mishaps can be bewildering. RingMD’s series on pregnancy health aims to straighten out misconceptions and address your pressing concerns so that you can focus on what’s most important--taking care of yourself and preparing for the birth of your baby. Blood Type
A particularly prevalent worry--sparked by the essentiality of matching compatible blood types during blood transfusions and donation--is that the baby will not have the same blood type as it’s mother, leading to a potential ABO or Rh incompatibility reaction when their blood mixes in utero. An ABO incompatibility reaction is a rare occurrence that can take place when a blood donation recipient is matched with the wrong type of blood. There are four main blood types--A, B, AB, and O--which each have a specific set of antibodies.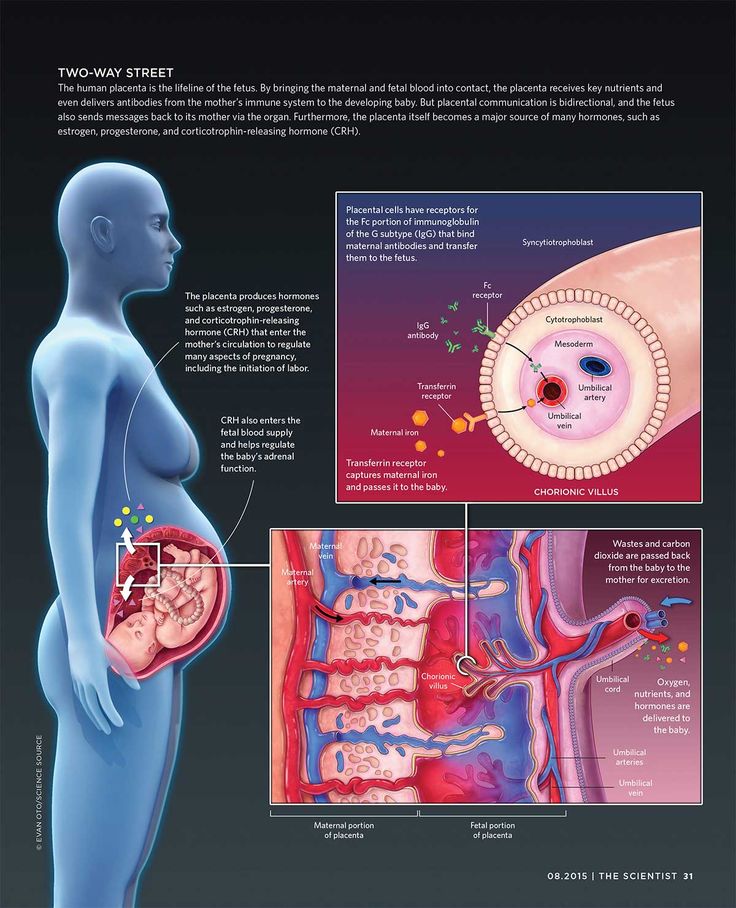 A and B each have specific A and B antibodies respectively, AB has both A and B antibodies, and O has none at all. This means that AB types are universal recipients and can receive any type of blood, while A can receive A and O, B can receive B and O, and O (although it is the universal donor) can only receive O blood. In rare instances, when an incompatible form of blood is used for a transfusion, the recipient’s immune system will mark the new red blood cells as a threat and begin destroying them, which triggers excessive clotting and may block the blood supply to vital organs.
A and B each have specific A and B antibodies respectively, AB has both A and B antibodies, and O has none at all. This means that AB types are universal recipients and can receive any type of blood, while A can receive A and O, B can receive B and O, and O (although it is the universal donor) can only receive O blood. In rare instances, when an incompatible form of blood is used for a transfusion, the recipient’s immune system will mark the new red blood cells as a threat and begin destroying them, which triggers excessive clotting and may block the blood supply to vital organs.
ABO incompatibility reactions, however, do not typically take place during pregnancy despite the mother and baby’s potentially having different blood types. This is because their blood doesn’t actually mix during pregnancy, but is instead separated by the placental membrane. The placenta is the organ which forms in utero and through which oxygen and nutrients pass from the mother to the baby. Blood, however, does not usually pass through the placental membrane during the pregnancy unless there is a miscarriage, but blood mixing can occur during childbirth.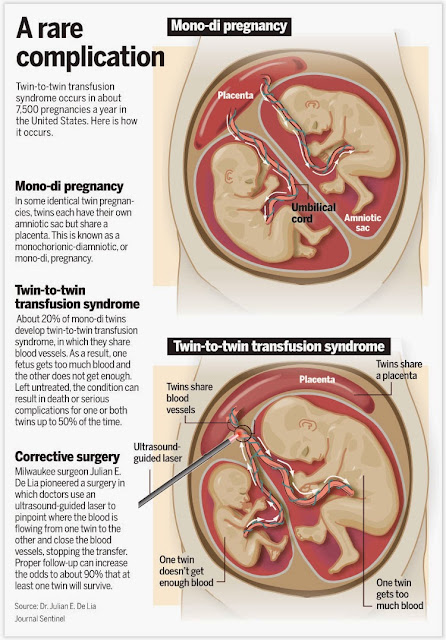 If a placental breach occurs and the two blood types mix, the destruction of red blood cells can cause the waste product bilirubin to accumulate, giving the baby a yellow color and leading to the condition commonly known as jaundice in the hours immediately after birth. Jaundice, however, is a treatable condition that normally does not pose any long-term harm to the infant. Severe conditions caused by extremely high bilirubin levels, such as acute bilirubin encephalopathy and kernicterus, only ensue if jaundice is left untreated and are fairly rare given that the signs of jaundice--yellowing of the skin and the whites of the eyes--are easy to spot. Although there is a slight risk that anaemia may occur following ABO incompatibility reaction, the infant will usually be monitored for low red blood cell count at the first sign of jaundice. Protein Incompatibility?
