Do they test for hep c in pregnancy
Test for Hepatitis C During Every Pregnancy
As of April 2020, the Centers for Disease Control and Prevention (CDC) recommends that prenatal care providers screen all pregnant persons for hepatitis C, a liver infection caused by the hepatitis C virus (HCV). Chronic HCV infection does not cause symptoms in most people but can lead to cirrhosis and liver cancer. Several studies have linked maternal HCV infection with worse pregnancy outcomes. Hepatitis C can be transmitted from a mother to her baby. Identifying hepatitis C in pregnant people allows them to access treatment and identifies at-risk infants in need of testing and ongoing monitoring, as needed.
Why Test All Your Pregnant Patients?
- New cases of hepatitis C are on the rise among reproductive aged adults. Rates of new HCV infections increased by more than 60% from 2015 to 2019. And in 2019, more than 63% of new HCV infections occurred among adults 20-39 years of age.
- CDC expects rates of perinatal hepatitis C to increase.
Rates of HCV infection nearly doubled during 2009–2014 among people with live births. From 2011-2014, an estimated 29,000 HCV-infected patients gave birth each year. HCV can be transmitted from an infected mother to the child during both pregnancy and childbirth.[i] HCV-infected mothers transmit their infection to their baby in 5.8% of pregnancies; the risk of transmission is higher if the mother is co-infected with HIV. As capacity for viral hepatitis surveillance improves, CDC anticipates that the number of perinatal hepatitis C cases identified and reported to CDC will increase.
- Hepatitis C can lead to serious liver disease. More than half of new hepatitis C infections progress to chronic HCV infection. Without treatment, approximately 15-20% of people living with chronic HCV infection will develop progressive liver fibrosis and cirrhosis.
- Hepatitis C can be cured. Over 90 percent of people infected with HCV can be cured with 8-12 weeks of oral therapy.
 [ii] Hepatitis C curative treatment is not currently approved for use during pregnancy; however, once the mother has given birth and completed breastfeeding, it is safe to begin this treatment. Furthermore, treatment is approved for children beginning at 3 years of age.
[ii] Hepatitis C curative treatment is not currently approved for use during pregnancy; however, once the mother has given birth and completed breastfeeding, it is safe to begin this treatment. Furthermore, treatment is approved for children beginning at 3 years of age. - Your patients aren’t aware of their risk. Almost half of people with hepatitis C are unaware of their infection. Testing is the first step to accessing curative treatment.
- Testing can connect mother and baby to care. All pregnant persons should be tested for hepatitis C during each pregnancy; screening during pregnancy can identify future care needs for both mother and baby.
What are CDC’s Hepatitis C Screening Recommendations?
All pregnant people should be screened for hepatitis C during each pregnancy, except in settings where the prevalence of HCV infection (HCV RNA-positivity) is <0.1%. [iii]
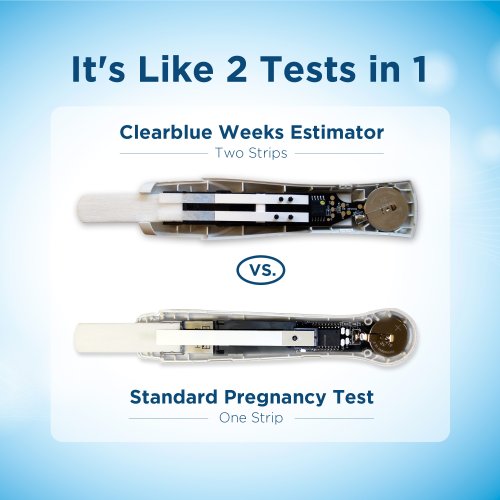
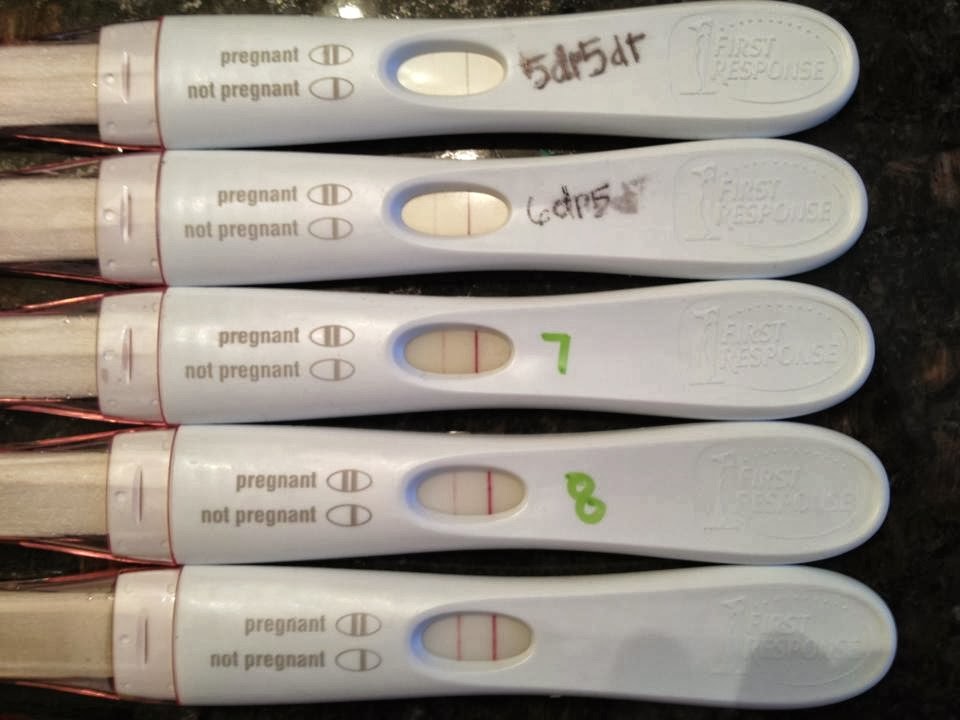
Hepatitis C testing is usually initiated with an HCV antibody test which, if positive, indicates a history of past or present HCV infection. Any pregnant person testing positive for antibodies to HCV should receive a PCR test for HCV RNA to determine current infection status. Children born to HCV-infected mothers should be tested for HCV; HCV RNA testing can occur as early as 2 months of age, whereas testing for HCV antibodies (anti-HCV) should not occur before 18 months of age because antibodies to HCV from the mother might last until this age.
