Burning vagina pregnant
Vaginal Burning: Causes, Relief, Pregnancy
Vagina burning like you’re in an inferno? No your pants aren’t on fire, but something is causing your bits to burn. Ummm… so should you be worried about this vaginal burning?
The occasional itch or irritation in your lower region is completely common and generally nothing to worry about. But, if persistent burning, itching, or irritation start to become your norm, something may be up.
Burning can creep up anywhere in your vaginal area, including your:
- vaginal opening
- labia
- clitoris
Here’s why you may be feeling the burn and what to do about it.
Some of the products you use on the daily might be working against you with chemicals that can irritate your vag. This can cause burning, itching, stinging, rawness, or even pain.
You may notice symptoms right away after switching to a new product, or it may take a few uses.
Products that can cause irritation include:
- scented soaps
- detergents
- bubble baths
- menstrual pads
- scented toilet papers
What to do about it? The best way to remedy this is to stop using the products and avoid using other scented or perfumed products on your nether region.
If symptoms continue after you’ve stopped using these products, talk to your doctor to discover if something else is going on downtown.
Some products or substances that are made to be in or around your vagina can irritate your genitals and fuel that fiery feeling. This includes:
- tampons
- latex condoms
- sprays
- creams
- douches
- certain topical medications
- semen
- spermicides
What to do about it? If you have a product that you’ve just started using, stop using it to see if the burning goes away. Not sure which product that is? Try patch testing a small area to help identify the irritant.
If you discover that the culprit is your preferred method of contraception, like latex condoms, talk to your doctor. They can help you find an alternative that won’t impede on your sexy time fun.
Certain clothing can also cause burning and irritation down below, such as:
- tight underwear
- tights
- tight or fitted pants/shorts
The culprit is most likely chafing or extra moisture irritating your bits. While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
What to do about it? Avoid irritation by not wearing tight clothing too often or for too long of periods of time. Be careful with wet clothing, too. Sitting too long in a wet swimsuit can lead to bacteria growth in your vagina and infections.
Bacterial vaginosis (BV) happens when there’s too much of certain bacteria in your vagina, throwing off your hoo-ha’s normal balance. And a not-so-fun fact: It’s the most common vaginal infection for women ages 15 to 44, according to the Centers for Disease Control and Prevention (CDC).
In some cases, you may not experience any symptoms of BV. For those that do, however, symptoms can include:
- burning
- itching
- pain
- white or gray vaginal discharge
- a fish-like odor, especially after sex
What to do about it? BV may disappear on its own, but you’ll usually need to see your doctor for antibiotics to clear the infection up. It’s essential that you take every dose prescribed, even if you start feeling better.
It’s essential that you take every dose prescribed, even if you start feeling better.
Yeast infections have nothing to do with quarantine bread-making, and everything to do with what happens when there’s excessive yeast growth in the vagina. Along with burning, signs of a yeast infection may be:
- soreness
- red rash outside your vagina
- itching or swelling of the vagina or the vulva
- pain when you pee or during sex
- thick, white discharge (think cottage cheese)
Nearly 75 percent of women experiencing at least one yeast infection in their lifetime. And, while the risk of getting a yeast infection is already high, it’s even higher for women who:
- are pregnant
- have diabetes
- are now or were recently on antibiotics
- are using hormonal birth control
- have a compromised immune system
What to do about it? Yeast infections can often be treated at home or with an over-the-counter (OTC) antifungal medication such as a cream, ointment, or suppository.
However, if you experience frequent yeast infections, your infection doesn’t clear up after treatment, or this is your first yeast infection ever, it’s best to see your doctor. They can confirm your diagnosis and help you determine the best treatment plan for you.
Urinary tract infections (aka UTIs) happen when bacteria gets in your urinary tract or bladder. You’ll likely experience a burning sensation when you pee, as well as other symptoms like:
- a frequent need to pee (often with little results)
- strong-smelling urine
- cloudy urine
- blood in your urine, making it red or pink
- fever or chills
- pain in the stomach, back, or pelvic area
What to do about it? Think you have a UTI? See your doctor. They’ll be able to prescribe you antibiotics to treat your infection.
Be sure to drink plenty of fluids and to take the full course of medication, even if symptoms have disappeared. If you don’t, you risk the infection returning.
Trichomoniasis (aka trich) is an STI, and one of the most common ones in the U.S. to boot. It appears more often in women than men. Symptoms only appear in about 30 percent of cases, so most women don’t even realize they have the infection.
Those that that do experience symptoms will likely have:
- vaginal burning, irritation, and/or itching
- clear, white, yellow, or green discharge
- lower abdominal pain
- foul odors down below
- discomfort while peeing or during sex
What to do about it? You’ll need to see your doctor, as prescription antibiotics are needed to clear up the infection. Typically, only a single dose will do the trick to treat your trich. Left untreated, however, trich can cause long-term complications, as well as increase your risk of getting other STIs.
Gonorrhea is another STI where bacteria infects mucous membranes like the cervix, uterus, or fallopian tubes. It’s most common in those ages 15 to 24 and rarely causes symptoms.
When symptoms do appear, they include:
- vaginal burning or irritation
- unusual discharge
- bleeding or spotting between periods
- burning or pain when urinating
What to do about it? Gonorrhea is treated with prescription antibiotics, so a trip to the doc is necessary. In some cases, a doctor may prescribe dual therapy, where two different meds will need to be taken at the same time.
