Cotton cheese discharge
Vaginal discharge | nidirect
It's normal and healthy to produce a clear or white discharge from your vagina. This mucus is produced naturally from the neck of the womb, known as the cervix.
How to tell if your discharge is unhealthy
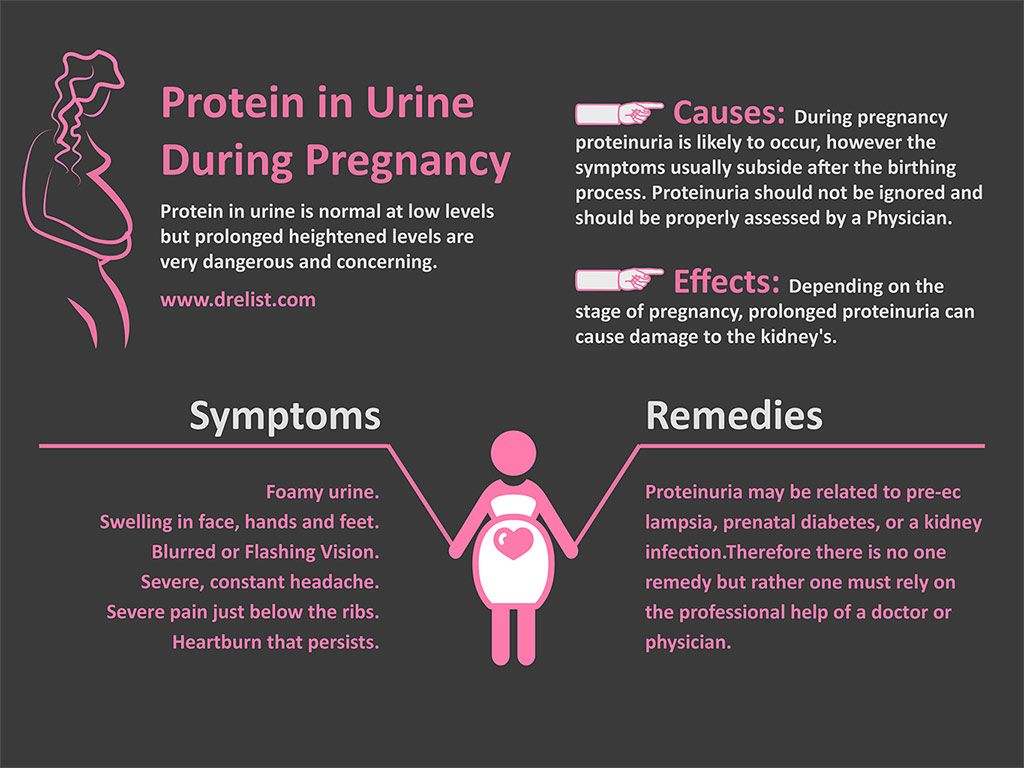
The amount of vaginal discharge varies throughout your menstrual cycle (brown discharge is usually the end of your period). Most pregnant women will get a ’pregnancy discharge’.
Healthy discharge doesn't have a strong smell or colour. You may feel an uncomfortable wetness, but you shouldn't have any itching or soreness around your vagina.
Any sudden change to your discharge may suggest a vaginal infection. You should be aware of how your discharge naturally varies throughout your cycle and what isn't normal. However, obvious warning signs of infection are:
- a change in colour or consistency
- a sudden bad smell
- an unusually large amount of discharge
- another symptom alongside the discharge, such as itching outside your vagina or pain in your pelvis or tummy
- unexpected bleeding from the vagina
If you're not sure whether your discharge is normal and are worried about it, see your GP or practice nurse at your GP surgery.
- Read about sexual health for information and advice
Common causes of abnormal discharge
There are many possible causes of abnormal vaginal discharge. However, it’s usually a sign of infection. The infection is often caused by something that upsets the natural balance of bacteria or yeast in your vagina, such as washing inside the vagina, or it may be sexually transmitted.
The most common causes are:
- thrush – a fungal infection that commonly affects the vagina
- bacterial vaginosis – a bacterial infection of the vagina
- trichomoniasis – a sexually transmitted infection (STI) caused by a tiny parasite
- gonorrhoea or chlamydia – STIs caused by bacteria
- genital herpes – an STI caused by the herpes simplex virus
The guide below may help you identify the cause of your discharge. However, it's important to see your GP for a proper diagnosis and advice on how to treat the infection.
Watery or white vaginal discharge with intense itchiness
If your discharge is thin and watery, or thick and white (like cottage cheese), you may have thrush.
This common fungal infection causes intense itchiness and soreness around your vagina. The discharge may smell slightly yeasty, but doesn't have a strong smell.
Almost all women get thrush from time to time and it's not sexually transmitted. It's easily treated with antifungal medicine, which can be bought over the counter from your pharmacist.
