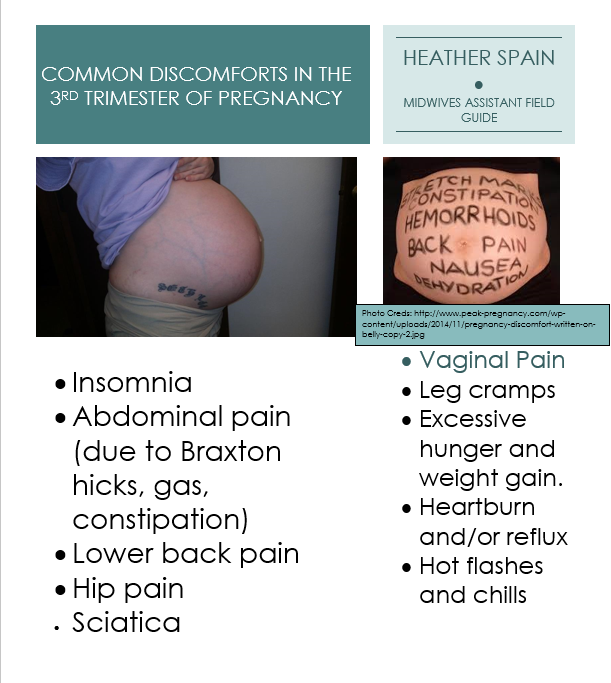
Common complaints during pregnancy
Common complaints during pregnancy | nidirect
Most health-related issues associated with pregnancy can be easily dealt with by a midwife, doctor or pharmacist. Some mothers may develop more complicated problems which could require going to hospital or an antenatal clinic.
Covid-19 guidance for pregnant women and information on what is happening in their regional unit can be found on NI Maternity
Morning sickness
Feeling nauseous or sick in the early stages of pregnancy is extremely common. Morning sickness usually occurs during the first three months of pregnancy, although for some women it may last longer.
Although it is known as morning sickness, it can last throughout the day.
Most sufferers will feel nauseous, but may not be sick, while other women find they are not able to keep any food down. Morning sickness is caused by hormones which are helping in the development of the baby and placenta. Although the symptoms are unpleasant, they won’t harm the developing baby.
You can help counter morning sickness by:
- eating small, frequent meals
- eating dry, carbohydrate snacks throughout the day
- taking rests throughout the day
- keeping well hydrated with water, avoid alcohol and caffeine
- wear comfortable clothing, tight waistbands can make you feel worse
If you are being sick all the time and cannot keep food down, tell your midwife or doctor. Some pregnant women experience severe nausea and vomiting. This condition is called hyperemesis gravidarum and needs specialist treatment.
Constipation
You may become constipated in early pregnancy because of the hormonal changes taking place in your body.
You can avoid constipation by;
- eating foods that are high in fibre, like wholemeal breads, wholegrain cereals, fruit and vegetables, beans and lentil
- exercising regularly to keep your muscles toned
- drinking plenty of water
- avoiding iron supplements – ask your doctor if you can manage without them or switch to a different type
Pain management during pregnancy
Pregnant women can suffer from mild headaches and other aches and pains. However, not all painkillers can be used during pregnancy.
However, not all painkillers can be used during pregnancy.
Non-steroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen are not safe to use in pregnancy. They may cause miscarriage in the early stages, or induce early labour, and may interfere with kidney function.
Aspirin is not recommended for pain relief as it can increase the risk of bleeding. Codeine-based analgesia can cause breathing problems for the baby in the later stages of pregnancy and should only be taken in the early stages under a doctor’s supervision.
Paracetamol is safe but should be taken only if necessary in pregnancy and for the shortest possible time.
If you come down with a cold during your pregnancy, be sure to speak with your pharmacist before taking any over-the-counter medication. Many will contain antihistamines or Codeine, which are not advised in pregnancy.
Paracetamol will help to relieve headaches.
Skin changes and rashes
Many women will experience changes in their skin during pregnancy. Most of these changes are termed ‘physiological’ which means they are entirely normal and associated with being pregnant.
