Cold sore breakout
Cold sore symptoms & treatments - Illnesses & conditions
Cold sores usually clear up without treatment within 7 to 10 days. Antiviral tablets or cream can be used to ease your symptoms and speed up the healing time.
If you develop a cold sore, some general advice to follow includes:
- drink plenty of fluids to avoid dehydration
- avoid acidic or salty foods and eat cool, soft foods
- if brushing your teeth is painful, use an antiseptic mouthwash
- dab creams on to sores rather than rubbing them in
- wash your hands using soap and water before and after applying cold sore creams
- avoid touching your cold sores, other than to apply cream, and don't share your cold sore cream with others
Antiviral creams and tablets
Antiviral creams such as aciclovir or penciclovir (also known as Fenistil®) may speed up the healing time of a recurrent cold sore infection if used correctly.
Cold sore creams are widely available over the counter from pharmacies without a prescription.
They're only effective if you apply them as soon as the first signs of a cold sore appear, when the herpes simplex virus is spreading and replicating. Using an antiviral cream after this initial period is unlikely to have much effect.
If you have frequently recurring bouts of cold sores, use antiviral medication as soon as you feel the tingling sensation that indicates a cold sore is about to develop. You'll need to apply the cream up to five times a day for four to five days.
Antiviral creams can only help to heal a current outbreak of cold sores. They don't get rid of the herpes simplex virus or prevent future outbreaks of cold sores occurring.
Antiviral tablets are generally more effective than creams at treating cold sores, but are usually only prescribed for more severe cases.
Cold sore patches
Cold sore patches that contain a special gel called hydrocolloid are also available. They're an effective treatment for skin wounds and are placed over the cold sore to hide the sore area while it heals.
Non-antiviral treatments
Several non-antiviral creams are also available over the counter from pharmacies without the need for a prescription.
These creams aren't specifically designed to treat cold sores and won't help them heal faster, but they may help ease any pain or irritation. Ask your pharmacist to recommend a suitable treatment for you.
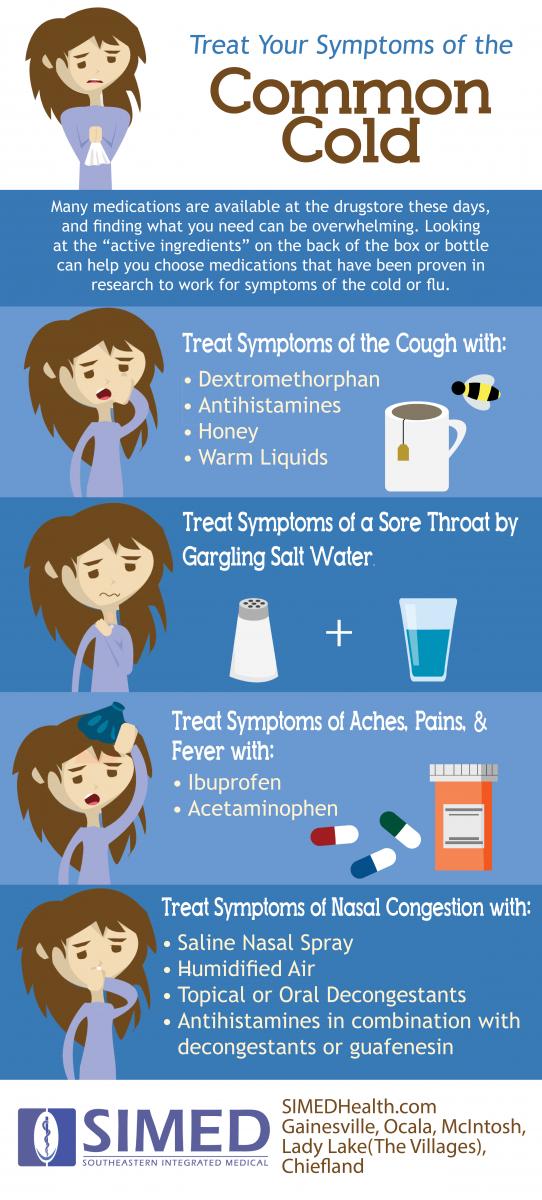
Pain can also be treated with painkillers such as ibuprofen or paracetamol – both are available in liquid form for young children.