- Find out more about thrush
White or grey fishy-smelling discharge
If your vaginal discharge is grey or develops a strong fishy smell, particularly after sexual intercourse, you could have bacterial vaginosis (BV). BV is an imbalance in the normal bacteria found in your vagina. It doesn't usually cause itching or irritation.
Like thrush, BV is very common and isn't sexually transmitted. It's easily treated with antibiotics. See your GP if you think you might have it.
Green, yellow or frothy discharge
Trichomoniasis is a common STI caused by a tiny parasite. It can make your vaginal discharge frothy, yellow or green. You may have a lot of discharge, which may also have an unpleasant fishy smell.
You may have a lot of discharge, which may also have an unpleasant fishy smell.
Other possible symptoms are soreness, swelling and itching around the vagina, and pain when passing urine.
Trichomoniasis is treated with an antibiotic that your GP can prescribe.
If you are sexually active and if you are unsure about your partner’s sexual history, you risk getting STIs.
If you have trichomoniasis, you should visit a local GUM or sexual health clinic as it can exist alongside other STIs.
Abnormal discharge with pain or bleeding
See your GP or go to a genitourinary medicine (GUM) clinic as soon as possible if your vaginal discharge is abnormal and you have:
- pain in your pelvis
- pain when you urinate
- bleeding between periods or after sex
You may have chlamydia or gonorrhoea (both STIs). Gonorrhoea can make your discharge turn green, although often the pain or bleeding are more noticeable.
Both conditions are treated with antibiotics. You will need to visit a local GUM or sexual health clinic or see your GP.
You will need to visit a local GUM or sexual health clinic or see your GP.
Untreated gonorrhoea or chlamydia may spread upwards and lead to pelvic inflammatory disease, a serious infection of the womb, fallopian tubes or ovaries.
If you ignore your symptoms you may have problems with fertility and pregnancy as a result of not being treated in time.
Abnormal discharge with blisters around the genitals
Genital herpes can cause painful, red blisters or sores to appear around your genitals, as well as an abnormal vaginal discharge. See your GP or go to a genitourinary medicine (GUM) clinic as soon as possible.
You may be offered a course of antiviral tablets, which stop the herpes virus multiplying, but the symptoms may have a tendency to return.
Young girls and post-menopausal women
It's unusual for young girls to have abnormal vaginal discharge before they've gone through puberty. If this happens, they should see a GP. A common cause is a type of vulvitis (inflammation of the vulval area), caused by a streptococcal infection.
Abnormal discharge is also unusual in older women. If you've gone through the menopause and suddenly notice an abnormal vaginal discharge, see your doctor as soon as possible. Possible causes include:
- a sexually transmitted infection (STI)
- cervical polyps – non-cancerous growths in the womb or lining of the cervix (neck of the womb)
- an intrauterine device (IUD)
It's also important to rule out cervical cancer or endometrial cancer.
Cleaning your vagina
The vagina is self-cleansing, so there is no need to wash inside it (called douching). Douching can upset the natural balance of bacteria and fungi in your vagina and lead to thrush or bacterial vaginosis.
Vaginal soreness and abnormal vaginal discharge can also be caused by overusing perfumed soaps, bubble baths and shower gels. Never clean your vagina with anything strongly perfumed. Use a mild soap and warm water to gently wash around your genitals.
More useful links
- How to use your health services
Help improve this page - send your feedback
You must have JavaScript enabled to use this form.
report a problem
leave feedback
ask a question
Report a problemWhich problem did you find on this page? (Tick all that apply)
A link, button or video is not working
There is a spelling mistake
Information is missing, outdated or wrong
I can't find what I'm looking for
Another issue
Messages
Tell us more about the problem you're having with the nidirect website.
Enter your feedback
What is your question about?Choose a topic for your question: - Select -AnglingBenefitsBirth certificatesBlue BadgeCareersCompensation due to a road problemChild MaintenanceCivil partnership certificatesCoronavirus (COVID-19)COVID vaccination certificateCriminal record checks (AccessNI)Death certificatesEducational Maintenance AllowanceEmployment rightsHigh Street Spend Local SchemeMarriage certificatesMotoringnidirect accountPassportsPenalty Charge NoticesPensionsPRONI - historical recordsRates or property valuationProblems with roads and streetsSmartpassMy question is about something else
What to do next
Vaginitis | Vulvovaginitis | MedlinePlus
On this page
Basics
- Summary
- Start Here
- Symptoms
- Diagnosis and Tests
- Prevention and Risk Factors
- Treatments and Therapies
Learn More
- Specifics
See, Play and Learn
- No links available
Research
- Clinical Trials
- Journal Articles
Resources
- No links available
For You
- Teenagers
- Patient Handouts
What is vaginitis?
Vaginitis, also called vulvovaginitis, is an inflammation or infection of the vagina. It can also affect the vulva, which is the external part of a woman's genitals. Vaginitis can cause itching, pain, discharge, and odor.
