Common problems during pregnancy
Pregnancy Complications | Maternal and Infant Health
Complications of pregnancy are health problems that occur during pregnancy. They can involve the mother’s health, the baby’s health, or both. Some women have health problems that arise during pregnancy, and other women have health problems before they become pregnant that could lead to complications. It is very important for women to receive health care before and during pregnancy to decrease the risk of pregnancy complications.
Before Pregnancy
Make sure to talk to your doctor about health problems you have now or have had in the past. If you are receiving treatment for a health problem, your health care provider might want to change the way your health problem is managed. For example, some medicines used to treat health problems could be harmful if taken during pregnancy. At the same time, stopping medicines that you need could be more harmful than the risks posed should you become pregnant. In addition, be sure to discuss any problems you had in any previous pregnancy. If health problems are under control and you get good prenatal care, you are likely to have a normal, healthy baby.
- Before Pregnancy
- During Pregnancy
- Research
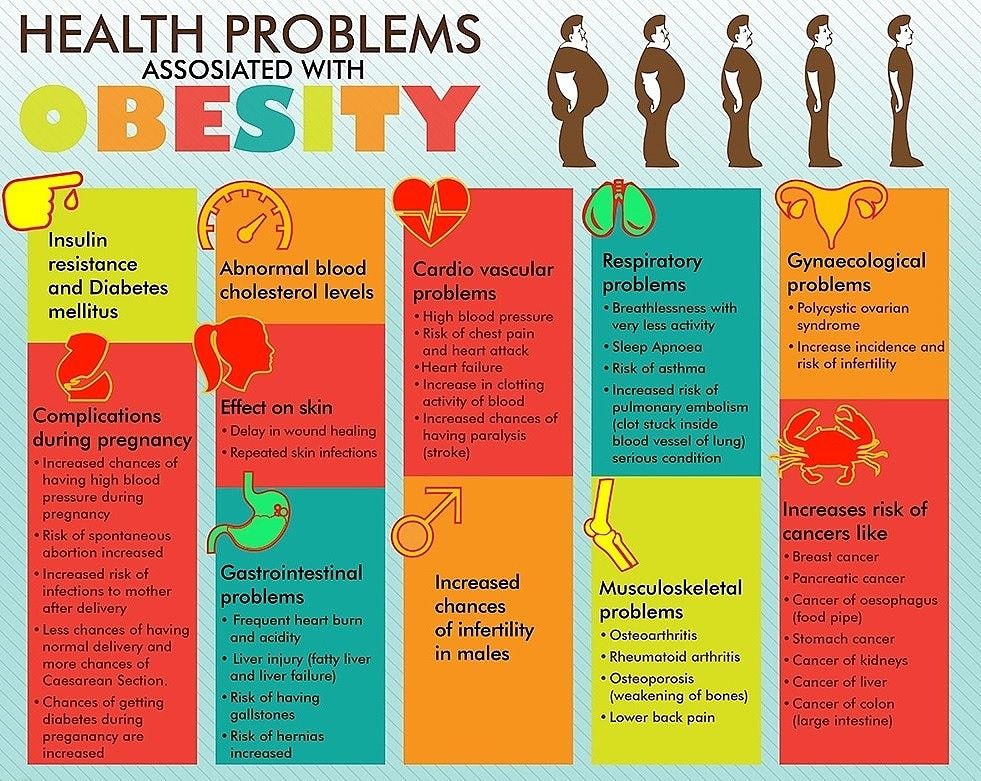
- Obesity
- Severe maternal morbidity in the United States
During Pregnancy
Pregnancy symptoms and complications can range from mild and annoying discomforts to severe, sometimes life-threatening, illnesses. Sometimes it can be difficult for a woman to determine which symptoms are normal and which are not. Problems during pregnancy may include physical and mental conditions that affect the health of the mother or the baby. These problems can be caused by or can be made worse by being pregnant. Many problems are mild and do not progress; however, when they do, they may harm the mother or her baby. Keep in mind that there are ways to manage problems that come up during pregnancy. Always contact your prenatal care provider if you have any concerns during your pregnancy.
The following are some common maternal health conditions or problems a woman may experience during pregnancy—
Anemiaexternal icon
Anemia is having lower than the normal number of healthy red blood cells. Treating the underlying cause of the anemia will help restore the number of healthy red blood cells. Women with pregnancy related anemia may feel tired and weak. This can be helped by taking iron and folic acid supplements. Your health care provider will check your iron levels throughout pregnancy.
The Hear Her campaign supports CDC’s efforts to prevent pregnancy-related deaths by sharing potentially life-saving messages about urgent warning signs.
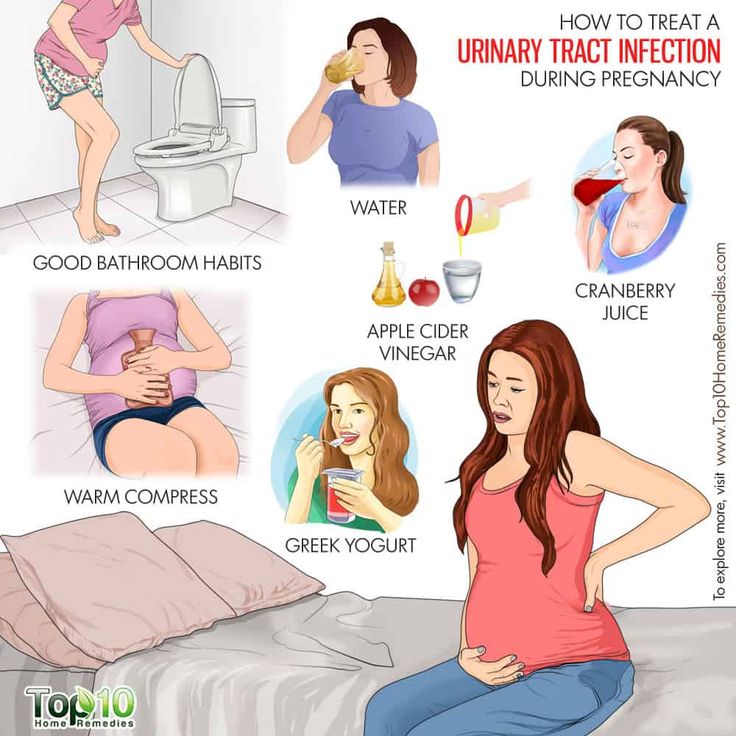
Urinary Tract Infectionsexternal icon (UTI)
A UTI is a bacterial infection in the urinary tract. You may have a UTI if you have—
- Pain or burning when you use the bathroom.
