Are you born with asthma
The Link Plus Other Risk Factors & Prevention
Asthma is a chronic (lifelong) lung condition that often runs in families. While it’s possible to develop asthma at any age, children of asthmatic parents are at an increased risk of getting it when they’re younger.
While there are strong links between asthma and genetics, not everyone with a family history of asthma will develop this complex illness. It’s also possible to experience remission from your symptoms. Others will develop asthma later in life with no family history.
The key to asthma management is to take your recommended medications while also avoiding any known triggers as much as possible.
While you can’t change your genes, there are still steps you can take to help control your asthma — and perhaps even lower your risk of developing it as an adult.
Genetic predisposition is one of the strongest risk factors for developing asthma.
While no one is born with asthma itself, you may be born with genes that dictate whether you’ll get it as an infant or young child.
In fact, it’s estimated that children are up to 3 times more likely to develop asthma if their mothers have it, and 2.5 times more likely if their fathers do.
However, there’s no guarantee that a genetic disposition will automatically mean you get asthma.
One study on twins with asthma found that 66 percent of cases were linked to environmental factors, while the other 34 percent were genetic. Another 2019 review states that the risk of twins developing asthma because of their genes ranges between 55 and 90 percent.
Other research supports the fact that while one sibling might get asthma from their parents, other siblings may not.
Due to the fact that asthma is one of the world’s leading chronic illnesses, researchers continue to expand their work in different aspects of genetics. Future clinical research may go beyond individual families and look specifically at ancestry.
Even if asthma doesn’t run in your family, it’s still possible to develop this condition at some point in your lifetime.
Other possible causes and risk factors for asthma development include:
- having a personal or family history of allergies
- a history of autoimmune diseases
- having hay fever or eczema
- premature birth
- obesity
- smoking or frequent exposure to cigarette smoke
- regular exposure to air pollution, gasses, and chemical fumes
- hormonal changes in women during menopause
Viral upper-respiratory infections are common causes of acute (or short-term) asthma, which usually improve after you’ve gotten over your illness. Lung infections (specifically RSV) at a younger age may also increase your risk of developing asthma as you get older.
