Blood type compatibility pregnancy
Rh Incompatibility During Pregnancy (for Parents)
One of the first tests a pregnant woman should expect is a blood-type test. This test checks her blood type and Rh factor. Her Rh factor may play a role in her baby's health, so it's important to know this information early in pregnancy.
What's an Rh Factor?
An Rh factor is a protein found on some red blood cells (RBCs). Not everyone carries this protein, though most do. They are Rh-positive. People who don't carry the protein are Rh-negative.
What if Parents Don't Have the Same Rh Factor?
When a mother-to-be and father-to-be are not both positive or negative for Rh factor, it's called Rh incompatibility.
For example:
- If a woman who is Rh negative and a man who is Rh positive conceive a baby, the fetus may have Rh-positive blood, inherited from the father. (About half of the children born to an Rh-negative mother and Rh-positive father will be Rh-positive.
)
Rh incompatibility usually isn't a problem if it's the mother's first pregnancy. That's because the baby's blood does not normally enter the mother's circulatory system during the pregnancy.
During the birth, though, the mother's and baby's blood can mix. If this happens, the mother's body recognizes the Rh protein as a foreign substance. It then might begin making antibodies (proteins that act as protectors if foreign cells enter the body) against the Rh protein.
Rh-negative pregnant women can be exposed to the Rh protein that might cause antibody production in other ways too. These include:
- blood transfusions with Rh-positive blood
- miscarriage
- ectopic pregnancy
When Is a Baby at Risk?
Rh antibodies are harmless until the mother's second or later pregnancies. If she is ever carrying another Rh-positive child, her Rh antibodies will recognize the Rh proteins on the surface of the baby's blood cells as foreign.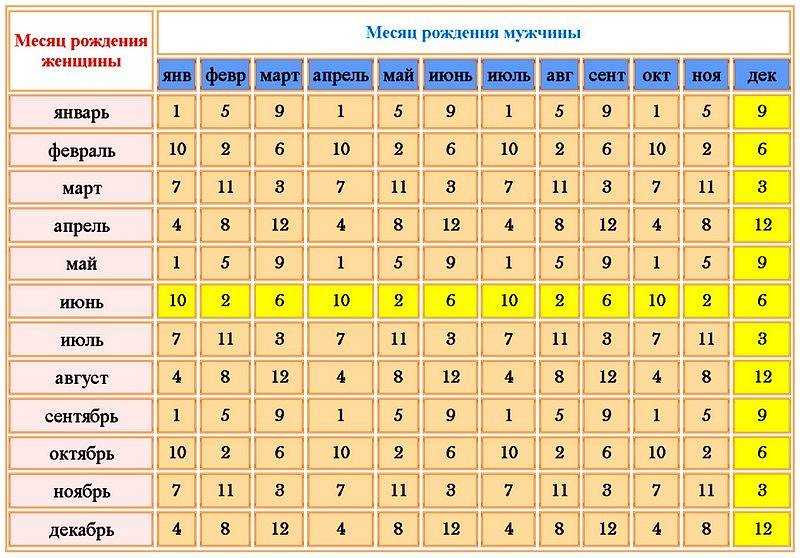 Her antibodies will pass into the baby's bloodstream and attack those cells.
Her antibodies will pass into the baby's bloodstream and attack those cells.
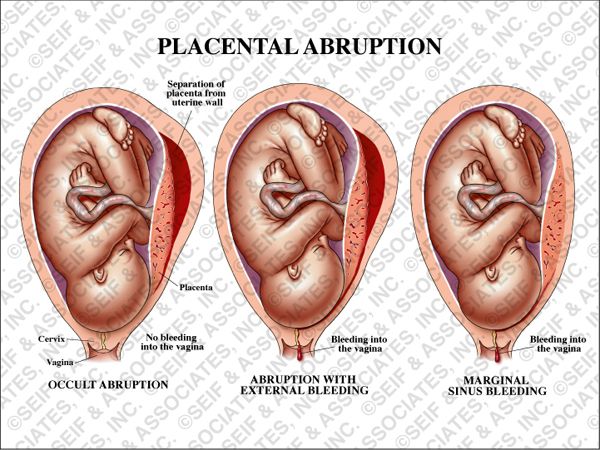
This can make the baby's red blood cells swell and rupture. This is known as hemolytic or Rh disease of the newborn. It can make a baby's blood count get very low.