- Fever, tiredness, or shakiness.
- An urge to use the bathroom often.

- Pressure in your lower belly.
- Urine that smells bad or looks cloudy or reddish.
- Nausea or back pain.
If you think you have a UTI, it is important to see your health care provider. He/she can tell if you have a UTI by testing a sample of your urine. Treatment with antibiotics to kill the infection will make it better, often in one or two days. Some women carry bacteria in their bladder without having symptoms. Your health care provider will likely test your urine in early pregnancy to see if this is the case and treat you with antibiotics if necessary.
Mental Health Conditions
Some women experience depression during or after pregnancy. Symptoms of depression are:
- A low or sad mood.
- Loss of interest in fun activities.
- Changes in appetite, sleep, and energy.
- Problems thinking, concentrating, and making decisions.
- Feelings of worthlessness, shame, or guilt.
- Thoughts that life is not worth living.

When many of these symptoms occur together and last for more than a week or two at a time, this is probably depression. Depression that persists during pregnancy can make it hard for a woman to care for herself and her baby. Having depression before pregnancy also is a risk factor for postpartum depression. Getting treatment is important for both mother and baby. If you have a history of depression, it is important to discuss this with your health care provider early in pregnancy so that a plan for management can be made.
Hypertension (High Blood Pressure)
Chronic poorly-controlled high blood pressure before and during pregnancy puts a pregnant woman and her baby at risk for problems. It is associated with an increased risk for maternal complications such as preeclampsiaexternal icon, placental abruption (when the placenta separates from the wall of the uterus), and gestational diabetes. These women also face a higher risk for poor birth outcomes such as preterm delivery, having an infant small for his/her gestational age, and infant death. The most important thing to do is to discuss blood pressure problems with your provider before you become pregnant so that appropriate treatment and control of your blood pressure occurs before pregnancy. Getting treatment for high blood pressure is important before, during, and after pregnancy.
The most important thing to do is to discuss blood pressure problems with your provider before you become pregnant so that appropriate treatment and control of your blood pressure occurs before pregnancy. Getting treatment for high blood pressure is important before, during, and after pregnancy.
Diabetes During Pregnancy
Learn about types of diabetes during pregnancy, the percentage of women affected, and what CDC is doing to address this important health topic. Managing diabetes can help women have healthy pregnancies and healthy babies.
Obesity and Weight Gain
Recent studies suggest that the heavier a woman is before she becomes pregnant, the greater her risk of pregnancy complications, including preeclampsia, GDM, stillbirth and cesarean delivery. Also, CDC research has shown that obesity during pregnancy is associated with increased use of health care and physician services, and longer hospital stays for delivery. Overweight and obese women who lose weight before pregnancy are likely to have healthier pregnancies. Learn more about ways to reach and maintain a healthy weight before you get pregnant.
Learn more about ways to reach and maintain a healthy weight before you get pregnant.
Infectionsexternal icon
During pregnancy, your baby is protected from many illnesses, like the common cold or a passing stomach bug. But some infections can be harmful to you, your baby, or both. Easy steps, such as hand washing, and avoiding certain foods, can help protect you from some infections. You won’t always know if you have an infection—sometimes you won’t even feel sick. If you think you might have an infection or think you are at risk, see your health care provider.
Infections with HIV, viral hepatitis, STDs, and TB can complicate pregnancy and may have serious consequences for a woman, her pregnancy outcomes, and her baby. Screening and treatment for these infections, and vaccinations against viruses, such as hepatitis B and human papillomavirus, can prevent many bad outcomes.
Hyperemesis Gravidarumexternal icon
Many women have some nausea or vomiting, or “morning sickness,” particularly during the first 3 months of pregnancy.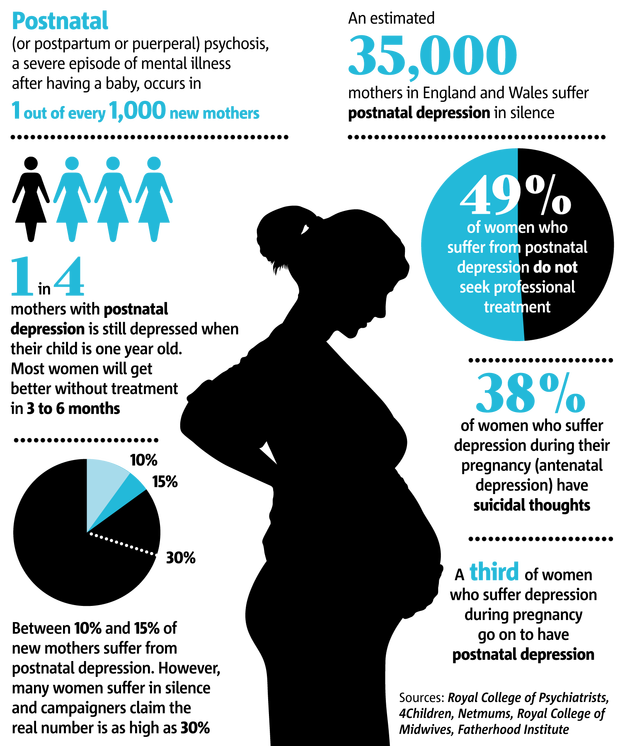 The cause of nausea and vomiting during pregnancy is believed to be rapidly rising blood levels of a hormone called HCG (human chorionic gonadotropin), which is released by the placenta. However, hyperemesis gravidarum occurs when there is severe, persistent nausea and vomiting during pregnancy—more extreme than “morning sickness.” This can lead to weight loss and dehydration and may require intensive treatment.
The cause of nausea and vomiting during pregnancy is believed to be rapidly rising blood levels of a hormone called HCG (human chorionic gonadotropin), which is released by the placenta. However, hyperemesis gravidarum occurs when there is severe, persistent nausea and vomiting during pregnancy—more extreme than “morning sickness.” This can lead to weight loss and dehydration and may require intensive treatment.
