Can early pregnancy cause herpes outbreak
Genital herpes and pregnancy: Understanding the risks | Your Pregnancy Matters
Be honest with your doctor about your history with herpes – or if you suspect you may have herpes. This allows them to take additional precautions beyond what they might normally provide during pregnancy, labor, and delivery to safeguard your baby from contracting the virus.Genital herpes is one of the most common health conditions in the U.S. The Centers for Disease Control and Prevention (CDC) estimates that 1 in 6 people between the ages of 14 and 49 have it. Approximately 22% of pregnant women in the U.S. have genital herpes. Two percent contract it during pregnancy – that's 1 in 50 pregnant women.
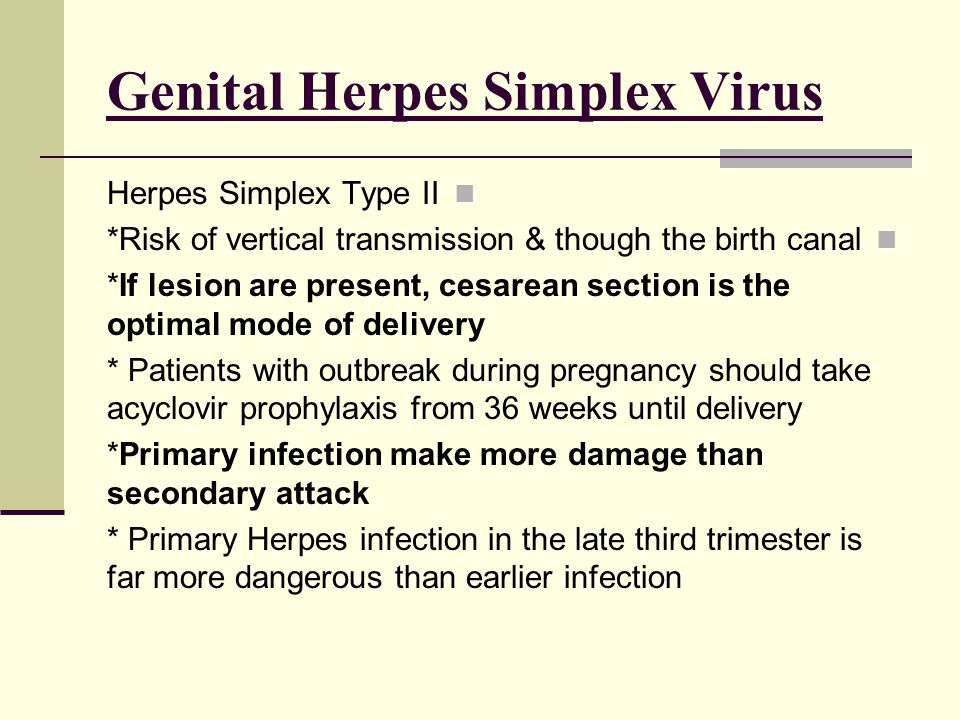
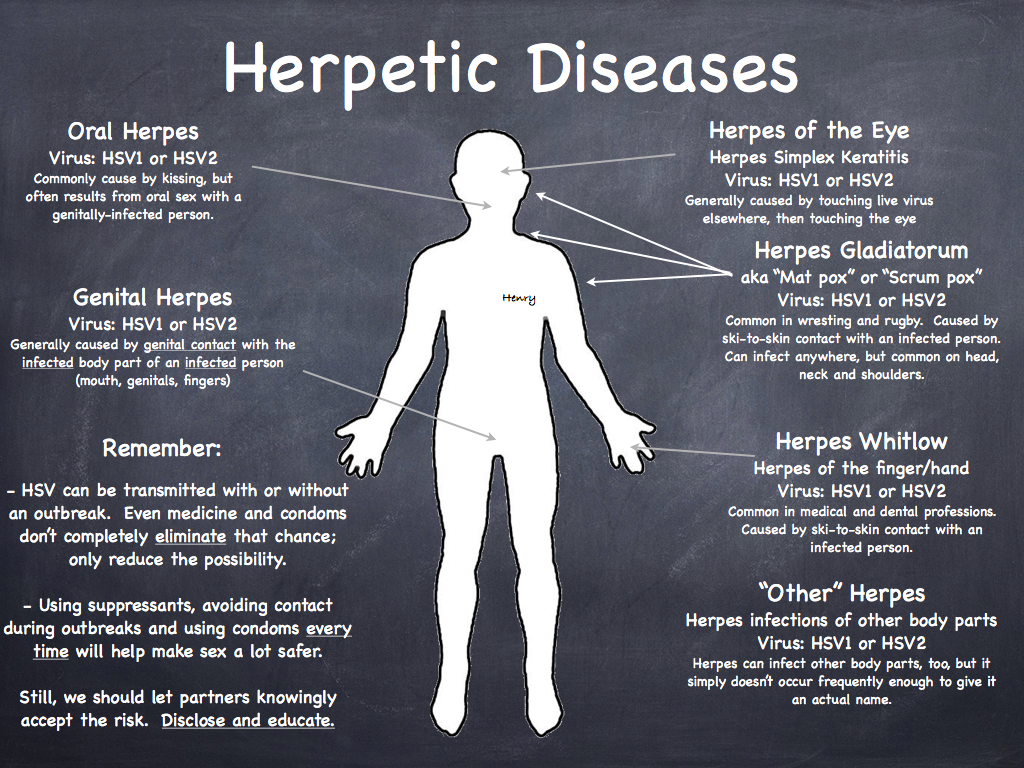
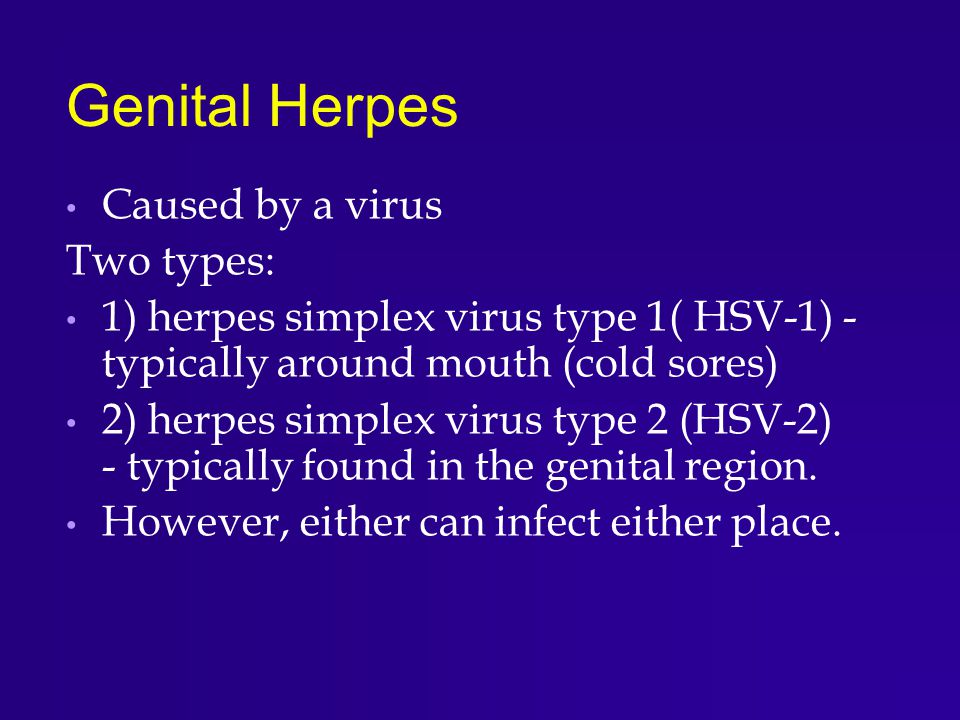
Two viral strains can cause genital herpes. HSV-2 (herpes simplex virus) is the most common and typically spreads through sexual contact. HSV-1, which is best known for causing cold sores, can also produce genital lesions (blisters or open sores). More than half of adults in America get HSV-1 at some point in their lives.
Herpes is generally manageable in adults. However, it can cause serious health problems in newborns. During delivery, your baby may be exposed to the virus, even if you are not having an outbreak.