Most of these changes are termed ‘physiological’ which means they are entirely normal and associated with being pregnant.
- hyperpigmentation – a darkening of the nipples and genital area
- Linea Nigra – a dark, sometimes hairy, line which runs from the belly button to the pubic area
- Striae Gravidarum – stretch marks around the abdomen as it expands, usually starting off pink and becoming white or shiny after delivery
- Varicose veins on the legs
Rashes
Pregnant women can also be affected by rashes such as eczema and psoriasis. Your doctor will advise you on whether using steroid or other cream or lotion is advisable and safe.
There are also:
- rashes specific to pregnancy, called specific dermatoses (skin disorders) of pregnancy
- non-specific rashes that could occur at any time
- itching without a rash
These disorders can cause harm to mother and baby, so seek medical advice if you spot skin changes that seem abnormal. Itching without a rash can be normal or abnormal in pregnancy. Advice should be sought if itching occurs, especially if it keeps getting worse.
Itching without a rash can be normal or abnormal in pregnancy. Advice should be sought if itching occurs, especially if it keeps getting worse.
Swollen ankles, feet and fingers
Ankles, feet and fingers often swell a little in pregnancy because your body is holding more water than usual.
You can minimise swelling by:
- avoiding standing for a long time
- wearing comfortable shoes
- putting your feet up as much as you can
- doing foot exercises
If the swelling does not reduce, ask your doctor or midwife to check your blood pressure.
Teeth and gums
Dental treatment is free during pregnancy and for a year after your baby’s birth, so you should make sure you go to your dentist for a check-up. Always tell your dentist that you are pregnant as this may affect your treatment.
During pregnancy, hormonal changes in your body can cause plaque to make your gums more inflamed and they may become swollen and bleed more easily. When your baby is born, your gums should return to normal.
When your baby is born, your gums should return to normal.
Ask your dentist if any new or replacement fillings should be delayed until after the baby is born.
- Dentist
- Health Service dental charges and treatments
Varicose veins
Varicose veins are veins which become swollen. The veins in the legs are most commonly affected.
Tell your doctor if you have varicose veins or if a close relative has ever had a clot or blood clotting disorder.
If you have varicose veins;
- avoid standing for long periods
- try not to sit with your legs crossed
- try not to put on too much weight
- sit with your legs up to ease the discomfort
- try support tights
- sleep with your legs higher than your body
- try antenatal exercises to help your circulation
Vaginal discharge
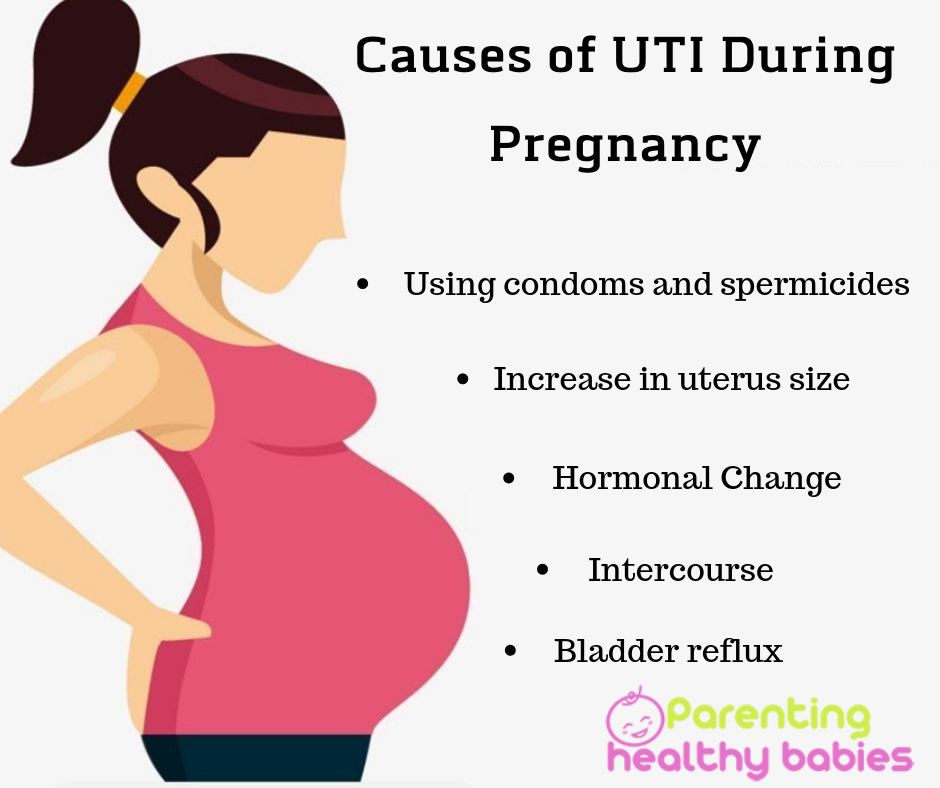
Almost all women have more vaginal discharge in pregnancy. It should be clear and white and should not smell unpleasant. If the discharge is coloured or smells strange, or if you feel itchy or sore, you may have an infection.
