Can you have an abortion at 9 months
Abortions Later in Pregnancy | KFF
|
Introduction
Abortions occurring at or after 21 weeks gestational age are rare. They are often difficult to obtain, as they are typically costly, time-intensive and only performed by a small subset of abortion providers. Yet these abortions receive a disproportionate amount of attention in the news, policy and the law, and discussions on this topic are often fraught with misinformation; for example, intense public discussions have been sparked after several policymakers have theorized about abortions occurring “moments before birth” or even “after birth.” In reality, these scenarios do not occur, nor are they legal, in the U.S. Discussion of this topic is further obscured due to the terms sometimes used to describe abortions later in pregnancy– including “late-term,” “post-viability,” “partial birth,” “dismemberment” and “born-alive” abortions—despite many medical professionals criticizing and opposing their use. This fact sheet explains why individuals may seek abortions later in pregnancy, how often these procedures occur, how the concepts of viability and fetal pain play into this topic, and the various laws which regulate access to abortions later in pregnancy.
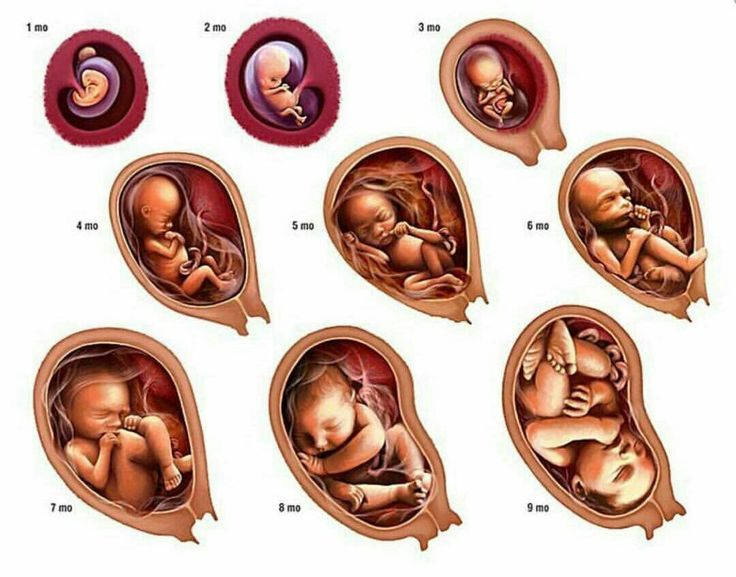
Clarifying Pregnancy Dating: pregnancies are measured using gestational age (GA), calculated in days and weeks since the first day of the last menstrual period (LMP). Since some people do not know the date of their LMP, ultrasound can also be used to calculate GA. Post-fertilization or fertilization age refers to the time since the egg and sperm fused to create a fertilized egg. Fertilization occurs approximately 2 weeks after menses, thus gestational age by LMP predates fertilization age by ~2 weeks. By convention, gestational age is used to discuss pregnancy dating as most pregnant individuals know their LMP, however certain abortion regulations reference fertilization age instead.
What is a so-called “late-term” abortion?
“Late term” abortion typically refers to abortions obtained at or after 21 weeks, however it is not an accepted medical term, nor is there a consensus around to which gestational ages it refers. Members of the medical community have criticized the term “late-term” abortion, as it implies abortions are taking place after a pregnancy has reached “term” (37 weeks) or “late term” (>41 weeks) which is false. In fact, the American College of Obstetricians and Gynecologists (ACOG) has written that “late-term abortion” has no medical meaning and should not be used in clinical or legal settings. As such, we will refer to abortions occurring at ≥21 weeks gestation as abortions later in pregnancy, but it should be noted that 21 weeks is a largely arbitrary cutoff based on how the CDC collects data on abortions. Abortions at this stage in pregnancy are sometimes referred to as “later abortions” by the medical community as well.
In fact, the American College of Obstetricians and Gynecologists (ACOG) has written that “late-term abortion” has no medical meaning and should not be used in clinical or legal settings. As such, we will refer to abortions occurring at ≥21 weeks gestation as abortions later in pregnancy, but it should be noted that 21 weeks is a largely arbitrary cutoff based on how the CDC collects data on abortions. Abortions at this stage in pregnancy are sometimes referred to as “later abortions” by the medical community as well.
What is viability? Why does it matter for abortions later in pregnancy?
Abortions later in pregnancy have been highly debated, in part because some people believe that this stage of pregnancy abuts the time around viability. In 1973, Roe v. Wade legalized abortion in the U.S., and in the process made “viability” the delineating factor in the abortion debate; before viability, a person has the right to obtain an abortion, whereas after viability, the state can restrict access to abortion in the interest of protecting the potential for human life, except in cases of health or life endangerment of the pregnant person.
The Supreme court made clear in Roe v. Wade that the courts are not in a position to assess when life begins and when viability has been reached, writing, “We need not resolve the difficult question of when life begins. When those trained in the respective disciplines of medicine, philosophy, and theology are unable to arrive at any consensus, the judiciary, at this point in the development of man’s knowledge, is not in a position to speculate as to the answer.” (Roe v. Wade) Given viability is case dependent and is only a possibility or probability of survival, rather than a guarantee of survival, the decision in Roe v. Wade left the right to an abortion after viability up to individual states to determine.
In a subsequent Supreme Court case on abortion, the court defined viability as follows:
“Viability is reached when, in the judgment of the attending physician on the particular facts of the case before him, there is a reasonable likelihood of the fetus’ sustained survival outside the womb, with or without artificial support.
Because this point may differ with each pregnancy, neither the legislature nor the courts may proclaim one of the elements entering into the ascertainment of viability – be it weeks of gestation or fetal weight or any other single factor – as the determinant of when the State has a compelling interest in the life or health of the fetus.” Colautti v. Franklin (1979)
Viability depends on many factors, including gestational age, fetal weight and sex, and medical interventions available. While viability does not refer to a specific gestational age, it is often presumed at 24 weeks gestation, with “periviability” referring to the time around viability (20 to 26 weeks gestation). For periviable births, the hospital at which the infant is delivered can greatly affect viability, and the patient’s insurance coverage may dictate where they can seek care. Infants born in resource-rich settings have a higher likelihood of survival than those born in resource-poor settings. This is in part due to access to neonatologists and maternal-fetal-medicine doctors, but also due to hospital-specific policies; in a study of 24 academic hospitals, active treatment for infants born at 22 weeks ranged from 0% to 100% depending on the hospital, showing that the criteria used to determine viability at one hospital may not be the same at another. If time allows and if the pregnant individual is clinically stable, they may be transferred to a facility better equipped for neonatal resuscitation before delivery, however this is not always possible. Further, insurance coverage and reimbursement for transfers in care varies by state and insurance plan.