Any pregnant person testing positive for antibodies to HCV should receive a PCR test for HCV RNA to determine current infection status. Children born to HCV-infected mothers should be tested for HCV; HCV RNA testing can occur as early as 2 months of age, whereas testing for HCV antibodies (anti-HCV) should not occur before 18 months of age because antibodies to HCV from the mother might last until this age.
What Should I do if a Pregnant Patient Tests Positive for Hepatitis C Virus?
- Test: The initial evaluation of persons diagnosed with HCV during pregnancy is generally similar to that of nonpregnant persons diagnosed with HCV and should include an HCV RNA level and a liver enzymes test. Pregnant persons with newly diagnosed HCV infection and abnormal serum aminotransferase and/or platelet levels should be promptly referred for further medical assessment to rule out liver fibrosis or injury and so antiviral treatment can be initiated at the appropriate time.
- Report: Providers should report HCV infection in a pregnant person to infant’s health care provider so that follow-up HCV testing can be conducted at the recommended time, and to the local health department so that ongoing risk factors can be assessed and relevant contacts can receive hepatitis A and hepatitis B testing and vaccination, as indicated, and can be linked, as appropriate, to preventive services.
Additional Resources
- CDC Recommendations for Hepatitis C Screening Among Adults — United States, 2020
- The ABCs of Hepatitis – For Health Professionals pdf icon[PDF – 3 pages] fact sheet
- Algorithm for testing and follow-up of HCV-exposed healthcare personnel pdf icon[PDF – 2 pages]
- Interpretation of Results of Tests for Hepatitis C Virus (HCV) Infection and Further Actions pdf icon[PDF – 1 page]
- Recommended Testing Sequence for Identifying Current Hepatitis C Virus (HCV) Infection pdf icon[PDF – 1 page]
- Increased Risk for Mother-to-Infant Transmission of Hepatitis C Virus Among Medicaid Recipients ― Wisconsin, 2011–2015
- Routine Hepatitis C Virus Screening in Pregnant Individualsexternal icon, Practice Advisory; American College of Obstetricians and Gynecologists, May 2021
- Hepatitis C Virus in Pregnancy: Are We Ready for Test and Treat?external icon
- University of Washington Hepatitis C Onlineexternal icon—up-to-date comprehensive educational website (offers CMEs) for diagnosing, monitoring, and managing HCV infection.
- Core Concepts – Perinatal HCV Transmission – Treatment of Key Populations and Unique Situations – Hepatitis C Online (uw.edu)
- CDC’s Know More Hepatitis website—resources to help educate your pregnant patients about hepatitis C.
- HCV Guidance: Recommendations Testing, Managing and Treating Hepatitis C; HCV in Pregnancyexternal icon
- Hughes et al. Hepatitis C in pregnancy: screening, treatment, and management. Am J Obstet Gynecol 2017;217:B2-B12. doi: 10.1016/j.ajog.2017.07.039. Epub 2017 Aug 4.
Notes
[i] Breastfeeding is not considered a route of transmission if nipples are not cracked and bleeding.
[ii] While there are currently no treatments approved for use in pregnancy to prevent transmission of HCV to infants, screening during pregnancy can connect both mother and infant to care.
[iii] See CDC’s hepatitis C testing guidelines for detailed information on calculating prevalence in a health-care setting.
Prenatal hepatitis C screening can spare women and babies from long-term liver damage | Your Pregnancy Matters
Getting a simple blood screening for hepatitis C can help spare you and your baby from potential liver damage.
In April 2020, the Centers for Disease Control and Prevention (CDC) began recommending routine prenatal screening for hepatitis C, a liver-damaging virus that can be passed to the fetus during pregnancy. The American College of Obstetricians and Gynecologists (ACOG) began recommending the same in May 2021.
Approximately 1-2% of U.S. adults have hepatitis C. According to the CDC, rates of new hepatitis C infections increased by more than 60% from 2015 to 2019. More than half of new cases in 2019 were diagnosed in adults ages 20-29 – the prime reproductive years.
According to ACOG, approximately 6% of babies born to mothers with hepatitis C are infected during pregnancy and delivery. While many infants clear the virus naturally by age 2, 20-25% may develop cirrhosis of the liver by age 8.
Unfortunately, hepatitis C – also called “hep C” – bears a stigma because it is spread through contact with infected blood. Patients may be infected during contact with unsterile needles from piercing or tattooing, needle-based drug use, unprotected sex, or receipt of a blood transfusion prior to 1992, when more stringent donor testing was implemented.
That last risk hits home. My daughters were born in 1991 and had to stay in the neonatal intensive care unit (NICU) where they received blood transfusions, putting them at higher risk.
Even if you feel these risk factors don’t apply to you today, it’s possible to have contracted the disease in the past without knowing it. Many patients with hepatitis C do not have symptoms; those who do may experience vague symptoms such as these within 6-12 weeks after infection:
- Fatigue
- Nausea
- Poor appetite
- Fever
- Chills
- Headache
- Sore throat
- Joint pain
Fortunately, more than 90% of adults with hepatitis C can be cured with 8-12 weeks of oral antiviral medication. However, without medical care, the disease may progress into chronic hepatitis C, which can cause cirrhosis of the liver (scarring of the liver tissue), liver failure, and liver cancer.
The goals of routine hepatitis C screening are twofold: to present women with judgment-free treatment options to pursue after delivery and to plan for proper screening and potential treatment of the baby, reducing the child’s risk of long-term liver damage.
