Can you have a vaginal birth with herpes
Genital herpes in pregnancy - InformedHealth.org
Created: July 12, 2018; Next update: 2021.
Herpes infections are only rarely passed on to babies during childbirth. If a woman already had herpes viruses inside her body at the start of pregnancy, there's no reason why she shouldn’t give birth naturally – unless there are signs of an outbreak shortly before she goes into labor.
Herpes infections can be life-threatening for newborn babies. Because of this, many women who have genital herpes are afraid of passing herpes viruses on to their child while giving birth. But this only rarely happens.
How best to deal with genital herpes in pregnancy, and whether a natural birth is possible, will depend on
whether there are any signs of a genital herpes outbreak shortly before the birth and
when the woman became infected with the virus.
Babies are most likely to become infected if their mother has a genital herpes outbreak at the time of the birth. They may then come into contact with the viruses as they move through the cervix and vagina. People who have herpes should also be particularly careful in the first eight weeks of the baby’s life. For instance, they should take care not to kiss the baby during this time, and wash their hands regularly. If the baby starts showing signs of a herpes infection – such as a fever, listlessness, loss of appetite or a rash – you should seek medical advice immediately.
The risk of infection is much smaller if the woman already had genital herpes before, or at the beginning of, pregnancy. This is because her immune system will have had a chance to produce antibodies to the virus. The mother passes these antibodies on to her unborn child through her placenta, giving him or her a certain amount of protection.
Infection before or at the beginning of pregnancy
Women who become infected with herpes before pregnancy, or in the first three months of pregnancy, only rarely infect their child with it.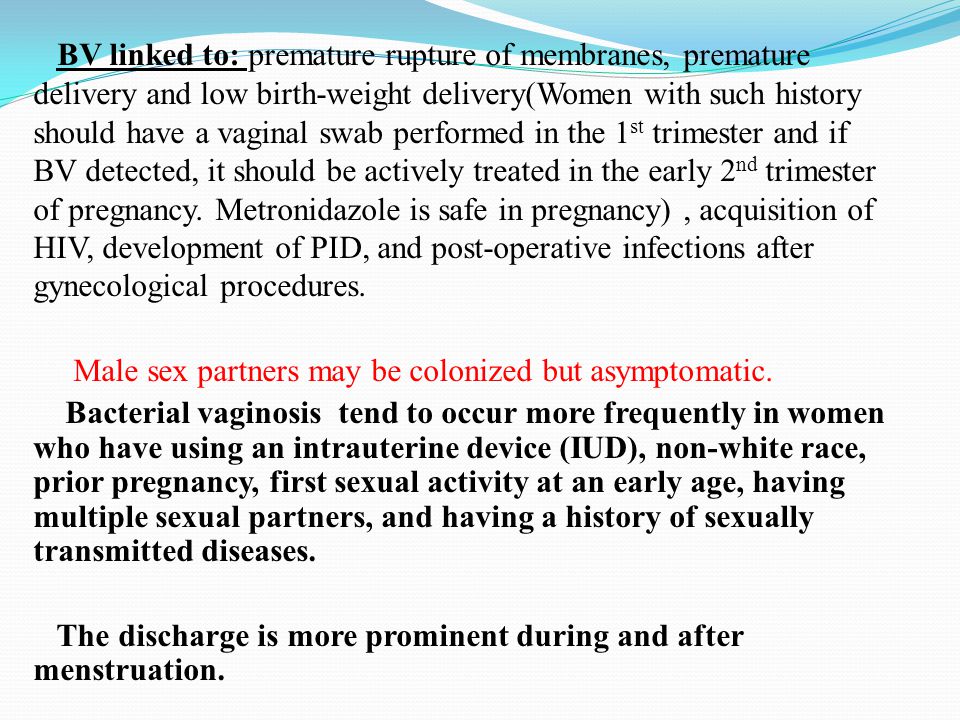 One big study found that 1 out of 100 babies became infected during childbirth.
One big study found that 1 out of 100 babies became infected during childbirth.
Pregnant women who have genital herpes should talk to their doctor about it. He or she can then check the skin for signs of an outbreak shortly before the birth. It’s also important to tell the doctor if there are any early signs of an outbreak, such as tingling in the genital area, around the time of the birth. If there are no signs of an outbreak, there’s no reason why the woman shouldn't give birth naturally. If there are, she is usually advised to have a Cesarean section. This greatly lowers the risk of infecting the baby.
It is estimated that about 13 out of 100 pregnant women who have genital herpes have an outbreak at the time of the birth. The risk of this happening can be reduced by preventive treatment with antiviral medication, which is then taken every day from 35 weeks of pregnancy until the birth. This also increases the chances of the woman being able to have a natural birth. Research has found that Cesarean sections were carried out in
13 out of 100 people who didn’t have preventive treatment with antiviral medication, compared to
only 4 out of 100 women who did have preventive antiviral treatment.

The drug aciclovir is generally used for this purpose because it is the drug that doctors have the most experience with. Studies haven’t found any evidence that it harms the baby.
Women can decide for themselves whether or not they would like to take medication to prevent a herpes outbreak: Some women really don’t want to take any medication while they are pregnant. Others would really like to give birth naturally if possible. And some trust that everything will go well, even without preventive treatment.
Infection in the last trimester of pregnancy
If women become infected with genital herpes in the last three months of pregnancy, the virus is passed on to their baby in about 30 to 50 out of 100 births. Because of this risk, women who get genital herpes in the last trimester of pregnancy usually have a Cesarean section in order to protect the child. It’s also a good idea to talk with a doctor who is specialized in the treatment of infectious diseases.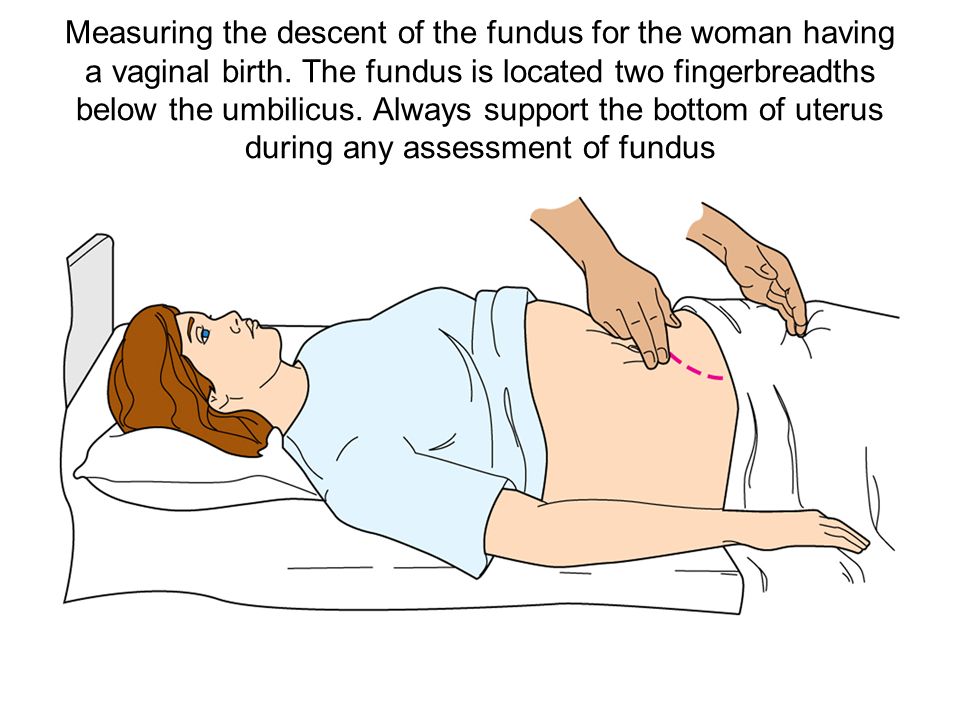
In order to prevent infection in the last three months of pregnancy, it’s best to avoid sex with people who have (or could have) genital herpes. This is also true when it comes to oral sex with people who have cold sores.