This is in part due to access to neonatologists and maternal-fetal-medicine doctors, but also due to hospital-specific policies; in a study of 24 academic hospitals, active treatment for infants born at 22 weeks ranged from 0% to 100% depending on the hospital, showing that the criteria used to determine viability at one hospital may not be the same at another. If time allows and if the pregnant individual is clinically stable, they may be transferred to a facility better equipped for neonatal resuscitation before delivery, however this is not always possible. Further, insurance coverage and reimbursement for transfers in care varies by state and insurance plan.
At the time of Roe v. Wade, the Supreme Court wrote that viability “is usually placed at about seven months (28 weeks), but may occur earlier, even at 24 weeks.” With medical advances, extremely preterm infants can now survive at lower gestational ages than previously thought possible, particularly at hospitals with Level IV neonatal intensive care units (NICUs). The question we come up against is this: with viability possible at lower gestational ages, will abortions be prohibited at lower gestational ages as well? Many favor leaving that decision up to the patient and their provider, given viability depends on the individual pregnancy. Others, including some policymakers, desire early gestational age limits on abortion, well before the possibility of viability. In subsequent sections, we outline policies that regulate the provision of abortions later in pregnancy, including gestational age restrictions.
The question we come up against is this: with viability possible at lower gestational ages, will abortions be prohibited at lower gestational ages as well? Many favor leaving that decision up to the patient and their provider, given viability depends on the individual pregnancy. Others, including some policymakers, desire early gestational age limits on abortion, well before the possibility of viability. In subsequent sections, we outline policies that regulate the provision of abortions later in pregnancy, including gestational age restrictions.
How common are abortions later in pregnancy?
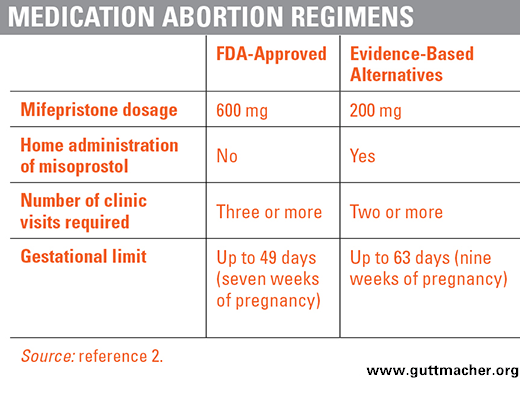
Abortions occurring at or after 21 weeks gestation are rare. According to the CDC’s Abortion Surveillance Data, the vast majority of abortions (91%) occur at or before 13 weeks gestation, while 7.7% occur from weeks 14 to 20 gestation, and just 1.2% of abortions are performed at or after 21 weeks (Figure 1). This amounts to approximately 5,200 abortions per year occurring at or after 21 weeks, however this is an underestimate as only 33 reporting areas report abortions to the CDC by gestational age. The percentage of abortions occurring at or before 13 weeks gestation has remained stable over the last few decades at 91-92%, however within this timeframe, more abortions are occurring earlier in pregnancy, at or before 8 weeks. This is likely in part due to the greater availability of medication abortions over the last two decades.
The percentage of abortions occurring at or before 13 weeks gestation has remained stable over the last few decades at 91-92%, however within this timeframe, more abortions are occurring earlier in pregnancy, at or before 8 weeks. This is likely in part due to the greater availability of medication abortions over the last two decades.
Figure 1: The Vast Majority of Abortions Occur Early in Pregnancy
The CDC does not elaborate on the breakdown by gestational age for abortions occurring past 21 weeks, but it is likely that the vast majority occur soon after 21 weeks rather than in the later in the pregnancy. While very limited data exists on this issue, a study from 1992 estimated 0.02% of all abortions occurred after 26 weeks gestation (320 to 600 cases per year). This may overestimate current day numbers, given the abortion rate is currently at a historic low, and restrictions on abortions later in pregnancy have increased.
Why do people have abortions later in pregnancy?
Non-Medical Reasons: Individuals seek abortions later in pregnancy for a number of reasons. As part of the Turnaway study out of the University of California San Francisco, from 2008-2010 over 440 women were asked about why they experienced delays in obtaining abortion care, if any (Figure 2). Almost half of individuals who obtained an abortion after 20 weeks did not suspect they were pregnant until later in pregnancy, and other barriers to care included lack of information about where to access an abortion, transportation difficulties, lack of insurance coverage and inability to pay for the procedure. This is unsurprising, given abortions can be cost-prohibitive for many; in a study from 2011-2012, the median cost of a surgical abortion at 10 weeks was $495, jumping to $1,350 at 20 weeks (range $750-$5,000) excluding the cost of travel and lost wages. Yet the Federal Reserve Board found 40% of U.S. adults do not have enough in savings to pay for a $400 emergency expense, meaning many individuals may need to delay having an abortion until they can raise the necessary funds.
As part of the Turnaway study out of the University of California San Francisco, from 2008-2010 over 440 women were asked about why they experienced delays in obtaining abortion care, if any (Figure 2). Almost half of individuals who obtained an abortion after 20 weeks did not suspect they were pregnant until later in pregnancy, and other barriers to care included lack of information about where to access an abortion, transportation difficulties, lack of insurance coverage and inability to pay for the procedure. This is unsurprising, given abortions can be cost-prohibitive for many; in a study from 2011-2012, the median cost of a surgical abortion at 10 weeks was $495, jumping to $1,350 at 20 weeks (range $750-$5,000) excluding the cost of travel and lost wages. Yet the Federal Reserve Board found 40% of U.S. adults do not have enough in savings to pay for a $400 emergency expense, meaning many individuals may need to delay having an abortion until they can raise the necessary funds.
Figure 2: Many Factors Contribute to Delays in Obtaining Abortion Care
Additionally, of all the abortion-providing facilities in the U.S., only 34% offer abortions at 20 weeks and just 16% at 24 weeks, meaning individuals may need to travel a significant distance to find an available, trained provider. Abortions at this stage also typically require two days to complete with inpatient care, as opposed to outpatient or at-home management that is possible earlier in pregnancy.1 In the years since these data were collected, dozens of abortion restrictions have been enacted across the county, including mandated waiting periods; it is therefore possible that individuals seeking abortion today may face even more delays in care than these data reflect.