If the discharge is coloured or smells strange, or if you feel itchy or sore, you may have an infection.
The most common infection is thrush, which your doctor can treat easily. You can help prevent thrush by wearing loose cotton underwear.
- Thrush
More useful links
- Complications in pregnancy
- Infections during pregnancy
- Travelling while pregnant
Help improve this page - send your feedback
You must have JavaScript enabled to use this form.
What do you want to do?report a problem
leave feedback
ask a question
Report a problemWhich problem did you find on this page? (Tick all that apply)
A link, button or video is not working
There is a spelling mistake
Information is missing, outdated or wrong
I can't find what I'm looking for
Another issue
Messages
Tell us more about the problem you're having with the nidirect website.
Enter your feedback
What is your question about?Choose a topic for your question: - Select -AnglingBenefitsBirth certificatesBlue BadgeCareersCompensation due to a road problemChild MaintenanceCivil partnership certificatesCoronavirus (COVID-19)COVID vaccination certificateCriminal record checks (AccessNI)Death certificatesEducational Maintenance AllowanceEmployment rightsHigh Street Spend Local SchemeMarriage certificatesMotoringnidirect accountPassportsPenalty Charge NoticesPensionsPRONI - historical recordsRates or property valuationProblems with roads and streetsSmartpassMy question is about something else
What to do next
Common Complaints in Pregnancy - Whole Health Library
Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc). 3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
VA » Health Care » Whole Health Library » Tools » Common Complaints in Pregnancy
Menu
Menu
- Whole Health Library
- More Health Care
Quick Links
Common Complaints in Pregnancy
This Whole Health tool focuses on what one might consider as part of a Whole Health approach to a number of pregnancy-related complaints including constipation, gastroesophageal reflux, nausea and vomiting, back pain, and round ligament pain.
Constipation
Constipation is prevalent among pregnant women, starting early in pregnancy and continuing into the postpartum period. The relaxin hormone causes slowing of the smooth muscle of the intestine, thus slowing intestinal transit. Constipation may be aggravated further by the use of prenatal vitamins that contain ferrous sulfate (a commonly used form of iron).
Ways to address constipation include the following:
- Lifestyle measures, such as increasing exercise, as well as increasing fluid and fiber intake, are a good start.
- Beet molasses is traditionally used at a dose of 1-2 tablespoons daily, and it may be worth trying.
- Ground flaxseed, prunes, and prune juice may also be added to the diet.
- Magnesium citrate supplementation at a dose of 120-240 mg by mouth, at bedtime, can be titrated so that a woman has one soft bowl movement daily. This is likely safe to use right up to delivery, although data is very limited.[1]
- Commonly used for constipation, senna, aloe, and cascara sagrada should be avoided in pregnancy, due to the risk of dependency and possible uterine-stimulating effects late in pregnancy.