If a placental breach occurs and the two blood types mix, the destruction of red blood cells can cause the waste product bilirubin to accumulate, giving the baby a yellow color and leading to the condition commonly known as jaundice in the hours immediately after birth. Jaundice, however, is a treatable condition that normally does not pose any long-term harm to the infant. Severe conditions caused by extremely high bilirubin levels, such as acute bilirubin encephalopathy and kernicterus, only ensue if jaundice is left untreated and are fairly rare given that the signs of jaundice--yellowing of the skin and the whites of the eyes--are easy to spot. Although there is a slight risk that anaemia may occur following ABO incompatibility reaction, the infant will usually be monitored for low red blood cell count at the first sign of jaundice. Protein Incompatibility?
Rh incompatibility reactions, although more common, poise a similarly low level of concern. Rh stands for ‘Rhesus factor,’ a specific protein found on the surface of blood cells, and its presence is indicated by either a positive or negative sign which accompanies the letter of your blood type (i.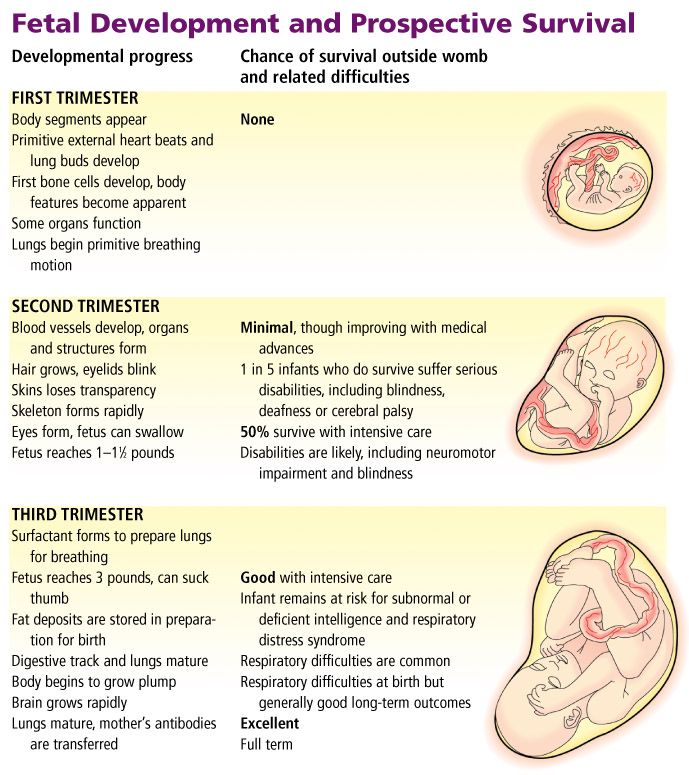 .e, AB+, O-). Like ABO incompatibility reactions, Rh incompatibility reactions are relatively rare occurrences that only occur during a placental breach--but there’s a slight twist involved. Most people (about 85%), are Rh+, and therefore there most women have no risk of health complications if there is a breach in the placental membrane. Potential problems arise, however, if the mother is Rh- and the baby is Rh+. In this case, if there is a breach and a mixing of Rh+ and Rh- within the mother’s body, she may develop Rh antibodies. These antibodies pose no risk to the mother following the birth of her first child, but if a second pregnancy occurs and blood mixing occurs once more, these antibodies will attack the red blood cells of the fetus and lead to anaemia. Fortunately, this can be prevented through injections of anti-D gammaglobulin (or simply ‘anti-D’) if the mother has not yet started to produce the antibodies. If she has, the fetus can be monitored and if necessary, receive a blood transfusion through the umbilical cord while in utero.
.e, AB+, O-). Like ABO incompatibility reactions, Rh incompatibility reactions are relatively rare occurrences that only occur during a placental breach--but there’s a slight twist involved. Most people (about 85%), are Rh+, and therefore there most women have no risk of health complications if there is a breach in the placental membrane. Potential problems arise, however, if the mother is Rh- and the baby is Rh+. In this case, if there is a breach and a mixing of Rh+ and Rh- within the mother’s body, she may develop Rh antibodies. These antibodies pose no risk to the mother following the birth of her first child, but if a second pregnancy occurs and blood mixing occurs once more, these antibodies will attack the red blood cells of the fetus and lead to anaemia. Fortunately, this can be prevented through injections of anti-D gammaglobulin (or simply ‘anti-D’) if the mother has not yet started to produce the antibodies. If she has, the fetus can be monitored and if necessary, receive a blood transfusion through the umbilical cord while in utero.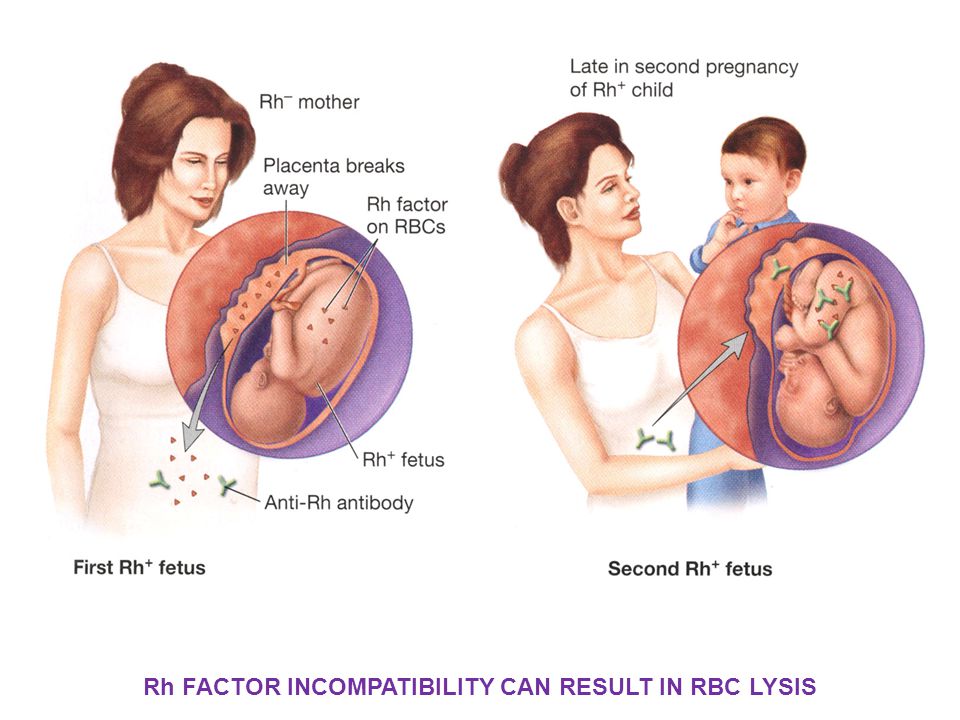
What does this mean for you?