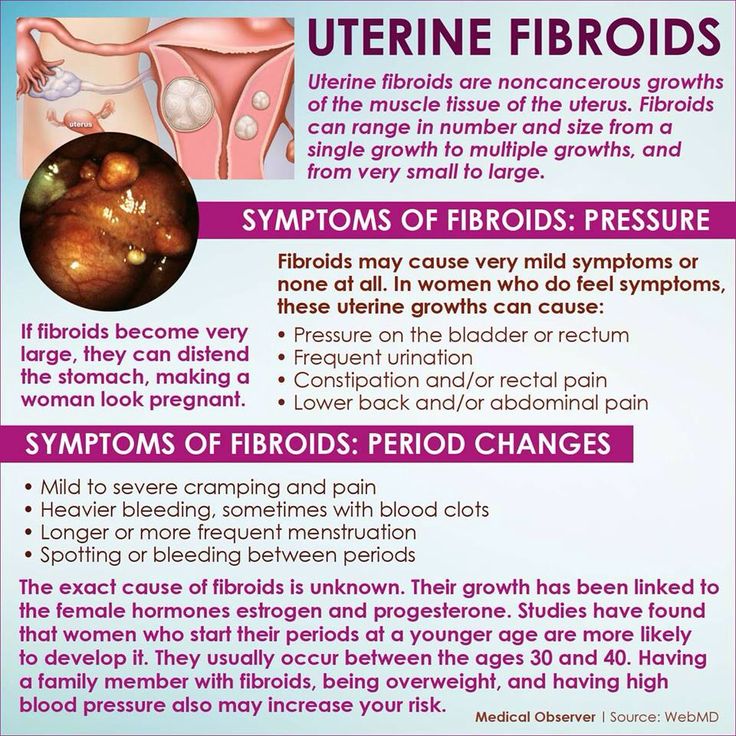
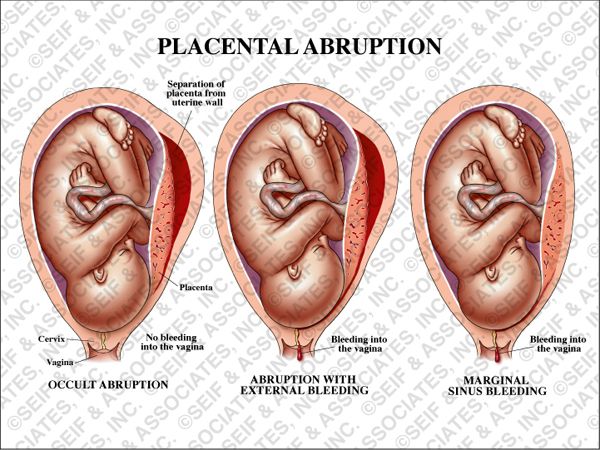
Fetal Anomalies: Individuals also seek abortions later in pregnancy due to medical reasons. With medical advances, many genetic fetal anomalies can be detected early in pregnancy; for example, chorionic villus sampling can diagnose Down Syndrome or cystic fibrosis as earlier as 10 weeks gestation. Structural fetal anomalies, however, are often detected much later in pregnancy. As part of routine care, a fetal anatomy scan is performed around 20 weeks, which entails ultrasound imaging of all the developing organs. Many structural anomalies are discovered at this time that would not have been apparent previously. A proportion of these are lethal fetal anomalies, meaning that the fetus will almost certainly die before or shortly after birth, meaning the fetus may be nonviable.2 In these cases, many individuals wish to terminate their pregnancies, rather than carrying the pregnancy until the fetus or newborn passes away. Very often these pregnancies are desired, making this decision exceedingly difficult for parents. Inadequate data exist to know how many abortions later in pregnancy occur due to fetal anomalies, but a study by Washington University Hospital showed almost all women whose fetuses had lethal fetal anomalies chose to terminate their pregnancies.
Structural fetal anomalies, however, are often detected much later in pregnancy. As part of routine care, a fetal anatomy scan is performed around 20 weeks, which entails ultrasound imaging of all the developing organs. Many structural anomalies are discovered at this time that would not have been apparent previously. A proportion of these are lethal fetal anomalies, meaning that the fetus will almost certainly die before or shortly after birth, meaning the fetus may be nonviable.2 In these cases, many individuals wish to terminate their pregnancies, rather than carrying the pregnancy until the fetus or newborn passes away. Very often these pregnancies are desired, making this decision exceedingly difficult for parents. Inadequate data exist to know how many abortions later in pregnancy occur due to fetal anomalies, but a study by Washington University Hospital showed almost all women whose fetuses had lethal fetal anomalies chose to terminate their pregnancies.
A study of maternal fetal medicine (MFM) doctors—specialists who manage pregnancies with fetal anomalies— found most agreed that termination of pregnancy due to a lethal fetal anomaly should be allowed in all circumstances (76%). The majority (75%) discuss abortion as a management option soon after diagnosing a lethal fetal anomaly, but services for terminating pregnancies in these scenarios are limited. Only 40% of MFMs worked at healthcare centers offering abortions past 24 weeks for lethal fetal anomalies. An additional 12% knew of available services <50 miles away.
The majority (75%) discuss abortion as a management option soon after diagnosing a lethal fetal anomaly, but services for terminating pregnancies in these scenarios are limited. Only 40% of MFMs worked at healthcare centers offering abortions past 24 weeks for lethal fetal anomalies. An additional 12% knew of available services <50 miles away.
Health Risk to the Pregnant Person: Life threatening conditions may also develop later in pregnancy. These include conditions like early severe preeclampsia, newly diagnosed cancer requiring prompt treatment, and intrauterine infection (chorioamnionitis) often in conjunction with premature rupture of the amniotic sac (PPROM). If these conditions arise before the fetus is viable, the pregnant individual may pursue termination of pregnancy to preserve their own health. If these conditions arise after the fetus is considered viable, Roe v. Wade still protects the right for these individuals to obtain an abortion in cases of health or life endangerment, however it may be difficult to find a provider for this service as previously mentioned. Typically every effort is made to save the life of both the pregnant individual and the fetus, pursuing delivery rather than abortion.
Typically every effort is made to save the life of both the pregnant individual and the fetus, pursuing delivery rather than abortion.