Gastroesophageal Reflux
Reflux and heartburn are experienced frequently by pregnant women, especially as they approach term. In addition to the usual lifestyle advice, one might consider suggesting a few supplements that may be beneficial. Unfortunately, none have been specifically studied for treating pregnancy-related gastroesophageal reflux.
- Chamomile (Matricaria recutita) is traditionally used for dyspepsia and is safe in pregnancy.[2] It can be consumed as a tea and is noted to have sedative properties.
- Marshmallow root (Althaea officinalis) is an herb which contains mucilage polysaccharides known to coat the esophagus and protect it from irritation.[3] To prepare it, patients should steep one-half to one ounce of dried herb in 1 quart of hot water for 30 minutes and drink as a tea.
- Papaya enzyme and probiotics are also reported by the midwifery community to be helpful, but there has not been any research into their use for pregnancy-related dyspepsia.

- Deglycyrrhizinated licorice (DGL) is a safe alternative to over-the-counter antacids. Women may chew 1-2 tablets prior to each meal. Licorice that has not been deglycyrrhizinated should be avoided by pregnant women.
Nausea and Vomiting in Pregnancy
Nausea and vomiting in early pregnancy, commonly called morning sickness, is often one of the first complaints prenatal patients experience. There are many options in treating the patient with morning sickness.[4]
- First-line therapy should be good hydration and the consumption of small, frequent meals. Increasing the protein content of meals may be helpful for some women, although this has not been studied.
- Crackers or bread at the bedside for eating prior to rising may be helpful for morning symptoms.
- Peppermint tea can be added to the diet for nausea, but it may exacerbate constipation and heartburn.
- Acupuncture is a safe and effective option as well, for women who can afford it.
 [5]
[5] - Ginger has been studied and found effective for morning sickness.[6] Ginger extract can be dosed at 125 mg four times daily.[7] Traditionally, ginger has been used most frequently in the powdered form for nausea in the powdered form. Powdered ginger should be dosed at 250 mg four times daily.[7] Two grams per day is considered a safe upper limit for consumption in pregnancy.[8] Women must take into account the amount of ginger present in real ginger ales, in addition to their supplement, recognizing that many ginger ales are artificially flavored and contain no ginger.
- Vitamin B6 and doxylamine (Unisom) have a long history of use by midwives and physicians for nausea and vomiting in pregnancy. The recommended dose of B6 is 2-50 mg every 1 to 8 hours.[9] It is recommended to start with B6, then if not totally effective, to add doxylamine. Patients should be warned that it may cause drowsiness. Some women may choose just to use a dose of 50 mg at bedtime to help with the morning nausea.
 [9]
[9] - Chamomile, spearmint, pomegranate, lemon, and cardamom may also be helpful.[10]
- Studies on psychological interventions have been of poor quality and inconclusive.[11]
Ginger tea can be made by chopping a piece of ginger root the size of the patient’s fifth digit (pinky finger) and then steeping this for 5-10 minutes. Chopping the root activates the therapeutic oils and sipping on the tea can help with both nausea and dehydration.
Round Ligament and Low Back Pain
Round ligament pain, pelvic pain, and low back pain are just two of many musculoskeletal complaints pregnant women present with. There are many nonpharmacological approaches one can consider.
- Prenatal yoga can be very soothing to the pregnant body, and poses (asanas) can often be tailored to specific complaints. Many communities have prenatal yoga classes available.
- Having women tilt the pelvis forward and backward while standing can relieve round ligament discomfort.

- Women can also get on all fours on the floor. They then alternatively arch and relax the back rhythmically to relieve low back pain. This is known as the cat-cow pose sequence in yoga.
- For a complete reference on exercises in pregnancy, read Essential Exercises for the Childbearing Year by Elizabeth Noble.[12]
- Prenatal massage is relaxing and can relieve muscular tension and spasm. One should guide patients to massage therapists specifically trained to work with pregnant women, since certain massage points may stimulate uterine contractions.