How can herpes outbreaks in pregnancy be treated?
Because initial outbreaks of genital herpes usually cause more severe symptoms, they are often treated with aciclovir in pregnant women, too. If the symptoms are particularly severe, the medication can be given intravenously (through an IV drip).
After that, further outbreaks are normally a lot milder, so antiviral drugs are often no longer used. But medication may be considered if the symptoms are severe or if complications arise.
Sources
Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant. JAMA 2003; 289(2): 203-209. [PubMed: 12517231]
Hollier LM, Wendel GD.
 Third trimester antiviral prophylaxis for preventing maternal genital herpes simplex virus (HSV) recurrences and neonatal infection. Cochrane Database Syst Rev 2008; (1): CD004946. [PubMed: 18254066]
Third trimester antiviral prophylaxis for preventing maternal genital herpes simplex virus (HSV) recurrences and neonatal infection. Cochrane Database Syst Rev 2008; (1): CD004946. [PubMed: 18254066]Patel R, Alderson S, Geretti A, Nilsen A, Foley E, Lautenschlager S et al. European guideline for the management of genital herpes, 2010. Int J STD AIDS 2011; 22(1): 1-10. [PubMed: 21364059]
Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64(RR-03): 1-137. [PMC free article: PMC5885289] [PubMed: 26042815]
World Health Organization (WHO). WHO Guideline for the Treatment of Genital Herpes Simplex Virus. Genf: WHO; 2016.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system.
 The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.
The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Herpes & Pregnancy – American Sexual Health Association
If a woman with genital herpes has virus present in the birth canal during delivery, herpes simplex virus (HSV) can be spread to an infant, causing neonatal herpes, a serious and sometimes fatal condition. Neonatal herpes can cause an overwhelming infection resulting in lasting damage to the central nervous system, mental retardation, or death. Medication, if given early, may help prevent or reduce lasting damage, but even with antiviral medication, this infection has serious consequences for most infected infants.
While neonatal herpes is a serious condition, it is also very rare. Less than 0.1% of babies born in the United States each year get neonatal herpes. By contrast, some 20-25% of pregnant women have genital herpes. This means that most women with genital herpes give birth to healthy babies.
Understanding the Risk
Babies are most at risk for neonatal herpes if the mother contracts genital herpes late in pregnancy. This is because a newly infected mother does not have antibodies against the virus, so there is no natural protection for the baby during birth. In addition, a new herpes infection is frequently active, so there is an increased possibility the virus will be present in the birth canal during delivery.
Women who have genital herpes before they become pregnant have a very low risk of transmitting the virus to their babies. This is because their immune systems make antibodies that are temporarily passed to the baby through the placenta. Even if herpes is active in the birth canal during delivery, the antibodies help protect the baby. In addition, if a mother knows she has genital herpes, her doctor or midwife can take steps to protect the baby.
In addition, if a mother knows she has genital herpes, her doctor or midwife can take steps to protect the baby.
Herpes can also be spread to the baby in the first weeks of life if he or she is kissed by someone with an active cold sore (oral herpes). In rare instances, herpes may be spread by touch, if someone touches an active cold sore and then immediately touches the baby. Again, simple precautions can be taken to protect an infant from this type of exposure. To protect your baby, don’t kiss him or her when you have a cold sore, and ask others not to. If you have a cold sore, wash your hands before touching the baby.
Managing Genital Herpes During Pregnancy
If you’re pregnant and you have genital herpes, you may be concerned about the risk of spreading the infection to your baby. Be reassured that the risk is extremely small—especially if you have had herpes for some time. The following steps can help make the risk even smaller:
- Talk with your obstetrician or midwife.
 Make sure they know you have genital herpes.
Make sure they know you have genital herpes. - At the time of labor, your healthcare provider should examine you early in labor with a strong light to detect any sores or signs of an outbreak. Let your provider know if you have any signs of an outbreak—itching, tingling, or pain.
- If you have an active outbreak at the time of delivery, the safest course is a Cesarean section to prevent the baby from coming into contact with virus in the birth canal. If you do not have an active outbreak, you can have a vaginal delivery.
- Ask your provider not to break the bag of waters around the baby unless necessary. The bag of waters may help protect the baby against any virus in the birth canal.
- Ask your provider not to use a fetal scalp monitor (scalp electrodes) during labor to monitor the baby’s heart rate unless medically necessary. This instrument makes tiny punctures in the baby’s scalp, which may allow herpes virus to enter. In most cases, an external monitor can be used instead.
- Ask that a vacuum or forceps not be used during delivery unless medically necessary. These instruments can also cause breaks in the baby’s scalp, allowing virus to enter.
- After birth, watch the baby closely for about three weeks. Symptoms of neonatal herpes may include a skin rash, fever, crankiness, or lack of appetite. While these can be symptoms of several mild illnesses, don’t wait to see if your baby will get better. Take him or her to the pediatrician at once. Be sure to tell the pediatrician you have genital herpes.
Remember, the odds are strongly in favor of your having a healthy baby.
Treatment while Pregnant
Many women wonder about taking antiviral medication during pregnancy to suppress outbreaks in the third trimester. The U.S. Food and Drug Administration (FDA) has approved no drug against herpes for this purpose. Nonetheless, acyclovir is used by some physicians to treat women with genital herpes at the end of pregnancy. Small studies suggest that acyclovir taken daily during the last month of pregnancy will prevent recurrences and, therefore, decrease the need for Cesarean sections, but some experts remain concerned about the safety of fetal exposure to the medication.
At the present time, acyclovir’s manufacturer does not recommend its use during pregnancy. On the other hand, the company has tracked the experiences of several hundred women who took the drug during pregnancy, some of them inadvertently, and the evidence to date suggests that acyclovir does not carry increased risk of birth defects or adverse pregnancy outcome. On the strength of this data, the use of daily, suppressive treatment during the last month of pregnancy is becoming increasingly common.
Women who Don’t Have Genital Herpes
The greatest risk of neonatal herpes is to babies whose mothers contract a genital infection late in pregnancy. While this is a rare occurrence, it does happen, and can cause a serious, even life-threatening, illness for the baby. The best way you can protect your baby is to know the facts about HSV and how to protect yourself. The first step may be finding out whether you already carry the virus.
You can talk to your healthcare provider about testing for genital herpes. If you test negative for genital herpes, but your partner has genital or oral herpes, you may acquire it unless you take steps to prevent transmission. The following steps can help protect you from getting an infection during pregnancy:
If you test negative for genital herpes, but your partner has genital or oral herpes, you may acquire it unless you take steps to prevent transmission. The following steps can help protect you from getting an infection during pregnancy:
- If your partner has genital herpes, abstain from sex during active outbreaks. Between outbreaks, use a condom from start to finish every time you have sexual contact, even if your partner has no symptoms. (HSV can spread when no symptoms are present.) Consider abstaining from sex (oral, vaginal, and anal) during the last trimester.
- Do not let your partner perform oral sex on you if your partner has an oral herpes (cold sores, fever blisters). This can give you genital herpes.
- If you don’t know whether your partner has genital HSV, you may wish to ask your partner to be tested.