In short, while blood mixing (either in utero or during childbirth) is possible, it is unlikely--and any potential consequences can most often either be prevented or properly monitored by hospital staff. If you have more questions on this topic, particularly with regard to how it applies to you, we recommend that you consult a doctor. Here are some tips on how to find a doctoror therapist in Singapore. You can also speak to a doctor online on RingMD from wherever you are (just click the button below).
Our world-class online doctors can provide you with medical advice, and depending on where you are, they may also be able to write you a medical certificate and online prescription. You have a right to deal with your pain. We’re working to make sure everyone takes health and wellness issues more seriously, and everyone gets the care they need.
If you're a doctor or wellness expert considering offering virtual care services, here are some arguments to consider.
Fetus shares stem cells to repair damaged mother's heart
A remarkable discovery was made by a group of American researchers led by Hina Chaudhry from New York's Mount Sinai Hospital. In experiments on transgenic laboratory mice, for the first time, it was possible to show that the fetus "provides" its cells to restore the functions of the damaged mother's myocardium.
Some facts
Our body contains cells that carry foreign DNA, that is, we are all chimeras. According to Greek mythology, a chimera is a creature that was considered invincible, whose body consisted of parts of many animals. In medicine, the term "chimerism" began to be used in cases where animals or humans acquire someone else's genetic component, for example, as a result of organ transplantation. In this case, the number of donor cells is large. During pregnancy, during blood transfusion, the amount of foreign cellular material is very small, and this phenomenon is called "microchimerism".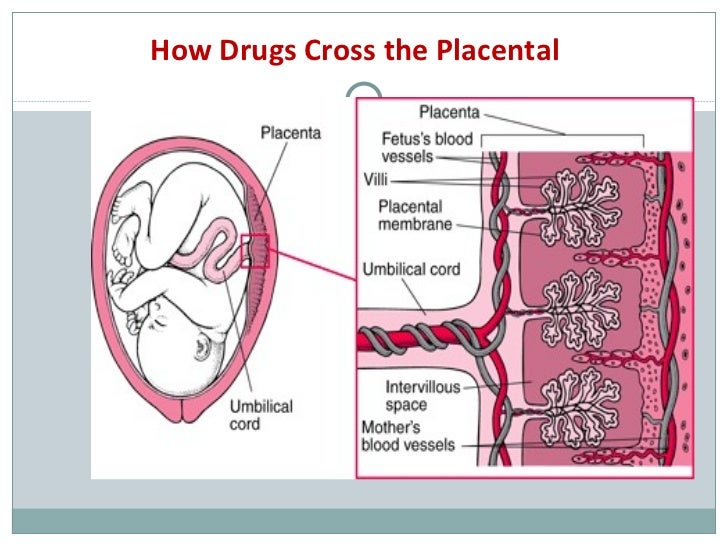 Scientists have found that mother's cells can enter the child's body through the placenta, while the fetus, in turn, is able to "share" its cells with the mother through the same placenta. Fraternal twins, while in the womb, also exchange cells. Apparently, through the mother's body, we can get the cells of older brothers and sisters who were in it before us, or almost the cells of grandmothers... It was possible to find preserved cells XX (female) in healthy adult men, and one of them by that time was 46 years old. The cells of the child in the body of the mother, as it turned out, could also demonstrate amazing vitality. For example, in a woman who had never received a transfusion of donor blood, the Y chromosome (male) was found in the blood several decades after she gave birth to sons.
Scientists have found that mother's cells can enter the child's body through the placenta, while the fetus, in turn, is able to "share" its cells with the mother through the same placenta. Fraternal twins, while in the womb, also exchange cells. Apparently, through the mother's body, we can get the cells of older brothers and sisters who were in it before us, or almost the cells of grandmothers... It was possible to find preserved cells XX (female) in healthy adult men, and one of them by that time was 46 years old. The cells of the child in the body of the mother, as it turned out, could also demonstrate amazing vitality. For example, in a woman who had never received a transfusion of donor blood, the Y chromosome (male) was found in the blood several decades after she gave birth to sons. Qui prodest - look for who benefits
Why do we need this constant traffic and what do "strangers" do in our body? What is the cost of maternity? There are many theories about this. Their essence lies in the dual effect of “little pieces of alien life” on the host organism, ranging from the repair of damaged organs and tissues to autoimmune diseases (does the immune system attack foreign cells?) and oncology.