However, don't take ibuprofen if you have asthma or stomach ulcers, or you've had them in the past.
Children under the age of 16 shouldn't be given aspirin.
Speak to your pharmacist if you have cold sores and you're pregnant.
Treating complications
If your cold sores are particularly severe or your immune system is damaged – for example, if you have HIV or you're having chemotherapy treatment – you may be at risk of developing serious complications.
For example, your risk of developing encephalitis or the infection spreading to other parts of your body, such as your eyes, is increased.
Speak to your GP if you're at risk. They may prescribe antiviral tablets and refer you for specialist treatment.
The type of treatment recommended will depend on the severity of your cold sore symptoms and the complication that's causing problems.
For example, if you develop herpetic keratoconjunctivitis – a secondary eye infection – you may need to see an ophthalmologist, a specialist eye doctor.
Gingivostomatitis
Visit your pharmacist if you or your child develops swollen, painful gums (gingivostomatitis) as a result of the primary herpes simplex infection. They'll be able to suggest treatments to help ease your symptoms.
If the infection is painful, your pharmacist may suggest using a preparation that contains benzydamine, which is available as an oral rinse or oral spray, to help relieve any pain in your mouth or throat.
Brushing your teeth may also be painful because of the swelling of your gums. Your pharmacist may suggest using an antiseptic mouthwash. This helps prevent secondary infections and will also control a build-up of plaque if you can't brush your teeth effectively.
This helps prevent secondary infections and will also control a build-up of plaque if you can't brush your teeth effectively.
As with the treatment of cold sores, any pain or fever can be treated using ibuprofen or paracetamol.
In rare cases of gingivostomatitis, it's possible for your lips to become stuck together in places. Using a lip barrier cream available from your local pharmacist will help prevent this.
Dehydration
If you or your child has gingivostomatitis, it's important to drink plenty of fluids to avoid becoming dehydrated. Young children are particularly at risk as they may refuse to eat or drink because of the pain in their mouth.
It's important to watch out for signs of dehydration, such as:
- headaches
- tiredness
- irritability
- lightheadedness
- low urine output
Most cases of gingivostomatitis get better in 7 to 14 days, although it may take up to three weeks for the sores to heal completely.
Specialist treatment
If you or your child still has symptoms of gingivostomatitis after two weeks or the infection is severe your pharmacist may advise you to contact your GP, who may refer you for specialist treatment.
Specialist referral may also be needed for gingivostomatitis if you're pregnant or have a weakened immune system.
Visit your GP if you have a newborn baby who develops gingivostomatitis, as they may also need to be referred for specialist treatment.
Cold sore - Symptoms and causes
Overview
Cold sore
Cold sore
Cold sores, often called fever blisters, are clustered, small, fluid-filled blisters. You may feel a tingling on your lip before a small, hard, painful spot appears (top). In a day or two, blisters form, which later break and ooze (bottom). Healing usually occurs in two to three weeks without scarring.
Cold sores — also called fever blisters — are a common viral infection. They are tiny, fluid-filled blisters on and around your lips. These blisters are often grouped together in patches. After the blisters break, a scab forms that can last several days. Cold sores usually heal in two to three weeks without leaving a scar.
They are tiny, fluid-filled blisters on and around your lips. These blisters are often grouped together in patches. After the blisters break, a scab forms that can last several days. Cold sores usually heal in two to three weeks without leaving a scar.
Cold sores spread from person to person by close contact, such as kissing. They're usually caused by herpes simplex virus type 1 (HSV-1), and less commonly herpes simplex virus type 2 (HSV-2). Both of these viruses can affect your mouth or genitals and can be spread by oral sex. Cold sores are contagious even if you don't see the sores.
There's no cure for cold sores, but treatment can help manage outbreaks. Prescription antiviral pills or creams can help sores heal more quickly. And they may reduce the frequency, length and severity of future outbreaks.