- If you experience genital symptoms, or believe you have been exposed to genital HSV, tell your obstetrician or midwife at once. However, be aware that herpes can lie dormant for several years.
 What appears to be a new infection is occasionally an old one that is causing symptoms for the first time. Talk with your provider about the best way to protect your baby.
What appears to be a new infection is occasionally an old one that is causing symptoms for the first time. Talk with your provider about the best way to protect your baby. - When a pregnant woman does contract a new genital HSV infection during the last trimester, many providers will prescribe antiviral medication. If lesions or prodromal symptoms are present at the time of labor, a Cesarean section is the safest course to prevent the baby from coming into contact with virus in the birth canal. If the infection is acquired late in pregnancy, many providers would recommend a Cesarean section even without lesions present.
Reproductive Health Education CenterReproductive Health Education Center
Having genital herpes doesn't mean you can't have children. According to the American Public Health Association (ASHA), only 0.1% of cases of herpes are transmitted during pregnancy from mother to unborn child. Most women with genital herpes successfully carry out pregnancy and give birth to healthy children .
Breastfeeding during herpes recurrence is possible. Except when herpetic eruptions are located on the nipples or mammary gland. If your doctor prescribes oral antiviral drugs during breastfeeding, the question of the advisability of continuing breastfeeding during the course of suppressive therapy should be discussed with your doctor.
The initial episode of genital herpes is usually a tragedy during pregnancy. It is characterized by pronounced manifestations, tk. there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. As a rule, fetal death and miscarriage occur in the first trimester. Damage to the developing organs of the fetus, the occurrence of congenital deformities are possible. Infection in the III trimester, especially after 36 weeks of pregnancy, is fraught with damage to the nervous system of the fetus, skin, liver, spleen.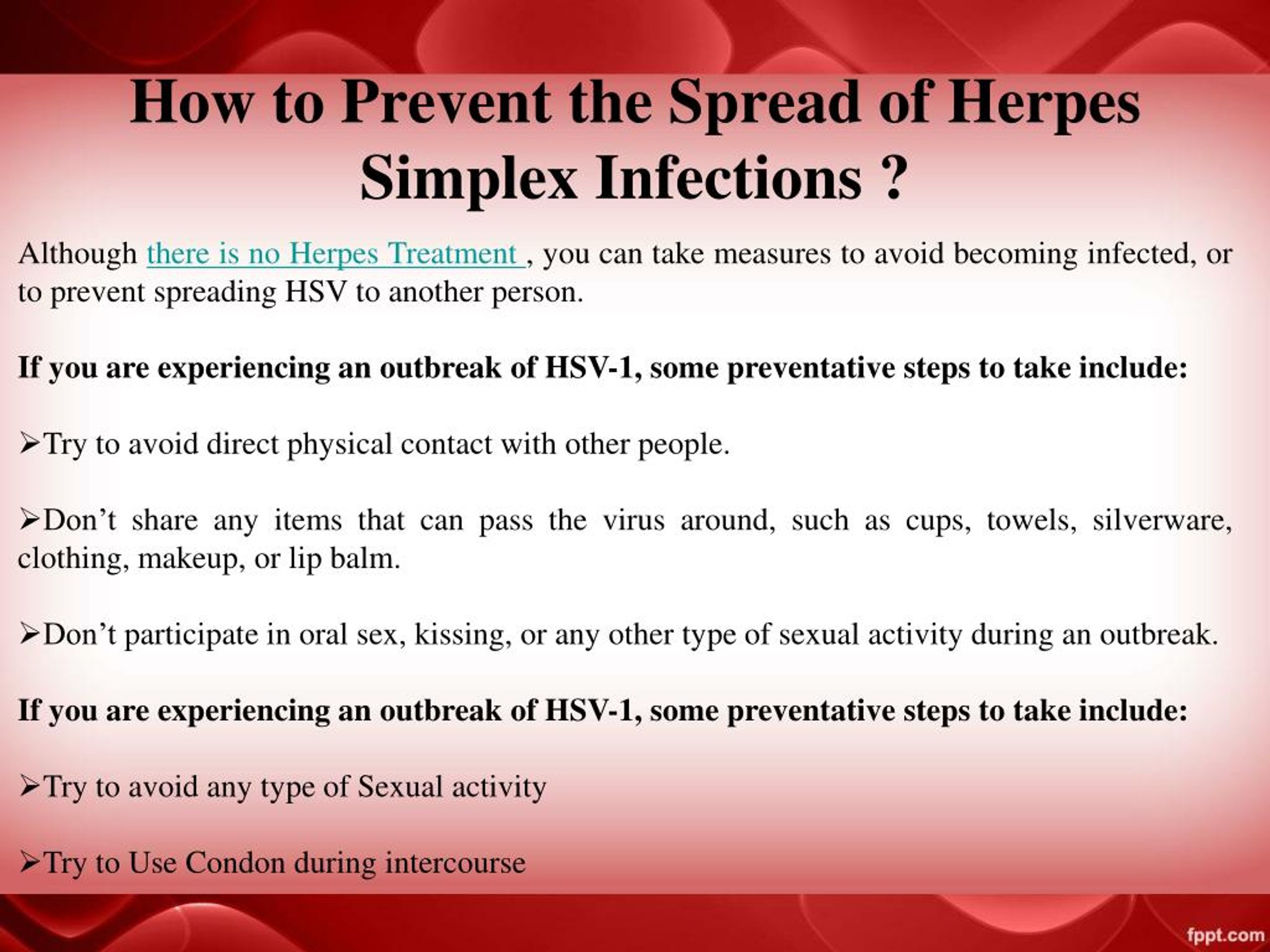 Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
HOW TO DETECT THAT I HAVE A PRIMARY EPISODE OF GENITAL HERPES?
What does primary episode mean? It means that in your life there has never been a recurrence of genital herpes and the body has not yet developed protective antibodies to HSV.
In some cases it is difficult to determine: what is it? Whether the first episode of genital herpes in life or the first recurrence with 90,003 visible symptoms of 90,004 genital herpes that was previously asymptomatic or with atypical symptoms. The fact is that in most people infected with HSV, the disease is almost asymptomatic.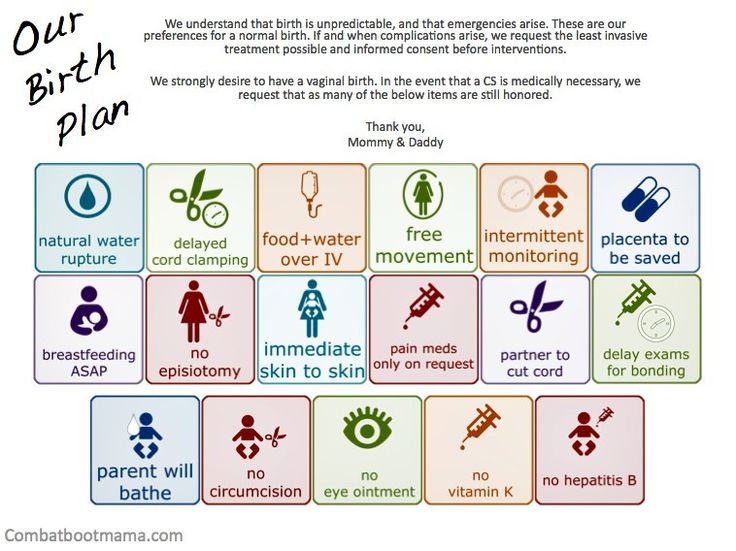 It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo.