It can also affect the vulva, which is the external part of a woman's genitals. Vaginitis can cause itching, pain, discharge, and odor.
Vaginitis is common, especially in women in their reproductive years. It usually happens when there is a change in the balance of bacteria or yeast that are normally found in your vagina. There are different types of vaginitis, and they have different causes, symptoms, and treatments.
What causes vaginitis?
Bacterial vaginosis (BV) is the most common vaginal infection in women ages 15-44. It happens when there is an imbalance between the "good" and "harmful" bacteria that are normally found in a woman's vagina. Many things can change the balance of bacteria, including:
- Taking antibiotics
- Douching
- Using an intrauterine device (IUD)
- Having unprotected sex with a new partner
- Having many sexual partners
Yeast infections (candidiasis) happen when too much candida grows in the vagina. Candida is the scientific name for yeast. It is a fungus that lives almost everywhere, including in your body. You may have too much growing in the vagina because of:
Candida is the scientific name for yeast. It is a fungus that lives almost everywhere, including in your body. You may have too much growing in the vagina because of:
- Antibiotics
- Pregnancy
- Diabetes, especially if it is not well-controlled
- Corticosteroid medicines
Trichomoniasis can also cause vaginitis. Trichomoniasis is a common sexually transmitted disease. It is caused by a parasite.
You can also have vaginitis if you are allergic or sensitive to certain products that you use. Examples include vaginal sprays, douches, spermicides, soaps, detergents, or fabric softeners. They can cause burning, itching, and discharge.
Hormonal changes can also cause vaginal irritation. Examples are when you are pregnant or breastfeeding, or when you have gone through menopause.
Sometimes you can have more than one cause of vaginitis at the same time.
What are the symptoms of vaginitis?
The symptoms of vaginitis depend on which type you have.
With BV, you may not have symptoms. You could have a thin white or gray vaginal discharge. There may be an odor, such as a strong fish-like odor, especially after sex.
Yeast infections produce a thick, white discharge from the vagina that can look like cottage cheese. The discharge can be watery and often has no smell. Yeast infections usually cause the vagina and vulva to become itchy and red.
You may not have symptoms when you have trichomoniasis. If you do have them, they include itching, burning, and soreness of the vagina and vulva. You may have burning during urination. You could also have gray-green discharge, which may smell bad.
How is the cause of vaginitis diagnosed?
To find out the cause of your symptoms, your health care provider may:
- Ask you about your medical history
- Do a pelvic exam
- Look for vaginal discharge, noting its color, qualities, and any odor
- Study a sample of your vaginal fluid under a microscope
In some cases, you may need more tests.
What are the treatments for vaginitis?
The treatment depends on which type of vaginitis you have.
BV is treatable with antibiotics. You may get pills to swallow, or cream or gel that you put in your vagina. During treatment, you should use a condom during sex or not have sex at all.
Yeast infections are usually treated with a cream or with medicine that you put inside your vagina. You can buy over-the-counter treatments for yeast infections, but you need to be sure that you do have a yeast infection and not another type of vaginitis. See your health care provider if this is the first time you have had symptoms. Even if you have had yeast infections before, it is a good idea to call your health care provider before using an over-the-counter treatment.
The treatment for trichomoniasis is usually a single-dose antibiotic. Both you and your partner(s) should be treated, to prevent spreading the infection to others and to keep from getting it again.
If your vaginitis is due to an allergy or sensitivity to a product, you need to figure out which product is causing the problem. It could be a product that you started using recently. Once you figure it out, you should stop using the product.
If the cause of your vaginitis is a hormonal change, your health care provider may give you estrogen cream to help with your symptoms.
Can vaginitis cause other health problems?
It is important to treat BV and trichomoniasis, because having either of them can increase your risk for getting HIV or another sexually transmitted disease. If you are pregnant, BV or trichomoniasis can increase your risk for preterm labor and preterm birth.
Can vaginitis be prevented?
To help prevent vaginitis:
- Do not douche or use vaginal sprays
- Use a latex condom when having sex. If your or your partner is allergic to latex, you can use polyurethane condoms.
- Avoid clothes that hold in heat and moisture
- Wear cotton underwear
- Vaginitis (American College of Obstetricians and Gynecologists)
- What Are the Symptoms of Bacterial Vaginosis? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Symptoms of Vaginitis? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Bacterial Vaginosis Test (National Library of Medicine) Also in Spanish
- How Do Health Care Providers Diagnose Bacterial Vaginosis (BV)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- How Do Health Care Providers Diagnose Vaginitis? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Can Vaginitis Be Prevented? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- How Is Vaginitis Treated? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Treatments for Bacterial Vaginosis (BV)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Bacterial Vaginosis (Centers for Disease Control and Prevention) Also in Spanish
- Bacterial Vaginosis (Department of Health and Human Services, Office on Women's Health)
- Trichomoniasis: MedlinePlus Health Topic (National Library of Medicine) Also in Spanish
- Vaginal Yeast Infections (Department of Health and Human Services, Office on Women's Health) Also in Spanish
- Yeast Infection (Vaginal) (Mayo Foundation for Medical Education and Research) Also in Spanish
- Yeast Infections: MedlinePlus Health Topic (National Library of Medicine) Also in Spanish
- ClinicalTrials.
gov: Candidiasis, Vulvovaginal (National Institutes of Health)
- ClinicalTrials.gov: Vaginitis (National Institutes of Health)
- ClinicalTrials.
gov: Vaginosis, Bacterial (National Institutes of Health)
- Article: A study on the accuracy of a new fluorescent detection method.