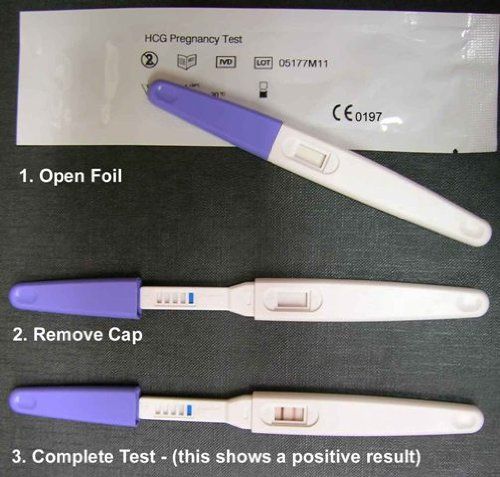
How does hepatitis C screening work?
A simple blood draw can tell us whether you have hepatitis C antibodies, which indicate a past infection. Patients whose past infections were successfully eradicated – either through treatment or by their body’s own immune system – are at very low risk of passing the virus to the baby after delivery.
The screening also detects bits of the hepatitis C virus in the blood, which can indicate a chronic infection. Patients with chronic hepatitis C will always have the virus and will need treatment to manage it.
Related reading: Hepatitis C doesn't have to be a life sentence
What if I have chronic hepatitis C?
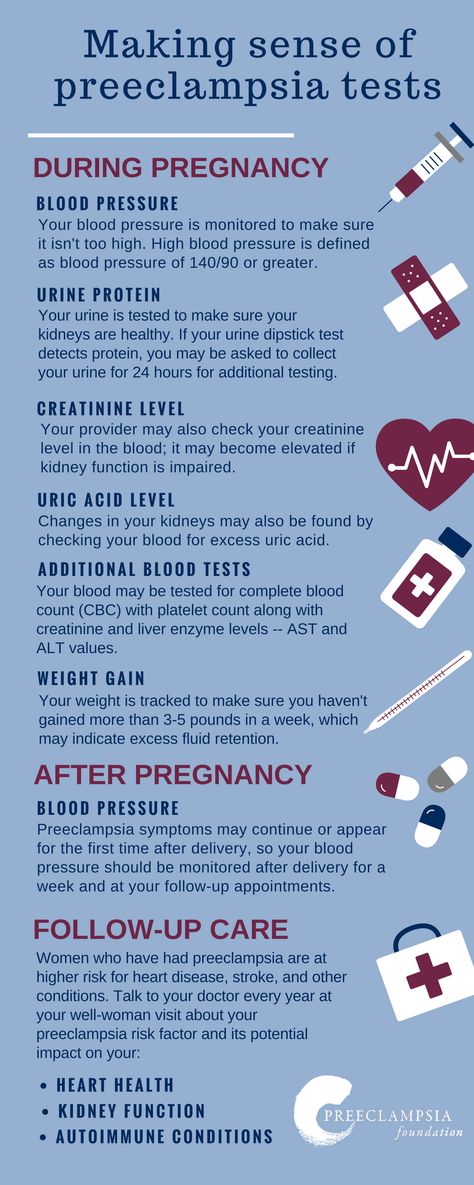
Talk with your doctor about the best strategies to protect your health and the baby’s long term. If you have liver disease, such as cirrhosis of the liver, you may be at increased risk of pregnancy complications such as preeclampsia or preterm birth.
To date, no treatment options for pregnant patients and children younger than 3 are approved by the U. S. Food and Drug Administration. This is because many antiviral drugs can increase the risk of pregnancy complications and/or birth defects.
S. Food and Drug Administration. This is because many antiviral drugs can increase the risk of pregnancy complications and/or birth defects.
After the baby arrives, you both might need specialized care, which may include:
- Getting you on medication to clear the infection and manage or prevent liver damage
- Screening or testing of the baby in the year after delivery
- Planning for treatment in early childhood if the baby is infected and does not clear the infection naturally by age 2
Related reading: Hepatitis C treatment after liver cancer reduces risk of death by 50%
What if I test positive for hepatitis C during pregnancy?
If you are diagnosed during pregnancy, know that there are safe, effective treatments you can get after your baby is born. Depending on the severity of your condition, you might need oral antiviral medication for eight to 12 weeks or a combination of pills and injections for 12-48 weeks to slow or stop the virus.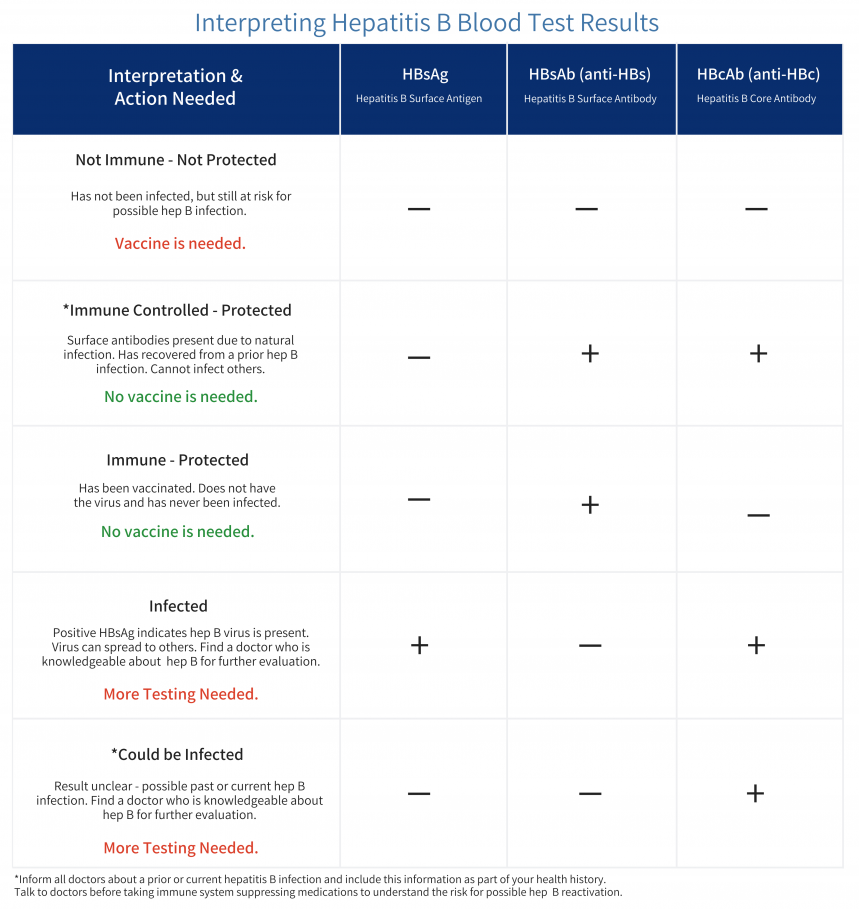
Although blood contact is the main transmission method of hepatitis C, the risk of the baby being infected during labor and delivery is low. Discuss with your doctor strategies that may reduce the risk of transmission.