Herpes infection occurs in less than 1% of births, but it can cause severe illness in newborns, such as:
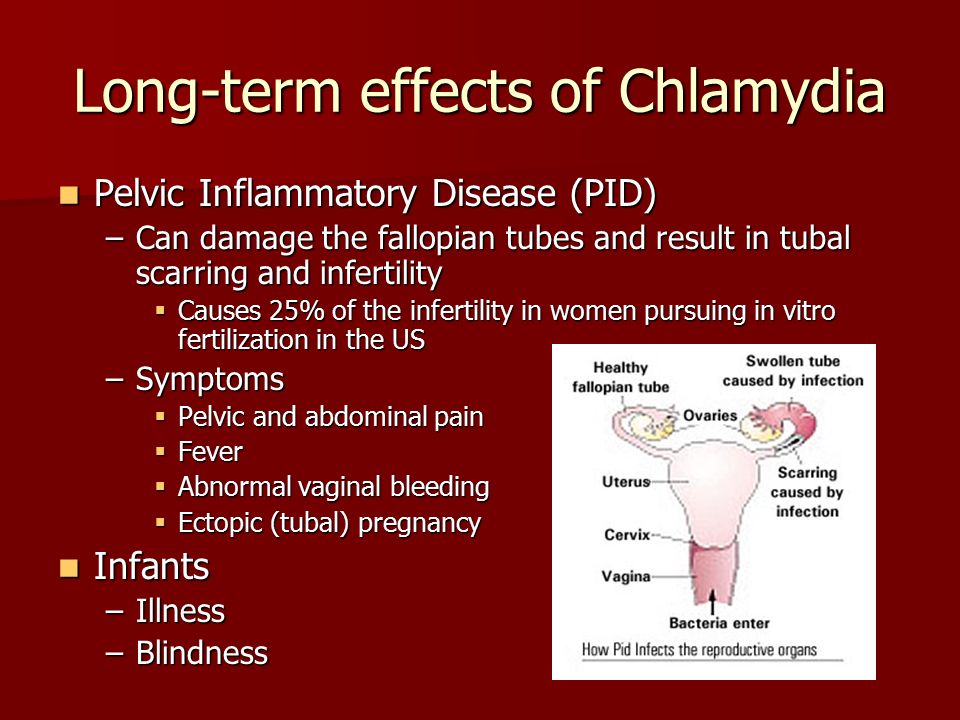
- Blindness
- Deafness
- Seizures
- Serious infections, such as viral meningitis
- Recurrent sores on the skin, eyes, genitals, or mouth
- organ damage, including to the liver, lungs, and heart
Tell your doctor if you or your partner have herpes or if you may have been exposed. By knowing, we can take extra precautions to reduce your baby's risk of infection during delivery and in their first few weeks at home. If you’re not certain but think you may have had herpes in the past, we can do a blood test to determine whether you have had the infection.
If you are concerned about privacy, we will note in your chart not to discuss the condition in front of anyone at your appointments – we are happy to accommodate this common request.
"Tell your doctor if you or your partner have herpes or if you may have been exposed. By knowing, we can take extra precautions to reduce your baby's risk of infection during delivery and in their first few weeks at home."
Robyn Horsager-Boeher, M.D.
How can I manage herpes during pregnancy?
There is no evidence to suggest pregnancy causes flare-ups. The American College of Obstetricians and Gynecologists says 75% of pregnant women who have herpes, however, can expect to have an outbreak during pregnancy.