It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo. If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
There are no specific methods for preventing the transmission of genital herpes during pregnancy. From non-specific, monogamous relationships, constant use of a condom can be recommended. If it is known that the father of the child is infected with genital herpes, and the mother is not, then you should either completely refrain from sexual activity during pregnancy (until the moment of delivery). Or a man should constantly use a condom + valaciclovir 1 tablet daily throughout the pregnancy. This measure will help to reduce the risk of transmission of genital herpes by 75%.
Should refrain from oral sex. Because if you have never had herpes of the lips in your life, and the husband or father of the child had it, then during cunniling he can bring the herpes simplex virus type I to your genitals. And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
Treatment with acyclovir and valtrex. However, these drugs do not always allow to achieve good success in treatment.
According to the US Centers for Disease Control, the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect fetal development. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Against the background of a primary episode of genital herpes, the loss of a desired pregnancy is a severe psychological trauma for both potential parents. But in any case, there is hope. The next pregnancy will proceed already against the background of recurrent genital herpes. After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
Recurrent genital herpes during pregnancy
As blasphemous as it may sound, but recurrent genital herpes is the most favorable option during pregnancy. If a woman has already had recurrences of genital herpes before the onset of this pregnancy, then the fetus is protected from infection by maternal antibodies that block the action of the herpes simplex virus. There is a 99% chance that your child will not get herpes.
STATISTICS:
During pregnancy, infection of a newborn with the herpes simplex virus from a mother with recurrent genital herpes occurs quite rarely: in approximately 0.02% of cases.
The risk of infection of a child in childbirth from a mother suffering from recurrent genital herpes is less than 1% (According to the study: Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
BEFORE PREGNANCY: Plan the onset of pregnancy , eliminate bad habits from your life, heal chronic diseases, take a course of restorative treatment, cure foci of chronic infection before pregnancy (sick teeth, sinusitis, gastritis).
In some cases, a woman cannot know whether she had recurrences of genital herpes before or not. This happens with herpes that occurs without symptoms or with an atypical course. In addition, it should be borne in mind that, unlike the stronger sex, the female genital organs are “not visible”. In order to find out if you have ever had a relapse, you should do a serological analysis. Donate blood for antibodies (immunoglobulins Ig G & Ig M) to HSV-1,2. If Ig G is present in the blood, then herpes is recurrent - herpes practically does not threaten pregnancy. The Ig G index is qualitative (higher than diagnostic titers).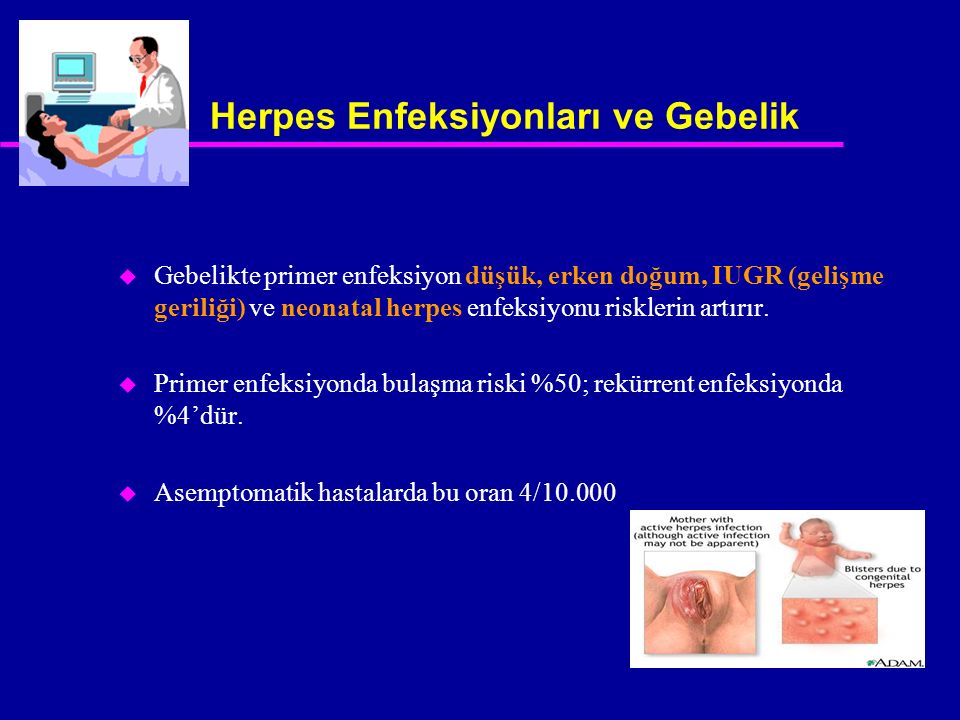 Regardless of the titer (the amount of Ig G & M), you can become pregnant.
Regardless of the titer (the amount of Ig G & M), you can become pregnant.
DURING PREGNANCY:
- When having sex always use a condom ;
- Avoid oral sex
If you get cold sores during pregnancy, you can transfer it to the penis of the father of your unborn child during oral sex. And he will transfer the infection to your genital tract with this member. This can lead to bad consequences for the child. On the other hand, if you allow your husband to cunniling and he has cold sores on his lips, he may bring a different type of herpes to your genitals. That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
PROPHYLAXIS DURING PREGNANCY:
To prevent recurrence during pregnancy after 36 weeks, your doctor may prescribe a course of preventive treatment with acyclovir or valaciclovir. During pregnancy, it is better to use acyclovir, manufactured by GlaxoSmithKline under the name Zovirax or Valtrex. Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
According to the US Centers for Disease Control, the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect fetal development. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Dynamic monitoring : Examination of pregnant women includes a mandatory three-time ultrasound examination: at 10-14 weeks of gestation, when the thickness of the nuchal space of the fetus is mainly assessed; at 20-24 weeks, ultrasound is performed to detect malformations and echographic markers of chromosomal diseases; an ultrasound examination at 32-34 weeks is performed in order to detect malformations with their late manifestation, as well as for the purpose of a functional assessment of the fetal condition. In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
Treatment: Only under medical supervision and prescription! Outwardly, you can use an ointment based on acyclovir. Ointments and creams are over-the-counter products. The ointment does not affect the fetus, because. it is not absorbed into the blood. To prevent rashes 2 weeks before delivery, the doctor may prescribe valacyclovir or acyclovir orally.
PREVENTION DURING DELIVERY:
Treatment of the soft birth canal with polyvidone iodine (Betadine, Vocadine) or other antiseptics during childbirth can reduce the risk of contracting neonatal herpes to the child. Genital herpes - abortion or childbirth?
Many women with recurrent genital herpes wonder how their illness might affect their unborn child.
The editor of the server received a letter describing a typical example of the illiterate approach of Soviet doctors to the management of pregnant women with genital herpes:
Professor D ***, from the Chelyabinsk Medical Academy, believes that it is highly undesirable to keep the pregnancy during an exacerbation of genital herpes in the early stages of pregnancy. He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
In developed countries, the optimal tactics for managing pregnant women with genital herpes has long been developed, based not on the private opinion of some “Professor D *** from the Chelyabinsk Medical Academy”, but on the data of long-term clinical studies and observations.
So that someone's subjective opinion does not lead you to an unnecessary abortion, we will tell you once again about what to do if you have herpes and pregnancy.
If a woman has the first time in her life Genital herpes recurs during pregnancy (primary genital herpes) or if the mother-to-be becomes infected with genital herpes during pregnancy, the fetus may be affected. The fact is that in this case, the mother's blood does not contain antibodies to the Herpes Simplex Virus - immunoglobulins G and Em (Ig G and Ig M), which block the pathological effect of the herpes simplex virus on fetal cells.