Products & Services
- Book: Mayo Clinic Book of Home Remedies
Symptoms
A cold sore usually passes through several stages:
- Tingling and itching.
 Many people feel itching, burning or tingling around the lips for a day or so before a small, hard, painful spot appears and blisters erupt.
Many people feel itching, burning or tingling around the lips for a day or so before a small, hard, painful spot appears and blisters erupt. - Blisters. Small fluid-filled blisters typically erupt along the border of your lips. Sometimes they appear around the nose or cheeks or inside the mouth.
- Oozing and crusting. The small blisters may merge and then burst, leaving shallow open sores that ooze and crust over.
Signs and symptoms vary, depending on whether this is your first outbreak or a recurrence. The first time you have a cold sore, symptoms may not start for up to 20 days after you were first exposed to the virus. The sores can last several days, and the blisters can take two to three weeks to heal completely. Recurrences typically appear at the same spot each time and tend to be less severe than the first outbreak.
In a first-time outbreak, you also might experience:
- Fever
- Painful gums
- Sore throat
- Headache
- Muscle aches
- Swollen lymph nodes
Children under 5 years old may have cold sores inside their mouths and the lesions are commonly mistaken for canker sores. Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
When to see a doctor
Cold sores generally clear up without treatment. See your doctor if:
- You have a weakened immune system
- The cold sores don't heal within two weeks
- Symptoms are severe
- You have frequent recurrences of cold sores
- You experience irritation in your eyes
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Cold sores are caused by certain strains of the herpes simplex virus (HSV). HSV-1 usually causes cold sores. HSV-2 is usually responsible for genital herpes. But either type can spread to the face or genitals through close contact, such as kissing or oral sex. Shared eating utensils, razors and towels might also spread HSV-1.
Cold sores are most contagious when you have oozing blisters because the virus easily spreads through contact with infected body fluids. But you can spread the virus even if you don't have blisters. Many people who are infected with the virus that causes cold sores never develop signs and symptoms.
Once you've had an episode of herpes infection, the virus lies dormant in nerve cells in your skin and may emerge as another cold sore at the same place as before. Recurrence may be triggered by:
- Viral infection or fever
- Hormonal changes, such as those related to menstruation
- Stress
- Fatigue
- Exposure to sunlight and wind
- Changes in the immune system
- Injury to the skin
Video: 3 things you didn't know about cold sores
Cold sores on the lips can be embarrassing and tough to hide. But, turns out, you might not have a reason to be embarrassed.
"About 70-plus percent of the U. S. population has been infected with herpes simplex 1. Now, a very small percentage of those people will actually develop cold sores."
S. population has been infected with herpes simplex 1. Now, a very small percentage of those people will actually develop cold sores."
Dr. Pritish Tosh, an infectious diseases specialist at Mayo Clinic, says, genetics determines whether a person will develop cold sores.
"A proportion of the population, they don't quite have the right immunologic genes and things like that and so they're not able to handle the virus as well as other people in the population."
The problem is people can spread the herpes virus whether they develop cold sores or not. Herpes virus spreads through physical contact like kissing, sharing a toothbrush — even sharing a drinking glass — or through sexual contact.
"Since the number of people who are infected but don't have symptoms vastly outnumber the people who are infected and have symptoms, most new transmissions occur from people who have no idea that they are infected."
For the Mayo Clinic News Network, I'm Ian Roth.
Risk factors
Almost everyone is at risk of cold sores. Most adults carry the virus that causes cold sores, even if they've never had symptoms.
Most adults carry the virus that causes cold sores, even if they've never had symptoms.
You're most at risk of complications from the virus if you have a weakened immune system from conditions and treatments such as:
- HIV/AIDS
- Atopic dermatitis (eczema)
- Cancer chemotherapy
- Anti-rejection drugs for organ transplants
Complications
In some people, the virus that causes cold sores can cause problems in other areas of the body, including:
- Fingertips. Both HSV-1 and HSV-2 can be spread to the fingers. This type of infection is often referred to as herpes whitlow. Children who suck their thumbs may transfer the infection from their mouths to their thumbs.