It’s also possible to enter remission from asthma at some point in your life, only for your symptoms to return later. These are often linked to asthma triggers, which may lead to short-term or long-term symptoms depending on the severity.
Common asthma triggers
Common triggers for asthma flare-ups include:
- seasonal allergies, such as tree, grass and ragweed pollen
- upper respiratory tract infections (viruses)
- air pollution or smoke
- weather changes, particularly extreme cold and dryness
- pet dander
- mold
- chemical odors
- dust mites
- cockroaches
- food additives — especially sulfites
- beta blocker medications, which are sometimes used for migraine and high blood pressure
- stress
- exercise
It may not be possible to prevent all cases of asthma.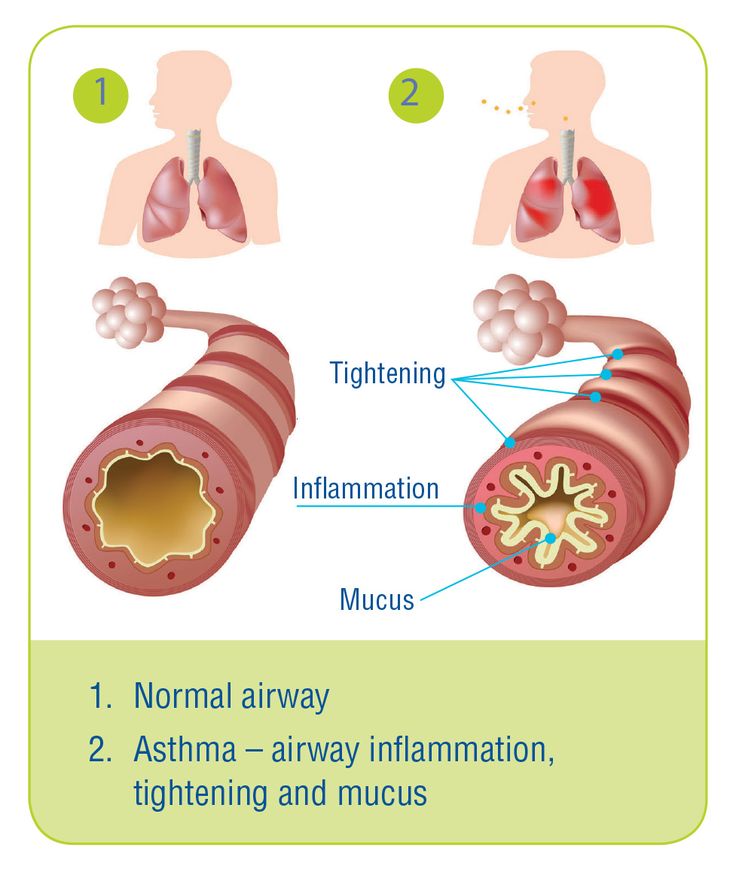 However, you can help control your risk of developing this chronic condition later in life by:
However, you can help control your risk of developing this chronic condition later in life by:
- quitting smoking and avoiding others who smoke
- avoiding occupational hazards that expose you to airborne chemicals and fumes
- controlling stress
- losing weight (if your doctor advises you to)
- keeping your home clean
- avoiding allergens and other triggers as much as possible
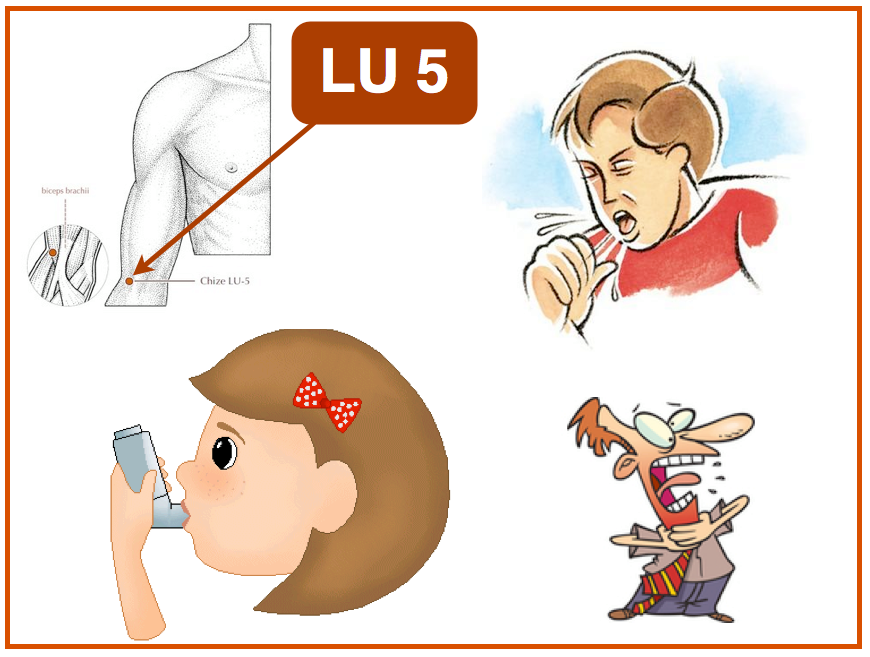
Asthma occurs as a result of constriction and inflammation (swelling) of the airways. This causes reduced airflow, resulting in the following symptoms:
- wheezing
- coughing
- tightness in the chest
- shortness of breath
- difficulty breathing
- increased mucus production
- fatigue
The more your asthma is controlled with medications, the fewer symptoms you should experience. However, if you continue to have asthma symptoms and rely on quick-relief inhalers, your asthma may be considered poorly controlled.
Other signs of poorly controlled asthma include:
- trouble sleeping at night
- difficulty exercising
- frequent asthma attacks
- not being able to do the activities you’d normally enjoy
It’s important to talk with your doctor right away if you’re experiencing worsening symptoms, or if your condition isn’t improving. They may modify your treatment plan to help better control your symptoms — and prevent damage to your airways.
They may modify your treatment plan to help better control your symptoms — and prevent damage to your airways.
For many people, asthma may be genetic. You’re much more likely to develop asthma if one or both of your parents has this chronic inflammatory lung disease.