In the case of the first recurrence of genital herpes in a woman's life, the virus can penetrate the placenta and multiply in the tissues of the embryo or fetus, which leads to fetal death, miscarriage, congenital deformities, damage to the brain, liver, and other organs of the fetus, non-developing pregnancy. The risk of fetal damage in primary genital herpes is 75%.
If the first recurrence of genital herpes occurs 30 days before delivery, delivery by caesarean section is recommended.
From 36 weeks of pregnancy, a doctor may prescribe Zovirax tablets to prevent the recurrence of herpes.
To prevent infection with genital herpes during pregnancy, it is imperative to use a condom and avoid oral sex, i.e. a man should not caress the sexual organs of a pregnant woman with his mouth. The reverse situation is allowed.
If a woman had recurrences of genital herpes before pregnancy, then antiherpetic antibodies float in the pregnant woman's blood, which limit the infection and neutralize the virus. These antibodies pass through the placenta to the fetus, protecting it. Therefore, recurrent genital herpes is not so dangerous during pregnancy. In this case, due to herpes, there are no deformities and lesions of internal organs.
In recurrent genital herpes , the baby can become infected during childbirth, passing through the birth canal, where the herpes virus is present. The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
Recurrent genital herpes is not an indication for abortion.
And despite all our clarifications about the relative safety of recurrent genital herpes during pregnancy, sometimes you have to receive such letters: A woman with recurrent genital herpes writes: “And most importantly, herpes is just natural selection. Nature removes lepers, because their offspring are doomed to death, so I don’t even dream of children ... ”It is ignorant to consider yourself a leper and refuse the happiness of motherhood just because you have recurrent genital herpes (the most favorable form for bearing and childbirth). Although, it cannot be ruled out that this is our medical defect.
There is also such a diagnosis as non-primary genital herpes . What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
Use of immunomodulators during pregnancy
The server editor received a letter describing a typical clinical situation:
« I have a problem that requires urgent consultation. My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
In my opinion, the use of immunomodulators during pregnancy is IMPOSSIBLE:
* In this case, herpes on the lips of a woman cannot bring any harm to either the woman or the child.
*Long-term effect of immunomodulatory drugs on the fetus is unknown. As you know, some of these drugs, easily penetrating the placenta into the body of the fetus, can cause congenital deformities in the latter, disorders of the immune system, and increase the risk of developing cancer.
*If the mother is ill with recurrent genital herpes, this would also not be dangerous for the fetus, because it is protected by maternal antiviral antibodies.
*Immunobiological preparations: immunomodulators, vaccines, immunoglobulins are a foreign protein and can cause various complications during pregnancy.
Based on the foregoing, I urge women who during pregnancy are trying to be treated for herpes on the lips or genital herpes with immunomodulators, immunoglobulins and other immunobiological preparations to run away from such doctors and such savage methods of treatment. World during pregnancy immunobiological preparations are not used for the treatment of herpesvirus infections .
Author: Ivan Yuryevich Kokotkin, doctor
Source: http://www.herpes.ru/
dangerous "recidivist" (j-l "9 months", No. 5, author obstetrician-gynecologist CIR, Gevorkova E .V.)
Elena Valerievna Gevorkova , Obstetrician-gynecologist
Viral infections are of particular relevance during pregnancy, as they can affect the health of not only the expectant mother, but also the fetus.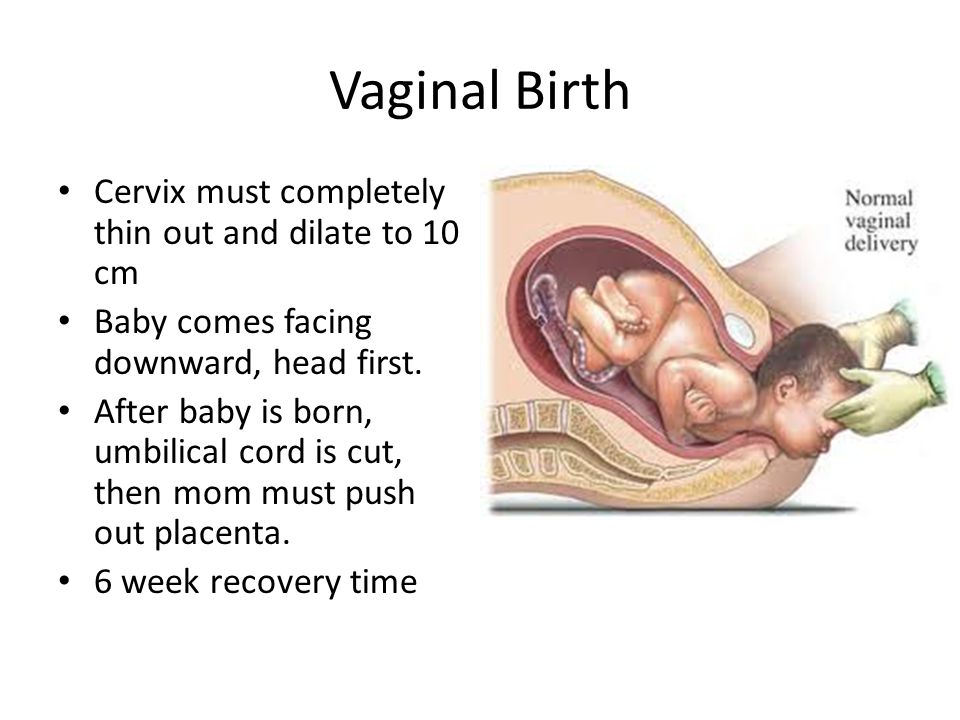 Herpes among them occupies one of the main places, since this disease is very common in pregnant women.
Herpes among them occupies one of the main places, since this disease is very common in pregnant women.
Herpes infection is a large group of infectious diseases caused by human herpes viruses. This is one of the most common human diseases. According to numerous studies, by the age of 18, more than 90% of the world's population is infected with one or more strains of herpes viruses. Among sexually transmitted infections, genital herpes ranks second after trichomoniasis.
A feature of herpes is its recurrent course. The dormant virus awakens when immunity is reduced, and pregnancy itself has the property of weakening the body's immune forces, since the woman's body bears a fetus that is half alien from an immunological point of view, which is impossible without reducing the intensity of a number of immunity links. That is why exacerbations of herpes during pregnancy occur quite often.
Many pregnant women panic when they discover they have blistering rashes, worrying about whether the infection will harm the baby. Most often, women know about the presence of herpes even before the onset of pregnancy, and the appearance of itchy vesicles filled with a clear liquid indicates a “revival” of the disease. But, fortunately, the dangerous impact of herpes is somewhat exaggerated, and there are not many situations when herpes can cause problems during pregnancy.
Most often, women know about the presence of herpes even before the onset of pregnancy, and the appearance of itchy vesicles filled with a clear liquid indicates a “revival” of the disease. But, fortunately, the dangerous impact of herpes is somewhat exaggerated, and there are not many situations when herpes can cause problems during pregnancy.
Manifestations of disease
The clinical manifestations of herpes depend on many factors - the type of virus, the location of the lesion, the age and immune status of the person. The classic symptomatology is the appearance of a group of small vesicles filled with a clear liquid. Herpes is characterized by the appearance of bubbles with the next relapse, always in the same place.
When localized in the upper half of the body, rashes occur mainly on the lips (the so-called "cold"), as well as on the mucous membrane of the nose, mouth, conjunctiva of the eyes, in the ear canal and on the eyelids.