However, there is no need to plan for a cesarean section (C-section) solely because a patient is infected. Women with hepatitis C also do not have to avoid breastfeeding unless their nipples are cracked or bleeding.
Will my baby need special testing if I have hepatitis C?
Testing the baby right after delivery will not provide a definitive “yes” or “no” about whether the baby is or will be infected. Though the risk is low, it is possible for the mother’s hepatitis C antibodies to appear in the baby’s blood for up to 18 months, even if the child itself is not infected.[MO2]
Current infant screening guidelines from the American Association for the Study of Liver Diseases and the CDC recommend that all babies born to women with hepatitis C get tested for antibodies at 18 months of age, and those who have antibodies should get tested after age 3 to confirm or rule out chronic infection.
While newborns get their first of three vaccinations against hepatitis B within 24 hours after birth, there is no vaccine against hepatitis C. Getting treatment after delivery for yourself and in early childhood for your baby can prevent years of potential liver damage by the hepatitis C virus.
Though it can be scary and overwhelming to talk with a doctor about hepatitis C, please know that our goal is to give you and your baby the very best care – now and in the long term.
To get pre-conception hepatitis C testing or expert prenatal care, call 214-645-8300 or request an appointment online.
What tests are taken during pregnancy
During the happiest period in the life of every woman, you need to think about your health. In addition, testing during pregnancy is mandatory in order to be able to register with a medical institution.
There are a number of mandatory tests for different periods of pregnancy that a woman must pass to determine her health status, as well as to study the conditions for the development of the unborn baby.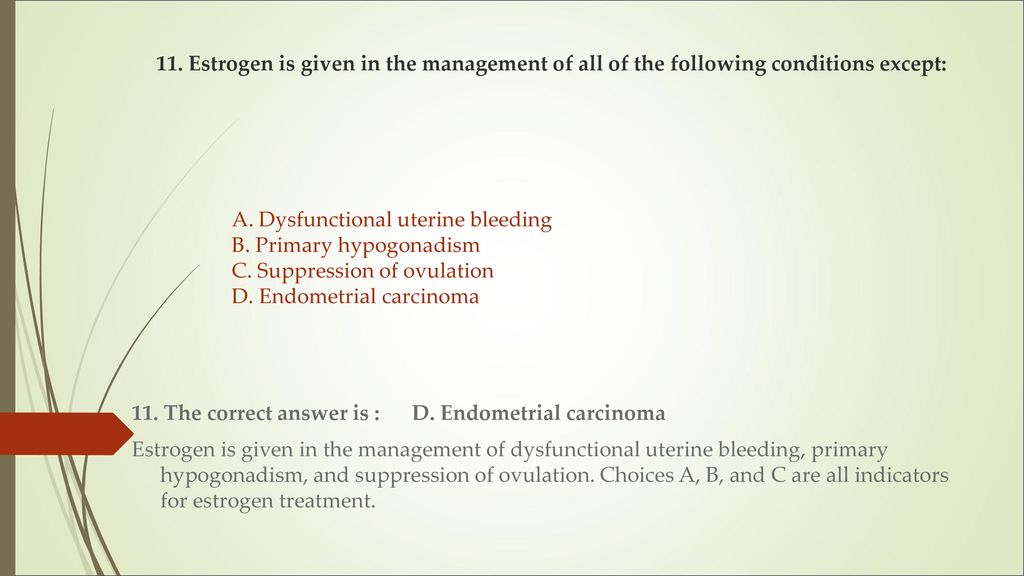 nine0003
nine0003
About what tests are taken during pregnancy, about the order of delivery and the importance of certain tests, we will understand in the article.
Blood tests are considered the most important tests. With the help of these data, it is possible to compile a general picture of the state of health of a pregnant woman, namely, the functional features of almost any organ, as well as the environment for the development of the child.
The first complete blood count is given to a pregnant woman up to 12 weeks. For a period of 18 to 30 weeks, the analysis is taken during each trimester. Blood sampling is done from a finger or a vein. The analysis shows the number of red blood cells, the level of hemoglobin in the blood, and other indicators. nine0003
At least 3 times during the entire pregnancy it is necessary to donate blood for testing for HIV infection and later stages of hepatitis. For analysis, venous blood is taken. The frequency of examination is determined by the fact that this type of infection appears only after 3 months. Women in labor who do not have time to donate blood for HIV and hepatitis are at risk.
Women in labor who do not have time to donate blood for HIV and hepatitis are at risk.