How do states regulate abortions later in pregnancy?
A few states have sought to expand access to abortions later in pregnancy. The New York Reproductive Health Act enacted in January 2019 expands protections for abortion providers and pregnant individuals who have abortions after 24 weeks in cases of health or life endangerment or lethal fetal anomalies. Virginia similarly proposed loosening restrictions on abortions later in pregnancy, by reducing the number of physicians who would need to approve an abortion after 28 weeks gestation from three to one, and by broadening maternal exceptions to include more general threats to mental and physical health. This bill failed to pass, but sparked national discussion about regulation of abortions later in pregnancy.
Many states have directed their efforts in the opposite direction, aiming to increase restrictions on abortions later in pregnancy.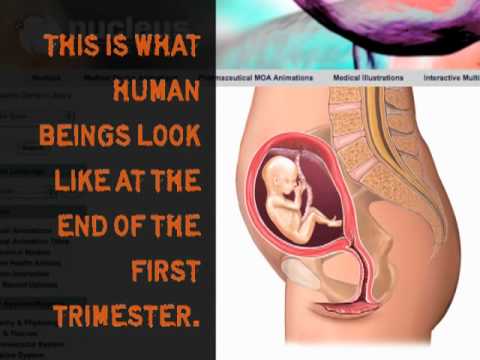 States most often do so by (1) placing gestational age limits on abortion, and/or (2) restricting the methods providers can use to perform abortions later in pregnancy. In discussion of these laws, it is important to note that most policymakers are not clinicians, therefore many of the terms used to discuss abortions later in pregnancy are designed to communicate a political message, not a precise medical concept. In the Appendix, we mention several terms written into policy and the law so that readers may be familiar with their meaning, but they are not medical terms.
States most often do so by (1) placing gestational age limits on abortion, and/or (2) restricting the methods providers can use to perform abortions later in pregnancy. In discussion of these laws, it is important to note that most policymakers are not clinicians, therefore many of the terms used to discuss abortions later in pregnancy are designed to communicate a political message, not a precise medical concept. In the Appendix, we mention several terms written into policy and the law so that readers may be familiar with their meaning, but they are not medical terms.
Abortion bans by gestational age
43 states prohibit abortions after a certain point in pregnancy, with almost half of states prohibiting abortion at “viability” or when viability is often presumed, at 24 weeks. Other states seek earlier gestational age limits on abortion. For example, so-called “heartbeat” bans propose banning abortion after the detectable presence of cardiac activity as early as 6 weeks gestation, months before viability. To date, all such “heartbeat” bans, along with others that seek to ban abortions before 20 weeks, are not in effect due to ongoing or resolved litigation. However, some states have enacted abortion bans from 20-22 weeks gestational age, using the rationale of fetal pain.
To date, all such “heartbeat” bans, along with others that seek to ban abortions before 20 weeks, are not in effect due to ongoing or resolved litigation. However, some states have enacted abortion bans from 20-22 weeks gestational age, using the rationale of fetal pain.
Fetal Pain
Many states restrict abortions at 22 weeks gestational age or 20 weeks post-fertilization, arguing the fetus has the ability to feel pain at this point in development, contrary to medical evidence. A systematic review of literature on fetal pain found that pain perception is unlikely before weeks 29 or 30 gestational age. ACOG has found “no legitimate scientific data or information” that supports the assertion that fetuses feel pain at 20 weeks post-fertilization, and the Royal College of Obstetricians and Gynecologists has also concluded fetal pain is not possible before 24 weeks, given immature brain development and neural networks.
Despite the medical evidence, policymakers have enacted gestational limits using the rationale that a fetus can feel pain at earlier stages in pregnancy. Mississippi bans abortion at 20 weeks gestation while abortion at 22 weeks gestation is banned by 17 other states (AL, AR, GA, IN, IA, KS, KY, LA, NE, ND, OH, OK, SC, SD, TX, WV, WI). Additionally, 13 states provide verbal or written counseling on fetal pain as part of pre-abortion counseling (AK, AR, GA, IN, KS, LA, MN, MO, OK, SD, TX, UT, WI) (Figure 3). Some states mandate this information be given to those seeking abortion later in pregnancy, while in others, this counseling is required at any stage of pregnancy. In Utah legislation was introduced, but not passed, that would have required providers to administer “fetal anesthesia” during abortions later in pregnancy. There is, however, no standard practice for how to provide fetal anesthesia during abortions, nor is there adequate safety data on how this would affect pregnant individuals.
Mississippi bans abortion at 20 weeks gestation while abortion at 22 weeks gestation is banned by 17 other states (AL, AR, GA, IN, IA, KS, KY, LA, NE, ND, OH, OK, SC, SD, TX, WV, WI). Additionally, 13 states provide verbal or written counseling on fetal pain as part of pre-abortion counseling (AK, AR, GA, IN, KS, LA, MN, MO, OK, SD, TX, UT, WI) (Figure 3). Some states mandate this information be given to those seeking abortion later in pregnancy, while in others, this counseling is required at any stage of pregnancy. In Utah legislation was introduced, but not passed, that would have required providers to administer “fetal anesthesia” during abortions later in pregnancy. There is, however, no standard practice for how to provide fetal anesthesia during abortions, nor is there adequate safety data on how this would affect pregnant individuals.
Figure 3: The Concept of Fetal Pain Plays a Role in Many Abortion Regulations
Bans on abortion methods used later in pregnancy
Almost all abortions performed at ≥21 weeks are performed by a dilation and evacuation (D&E) procedure (93–95% per CDC data). This involves dilating the cervix and evacuating the pregnancy tissue using forceps, with or without suction. D&Es can be performed safely up to at least 28 weeks gestational age, and when compared to their alternative of labor induction, have been found to be quicker and result in fewer complications; further, many women prefer surgical management as they will be sedated and do not have to undergo labor and delivery of the fetus.
This involves dilating the cervix and evacuating the pregnancy tissue using forceps, with or without suction. D&Es can be performed safely up to at least 28 weeks gestational age, and when compared to their alternative of labor induction, have been found to be quicker and result in fewer complications; further, many women prefer surgical management as they will be sedated and do not have to undergo labor and delivery of the fetus.