In the genital herpes variant, the rash is localized on the labia, on the skin of the perineum, inner thighs, pubis, or around the anus.
A few days before the rash appears, there may be a feeling of itching and discomfort at the site of future rashes (herpetic "bell").
The rash is accompanied by discomfort, itching, burning, pain. Then the bubbles burst, in their place first sores are formed, then crusts. Herpetic sores are characteristically painful, and the crusts formed in their place disappear without a trace after 2-3 days, leaving no pigmentation or scars on the skin.
The general symptoms of the disease are very diverse: fever, swollen lymph nodes (often inguinal), joint and muscle pain, persistent migraines, irritability, lack of appetite, etc.
The typical clinical picture appears in no more than a third of cases of genital herpes carriers. Often, genital herpes is asymptomatic or without characteristic rashes.
The atypical course of herpes is more insidious: the absence of blisters is more than compensated by the variety of common manifestations, which often creates difficulties in making a correct diagnosis. Symptoms of atypical herpes - burning, cracks in the perineum, labia or anus, swelling, redness of the mucous membranes. In such cases, the diagnosis is often made incorrectly, or women who are confident in the presence of candidiasis (thrush) or bacterial vaginosis self-medicate to no avail.
Symptoms of atypical herpes - burning, cracks in the perineum, labia or anus, swelling, redness of the mucous membranes. In such cases, the diagnosis is often made incorrectly, or women who are confident in the presence of candidiasis (thrush) or bacterial vaginosis self-medicate to no avail.
The severity of any manifestations of herpes infection is determined by the state of immunity.
Varieties of the virus
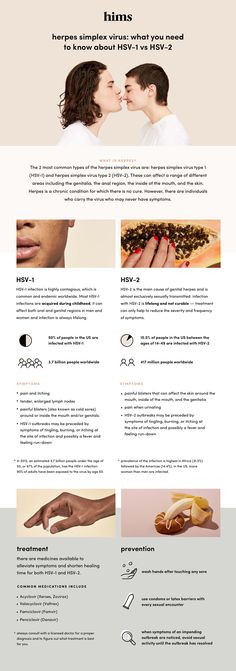
The most common are HSV 1 and 2 - the herpes simplex virus of the first and second types. HSV 1 most often manifests itself in the form of blistering rashes on the lips, damage to the eyes, mouth, nose is possible. The classic localization of HSV 2 (genital herpes) is the mucous membrane of the genitourinary tract. In some cases, the following phenomenon of cross-infection is observed: the culprit of herpetic eruptions of the upper half of the body is HSV 2 (genital) and vice versa - HSV 1 causes the development of infection of the lower half. As a rule, this is due to two reasons: a violation of elementary hygiene rules, when self-infection occurs - the transfer of the virus through the skin and mucous membranes, and oral-genital contacts.
Infection with herpes of the genital tract occurs mainly only through unprotected sexual contact. In rare cases, it is possible to transmit the infection through a kiss, the use of common dishes and linen. This is the so-called horizontal transmission path. With a vertical transmission route, the virus is transmitted from the mother to the fetus during pregnancy (when the child passes through the birth canal, provided that the herpes virus is present in the mucosa, that is, during childbirth at the time of exacerbation of the herpes virus infection). With the localization of foci on the lips, you can become infected through common dishes, towels and kisses. It should be noted that the risk of intrauterine infection of the fetus with primary herpes is 50%, with relapse - no more than 4%, during childbirth in the presence of rashes on the cervix and external genital organs - 90%.
How does the virus work?
Consider some features of the interaction of the virus with the human body.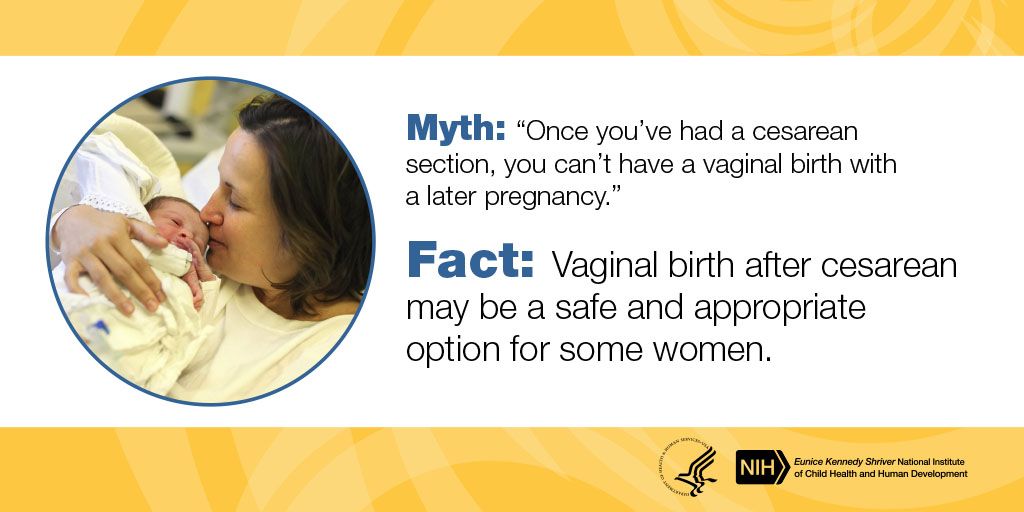
- Getting into the cell, the herpes virus (however, like any other virus) penetrates into its nucleus and causes the human cell to produce herpes viruses. Thus, the human cell "hand-made" produces new generations of viruses.
- Herpes simplex virus (HSV) spreads throughout the body via nerve fibers. For a period of downtime (remission), when a person does not feel the presence of a virus in the body, the virus chooses nerve plexuses - ganglia. And spends time there in anticipation of a decrease in the host's immunity. During this period, the carriage of herpes does not manifest itself in any way and it is almost impossible to detect it. HSV of the first type is deposited in the trigeminal ganglion (this is a special plexus of nerve fibers located in the cranial cavity), and HSV of the second type is deposited in the sacral ganglia (nerve plexuses of the pelvic organs).
When conditions favorable for the virus (hypothermia, stress, pregnancy) occur, it exits and further spreads through the skin and mucous membranes.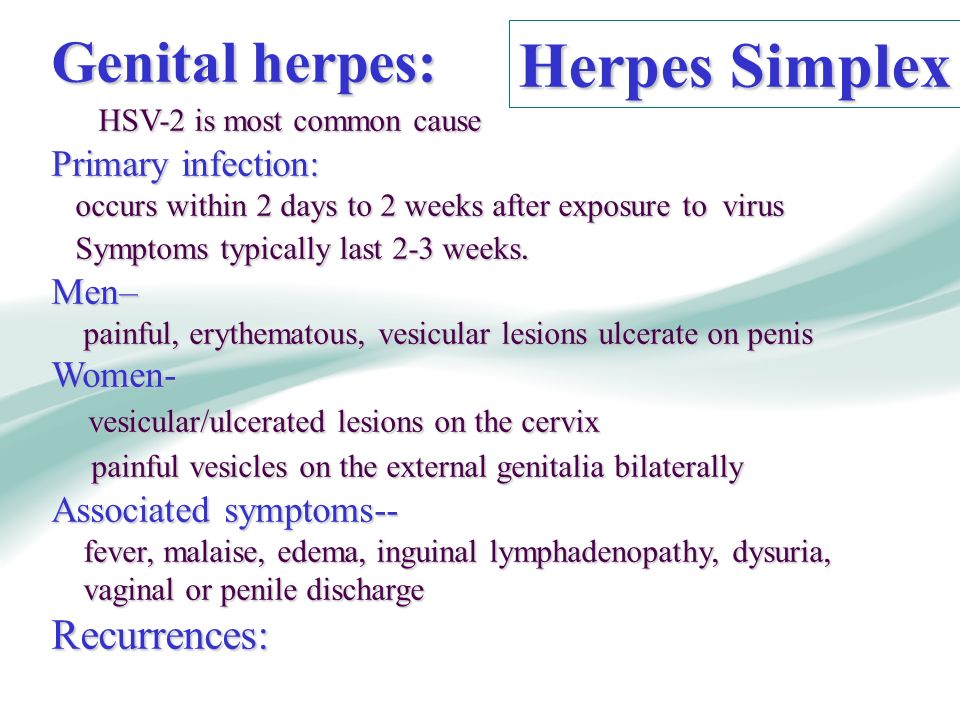
- Under the influence of various factors that damage the immune system, it is possible to weaken the controlling mechanisms of the "host" (human body) and the transition to active reproduction of the virus - this is how a relapse develops, which is manifested by an exacerbation of herpes.