During pregnancy, you should watch for symptoms of the virus becoming active, such as tingling, itching, or burning around where the sore will eventually appear.
If you have a history of herpes (or your blood test is positive), your provider may prescribe an antiviral medication such as acyclovir (Valtrex) to reduce the risk of spreading the virus or having an outbreak around the time of your delivery.
We typically recommend starting an antiviral at 36 weeks or sooner if you are at risk for preterm birth. The antiviral medications are safe during pregnancy. In fact, we can give the same medications to your baby if needed.
Will I need a C-section if I have herpes?
A cesarean (C-section) can’t completely prevent herpes transmission. But it does substantially decrease the risk to your baby if you have a lesion or report typical symptoms by bypassing contact with the vagina and labia.
Once you go into labor, we’ll carefully examine you for genital lesions. If we see something suspicious, we will recommend a C-section.
If you have no symptoms and no sores in the genital region, a vaginal delivery may be safe. Lesions can sometimes appear in other areas, such as the legs or back. If this is the case, we’ll cover them to make sure the baby doesn’t come into contact with them.
If this is the case, we’ll cover them to make sure the baby doesn’t come into contact with them.
How can I protect my newborn from getting herpes?
If your partner has herpes and you don’t, do not have sex and oral sex the last few weeks of pregnancy. Condoms can reduce the risk of transmission but aren’t 100% effective. There’s no reason to risk a new infection close to delivery.
In the unlikely event your baby has been exposed, we’ll treat the baby with antiviral medications. HSV can’t be passed through breast milk, so unless you have sores or lesion on your breasts, breastfeeding is safe.
With visitors, do not allow anyone who has a cold sore or has had one recently to hold your baby. Same goes for people who have a cold or virus. Insist that anyone who wants to hold or touch your newborn wash their hands first – this should be the norm anyway due to COVID-19.
Genital herpes is a common condition, and we are well-equipped to help reduce your baby's risks. If you or your partner has a history of herpes, talk with your Ob/Gyn. We are eager to help you have a safe pregnancy and delivery.
If you or your partner has a history of herpes, talk with your Ob/Gyn. We are eager to help you have a safe pregnancy and delivery.
To visit with an Ob/Gyn, call 214-645-8300 or request an appointment online.
Herpes & Pregnancy – American Sexual Health Association
If a woman with genital herpes has virus present in the birth canal during delivery, herpes simplex virus (HSV) can be spread to an infant, causing neonatal herpes, a serious and sometimes fatal condition. Neonatal herpes can cause an overwhelming infection resulting in lasting damage to the central nervous system, mental retardation, or death. Medication, if given early, may help prevent or reduce lasting damage, but even with antiviral medication, this infection has serious consequences for most infected infants.
While neonatal herpes is a serious condition, it is also very rare. Less than 0.1% of babies born in the United States each year get neonatal herpes. By contrast, some 20-25% of pregnant women have genital herpes. This means that most women with genital herpes give birth to healthy babies.
By contrast, some 20-25% of pregnant women have genital herpes. This means that most women with genital herpes give birth to healthy babies.
Understanding the Risk
Babies are most at risk for neonatal herpes if the mother contracts genital herpes late in pregnancy. This is because a newly infected mother does not have antibodies against the virus, so there is no natural protection for the baby during birth. In addition, a new herpes infection is frequently active, so there is an increased possibility the virus will be present in the birth canal during delivery.
Women who have genital herpes before they become pregnant have a very low risk of transmitting the virus to their babies. This is because their immune systems make antibodies that are temporarily passed to the baby through the placenta. Even if herpes is active in the birth canal during delivery, the antibodies help protect the baby. In addition, if a mother knows she has genital herpes, her doctor or midwife can take steps to protect the baby.
Herpes can also be spread to the baby in the first weeks of life if he or she is kissed by someone with an active cold sore (oral herpes). In rare instances, herpes may be spread by touch, if someone touches an active cold sore and then immediately touches the baby. Again, simple precautions can be taken to protect an infant from this type of exposure. To protect your baby, don’t kiss him or her when you have a cold sore, and ask others not to. If you have a cold sore, wash your hands before touching the baby.
Managing Genital Herpes During Pregnancy
If you’re pregnant and you have genital herpes, you may be concerned about the risk of spreading the infection to your baby. Be reassured that the risk is extremely small—especially if you have had herpes for some time. The following steps can help make the risk even smaller:
- Talk with your obstetrician or midwife. Make sure they know you have genital herpes.
- At the time of labor, your healthcare provider should examine you early in labor with a strong light to detect any sores or signs of an outbreak.
 Let your provider know if you have any signs of an outbreak—itching, tingling, or pain.
Let your provider know if you have any signs of an outbreak—itching, tingling, or pain. - If you have an active outbreak at the time of delivery, the safest course is a Cesarean section to prevent the baby from coming into contact with virus in the birth canal. If you do not have an active outbreak, you can have a vaginal delivery.
- Ask your provider not to break the bag of waters around the baby unless necessary. The bag of waters may help protect the baby against any virus in the birth canal.
- Ask your provider not to use a fetal scalp monitor (scalp electrodes) during labor to monitor the baby’s heart rate unless medically necessary. This instrument makes tiny punctures in the baby’s scalp, which may allow herpes virus to enter. In most cases, an external monitor can be used instead.
- Ask that a vacuum or forceps not be used during delivery unless medically necessary. These instruments can also cause breaks in the baby’s scalp, allowing virus to enter.
- After birth, watch the baby closely for about three weeks.
 Symptoms of neonatal herpes may include a skin rash, fever, crankiness, or lack of appetite. While these can be symptoms of several mild illnesses, don’t wait to see if your baby will get better. Take him or her to the pediatrician at once. Be sure to tell the pediatrician you have genital herpes.