Several states have sought to ban D&E procedures, which would significantly limit how providers are able to perform abortions later in pregnancy. Currently, Mississippi and West Virginia have enacted D&E bans, while bans are temporarily enjoined in 6 states and over 25 states have attempted to pass such legislation. 20 states ban dilation and extractions (D&Xs), a rarely used abortion procedure also referred to as an intact D&E or a “partial birth abortion” by policymakers (Appendix). In total, 21 states have enacted bans on abortion methods used later in pregnancy (Figure 4).
Figure 4: Many States Ban Certain Abortion Procedures Used Later in Pregnancy
In addition to gestational age limits and method bans used for abortions later in pregnancy, it is important to remember these abortions are also subject to the same regulations that apply for abortions earlier in pregnancy, including mandatory waiting periods and physician and hospital requirements.
| The authors would like to acknowledge Jennifer Karlin, MD, PhD (University of California, San Francisco) for her review of an earlier draft of this fact sheet. |
Appendix
| Term | Description |
| Late-term abortion: | Non-medical term that typically refers to abortions occurring at or after 21 weeks gestational age, but does not consistently refer to a specific gestational age cutoff. |
| Post-viability abortion: | Non-medical term used to refer to abortions occurring after the fetus is considered viable, and sometimes used synonymously with late-term abortions. |
| Born-alive abortion: | Non-medical term used to refer to the exceedingly rare circumstance in which a newborn shows signs of life after an abortion, including breathing, a beating heart and voluntary movement. These cases are the subject of the proposed “Born-Alive Abortion Survivors Protection Act,” mandating healthcare workers provide care to infants who show signs of life after an attempted abortion. |
| Partial birth abortion: | Non-medical term often used to refer to a rarely used abortion procedure called dilation and extraction (D&X, also known an intact D&E). Has sometimes been used to refer to all dilation and evacuations (D&Es), the most common abortion procedure used from 14-28 weeks gestational age. |
| Dismemberment abortion: | Non-medical term sometimes used to refer to D&Es. |
NOTES: KFF does not endorse use of these terms. | |
Euthanasia and newborn infants | Euthanasia
Children are occasionally born with such serious disorders that termination of life is regarded as the best option.
The law permits physicians to terminate the lives of newborn infants and to perform late-term abortion only on condition that they fulfil the following due care criteria:
- In the light of prevailing medical opinion, the child’s suffering must be unbearable and with no prospect of improvement. This means that the decision to discontinue treatment is justified. There must be no doubt about the diagnosis and prognosis;
- Both the physician and the parents must be convinced that there is no reasonable alternative solution given the child’s situation;
- The parents must have given their consent for the termination of life;
- The parents must have been fully informed of the diagnosis and prognosis;
- At least one other, independent physician must have examined the child and given a written opinion on compliance with the due care criteria listed above
- The termination must be performed with all due care.
Late term abortion
The Dutch Termination of Pregnancy Act allows abortions to be carried out up to the 24th week of pregnancy. This is the point at which the foetus becomes viable outside the mother’s womb. Late-term abortions – after the 24th week – are excluded from the Termination of Pregnancy Act and fall under the criminal law. Doctors have a duty to notify them to the review committee.
Late-term abortions may be performed only in exceptional circumstances. The following due care criteria apply:
- The unborn child must have a disorder so serious that medical experts believe that medical treatment following the birth will be futile. There must be no doubt about the diagnosis and prognosis;
- The unborn child must be suffering, or must be likely to suffer following its birth, with no prospect of improvement;
- The mother must make an explicit request for the pregnancy to be terminated on the grounds of the physical or mental suffering the situation is causing her;
- The physician must have given the parents a full explanation of the diagnosis and prognosis.
 This means that both the physician and the parents must be convinced that there is no reasonable alternative solution given the child’s situation;
This means that both the physician and the parents must be convinced that there is no reasonable alternative solution given the child’s situation; - At least one other, independent physician must have examined the child and given a written opinion on compliance with the due care criteria listed above;
- The pregnancy must be terminated with all due care.
Physician notification procedure
Following a late-term abortion or termination of the life of a newborn infant, the physician has an immediate duty to observe the following procedure He must notify the municipal pathologist, who will then contact the Public Prosecution Office.
If it sees no particular reason for delay, the Public Prosecution Service will issue consent for the funeral. Thereafter, the pathologist will send the details of the case to the Central Committee of Experts on late-term abortion and termination of infants.
The pathologist assesses whether the physician has acted with due care. The Committee reports its findings to the Public Prosecution Service. Finally, the Public Prosecution Service decides whether any action should be taken against the physician concerned.
The Committee reports its findings to the Public Prosecution Service. Finally, the Public Prosecution Service decides whether any action should be taken against the physician concerned.
why terminate a pregnancy in the later stages and how it is done in Krasnoyarsk
“Like a bolt from the blue”
“We counted the fingers and toes, saw how the heart was beating. Then there was a short pause, and the doctor asked us to go for a walk so that the baby would roll over and he could finish the study. When we returned, there were already two doctors in the doctor's office. Now they were staring at the monitor together and trying to see something. I understood that there were some problems. nine0003
And suddenly, like a bolt from the blue, the phrase sounded: “I can’t see the baby’s bladder. There is some kind of education, but what it is is too hard to understand ", - there are hundreds of stories with a similar beginning.
For many women, becoming a mother is a cherished dream. In most cases, pregnancy ends safely - the birth of a healthy baby. But sometimes families get a disappointing prognosis even at the stage of the first ultrasound and tests. Finding out that a child has serious illnesses is always difficult, especially if the health of the father and mother is all right and there are no prerequisites for terrible diagnoses. nine0003
In most cases, pregnancy ends safely - the birth of a healthy baby. But sometimes families get a disappointing prognosis even at the stage of the first ultrasound and tests. Finding out that a child has serious illnesses is always difficult, especially if the health of the father and mother is all right and there are no prerequisites for terrible diagnoses. nine0003
Where to go, what to do, what decisions to make? These are only the first questions that arise in pregnant women who have received a poor prognosis.
It is not customary in society to discuss this topic. In our time, when the question of whether abortion is considered murder is still unresolved, the topic of late pregnancy termination, when the unborn child is not just an embryo, but already looks like a full-fledged baby, is painful even for the medical community.
"No error"
Memories of mothers who have experienced the loss of a child (from the forum of the charity fund "Light in Hands"): "After 12 weeks, no one will terminate a pregnancy without a special consultation of doctors and a clearly established diagnosis. Needless to say, none of the doctors spoke to us normally, no one explained a clear sequence of actions, terms, risks, what does “abortion of pregnancy”, etc. mean in general?