- Eyes. The virus can sometimes cause eye infection.
 Repeated infections can cause scarring and injury, which may lead to vision problems or loss of vision.
Repeated infections can cause scarring and injury, which may lead to vision problems or loss of vision. - Widespread areas of skin. People who have a skin condition called atopic dermatitis (eczema) are at higher risk of cold sores spreading all across their bodies. This can become a medical emergency.
Prevention
Your doctor may prescribe an antiviral medication for you to take on a regular basis if you develop cold sores more than nine times a year or if you're at high risk of serious complications. If sunlight seems to trigger your recurrences, apply sunblock to the spot where the cold sore tends to erupt. Or talk with your doctor about using an oral antiviral drug as a preventive if you expect to be doing an activity that tends to trigger your condition, such as intense sunlight exposure.
To help avoid spreading cold sores to other people or to other parts of your body, you might try some of the following precautions:
- Avoid kissing and skin contact with people while blisters are present.
 The virus spreads most easily when the blisters leak fluid.
The virus spreads most easily when the blisters leak fluid. - Avoid sharing items. Utensils, towels, lip balm and other personal items can spread the virus when blisters are present.
- Keep your hands clean. When you have a cold sore, wash your hands carefully before touching yourself and other people, especially babies.
By Mayo Clinic Staff
Types of herpes, causes, symptoms, treatment — Doctor Bogolyubov Medical Center Network
Herpes is a viral disease that manifests itself in characteristic rashes in the form of vesicles with liquid. The virus penetrates through the mucous membranes and remains in the body for life. It is activated when immunity is weakened, hypothermia and other adverse factors. Herpes affects the mucous membranes of the mouth and genitals, skin, eyes, immune system and nerve fibers. A dermatologist directs for tests to detect the virus, and after confirming the diagnosis, he will tell you how to get rid of herpes.
Types of herpes
More than 100 types of herpes viruses are isolated, while only 8 of them affect humans, causing different diseases and symptoms.
Herpes simplex
Herpes simplex virus type 1 is the most common and highly contagious. Usually infection occurs in childhood through common household items and toys. HSV-1 causes the appearance of characteristic blisters on the lips and skin of the nasolabial triangle. First, small rashes grow to a noticeable size, after which the bubble bursts and the liquid comes out. A crust forms at this place - after 3-5 days it disappears on its own.
In addition to blisters, herpes on the lips is accompanied by symptoms of intoxication:
- high body temperature;
- general weakness and drowsiness;
- headache, muscle and joint pain.
The disease lasts for a week, after which the symptoms disappear, and the wounds on the lips heal without a trace. The virus goes into a dormant state and "lives" in the cells of the nervous tissue until the next episode of exacerbation.
Diagnosis can only be made by symptoms, but laboratory diagnostics are sometimes used:
- enzyme immunoassay method: detection of IgG antibodies in blood;
- detection of virus DNA in blood by PCR.
There is no permanent cure for HSV type 1. During relapses, drugs against the virus based on acyclovir are taken and ointments are applied to the elements of the lesion - they will stop the spread of the process and accelerate healing.
Genital
Genital herpes causes HSV-2. It is sexually transmitted and is accompanied by the appearance of painful blisters in the genital area and anus. Penetrating deep into the body through microcracks in the mucous membrane, the virus reaches the nerve ganglia and remains in them for life.
In addition to blisters, genital herpes is accompanied by the following symptoms:
- pain, burning and redness of the skin in the affected area;
- fever;
- pain in the head and muscles;
- sores in place of vesicles;
- discomfort during urination.
The illness lasts 1-2 weeks. Several tests are used to make a diagnosis:
- detection of IgG antibodies in blood or smears;
- isolation of pathogen DNA by polymerase chain reaction (PCR).
It is impossible to completely cure HSV-2, as the virus penetrates into the nerve ganglia. At the time of exacerbation, antiviral drugs based on acyclovir and valciclovir are taken in the form of tablets and ointments - they will help alleviate unpleasant symptoms, speed up recovery and prolong remission.