Symptoms of neonatal herpes may include a skin rash, fever, crankiness, or lack of appetite. While these can be symptoms of several mild illnesses, don’t wait to see if your baby will get better. Take him or her to the pediatrician at once. Be sure to tell the pediatrician you have genital herpes.
Remember, the odds are strongly in favor of your having a healthy baby.
Treatment while Pregnant
Many women wonder about taking antiviral medication during pregnancy to suppress outbreaks in the third trimester. The U.S. Food and Drug Administration (FDA) has approved no drug against herpes for this purpose. Nonetheless, acyclovir is used by some physicians to treat women with genital herpes at the end of pregnancy. Small studies suggest that acyclovir taken daily during the last month of pregnancy will prevent recurrences and, therefore, decrease the need for Cesarean sections, but some experts remain concerned about the safety of fetal exposure to the medication.
At the present time, acyclovir’s manufacturer does not recommend its use during pregnancy. On the other hand, the company has tracked the experiences of several hundred women who took the drug during pregnancy, some of them inadvertently, and the evidence to date suggests that acyclovir does not carry increased risk of birth defects or adverse pregnancy outcome. On the strength of this data, the use of daily, suppressive treatment during the last month of pregnancy is becoming increasingly common.
On the other hand, the company has tracked the experiences of several hundred women who took the drug during pregnancy, some of them inadvertently, and the evidence to date suggests that acyclovir does not carry increased risk of birth defects or adverse pregnancy outcome. On the strength of this data, the use of daily, suppressive treatment during the last month of pregnancy is becoming increasingly common.
Women who Don’t Have Genital Herpes
The greatest risk of neonatal herpes is to babies whose mothers contract a genital infection late in pregnancy. While this is a rare occurrence, it does happen, and can cause a serious, even life-threatening, illness for the baby. The best way you can protect your baby is to know the facts about HSV and how to protect yourself. The first step may be finding out whether you already carry the virus.
You can talk to your healthcare provider about testing for genital herpes. If you test negative for genital herpes, but your partner has genital or oral herpes, you may acquire it unless you take steps to prevent transmission.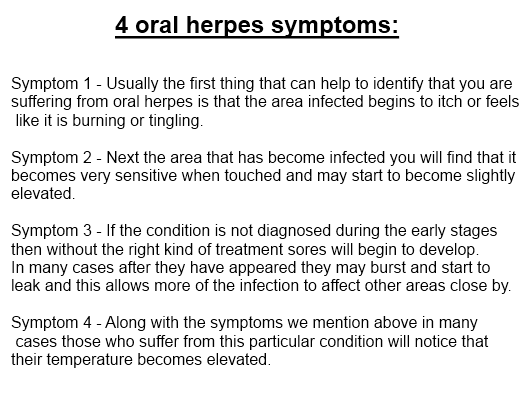 The following steps can help protect you from getting an infection during pregnancy:
The following steps can help protect you from getting an infection during pregnancy:
- If your partner has genital herpes, abstain from sex during active outbreaks. Between outbreaks, use a condom from start to finish every time you have sexual contact, even if your partner has no symptoms. (HSV can spread when no symptoms are present.) Consider abstaining from sex (oral, vaginal, and anal) during the last trimester.
- Do not let your partner perform oral sex on you if your partner has an oral herpes (cold sores, fever blisters). This can give you genital herpes.
- If you don’t know whether your partner has genital HSV, you may wish to ask your partner to be tested.
- If you experience genital symptoms, or believe you have been exposed to genital HSV, tell your obstetrician or midwife at once. However, be aware that herpes can lie dormant for several years. What appears to be a new infection is occasionally an old one that is causing symptoms for the first time.
 Talk with your provider about the best way to protect your baby.
Talk with your provider about the best way to protect your baby. - When a pregnant woman does contract a new genital HSV infection during the last trimester, many providers will prescribe antiviral medication. If lesions or prodromal symptoms are present at the time of labor, a Cesarean section is the safest course to prevent the baby from coming into contact with virus in the birth canal. If the infection is acquired late in pregnancy, many providers would recommend a Cesarean section even without lesions present.
Reproductive Health Education CenterReproductive Health Education Center
Having genital herpes doesn't mean you can't have children. According to the American Public Health Association (ASHA), only 0.1% of cases of herpes are transmitted during pregnancy from mother to unborn child. Most women with genital herpes successfully carry out pregnancy and give birth to healthy children .
Breastfeeding during herpes recurrence is possible. Except when herpetic eruptions are located on the nipples or mammary gland. If your doctor prescribes oral antiviral drugs during breastfeeding, the question of the advisability of continuing breastfeeding during the course of suppressive therapy should be discussed with your doctor.
Except when herpetic eruptions are located on the nipples or mammary gland. If your doctor prescribes oral antiviral drugs during breastfeeding, the question of the advisability of continuing breastfeeding during the course of suppressive therapy should be discussed with your doctor.
The initial episode of genital herpes is usually a tragedy during pregnancy. It is characterized by pronounced manifestations, tk. there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. As a rule, fetal death and miscarriage occur in the first trimester. Damage to the developing organs of the fetus, the occurrence of congenital deformities are possible. Infection in the III trimester, especially after 36 weeks of pregnancy, is fraught with damage to the nervous system of the fetus, skin, liver, spleen. Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
HOW TO DETECT THAT I HAVE A PRIMARY EPISODE OF GENITAL HERPES?
What does primary episode mean? It means that in your life there has never been a recurrence of genital herpes and the body has not yet developed protective antibodies to HSV.