Gonorrhea can lead to serious complications if it’s left untreated, including infertility and pelvic inflammatory disease (PID).
Chlamydia is another common STI caused by bacteria. It’s often known as a “silent” infection because, much like trich, about 70 percent of those with the infection don’t experience symptoms.
Those that do exhibit symptoms will likely experience:
- burning sensations
- abnormal discharge
- bleeding between periods or during sex
- pain during urination or sex
What to do about it? Prescription antibiotics are needed to cure chlamydia, so a trip to the doctor is necessary. Health professionals are also required to report chlamydia cases in order to track the infection.
Health professionals are also required to report chlamydia cases in order to track the infection.
If left untreated, chlamydia can wreak havoc on your reproductive system, and cause permanent damage. Repeat infection is also common with chlamydia, and each time you contract the infection can increase your chances of having issues with fertility.
Genital herpes is an incurable viral infection that’s caused by skin-to-skin contact with someone who has the herpes simplex virus (HSV). According to the CDC, an estimated 1 in 6 people in the U.S. between ages 14 to 49 has genital herpes.
Symptoms may not develop right away — in fact, it could be years before the virus becomes active and symptoms appear. When symptoms do appear, they’ll likely include:
- burning, itching, or tingling sensation in the vagina
- painful sores, blisters, or ulcers
- swollen glands
- vaginal pain, especially during urination
- flu-like symptoms
- abnormal vaginal discharge
What to do about it? The herpes virus stays in your body forever; there is no cure. However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
Your doctor about can also prescribe medication to help reduce the risk of transferring genital herpes to others.
The most common STI in the U.S. is human papillomavirus, more commonly known as HPV. HPV can cause genital warts, which can appear:
- on your vulva, vagina, cervix, or anus
- in clusters or as one or two bumps
- as white or flesh-colored bumps
What to do about it? While genital warts may disappear on their own, there’s no cure for them. You can choose to have them medically removed, which can lower your risk of transmitting the infection to others. HPV is also linked to different cancers, including anal cancer and cervical cancer.
Did you get the HPV vaccine?
To reduce the risk of HPV-related diseases and infections, the CDC, American Academy of Family Physicians, and other health experts recommend that preteens receive an HPV vaccination before becoming sexually active.
A rare skin condition, lichen sclerosus causes thin, white patches to appear on the vagina — especially around the vulva. These patches can lead to permanent scarring.
Other symptoms include:
- itching or burning
- pain or discomfort
- redness
- bleeding
- blisters or sores
- painful sex
Women can develop lichen sclerosis at any age, but it’s most common in postmenopausal women.
What to do about it? To treat lichen sclerosus, you’ll need to see your doctor, who can prescribe a strong topical steroid to ease symptoms. You’ll also want to regularly see your doctor to monitor any changes in the skin or permanent complications, like scarring, or thinning of the skin.
Wait, aren’t you a little young to be worried about menopause? Premature menopause is when you go through menopause before age 40. It isn’t very common and only affects about 1 percent of women (and a lot of times it’s genetic).
During menopause your estrogen and progesterone levels get super low, and you’ll stop having a menstrual cycle. This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
Menopause can also cause symptoms like:
- hot flashes
- irritability
- insomnia
- fatigue
- reduced sex drive
- night sweats
What to do about it? Menopause can’t be stopped, but it’s symptoms can be eased. One thing your doc may do is prescribe an estrogen supplement or other hormone therapy. If hormonal supplements aren’t your cup of tea, your doctor can work with you to find the best option for you.
If sex conjures up images of burning naughty bits rather than burning passion, you’re not alone. It’s not uncommon to experience a burning sensation after and during sex.
This can generally be attributed to:
- too much friction
- not enough lubricant being used
- allergic reaction to semen
- allergic reaction to products being used (like latex condoms, toys, or scented lotions)
- PH imbalance caused by douching
- hormonal birth controls
- UTIs, STIs, or other infections
How to find relief
Working in some extra lube or some additional foreplay to make matters more slippery can help you avoid that burning feeling in the future.
However, if sex continues to cause pain or other symptoms arise, it’s time to see the doctor. They can help figure out what’s going on and help you determine treatment or next steps.
Vaginal irritation is normal during pregnancy, and you’ll likely experience it more than once. This can be caused by a variety of reasons, including:
- increase in vaginal discharge
- vaginal dryness
- sensitivity to products
- hormonal changes
- UTIs or other bacterial infections
How to find relief
In many cases, it’s nothing to worry about, and you can ease your itch right at home by:
- taking a cool bath or using a cool compress
- using product elimination to determine the cause
- taking a bath with baking soda
Because pregnancy is a delicate time and you’re experiencing many physical changes, it’s always best to talk to your doctor if you have questions or something seems out of sorts.