Herpes type 3
The herpes virus type 3 is called Varicella Zoster. It causes chicken pox and shingles. As a rule, after infection in childhood, chicken pox develops. It is transmitted from a sick person by airborne droplets, penetrates through the mucous membrane of the nose and mouth. The first symptoms appear 10-20 days after infection - the temperature rises, bubbles with liquid appear on the body. Gradually, they dry out with the formation of crusts and heal within 2 weeks.
After chicken pox, the type 3 virus does not die, but settles in the nerve ganglia. Under the influence of stress, hypothermia or other adverse factors, the virus reactivates and causes shingles. Bubbles appear on the patient's body along the nerve fibers. General well-being suffers - the patient experiences severe pain and problems with sleep.
Chickenpox is treated symptomatically. With herpes zoster, it is important to start treatment with antiviral drugs as soon as possible in order to suppress the spread of the virus and further damage to the nerve fibers.
Epstein-Barr virus
Herpesvirus type 4 provokes infectious mononucleosis. The causative agent penetrates through the mucous membrane of the mouth and affects the cells of the immune system, due to which the tonsils and lymph nodes increase.
Other symptoms of mononucleosis:
- high body temperature;
- pain in muscles, joints, head and throat;
- small rashes on the oral mucosa;
- general weakness and drowsiness;
- enlargement of the spleen.

Epstein-Barr virus is diagnosed using a blood test for the DNA of the pathogen by PCR. There is no specific treatment, therefore, antipyretic and pain medications are taken to eliminate symptoms. In severe cases, anti-herpetic drugs are prescribed.
Cytomegalovirus
Herpes type 5 is the causative agent of cytomegalovirus disease. The virus is transmitted through body fluids - saliva, blood, breast milk. Cytomegalovirus usually lies dormant in the body and is only activated when the immune system is weakened. Symptoms of a primary infection with cytomegalovirus are similar to a common viral infection - weakness, sore throat, fever, body aches.
Blood tests are used to diagnose cytomegalovirus infection. Specific IgG and IgM antibodies are detected, as well as PCR to detect viral DNA. There is no cure - cytomegalovirus remains in the body for life.
Herpes 6, 7, 8 types
Herpes virus type 6 is considered one of the provocateurs of the development of multiple sclerosis - a serious autoimmune disease that affects the central nervous system.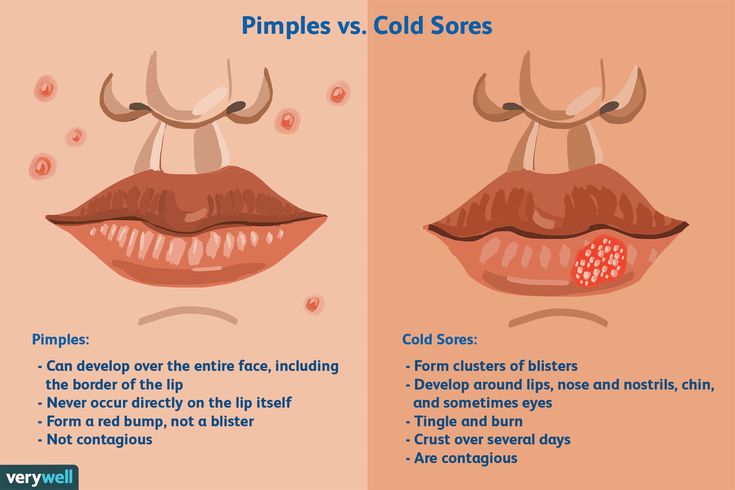 The treatment of type 6 herpes is complex - the patient is selected drugs depending on the clinical picture, which will help stop the development of the disease.
The treatment of type 6 herpes is complex - the patient is selected drugs depending on the clinical picture, which will help stop the development of the disease.
Herpes type 7 is usually transmitted with virus 6 and causes chronic fatigue syndrome. Herpes type 8 after entering the body can be in a “sleeping” state for a long time. Under adverse conditions, it can provoke Kaposi's sarcoma - a disease in which multiple malignant neoplasms occur on the skin.
