Cold and flu medications safe for pregnancy
Which Cold & Flu Medication Is Safe to Take During Pregnancy? | UNM Health Blog
By Maria Montoya, MD | February 04, 2022
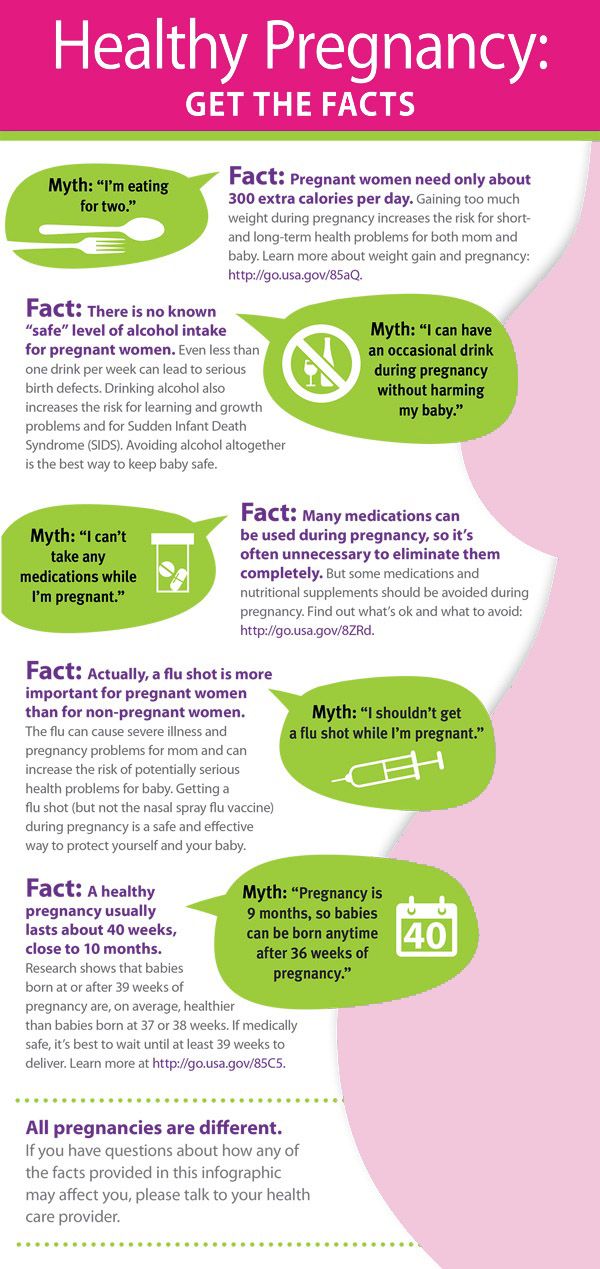
You are pregnant and start feeling sick. Before you reach for that bottle of cold or flu medicine, are you certain it is safe for your baby?
When you are pregnant, your baby will be exposed to everything you are exposed to. This means that when you are sick with a cold or flu your baby will not only be exposed to the cold or flu virus, but also any medication you may take.
Typically, with most viruses, you must wait for your immune system to fight the infection. Over-the-counter medications can help soothe your symptoms while you wait.
However, not all over-the-counter medicines are safe to take during pregnancy. Certain medications may hurt the baby or cause problems for you, such as increasing your blood pressure.
Use this quick list of pregnancy-safe natural cold and flu remedies and over-the-counter medications as a starting point. Remember, read the directions on the package for any medication you might take. It’s also a good idea to talk with your doctor or midwife before taking a cold or flu medication.
Natural, Pregnancy-Safe Remedies
Before you try any medications, there are natural remedies you may find adequate relief from first. Here are a couple of safe, natural remedies to try:
- Gargle warm salt water
- Get as much restful sleep as possible
- Sip honey in hot water
- Stay well hydrated
- Use nasal saline sprays
- Try a humidifier
While not all herbs and supplements are safe in pregnancy. You may be able to safely take:
- Vitamin C
- Zinc
- Manuka Honey
- Elderberry
Talk with your doctor or midwife before taking any supplements or trying at-home remedies or essential oils during pregnancy.
If natural remedies don’t provide enough relief, consider these pregnancy-safe medications.
Pregnancy-Safe Cold & Flu Medication
It is best to avoid taking medications when possible. If you do need to take something, follow the package directions carefully. Talk with your doctor or midwife before taking medication during pregnancy.