- Topical herbs that are safe for use during massage include camphor, cajeput oil, wintergreen oil, and eucalyptol. Women can purchase these for their own use at home or have a therapist incorporate them into the massage of painful areas. There are some essential oils which should not be used in pregnancy. Women should consult an experienced practitioner prior to using other essential oils.
- Osteopathic manipulative treatment can be effective for pelvic and low back pain.
 [13][14] Women should see out an experienced practitioner.
[13][14] Women should see out an experienced practitioner. - Acupuncture, exercise, Craniosacral Therapy, and pelvic belts can also be effective for low back and pelvic pain.[14][15]
- Prenatal Physical Therapy can play a role in the prevention of pelvic and low back pain[16][17]
Author(s)
“Common Complaints in Pregnancy” was written by Jill Mallory, MD (2014, updated 2020).
References
- Vutyavanich T, Wongtra-ngan S, Ruangsri R. Pyridoxine for nausea and vomiting of pregnancy: a randomized, double-blind, placebo-controlled trial. Am J Obstet Gynecol. 1995;173(3 Pt 1):881-884. ↩
- Madisch A, Holtmann G, Mayr G, Vinson B, Hotz J. Treatment of functional dyspepsia with a herbal preparation. A double-blind, randomized, placebo-controlled, multicenter trial. Digestion. 2004;69(1):45-52. ↩
- Basch E, Ulbricht C, Hammerness P, Vora M. Marshmallow (Althaea officinalis L.
 ) monograph. J Herb Pharmacother. 2003;3(3):71-81. ↩
) monograph. J Herb Pharmacother. 2003;3(3):71-81. ↩ - DiGaetano A. Nausea and Vomiting in Pregnancy. In: Rakel D, ed. Integrative Medicine. Philadelphia, PA: Elsevier Saunders; 2007. ↩
- Sridharan K, Sivaramakrishnan G. Interventions for treating nausea and vomiting in pregnancy: a network meta-analysis and trial sequential analysis of randomized clinical trials. Expert Rev Clin Pharmacol. 2018;11(11):1143-1150. ↩
- McParlin C, O’Donnell A, Robson SC, et al. Treatments for hyperemesis gravidarum and nausea and vomiting in pregnancy: a systematic review. JAMA. 2016;316(13):1392-1401. ↩
- Portnoi G, Chng LA, Karimi-Tabesh L, Koren G, Tan MP, Einarson A. Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. Am J Obstet Gynecol. 2003;189(5):1374-1377. ↩
- Stanisiere J, Mousset PY, Lafay S.
 How safe is ginger rhizome for decreasing nausea and vomiting in women during early pregnancy? Foods (Basel, Switzerland). 2018;7(4). ↩
How safe is ginger rhizome for decreasing nausea and vomiting in women during early pregnancy? Foods (Basel, Switzerland). 2018;7(4). ↩ - O’Donnell A, McParlin C, Robson SC, et al. Treatments for hyperemesis gravidarum and nausea and vomiting in pregnancy: a systematic review and economic assessment. Health Technol Assess. 2016;20(74):1-268. ↩
- Khorasani F, Aryan H, Sobhi A, et al. A systematic review of the efficacy of alternative medicine in the treatment of nausea and vomiting of pregnancy. J Obstet Gynaecol. 2020;40(1):10-19. ↩
- Emami-Sahebi A, Elyasi F, Yazdani-Charati J, Shahhosseini Z. Psychological interventions for nausea and vomiting of pregnancy: A systematic review. Taiwan J Obstet Gynecol. 2018;57(5):644-649. ↩
- Noble E, Artal Mittelmark R, Keith LG. Essential Exercises for the Childbearing Year: A Guide to Health and Comfort Before and After Your Baby is Born.