..
- Article: Cytological diagnosis of genital ureaplasma urealyticum and its importance in cervical...
- Article: Qualitative and Quantitative Detection of Multiple Sexually Transmitted Infection Pathogens Reveals.
..
- Vaginitis -- see more articles
- Bacterial Vaginosis (American Academy of Pediatrics) Also in Spanish
- Vaginal Yeast Infections (Nemours Foundation) Also in Spanish
Curdled discharge in women: causes, treatment, preparations
Where can I buy?
Encyclopedia
Diseases of the intimate area
Vaginal discharge is the most common gynecological complaint with which millions of women around the world seek medical attention 1 .
The author of the article
Molchanov Oleg Leonidovich
Gynecologist, reproductive specialist, doctor of medical sciences.
Audio version of the page:
Types of discharge in women
Vaginal discharge in women is a normal, physiological phenomenon. However, sometimes they indicate various diseases and pathological conditions of the pelvic organs. It is important for women to know what is the norm in this case, and what is a pathology in order to consult a doctor in time in case of symptoms of the disease 1.2 .
Normal vaginal discharge has the following features
- Clear or translucent with a whitish (sometimes yellowish) tint
- Small
- Odorless or slightly acidic odor
- Not accompanied by itching, pain or other discomfort
The nature of discharge in women may vary depending on the phase of the menstrual cycle, which is associated with fluctuations in the levels of sex hormones in the blood. As a rule, in the middle of the cycle, the discharge becomes transparent, mucous in nature, becomes "viscous" and more abundant. In the second half of the cycle, vaginal discharge becomes thicker, creamy, and their number decreases.
Changes in the hormonal background during pregnancy, breastfeeding or the use of hormonal drugs also affect the nature of vaginal discharge 1.3 .
Pathological discharge, which may indicate the presence of a disease of the genital organs
- Have a color different from normal vaginal discharge (more saturated, yellow, gray or even green).
- Become more abundant.
- Acquire an unpleasant odour.
- May be accompanied by itching, soreness in the vagina, pain during intercourse or urination.
- Sometimes have bloody patches that do not coincide with the days of menstrual bleeding (for example, after intercourse).
Causes of white curdled discharge in women
Curdled vaginal discharge is an abnormal discharge. According to statistics, up to 2/3 of women of reproductive age face them 4 .
Curdled discharge can be a sign of various vaginal diseases. However, the most common cause of cheesy discharge is vulvovaginal candidiasis or, as it is often called, "thrush".
Thrush is a common cause of white cheesy discharge
What is thrush
Vaginal candidiasis, or "thrush", is a common infectious disease of the vulva and vaginal mucosa. Its causative agent is various fungi of the genus Candida, which are normally present in the vagina in small amounts 4.5 . The most common species is Candida albicans. In more rare cases, other fungi of the same genus, which are classified as Candida non-albicans.
Causes of thrush
A feature of yeast-like fungi of the genus Candida is their ability under certain conditions (unfavorable for humans: illness, reduced immunity, antibiotics, etc.) to actively multiply, which leads to the development of vaginal candidiasis, or "thrush". Fungi of the genus Candida penetrate the epithelium of the mucous membrane of the vagina and external genital organs, causing the development of inflammation and swelling in the intimate area.
Symptoms of thrush
In addition to cheesy vaginal discharge, symptoms of thrush are:
Redness of the skin and mucous membranes in places affected by fungi
Pain during sexual intercourse
Pain during sexual intercourse
Treatment of curdled discharge in women
General characteristics of preparations
The main goal in the treatment of diseases accompanied by pathological secretions is the destruction (elimination) of the pathogen and the reduction of symptoms, such as itching, burning.
Antifungal drugs of various groups are used to treat candidiasis, which causes the appearance of a curdled discharge from the vagina.
In medicine, all antifungal drugs have certain requirements. The drug must be:
- effective against various types of fungi that cause thrush
- have a high security profile
The mechanism of action of all antifungal drugs is associated with the destruction of the cell wall of fungi and, as a result, a violation of their vital activity. Thus, there is a "double effect" on the mushrooms. On the one hand, the drug stops the growth and reproduction of fungi, reducing their number (fungistatic action), and on the other hand, it destroys active cells (fungicidal action) 6 .