These over-the-counter medications are considered safe for most pregnant patients:
- Acetaminophen (Tylenol)
- Safe during the entire pregnancy.
- Take only as needed.
- Try to limit regular exposure.
- Not safe if you are allergic to it or have liver problems.
- Pseudoephedrine (Sudafed)
- Safe in the second and third trimester
- Not safe in the first trimester due to a small risk of abdominal wall birth defects
- Not safe if you have high blood pressure (hypertension) or a history of heart disease
- Chlorpheniramine (Chlor-Trimeton)
- Safe during pregnancy.
- Not safe while breastfeeding.

- Diphenhydramine (Benadryl)
- Safe throughout pregnancy.
Watch out for extra ingredients. Many cold and flu medications treat more symptoms than you may be experiencing. For example, Tylenol Cold Multi-Symptom treats headaches, fever, body aches, cough, chest congestion, stuffy nose, and more. If you just have a stuffy nose, this is more medication than you need.
A word about antibiotics. Some sinus infections are treated with antibiotics. In general, pregnant patients should not take antibiotics unless it is necessary. Make sure your health care provider knows you are pregnant if they prescribe antibiotics.
The dangers of high blood pressure in pregnancy
How to spot symptoms and get help
Read More
Medications to Avoid in Pregnancy
Nonsteroidal anti-inflammatory (NSAID) medications can hurt your developing baby. Do not take NSAIDs such as these when you are pregnant:
Do not take NSAIDs such as these when you are pregnant:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve, Midol)
- Celecoxib (Celebrex)
- Aspirin (Bayer), unless your doctor or midwife prescribes daily low-dose aspirin.
Do not take these medications during pregnancy. These drugs can hurt the developing baby:
- Benzocaine (throat lozenges/throat sprays)
- Codeine (a pain and cough medication)
- Phenylephrine (i.e., Sudafed PE): it not considered safe while pregnant because studies with animals showed adverse effects to the fetus.
When you don’t feel well, the last thing you might want to do is read a medication label. However, it is worth taking a few extra moments to read the label and avoid additional risks. If you’re not sure what medicine is safe to take, call us. We are always here to help you.
To find out whether you or a loved one might benefit from Ob/Gyn care
Call 505-272-2245.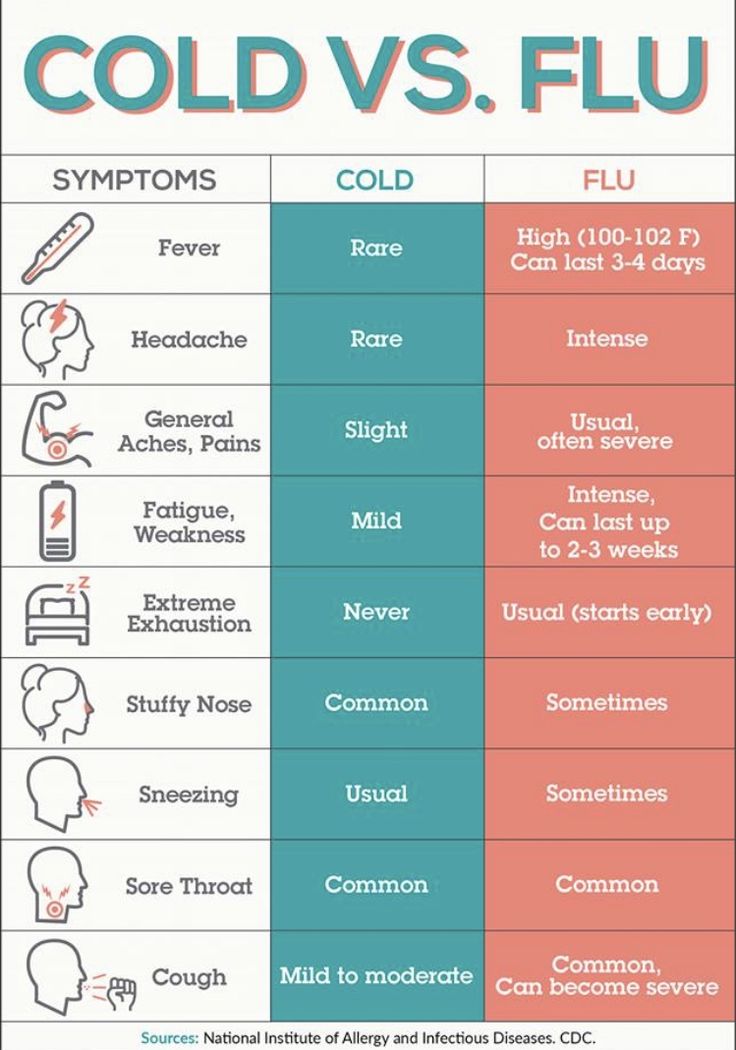
Categories: Women's Health
medicine that's safe for pregnant women?