If you think your symptoms are caused by an infection of any kind, talk to your doctor before taking any medications, including common OTC treatments.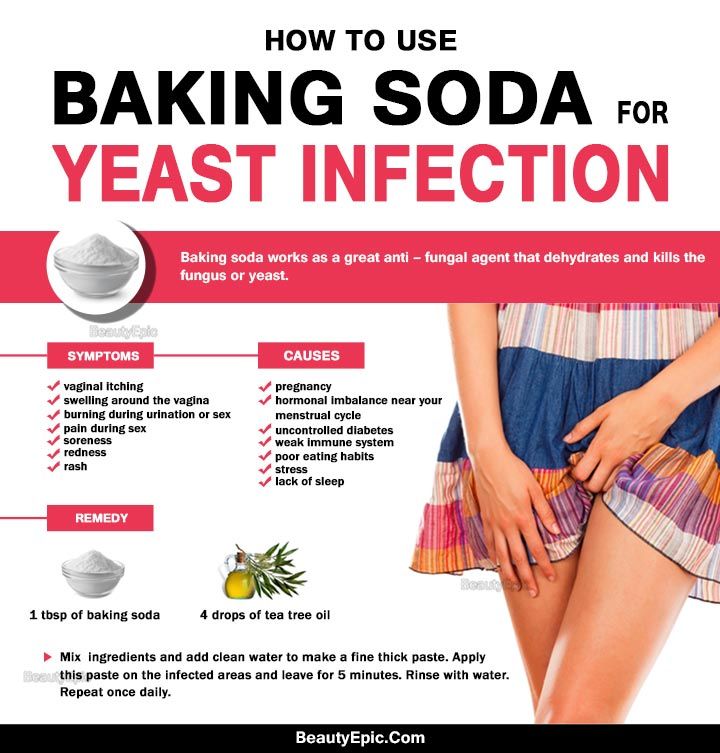 They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
Occasional itching or irritation on your vagina is normal, and there generally isn’t cause for concern. However, if you begin to experience persistent burning, increased irritation, or other symptoms that are out of the norm, there may be an underlying condition at play.
Talk to your doctor if you think something’s up (or even if you don’t… better safe than sorry!). In some cases, a simple prescription medication will make your condition disappear while others will require lifelong treatment or monitoring.
Your doctor can help identify what’s setting your bits to be on fire and help you find relief.
Vaginal Burning: Causes, Relief, Pregnancy
Vagina burning like you’re in an inferno? No your pants aren’t on fire, but something is causing your bits to burn. Ummm… so should you be worried about this vaginal burning?
The occasional itch or irritation in your lower region is completely common and generally nothing to worry about. But, if persistent burning, itching, or irritation start to become your norm, something may be up.
But, if persistent burning, itching, or irritation start to become your norm, something may be up.
Burning can creep up anywhere in your vaginal area, including your:
- vaginal opening
- labia
- clitoris
Here’s why you may be feeling the burn and what to do about it.
Some of the products you use on the daily might be working against you with chemicals that can irritate your vag. This can cause burning, itching, stinging, rawness, or even pain.
You may notice symptoms right away after switching to a new product, or it may take a few uses.
Products that can cause irritation include:
- scented soaps
- detergents
- bubble baths
- menstrual pads
- scented toilet papers
What to do about it? The best way to remedy this is to stop using the products and avoid using other scented or perfumed products on your nether region.
If symptoms continue after you’ve stopped using these products, talk to your doctor to discover if something else is going on downtown.
Some products or substances that are made to be in or around your vagina can irritate your genitals and fuel that fiery feeling. This includes:
- tampons
- latex condoms
- sprays
- creams
- douches
- certain topical medications
- semen
- spermicides
What to do about it? If you have a product that you’ve just started using, stop using it to see if the burning goes away. Not sure which product that is? Try patch testing a small area to help identify the irritant.
If you discover that the culprit is your preferred method of contraception, like latex condoms, talk to your doctor. They can help you find an alternative that won’t impede on your sexy time fun.
Certain clothing can also cause burning and irritation down below, such as:
- tight underwear
- tights
- tight or fitted pants/shorts
The culprit is most likely chafing or extra moisture irritating your bits. While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
What to do about it? Avoid irritation by not wearing tight clothing too often or for too long of periods of time. Be careful with wet clothing, too. Sitting too long in a wet swimsuit can lead to bacteria growth in your vagina and infections.
Bacterial vaginosis (BV) happens when there’s too much of certain bacteria in your vagina, throwing off your hoo-ha’s normal balance. And a not-so-fun fact: It’s the most common vaginal infection for women ages 15 to 44, according to the Centers for Disease Control and Prevention (CDC).
In some cases, you may not experience any symptoms of BV. For those that do, however, symptoms can include:
- burning
- itching
- pain
- white or gray vaginal discharge
- a fish-like odor, especially after sex
What to do about it? BV may disappear on its own, but you’ll usually need to see your doctor for antibiotics to clear the infection up. It’s essential that you take every dose prescribed, even if you start feeling better.
It’s essential that you take every dose prescribed, even if you start feeling better.
Yeast infections have nothing to do with quarantine bread-making, and everything to do with what happens when there’s excessive yeast growth in the vagina. Along with burning, signs of a yeast infection may be:
- soreness
- red rash outside your vagina
- itching or swelling of the vagina or the vulva
- pain when you pee or during sex
- thick, white discharge (think cottage cheese)
Nearly 75 percent of women experiencing at least one yeast infection in their lifetime. And, while the risk of getting a yeast infection is already high, it’s even higher for women who:
- are pregnant
- have diabetes
- are now or were recently on antibiotics
- are using hormonal birth control
- have a compromised immune system
What to do about it? Yeast infections can often be treated at home or with an over-the-counter (OTC) antifungal medication such as a cream, ointment, or suppository.