Complications
In weakened immunocompromised people, the virus can attack the nervous system with the development of herpes encephalitis and meningoencephalitis. Contact with the pathogen on the conjunctiva causes ophthalmic herpes - eye damage with subsequent visual impairment. With improper treatment, a bacterial infection can join, causing suppuration of the blisters. Herpes is especially dangerous during pregnancy - upon initial contact with the virus, there is a risk of intrauterine infection of the fetus and the development of congenital herpes infection.
Herpes in children
In children, types 1 and 3 of the virus are most common, provoking rashes on the lips and chickenpox. As a rule, children carry the disease easily and remain carriers of the virus forever. Lifelong immunity is formed to chickenpox, and labial herpes can occur again when immunity is weakened.
In addition, viruses of types 6 and 7 provoke roseola in children - a sudden exanthema or a three-day fever. The disease begins suddenly with a rise in temperature to 40 ℃, which subsides for 3-4 days, after which a pink rash appears.
Measures to prevent herpes
To prevent infection or recurrence of the disease, follow the recommendations:
- maintain personal hygiene;
- strengthen immunity - eat right, temper, give up bad habits;
- exclude the use of common household items with a sick person;
- to diagnose antibodies to herpes in women during pregnancy and, in their absence, strictly limit contact with sick people;
- use contraceptives;
- vaccinate against varicella.

Where can I get tested for herpes?
- Opportunity to take tests without queues, at the nearest office of the medical center "Doctor Bogolyubov".
- Quick and painless blood sampling for both adults and children.
- Readiness of results in a short time.
- A wide range of services - you can donate blood at a time to study several indicators.
How to cure herpes?
Antiviral and immunomodulatory drugs are used to treat herpes in adults. It is important to start taking drugs as soon as possible so that the disease stops its development at an early stage. Local preparations are used - gels and ointments that need to be applied to the affected areas of the skin. Additionally, painkillers, antihistamines and anti-inflammatory drugs are used to eliminate unpleasant symptoms and fever. After recovery, the doctor may prescribe vitamin preparations to maintain immunity.
What can cause herpes?
Relapses of herpes can cause hypothermia, stress, immunodeficiencies, trauma to the skin and mucous membranes, lack of sleep and lack of vitamins. In addition, rashes on the lips are more likely to develop in smokers.
In addition, rashes on the lips are more likely to develop in smokers.
How long does it take to treat herpes on the lips?
On average, the treatment of labial herpes lasts 7-10 days - during this time, the crusts fall off, and the wounds heal without a trace.
How long does herpes on the body take to heal?
Chickenpox lasts up to 10 days, after which the rash heals quickly. Herpes in children is often mild and does not require complex drug therapy. Herpes zoster requires long-term treatment - up to 4 weeks.
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find a country »
- A
- Б
- В
- Г
- Д
- Е
- Ё
- Ж
- З
- И
- Й
- К
- Л
- М
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- Э
- Ю
- Я
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/
- Herpes simplex virus
Key facts
- There are two types of herpes simplex virus (HSV): HSV-1 and HSV-2.

- HSV-1 is transmitted primarily by oral contact and causes oral herpes (which may present as "fever on the lips"), but can also cause genital herpes.
- HSV-2 is a sexually transmitted infection that causes genital herpes.
- An estimated 3.7 billion people under the age of 50 (67%) worldwide are infected with HSV-1.
- An estimated 491 million people aged 15 to 49 (13%) worldwide are infected with HSV-2.
- Most HSV infections are asymptomatic, but herpes can present with symptoms such as painful blisters or sores that may recur over time.
- HSV-2 infection increases the risk of HIV infection and transmission.