Mid-Atlantic Women’s Care Obstetrics
When you are pregnant, your immune system doesn’t operate at maximum capacity, which is actually a good thing because it keeps your growing baby protected, and stops your body from thinking the fetus is an intruder. However, this comes with the downside that your body can’t ward off the viruses that cause the common cold quite as effectively. This can leave you vulnerable to the symptoms that come along, including a congested nose, cough, and sore throat.
As we move into cold and flu season, you may find yourself coming down with a cold, and while you can rest assured that your baby isn’t experiencing any of them, you want to get rid of the symptoms quickly and safely. While colds are mostly an uncomfortable annoyance best managed by a little extra rest, fluids, and patience, you may find yourself seeking out cold medications to alleviate your symptoms. We recommend making a call to your OBGYN so they can steer you in the right direction in terms of cold medications that are considered safe during pregnancy. Here are our own recommendations on what to do if you get sick while pregnant.
While colds are mostly an uncomfortable annoyance best managed by a little extra rest, fluids, and patience, you may find yourself seeking out cold medications to alleviate your symptoms. We recommend making a call to your OBGYN so they can steer you in the right direction in terms of cold medications that are considered safe during pregnancy. Here are our own recommendations on what to do if you get sick while pregnant.
Common cold symptoms during pregnancy
Generally, a cold will start with a sore or scratchy throat lasting about a day or two, followed by the gradual onset of other symptoms which may include:
- Sneezing
- Mild fatigue
- A runny, then later stuffy nose
- A dry cough, particularly as the cold is ending which may continue for a week or more after the other symptoms have mostly subsided
- A low-grade fever typically under 100 degrees Fahrenheit
Cold symptoms usually last between 10 to 14 days. However, if your symptoms persist longer than that time frame or seem to progressively worsen, you should talk to your primary care physician so they can ensure it hasn’t turned into something more serious like an infection or the flu.
Is it a cold or the flu?
The best way to tell the difference between a cold and the flu is to take account of the typical symptoms.
- A cold is milder than the flu. Its symptoms come on gradually and typically you only run a low-grade to no fever. It generally starts off with a sore throat that goes away after a day or two, a cold ends with the main symptoms of a runny nose and cough.
- Influenza, commonly called the flu, is more severe and the onset is more sudden than a cold. Symptoms include a high fever (typically 101-104 degrees F or higher), headache, chills, a sore throat that typically worsens by the second or third day, intense muscle soreness, and a general feeling of weakness and fatigue. These symptoms, along with sneezing and a cough, can last a couple of weeks or longer.
What to do if you get a cold while pregnant
Before turning to medicine, there are some effective cold remedies that don’t come from a pharmacy shelf. Here are ways to alleviate symptoms and feel better fast:
Here are ways to alleviate symptoms and feel better fast:
- Keep eating: It’s common to not have much of an appetite when you have a cold but it is important to eat a healthy diet while you are sick and pregnant.
- Rest: While this won’t necessarily shorten the duration of your cold, your body needs rest. Sleeping can prove to be a bit difficult when sick with a cold. Breathe easier by elevating your head with a few pillows. Nasal strips can also help as they gently pull your nasal passages open. They are easy to find, sold over the counter and are drug-free.
- Stay active: If you can, do some light to moderate, pregnancy-safe exercises. It will help your body to fight off the cold faster.
- Drink lots of fluids: Symptoms of colds like sneezing, runny nose, and fever causes your body to lose fluids that are essential to you and your baby. Warm beverages like tea with honey (which helps to suppress a dry cough) or hot soup with broth are soothing for your symptoms and cold water and juices work fine as well.
- Eat foods with vitamin C: Foods like citrus fruits, tomatoes, bell peppers, broccoli, spinach, melon, kiwi, and red cabbage are packed with vitamin C which will help to boost your immune system.