In some cases it is difficult to determine: what is it? Whether the first episode of genital herpes in life or the first recurrence with 90,003 visible symptoms of 90,004 genital herpes that was previously asymptomatic or with atypical symptoms. The fact is that in most people infected with HSV, the disease is almost asymptomatic. It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo. If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo. If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
There are no specific methods for preventing the transmission of genital herpes during pregnancy. From non-specific, monogamous relationships, constant use of a condom can be recommended. If it is known that the father of the child is infected with genital herpes, and the mother is not, then you should either completely refrain from sexual activity during pregnancy (until the moment of delivery). Or a man should constantly use a condom + valaciclovir 1 tablet daily throughout the pregnancy. This measure will help to reduce the risk of transmission of genital herpes by 75%.
From non-specific, monogamous relationships, constant use of a condom can be recommended. If it is known that the father of the child is infected with genital herpes, and the mother is not, then you should either completely refrain from sexual activity during pregnancy (until the moment of delivery). Or a man should constantly use a condom + valaciclovir 1 tablet daily throughout the pregnancy. This measure will help to reduce the risk of transmission of genital herpes by 75%.
Should refrain from oral sex. Because if you have never had herpes of the lips in your life, and the husband or father of the child had it, then during cunniling he can bring the herpes simplex virus type I to your genitals. And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
Treatment with acyclovir and valtrex. However, these drugs do not always allow to achieve good success in treatment.
However, these drugs do not always allow to achieve good success in treatment.
According to the US Centers for Disease Control, the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect fetal development. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Against the background of a primary episode of genital herpes, the loss of a desired pregnancy is a severe psychological trauma for both potential parents. But in any case, there is hope. The next pregnancy will proceed already against the background of recurrent genital herpes. After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
Recurrent genital herpes during pregnancy
As blasphemous as it may sound, but recurrent genital herpes is the most favorable option during pregnancy.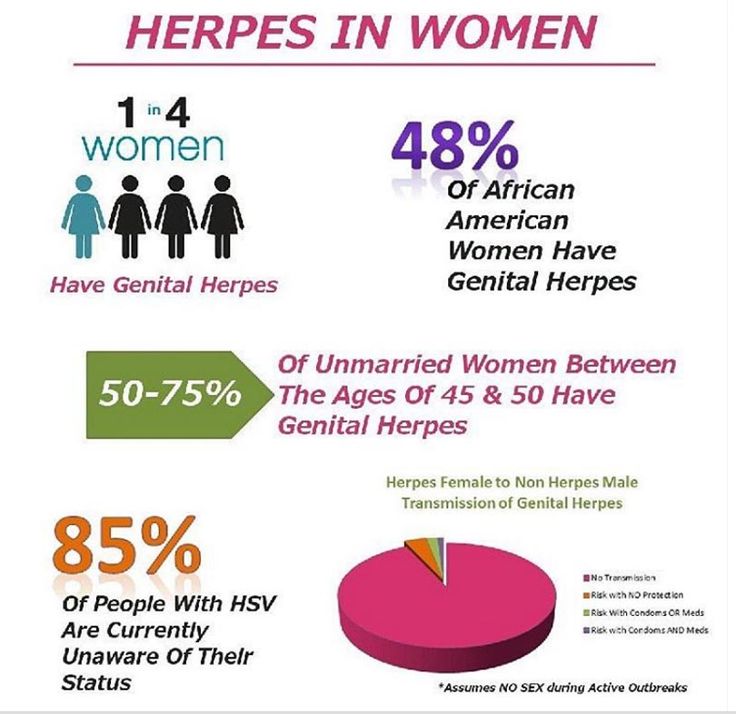 If a woman before the onset of this pregnancy already had relapses of genital herpes, then the fetus is protected from infection by maternal antibodies that block the action of the herpes simplex virus. There is a 99% chance that your child will not get herpes.
If a woman before the onset of this pregnancy already had relapses of genital herpes, then the fetus is protected from infection by maternal antibodies that block the action of the herpes simplex virus. There is a 99% chance that your child will not get herpes.
STATISTICS:
During pregnancy, infection of a newborn with herpes simplex virus from a mother with recurrent genital herpes occurs quite rarely: in approximately 0.02% of cases.
Less than 1% risk of infection of a child in childbirth from a mother with recurrent genital herpes (According to the study: Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
BEFORE PREGNANCY: Plan the onset of pregnancy , eliminate bad habits from your life, heal chronic diseases, take a course of restorative treatment, cure foci of chronic infection before pregnancy (sick teeth, sinusitis, gastritis).
In some cases, a woman cannot know whether she had recurrences of genital herpes before or not.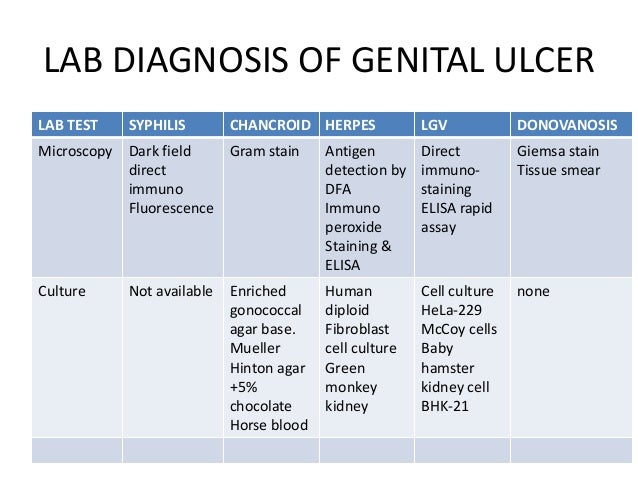 This happens with herpes that occurs without symptoms or with an atypical course. In addition, it should be borne in mind that, unlike the stronger sex, the female genital organs are “not visible”. In order to find out if you have ever had a relapse, you should do a serological analysis. Donate blood for antibodies (immunoglobulins Ig G & Ig M) to HSV-1,2. If Ig G is present in the blood, then herpes is recurrent - herpes practically does not threaten pregnancy. The Ig G index is qualitative (higher than diagnostic titers). Regardless of the titer (the amount of Ig G & M), you can become pregnant.