However, if you experience frequent yeast infections, your infection doesn’t clear up after treatment, or this is your first yeast infection ever, it’s best to see your doctor. They can confirm your diagnosis and help you determine the best treatment plan for you.
Urinary tract infections (aka UTIs) happen when bacteria gets in your urinary tract or bladder. You’ll likely experience a burning sensation when you pee, as well as other symptoms like:
- a frequent need to pee (often with little results)
- strong-smelling urine
- cloudy urine
- blood in your urine, making it red or pink
- fever or chills
- pain in the stomach, back, or pelvic area
What to do about it? Think you have a UTI? See your doctor. They’ll be able to prescribe you antibiotics to treat your infection.
Be sure to drink plenty of fluids and to take the full course of medication, even if symptoms have disappeared. If you don’t, you risk the infection returning.
Trichomoniasis (aka trich) is an STI, and one of the most common ones in the U.S. to boot. It appears more often in women than men. Symptoms only appear in about 30 percent of cases, so most women don’t even realize they have the infection.
Those that that do experience symptoms will likely have:
- vaginal burning, irritation, and/or itching
- clear, white, yellow, or green discharge
- lower abdominal pain
- foul odors down below
- discomfort while peeing or during sex
What to do about it? You’ll need to see your doctor, as prescription antibiotics are needed to clear up the infection. Typically, only a single dose will do the trick to treat your trich. Left untreated, however, trich can cause long-term complications, as well as increase your risk of getting other STIs.
Gonorrhea is another STI where bacteria infects mucous membranes like the cervix, uterus, or fallopian tubes. It’s most common in those ages 15 to 24 and rarely causes symptoms.
When symptoms do appear, they include:
- vaginal burning or irritation
- unusual discharge
- bleeding or spotting between periods
- burning or pain when urinating
What to do about it? Gonorrhea is treated with prescription antibiotics, so a trip to the doc is necessary. In some cases, a doctor may prescribe dual therapy, where two different meds will need to be taken at the same time.
Gonorrhea can lead to serious complications if it’s left untreated, including infertility and pelvic inflammatory disease (PID).
Chlamydia is another common STI caused by bacteria. It’s often known as a “silent” infection because, much like trich, about 70 percent of those with the infection don’t experience symptoms.
Those that do exhibit symptoms will likely experience:
- burning sensations
- abnormal discharge
- bleeding between periods or during sex
- pain during urination or sex
What to do about it? Prescription antibiotics are needed to cure chlamydia, so a trip to the doctor is necessary. Health professionals are also required to report chlamydia cases in order to track the infection.
Health professionals are also required to report chlamydia cases in order to track the infection.
If left untreated, chlamydia can wreak havoc on your reproductive system, and cause permanent damage. Repeat infection is also common with chlamydia, and each time you contract the infection can increase your chances of having issues with fertility.
Genital herpes is an incurable viral infection that’s caused by skin-to-skin contact with someone who has the herpes simplex virus (HSV). According to the CDC, an estimated 1 in 6 people in the U.S. between ages 14 to 49 has genital herpes.
Symptoms may not develop right away — in fact, it could be years before the virus becomes active and symptoms appear. When symptoms do appear, they’ll likely include:
- burning, itching, or tingling sensation in the vagina
- painful sores, blisters, or ulcers
- swollen glands
- vaginal pain, especially during urination
- flu-like symptoms
- abnormal vaginal discharge
What to do about it? The herpes virus stays in your body forever; there is no cure. However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
Your doctor about can also prescribe medication to help reduce the risk of transferring genital herpes to others.
The most common STI in the U.S. is human papillomavirus, more commonly known as HPV. HPV can cause genital warts, which can appear:
- on your vulva, vagina, cervix, or anus
- in clusters or as one or two bumps
- as white or flesh-colored bumps
What to do about it? While genital warts may disappear on their own, there’s no cure for them. You can choose to have them medically removed, which can lower your risk of transmitting the infection to others. HPV is also linked to different cancers, including anal cancer and cervical cancer.
Did you get the HPV vaccine?
To reduce the risk of HPV-related diseases and infections, the CDC, American Academy of Family Physicians, and other health experts recommend that preteens receive an HPV vaccination before becoming sexually active.
A rare skin condition, lichen sclerosus causes thin, white patches to appear on the vagina — especially around the vulva. These patches can lead to permanent scarring.
Other symptoms include:
- itching or burning
- pain or discomfort
- redness
- bleeding
- blisters or sores
- painful sex
Women can develop lichen sclerosis at any age, but it’s most common in postmenopausal women.
What to do about it? To treat lichen sclerosus, you’ll need to see your doctor, who can prescribe a strong topical steroid to ease symptoms. You’ll also want to regularly see your doctor to monitor any changes in the skin or permanent complications, like scarring, or thinning of the skin.
Wait, aren’t you a little young to be worried about menopause? Premature menopause is when you go through menopause before age 40. It isn’t very common and only affects about 1 percent of women (and a lot of times it’s genetic).