Elegant experiment Hina Chaudhry
Scientists managed to introduce the green fluorescent protein gene into the body of male mice, and this led to the fact that almost all somatic cells had a green glow. Such "glowing" males were crossed with ordinary females, however, with an experimentally damaged heart. In half of the embryos, the cells carried the green fluorescent protein gene. Two weeks after conception, the females' hearts were removed and found to contain "green" vascular cells and cardiomyocytes. By the way, no green cells were found in any other (healthy) maternal organ. The conclusion here is unequivocal: the fetus came to the aid of the mother, nobly sharing its cellular material ... True, the head of the study, Dr. Chaudhry, makes a more prosaic conclusion: “The usual evolutionary mechanism is evident: the fetus, in order to survive, must be involved in the repair of the damaged host organ.” Fetal Cells Traffic to Injured Maternal Myocardium and Undergo Cardiac differentiation Rina J.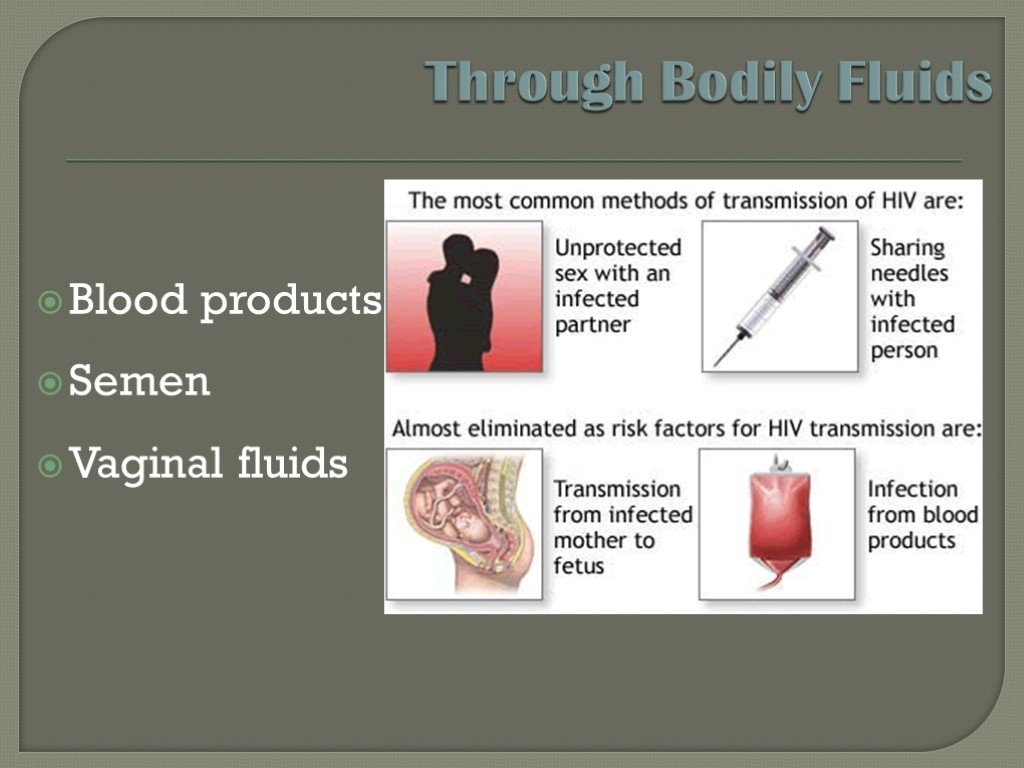 Kara, Paola Bolli, Ioannis Karakikes, Iwao Matsunaga, Joseph Tripodi, Omar Tanweer, Perry Altman, Neil S. Shachter, Austin Nakano, Vesna Najfeld and Hina W. Chaudhry Circulation Research published online November 14, 2011
Kara, Paola Bolli, Ioannis Karakikes, Iwao Matsunaga, Joseph Tripodi, Omar Tanweer, Perry Altman, Neil S. Shachter, Austin Nakano, Vesna Najfeld and Hina W. Chaudhry Circulation Research published online November 14, 2011 Makarov I.O. • The placenta and its role in the development of pregnancy
Ultrasound scanner WS80
An ideal tool for prenatal examinations. Unique image quality and a full range of diagnostic programs for an expert assessment of a woman's health.
From the very beginning of pregnancy and up to its end, the mother-placenta-fetus system is formed and functions . The most important component of this system is the placenta , which is a complex organ in the formation of which derivatives of the trophoblast and embryoblast take part, as well as decidual tissue . The function of the placenta, first of all, is aimed at providing sufficient conditions for the physiological course of pregnancy and the normal development of the fetus.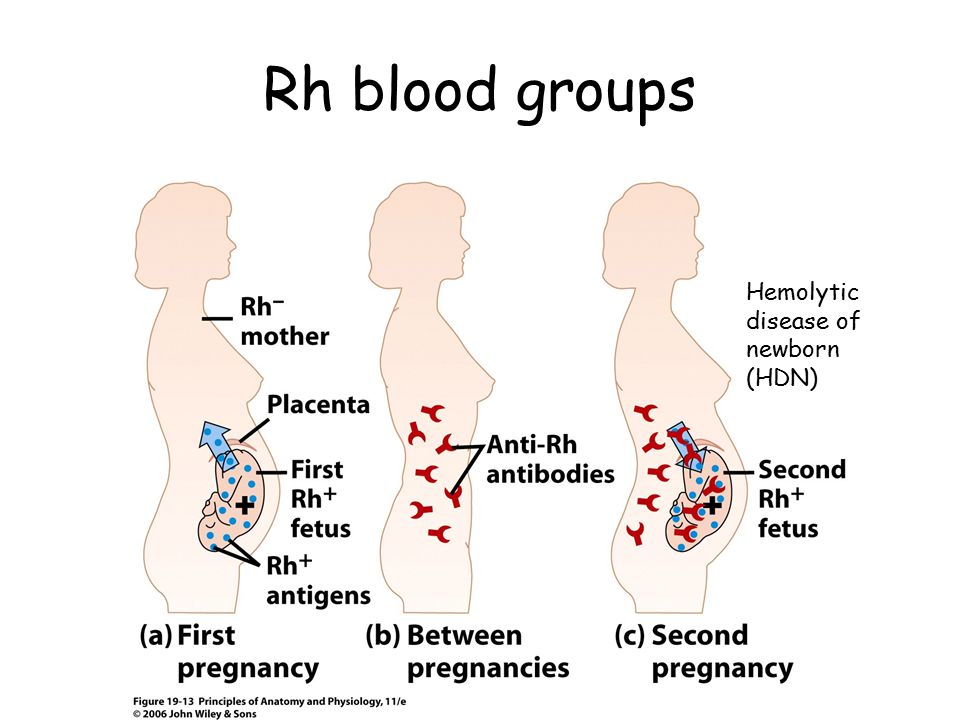 These functions include: respiratory, nutritional, excretory, protective, endocrine. All metabolic, hormonal, immune processes during pregnancy are provided through maternal and fetal vascular system . Despite the fact that the blood of the mother and fetus does not mix, since their is separated by the placental barrier , the fetus receives all the necessary nutrients and oxygen from the mother's blood. The main structural component of the placenta is villous tree .