Herpes exacerbations can be associated with two factors:
- already existing immunodeficiency, which is a trigger for the recurrence of herpes infection;
- the effect of the virus on the immune system itself. Prolonged presence of herpes in the body has a direct damaging effect on the cells of the immune system. Thus, a vicious circle develops: a weakened immune system triggers a recurrence of a herpes infection, and the herpes virus further aggravates the existing immunodeficiency.
Diagnosis
The diagnosis of herpes in a typical picture is not difficult for the doctor (and for the patient too). Clinical manifestations of herpetic infection are very bright: characteristic bubble rashes, recurrent course speak for themselves.
Clinical manifestations of herpetic infection are very bright: characteristic bubble rashes, recurrent course speak for themselves.
In cases of atypical herpes, virus carriers and during preventive examinations, laboratory diagnostic methods are of particular importance.
Main areas of laboratory research methods:
- Determination of the viral particles themselves. For this, electron microscopy methods are used using special smear staining methods, ELISA (enzymatic immunoassay) and PCR. The last method (polymerase chain reaction) is widely used and gives fairly accurate results - it is accessible, highly sensitive, and specific. As a rule, material for PCR analysis is taken by scraping (smear) from the cervix, vagina, urethra, scraping from the bottom of the wound or the contents of the vesicle are also examined. If a latent course of infection is suspected, urine and saliva are also examined.
- A blood test for antibodies to herpes simplex virus, which detects immunoglobulins of classes M and G.
 If a person is infected for the first time (primary infection) or at the time of diagnosis corresponds to the acute phase of the disease (relapse), then early antibodies of class M are detected in the blood.
If a person is infected for the first time (primary infection) or at the time of diagnosis corresponds to the acute phase of the disease (relapse), then early antibodies of class M are detected in the blood.
The determination of class G late immunoglobulins indicates that the organism's encounter with the virus has already occurred much earlier.
Particular attention is paid to laboratory diagnostics in case of newly diagnosed symptoms of herpes during pregnancy. This situation can correspond to both the primary episode and the first relapse (i.e., the body has already met with the virus before, but did not show any manifestations).
If there are IgG (late immunoglobulins) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo. If there is no Ig in the blood, but there is IgM, then it is necessary to show an extreme degree of alertness, since this is a laboratory confirmation of the primary episode.
Genital herpes and pregnancy
In the event of an exacerbation of type 1 herpes, it is only necessary to carefully follow preventive measures to prevent the transfer of the virus to the “below the belt” zone. With recurrent genital herpes or virus carriers, the risk to the fetus becomes minimal, since maternal antibodies help to cope with the virus even in cases of active relapse.
With recurrent genital herpes or virus carriers, the risk to the fetus becomes minimal, since maternal antibodies help to cope with the virus even in cases of active relapse.
Genital herpes is of particular relevance during pregnancy.
During pregnancy there is a powerful restructuring of all systems, including immunity. Pregnancy itself is a physiological immunosuppressive factor; there is a natural decrease in the protective properties of the body in order to prevent miscarriage. The reverse side of this immunological retreat is the manifestation of previously "dormant" infections, including genital herpes.
Obviously, when the problem of herpes arises, the expectant mother has a lot of worries. Fortunately, in most cases these worries are unfounded.
When is there really cause for concern? The greatest danger is the situation when infection with herpes occurs in a woman during pregnancy - the primary episode of genital herpes. This situation is characterized by pronounced manifestations, because.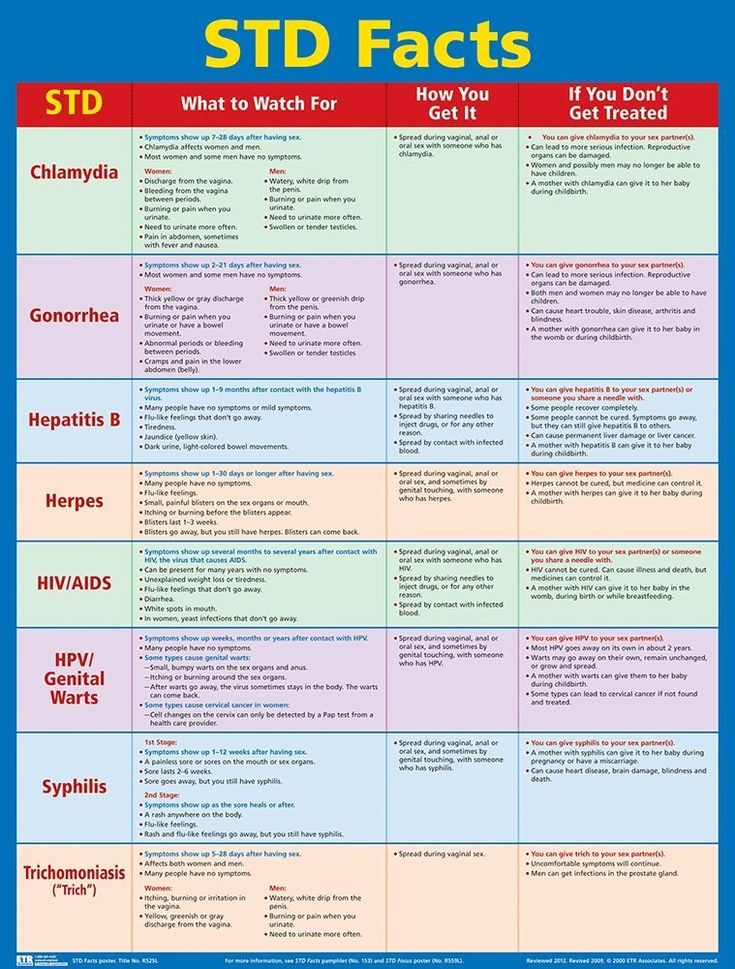 there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. Infection of the fetus in the first trimester of pregnancy leads to hydrocephalus (accumulation of fluid in the brain), heart defects, anomalies in the development of the gastrointestinal tract, etc. Such cases are extremely rare, since during the primary episode of herpes, as a rule, spontaneous abortion occurs before period of 10 weeks.
there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. Infection of the fetus in the first trimester of pregnancy leads to hydrocephalus (accumulation of fluid in the brain), heart defects, anomalies in the development of the gastrointestinal tract, etc. Such cases are extremely rare, since during the primary episode of herpes, as a rule, spontaneous abortion occurs before period of 10 weeks.