Learn more about pregnancy complications from womenshealth.gov.external icon
Top of Page
Research
CDC’s Division of Reproductive Health conducts research to better understand pregnancy-related problems, with the aims of making pregnancy healthier, preventing or managing complications, and reducing poor pregnancy outcomes, including death—the most extreme adverse outcome. There are approximately 6 million pregnancies each year in the United States. Small advances in preventing pregnancy-related complications can improve the quality of life for thousands of pregnant women. We can further the development of evidence-based public health prevention with improved sources of maternal health data, and methods for measuring and studying the data. Highlights of some of our research follow
We can further the development of evidence-based public health prevention with improved sources of maternal health data, and methods for measuring and studying the data. Highlights of some of our research follow
Obesity
In the United States, obesity during pregnancy is common and it increases obstetrical risks. In collaboration with Kaiser Permanente Northwest, CDC conducted a study to assess associations between indicators of use of health care services and body-mass index before pregnancy or in early pregnancy and found that obesity during pregnancy is associated with increased use of health care services. A higher-than-normal BMI was associated with significantly more prenatal fetal tests, obstetrical ultrasonographic examinations, medications dispensed from the outpatient pharmacy, telephone calls to the department of obstetrics and gynecology, and prenatal visits with physicians. It was also associated with significantly fewer prenatal visits with nurse practitioners and physician assistants. Most of the increase in length of stay associated with higher BMI was related to increased rates of cesarean delivery and obesity-related high-risk conditions. (Association between obesity during pregnancy and increased use of health careexternal icon. N Engl J Med 2008;358:1444–53.)
Most of the increase in length of stay associated with higher BMI was related to increased rates of cesarean delivery and obesity-related high-risk conditions. (Association between obesity during pregnancy and increased use of health careexternal icon. N Engl J Med 2008;358:1444–53.)
CDC has supported university investigators from Brigham and Women’s Hospital to develop Balance after Baby, a lifestyle intervention program tailored specifically to meet the needs of postpartum women. The primary aim of this study was to assist women with a new baby to return to a normal weight through an Internet-based program of healthy eating and physical activity, which they could participate in at their convenience.
Severe maternal morbidity in the United States
Maternal morbidity includes physical and psychologic conditions that result from or are aggravated by pregnancy and have an adverse effect on a woman’s health. The most severe complications of pregnancy, generally referred to as severe maternal morbidity (SMM), affect more than 50,000 women in the United States every year. Based on recent trends, this burden has been steadily increasing.
Based on recent trends, this burden has been steadily increasing.
Rises in SMM are likely driven by a combination of factors, including increases in maternal age, pre-pregnancy obesity, pre-existing chronic medical conditions, and cesarean delivery. The consequences of the increasing SMM prevalence are wide-ranging and include higher health service use, higher direct medical costs, extended hospitalization stays, and long-term rehabilitation. The review of SMM cases provides an opportunity to identify points of intervention for quality improvements in maternal care. Tracking SMM will help monitor the effectiveness of such interventions.
Top of Page
Complications of Pregnancy | Johns Hopkins Medicine
What are some of the more common complications of pregnancy?
Although the majority of pregnancies are uneventful, sometimes complications do happen. The following are some of the more common pregnancy complications.
Amniotic fluid complications
Too much or too little amniotic fluid in the sac around the fetus may be a sign of a problem with the pregnancy. Too much fluid can put too much pressure on the mother's uterus, leading to preterm labor. It also can cause pressure on the mother's diaphragm. This can lead to breathing difficulties. Fluids tend to build up in cases of uncontrolled diabetes, a multiple pregnancy, incompatible blood types, or birth defects. Too little fluid may be a sign of birth defects, growth retardation, or stillbirth.
Too much fluid can put too much pressure on the mother's uterus, leading to preterm labor. It also can cause pressure on the mother's diaphragm. This can lead to breathing difficulties. Fluids tend to build up in cases of uncontrolled diabetes, a multiple pregnancy, incompatible blood types, or birth defects. Too little fluid may be a sign of birth defects, growth retardation, or stillbirth.
Bleeding
Bleeding in late pregnancy may be a sign of placental complications, a vaginal or cervical infection, or preterm labor. Women who bleed in late pregnancy may be at greater risk of losing the fetus and bleeding excessively. Bleeding at any time during the pregnancy should be reported to your healthcare provider right away.
Ectopic pregnancy
An ectopic pregnancy is the development of the fetus outside of the uterus. This can happen in the fallopian tubes, cervical canal, or the pelvic or belly. The cause of an ectopic pregnancy is usually scar tissue in the fallopian tube from infection or disease.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) The risk of ectopic pregnancy is increased in women who have had tubal sterilization procedures, especially women who were younger than age 30 at the time of sterilization.
The risk of ectopic pregnancy is increased in women who have had tubal sterilization procedures, especially women who were younger than age 30 at the time of sterilization.
Ectopic pregnancies happen in about 1 out of 50 pregnancies and can be very dangerous to the mother. Symptoms may include spotting and cramping. The longer an ectopic pregnancy goes on, the greater the chance that a fallopian tube will rupture. An ultrasound and blood tests may confirm the diagnosis. Treatment of an ectopic pregnancy may include medicine or surgical removal of the fetus.
Miscarriage or fetal loss
A miscarriage is pregnancy loss that happens up to 20 weeks of gestation. Most miscarriages happen before 12 weeks. Miscarriages happen in about 15% of all pregnancies and are usually due to genetic or chromosomal abnormalities.
Miscarriages are usually preceded by spotting and intense cramping. To confirm a miscarriage, an ultrasound and blood tests may be done. The fetus and contents of the uterus are often naturally expelled. If this does not happen, a procedure called a dilation and curettage (D & C) may be necessary. This procedure uses special instruments to remove the abnormal pregnancy.
If this does not happen, a procedure called a dilation and curettage (D & C) may be necessary. This procedure uses special instruments to remove the abnormal pregnancy.
Fetal loss in the second trimester may happen if the cervix is weak and opens too early. This is called incompetent cervix. In some cases of incompetent cervix, a healthcare provider can help prevent pregnancy loss by stitching the cervix closed until delivery.