General information
Infection with the herpes simplex virus (HSV), commonly referred to as herpes, is widespread throughout the world.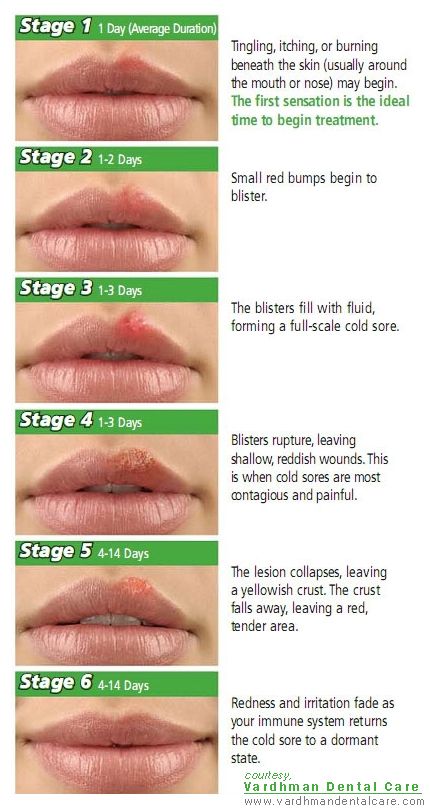 HSV type 1 (HSV-1) is usually transmitted by oral contact, causing an infection in or around the mouth (oral herpes), but can also cause genital herpes. HSV-2 is transmitted mainly through sexual contact and causes genital herpes.
HSV type 1 (HSV-1) is usually transmitted by oral contact, causing an infection in or around the mouth (oral herpes), but can also cause genital herpes. HSV-2 is transmitted mainly through sexual contact and causes genital herpes.
Both oral herpes and genital herpes are mostly asymptomatic or go unrecognized, but can cause symptoms such as painful blisters or sores at the site of infection, in both mild and severe forms. The infection is present in the body for life, and its symptoms may recur after many years. There are drugs that reduce the severity and frequency of symptoms but do not cure the infection.
Recurrent symptoms of oral and genital herpes can cause significant discomfort. The presence of genital herpes can also lead to stigmatization and negatively affect sexual life. However, over time, most carriers both types of herpes adapt to life with infection.
Magnitude of the problem
In 2016 (latest year for which estimates are available), 3.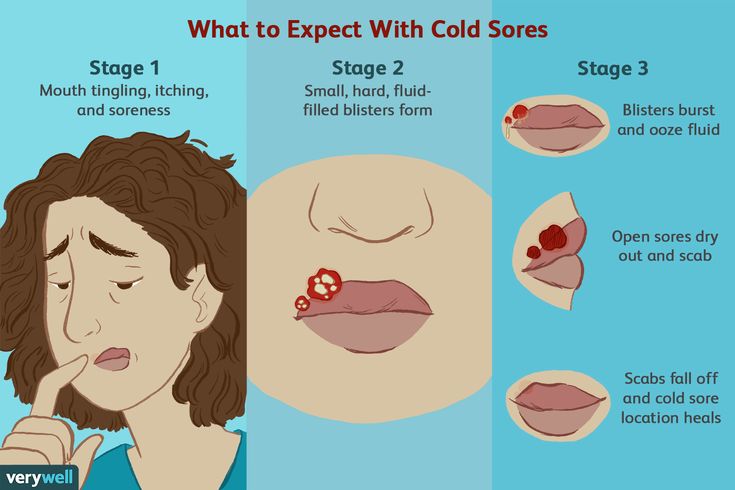 7 billion people under the age of 50, or 67% of the population, were infected with HSV-1 (in the form of oral or genital herpes). In most cases, HSV-1 infection occurs in childhood.
7 billion people under the age of 50, or 67% of the population, were infected with HSV-1 (in the form of oral or genital herpes). In most cases, HSV-1 infection occurs in childhood.
The number of people with HSV-2 genital herpes in 2016 was estimated at 491 million people aged 15–49 years (13% of the global population). Women are infected with HSV-2 almost twice as often as men, since the infection is more easily transmitted sexually from a man to a woman. The prevalence of this infection increases with age, although the greatest number of new infections occurs among adolescents.
Signs and symptoms
Oral herpes is usually asymptomatic, but may be accompanied by painful blisters or open lesions (sores) in or around the mouth. Before lesions appear, infected individuals often experience tingling, itching, or burning in the mouth. These symptoms may recur periodically, and the frequency of their occurrence varies from person to person.