Needless to say, none of the doctors spoke to us normally, no one explained a clear sequence of actions, terms, risks, what does “abortion of pregnancy”, etc. mean in general?
Genetic abnormalities are detected at the stage of pregnancy screenings, there are three in total. Screening is a set of studies that allows you to get the most complete information about the health of the fetus. If the ultrasound doctor has doubts during the examination, the patient is sent to the Medical Genetic Center. nine0003
“Of course, most of all we are tuned in to early diagnosis, namely, to identify some abnormalities up to 12 weeks, less often up to 21-22 weeks. But sometimes there are cases when deviations can be detected only in the second half of the term: usually this happens either when a woman registers late and has never been examined before, or when the pathology manifests itself late. Then a decision is already made on a more detailed examination and on the possible termination of such a pregnancy, ”said Tatyana Elizaryeva, head physician of the medical genetic center. nine0003
nine0003
The Medical Genetic Center of Krasnoyarsk sees patients from all over the Krasnoyarsk Territory. In the event that the doctor has doubts about the health of the child during the screening, the pregnant woman is sent for a more detailed examination
If the woman has passed all the examinations and the diagnosis is confirmed, she is invited to the medical commission of the genetic center. You can come to it either alone or with your husband or family members, usually the patient is asked how it is convenient for her. The commission includes several specialists: an ultrasound diagnostician, a neonatologist, an obstetrician-gynecologist, a doctor specializing in a particular pathology (cardiac surgeon, neurosurgeon, pediatric surgeon, etc.). There, the woman is told in detail about what is happening, what kind of pathology the child has, whether it can be treated and what kind of treatment it is. nine0003
“It is important to let a woman understand what she is facing and offer all possible options. If these are chromosomal disorders and an intellectual deficiency in the fetus, for example, Down's syndrome, we explain that a child can be born and, in the absence of any physical disabilities, even be able to develop - sit, perhaps write and draw, communicate a little. But we also make it clear that such a child will never be able to live independently, especially after the departure of parents or other guardians, such a child requires rather large financial costs, which not every family is ready for, such a child will always require more attention and strength, and for his parents will have to fight every step in his development. All this is necessary so that families understand what they are getting into in both cases. In any situation, we, as doctors, are obliged to respect their choice,” emphasizes Tatiana Elizarieva. nine0003
If these are chromosomal disorders and an intellectual deficiency in the fetus, for example, Down's syndrome, we explain that a child can be born and, in the absence of any physical disabilities, even be able to develop - sit, perhaps write and draw, communicate a little. But we also make it clear that such a child will never be able to live independently, especially after the departure of parents or other guardians, such a child requires rather large financial costs, which not every family is ready for, such a child will always require more attention and strength, and for his parents will have to fight every step in his development. All this is necessary so that families understand what they are getting into in both cases. In any situation, we, as doctors, are obliged to respect their choice,” emphasizes Tatiana Elizarieva. nine0003
After a medical consultation, any couple has time to think and make an informed decision. Doctors note that today the equipment and technology of the medical genetic center excludes even the very possibility of making an incorrect diagnosis. In addition, in each case, the results of the tests are processed by several doctors, each giving an opinion and recommendations on pregnancy.
In addition, in each case, the results of the tests are processed by several doctors, each giving an opinion and recommendations on pregnancy.
“This is a forced measure”
Up to 22 weeks, pregnancy can be terminated, including by medication. The procedure is carried out in the Krasnoyarsk maternity hospital No. 4.
“Medical indications for termination of pregnancy from 12 to 22 weeks are fetal developmental anomalies that are incompatible with life and cannot be surgically corrected,” said Lyudmila Popova, chief physician of maternity hospital No. 4.
This is a chromosome analysis. In a healthy person, all chromosomes are paired, in the picture at number 21 there are three chromosomes instead of two. This is what Down syndrome looks like
According to doctors, a woman can choose to terminate her pregnancy or report it. But often mothers do not fully realize what they doom themselves and their families to when they give birth to children with serious pathologies or non-viable ones. nine0003
nine0003
Memoirs of mothers who experienced the loss of a child from the forum of the charity foundation "Light in Hands"): "The diagnosis was terrible, the doctors said that children with such pathologies are born dead or die in infancy. Realizing that losing a baby, a long-awaited daughter, after her birth would be simply fatal for me, I agreed to an abortion for medical reasons. To be honest, I still don’t understand if I did the right thing, and I blame myself that I went along with my relatives and doctors by agreeing to this abortion.” nine0018
“It is very hard to survive. Walk for 9 months and know that a child can die on the first or second day. What is more difficult: walking and knowing that it will be so, or terminating a pregnancy in the middle? Usually women agree with the opinion of doctors, but sometimes they still decide to leave the child, ”says Lyudmila Popova.