- Get more zinc: Pregnant women should try to get 11-15 milligrams of zinc each day, including the zinc in prenatal vitamins. Foods like turkey, beef, eggs, yogurt, wheat germ, oatmeal, and pork will also help to boost your immune system.
- Use a humidifier: Dry conditions in your home can aggravate your symptoms so using a cold or warm air humidifier at night can really help.
- Use saline nose drops, rinses, and sprays. All of these can help to moisten nasal passages, and they’re unmedicated, so they are safe for use while pregnant. We do recommend avoiding neti pots, however, as they can spread germs.
- Gargle with warm salt water: Gargling with warm salt water can help to ease a scratchy throat and help control a cough.
Medications that are safe for pregnant women to take for a cold
Before reaching for the medications in your medicine cabinet, reach for the phone and call your OBGYN to discuss the recommended remedies you can take for a cold while pregnant. Here are cold medications that are generally safe during pregnancy.
Here are cold medications that are generally safe during pregnancy.
Acetaminophen
Taking acetaminophen like Tylenol can help in the short-term to reduce head and body aches and break a fever.
Cough medicine
Expectorants like Mucinex, cough suppressants like Robitussin, vapor rubs like Vicks VapoRub, and cough drops are all considered safe during pregnancy. But again, make sure to consult your OBGYN about safe dosages.
Nasal sprays
Plain saline drops and sprays are safe and can help to moisturize and clear a stuffy nose. Most steroid-containing nasal sprays are also safe but you should check with your doctor about brands and dosing.
Antihistamines
Benadryl and Claritin are generally safe during pregnancy but, as usual, check with your doctor as some will advise against them during the first trimester.
Medications to avoid during pregnancy
Always check with your doctor or OBGYN before taking any medications – prescription, over-the-counter, or homeopathic – particularly the following.
- Pain relievers and fever reducers like aspirin, ibuprofen, and naproxen can cause pregnancy complications, particularly if taken during the third trimester.
- Decongestants like Sudafed and DayQuil are generally cautioned against after the first trimester and only in a limited amount.
- Avoid non-steroidal nasal sprays containing oxymetazoline.
- Don’t take supplemental vitamins or herbal remedies without medical approval.
Pregnancy and medicines / Obstetrics and gynecology, reproductive medicine / Articles about health / Articles and encyclopedia / madez.ru
We have been actively planning for a baby for a long time, but we never think about the dangers of drugs during pregnancy!
Gynecologist, gynecologist endocrinologist Popova Natalya Vladimirovna will tell you what medicines can be taken during pregnancy, and which ones are categorically not recommended.
One of the most important periods in a woman's life is the period of bearing a child. And in these few months, the expectant mother must do everything in her power to give birth to a healthy baby. But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
And in these few months, the expectant mother must do everything in her power to give birth to a healthy baby. But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
If it is necessary to use any drug during pregnancy, the mother-to-be should remember:
- Any drug during pregnancy (at any stage) can be used only in accordance with the indications and only as prescribed by the attending physician;
- When choosing a medicinal product, preference should be given only to those medicinal products that have proven efficacy;
- Prefer monotherapy, i.e. treatment with only one drug if possible; combined treatment during this period is undesirable;
- Topical treatment is more desirable than systemic (oral, intravenous, intramuscular) administration of the drug.
- A pregnant woman should remember that completely safe and absolutely harmless drugs do not exist.
The most dangerous period for the use of any drugs, both of chemical and natural origin, is considered the first trimester of pregnancy (the first 12 gestational weeks), when all organs and systems are laid in the fetus, which in the future will only develop and form the placenta. It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
Pronounced mutagenic hazard:
1. in industry - asbestos, acetaldehyde, vinyl chloride, dimethyl sulfate; factors of metallurgical and rubber industries;
Metals: copper, nickel, lead, zinc, cadmium, mercury, chromium, arsenic, styrene, formaldehyde, chloroprene, epichlorohydrin, ethylene oxide.
2. agriculture - a mixture of defoliants, pesticides, insectiosides, repellents, fungicides, pesticides, methylpartion, phthalaphos, chlorophos, gardona, DDT, contan.
If you work in a hazardous industry and come into contact with these chemicals, from early pregnancy, switch to "light work".