How Is Rh Incompatibility Treated?
If a pregnant woman has the potential to develop Rh incompatibility, doctors give her a series of two Rh immune-globulin shots during her first pregnancy. She'll get:
- the first shot around the 28th week of pregnancy
- the second shot within 72 hours of giving birth
Rh immune-globulin acts like a vaccine. It prevents the mother's body from making any Rh antibodies that could cause serious health problems in the newborn or affect a future pregnancy.
A woman also might get a dose of Rh immune-globulin if she has a miscarriage, an amniocentesis, or any bleeding during pregnancy.
If a doctor finds that a woman has already developed Rh antibodies, her pregnancy will be closely watched to make sure that those levels are not too high.
In rare cases, if the incompatibility is severe and a baby is in danger, the baby can get special blood transfusions called exchange transfusions either before birth (intrauterine fetal transfusions) or after delivery. Exchange transfusions replace the baby's blood with blood with Rh-negative blood cells. This stabilizes the level of red blood cells and minimizes damage from Rh antibodies already in the baby's bloodstream.
Thanks to the success rate of Rh immune-globulin shots, exchange transfusions in Rh-incompatible pregnancies are rarely needed in the United States.
What Else Should I Know?
If you're not sure what your Rh factor is and think you're pregnant, it's important to start regular prenatal care as soon as possible — including blood-type testing. With early detection and treatment of Rh incompatibility, you can focus on more important things — like welcoming a new, healthy baby.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
Blood Types (for Parents) - Nemours KidsHealth
Blood transfusions are a lifesaving treatment for many Americans. Blood transfusions are needed for many reasons, including surgery, after accidents, and for patients with
Blood transfusions are needed for many reasons, including surgery, after accidents, and for patients with
chronicillnesses and cancer. Every 2 seconds, someone needs a blood transfusion.
Blood cannot be artificially made, so doctors rely on volunteer donations. To keep the blood supply safe, every donation is tested for blood type and checked for infectious diseases.
What Are the Components of Blood?
All blood contains these basic components:
- red blood cells that deliver oxygen
- white blood cells that fight infections
- platelets that help blood clot
- plasma, the liquid part of blood
But not everyone has the same blood type.
What Are the Blood Types?
Categorizing blood according to type helps prevent reactions when someone gets a blood transfusion. Red blood cells have markers on their surface that characterize the cell type.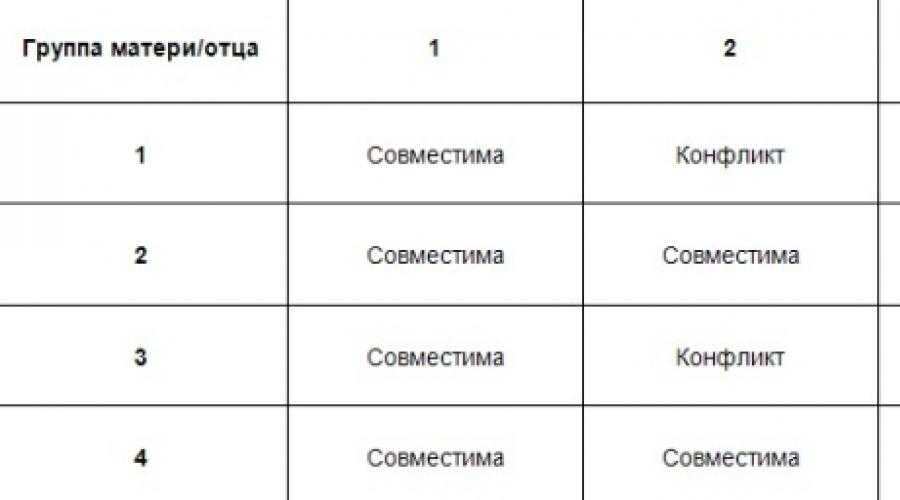 These markers (also called antigens) are proteins and sugars that our bodies use to identify the blood cells as belonging in us.
These markers (also called antigens) are proteins and sugars that our bodies use to identify the blood cells as belonging in us.
The two main blood groups are ABO and Rh.