These functions include: respiratory, nutritional, excretory, protective, endocrine. All metabolic, hormonal, immune processes during pregnancy are provided through maternal and fetal vascular system . Despite the fact that the blood of the mother and fetus does not mix, since their is separated by the placental barrier , the fetus receives all the necessary nutrients and oxygen from the mother's blood. The main structural component of the placenta is villous tree .
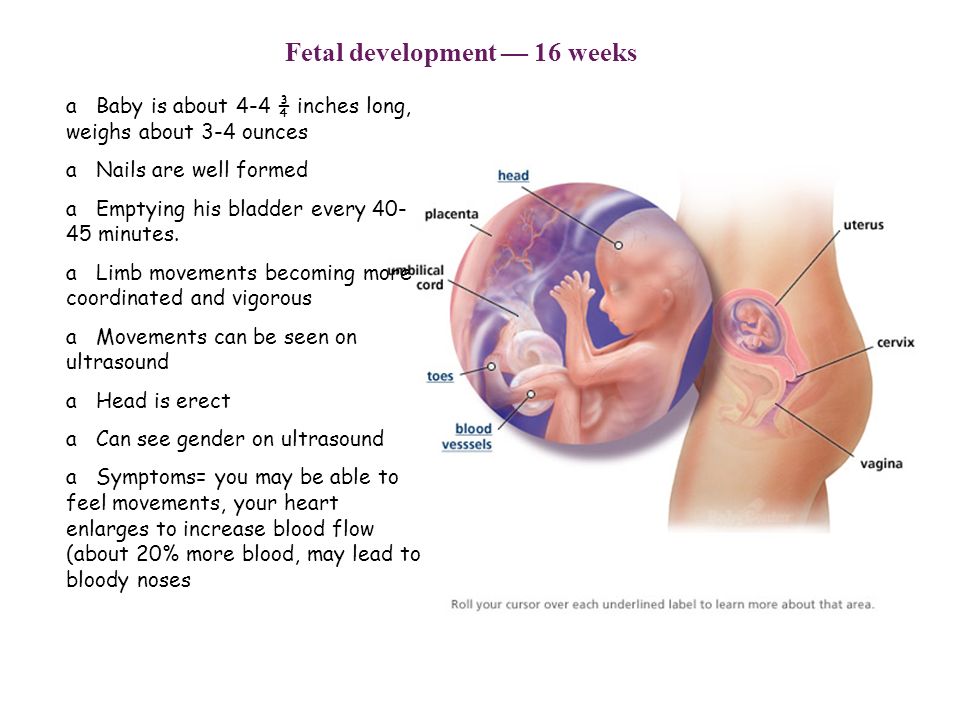
In the normal development of pregnancy, there is a relationship between the growth of the fetus, its body weight and the size, thickness, weight of the placenta. Up to 16 weeks of pregnancy, the development of the placenta outstrips the growth rate of the fetus. In case of death embryo (fetus) inhibition of growth and development of chorionic villi and progression of involution-dystrophic processes in the placenta. Having reached the required maturity at 38-40 weeks of pregnancy, the processes of formation of new vessels and villi in the placenta stop.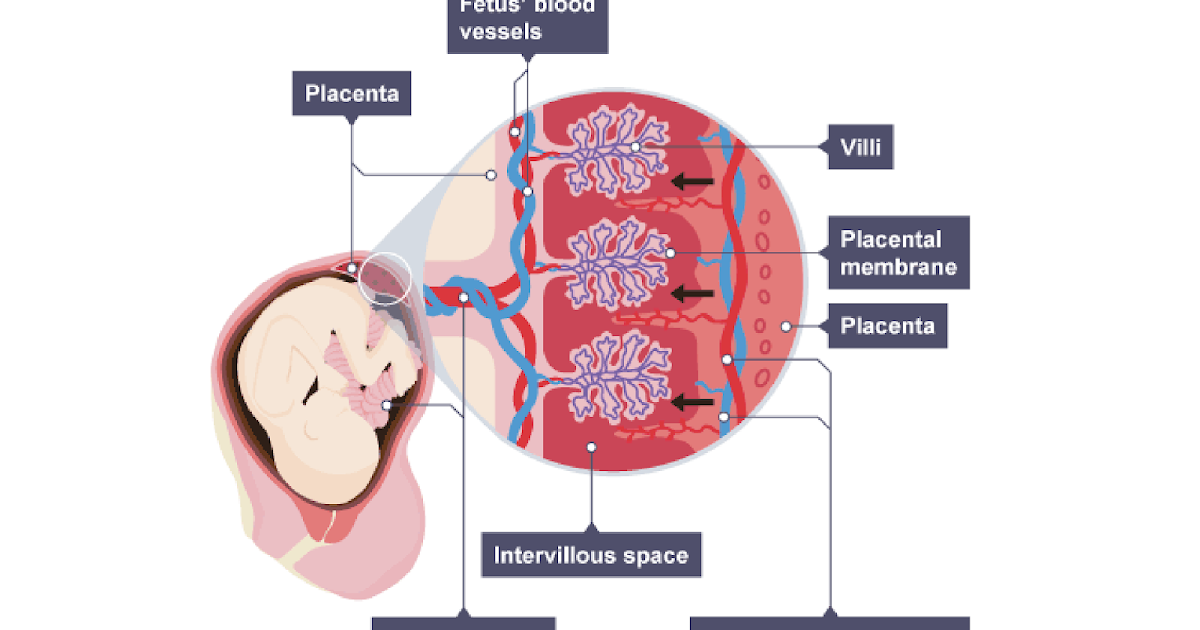
Diagram of the structure of the placenta and uteroplacental circulation
1 - umbilical cord arteries
2 - stem villi
3 - decidual septum
4 - decidua
5 - myometrium
6 - veins
7 - spiral arteries
8 - chorion
9 - amnion
10 - intervillous space
11 - vein of the umbilical cord
12 - cotyledon