Symptoms may fluctuate throughout your life, so it’s important to follow your asthma action plan as outlined by your doctor.
In other cases, asthma may be caused by environmental factors. Severe allergies, smoke exposure, and stress are all possible causes. It’s also possible to develop asthma later in adulthood due to a severe illness or hormone fluctuations.
No matter the cause, it’s important to keep track of your asthma symptoms and talk with your doctor if you aren’t noticing any improvements despite treatment.
Are You Born with Asthma?: Alpha Internal Medicine: Internal Medicine
Are You Born with Asthma?: Alpha Internal Medicine: Internal MedicineWe offer same day appointments.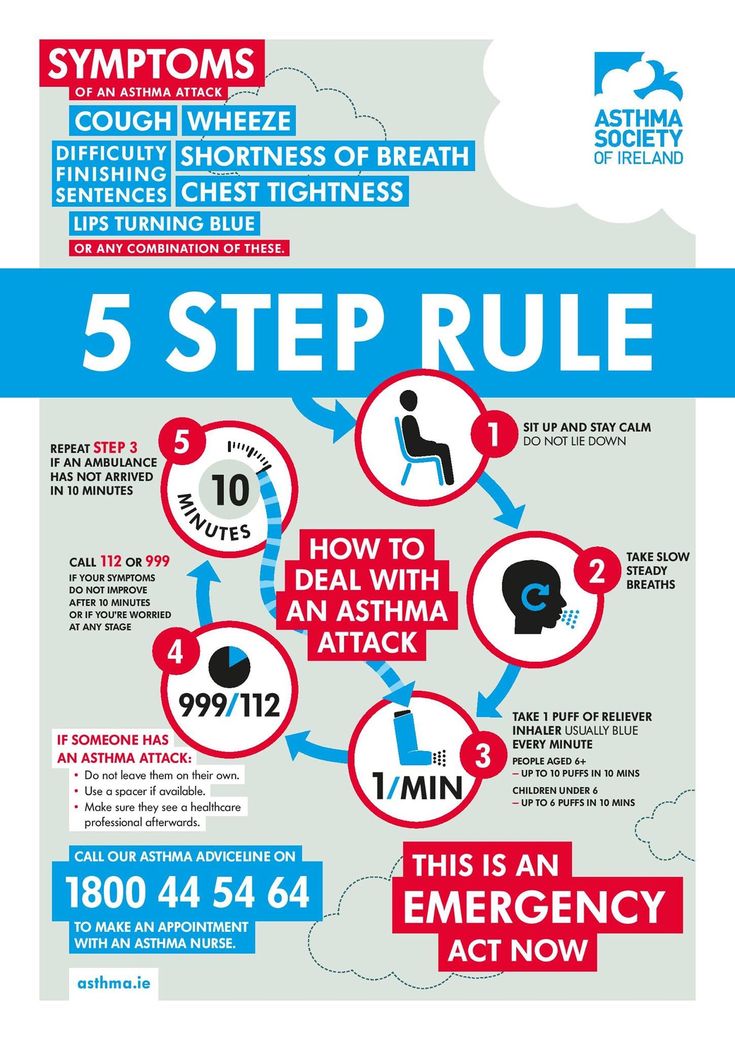
Asthma results from a breathing condition caused by swollen airways that constrict the passage of air. Common symptoms include dry cough, shortness of breath, and wheezing. It’s a common childhood condition, affecting over eight percent of children in the United States.
However, people of all ages develop asthma. Childhood asthma may disappear for good in adolescence for some people, while it reemerges for others. Asthma can be controlled, but it can’t be cured, so visiting an asthma specialist like Alpha Internal Medicine is your best choice for limiting the effects of the disease on your life.