During menopause your estrogen and progesterone levels get super low, and you’ll stop having a menstrual cycle. This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
Menopause can also cause symptoms like:
- hot flashes
- irritability
- insomnia
- fatigue
- reduced sex drive
- night sweats
What to do about it? Menopause can’t be stopped, but it’s symptoms can be eased. One thing your doc may do is prescribe an estrogen supplement or other hormone therapy. If hormonal supplements aren’t your cup of tea, your doctor can work with you to find the best option for you.
If sex conjures up images of burning naughty bits rather than burning passion, you’re not alone. It’s not uncommon to experience a burning sensation after and during sex.
This can generally be attributed to:
- too much friction
- not enough lubricant being used
- allergic reaction to semen
- allergic reaction to products being used (like latex condoms, toys, or scented lotions)
- PH imbalance caused by douching
- hormonal birth controls
- UTIs, STIs, or other infections
How to find relief
Working in some extra lube or some additional foreplay to make matters more slippery can help you avoid that burning feeling in the future.
However, if sex continues to cause pain or other symptoms arise, it’s time to see the doctor. They can help figure out what’s going on and help you determine treatment or next steps.
Vaginal irritation is normal during pregnancy, and you’ll likely experience it more than once. This can be caused by a variety of reasons, including:
- increase in vaginal discharge
- vaginal dryness
- sensitivity to products
- hormonal changes
- UTIs or other bacterial infections
How to find relief
In many cases, it’s nothing to worry about, and you can ease your itch right at home by:
- taking a cool bath or using a cool compress
- using product elimination to determine the cause
- taking a bath with baking soda
Because pregnancy is a delicate time and you’re experiencing many physical changes, it’s always best to talk to your doctor if you have questions or something seems out of sorts.
If you think your symptoms are caused by an infection of any kind, talk to your doctor before taking any medications, including common OTC treatments. They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
Occasional itching or irritation on your vagina is normal, and there generally isn’t cause for concern. However, if you begin to experience persistent burning, increased irritation, or other symptoms that are out of the norm, there may be an underlying condition at play.
Talk to your doctor if you think something’s up (or even if you don’t… better safe than sorry!). In some cases, a simple prescription medication will make your condition disappear while others will require lifelong treatment or monitoring.
Your doctor can help identify what’s setting your bits to be on fire and help you find relief.
The 7 Best Sex Positions for Pregnant Women
February 26, 2020 Which doesn't make it any worse.
Share
0Is it possible to have sex during pregnancy
If the pregnancy proceeds without complications, there is no reason to refuse the joys of love. The penis will not penetrate further than the vagina and in no way harm the child, which is reliably protected by the muscles of the uterus and amniotic fluid.
The penis will not penetrate further than the vagina and in no way harm the child, which is reliably protected by the muscles of the uterus and amniotic fluid.
Concerns that sex can cause preterm labor are also unfounded. True, in the third trimester, an orgasm can lead to false contractions. But they are considered the norm, do not harm the body at all and, on the contrary, prepare it for childbirth.
However, in certain cases, the doctor may still advise you to abstain from sex. As a rule, such a recommendation sounds with the following complications:
- threatened miscarriage;
- vaginal bleeding;
- leakage of amniotic fluid;
- early dilatation of the cervix;
- placenta previa.
Multiple pregnancy is also considered a contraindication for sex.
Reading now 🔥
- 10 vagina myths that keep you from living
Things to consider when having sex during pregnancy
Your body and hormones change during pregnancy, and this leads to the following phenomena that you have to take into account:
- Libido surges.
 Often, it drops sharply in the first trimester: the body is undergoing active restructuring, and sexual desire is suppressed by toxicosis. In the second trimester, the state of health returns to normal, and the craving for intimacy can even worsen. In the third trimester, physical intimacy is beneficial because, as mentioned above, orgasm helps prepare the body for childbirth. And additional releases of oxytocin relieve anxiety.
Often, it drops sharply in the first trimester: the body is undergoing active restructuring, and sexual desire is suppressed by toxicosis. In the second trimester, the state of health returns to normal, and the craving for intimacy can even worsen. In the third trimester, physical intimacy is beneficial because, as mentioned above, orgasm helps prepare the body for childbirth. And additional releases of oxytocin relieve anxiety. - Hypersensitivity. The breasts, clitoris and vagina swell and become more sensitive during pregnancy. On the one hand, it exacerbates pleasure. On the other hand, it is fraught with painful sensations, so the partner should be more sensual and gentle.
- Uncomfortable habitual postures. We'll have to forget about acrobatic stunts in bed and aggressive sex with deep penetration for a while. Even the usual missionary position can become uncomfortable. And after the 20th week, the “sandwich” is recommended to be excluded from the sexual menu altogether.
 The thing is that in this position, the heavier uterus presses on the vessels, making it difficult for blood circulation. Fortunately, there are many other options.
The thing is that in this position, the heavier uterus presses on the vessels, making it difficult for blood circulation. Fortunately, there are many other options.
What are the most comfortable sex positions for pregnant women
Your preferences may vary depending on the duration of your pregnancy. But first of all, try poses in which the risk of discomfort or pain is minimal.
1. Spoons
Illustration: a.frizen/ShutterstockTiming advice. In a position where a woman lies with her back to a man, it is convenient to have sex at any time. But you will especially appreciate the position in the third trimester: because of the grown belly, it will be difficult for you to face each other.