 Harwich: New Life Images; 2003. ↩
Harwich: New Life Images; 2003. ↩ - Franke H, Franke JD, Belz S, Fryer G. Osteopathic manipulative treatment for low back and pelvic girdle pain during and after pregnancy: a systematic review and meta-analysis. J Bodyw Mov Ther. 2017;21(4):752-762. ↩
- Liddle SD, Pennick V. Interventions for preventing and treating low-back and pelvic pain during pregnancy. Cochrane Database Syst Rev. 2015(9):Cd001139. ↩
- Gutke A, Betten C, Degerskar K, Pousette S, Olsen MF. Treatments for pregnancy-related lumbopelvic pain: a systematic review of physiotherapy modalities. Acta Obstet Gynecol Scand. 2015;94(11):1156-1167. ↩
- Bergamo TR, Latorraca COC, Pachito DV, Martimbianco ALC, Riera R. Findings and methodological quality of systematic reviews focusing on acupuncture for pregnancy-related acute conditions. Acupunct Med. 2018;36(3):146-152. ↩
- </codeVan Kampen M, Devoogdt N, De Groef A, Gielen A, Geraerts I.
 The efficacy of physiotherapy for the prevention and treatment of prenatal symptoms: a systematic review. Int Urogynecol J. 2015;26(11):1575-1586. ↩
The efficacy of physiotherapy for the prevention and treatment of prenatal symptoms: a systematic review. Int Urogynecol J. 2015;26(11):1575-1586. ↩
sections
- Pregnancy against the background of diseases
- Pregnancy
- Ectopic pregnancy
- Pregnancy Issues
- Where and how to give birth
- Decree 9000
- 9000 9000
- Artificial artistic artistic artistic artistic artistic artificial artistic artificial artistic artificial artificial artificial artificial artificial artificial fertilization
- Pregnancy calendar
- Caesarean section
- Breastfeeding
- Beauty and pregnancy
- Courses for pregnant women
- Medicines and pregnancy
- Miscarriage
- Non-traditional childbirth
- Labor pain relief
- Lifestyle
- Ovulation.
 Conception
Conception - Pregnancy complications
- Corn complications
- Pregnancy planning
- Buying for mom and baby
- after giving birth
- Premetic Pregnancy
- Child Born ,0005 Typical complaints of pregnant women
- Physiology of pregnancy
- Physiology of childbirth
006
Preeclampsia
Pregnancy in many women is accompanied by nausea, swelling and headache. In the early stages, this is most often normal and harmless, but in the third trimester the same symptoms can occur as a precursor to preeclampsia. This is a complication of pregnancy that threatens the health and life of both the woman and the baby. To reduce the risks associated with preeclampsia, it is important to recognize it as early as possible. To do this, obstetricians-gynecologists prescribe urine tests to all pregnant women and ask them to control blood pressure. About how to notice in time and how to treat preeclampsia - in our article.
Common complaints during pregnancy
Everyone knows that pregnancy is not a disease, but one of the normal physiological conditions of a woman.
Back pain during pregnancy
Pregnancy is a special period in a woman's life. He gives her a lot of pleasant sensations - the cherished two strips on the test, the first movements in the stomach, congratulations from loved ones. But the joy of waiting for a meeting with the baby can be overshadowed by a variety of unpleasant symptoms. One of them is back pain. It can appear at different times, but most often back problems are especially noticeable in the third trimester, when the fetus is actively gaining weight. Of course, not all pregnant women suffer from acute pain in the back, but every expectant mother should know the causes of pain and how to deal with them if they suddenly begin.
Early toxicosis of pregnant women
The most important period of pregnancy is the first trimester, when all organs and systems of the child are laid and formed.
Toxicosis
Toxicosis sometimes acts as an early diagnostic test and tells a woman that she will soon become a mother. This condition occurs in many pregnant women, but it does not always take on dangerous forms. We will tell you what to do, how to eat to cope with nausea and when to seek help from a doctor.
Preeclampsia (late toxicosis of pregnant women)
Too rapid weight gain may indicate preeclampsia (late toxicosis), especially if edema appears, so it is necessary to inform the doctor about this.
Uterine hypertonicity
Uterine hypertonicity is not an independent disease, it is only a sign of trouble in a woman's body, which cannot be ignored, as it indicates the threat of spontaneous abortion.
Constipation during pregnancy
Two thirds of women complain of constipation during pregnancy and one in three complain of constipation after childbirth.