The mature placenta is a disk-shaped structure 15-20 cm in diameter and 2.5-3.5 cm thick. Its mass reaches 500-600 g. The maternal surface of the placenta , which faces the uterine wall, has a rough surface formed by the structures of the basal part of the decidua.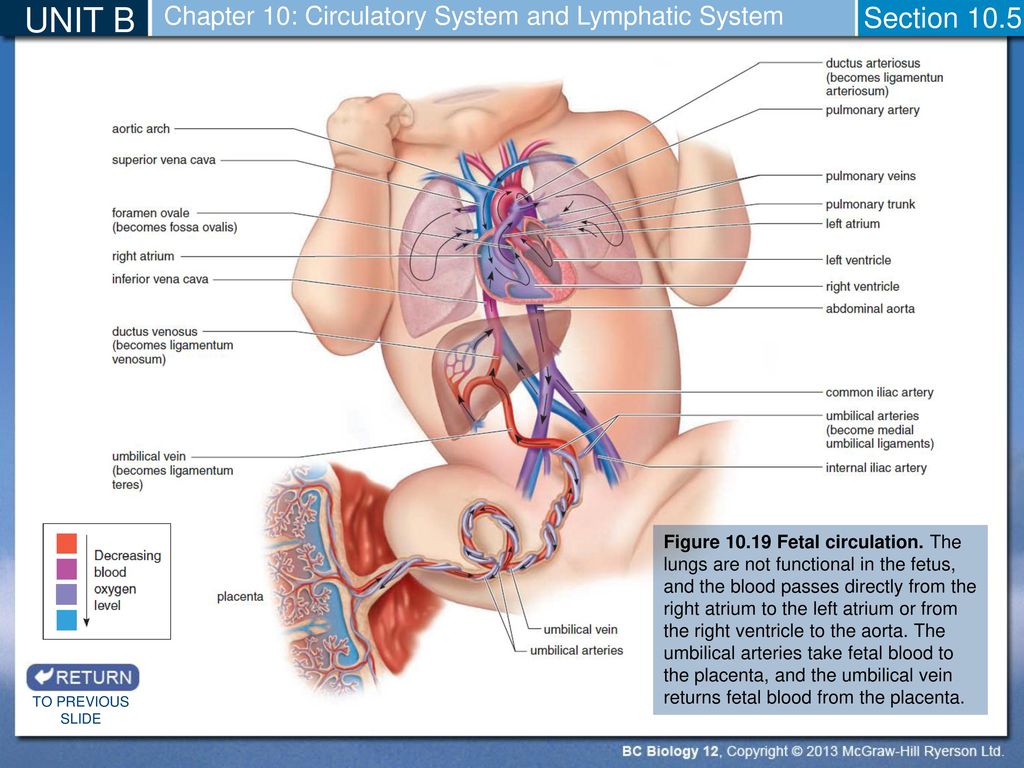 The fetal surface of the placenta , which faces the fetus, is covered with amniotic sheath . Under it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fruiting part of the placenta is represented by numerous chorionic villi , which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta, there are 30 to 50 cotyledons. Cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the 1st order are its trunk, the villi of the 2nd and 3rd orders are large and small branches, the intermediate villi are small branches, and the terminal villi are leaves. Cotyledons are separated from each other by partitions (septa) emanating from the basal plate.
The fetal surface of the placenta , which faces the fetus, is covered with amniotic sheath . Under it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fruiting part of the placenta is represented by numerous chorionic villi , which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta, there are 30 to 50 cotyledons. Cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the 1st order are its trunk, the villi of the 2nd and 3rd orders are large and small branches, the intermediate villi are small branches, and the terminal villi are leaves. Cotyledons are separated from each other by partitions (septa) emanating from the basal plate.