In the “spoon” position, it is convenient to caress the partner's clitoris and breasts. And the penetration will not be deep, which reduces the risk of hurting the cervix, which becomes extremely sensitive during pregnancy.
2. Lying facing each other
Illustration: a. frizen/Shutterstock
frizen/Shutterstock Timing recommendations. Suitable for first and second trimesters.
It will be convenient for you to experiment with the angle of penetration and engage in slow sensual sex. The special charm is that you can look into each other's eyes, maintaining an emotional connection. And to make you even more comfortable, place a small pillow or rolled towel under your stomach.
3. Doggystyle
Illustration: a.frizen/ShutterstockTiming recommendations. Doggy style is good in any trimester. But in the last stages of pregnancy, it is almost indispensable.
The knee-and-elbow pose relieves stress on the back and lower back, which are areas of the body that many experience pain during pregnancy. It also reduces pressure on the bladder. A woman can simply relax, leaving all the initiative to her partner. For added comfort, you can place a pillow under your chest or stomach.
Men are advised to act gently and carefully. Since the position allows for deep penetration, it is important not to get too carried away so as not to hurt the pregnant partner.
Since the position allows for deep penetration, it is important not to get too carried away so as not to hurt the pregnant partner.
4. Against the wall
Illustration: a.frizen/ShutterstockTiming recommendations. You can have sex against the wall as long as the woman does not experience congestion. For long periods and with a large fetus, the expectant mother can be hard and want to lie down.
A variation on the "man behind" theme is a chance for parents-to-be to play pranks and have quick sex. The advantage is that in this case it is easier for a woman to control the depth of penetration. And the emphasis on the wall allows you to conveniently distribute the load.
5. Rider
Illustration: a.frizen/ShutterstockTiming advice. Excellent option for the first two trimesters. In the later stages, it becomes more difficult for a woman to actively move due to her large belly.
The cowgirl position is ideal for almost all pregnant women, because it does not create pressure on the stomach and allows the expectant mother to set the right rhythm for her and find the most pleasant angle of penetration.
For optimal balance, you can rest your hands on the back or front of the head of the bed. At the same time, nothing prevents a man from caressing his chest and other erogenous zones of his partner.
6. Reverse Cowgirl
Illustration: a.frizen/ShutterstockTiming advice. Do not deprive yourself of this pleasure the first two trimesters. But you can experiment on the third.
In addition to control, the posture will also give a woman additional stimulation of the anterior wall of the vagina, where perhaps the mysterious G-spot is located. Considering that pregnant women have increased sensitivity, this is a real chance to achieve a vaginal orgasm.
7. Scissors
Illustration: a.frizen/ShutterstockTiming advice. This pose can be used in the first two trimesters. And sometimes in the third, if the woman does not experience dizziness and other unpleasant sensations.
The meaning of “scissors” is that the partner settles on her back as comfortably as possible, if necessary, leaning on the pillows. She throws her legs at the man, and he lays down at an angle to her and slowly enters her. Due to the small depth of penetration, the risk of pain is minimal. The position is conducive to unhurried lovemaking, caresses of the chest and clitoris, and deep emotional communication.
She throws her legs at the man, and he lays down at an angle to her and slowly enters her. Due to the small depth of penetration, the risk of pain is minimal. The position is conducive to unhurried lovemaking, caresses of the chest and clitoris, and deep emotional communication.
Read also 🍓🍌🤰
- How and why to practice yoga for pregnant women
- 10 life hacks that will greatly facilitate pregnancy
- 7 myths about sex during pregnancy
- What you need to know about sex during your period
- What you need to know for a happy pregnancy: advice from Lesya Ryabtseva
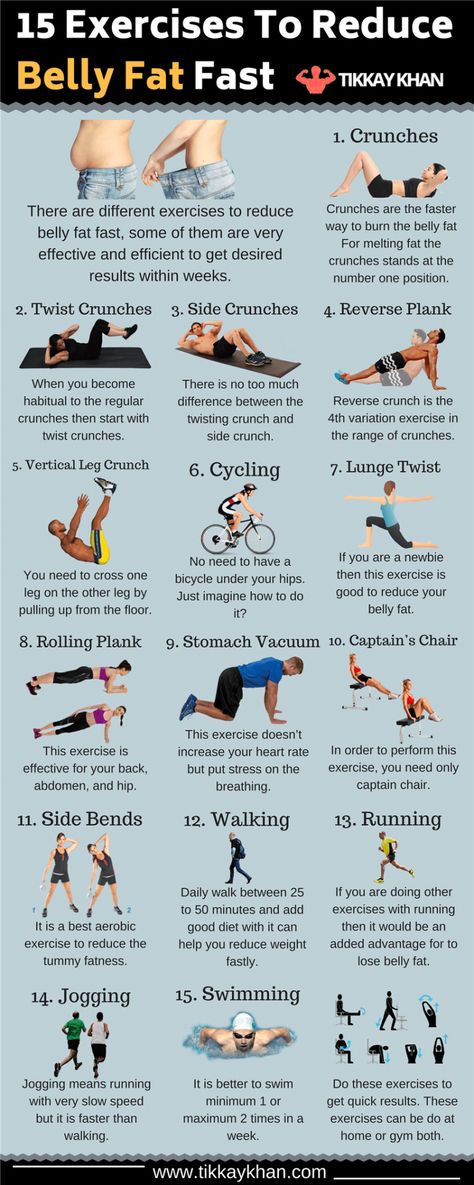
12 Doctors Recommended Exercises for Pregnancy
March 21, 2021LikbezSports and Fitness
Even if you've never been into fitness, now is the time to start.