Blood test for biochemistry is an equally important test for pregnant women. With the help of the results obtained, it is possible to determine the functions of the organs and systems of the expectant mother. Such an analysis is simply necessary for pregnant women with chronic diseases of the internal organs. A biochemical analysis is given when registering a pregnant woman, at 18 weeks and at 30. With the help of a biochemical analysis, blood is checked for sugar, that is, for the presence of diabetes mellitus, as well as the function of the kidneys and urinary system. A biochemical blood test also shows the protein composition of the blood, iron, blood electrolytes, cholesterol, creatine and urea. nine0003
When registering, a pregnant woman must make a mandatory blood test for group and Rh, such an analysis is performed even if she knows it. The reason for this is the difficulties that sometimes arise in the case of a negative Rh factor in a pregnant woman and a positive child in the father, or she has the first blood type, and the father has any other.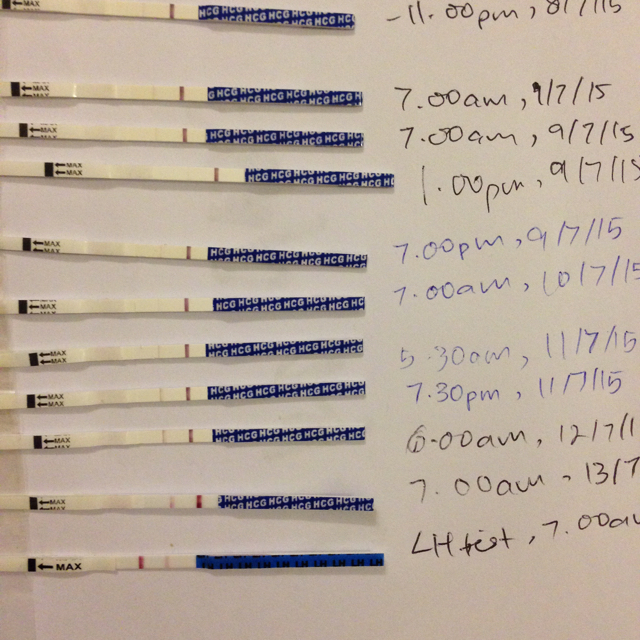 In this case, it is necessary to donate blood for the presence of antibodies and their number once a month. After the twentieth week of pregnancy, you will have to donate blood at least once every two weeks. nine0003
In this case, it is necessary to donate blood for the presence of antibodies and their number once a month. After the twentieth week of pregnancy, you will have to donate blood at least once every two weeks. nine0003
This is a test for the most common infections that can harm the fetus. The analysis is given at the first visit to the doctor, the number of subsequent samplings depends on the results of the analysis. Even if you do not know exactly what tests are taken during pregnancy, you will be warned about the importance of research on these viruses.
The test is taken during a gynecological examination, used to diagnose inflammatory diseases, and can also be used to identify sexually transmitted diseases. nine0003
It is a scraping from the cervix to analyze the cells covering the mucosa. It is used to diagnose diseases of the cervix, namely: background, cancerous and precancerous diseases. This is the type of analysis that a woman or girl over 18 years of age is required to take during an annual gynecological examination.
The essence of colposcopy is to determine the presence of abnormal cells of the cervix.
During pregnancy, a woman should undergo three routine examinations: at 10-14 weeks of pregnancy, at 20-23 weeks and at 30-34. At the first ultrasound, the condition of the placenta, the position of the fetus are determined, and it also determines the exact gestational age and compares the size of the embryo with the norm for this period. At the second ultrasound, the results are compared with the first test, and all indicators are also studied. At the second examination, you can find out the sex of the unborn child. The third ultrasound shows the position of the fetus, and the doctor evaluates these indicators for future births. nine0003
Urinalysis allows you to determine how the kidneys of a pregnant woman are working. During pregnancy, they are very overloaded. The results of the analysis show the number of leukocytes in the urine, the presence of protein in the urine, the level of sugar.
Another very important test during pregnancy is the electrocardiogram. With its help, you can monitor the work of the heart, because during pregnancy it receives additional stress. With the help of an ECG, you can track all deviations and interruptions in the work of the heart, cure them in a timely manner, so that the expectant mother can give birth to a baby normally. nine0003
Apparently, there will be more than enough tests during pregnancy, but every woman should think about the future of her child. After all, it is at this moment, the moment of his development that his body is formed in the womb, and if something goes wrong, the echoes of this will sound throughout his life. Therefore, any woman should know what tests are taken during pregnancy.
Taking care of her health and the health of her baby is the true purpose of any woman. Responsive and highly qualified employees of the medical center will always help with this. nine0003
There are contraindications. Read the instructions or consult a specialist.
Read the instructions or consult a specialist.
Visit other sections of the site:
- Pregnancy monitoring program in Yekaterinburg
- Ultrasound during pregnancy
- Early pregnancy ultrasound
HIV, hepatitis B and C, syphilis during pregnancy - how to get tested
- Syphilis during pregnancy
- HIV infection (AIDS)
- Hepatitis B
- Hepatitis C
- Diagnosis of infections during pregnancy
- Management of pregnancy and childbirth with positive tests
The examination plan of the expectant mother must include the diagnosis of HIV infection, syphilis, viral hepatitis B and C. The importance of these tests is due to the fact that these infections can have a great negative impact on the development of the fetus, and also be transmitted from a pregnant woman to other patients and medical personnel. nine0073
Early diagnosis of syphilis, HIV infections, viral hepatitis B and C allows you to protect the unborn child from infection or prepare in advance for problems if intrauterine infection does occur. All these viral diseases are equally dangerous for the development of pathologies in the fetus, but differ in the degree of contagiousness (the ability to be transmitted from mother to baby), symptoms and diagnostic methods.
All these viral diseases are equally dangerous for the development of pathologies in the fetus, but differ in the degree of contagiousness (the ability to be transmitted from mother to baby), symptoms and diagnostic methods.
Syphilis during pregnancy
This is a sexually transmitted disease caused by Treponema pallidum. In the early stages, syphilis is manifested by painless ulceration in the genital area, most often on the cervix, so outwardly a woman may not notice it at all. If left untreated, the symptoms may subside, and after a while a small rash appears on the palms and feet. It can take from 6 weeks to 6 months before the rash appears from the moment of infection. This stage is called secondary syphilis. If left untreated, the rash resolves on its own, but may reappear periodically within 2 years. At a later stage of the disease - tertiary syphilis - the cardiovascular and nervous systems are affected. The risk of intrauterine infection is very high in primary and secondary syphilis. With intrauterine infection of the fetus, its death often occurs or a child is born with damage to the nervous system, bones, mouth, eyes. nine0003
With intrauterine infection of the fetus, its death often occurs or a child is born with damage to the nervous system, bones, mouth, eyes. nine0003
HIV infection (AIDS)
The human immunodeficiency virus causes damage to cells of the immune system. HIV is transmitted sexually, through blood when using medical instruments, from mother to child during pregnancy, childbirth or breastfeeding.