Placental complications
Under normal circumstances, the placenta attaches to the uterine wall. However, two types of placental complications may happen, including:
Placental abruption is more common in women who smoke, have high blood pressure, and/or have a multiple pregnancy. It also happens in women who have had previous children or a history of placental abruption. Symptoms and treatment of placental abruption depend on the degree of detachment. Symptoms may include bleeding, cramping, and belly tenderness. Diagnosis is usually confirmed by doing a complete physical exam and an ultrasound. Women are usually put in the hospital for this condition. They may have to deliver the baby early.
Women are usually put in the hospital for this condition. They may have to deliver the baby early.
Placenta previa. Normally, the placenta is located in the upper part of the uterus. Placenta previa is a condition in which the placenta is attached close to or covering the cervix (the opening into the uterus). This type of placental complication happens in about 1 in every 200 deliveries and happens more often in women who have scarring of the uterus from previous pregnancies. It also happens in women who have fibroids or other problems in the uterus, or in women who have had previous uterine surgeries.
Symptoms may include vaginal bleeding that is bright red and not associated with belly tenderness or pain. Diagnosis is confirmed by doing a physical exam and an ultrasound. Depending on how bad the problem is and the stage of pregnancy, a change in activities or bed rest may be ordered. The baby usually has to be delivered by cesarean section to keep the placenta from detaching early and depriving the baby of oxygen during delivery.
Preeclampsia or eclampsia
Preeclampsia, formerly called toxemia, is characterized by pregnancy-induced high blood pressure. It is accompanied by protein in the urine. Sometimes swelling due to fluid retention is also present. Eclampsia is the more severe form of this problem. This can lead to seizures, coma, or even death.
The cause of preeclampsia is unknown, but it is more common in first pregnancies. It affects about 5% to 8% of all pregnant women. Other risk factors for preeclampsia include:
A woman carrying multiple fetuses
A teenage mother
A woman older than 40
A woman with high blood pressure, diabetes, and/or kidney disease before she became pregnant
A woman who is obese with a BMI greater than 30
Symptoms may include severe swelling of the hands and face, high blood pressure, headache, dizziness, irritability, decreased urine output, belly pain, and blurred vision. Treatment will vary according to the severity of the condition and the stage of the pregnancy. Treatment may include hospitalization, bed rest, medicine to lower blood pressure, and close monitoring of both the fetus and the mother.
Treatment may include hospitalization, bed rest, medicine to lower blood pressure, and close monitoring of both the fetus and the mother.
Pathologies of pregnancy and childbirth: treatment
Preservation of pregnancy
Pregnancy is a natural process for the female body. However, not every organism can independently adapt to the role of a future mother. In this case, various pathologies of pregnancy may occur - disturbances in the work of the endocrine, central nervous and vascular systems of the body during the physiological process of bearing a child. The most common pathologies are toxicosis of pregnant women, or gestosis. Toxicosis can occur at different stages of pregnancy. Each of them can pose a serious danger to the health and life of the mother and child. In the Department of Pathology of Pregnancy, we provide both outpatient and inpatient treatment in order to maintain pregnancy, reduce the negative factors of its development, and improve well-being.
There is a "risk group" during pregnancy - these are women with hypertension, arterial hypotension, varicose veins, heart defects, bronchial asthma, pyelonephritis, diabetes mellitus and a number of other chronic diseases of various systems and organs. An additional risk factor is the woman's age. Pregnancy after 35 years of age can be accompanied by complications.
An additional risk factor is the woman's age. Pregnancy after 35 years of age can be accompanied by complications.
Most expectant mothers, to one degree or another, need qualified medical support from the first weeks of pregnancy - for the safe bearing and birth of a healthy baby. It is important to note: if the gynecologist recommends pregnancy support in a hospital, this recommendation should not be neglected. Preservation of pregnancy in hospital conditions is a guarantee of safety for your life and the life of the baby, because you will be under the constant supervision of competent specialists who can provide timely assistance.
Management of complicated pregnancy, treatment of pathologies of pregnancy - a specialized area of obstetric departments of medical clinics "Mother and Child". Each treatment program is created individually as a result of the interaction of highly qualified specialists from various fields of medicine, while meeting all the standards of pregnancy management in Russia.
Depending on the medical situation, the plan of the treatment program can be simultaneously worked on by: an obstetrician-gynecologist, specialists in the field of laboratory, functional and prenatal diagnostics, an endocrinologist, a reproductive specialist, a geneticist, a gastroenterologist, a cardiologist, a neurologist, a psychotherapist, a nephrologist, a leukologist, a surgeon, oncologist - those doctors whose competence is medical care for a woman and a child. We use effective and safe methods of diagnostics, drug therapy, surgical treatment of pregnant women.
Departments of Pathology of Pregnancy "Mother and Child" include hospitals equipped with all necessary equipment for continuous monitoring of the condition of mother and child, effective and safe treatment of various obstetric and extragenital pathologies. Preparation for a planned caesarean section is also carried out in the hospital of the pregnancy pathology department.
Departments of Pathology of Pregnancy "Mother and Child" - these are hospitals where:
- Diagnosis and treatment of nephropathy in pregnancy
- Diagnosis and treatment of pathologies of the fetoplacental system
- Diagnosis and treatment of late toxicosis - OPG-preeclampsia: edema, proteinuria, hypertension in pregnancy, preeclampsia of varying severity.

- Diagnosis and treatment of pre-eclampsia and eclampsia of pregnancy
- Diagnosis and treatment of early toxicosis, dermatosis of pregnant women
- Overcoming the threat of miscarriage and preterm birth
- Prevention of toxemia during pregnancy
Preservation of pregnancy in "Mother and Child" is possible with :
- Diseases of the gastrointestinal tract
- Diseases of the organs of vision
- Blood diseases
- Respiratory diseases: bronchial asthma, chronic bronchitis, pneumonia
- Diseases of the kidneys and urinary system: pyelonephritis, glomerulonephritis, cystitis
- Multiple pregnancy
- Presence of uterine fibroids
- History of cancer
- Tumors of the ovaries
- Amniotic fluid pathologies
- Recurrent miscarriage
- Various forms of bacterial and viral infections
- Various forms of inflammatory diseases of the urinary-genital system
- Rhesus-conflict blood
- Cardiovascular diseases: various cardiac arrhythmias, congenital and acquired heart defects, mitral valve prolapse, hypertension
- Fetal growth retardation syndrome
- Placental insufficiency syndrome
- Fetoplacental insufficiency
- Endocrinological diseases: thyroid pathology, diabetes mellitus
In the medical clinics "Mother and Child" outpatient and inpatient treatment of pregnancy pathologies is possible. We do our best to ensure that every woman safely bears a pregnancy - and a healthy baby is born.