In general, most often, before the 22nd week, women agree and go for an abortion.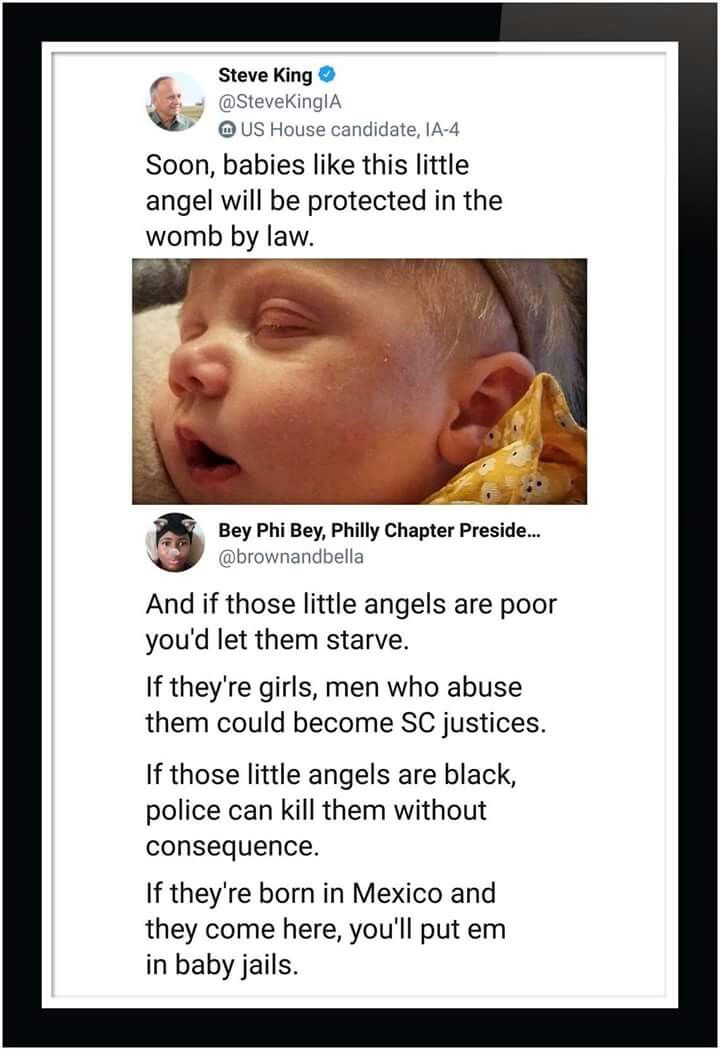
“This is not just an abortion at the request of a woman, this is a forced measure. Because then supporting the lives of these children is a colossal burden. It happens that mothers then refuse them, because they cannot cope, they give them to the Homes for the Disabled, and then the state takes care of these children, ”concluded Lyudmila Popova. nine0003
“After 22 weeks, this is already a full-fledged birth”
Until 2019, in the Krasnoyarsk Territory, pregnancy was not terminated at later stages (after 22 weeks of pregnancy) due to indications from the fetus (congenital malformations incompatible with life, which for some reason have not been previously identified). Women had only one way out - to give birth to a child with a pathology. And only at the end of 2018, the clinical protocol of the Ministry of Health of the Russian Federation "Artificial termination of pregnancy at a later date for medical reasons in the presence of fetal developmental anomalies" was approved, on the basis of which this medical technology was introduced in the Krasnoyarsk Regional Clinical Center for Maternal and Child Health. nine0003
nine0003
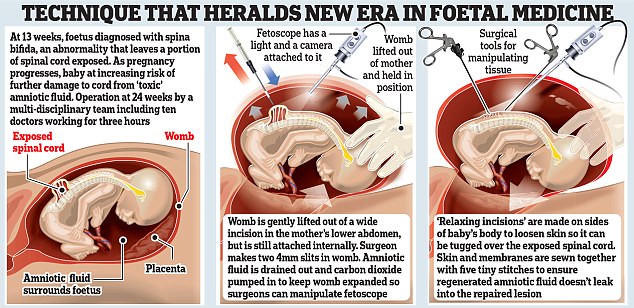
The procedure for terminating a pregnancy at a later date is the same throughout Russia: an anesthetic is administered to the fetus in utero, after which the elimination (cardiac arrest) of the fetus is carried out, and labor is induced. The procedure is performed by an ultrasound doctor, an anesthesiologist, an anesthetist nurse and a laboratory assistant.
“Like any manipulation, the interruption procedure has certain risks associated with both the use of medications and the operation. Bleeding may develop, there may be negative consequences from drugs - side effects, allergies. Any intervention in a woman's body, even at the present stage of the development of medicine, is always a health risk that can lead to complete deprivation of reproductive function. Many couples decide to prolong the pregnancy, hoping for a miracle, for a diagnostic error, ”says Pavel Baurov, head of the advisory clinic at the Regional Clinical Center for Maternal and Childhood Welfare.
nine0003
Head of the advisory polyclinic of the Regional Clinical Center for Maternal and Childhood Pavel Baurov
Women who refuse to terminate a pregnancy in case of medical indications, most often name their personal beliefs as the reasons, as well as their families. In the case when a decision is made to leave a non-viable child, the patient continues to be observed in the consultation.
How to survive the impossible
Late pregnancy termination is a severe psychological trauma. After the procedure itself, each woman is waiting for the rehabilitation process, a psychologist always works with her. Now there are such specialists at every antenatal clinic. A psychologist from the Center for Maternal and Childhood Welfare talks with a patient before and after the procedure.
“A woman in such a situation has a lot of difficult experiences. And one of the most difficult that appears at such moments is the feeling of guilt.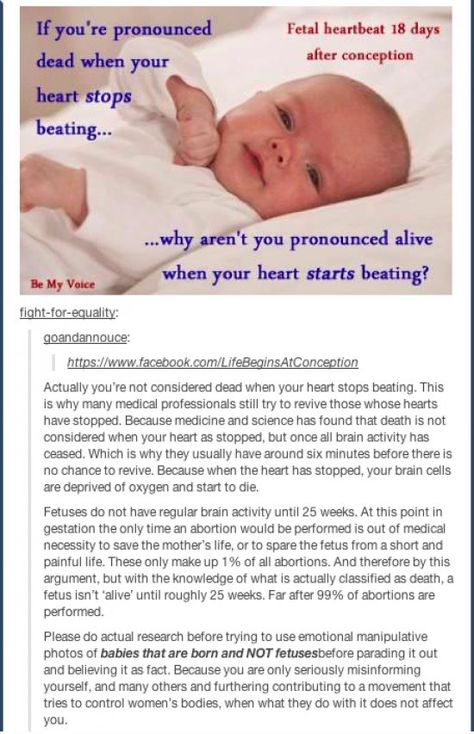 Thoughts often arise in the mother’s head: “How could I allow this to be done?”, even if the situation is completely hopeless. The moment of choice also leaves an imprint - the woman still decides whether to terminate her pregnancy or keep it. Guilt, as a rule, is irrational, not corresponding to the real situation, ”the psychologist notes. nine0003
Thoughts often arise in the mother’s head: “How could I allow this to be done?”, even if the situation is completely hopeless. The moment of choice also leaves an imprint - the woman still decides whether to terminate her pregnancy or keep it. Guilt, as a rule, is irrational, not corresponding to the real situation, ”the psychologist notes. nine0003
Memories of mothers who have experienced the loss of a child (from the forum of the charitable foundation "Light in Hands"): “Two years have passed. And yes, we still gave birth to a child, a beautiful daughter. But there was not a day that I did not remember my first daughter. I wake up in the middle of the night and remember those days. I keep these memories as the only thing left of my child.”
Medical termination is exactly the same antenatal loss ( situation where the baby dies at during pregnancy — ed. ). A woman loses a baby for a long time, despite the fact that from the end of the first trimester she already perceives him as a person, interacts with him, communicates internally.