Types of antifungals
All antifungal agents can be divided into 2 broad categories:
Topical preparations
used on the mucous membrane in the vagina
Systemic preparations
taken orally (by mouth), have a general effect on the whole body
Antifungals are also divided for different types depending on the main active ingredient in their composition 6. 7 .
Efficacy of sertaconazole for the treatment of cheesy discharge
As a representative of the azole group of drugs, sertaconazole demonstrates a triple action against fungi 13 (both fungistatic - inhibits the growth and reproduction of fungi, and fungicidal - destroys active fungi), and also prevents the transition of fungi of the genus Candida from an inert form to a pathogenic one. This is possible due to the special chemical structure of sertaconazole 13 .
Antimicrobial effect on fungi with sertaconazole begins within minutes 7 . Studies show that already 90% of fungal cells die within one hour when using the recommended dose of sertaconazole 8 .
Some studies have shown that the antimicrobial activity of sertaconazole may be higher than, for example, similar drugs based on fluconazole, itraconazole and a number of other azole compounds 9 .
The high efficiency of sertaconazole against fungi of the genus Candida may also be due to the fact that other "azoles" appeared earlier, which means that a larger number of representatives of fungi developed an "addiction" to them, which in medicine has a term - resistance (insensitivity) 10 .
Thus, sertaconazole demonstrates its activity against a wide range of microorganisms: both yeast-like fungi and various types of bacteria, which is especially important in diseases of the vulva and vagina caused by several types of microorganisms at once, as well as if it is necessary to prevent relapses (frequent disease recurrence).
The use of 1 vaginal suppository for the course of treatment of "thrush" is explained by the fact that Zalain ® has a high lipophilicity (it dissolves well in lipid (fatty) cell structures), which allows it to remain in the vaginal mucosa for a long time (7 days) at a therapeutic concentration.
Why does one Zalain candle last 7 days?
Contents
Types of secretions
Causes
Treatment
Preparations
0% read
Zalain ® Suppositories for the treatment of vaginal candidiasis causing white cheesy discharge
Sertaconazole preparations are available in various forms: Zalain ® cream for external use, Zalain ® 9 vaginal suppositories0010 .
1 suppository once (effective for 7 days in the treatment of vulovovaginal candidiasis - thrush)
Local action of the drug
Absorption of sertaconazole into the bloodstream does not occur 13
Can be used during pregnancy and lactation, if the benefit exceeds the risks
Zalain ® Suppositories for the treatment of vaginal candidiasis causing white cheesy discharge
InstructionPrevention of fungal infections of the vagina
Prevention of fungal infections of the vagina is important due to the frequent cases of fungal resistance to standard treatment, the formation of chronic forms of thrush with frequent episodes of exacerbations (relapses), as well as the high proportion of women who stop treatment earlier than it is required.
How to prevent candidiasis?
boost immunity
avoid synthetic and tight underwear
do not use scented sanitary pads
follow the rules of intimate hygiene
lead a healthy lifestyle
use barrier methods of contraception
Specially developed cosmetic product for intimate hygiene of delicate areas — Zalagel ® Intim.
Zalagel ® Intim
Cosmetic product Zalagel ® Intim has a cleansing, moisturizing and protective action for the intimate area. It contains substances that have antimicrobial properties that prevent the growth of fungi and bacteria. In addition, this remedy has a calming effect on discomfort and irritation.
It is recommended to use Zalagel Intim ® once a day as a hygiene product or twice a day when there is a feeling of discomfort in the genital area, as well as during menstruation. 11
Delicately cleanses the intimate area
Creates a destructive environment for fungi of the Candida genus
Protects the female genital organs from infections
Tea tree oil in the composition of the product has antibacterial and antiviral effects
Reduces itching and irritation
Where to buy Zalagel ® Intim
or
Find the nearest pharmacy
InstructionAnswers to frequently asked questions
What other diseases can cause curdled vaginal discharge?
Answer: Sometimes there is a combination of fungal and bacterial infection. Therefore, the amount, color and smell of vaginal discharge can be different. In any case, you need to contact a specialist.
Is the appearance of curdled discharge always a reason to see a doctor? Is self-healing possible?
Answer: , taking into account the possible combinations of various diseases, as well as the development of complications and the chronic course of candidiasis in the absence of treatment, doctors strongly recommend that you contact a specialist at the first symptoms.
Can I continue to be sexually active while treating candidiasis?
Answer: there are forms of antifungal drugs, for the duration of which you should stop having sexual intercourse. However, specific recommendations are given by the attending physician, based on the specific treatment chosen.
Popular articles
More articles
Thrush
Causes of a fungal disease - thrush. Symptoms, types of diagnosis, methods of treatment and prevention.
White, creamy vaginal discharge
Types of discharge in women. Why do white, creamy discharge appear and how to treat it?