Intervillous space on the fruit side is formed by the chorionic plate and villi attached to it, and on the maternal side it is limited by the basal plate, decidua and septa extending from it.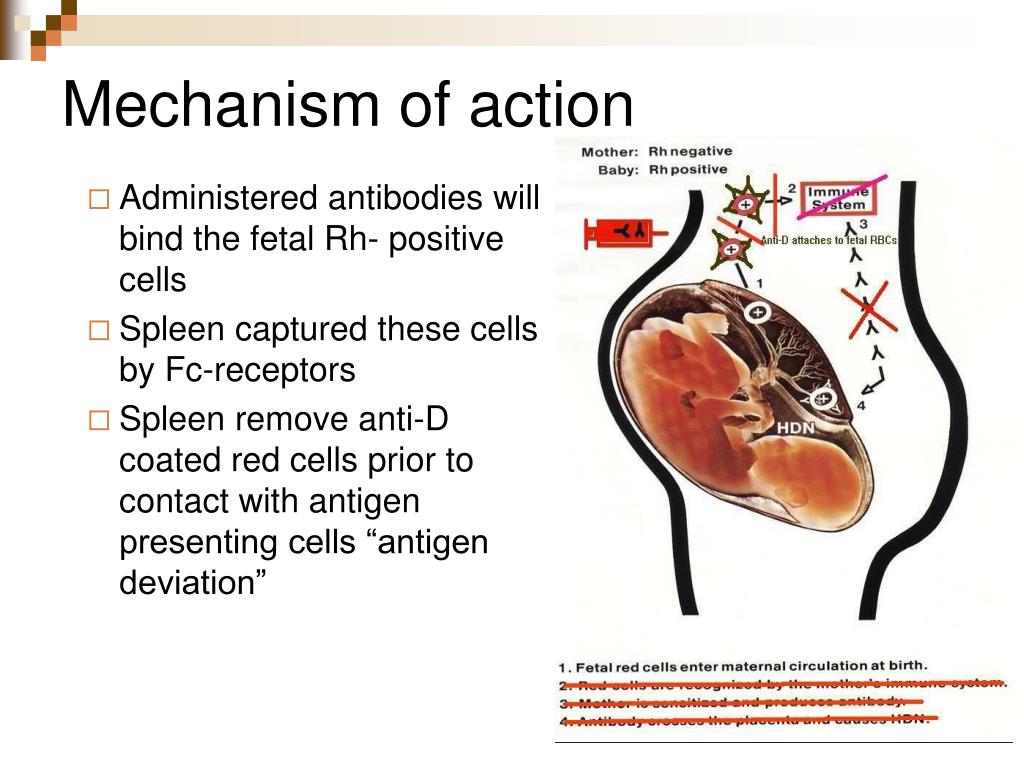 Most placental villi are freely immersed in the intervillous space and are bathed in maternal blood . There are also anchor villi, which are fixed to the basal decidua and provide attachment of the placenta to the wall of the uterus.
Most placental villi are freely immersed in the intervillous space and are bathed in maternal blood . There are also anchor villi, which are fixed to the basal decidua and provide attachment of the placenta to the wall of the uterus.
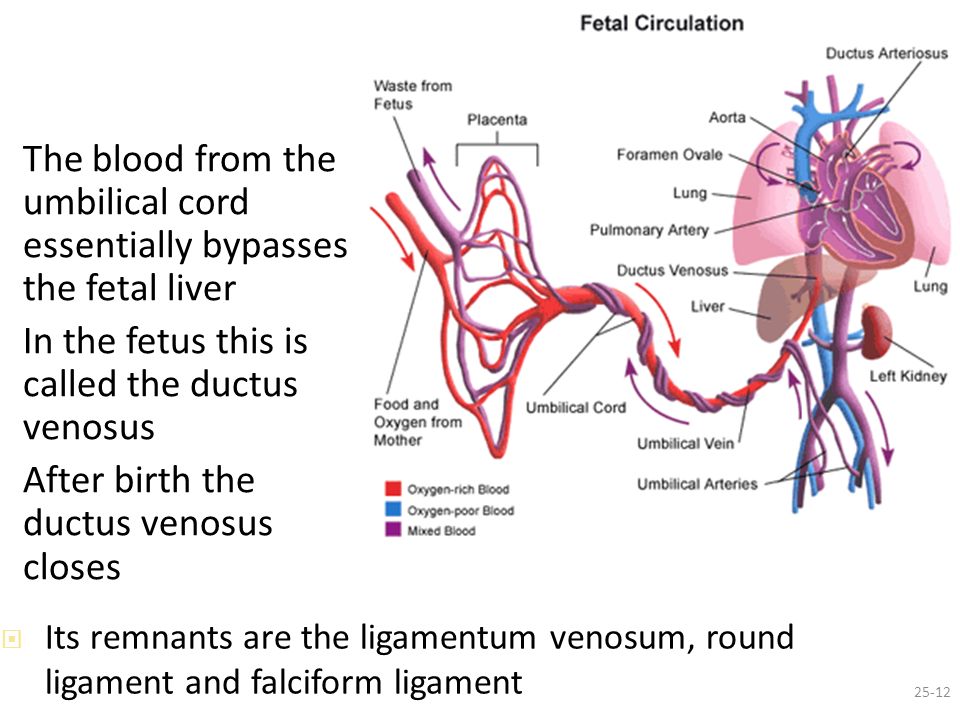
Diagram of blood circulation in the fetus
1 - superior vena cava
2 - oval hole
3 - inferior vena cava
4 - venous duct
5 - portal sinus
6 - portal vein
7 - vein of the umbilical cord
8 - umbilical cord arteries
9 - placenta
10 - epigastric arteries
11 - ductus arteriosus
Spiral arteries , which are the terminal branches of the uterine and ovarian arteries, supplying the pregnant uterus , open into the intervillous space with 120-150 orifices, providing a constant flow of maternal oxygen-rich blood into the intervillous space.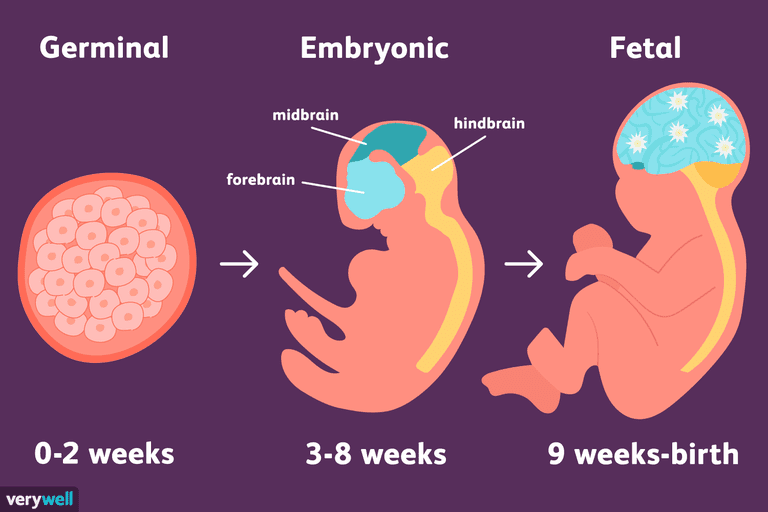 Due to pressure difference , which is higher in the maternal arterial bed compared to the intervillous space, oxygenated blood from the orifices of the spiral arteries is directed through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the maternal blood flow through venous orifices. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix among themselves.