Infection in the second and third trimesters leads to the development of diseases of the liver (hepatitis), pancreas (pancreatitis), lungs (pneumonia), brain (encephalitis) in the fetus. Primary infection in the second half of pregnancy is almost always manifested by rashes, which allows for early diagnosis and timely treatment. With recurrent genital herpes or virus carriers, the risk to the fetus becomes minimal, since maternal antibodies help to cope with the virus even in cases of active relapse.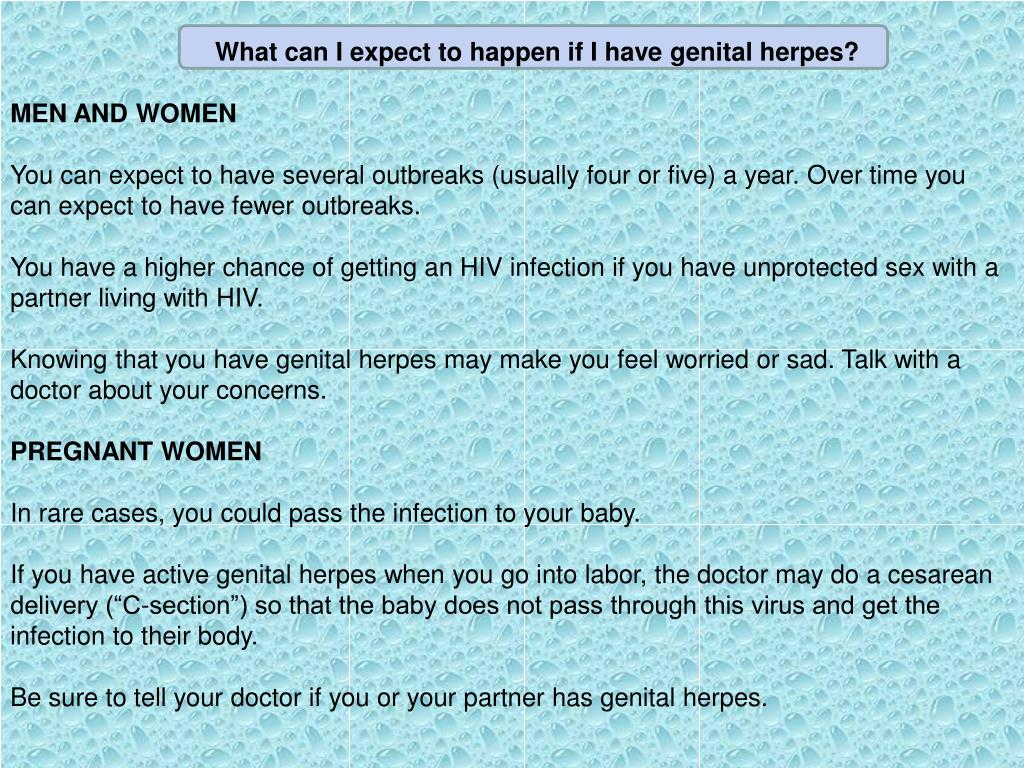
Treatment of herpes during pregnancy
In case of proven primary infection in early pregnancy, termination is discussed.
Treatment of herpes relapses during pregnancy and outside of it has no fundamental differences. In any case, the same goals are pursued: reducing the severity of symptoms (pain, itching, fever, etc.), reducing the time for wound healing, and preventing new exacerbations. It should be remembered that the sooner treatment is started, the greater the effect it will have. If treatment is started in the prodromal period (when the initial signs of the disease appear - tingling or slight itching at the site of future blisters, chills, malaise), then this will significantly help reduce the severity of herpes manifestations.
A feature of the treatment of herpes infection is the exact observance of the prescribed dose and regimen of medication. If the next dose of an antiviral drug is missed, then the herpes virus may have time to multiply during this period, which will lead to treatment failure.
The only drugs with proven efficacy in the treatment of herpes infection are specific virostatics - nucleoside analogues (ACICLOVIR, VALACIKLOVIR, PENCICLOVIR, FAMCICLOVIR).
Treatment of herpes infection during pregnancy involves the use of approved antiviral drugs (acyclovir ZOVIRAX and valaciclovir VALTREX) in the form of ointments, creams and tablets.
Simultaneously with antiviral drugs in complex treatment, immunomodulators (VIFERON), vitamins, physiotherapeutic methods, local antiseptics are used for faster wound healing.
Of course, the appropriateness and course of treatment is determined in each individual case. The situation of a combination of pregnancy and herpes should be under the vigilant supervision of a doctor and self-medication in these cases is simply unacceptable.
Herpes of the newborn
In what cases does the insidious virus still reach its goal and cause illness in newborns? In the vast majority of cases (90%), infection occurs by contact during passage through the birth canal. Intrauterine infection of a newborn is noted only in 5% of cases of herpes in newborns. Moreover, an important condition is the presence of a primary episode of genital herpes in the mother, in cases of asymptomatic carriage or recurrent herpes, infection of the fetus during childbirth occurs no more than in 4% of cases.
Intrauterine infection of a newborn is noted only in 5% of cases of herpes in newborns. Moreover, an important condition is the presence of a primary episode of genital herpes in the mother, in cases of asymptomatic carriage or recurrent herpes, infection of the fetus during childbirth occurs no more than in 4% of cases.
Symptoms and signs of herpes in babies appear as early as 2 weeks after birth. Herpes of the newborn is characterized by the presence of vesicles on the skin, mucous membranes (oral cavity, genital organs) and conjunctiva of the eyes. The more premature babies are born, the more difficult the infection is; in such cases, damage to the brain (herpetic encephalitis) is common.
Prevention
Unfortunately, there are no specific methods for the prevention of herpes. Prevention of infection at the planning stage, during pregnancy and after childbirth is exclusively preventive. The following measures apply:
- Examination of the body before pregnancy is an extremely important stage of pregnancy planning.
- Strengthening immunity during pregnancy.
- Physical activity (swimming, fitness, outdoor walks and other types of hardening), taking multivitamins, rational nutrition, a favorable emotional background - all this will help the immune system to cope with its work perfectly.
- A categorical rejection of bad habits (smoking, alcohol, drugs) - and not only because of the fear of a herpes infection ...
- Certain rules for sexual relations during pregnancy. If the expectant mother does not have late antibodies (IgG), and the sexual partner has signs of herpes or laboratory confirmation of herpes carriage, then it is recommended to refuse sexual intercourse, even using condoms. In other cases, the rules are less categorical: it is enough to use condoms and refrain from oral sex, since in this case, type 1 HSV can be transferred to the genitals and cross-infection of the genital organs, followed by infection of the fetus. If there are people with rashes on the lips surrounded by a pregnant woman, then you should pay special attention to the rules of personal hygiene (do not use common dishes, towels, avoid close contact - kiss, touch the rashes with your hands).
 This is especially true for women who do not have immunity to the herpes virus. It is possible to determine it by a blood test: with positive values of class G immunoglobulins, there is immunity, with negative ones - no.
This is especially true for women who do not have immunity to the herpes virus. It is possible to determine it by a blood test: with positive values of class G immunoglobulins, there is immunity, with negative ones - no. - As a prophylaxis for neonatal herpes in the presence of a recurrence of infection in the mother 4 weeks before delivery, delivery by caesarean section is indicated. This is a common tactic aimed at eliminating the slightest possibility of infection of the child during childbirth. However, according to many studies, even in the case of physiological childbirth, there is no serious danger, since the antibodies present in the mother's body pass through the placenta to the fetus and protect it during pregnancy, childbirth and after childbirth. However, today the presence of rashes on the cervix and genital tract at the time of delivery is an indication for operative delivery. In cases of herpes carriage without activation, childbirth is carried out naturally.