We do our best to ensure that every woman safely bears a pregnancy - and a healthy baby is born.
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
All directionsGynecological proceduresSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.
Gynecological procedures
02.
Consultations of specialists (adults)
03.
Consultations of specialists (children's)
04.
Laboratory of molecular genetics
05.
General studies
06 for adults
08.
Therapeutic investigations
09.
Adult ultrasound examinations
Nothing found
The administration of the clinic takes all measures to update the price list posted on the website in a timely manner, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Questions from pregnant women • pregnancy • answers from a gynecologist
Questions from pregnant women • pregnancy • answers from a gynecologistI agree
We use cookies to help us provide a convenient and secure experience for visitors to the site. By clicking the "Agree" button, you consent to the use of cookies. You can revoke your consent at any time by changing your browser settings and deleting your saved cookies.
By clicking the "Agree" button, you consent to the use of cookies. You can revoke your consent at any time by changing your browser settings and deleting your saved cookies.
Answers to questions prepared by gynecologists, specialists in childbirth clinic Premium Medical.
What week of pregnancy should I register and why? Open
- You need to register before the 12th week of pregnancy in order to do all the necessary tests, including genetic, and ultrasonoscopy. Based on this information, the doctor can timely detect and better help in case of various complications, as well as more accurately calculate the expected due date.
How many times during pregnancy will I need to visit a gynecologist? What for? Open
- According to the state program, visits to the gynecologist during pregnancy are provided at least 6 times, but in each case the doctor draws up an individual plan for monitoring the pregnant woman, and it often happens that additional examinations or a visit are needed.
 You need to go to the doctor in order to detect complications in a timely manner, which, if not eliminated, can be dangerous for both the woman and the fetus. For example, advanced urinary tract infection or anemia adversely affects fetal development, and undiagnosed and untreated diabetes or high blood pressure can even be life-threatening for the mother and fetus.
You need to go to the doctor in order to detect complications in a timely manner, which, if not eliminated, can be dangerous for both the woman and the fetus. For example, advanced urinary tract infection or anemia adversely affects fetal development, and undiagnosed and untreated diabetes or high blood pressure can even be life-threatening for the mother and fetus.
What does the gynecologist do during the monthly follow-up visit? Open
- During a monthly visit, the gynecologist discusses the course of pregnancy with the pregnant woman, listens to complaints, explains the results of tests, answers questions, gives recommendations on the regimen and nutrition at each stage of pregnancy, examines and evaluates the general state of health (if there is anemia, high blood pressure, edema), weighs the woman and assesses weight gain, measures the diameter of the abdomen, which indicates adequate fetal growth, determines the position of the fetus, which is necessary for planning childbirth, sends for a urinalysis to prevent urinary tract infections that are common in pregnant women, listens to the fetal heartbeat and based on the information received, he prescribes the necessary tests or additional examinations for the next time.

Is spotting normal during pregnancy? In what cases - yes and in what - no? What to do in this case? Open
- Many women complain of spotting during pregnancy. In most cases, everything ends well, but discharge cannot be considered normal, because it often indicates serious problems, so you should always consult a doctor. Without a doctor's examination, it is impossible to say whether spotting is dangerous or not.
For which sensations, complaints and symptoms, you should definitely contact your gynecologist or the nearest hospital? Open
- A doctor should be consulted in case of sudden, sharp, severe pain in any part of the abdomen that does not go away, in case of pulling, sharp pain in the lower abdomen, which intensifies, or bleeding. A consultation with a doctor is also necessary if there are serious symptoms not related to pregnancy, for example, prolonged, repeated vomiting, high fever (above 38.5), etc.

About Magne B6, folic acid, iron supplements and vitamins - do all pregnant women need them? Open
- All pregnant women before the 12th week of pregnancy should take folic acid, because it is responsible for the development of the fetal nervous system. The need for the use of other vitamins is determined by the gynecologist, depending on the time of year, diet and the general condition of the woman. Iron-containing drugs should be taken if the tests indicate anemia (including latent) or its threat. The need to take magnesium supplements is also assessed by the doctor. These drugs should not be taken by all pregnant women - you should consult your doctor.
Will I harm myself and my baby by attending pregnancy gymnastics classes? Open
- Gymnastics for pregnant women cannot do any harm to the baby - on the contrary. If there is no risk of abortion and the doctor allows gymnastics, it must be done. Exercising helps prepare for childbirth, reduces back pain that often occurs during pregnancy, improves overall well-being and provides additional energy.

What is 1st trimester screening? Why is it being done? Open
- The 1st trimester biochemical screening is a blood test given by a pregnant woman around the 10th week of pregnancy to determine the level of PAPP-A and free b-HCG in the mother's blood. For more accurate results, this analysis is combined with fetal ultrasonoscopy at 12-13 weeks. To make the screening results more accurate, the exact gestational age, weight and age of the pregnant woman are important, because taking into account these indicators and the results of the study, the risk of Down syndrome is calculated using a computer program.
First trimester screening identifies approximately 80% of fetal genetic abnormalities, and the number of diagnosed cases increases to 90% if fetal ultrasonography is accurate. The changes revealed by the screening method do not yet mean the presence of a congenital pathology. The purpose of screening is to timely identify a group of pregnant women at risk of giving birth to a child with genetic diseases or congenital malformations.
 Pregnant women from the high genetic risk group are referred to a geneticist for additional research.
Pregnant women from the high genetic risk group are referred to a geneticist for additional research.
How to interpret "poor" 1st trimester screening results? Open
- "Bad" results of biochemical screening do not yet mean that the fetus really has some kind of congenital pathology. The results only show the risk. For example, a score of 1:50 is considered high risk, which means that out of 50 women, one may have a fetus with a genetic disease. If biochemical screening and ultrasonoscopy of the first trimester state an increased genetic risk, the pregnant woman is referred for an additional examination to a geneticist.
I am 8 weeks pregnant and have a 4cm cyst! Is it harming my pregnancy? There were pains in the lower abdomen, from the side of the back, in the side where the cyst was found. Open
- During pregnancy, the so-called corpus luteum works in the ovaries, which produces progesterone, a hormone that protects pregnancy.