Symptoms and manifestations of it may be different, since immunodeficiency may first manifest itself as a lesion of any organs and systems. Usually, a few weeks after infection, a sharp increase in body temperature, a rash on the body, pain in the throat, and in the eyes can occur. Over the next few years, there is a gradual weakening of immunity, against which various infections develop. In the absence of therapy, AIDS develops after about 10 years, which is characterized by the development of serious infections that threaten human life or the appearance of malignant neoplasms. Without preventive measures, infection of the fetus during pregnancy occurs in 25-40% of cases.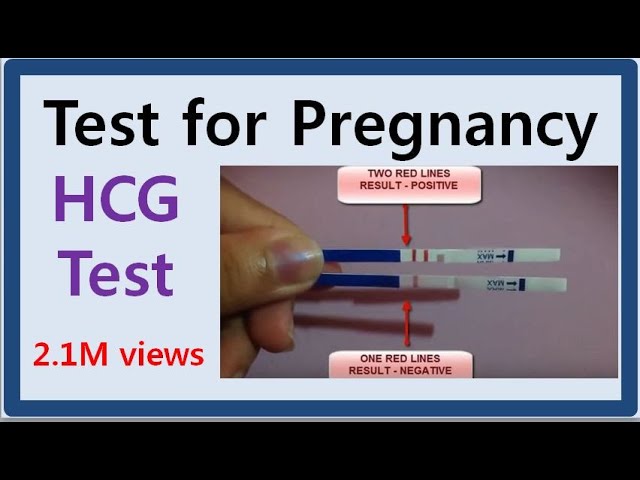 Most infections occur during the passage of the fetus through the natural birth canal. In addition, the risk of infection during breastfeeding is high. With HIV infection, to reduce the risk of transmission to the fetus, treatment with an antiviral drug is carried out in the second half of pregnancy. nine0003
Most infections occur during the passage of the fetus through the natural birth canal. In addition, the risk of infection during breastfeeding is high. With HIV infection, to reduce the risk of transmission to the fetus, treatment with an antiviral drug is carried out in the second half of pregnancy. nine0003
Hepatitis B
Viral hepatitis B is a serious infectious disease that can eventually lead to severe liver disease, cirrhosis of the liver. It is transmitted sexually, through blood, instruments, and also during pregnancy from mother to fetus. Most often, infection with the hepatitis B virus is asymptomatic, and only a fifth of the cases show jaundice. Hepatitis B is treated with antiviral drugs by a hepatologist.
Learn more about the services:
- Pregnancy tests
Hepatitis C
This is the most severe form of viral hepatitis, the chronic form of which often progresses to cirrhosis and liver cancer. Acute hepatitis C is also often asymptomatic.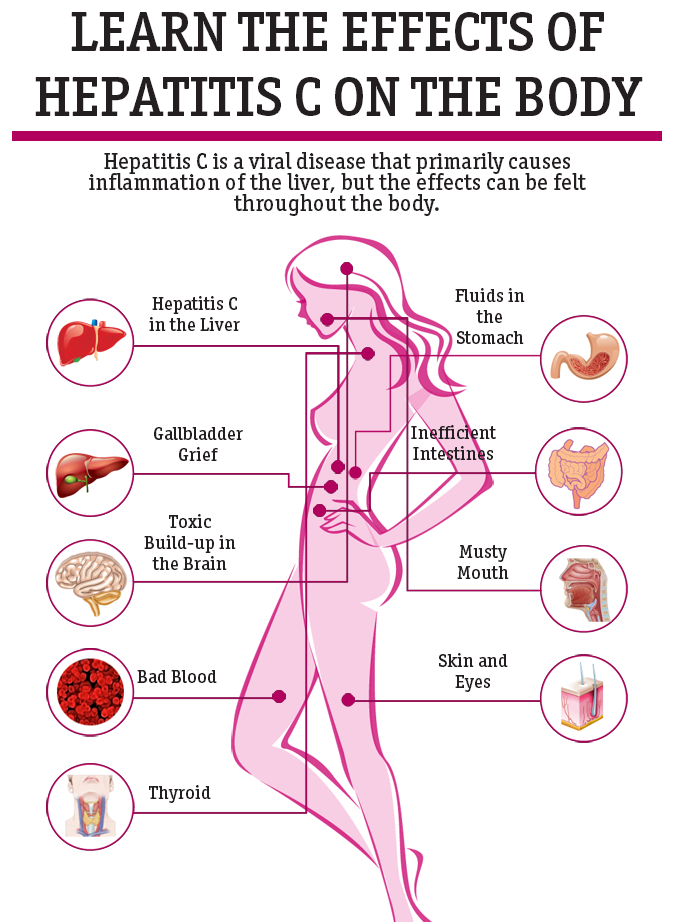 The hepatitis C virus is most often transmitted through the blood, the risk of sexual transmission is extremely small. It is also very rare for the virus to be transmitted from mother to fetus, although the risk of transmission increases if there is concomitant HIV infection. The risk of infection also increases in the presence of an acute process and active reproduction of the virus. In this case, premature termination of pregnancy and intrauterine growth retardation are possible. nine0003
The hepatitis C virus is most often transmitted through the blood, the risk of sexual transmission is extremely small. It is also very rare for the virus to be transmitted from mother to fetus, although the risk of transmission increases if there is concomitant HIV infection. The risk of infection also increases in the presence of an acute process and active reproduction of the virus. In this case, premature termination of pregnancy and intrauterine growth retardation are possible. nine0003
Testing for HIV, hepatitis and syphilis is carried out several times during pregnancy. Blood for syphilis must be given at registration, then at 30 weeks and 2-3 weeks before delivery, that is, at about 37 weeks. Blood for HIV and hepatitis B and C is examined twice - when registering at the antenatal clinic and at 30 weeks. This frequency of testing allows you to fully identify cases of infection in pregnant women. After infection with these infections, the detection of specific proteins in the blood that indicate the disease does not occur immediately. Within a few weeks or months, a blood test of a sick person may be negative. This is the so-called seronegative period of the disease. For different infections, this period varies in duration, from 21 days with syphilis to six months with HIV infection. nine0003
Within a few weeks or months, a blood test of a sick person may be negative. This is the so-called seronegative period of the disease. For different infections, this period varies in duration, from 21 days with syphilis to six months with HIV infection. nine0003
Diagnosis of infections during pregnancy
Testing for HIV, hepatitis B and C, syphilis is subject to absolutely all pregnant women who are registered for pregnancy at the antenatal clinic. For general screening, that is, an examination that all women undergo, I use the simplest, cheapest and fastest tests.