A psychologist has no influence on a woman's choice - such is the professional position. It helps to realize some things, provides psychological support. Sometimes the situation itself can be completely hopeless when a diagnosis of a pathology that is incompatible with life is made, but even this does not always affect the final choice of a couple. A psychologist helps to dispel any doubts, relieve tension and at least slightly alleviate the moment of suffering. nine0003
After the interruption, the woman goes through the process of mourning, as after any other loss. If adaptation is disrupted for too long and a person cannot live a full life, then psychologists talk about pathological mourning, which requires more serious treatment. It is very important that the environment of the woman also helps to survive the crisis.
“Unfortunately, no one taught us sympathy, our society, and usually people feel discomfort next to those who have suffered a loss. As a rule, a woman's relatives think that the most important thing is that she stopped worrying about .This is where all these tips start: “stop crying”, “live on”, “get together”, and so on. But a woman doesn’t need this, she needs to live her grief, cry out her tears, she needs to speak out, ”says psychologist Svetlana Chursina.
Rehabilitation usually takes months, but even when a woman returned to normal life, this difficult moment will remain in her memory forever, it is impossible to erase it. From time to time, with tears, she will still remember her unborn baby. nine0003
Clinical psychologist of the Center for Maternal and Child Health Svetlana Chursina
Patients often ask the question: “What should I do with the child? What will happen to him after I give birth to him?
“The doctor cannot insist, but still it is better if you look at the baby and say goodbye to him. It is better to keep some of his things related to pregnancy, ultrasound scans and so on. Firstly, the brain is arranged in such a way that until it sees it, it will not believe that this is final, therefore subconsciously it will not give you rest, there will always be doubts: “What if he were alive, but if he were healthy? “.Secondly, after some time, women who could not look at the child and say goodbye may regret it. Still, over time, this is perceived as the loss and death of a loved one, so you should not completely depersonalize the baby. But in any case, the choice is up to the woman herself. You can offer, but in no case insist,” advises Svetlana Chursina. nine0075
At the Maternity and Child Care Center, a woman receives 1-2 consultations, after which the doctors recommend (if necessary) that she contact a psychologist at the antenatal clinic, or visit free support groups. In Russia, the charitable foundation "Light in Hands" works with mothers who have suffered perinatal loss. You can get advice and find out all the working conditions on the fund’s hotline.
Psychologists advise relatives, friends and colleagues to start from the desires of a woman - do not impose help, insist on talking if she does not want it. “Time heals” is one of the main principles of recovery, so the main thing is to give a woman this time.
nine0003
As the doctors say, there are no right or wrong decisions when it comes to terminating a pregnancy, there are only those with which the family can live on. The task of doctors is to support the life and health of both the mother and her child at any cost. Life and quality of life depend only on the family where they faced the problem. It is impossible to predict possible risks by 100%, and you need to remember that no family is immune from this. Today in the Krasnoyarsk Territory there is all the necessary medical support for pregnant women with pathologies of the unborn baby and for those who decide to terminate the pregnancy. We hope that as few families as possible will need such assistance. nine0003
Valya Kotlyar especially for Newslab online newspaper.
Photographs by Alina Kovrigina.Terms of termination of pregnancy at the request of a woman
Abortion is an artificial termination of pregnancy, which is included in the system of compulsory health insurance.
According to the Federal Law of November 21, 2011 N 323-FZ (as amended on December 8, 2020) “On the Basics of Protecting the Health of Citizens in the Russian Federation”, the terms for terminating a pregnancy at the request of a woman are possible up to 12 weeks, for social reasons - up to 22 weeks, for medical indications - at any stage of pregnancy.Only a gynecologist can accurately recommend a method for terminating a pregnancy by doing an ultrasound to determine the gestational age.
Early abortion methods
Up to 7-8 weeks, pregnancy can be terminated by medication or by vacuum aspiration. With the medical method, in the presence of a doctor, a woman drinks a pill, the gynecologist observes her condition for some time, gives recommendations and sends her home. The medicine provokes a miscarriage, the fetus, along with blood clots, leaves the uterus. To assess whether the fetus is completely out, after a week it is necessary to do a control ultrasound.
If fetal remains are found in the uterine cavity, they will only have to be removed surgically. nine0003
An alternative to early medical abortion is vacuum aspiration. The procedure is performed without the use of traumatic instruments. The fetus is removed from the uterine cavity under high pressure using special equipment. During the procedure, local anesthesia is used, so the woman is conscious all the time and can leave the hospital in a few hours. Vacuum aspiration is indicated up to 6 weeks of gestation, while the fetus is not yet firmly fixed in the uterus and is easily removed from the cavity. nine0003
Abortions up to 12 weeks
For a period of 8 to 12 weeks, the fetus is removed from the uterine cavity only by surgical curettage. This is an effective, but the most traumatic method, which has many side effects. Trusting a surgical abortion is only an experienced and responsible doctor who will carry out the procedure as carefully as possible using sterile instruments.
Surgical abortion is performed in a hospital under general anesthesia. Within a few hours after curettage, the woman is under the supervision of a doctor, after which she can leave
To reduce the risk of complications after a surgical abortion, a woman is given medication. Especially it should not be ignored at the first abortion. After a few weeks, the patient needs to do an ultrasound, and after a month, visit a gynecologist for an examination.
No doctor will break the law and perform an abortion at the request of a woman for more than 12 weeks. Therefore, a decision to terminate a pregnancy must be made in a timely manner.
Abortion after 12 weeks
Up to 22 weeks, a woman can have an abortion if diagnosed with diseases that pose a great threat to both her and the unborn child:
- Oncology requiring treatment with chemotherapy.
- Open form of pulmonary tuberculosis.
- Severe heart defects.
- Neurodegenerative diseases, mental disorders.

- Autoimmune diseases in the acute stage.
According to social indications, abortion is carried out only in one case - the pregnancy occurred as a result of rape. nine0003
If a woman goes for an abortion after 12 weeks, she must have in her hands the opinion of the commission authorizing the abortion at a later date. Artificial childbirth is a very complex procedure that must be performed in a medical facility with intensive care.
After 22 weeks, an abortion can be done only for medical reasons - if the mother or fetus has pathologies that are incompatible with life. It's not an abortion, it's a premature birth. With the help of medications, the doctor stimulates delivery and the fetus comes out naturally. The procedure is difficult for a woman both mentally and physically. Often, in addition to physical health, it is necessary to restore psychological health as well. nine0003
Abortion for up to 12 weeks can be done both in the only family planning center in St.