 Sometimes it happens that a cyst forms around this corpus luteum during pregnancy. These cysts usually resolve on their own before the 16th week and are rarely operated on unless the cysts are very large. These cysts, as a rule, do not have any bad effect on the development of the fetus. The size of the cyst can be monitored by ultrasonography. The final decision on what and how to deal with the cyst will be made by your doctor, after evaluating other factors as well.
Sometimes it happens that a cyst forms around this corpus luteum during pregnancy. These cysts usually resolve on their own before the 16th week and are rarely operated on unless the cysts are very large. These cysts, as a rule, do not have any bad effect on the development of the fetus. The size of the cyst can be monitored by ultrasonography. The final decision on what and how to deal with the cyst will be made by your doctor, after evaluating other factors as well.
Can a 4D USG (4D fetal imaging) be done at Premium Medical? What does it give? Does this affect the course of pregnancy? Open
- Yes, 4D USG can be done at Premium Medical Clinic. This does not affect either the course of pregnancy or the fetus and allows you to get an anatomical image of the fetus, examine the face (jaw anomalies), bone pathologies, heart function, etc.
What does listening to fetal heart sounds mean? When is it done and why? Open
- Fetal heart sounds from about the 12th week can be heard through the mother's abdomen with the so-called doppler.
 Previously, this was done with a stethoscope. Thus, the doctor hears how fast the fetal cardiac activity is, whether it is rhythmic. This check is carried out at each visit. At the end of pregnancy, the fetal heart sounds can be recorded on paper tape - this is called cardiotocography (KTG).
Previously, this was done with a stethoscope. Thus, the doctor hears how fast the fetal cardiac activity is, whether it is rhythmic. This check is carried out at each visit. At the end of pregnancy, the fetal heart sounds can be recorded on paper tape - this is called cardiotocography (KTG). KTG recording takes 15-30 minutes. There are two detectors on the woman's abdomen: one registers the heart sounds of the fetus, the second - the activity of the uterus. The results of KTG are evaluated by a specialist on a 10-point scale. KTG at the end of pregnancy is a good and easy test to check the health of the fetus. If the KTG is low, the doctor knows how to act to help the fetus. If the KTG readings are good, then the fetus is doing well at the moment.
What should I do if I am afraid of giving birth and my gynecologist thinks that I have no gynecological obstacles for natural childbirth? Open
- You need to understand why you are afraid of childbirth.
 The advice of a professional is best here - talk with your doctor, with a psychologist, attend preparatory classes. We are always afraid of the unknown, and knowledge helps to overcome fears. If you are afraid of pain, then talk to your doctor about the possibility of epidural anesthesia. If you're afraid of being alone, look for opportunities to give birth with your chosen doctor, midwife, or "spiritual midwife". If there are no serious obstacles to this, then an easy natural birth is the best way to bring a child into the world (it is the best way for both mother and child).
The advice of a professional is best here - talk with your doctor, with a psychologist, attend preparatory classes. We are always afraid of the unknown, and knowledge helps to overcome fears. If you are afraid of pain, then talk to your doctor about the possibility of epidural anesthesia. If you're afraid of being alone, look for opportunities to give birth with your chosen doctor, midwife, or "spiritual midwife". If there are no serious obstacles to this, then an easy natural birth is the best way to bring a child into the world (it is the best way for both mother and child).
How to prepare for an easier birth? Open
- Premium Medical gynecologist, childbirth specialist Gita Ruttasa answers.
Today, there are several ways to reduce the pain of childbirth and make the experience of childbirth easier if needed. Although expectant mothers have this option in mind, most still want to fully experience the birth of a baby. It may seem that natural and easy childbirth do not go hand in hand, but this experience largely depends on the woman herself, on the attitude to childbirth and understanding of how it occurs.
 In order not to tremble with fear in anticipation of this big event, both the body and the mind must be prepared for it.
In order not to tremble with fear in anticipation of this big event, both the body and the mind must be prepared for it.
What should a mother-to-be take into account already during pregnancy in order to prepare for an easier birth? Open
- Expectant mothers during the entire period of pregnancy should keep in mind that the purpose of pregnancy is childbirth, and to achieve this goal, you need to prepare for the entire period of pregnancy. It is very important to be physically active during pregnancy and eat a balanced, light diet. It is no longer believed that a pregnant woman should "eat for two." This, of course, is a woman's dream - to eat whatever you want, without consequences, but the wrong choice of food will affect it during childbirth, and will also affect the figure of a woman after childbirth. During pregnancy, each day a woman should receive an additional 200 calories, which is equal to one bowl of grain products. Childbirth requires not only physical effort from a woman, but also a lot of emotions, so emotional preparation is very important.
 The expectant mother must gain calmness and determination in preparation for an important event. The more a pregnant woman is aware of the process of childbirth, the easier it is. The unknown scares us, and knowledge reduces fear.
The expectant mother must gain calmness and determination in preparation for an important event. The more a pregnant woman is aware of the process of childbirth, the easier it is. The unknown scares us, and knowledge reduces fear. During pregnancy, you should try to establish an emotional connection with the baby, the mother should feel with him as a whole, this will help her to obey her instincts during childbirth. Emotional connection can be achieved if you regularly talk to the child, putting one hand on the stomach in the place where the fetal head is, and with the other hand stroke the stomach and talk. The baby begins to hear from the 14th week of pregnancy. You can listen to your favorite music and play it during childbirth, which will help create a pleasant atmosphere.
Birth is the day the baby comes into the world, it is the first day of a newborn's life, and pain is part of that wonderful process. The fuller the contractions, the easier and faster the baby is born - this must be realized and accepted.
 If the expectant mother has a low pain threshold, there is no need to be afraid of using epidural anesthesia or the so-called laughing gas. The most important thing is for a woman to be in harmony with what is happening.
If the expectant mother has a low pain threshold, there is no need to be afraid of using epidural anesthesia or the so-called laughing gas. The most important thing is for a woman to be in harmony with what is happening.