Increased vaginal discharge
Almost all women are concerned about increased vaginal discharge during pregnancy. This is an absolutely normal phenomenon associated with hormonal changes in the body.
This is an absolutely normal phenomenon associated with hormonal changes in the body.
Convulsions in expectant mothers
Convulsions in pregnant women are not uncommon. Should I be scared or worried?
Thrush during pregnancy
During pregnancy, a woman is usually concerned about increased vaginal discharge. If the discharge is white, curdled, accompanied by burning and itching, then most likely it is thrush.
Insomnia during pregnancy
Large belly, baby movements, frequent urination prevent many pregnant women from getting a good night's sleep. Someone has trouble falling asleep, and someone wakes up in the middle of the night and then can't fall back asleep.
Why does the stomach pull in the early stages of pregnancy?
Why does the stomach pull in the early stages of pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Abdominal pain during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Discomfort in the lower abdomen is rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention from the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy can be:
- "obstetrical";
- "non-obstetric".
Pain associated with pregnancy may be associated with the development of:
- physiological changes during pregnancy;
- threatened miscarriage;
- missed pregnancy;
- ectopic pregnancy.
Pain not related to pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.
Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- sprains and muscles associated with uterine growth.
Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good when menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all.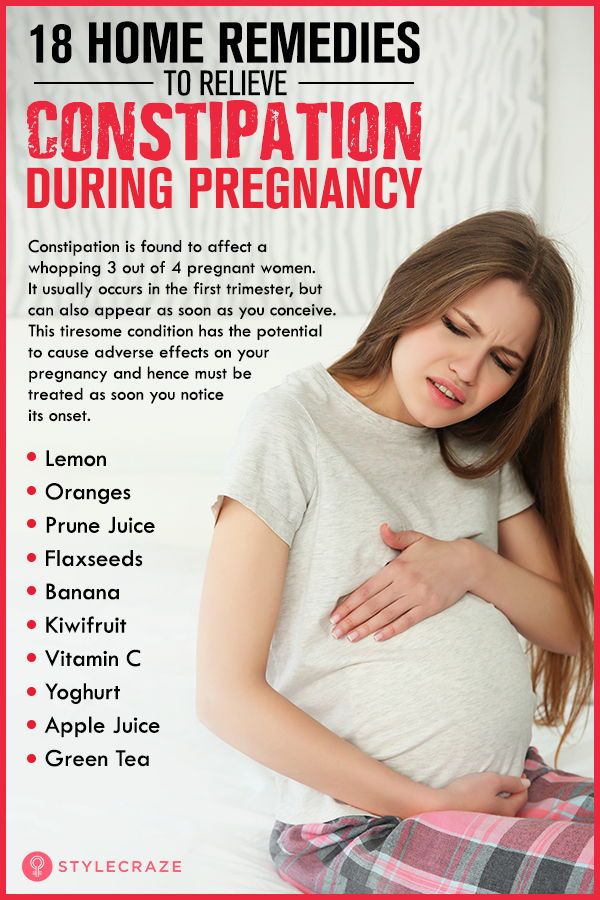 Each woman is individual.
Each woman is individual.
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes. The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the insertion of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Among the reasons that may cause a miscarriage may be:
- severe physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from threats of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- Aching or drawing pains in the small of the back or sacrum.

- bloody discharge from the genital tract.
If you have pain in the lower abdomen, you should consult a doctor, as a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance must be called if:
- pain in the lower abdomen increases;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.
Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.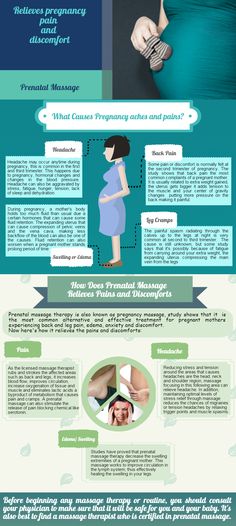
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Illegal pregnancy
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death. Most often, miscarriage occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery. In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Cystitis, due to the anatomical features of a woman, can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.