The ABO blood system has four main types:
- Type A: This blood type has a marker known as A.
- Type B: This blood type has a marker known as B.
- Type AB: This blood type has both A and B markers.
- Type O: This blood type has neither A nor B markers.
Blood is further classified as being either "Rh positive" (meaning it has Rh factor) or "Rh negative" (without Rh factor).
So, there are eight possible blood types:
- O negative. This blood type doesn't have A or B markers, and it doesn't have Rh factor.
- O positive. This blood type doesn't have A or B markers, but it does have Rh factor. O positive blood is one of the two most common blood types (the other is A positive).
- A negative. This blood type has A marker only.
- A positive. This blood type has A marker and Rh factor, but not B marker. Along with O positive, it's one of the two most common blood types.
- B negative. This blood type has B marker only.
- B positive. This blood type has B marker and Rh factor, but not A marker.
- AB negative. This blood type has A and B markers, but not Rh factor.
- AB positive. This blood type has all three types of markers — A, B, and Rh factor.
Having any of these markers (or none of them) doesn't make a person's blood any healthier or stronger. It's just a genetic difference, like having green eyes instead of blue or straight hair instead of curly.
Why Are Blood Types Important?
The immune system is the body's protection against invaders. It can identify antigens as self or nonself. To get a blood transfusion safely, a person's immune system must recognize the donor cells as a match to his or her own cells. If a match isn't recognized, the cells are rejected.
To get a blood transfusion safely, a person's immune system must recognize the donor cells as a match to his or her own cells. If a match isn't recognized, the cells are rejected.
The immune system makes proteins called antibodies that act as protectors if foreign cells enter the body. Depending on which blood type a person has, the immune system will make antibodies to react against other blood types.
If a patient gets the wrong blood type, the antibodies immediately set out to destroy the invading cells. This aggressive, whole-body response can give someone a fever, chills, and low blood pressure. It can even cause vital body systems — like breathing or the kidneys — to fail.
Here's an example of how the blood type-antibody process works:
- Let's say you have type A blood. Because your blood contains the A marker, it makes B antibodies.
- If B markers (found in type B or type AB blood) enter your body, your type A immune system gets fired up against them.

- This means that you can only get a transfusion from someone with A or O blood, not from someone with B or AB blood.
In the same way, if you have the B marker, your body makes A antibodies. So as a person with type B blood, you could get a transfusion from someone with B or O blood, but not A or AB.
Things are a little different for people with type AB or type O blood:
- If you have both A and B markers on the surface of your cells (type AB blood), your body does not need to fight the presence of either.
- This means that someone with AB blood can get a transfusion from someone with A, B, AB, or O blood.
But if you have type O blood, your red blood cells have no A or B markers. So:
- Your body will have both A and B antibodies and will therefore feel the need to defend itself against A, B, and AB blood.
- A person with O blood can only get a transfusion with O blood.
Blood transfusions are one of the most frequent lifesaving procedures hospitals do. Blood is collected from healthy donors every day, and more blood donors are always needed. One blood donation can save up to three lives.
Blood is collected from healthy donors every day, and more blood donors are always needed. One blood donation can save up to three lives.
Incompatibility of blood types for conception, Rh-conflict of blood types
Incompatibility of blood types for conception of a child
Almost all people know their blood type, but few people think about the compatibility of partners and the need to check at the stage of pregnancy planning.
Blood type and Rh factor are of great importance in the birth of healthy children.
Today, the incompatibility of blood types for conception is fully studied and the knowledge of fertility doctors helps to give birth to a healthy baby. According to studies, every fourth woman on earth has a negative Rh factor, and 40% of women in the world have the first blood type. Both those and others can get a Rh-conflict with a future baby. Rhesus conflict can occur not only by Rhesus, but also by blood group. With a Rh conflict, the mother's body defines the child as a foreign object and tries to get rid of it. Such a pregnancy passes with complications, but often ends in the birth of a healthy child. nine0005
Such a pregnancy passes with complications, but often ends in the birth of a healthy child. nine0005
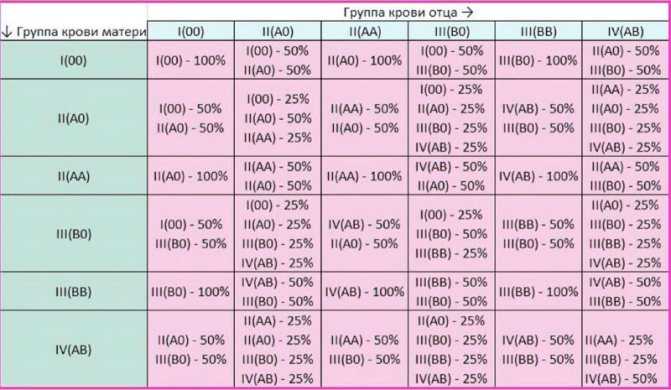
What is a blood group
A blood group is a complex of proteins on the surface of red blood cells. ABO is the main system for determining the compatibility and incompatibility of blood for conception and transfusions. According to the system, 4 blood groups are distinguished:
I ( O ) - the absence of antigens A and B.