Candles for thrush
What are the candles for thrush, how do they differ, and how to choose the most effective.
Sources
- Sim M, Logan S, Goh LH. Vaginal discharge: evaluation and management in primary care. Singapore Med J. 2020;61(6):297-301. doi:10.11622/smedj.2020088
- Singh K, editor. Integrated Approach to Obstetrics and Gynaecology. New Jersey: World Scientific 2016
- Sherrard J, Wilson J, Donders G, Mendling W, Jensen JS.
2018 European (IUSTI/WHO) International Union against sexually transmitted infections (IUSTI) World Health Organization (WHO) guideline on the management of vaginal discharge. Int J STD AIDS. 2018 Nov;29(13):1258-1272. doi: 10.1177/0956462418785451. Epub 2018 Jul 27. PMID: 30049258.
- Federal clinical guidelines for the management of patients with urogenital candidiasis. / ROAG / Moscow - 2020
- Böcher S, Helmig RB, Arpi M, Bjerrum L. [Diagnosis of vaginal discharge]. Ugeskr Laeger. 2018 Jan 15;180(3):V03170229. Danish. PMID: 29336298.
- Khashukoeva A.Z., Safonina M.S., Andreasyan G.O., Myasoutova A.I., Overko A.V. Therapeutic approaches in the treatment of vulvovaginal candidiasis. Medical advice. 2020;(13):138–146. doi: 10.21518/2079-701X-2020-13-138-146.
- Carrillo-Muñoz AJ, Tur-Tur C, Cárdenes DC, Estivill D, Giusiano G. Sertaconazole nitrate shows fungicidal and fungistatic activities against Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum, causative agents of tinea pedis.
Antimicrob. Agents Chemother. 2011;55(9):4420-4431
- Agut J, Palacin C, Salgado J, Casas E, Sacristan A, Ortiz JA. Direct Membrane-Damaging effect of Sertaconazole on Candida albicans as a Mechanism of its Fungicidal Activity. Arzneim-Forsh Drug Res. 1992;42(5):721-724
- Carrillo-Munoz AJ, Guglietta A, Palacin C, et al. In vitro antifungal activity of sertaconazole compared with nine other drugs against 250 clinical isolates of dermatophytes and Scopulariopsis brevicaulis. Chemotherapy. 2004;50(6):308-313
- Croxtall JD, Plosker GL. Sertaconazole. A Review of Its Use in the Management of Superficial Mycoses in Dermatology and Gynaecology. Drugs.2009;69(3):339-359.
- According to the official instructions for Zalagel Intim®.
- Carrillo-Muñoz AJ, Tur-Tur C, Giusiano G, Marcos-Arias C, Eraso E, Jauregizar N, Quindós G. Sertaconazole: an antifungal agent for the topical treatment of superficial candidiasis. Expert Rev Anti Infect Ther. 2013 Apr;11(4):347-58.
doi: 10.1586/eri.13.17. PMID: 23566144.
- Carrillo-Muñoz AJ, Tur-Tur C, Giusiano G, Marcos-Arias C, Eraso E, Jauregizar N, Quindós G. Sertaconazole: an antifungal agent for the topical treatment of superficial candidiasis. Expert Rev Anti Infect Ther. 2013 Apr;11(4):347-58. doi: 10.1586/eri.13.17. PMID: 23566144.
HAS CONTRAINDICATIONS.
YOU NEED TO CONSULT A PROFESSIONAL
Your browser is outdated, we recommend updating it to the latest version
or using another more modern one.
Vaginal discharge: types, causes, deviations
The article was checked by a doctor: Sokolova Marina Olegovna
Consultation with a specialist:
Vaginal discharge is the result of the work of glands located in the mucous membrane of the vagina. By the nature of the discharge, it is possible to assess the state of the organs of the female genital area.
Normal vaginal discharge is not considered a disease, as it is necessary for the normal functioning of the reproductive system. In the vestibule of the vagina and near the cervix, there are secretory glands that produce mucus, which is necessary to moisturize the mucous membrane and form a healthy microflora. Healthy secretions are formed in a small volume, they are transparent, odorless and are not accompanied by pain and itching. When the type of discharge changes, this indicates the presence of a pathological process in the organs of the female genital area.
Types of vaginal discharge
Depending on the amount of mucus produced, the discharge is divided into scanty, abundant and normal.
Meager is called discharge, which is not enough for the normal functioning of the vagina and external genitalia. The mucous membranes begin to dry out and crack. During sexual intercourse, friction and pain are felt. Scanty discharge is the result of hormonal changes due to age, endocrine disease, or taking hormonal drugs.
Abundant discharge is called, which leads to a constant feeling of moisture in the vagina. They are visible on underwear. Abundant discharge can be diagnosed in young women during ovulation in the middle of the menstrual cycle, they are transparent and do not have an unpleasant odor. During pregnancy, especially before childbirth, the discharge also becomes more abundant. These are healthy secretions, they should not be feared. If the consistency, volume, color or smell of the discharge changes, this indicates the beginning of the pathological process.