Diagnosis of syphilis
Detection of syphilis is carried out using so-called non-treponemal tests. They are based on the detection in the blood of patients of protein antibodies that the body has developed not against the pathogens themselves, but against tissues destroyed under the influence of syphilis, and fats that make up the wall of the causative agent of syphilis - pale treponema. These tests are always positive in the presence of syphilis. However, non-treponemal tests can also be positive in some non-communicable diseases, which are characterized by the production of antibodies to the body's own cells - these are the so-called autoimmune diseases, such as systemic lupus erythematosus, other connective tissue diseases, antiphospholipid syndrome (a disease in which the body produces antibodies against the membranes body cells). nine0003
However, non-treponemal tests can also be positive in some non-communicable diseases, which are characterized by the production of antibodies to the body's own cells - these are the so-called autoimmune diseases, such as systemic lupus erythematosus, other connective tissue diseases, antiphospholipid syndrome (a disease in which the body produces antibodies against the membranes body cells). nine0003
Non-treponemal tests for the diagnosis of syphilis include the previously widely used Wassermann test, as well as more modern methods - the Rapid Plasma Reagins (RPR) test and the VDRL (Venereal Disease Research laboratory) microscopic test. Cure of syphilis is also usually diagnosed using quantitative non-treponemal tests.
Disadvantages of non-treponemal tests
- false-negative results with high levels of antibodies in the blood. This phenomenon can be observed in the early stages of syphilis and in patients co-infected with HIV,
- insufficient sensitivity for diagnosing advanced syphilis,
- false-positive results in the presence of other acute or chronic diseases.
If a patient has a positive result of a non-treponemal test, the doctor will definitely refer her to a venereologist to clarify the diagnosis, who will prescribe additional tests, namely treponemal tests for syphilis. Treponemal tests are performed to detect antibodies to the causative agent of syphilis - Treponema pallidum, so they are highly sensitive and specific, that is, they can only be positive for syphilis. These tests are used only to diagnose syphilis, they are not suitable for monitoring cure, as they can remain positive throughout life. nine0003
The following treponemal tests are most commonly used:
- Immunofluorescence test (RIF-FTA) in various modifications,
- Passive agglutination test (TPHA),
- Enzyme immunoassay (ELISA -EIA) including recombinant ELISA,
- Treponema pallidum immobilization test (RIBT),
- Immunoblotting
Diagnosis of syphilis requires positive results from one non-treponemal and two treponemal blood tests. nine0054 In the maternity hospital, all patients upon admission undergo a blood test for syphilis by two methods - one non-treponemal and necessarily RPHA. Therefore, in the case of previously transferred and cured syphilis, it is imperative to inform the doctor about this so that the treatment tactics are chosen correctly.
nine0054 In the maternity hospital, all patients upon admission undergo a blood test for syphilis by two methods - one non-treponemal and necessarily RPHA. Therefore, in the case of previously transferred and cured syphilis, it is imperative to inform the doctor about this so that the treatment tactics are chosen correctly.
Diagnosis of HIV infection
For screening of all pregnant women to detect HIV infection, a method is used to determine specific proteins produced in the body for the HIV virus using enzyme immunoassay (ELISA). nine0003
Disadvantages of ELISA
- serological diagnosis is ineffective during the so-called “serological window”, when in the first weeks after infection, antibodies to HIV cannot be detected by ELISA due to their absence or low concentration,
- the possibility of false positive results in pregnancy, oncological diseases.
Two methods are used to confirm the presence of HIV infection - the immunoblotting method and the polymerase chain reaction (PCR) method. The PCR method is used more often because it allows it to be less expensive. The same method is used for questionable ELISA results, since it is more sensitive, PCR detects the virus in the blood about 11 days earlier than the ELISA becomes positive. nine0003
The PCR method is used more often because it allows it to be less expensive. The same method is used for questionable ELISA results, since it is more sensitive, PCR detects the virus in the blood about 11 days earlier than the ELISA becomes positive. nine0003
Diagnosis of hepatitis B and C
Screening for hepatitis B is the determination of the HBsAg surface antigen by enzyme immunoassay (ELISA). When infected with the hepatitis B virus, HBsAg appears in the blood first, a few weeks before the onset of symptoms and increased activity of liver enzymes, antibodies to the hepatitis B virus (anti-HBs) appear in the blood approximately 6 weeks after the onset of the disease and usually persist until the end of life. A blood test for HBsAg is a fairly sensitive method of research, false positive results are rare. Patients whose blood test for HBsAg turned out to be positive are subjected to a more detailed examination, in particular, qualitative and quantitative determination of hepatitis B virus DNA by PCR is carried out. nine0003
nine0003
Screening test for hepatitis C is the detection of antibodies to the hepatitis C virus - anti-HCV and the use of enzyme-linked immunosorbent assay (ELISA). These antibodies are detected approximately 50-140 days after infection. To confirm the standard test, an auxiliary test of recombinant immunoblotting (RIBA) or detection of virus RNA using polymerase chain reaction, PCR is used. If both tests are positive, this confirms the diagnosis of hepatitis C, in this case, infectious disease doctors prescribe an additional quantitative PCR to determine the viral load, that is, the number of viruses in the blood, which makes it possible to judge the activity or rate of reproduction of viruses. The higher the viral load, the more active the reproduction of viruses. In the case of active hepatitis C, an analysis of the HCV genotype may also be required, which is required to select an effective hepatitis treatment regimen. nine0003
Management of pregnancy and childbirth with positive tests
Syphilis
Upon receipt of positive test results for syphilis, the issue of the past syphilis, or its presence at the moment, must be resolved. If syphilis has been treated for a long time, but the tests are still positive, prophylactic antibiotic treatment is carried out at 20-24 weeks of gestation, and the child after birth is necessarily checked for congenital syphilis. In such situations, with the permission of a venereologist, childbirth can be carried out in ordinary maternity hospitals. nine0003
If syphilis has been treated for a long time, but the tests are still positive, prophylactic antibiotic treatment is carried out at 20-24 weeks of gestation, and the child after birth is necessarily checked for congenital syphilis. In such situations, with the permission of a venereologist, childbirth can be carried out in ordinary maternity hospitals. nine0003
In case of confirmed syphilis during pregnancy, a woman must be hospitalized in a specialized dermatovenerological hospital for antibacterial treatment. For treatment, antibiotics of the penicillin group are more often used - Penicillin, bicillin, extencillin or erythromycin and ceftriaxone (with intolerance to penicillin). The duration of treatment depends on the stage of the disease - with primary syphilis, treatment lasts several weeks, with tertiary - several years. All pregnant women who underwent treatment during pregnancy are additionally given a prophylactic course of antibiotics as early as 20-24 weeks. After birth, all children born to sick mothers who have not completed full courses of treatment and prevention are also given a preventive course of antibiotic treatment. nine0003
After birth, all children born to sick mothers who have not completed full courses of treatment and prevention are also given a preventive course of antibiotic treatment. nine0003
Currently, there are no clear recommendations on when to terminate a pregnancy due to syphilis. Modern methods of treatment of syphilis can prevent congenital syphilis when the disease is detected in the mother in the first half of pregnancy. If syphilis is detected after 12 weeks of pregnancy, then the treatment of the pregnant woman is already the treatment of the fetus. Childbirth of patients with syphilis is carried out necessarily in specialized maternity hospitals.