II (A) - the presence of antigen A (Ao or AA phenotype).
III (B) - the presence of antigen B (phenotype BO and BB).
IV (AB) - the presence of antigens A and B (AB phenotype)
The baby inherits from the parent the blood group whose gene is dominant. The strongest genes are A and B. If the father has blood type A and the mother has B, the child can inherit any of the four groups. If a child inherits the O gene from one parent and the A gene from the other, then he will have an A or O blood type. If the baby inherited the O gene from two parents, then he will have an O blood type.
Fertility doctors can determine incompatibility by the blood type of husband and wife.
- A husband and wife with 1 blood type have children with the absence of type A and B antigens.
- From father and mother with 1 and 2 blood groups, children will inherit 1 and 2 blood groups.
- Parents with blood groups 1 and 3 will have children with blood groups 1 and 3.
- Mother and father with group 4 can have children with any blood group except 1
Effects of blood type incompatibility on pregnancy
- Fetal hypoxia;
- Hemolytic disease of the newborn;
- Thickening of the placenta and umbilical cord;
- Violation of the cardiovascular system and brain; nine0028
- Mental and physical retardation;
- Jaundice of the skin
Solution of the problem of blood type incompatibility
Modern medicine allows to solve the problem of blood type incompatibility for pregnancy with timely treatment.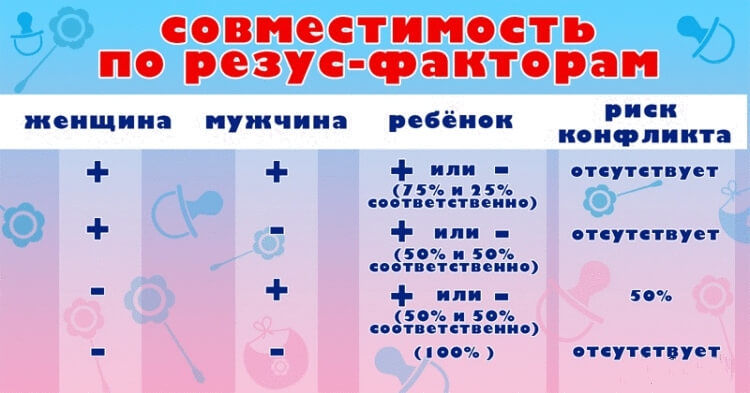 Today, an increasing number of couples are planning a pregnancy and undergo a complete examination of the body. This is the right approach that allows you to correct your health and solve a number of hidden problems, including the incompatibility of spouses by blood type. nine0005
Today, an increasing number of couples are planning a pregnancy and undergo a complete examination of the body. This is the right approach that allows you to correct your health and solve a number of hidden problems, including the incompatibility of spouses by blood type. nine0005
Doctors of the Medical Center for Reproductive Health "Gameta" are ready to answer your questions and conduct a complete examination of the body for Rhesus conflict. Reproductologists, professors and candidates of medical sciences with extensive experience work in our center. All studies are carried out on advanced European equipment, which guarantees high accuracy of the results.
Book a consultation by phone or fill out a short form on our website. We will offer a convenient time for you. nine0005
Pregnancy with various Rh blood factors
Dear future parents!