Genital herpes may be asymptomatic or with mild symptoms that go unrecognized. When symptoms appear, genital herpes is characterized by the formation of one or more blisters or sores in the genital or anal area. areas. In addition, a new infection may present with fever, body aches, and swollen lymph nodes. After the initial episode, which may be severe, symptoms may reappear. For genital herpes caused by HSV-1, frequent relapses are not typical. In the case of HSV-2, recurrence of symptoms occurs frequently. Such relapses, however, are often milder than in the first episode and tend to subside over time.
When symptoms appear, genital herpes is characterized by the formation of one or more blisters or sores in the genital or anal area. areas. In addition, a new infection may present with fever, body aches, and swollen lymph nodes. After the initial episode, which may be severe, symptoms may reappear. For genital herpes caused by HSV-1, frequent relapses are not typical. In the case of HSV-2, recurrence of symptoms occurs frequently. Such relapses, however, are often milder than in the first episode and tend to subside over time.
Transmission
HSV-1 is transmitted primarily through contact with the virus present in lesions, saliva and surfaces in or around the mouth. Through oral-genital contact, HSV-1 can also enter the genital area and cause genital herpes. It can be transmitted through a surface of the mouth or skin that appears normal, but the risk of transmission is highest when active lesions are present. Those already infected with HSV-1 cannot be re-infected, but nonetheless are at risk of HSV-2 infection.
HSV-2 is transmitted primarily through sexual intercourse through contact with genital or anal surfaces, skin, lesions, or fluids of a person infected with the virus. HSV-2 can even be transmitted through the skin, which appears normal, and is often transmitted in the absence of symptoms.
In rare cases, herpes (HSV-1 and HSV-2) can be passed from mother to child during childbirth and lead to neonatal herpes.
Possible complications
HSV-2 and HIV infection
The presence of HSV-2 increases the risk of HIV infection by about three times. In addition, people infected with HIV and HSV-2 are more likely to transmit HIV to others. HSV-2 is one of the most common infections among HIV-infected individuals.
Severe disease
People with weakened immune systems, including those with advanced HIV infection, often have herpes with more severe symptoms and more frequent recurrences. Rare complications of HSV-2 include meningoencephalitis (infection of the head brain) and disseminated infection. Rarely, HSV-1 infection can also lead to more severe complications such as encephalitis (brain infection) or keratitis (eye infection).
Rarely, HSV-1 infection can also lead to more severe complications such as encephalitis (brain infection) or keratitis (eye infection).
Neonatal herpes
Neonatal herpes can develop when a newborn comes into contact with HSV during childbirth. Neonatal herpes is rare, with an estimated 10 out of 100,000 births worldwide. However, this severe condition can lead to persistent neurological disability or death. The greatest risk of neonatal herpes occurs when a woman first becomes infected with HSV late in pregnancy.
Treatment
Antivirals such as acyclovir, famciclovir and valaciclovir are the most effective drugs for people infected with HSV (see WHO recommendations). They help reduce the severity and frequency of symptoms, but do not cure the infection.
Prevention.
Persons with active symptoms of oral herpes should avoid oral contact with other people (including oral sex) and sharing objects that have come into contact with saliva. Individuals with symptoms of genital herpes should refrain from sexual activity during the period of symptoms. Both HSV-1 and HSV-2 are most contagious during the presence of lesions, but can also be transmitted when no symptoms are felt or observed.
Individuals with symptoms of genital herpes should refrain from sexual activity during the period of symptoms. Both HSV-1 and HSV-2 are most contagious during the presence of lesions, but can also be transmitted when no symptoms are felt or observed.
The most effective way to prevent genital herpes and other STIs in sexually active persons is the consistent and correct use of condoms. At the same time, however, HSV infection through contact with unprotected condom sections of the genitals and anal area. Medical male circumcision can provide men with lifelong partial protection against HSV-2, as well as HIV and human papillomavirus (HPV).
Individuals with symptoms suggestive of genital herpes should be offered HIV testing.
Pregnant women with symptoms of genital herpes should inform health care providers. Prevention of HSV-2 infection is especially important for women in late pregnancy, as during this period there is the highest risk development of neonatal herpes.