How can you physically prepare for childbirth to make the process easier? Open
- To physically prepare your body for childbirth, you need to follow a diet. Many moms-to-be may frown upon hearing this, but it's a sad truth. The period of pregnancy is not provided in order to feast on everything that the soul desires. Modern food products have a high energy value and are very seductively decorated, it is difficult to refrain from eating them. If you really want, from time to time you can afford some kind of delicacy, but observing the measure. Pregnant women should try to avoid foods with wheat and refined carbohydrates, which, unfortunately, are present in desserts, chocolate, bread, cookies, etc. Foods containing wheat lead to water retention in the body, which can contribute to swelling of the vaginal tissues and prevent easy opening and dilation of the cervix.
 If you refuse wheat products, the body will absorb iron better, and you will have to take less iron supplements. You should try to eat meat with salad once a day, which will help to avoid anemia - lack of iron. In the case of anemia, tissues receive less oxygen and cannot fully function, and during childbirth, a lot of energy is needed. You should also try to reduce your intake of sugar and sugar-containing foods. There may be days when you feel frustrated and angry because you can't eat everything you want, but you need to remember that the compromise you make now will pay off in the future.
If you refuse wheat products, the body will absorb iron better, and you will have to take less iron supplements. You should try to eat meat with salad once a day, which will help to avoid anemia - lack of iron. In the case of anemia, tissues receive less oxygen and cannot fully function, and during childbirth, a lot of energy is needed. You should also try to reduce your intake of sugar and sugar-containing foods. There may be days when you feel frustrated and angry because you can't eat everything you want, but you need to remember that the compromise you make now will pay off in the future. Healthy eating must be combined with physical activity. Many women cut back on physical activity as they become pregnant. At the very beginning of pregnancy, this is natural, since weakness, nausea and other phenomena that prevent physical activity are possible. However, if only laziness interferes, you should not indulge in it. During pregnancy, a woman is rapidly gaining weight, and it becomes a big burden on the bones and joints.
 Proper nutrition will help not to gain extra pounds, and everyday physical activity will allow you not to feel like a "ball". Walks are highly recommended. While walking, the baby's head moves with every step, which can stretch the cervix. It is advisable to walk in a rhythmic step, but without accelerated breathing, so that the walk does not feel like a difficulty. A walk along the sea or through a pine forest will help you achieve peace and inner harmony. Swimming and water aerobics are recommended during pregnancy. Swimming helps the child to take the correct position, and also unloads the joints of the pregnant woman, this is an excellent load for the circulatory system. Gymnastics for pregnant women is also a good way to increase your physical endurance under the guidance of a specialist. To make childbirth easy, it is important that the joints in the lower back, lower back and coccyx are mobile.
Proper nutrition will help not to gain extra pounds, and everyday physical activity will allow you not to feel like a "ball". Walks are highly recommended. While walking, the baby's head moves with every step, which can stretch the cervix. It is advisable to walk in a rhythmic step, but without accelerated breathing, so that the walk does not feel like a difficulty. A walk along the sea or through a pine forest will help you achieve peace and inner harmony. Swimming and water aerobics are recommended during pregnancy. Swimming helps the child to take the correct position, and also unloads the joints of the pregnant woman, this is an excellent load for the circulatory system. Gymnastics for pregnant women is also a good way to increase your physical endurance under the guidance of a specialist. To make childbirth easy, it is important that the joints in the lower back, lower back and coccyx are mobile. From time to time, a pregnancy massage should be done, focusing on the areas where you feel the most tension.
You can also massage the intimate area with massage oil, lightly, in a circular motion, applying a small amount of oil to the skin of the perineum. It is advisable to use proven products so that the oil does not contain parabens, preservatives and other chemical impurities.
How can a future mother emotionally prepare herself for a big event, how to overcome fear if it arises? Open
- The process of childbirth is very dependent on the psycho-emotional state of the woman. The resulting fear of childbirth can be overcome by reading positive stories about childbirth, getting acquainted with the experience of other women. Sometimes you can get encouragement from a mother who has had a positive experience with childbirth. It is recommended not to read anything on the Internet about difficult, unsuccessful births. Fear is a major hindrance to easy labor because it releases adrenaline, which tightens the muscles, which can stop the cervical dilation and prevent effective contractions.
 Breathing exercises can help reduce anxiety and fear.
Breathing exercises can help reduce anxiety and fear. Proper breathing during childbirth will divert attention from pain and improve the oxygen supply to mother and baby. It is recommended to master diaphragmatic breathing. Sit on a chair or stand with your back straight, if you want, you can lie down on the floor, it is important that the base is hard. Place one hand on your chest, the other on your stomach, inhale slowly through your nose, counting to four. Try to push the air that you inhale into the stomach - the stomach rises like a ball. You feel the hand placed on your stomach rise. Exhale slowly through your mouth to the count of six. Light pressure of the hand on the abdomen can help the diaphragm to descend. Exercise is recommended to be performed at least 1-2 times a day daily. Only in this way will the body learn to recognize the relaxing effect of breathing. Deep breathing has a positive effect on the autonomic nervous system, reduces the symptoms of anxiety and does not allow them to grow.
 Note that with this breath, the exhalation should always be longer than the inhalation.
Note that with this breath, the exhalation should always be longer than the inhalation. Our body instinctively knows what to do - fear and anxiety raise their heads and make us feel nervous tension. To better prepare for the big event, you can also attend childbirth preparation courses. If you have received more information and understand how the birth process proceeds, you will not have the feeling of meeting the unknown, and this is one of the reasons for fear. Classes are a great way to involve your partner in the process of preparing for childbirth, the opportunity to get closer to him even more.
How can a partner help make childbirth easier? Open
- The role of a man is to support - both emotionally and physically, especially if a woman has a bad relationship with her mother, from whom she should draw positive experience and encouragement. In this case, it is desirable that this role be performed by a partner.
The father is not physically involved in the pregnancy, but his presence is extremely important for the woman.
 For a woman, the feeling that she is being cared for and pampered plays a very important role in the emotional preparation for childbirth. The more a pregnant woman trusts her partner, the more secure she will feel during childbirth. A woman herself manages her birth, and often the support of a partner is needed for her to realize this. Childbirth is a transition from the status of a daughter to the status of a mother, this is a time of great change for a woman, the most beautiful moment in her life!
For a woman, the feeling that she is being cared for and pampered plays a very important role in the emotional preparation for childbirth. The more a pregnant woman trusts her partner, the more secure she will feel during childbirth. A woman herself manages her birth, and often the support of a partner is needed for her to realize this. Childbirth is a transition from the status of a daughter to the status of a mother, this is a time of great change for a woman, the most beautiful moment in her life!