Discharge is considered natural if it sufficiently moisturizes the vagina and does not cause anxiety. In the presence of normal discharge, additional moistening of the vagina before intercourse is not required.
According to the consistency, the discharges differ in watery, mucous, cheesy and foamy.
- Liquid discharge - watery and slimy - odorless and color appear normal. Watery discharge is noted in the middle of the cycle during the period of ovulation, mucous membranes appear during intercourse and serve as a lubricant.
- Thick curdled discharge indicates the presence of a fungal infection. Doctors usually diagnose candidiasis. The secretions resemble liquid cottage cheese, they are not uniform in consistency.
- Foamy discharge indicates the presence of a bacterial infection. This is especially dangerous if they have an unpleasant odor or a pronounced color. Foamy discharge is a hallmark of trichomoniasis.
The color of the discharge distinguishes between transparent (normal), white, bloody, yellow, green and brown.
- Clear discharge is normal. Usually they are invisible on underwear and on the body.
- Thick white discharge indicates the presence of candidiasis (thrush). In a healthy state, white discharge may appear before childbirth.
- Bloody and brown discharge is the most dangerous, as it indicates the presence of blood in the vagina. Normally, they occur only during menstruation. When taking hormonal contraception, especially in the first months, the appearance of intermenstrual spotting is acceptable, this is considered normal and reports the adaptation of the body to artificial hormones.
In other cases, bleeding indicates the presence of a serious pathology or the onset of bleeding.
- Yellow and green discharge indicates the presence of an infectious-inflammatory process.
Odorless secretions, with a sweetish odor, with a sour odor, with an unpleasant odor are differentiated by smell.
- The phrase “odorless discharge” is arbitrary, since all human discharge is characterized by some odor. In a healthy state, this smell is pleasant and barely perceptible. It is individual for each person. Since a person constantly feels it, he eventually ceases to feel it. If a woman does not smell the discharge, it can be said that the discharge is odorless.
- Discharge with a sweetish or sour smell most often speaks of thrush. Candida fungi use sugar for food, love it and settle in a sugar-rich environment.
- Foul-smelling discharge is caused by a bacterial infection. They often smell like stale fish. Anaerobic bacteria give the characteristic smell of fish.
The stronger the smell, the stronger the infection.
Call now
+7 (495) 215-56-90
Sign up
Causes of vaginal discharge
Intimate secretions serve as a kind of indicator of the health of the female sphere.
With natural secretions that do not cause discomfort, we can conclude that the organs of the female reproductive system are healthy. However, regular examinations by a gynecologist at the beginning of the cycle are still necessary. Many pathological processes pass without symptoms; only a gynecological examination and laboratory tests can show their presence.
Several factors can affect the type of discharge in a healthy woman. These are stress, climate change, taking hormonal drugs, taking potent drugs, and allergic reactions. Also, the nature of the discharge can be affected by personal hygiene.
A woman should be concerned when the discharge changes in consistency, acquires a strange color or smell, or changes in intensity. Often, such discharge is accompanied by pain in the lower abdomen, itching, pain in the perineum, irritation of the external genital organs, and discomfort during urination.
There are some symptoms by which you can preliminarily determine the disease. Of course, an accurate diagnosis is possible only with a doctor after an examination and laboratory diagnosis, but the appearance of some can give a more or less accurate picture of the disease.
Curdled discharge white with a sweetish or sour smell indicates candidiasis. Other symptoms of candidiasis are:
- burning, itching in the vagina and vulva;
- swelling of the vagina after intercourse;
- pain during urination and during intercourse.
Abundant yellow or bloody discharge with an unpleasant odor may indicate bacterial vaginitis. This is an inflammation of the vagina caused by a violation of the microflora. This means that local immunity cannot restrain the growth of pathogenic bacteria, they attack the cells of the vagina, and the inflammatory process begins. Typical symptoms of bacterial vaginitis:
- redness, itching and swelling of the genitals;
- drawing pains in the lower abdomen;
- painful intercourse;
- slight increase in body temperature;
- weakness and fatigue;
- frequent urination.
Abundant frothy leucorrhoea with an unpleasant odor may indicate trichomoniasis. The causative agent of the disease are Trichomonas. The following symptoms are also observed:
- irritation of the genitals and inner thighs;
- erosion of the mucous membranes of the intimate area;
- pain when urinating;
- pain in the lower abdomen;
- pain during sexual contact.
Homogeneous yellow-green discharge with an unpleasant odor may be a sign of gonorrhea. This is an acute infectious disease caused by gonococcus and sexually transmitted. The symptoms of gonorrhea are:
- itching and pain in the urethra and vagina;
- fever;
- discharge of pus from the vagina;
- frequent painful urination;
- swollen and sore lymph nodes;
- weakness;
- nausea;
- appetite disturbance.