Global trends in early pregnancy from the point of view of evidence-based medicine are unambiguous: the need for rational diet therapy , intake of folic acid at least 400 mcg/day and potassium iodide 200 mg/day.
After 12-14 weeks of pregnancy, with an inadequate diet, the use of vitamin preparations during pregnancy and lactation is recommended as a way to improve the health of the mother and fetus . Vitamin complexes intended for other groups of the population (including children) are contraindicated for pregnant women!
Medicines during pregnancy
In existing classifications, it is customary to subdivide drugs during pregnancy into groups - safe, relatively safe, relatively unsafe and dangerous. Moreover, the list of drugs is periodically updated.
- Category A - safe drugs.
 Controlled trials have shown no risk to the fetus for the first 12 weeks of pregnancy. Regarding them, there is no evidence of a harmful effect on the fetus in late pregnancy. These are folic acid, levothyroxine sodium, paracetamol, magnesium sulfate.
Controlled trials have shown no risk to the fetus for the first 12 weeks of pregnancy. Regarding them, there is no evidence of a harmful effect on the fetus in late pregnancy. These are folic acid, levothyroxine sodium, paracetamol, magnesium sulfate. - Category B - relatively safe drugs. Experimental studies have generally not shown their teratogenic effects in animals and children whose mothers took such drugs. These are amoxicillin, heparin, insulin, aspirin, metronidazole (except for the first trimester)
- Category C - relatively unsafe drugs. When testing these drugs on animals, their teratogenic or embryotoxic effects were revealed. Controlled trials have not been conducted or the effect of the drug has not been studied (isoniazid, fluoroquinolones, gentamicin, antidepressants, antiparkinsonian drugs). These drugs should only be used if the potential benefit outweighs the potential risk.
- Caregory D - dangerous drugs.
 The use of drugs in this group is associated with a certain risk to the fetus, but despite this, it is possible to use the drug for health reasons (anticonvulsants, doxycycline, kanamycin, diclofenac).
The use of drugs in this group is associated with a certain risk to the fetus, but despite this, it is possible to use the drug for health reasons (anticonvulsants, doxycycline, kanamycin, diclofenac). - Category X - dangerous drugs that are contraindicated for use.
The teratogenic effect of drugs in this group has been proven, their use is contraindicated during pregnancy, as well as when planning a pregnancy.
Although almost 1000 chemicals are known to be teratogenic in animals, only a few chemicals have been proven to be permanently teratogenic in humans. These include a number of narcotic analgesics, chemotherapeutic drugs (antimetabolites, alkylating agents), anticonvulsants (trimethadione, valproic acid, fenithione, carbamazepine), androgens, warfarin, danazol, lithium, retinoids, thalidomide.
The safest drugs
(Larimore W. L., Petrie K.A., 2000)
L., Petrie K.A., 2000)
| Drug groups | The safest drugs |
| Analgesics | Paracetamol, narcotic analgesics (short courses), NSAIDs (except due date) |
| Antibiotics | Aminopenicillins, macrolides (Vilprafen), azithromycin, cephalosporins, clindamycin, erythromycin, metronidazole (except 1st trimester), penicillins, trimethoprim (except 1st trimester) |
| Antidepressants | Venlafaxine, fluoxetine, trazodone |
| Antidiarrheals | Loperamide |
| Antiemetics | Andacids, doxylamine, prochlorperazine, promethazine, vitamin B |
| Antihypertensives | B-blockers, hydralazine, methyldopa, prazosin |
| Antiparasitics | Permethrin |
| Antituberculous drugs | Ethambutol, isoniazid |
| Antivirals | Amantadine, acyclovir |
| Antihistamines | Cetirizine, loratadine |
| Anti-asthma/anti-allergy products | Epinephrine, inhaled bronchodilators, theophylline |
| Cardiovascular medicines | B-blockers, calcium channel blockers, digoxin, nitroglycerin |
| Constipation products | Bisacodyl, methylcellulose |
| Antidiabetics | Insulin |
| Gastrointestinal drugs | Sucralfate, metoclopramide |
| Thyroid hormones | Levothyroxine, liothyronine |
Terminals
It is very important that every pregnant woman remember that any drug during pregnancy can bring not only benefits, but also considerable harm, therefore, any self-administration during this period is not permissible, since their consequences are unpredictable and in many cases can cause irreparable harm to the developing fetus.