Iya Zorina
Author of Lifehacker, athlete, CCM
Share
0Why do exercises for pregnant women
Scientists and doctors agree that pregnancy is not a reason to stop training. You should continue to engage in your usual physical activity as long as you feel comfortable doing it.
You should continue to engage in your usual physical activity as long as you feel comfortable doing it.
In addition, women who were inactive before pregnancy are advised to add more movement, as exercise provides several benefits at once:
- strengthens muscles, which helps you better cope with the extra weight that you will gain during pregnancy;
- improve blood circulation;
- strengthen joints;
- help with back pain that can develop as the belly grows;
- have a positive effect on the duration of labor and its outcome;
- reduce the risk of complications in late pregnancy and childbirth.
The American College of Sports Medicine recommends that pregnant women exercise for at least 30 minutes a day most of the week. But this applies to healthy women without contraindications to exercise.
How to know if you can do pregnancy exercises
While healthy women have few contraindications to exercise, there are several conditions where physical activity can be harmful.
Exercise during pregnancy is contraindicated in:
- gestational hypertension;
- preeclampsia;
- rupture of membranes;
- cervical incompetence;
- bleeding in the second or third trimester;
- multiple pregnancy at risk of preterm delivery;
- placenta previa;
- threatened preterm birth.
Exercise caution should also be exercised in cases of growth restriction, extreme weight, and poorly controlled comorbidities such as type 1 diabetes, hypertension, seizure disorders, and thyroid disease.
Even if you feel fine and do not have any illness, please consult your pregnancy doctor before beginning any activity.
He will assess the risks and your level of activity before pregnancy and will give recommendations on the types, intensity and duration of activities.
Things to consider when doing exercises for pregnant women
First of all, it is worth reducing the intensity to a comfortable level. Stick to the Conversation Rule: If you can carry on a conversation during a workout without getting out of breath, the intensity is right.
Stick to the Conversation Rule: If you can carry on a conversation during a workout without getting out of breath, the intensity is right.
If you did not exercise before pregnancy, start with 15 minutes of exercise a day. Gradually bring this time up to 30 minutes, but not quickly - focus on the sensations of your body and do not overload.
Also follow a few rules:
- always warm up before training and cool down after training;
- avoid strenuous exercise in hot conditions;
- drink enough water;
- if you are going to work with a trainer, make sure that he has a special education and tell him about the pregnancy.
Exercises to avoid during pregnancy
There are several types of exercises that can lead to undesirable consequences or make you uncomfortable:
- Movements in which you lie on your back for a long time (after 16 weeks of pregnancy). Because the weight of the abdomen compresses the main blood vessels that bring blood to the heart, lying on your back can cause weakness.

- An activity that requires you to stand for long periods of time.
- Contact sports that increase the risk of getting hit.
- Exercise and activity that can lead to a fall. If you feel insecure, ask your relatives to insure.
What Pregnancy Exercises to Do
Here are some safe pregnancy exercises you can do if there are no contraindications.
1. Wall Push-ups
This exercise will strengthen your chest muscles and the back of your shoulders.
Stand one step away from a wall with your feet hip-width apart. Press your palms against the wall at shoulder level, bend your elbows, and do a push-up. Keep your back straight, do not spread your elbows to the sides, place your shoulders at an angle of 45 ° from the body. Gradually work your way up to 15 reps.
2. Fitness Ball Squat
This exercise strengthens your hips and back, improves your ability to get into and out of a chair with new weight and a shifted center of gravity.
Stand up straight with a fitness ball between your lower back and a wall. Place your feet shoulder-width apart. Lower yourself down to a right angle at the knees. Make sure your heels do not come off the floor.
If you find it difficult to squat to a right angle at the knees, do the exercise as low as you can. Then straighten your legs, returning to the starting position, and repeat the movement.
If you feel unsure, ask someone to stand next to you to help you if you lose your balance. Perform 10-12 times.
3. Leg raises on all fours
This exercise strengthens the muscles of the back and abdomen.
Get on all fours, place your wrists under your shoulders, straighten your arms. Raise your right knee and straighten your leg back parallel to the floor. Return it to the floor and repeat on the other side. Do 10 reps with each leg.
4. Steps
Functional movement that will help you strengthen your legs and buttocks and improve your sense of balance. You can step onto a step stand or a ladder rung. Make sure the chosen support is stable.
You can step onto a step stand or a ladder rung. Make sure the chosen support is stable.
Step up the hill, then back down and repeat with the other leg. During the exercise, keep your back straight and fully press the foot to the surface of the platform.
Do as many reps as you can, depending on your fitness level. Stop when you get tired or the form of the exercise begins to suffer.
5. Elbow Side Plank
This exercise strengthens core muscles and helps increase stability and balance.