Serous-purulent discharge with blood often indicates the presence of a cyst in the uterus or its appendages. Symptoms of a cyst, in addition to spotting, are:
- vaginal discomfort;
- pain in lower abdomen;
- pain during intercourse;
- increase in menstrual flow;
- menstrual disorders;
- painful menstruation.
Bright yellow and green discharge in copious amounts with a very unpleasant odor indicate endometritis. This is an inflammation of the uterus caused by bacteria or trauma. Symptoms of endometritis:
- acute pain in the abdomen, in its lower part;
- fever with chills;
- increased heart rate;
- painful urination;
- weakness;
- enlargement of the uterus due to tissue inflammation;
- profuse and painful periods;
- infertility.
Brown discharge during delayed menstruation may indicate a pathological course of pregnancy, such as an ectopic pregnancy. You can judge the likelihood of this pathology by the following symptoms:
- absence of menstruation;
- sharp or cramping pain in the lower abdomen, usually on the side;
- toxicosis and other signs of pregnancy.
This is a very dangerous condition that requires immediate medical attention. Even if the pregnancy is uterine, but spotting is present, you should immediately consult a doctor, as this is a sign of a threatened abortion.
Which doctor should I contact for unhealthy vaginal discharge?
If the discharge is unnatural in color, smell or consistency, you should visit a gynecologist. The doctor will ask about the symptoms, conduct a visual examination, take a swab from the vagina and make a diagnosis based on the results of the studies. Analysis of vaginal discharge will show if there is a bacterial, viral or fungal infection, what is the degree of infection. After that, an ultrasound examination of the organs of the reproductive system is prescribed. Ultrasound will show the size of the organs of the female system, their position, the presence of neoplasms, such as cysts or tumors, and will help to specify the diagnosis. In addition, the doctor prescribes a complete blood count, cytological examination and / or colposcopy.
With a cyst or tumor, an additional consultation with an oncologist will be required. If there is a heavy discharge due to stress, it is useful to consult a psychologist. If sexually transmitted diseases are detected, an immunologist's consultation will be required. With a long course of diseases, it is useful to contact an immunologist and assess the immune status. In case of abundant discharge against the background of allergies, it is recommended to consult an allergist. In children, unhealthy discharge is evaluated by a pediatric gynecologist and pediatrician.
Treatment of abnormal vaginal discharge
Treatment of problematic discharge should always be carried out with the participation of a doctor after a thorough diagnosis.
In case of a bacterial infection and inflammation against its background, antimicrobial drugs are prescribed. Antibiotics are prescribed orally and topically in the form of suppositories, creams, ointments.
For fungal infections, antifungal drugs are prescribed. It is worth remembering that thrush is a local manifestation of extensive damage to the body by a fungus, and its treatment is not limited to suppositories and creams. The bulk of the fungus is in the intestines, so the whole body as a whole, and not just the vagina, should be treated.
With a viral infection, antiviral drugs are prescribed. Viruses are dangerous organisms, and doctors have not yet learned how to treat them effectively. This is where immunity plays an important role.
When neoplasms appear, their conservative treatment or removal is possible. Here the decisive role is played by the nature of the neoplasm - benign or malignant - and the rate of its development.
In case of uterine pregnancy with a threat of miscarriage, the patient is sent to a hospital, the condition of the uterus, placenta, and fetus is examined. In case of an ectopic pregnancy, the immediate removal of the fetal egg from the woman's body is required.
In any case, when an unhealthy discharge appears, very careful hygiene is required, since many pathological discharges corrode the skin of the genitals. Sometimes the doctor prescribes baths with therapeutic solutions and douching.
There are many folk methods for treating discharge. They sometimes help, but sometimes they can blur the clinical picture and make it difficult to diagnose and treat the disease. Of the folk methods, washing with decoctions of herbs is considered safe and useful. Chamomile, calendula, St. John's wort relieve inflammation, increase local immunity and soothe irritated skin. In no case should foreign objects be introduced into the vagina, as some folk recipes advise. This can harm the microflora and injure the already irritated vaginal mucosa.
How to prevent abnormal vaginal discharge?
The first rule of preventing painful discharge is regular hygiene. It is necessary to wash yourself every time after visiting the toilet and in the evening before going to bed. Washing is carried out with clean warm water with special means for intimate hygiene. Ordinary soap can destroy the natural microflora and promote the growth of pathogenic bacteria. Hot water kills beneficial lactobacilli, while cold water can exacerbate a viral infection.
Underwear should be changed daily. Linen should allow air to pass through and absorb moisture, therefore, linen made from natural fabrics - cotton, linen is recommended. Synthetic underwear should not be worn all the time. Tight underwear and thongs irritate the skin of the genitals and reduce local immunity. Gynecologists do not recommend using panty liners, as they interfere with air exchange.