Key words
Antivirals for pregnant women - what to do if a pregnant woman has a cold in the 1st, 2nd, 3rd trimester
January 17, 2022
17.01
5 minutes
5 minutes.
42176
42
3
What is possible and what is not possible for pregnant women with a cold is one of the main issues that concern the expectant mother.
Article content
- Features of the treatment of acute respiratory viral infections in the 1st trimester
- Cold therapy in the 2nd trimester
- Treatment of acute respiratory viral infection in the 3rd trimester
- FAQ
Peculiarities of ARVI treatment in the 1st trimester
Perhaps the most difficult in the appointment of therapy.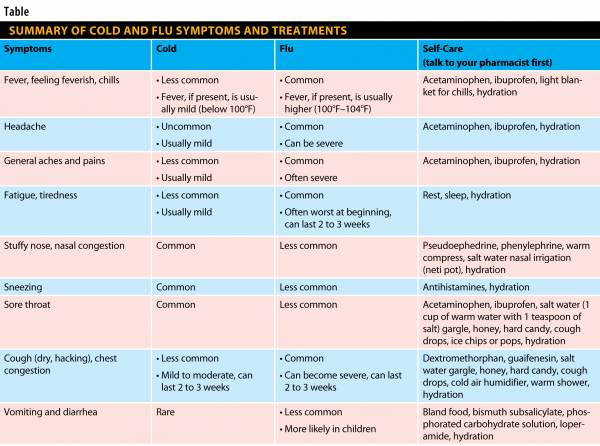 The fact is that it is at this time that the baby's internal organs are laid, as well as the nervous system. Exposure to various chemicals can adversely affect this process and cause the formation of malformations.
The fact is that it is at this time that the baby's internal organs are laid, as well as the nervous system. Exposure to various chemicals can adversely affect this process and cause the formation of malformations.
If the expectant mother fell ill in the first trimester, she is recommended to have more rest, take vitamins C and D, drink plenty of water and fresh cranberry juice. For sore throats, rinsing with a warm solution of furacilin or sage infusion is prescribed, rinsing the nose with sea water to treat a runny nose and inhaling with alkaline mineral water on a nebulizer when coughing.
At the first sign of a cold or SARS, you should consult a competent doctor. Our doctor will consult remotely: draw up a treatment regimen taking into account the well-being of the expectant mother, potential risks for the child and the timing of pregnancy.
2nd trimester cold therapy
In the second trimester, it is already easier for the doctor to choose drugs that are effective for the mother and safe for her baby for the treatment of colds. By this time, the placenta is formed in the uterus - a kind of barrier that can neutralize certain drugs. In the second trimester, antiviral drugs are already prescribed, most often interferon-based drugs, as well as antibiotics when bacterial complications are attached. Treatment of a runny nose, cough and sore throat is recommended in the same way as in the first trimester.
By this time, the placenta is formed in the uterus - a kind of barrier that can neutralize certain drugs. In the second trimester, antiviral drugs are already prescribed, most often interferon-based drugs, as well as antibiotics when bacterial complications are attached. Treatment of a runny nose, cough and sore throat is recommended in the same way as in the first trimester.
Pay attention! The lack of high-quality and comprehensive treatment of acute respiratory viral infection during pregnancy can cause placental insufficiency, a condition that is dangerous for the health and life of the child.
Treatment of acute respiratory viral infection in the 3rd trimester
At this time, the fetus is almost completely formed, so the list of approved drugs, including antiviral agents, is expanding. However, self-medication is still not recommended! It is very important to remember that some seemingly harmless plants can cause premature birth. So, for example, horsetail and sage stimulate the release of estrogen hormones into the blood, which stimulate the contraction of the smooth muscles of the uterus.
Example
A pregnant woman fell ill with ARVI for a period of 30 weeks. There were complaints of fever, cough and runny nose. They were prescribed: antiviral agents, antipyretic based on paracetamol, vitamins and inhalation on a nebulizer with alkaline mineral water and washing the nose with sea water. Against the background of the therapy, on the third day the woman felt an improvement, on the 7th day of the disease, the symptoms leveled off. Studies have shown that the fetus is fine.
The use of certain antiviral drugs should be discussed with a doctor. The fact is that not only the gestational age, but also the individual characteristics of the expectant mother can become a ban on their use. Contact our doctors by phone at any time of the day - they will check the drugs prescribed for you and give recommendations.