Lie on your left side, bend your knees so that your thighs are in line with your body. Then lift your body off the floor, resting on your knees and left forearm. Place your right hand on your right side. Hold the position for a few seconds, then lower yourself to the floor and repeat. Do 10 reps on each side.
6. Leg extension with lumbar support
This movement will help strengthen the abdominal muscles.
Lie down on a mat with a folded blanket under your lower back and place your hands on your forearms.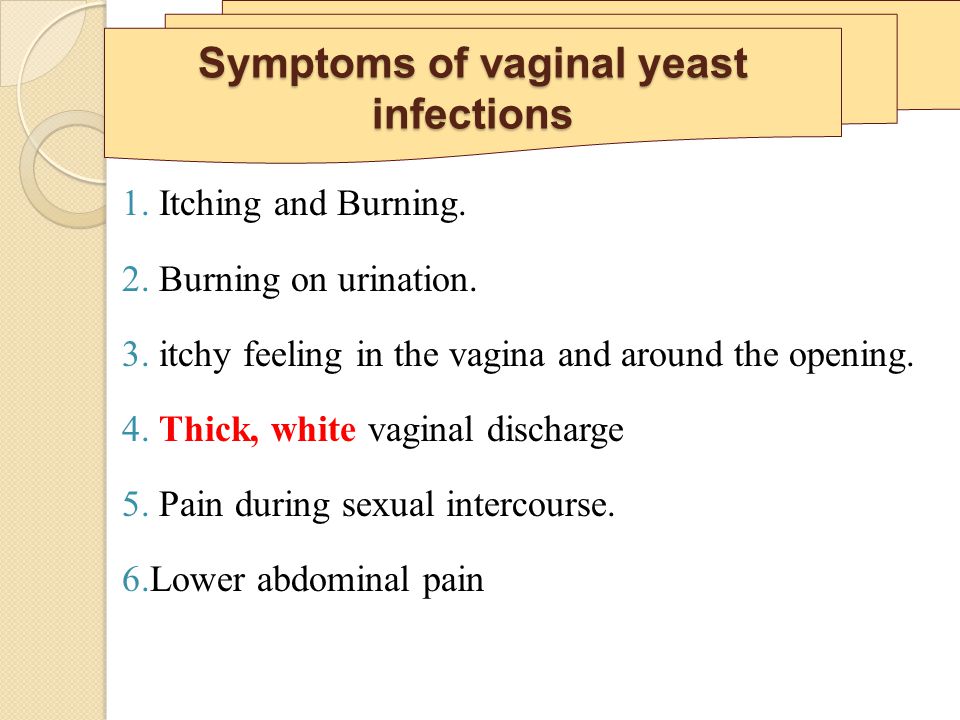 Bend your knees at a right angle and place your feet on the mat. Straighten one knee, extending the leg, then return it to the starting position and repeat with the other leg. Do 10 times with each leg.
Bend your knees at a right angle and place your feet on the mat. Straighten one knee, extending the leg, then return it to the starting position and repeat with the other leg. Do 10 times with each leg.
7. Bosu V-Position Hold
You can perform the ab hold while sitting on an unstable platform.
Sit on the Bosu with your knees bent at a right angle and your feet flat on the floor. You can stretch your arms out in front of you or leave them pressed against the platform if you feel insecure.
Lean your back straight and tighten your abs. Hold this pose for a few seconds, then return to the starting position and repeat. Aim for 10 reps.
If you find it easy to do the V-fold on two legs, try doing it on one. When you tilt your body back, lift one leg off the mat and extend it parallel to the floor.
Hold for a few seconds, then return to the starting position. Repeat 10 times and do with the other leg.
8. Seated Stomach Row
This exercise strengthens the muscles of the upper back.
Sit on a chair, press the band with your feet, placing it under the balls of your feet. Grasp the handles or loops of the expander, turning the brushes with your palms facing you. Lean your body forward with a straight back.
Overcoming the resistance of the elastic band, pull the handles to the belt. Feel how your shoulder blades converge. Return to starting position and repeat. Do 15 times.
You can also do this exercise while sitting on a fitball. It is good if there is a person nearby who can insure you in case of loss of balance.
9. Seated Band Deadlift
This exercise will strengthen the back extensor muscles.
Sit on a fitness ball or chair with your feet shoulder-width apart and your feet flat on the floor. Place the expander under the arches of the feet. Holding the handles in straight arms, bend at the hip joint. Bring your belly close to your hips, keeping your back straight, then return to the starting position and repeat. Do 15 reps.
Do 15 reps.
To make this exercise harder, wrap the band around your wrists to provide more resistance and stress on your back muscles.
10. Backbend on all fours
Get on all fours with your knees under your hips and your hands under your shoulders with your fingers forward. Make sure your lower back stays neutral and doesn't arch. Pull in your stomach and raise your back to the ceiling, arching it in an arc. Leave your head hanging relaxed, do not block the elbow joint. Move within a comfortable range.
Hold the pose for a few seconds, then slowly return to the starting position. Again, check that the lower back is in a neutral position, and does not sag in an arch. Perform the exercise slowly and rhythmically 10 times, feel how the back muscles work.
11. Pelvic tilt
Stand up straight with your shoulders and buttocks against the wall, do not strain your knees or lock your joints. Pull your navel towards your spine so that your lower back is fully pressed against the wall.