This happens with herpes that occurs without symptoms or with an atypical course. In addition, it should be borne in mind that, unlike the stronger sex, the female genital organs are “not visible”. In order to find out if you have ever had a relapse, you should do a serological analysis. Donate blood for antibodies (immunoglobulins Ig G & Ig M) to HSV-1,2. If Ig G is present in the blood, then herpes is recurrent - herpes practically does not threaten pregnancy. The Ig G index is qualitative (higher than diagnostic titers). Regardless of the titer (the amount of Ig G & M), you can become pregnant.
DURING PREGNANCY:
- When having sex always use a condom ;
- Avoid oral sex
If you get cold sores during pregnancy, you can transfer it to the penis of the father of your unborn child during oral sex. And he will transfer the infection to your genital tract with this member. This can lead to bad consequences for the child. On the other hand, if you allow your husband to cunniling and he has cold sores on his lips, he may bring a different type of herpes to your genitals. That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
PROPHYLAXIS DURING PREGNANCY:
To prevent recurrence during pregnancy after 36 weeks, your doctor may prescribe a course of preventive treatment with acyclovir or valaciclovir. During pregnancy, it is better to use acyclovir, manufactured by GlaxoSmithKline under the name Zovirax or Valtrex. Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
According to the US Centers for Disease Control, the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect fetal development. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Dynamic monitoring : Examination of pregnant women includes a mandatory three-time ultrasound examination: at 10-14 weeks of gestation, when the thickness of the nuchal space of the fetus is mainly assessed; at 20-24 weeks, ultrasound is performed to detect malformations and echographic markers of chromosomal diseases; an ultrasound examination at 32-34 weeks is performed in order to detect malformations with their late manifestation, as well as for the purpose of a functional assessment of the fetal condition. In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
Treatment: Only under medical supervision and prescription! Outwardly, you can use an ointment based on acyclovir. Ointments and creams are over-the-counter products. The ointment does not affect the fetus, because. it is not absorbed into the blood. To prevent rashes 2 weeks before delivery, the doctor may prescribe valacyclovir or acyclovir orally.
PREVENTION DURING DELIVERY:
Treatment of the soft birth canal with polyvidone iodine (Betadine, Vocadine) or other antiseptics during childbirth can reduce the risk of contracting neonatal herpes to the child. Genital herpes - abortion or childbirth?
Many women with recurrent genital herpes wonder how their illness might affect their unborn child.
The editor of the server received a letter describing a typical example of the illiterate approach of Soviet doctors to the management of pregnant women with genital herpes:
Professor D ***, from the Chelyabinsk Medical Academy, believes that it is highly undesirable to keep the pregnancy during an exacerbation of genital herpes in the early stages of pregnancy. He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
In developed countries, the optimal tactics for managing pregnant women with genital herpes has long been developed, based not on the private opinion of some “Professor D *** from the Chelyabinsk Medical Academy”, but on the data of long-term clinical studies and observations.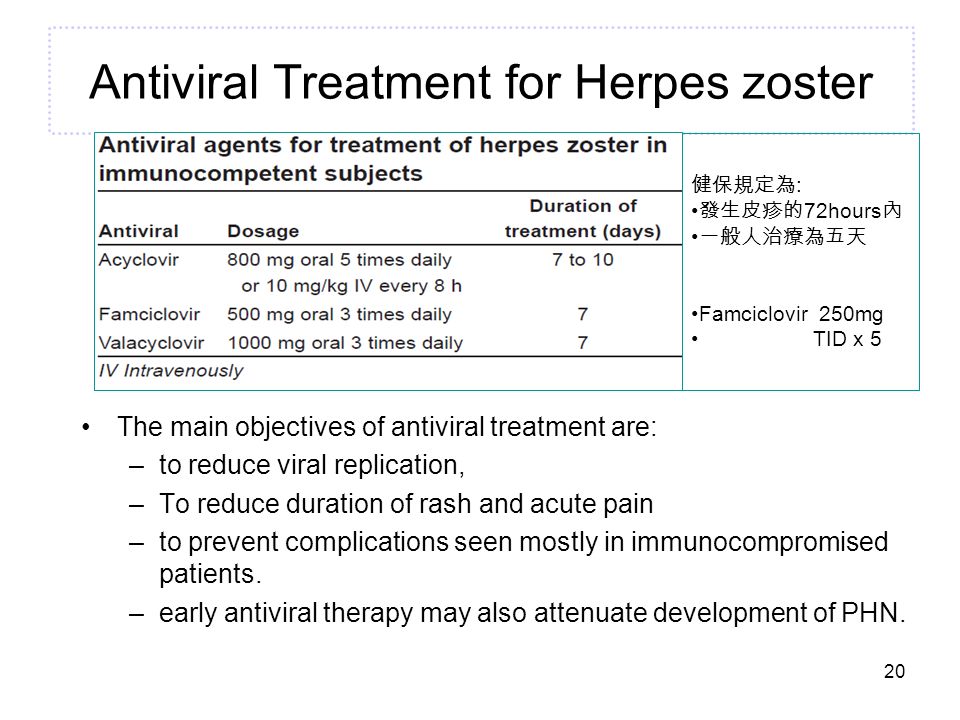
So that someone's subjective opinion does not lead you to an unnecessary abortion, we will tell you once again about what to do if you have herpes and pregnancy.
If a woman has the first time in her life Genital herpes recurs during pregnancy (primary genital herpes) or if the mother-to-be becomes infected with genital herpes during pregnancy, the fetus may be affected. The fact is that in this case, the mother's blood does not contain antibodies to the Herpes Simplex Virus - immunoglobulins G and Em (Ig G and Ig M), which block the pathological effect of the herpes simplex virus on fetal cells.