How to avoid stretch marks and how to deal with them after childbirth? Open
- Premium Medical cosmetologist Marina Tkachenko answers
During pregnancy, the shape of the female body rapidly changes, it becomes fuller, in some places ruptures of connective tissues are possible. Subcutaneous tissue ruptures, or stretch marks, are caused by excessive stretching of the skin. If the skin is not elastic enough and lacks collagen, then in places that react most quickly to weight changes (anterior and lateral walls of the abdomen, thighs, forearms), we can observe the formation of stretch marks.
 Stretch marks are not only dependent on the elasticity of the skin, they are influenced by a number of factors - the woman's age, heredity, general health and lifestyle, as well as the time and attention paid to skin care during pregnancy. Although you cannot completely prevent stretch marks, you can cosmetically reduce their formation, reduce the area, even out them and achieve the skin looking young and firm.
Stretch marks are not only dependent on the elasticity of the skin, they are influenced by a number of factors - the woman's age, heredity, general health and lifestyle, as well as the time and attention paid to skin care during pregnancy. Although you cannot completely prevent stretch marks, you can cosmetically reduce their formation, reduce the area, even out them and achieve the skin looking young and firm.
What can be done to reduce the risk of stretch marks? Open
- To avoid the formation of stretch marks, you need to think about skin care during pregnancy in a timely manner. Preventive skin care is the most effective way to avoid stretch marks and other problems. It is important to skillfully use the resources that we already have in us so that we do not have to deal with the problem in an artificial way. Prevention is based on a healthy lifestyle.
A healthy and balanced diet is the first step to good health and appearance. The body, taking healthy food, receives all the vitamins and nutrients it needs, vitamins A, D3, E, and omega-3 and omega-6 fatty acids will take care of the skin condition.
 To be sure that her diet is balanced and complete, a woman can go to a consultation with a nutrition specialist who will talk in more depth about the principles of proper nutrition. If you still have to take additional vitamins, this will be reported by a doctor who monitors your state of health. It is also very important to drink enough water so that the body functions fully and the skin is provided with the right level of hydration.
To be sure that her diet is balanced and complete, a woman can go to a consultation with a nutrition specialist who will talk in more depth about the principles of proper nutrition. If you still have to take additional vitamins, this will be reported by a doctor who monitors your state of health. It is also very important to drink enough water so that the body functions fully and the skin is provided with the right level of hydration. Since the received vitamins and nutrients are mainly spent on the normal functioning of the body, very little remains for the skin. The main function of the skin is protective, so we must additionally help it to be in good shape using various cosmetic products. Already from the first months of pregnancy, it is recommended to smear the body with cream or body oil. The offer of body care products is very wide, you can buy special creams against stretch marks, but the nourishing and moisturizing cream that we use on a daily basis is also suitable for this.
 The most important thing is not only to apply cream or oil to the body, but also to massage it thoroughly, giving the process more time and attention. This is how you care for and show love not only to the unborn child, but also to your body.
The most important thing is not only to apply cream or oil to the body, but also to massage it thoroughly, giving the process more time and attention. This is how you care for and show love not only to the unborn child, but also to your body. Contrast showers, Charcot showers are also excellent prophylactic measures, if only these procedures are pleasant for the expectant mother and do not cause discomfort. Do not forget about physical activity, you should be in the fresh air as much as possible, take long walks or go to therapeutic exercises.
If stretch marks still form, can they be reduced by any procedures, cosmetics? Open
- If stretch marks are nevertheless formed and there is a desire to reduce them, it is advisable to do this as soon as possible, while the stretch marks are relatively fresh and easier to correct. If you are a breastfeeding mother, you should consult your doctor before undertaking any cosmetic procedures.
One of the most common treatments for reducing stretch marks is body massage.
 Depending on the type of massage, it will help restore skin elasticity after childbirth, strengthen muscles, stimulate skin blood circulation, which in turn promotes the formation of collagen. To improve skin tone, wraps, vacuum massage, lymphatic drainage massage, body peeling (AHA, chemical and abrasive peeling) are recommended to help reduce stretch marks. It should be noted that these procedures are carried out in a course, one or two times will not be enough. Also, body treatments should be combined with regular physical activity (walking, swimming in the pool, therapeutic exercises) and a balanced, healthy diet.
Depending on the type of massage, it will help restore skin elasticity after childbirth, strengthen muscles, stimulate skin blood circulation, which in turn promotes the formation of collagen. To improve skin tone, wraps, vacuum massage, lymphatic drainage massage, body peeling (AHA, chemical and abrasive peeling) are recommended to help reduce stretch marks. It should be noted that these procedures are carried out in a course, one or two times will not be enough. Also, body treatments should be combined with regular physical activity (walking, swimming in the pool, therapeutic exercises) and a balanced, healthy diet. Body mesotherapy is often used to reduce stretch marks. These are subcutaneous injections of natural, biologically active substances that stimulate the self-healing of the skin, contribute to its elasticity and tone. The procedure uses microneedles, through which extracts of plant and animal origin, vitamins, amino acids and minerals are injected under the skin, which in the form of injections act much more effectively than traditional cosmetics.
 Getting under the skin, active substances act on certain places - mesotherapeutic preparations are injected in small doses precisely into problem areas. Depending on the desired effect, you can choose different mesotherapy cocktails. This procedure is carried out in a course, and then prevention is desirable - a repetition of the procedure every 3-6 months.
Getting under the skin, active substances act on certain places - mesotherapeutic preparations are injected in small doses precisely into problem areas. Depending on the desired effect, you can choose different mesotherapy cocktails. This procedure is carried out in a course, and then prevention is desirable - a repetition of the procedure every 3-6 months. One of the most advanced treatments for effectively reducing stretch marks is Plasmolifting, or I-PRF. This is a progressive treatment method that helps to restore the skin and improve its condition. The main advantage of this method is the absence of side effects, because the patient's own blood is used, to which no other chemicals are added. Thus, there is no risk of allergic reactions and infections. This is a reliable and natural method that allows you to improve the condition and appearance of the skin, using the resources of the patient. In addition, during the procedure, the patient feels only slight discomfort, because thin needles are used, which practically do not cause pain.