FAQ
How to treat SARS during pregnancy? Am I in 1st trimester?
+
Under the supervision of a doctor is the most important thing. It is recommended to rest more, ventilate the room more often, take vitamins C and D. If you have a sore throat, you can rinse with a warm solution of furacilin or sage infusion, rinse your nose with sea water if you have a cold, and inhale with alkaline mineral water if you cough.
It is recommended to rest more, ventilate the room more often, take vitamins C and D. If you have a sore throat, you can rinse with a warm solution of furacilin or sage infusion, rinse your nose with sea water if you have a cold, and inhale with alkaline mineral water if you cough.
What to do if a pregnant woman has a cold?
+
Do not self-medicate, but immediately consult a doctor. Of course, most of us know how to treat a cold on our own and have such experience. But this knowledge cannot be useful in this situation, because now it is important not only to effectively treat the disease in the mother, but also not to harm the baby. Therefore, a doctor is needed - a specialist who will assess the risks and help you choose the most effective and at the same time safe treatment.
What is the treatment for SARS during pregnancy in the 1st trimester?
+
At this time, the laying of the internal organs of the fetus occurs, so you need to act as delicately as possible. Preparations during this period must be selected carefully so as not to disrupt the processes of organ formation and not provoke malformations.
Preparations during this period must be selected carefully so as not to disrupt the processes of organ formation and not provoke malformations.
How to bring down the temperature during pregnancy?
+
The temperature during pregnancy can be brought down in several ways - with the help of physical cooling, for example, a cool compress on the forehead or rubbing the body with cold water. It is only important to understand that hypothermia will not benefit and act carefully. Of the antipyretic drugs, paracetamol-based products are recommended for expectant mothers.
What pills can pregnant women?
+
The expectant mother can take the drugs prescribed by a competent doctor. The specialist will assess the need for a particular remedy, as well as the potential risk to her baby. I also recommend that you always read the annotations to the drugs, there is a section "use during pregnancy" and breastfeeding. It contains information about whether these tablets and capsules are allowed for the expectant mother.
It contains information about whether these tablets and capsules are allowed for the expectant mother.
What can a low temperature during pregnancy in the 3rd trimester mean?
+
Most often, this situation is observed with a decline in strength and a decrease in immunity. If the situation persists for 2-3 days, it is recommended to consult a doctor observing the pregnancy. It also makes sense to double-check the thermometer readings by measuring the temperature on the control device.
What antipyretics can I take during pregnancy in the 3rd trimester?
+
The temperature during pregnancy in the 3rd trimester can be paracetamol-based. Such drugs do not have a negative effect on the fetus, while helping the mother - they reduce fever and reduce pain, which often accompanies colds.
What antiviral can be used during pregnancy in the 3rd trimester?
+
Interferon-based antiviral drugs are well suited for the treatment of SARS in the third trimester.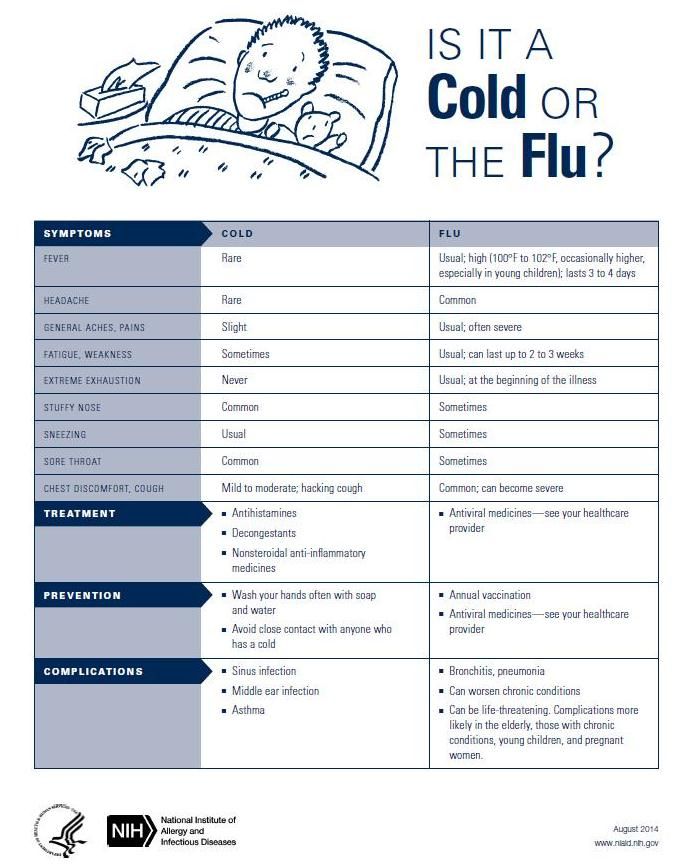 It is important that the annotation states that the drug is approved for use during pregnancy and the period of breastfeeding.