In the case of the first recurrence of genital herpes in a woman's life, the virus can penetrate the placenta and multiply in the tissues of the embryo or fetus, which leads to fetal death, miscarriage, congenital deformities, damage to the brain, liver, and other organs of the fetus, non-developing pregnancy. The risk of fetal damage in primary genital herpes is 75%.
If the first recurrence of genital herpes occurs 30 days before delivery, delivery by caesarean section is recommended.
From 36 weeks of pregnancy, the doctor may prescribe Zovirax tablets to prevent the recurrence of herpes.
To prevent infection with genital herpes during pregnancy, it is imperative to use a condom and avoid oral sex, i.e. a man should not caress the sexual organs of a pregnant woman with his mouth. The reverse situation is allowed.
If a woman had recurrences of genital herpes before pregnancy, then antiherpetic antibodies float in the pregnant woman's blood, which limit the infection and neutralize the virus. These antibodies pass through the placenta to the fetus, protecting it. Therefore, recurrent genital herpes is not so dangerous during pregnancy. In this case, due to herpes, there are no deformities and lesions of internal organs.
In recurrent genital herpes , the baby can become infected during childbirth, passing through the birth canal, where the herpes virus is present.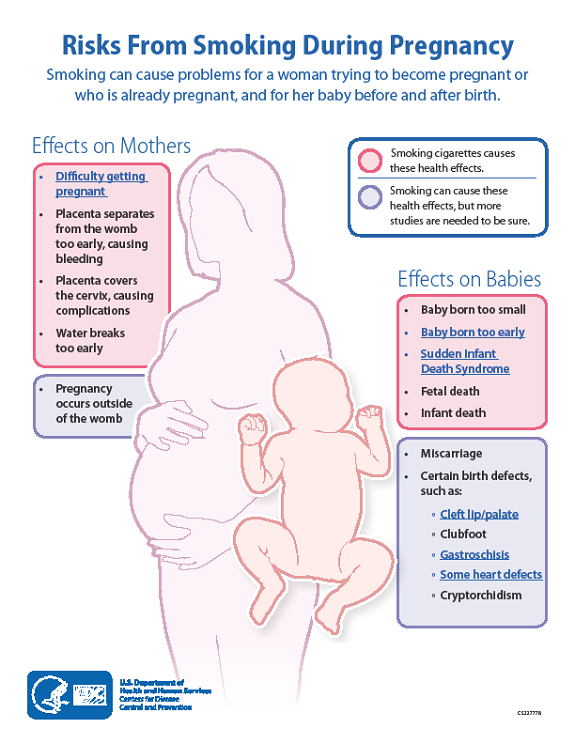 The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
Recurrent genital herpes is not an indication for abortion.
And despite all our clarifications about the relative safety of recurrent genital herpes during pregnancy, sometimes you have to receive such letters: A woman with recurrent genital herpes writes: “And most importantly, herpes is just natural selection. Nature removes lepers, because their offspring are doomed to death, so I don’t even dream of children ... ”It is ignorant to consider yourself a leper and refuse the happiness of motherhood just because you have recurrent genital herpes (the most favorable form for bearing and childbirth). Although, it cannot be ruled out that this is our medical defect.
There is also such a diagnosis as non-primary genital herpes . What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
Use of immunomodulators during pregnancy
The server editor received a letter describing a typical clinical situation:
« I have a problem that requires urgent consultation. My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
In my opinion, the use of immunomodulators during pregnancy is IMPOSSIBLE:
* In this case, herpes on the lips of a woman cannot bring any harm to either the woman or the child.
*Long-term effect of immunomodulatory drugs on the fetus is unknown. As you know, some of these drugs, easily penetrating the placenta into the body of the fetus, can cause congenital deformities in the latter, disorders of the immune system, and increase the risk of developing cancer.
*If the mother is ill with recurrent genital herpes, this would also not be dangerous for the fetus, because it is protected by maternal antiviral antibodies.
*Immunobiological preparations: immunomodulators, vaccines, immunoglobulins are a foreign protein and can cause various complications during pregnancy.
Based on the foregoing, I urge women who during pregnancy are trying to be treated for herpes on the lips or genital herpes with immunomodulators, immunoglobulins and other immunobiological preparations to run away from such doctors and such savage methods of treatment. World during pregnancy immunobiological preparations are not used for the treatment of herpesvirus infections .
Author: Ivan Yurievich Kokotkin, doctor
Source: http://www.herpes.ru/
Herpes, cytomegalovirus, Epstein-Barr virus in pregnant women
Expecting a baby is always stressful for the female body, which has to work hard for nine months.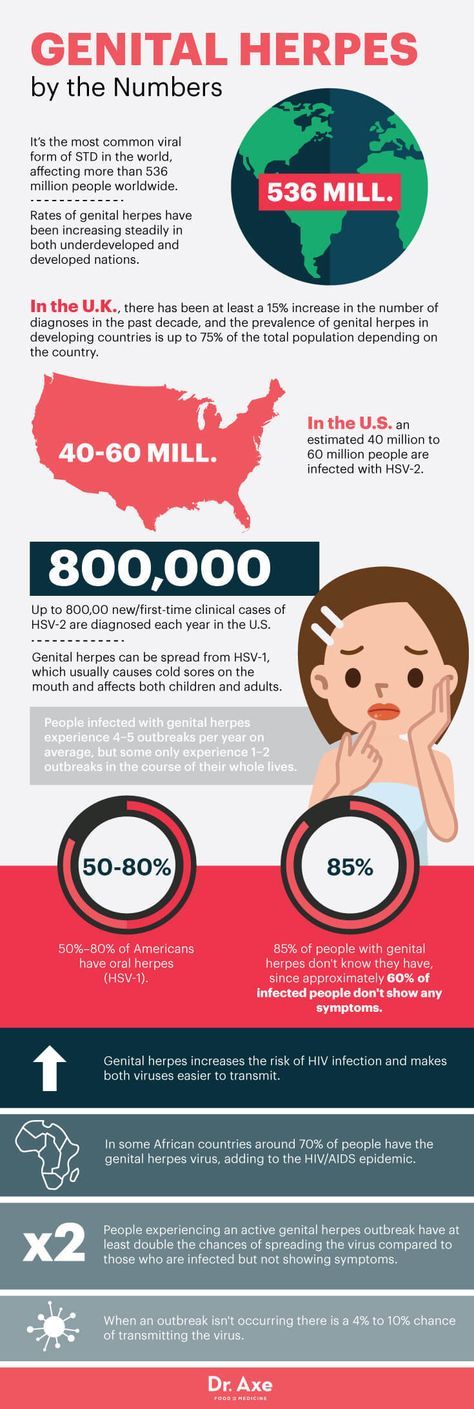 And during pregnancy, the expectant mother has a lot of reasons for unrest. Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail.