HIV infection
If HIV infection is detected during pregnancy, a woman must be referred to an infectious disease virologist to decide whether the pregnancy can be prolonged, since pregnancy, due to a natural decrease in immunity, can accelerate and worsen the course of HIV infection. Pregnancy management is carried out jointly by an obstetrician-gynecologist and an infectious disease virologist. During pregnancy, HIV infection is treated with Zidovudine under the control of the immunological status of the pregnant woman. This drug crosses the placenta and reduces the likelihood of infection of the fetus by 3 times. Childbirth of HIV-infected women is carried out in specialized maternity hospitals. If antiviral therapy was carried out during pregnancy, childbirth is carried out through the natural birth canal, in the absence of therapy during pregnancy, a caesarean section is indicated to reduce the risk of infection of the baby. Breastfeeding of HIV-infected women is contraindicated, since very often the infection of a child with HIV occurs precisely through breast milk. nine0003
During pregnancy, HIV infection is treated with Zidovudine under the control of the immunological status of the pregnant woman. This drug crosses the placenta and reduces the likelihood of infection of the fetus by 3 times. Childbirth of HIV-infected women is carried out in specialized maternity hospitals. If antiviral therapy was carried out during pregnancy, childbirth is carried out through the natural birth canal, in the absence of therapy during pregnancy, a caesarean section is indicated to reduce the risk of infection of the baby. Breastfeeding of HIV-infected women is contraindicated, since very often the infection of a child with HIV occurs precisely through breast milk. nine0003
Hepatitis B and C
All patients who have positive tests for hepatitis B or C must be observed during pregnancy by an infectious disease specialist. In acute hepatitis, pregnancy can significantly worsen the course of the disease, and the virus often crosses the placenta to the fetus, causing birth defects.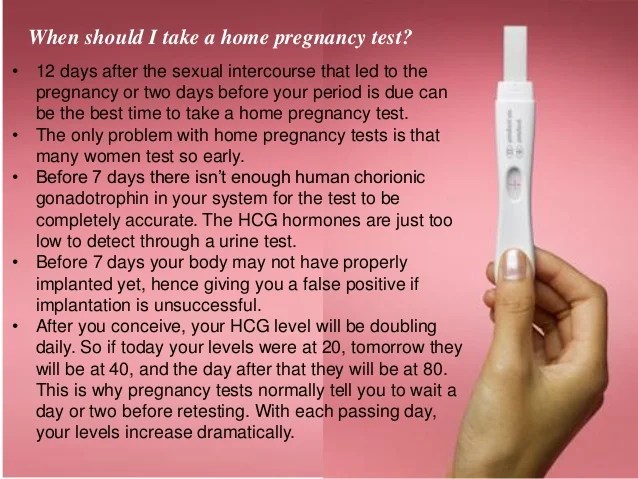 Therefore, when a woman becomes ill with hepatitis in the first trimester of pregnancy, the issue of abortion is decided. In chronic forms of hepatitis B and C, specific treatment is usually not carried out; liver tests are monitored in each trimester of pregnancy. With the development of clinical symptoms, they should be hospitalized in special departments of infectious diseases hospitals for inpatient observation. In particularly severe cases, medical termination of pregnancy may be required. Childbirth of patients with hepatitis can be carried out in a specialized maternity hospital or in the observational department of a conventional maternity hospital, and are carried out in the absence of other indications, through the natural birth canal. Breastfeeding in hepatitis B is contraindicated; patients with inactive hepatitis C are allowed to breastfeed. A child whose mother is ill with hepatitis B immediately after childbirth is prevented from hepatitis - a specific immunoglobulin is administered and vaccination against hepatitis B is carried out.
Therefore, when a woman becomes ill with hepatitis in the first trimester of pregnancy, the issue of abortion is decided. In chronic forms of hepatitis B and C, specific treatment is usually not carried out; liver tests are monitored in each trimester of pregnancy. With the development of clinical symptoms, they should be hospitalized in special departments of infectious diseases hospitals for inpatient observation. In particularly severe cases, medical termination of pregnancy may be required. Childbirth of patients with hepatitis can be carried out in a specialized maternity hospital or in the observational department of a conventional maternity hospital, and are carried out in the absence of other indications, through the natural birth canal. Breastfeeding in hepatitis B is contraindicated; patients with inactive hepatitis C are allowed to breastfeed. A child whose mother is ill with hepatitis B immediately after childbirth is prevented from hepatitis - a specific immunoglobulin is administered and vaccination against hepatitis B is carried out.