Each of us in our lives met with such concepts as blood group and Rh factor, but not everyone appreciates the importance and necessity of determining these blood indicators during planning and carrying a desired pregnancy.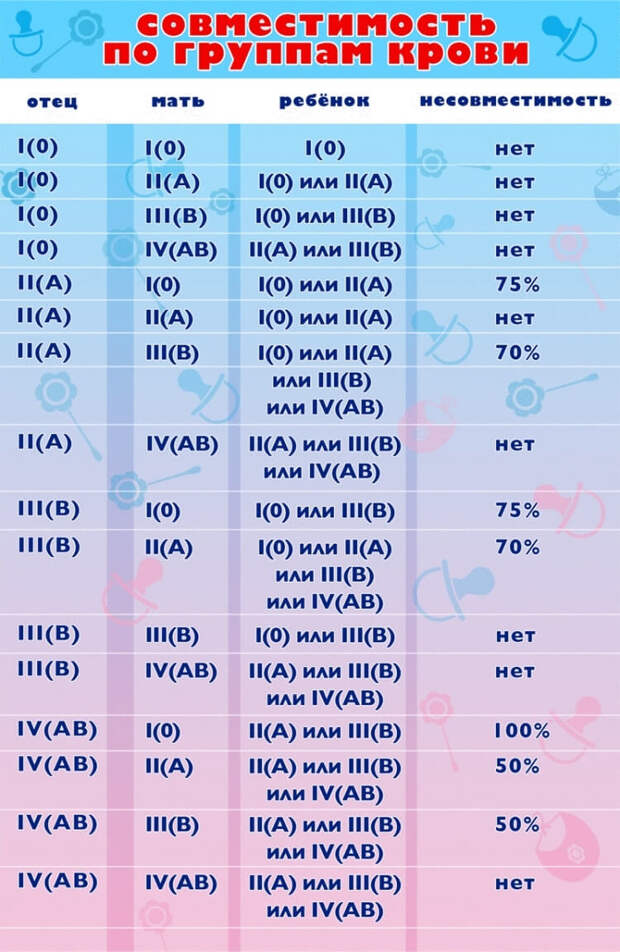
In order to understand this issue, we want to provide you with the necessary information and tell you about the clinical activities that are carried out in our center. nine0005
The Rh factor is a protein found on the surface of red blood cells (red blood cells that carry oxygen to tissues). If this protein is absent, then the Rh factor is considered negative. If the Rh protein is present in the blood, the Rh factor is considered positive. We all have either a negative or a positive Rh factor.
Future mom and dad, as you know, may have different blood Rh factors. If both parents are Rh-positive, then the child, as a rule (in 75% of cases), inherits a positive Rh factor. If both parents have Rh-negative blood, the situation is similar, the child in this case will be born with Rh-negative blood factor. If the mother is Rh-positive and the father is Rh-negative, there will be no complications during pregnancy. nine0005
Couples deserve great attention, where the mother has a negative Rh factor of the blood, and the future father has a positive one. In this situation, there is a risk of developing a Rh conflict - incompatibility of the blood of the mother and fetus.
In this situation, there is a risk of developing a Rh conflict - incompatibility of the blood of the mother and fetus.
The mechanism of development of the Rhesus conflict, as a rule, is based on the work of our immune system. The body of a pregnant woman with Rh-negative blood begins to produce antibodies to red blood cells - the red blood cells of the unborn child. But this situation occurs only if the Rh factor of the fetus is positive, inherited from the father. It is these antibodies, penetrating the placenta, that can destroy the erythrocytes of the unborn child, and as a result, cause a decrease in hemoglobin, intoxication and disruption of the work of all vital organs and systems. The outcomes of the course of such a pregnancy, often unfavorable, are the threat of miscarriage, hemolytic disease of the fetus, high risks of intrauterine death of the child, premature birth, etc. nine0005
In order to avoid adverse outcomes, the following rules should be followed:
- Parents-to-be should determine their blood type and Rh factor prior to conception.
- It must be remembered that abortions, miscarriages, blood transfusions, invasive procedures, can lead to increased sensitization (ie, the appearance of immune antibodies) in the body of an Rh-negative woman.