And during pregnancy, the expectant mother has a lot of reasons for unrest. Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail.
Herpes
The concept of "herpes during pregnancy" is too broad and often becomes a cause for unreasonable panic among pregnant women who do not know what and in what cases a threat to their unborn child may appear. It is important for a pregnant woman to have information about all the features of this disease at different stages of pregnancy in order to contact a gynecologist in time and understand when there is really a danger to the fetus when a cold appears on the lips.
If a woman in an interesting position has a recurrent form of the virus, that is, she has already encountered it before pregnancy, almost any manifestation of herpes is not dangerous for the mother and child. A simple herpes virus can only be a threat during pregnancy if it is a primary infection, especially in the early stages, when all the internal organs of the baby are laid and, most dangerously, the neural tube.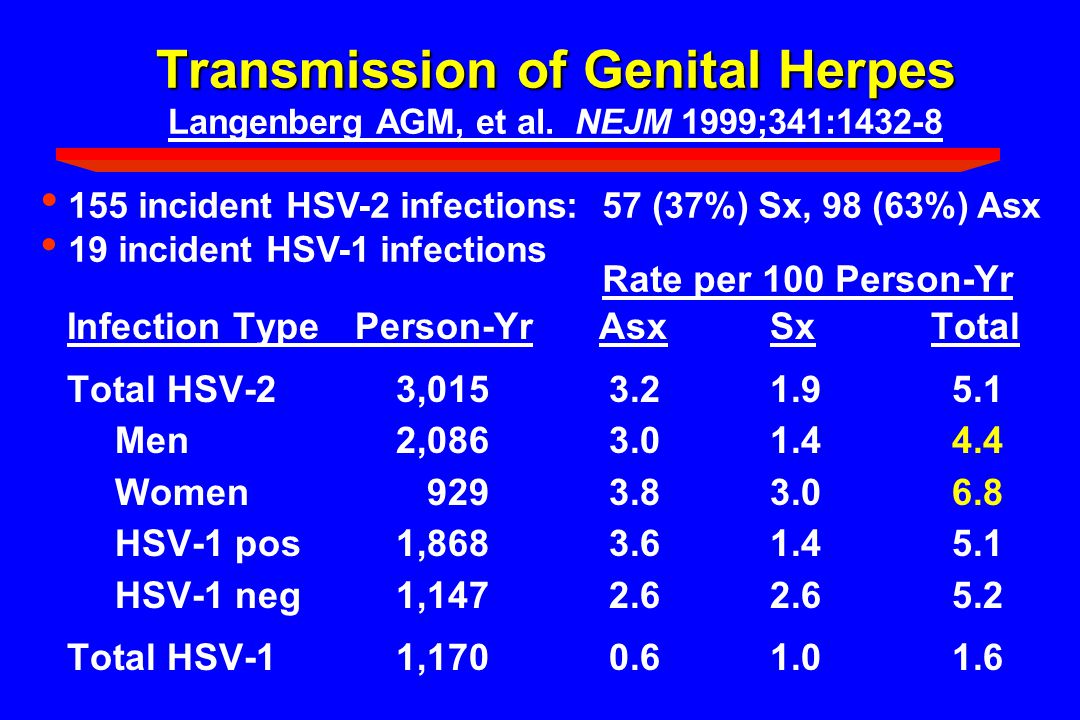 Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
Cytomegalovirus
For a pregnant woman, the virus is dangerous during the primary infection during the expectation of a child. Infection from a sick person with an acute cytomegalovirus infection is the worst option for a pregnant woman, because due to the lack of antibodies in the blood, the virus easily crosses the placenta and has a negative effect on the fetus. According to statistics, infection of the fetus occurs in 40-50% of cases. The degree of adverse effect of the virus on the fetus depends on the duration of pregnancy. If the fetus is infected in early pregnancy, there is a high probability of spontaneous miscarriage or anomalies in the development of the child. If the infection happened at a later date, no fetal malformations are observed, but quite often polyhydramnios occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia.
If the infection happened at a later date, no fetal malformations are observed, but quite often polyhydramnios occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia.
Eppstein-Barr virus
The Epstein-Barr virus predisposes to premature termination of pregnancy, fetal malnutrition, in newborn children causes damage to the nervous system, organs of vision, recurrent chroniosepsis, hepatopathy and respiratory distress syndrome. However, this virus provokes the listed pathologies only under certain conditions, in the presence of which during pregnancy it becomes dangerous. It is very bad if a pregnant woman has not previously encountered the Eppstein-Barr virus, which is why she does not have antibodies to this virus in her body. If there was still contact, and antibodies were found after treatment, then this is a good sign, because in this case there is nothing to be afraid of.