Due to pressure difference , which is higher in the maternal arterial bed compared to the intervillous space, oxygenated blood from the orifices of the spiral arteries is directed through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the maternal blood flow through venous orifices. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix among themselves.
The transition of blood gases, nutrients , metabolic products and other substances from maternal blood to fetal and back is carried out at the moment of contact of the villi with the mother's blood through the placental barrier . It is formed by the outer epithelial layer of the villus, the stroma of the villus, and the wall of the blood capillary located inside each villus. Fetal blood flows through this capillary. Saturated in this way with oxygen, the blood of the fetus from the capillaries of the villi is collected into larger vessels, which eventually combine into vein of the umbilical cord , through which oxygenated blood flows to the fetus .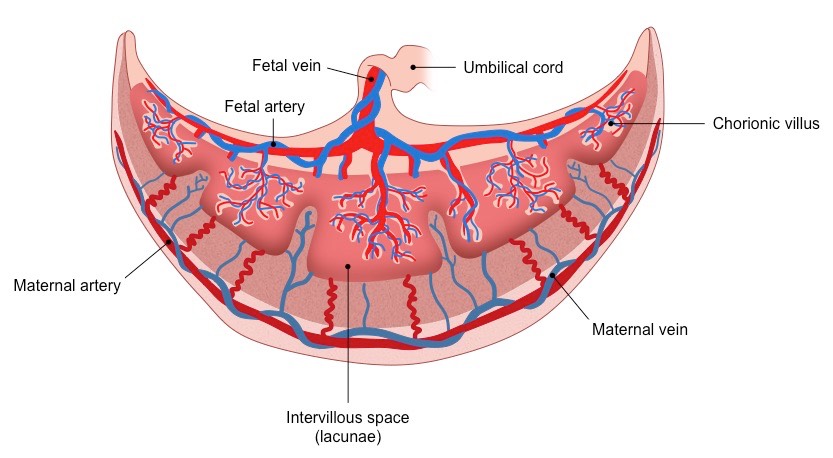 Having given up oxygen and nutrients in the fetal body, blood, depleted in oxygen and rich in carbon dioxide, flows from the fetus through two umbilical arteries to the placenta , where these vessels divide radially in accordance with the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage through the placental barrier of blood gases and nutrients, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the bloodstream of the fetus and carbon dioxide and other metabolic products of the fetus are excreted . At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.
Having given up oxygen and nutrients in the fetal body, blood, depleted in oxygen and rich in carbon dioxide, flows from the fetus through two umbilical arteries to the placenta , where these vessels divide radially in accordance with the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage through the placental barrier of blood gases and nutrients, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the bloodstream of the fetus and carbon dioxide and other metabolic products of the fetus are excreted . At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.
Scheme of the placental barrier
1 - capillary endothelium of terminal villi
2 - villi capillary
3 - villus stroma
4 - epithelial cover of villi
The placenta performs an important protective (barrier) function through the placental barrier, which is selectively permeable in both directions. In the normal course of pregnancy, the permeability of the placental barrier increases up to 32-34 weeks of pregnancy, after which it decreases in a certain way. However, unfortunately, a fairly large number of drugs, nicotine, alcohol, narcotic substances, pesticides, other toxic chemicals, as well as a number of pathogens of infectious diseases penetrate the placental barrier relatively easily into the fetal circulation, which has an adverse effect on the fetus. In addition, under the influence of pathogenic factors, the barrier function of the placenta is even more disturbed.
In the normal course of pregnancy, the permeability of the placental barrier increases up to 32-34 weeks of pregnancy, after which it decreases in a certain way. However, unfortunately, a fairly large number of drugs, nicotine, alcohol, narcotic substances, pesticides, other toxic chemicals, as well as a number of pathogens of infectious diseases penetrate the placental barrier relatively easily into the fetal circulation, which has an adverse effect on the fetus. In addition, under the influence of pathogenic factors, the barrier function of the placenta is even more disturbed.
The placenta is anatomically and functionally related to the amnion (aqueous membrane) that surrounds the fetus. The amnion is a thin membrane that lines the surface of the placenta facing the fetus, passes to the umbilical cord and merges with the skin of the fetus at the umbilical ring. Amnion is actively involved in the exchange of amniotic fluid , in a number of metabolic processes, and also performs a protective function.