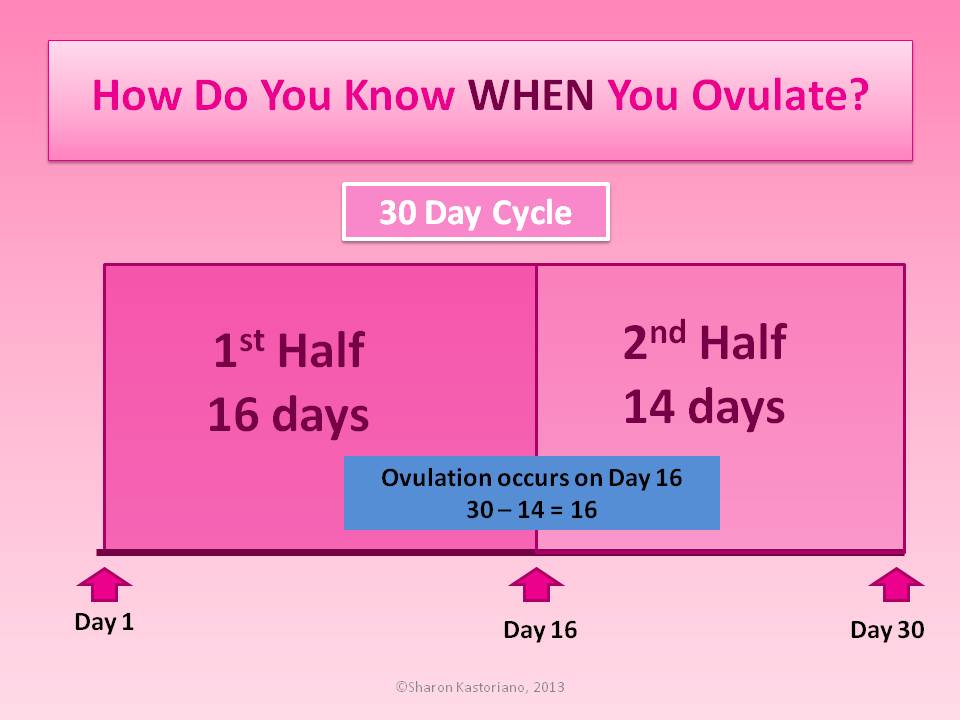
- If the Rh factor of the future mother turned out to be negative, and the father of the child is positive, it is necessary to determine the titer of anti-erythrocyte antibodies in the blood of a pregnant woman up to 20 weeks of pregnancy 1 time per month, then 1 time in 2 weeks. More frequent determination of antibody titer is carried out according to the doctor's prescription, depending on the indications. nine0028
- Upon reaching the gestational age of 28 weeks, in the absence of an antibody titer, it is necessary to enter 1 dose of anti-Rh-D-immunoglobulin. This drug prevents the formation of antibodies to the Rh factor, and therefore prevents the destruction of red blood cells in the fetus.
Due to the administration of the drug, specific antibodies may appear in the blood, therefore, after the administration of immunoglobulin, the determination of anti-erythrocyte antibodies is not carried out. The second dose of immunoglobulin is administered within the first 72 hours after delivery, provided that the baby's Rh factor is positive. It is also necessary to administer anti-Rhesus immunoglobulin within 72 hours during invasive procedures during pregnancy: chorion biopsy, placental biopsy, cordocenesis, amniocentesis, and for any adverse pregnancy outcome: abortion, miscarriage, ectopic pregnancy, cystic mole. nine0028
The second dose of immunoglobulin is administered within the first 72 hours after delivery, provided that the baby's Rh factor is positive. It is also necessary to administer anti-Rhesus immunoglobulin within 72 hours during invasive procedures during pregnancy: chorion biopsy, placental biopsy, cordocenesis, amniocentesis, and for any adverse pregnancy outcome: abortion, miscarriage, ectopic pregnancy, cystic mole. nine0028
Currently, at the Medical Company "Life" it has become possible to determine the Rh factor of the fetus using a modern, non-invasive technique using the mother's blood. The reliability of this result is quite high, it is 99%. The test allows not only to determine the affiliation of the Rh factor of the future baby at an early stage of pregnancy, but also to identify the risk group of pregnant women for the development of the Rh conflict. This study makes it possible to predict the course of pregnancy in Rh-negative women, timely take preventive measures to prevent the development of Rh-conflict and identify the exact category of patients who need to study the titer of anti-erythrocyte antibodies throughout pregnancy and the introduction of anti-Rh immunoglobulin.