It is important that the annotation states that the drug is approved for use during pregnancy and the period of breastfeeding.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Articles 46
Specialist with extensive practical experience.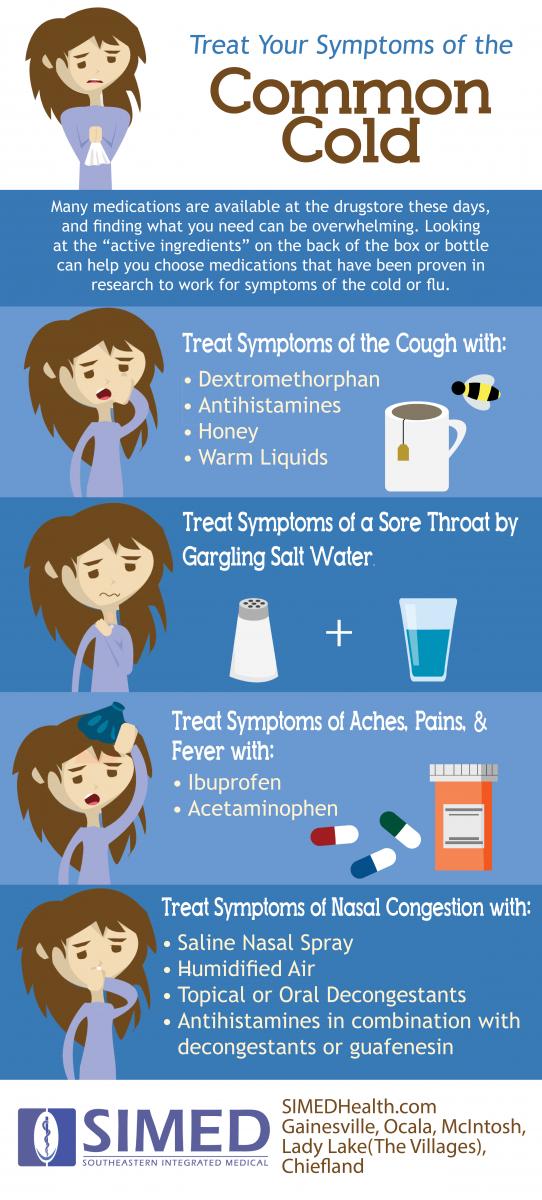 He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
- 1982 - 1986 NPO MONIIAG - obstetrician-gynecologist
- 1987 - 1989 VNITs OZMIR - obstetrician-gynecologist
- 1989 - 1992 departmental polyclinic st. Moscow - Kurskaya - obstetrician-gynecologist
- 1992 - 2001 NPO MONIIAG - obstetrician-gynecologist
- 2007 - 2008 NP KMIKM - doctor administrator
- 2009 - 2013 Pereslavl Central District Hospital, women's consultation - obstetrician-gynecologist
- 2020 to present Teledoctor24 LLC - doctor - consultant (gynecologist)
Sources
- ... P.V.Budanov, A.N.Strizhakov, V.V.Malinovskaya, Yu.V.Kazarova, “Discoordination of systemic inflammation in intrauterine infection”, Issues of gynecology, obstetrics and perinatology, 2009.

- ... Guidelines for the diagnosis, treatment and prevention of influenza in pregnant women, 2014
- ... Klimanova R.R., Malinovskaya V.V., Parshina O.V., Guseva T.S., Novikova S.V., Torshina Z.V., Zarochentseva N.V. "The effect of viral infections on the cytokine profile in pregnant women with a burdened obstetric history and immunocorrective therapy with interferon
Share:
Category: Pregnancy and childbirth
About health Pregnancy and childbirth About children healthy lifestyle Psychology Neurology Gastroenterology Personal care Medicines and dietary supplementsPrevious article
Medical interruption .