Asthma symptoms
While each patient may develop their own combination of asthma symptoms, the overall collection of symptoms and signs of the disease are common. The most frequently experienced effects include:
- Tightness or pain in the chest
- Breathing difficulties, shortness of breath
- Dry cough
- Wheezing upon exhalation
- Sleep difficulties related to breathing
- Cough, wheezing, or breathing difficulties are aggravated by respiratory illnesses
The childhood asthma experience
While the symptom pool is the same for children and adults, there are pattern differences.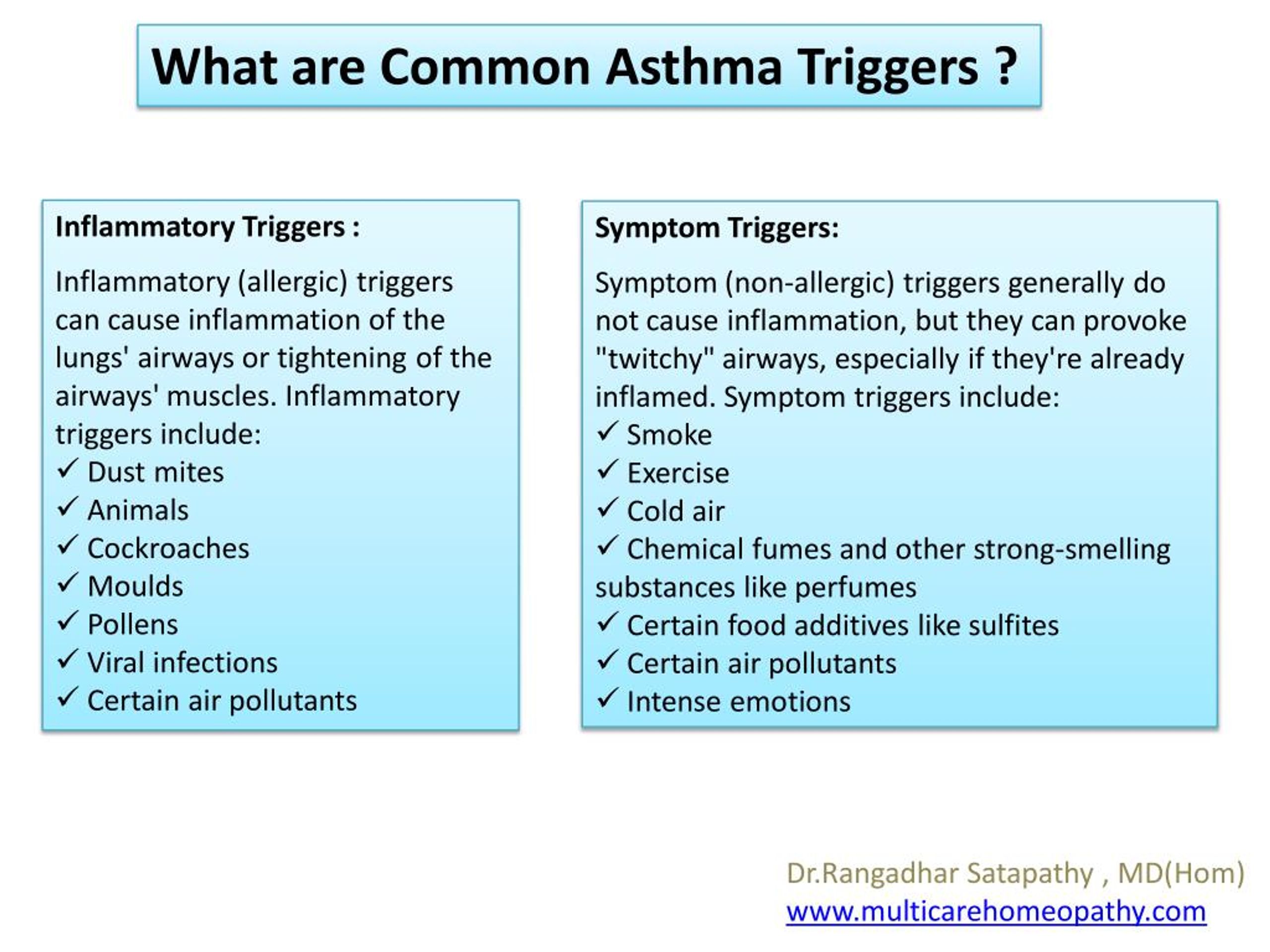 Persistent cough is often the first and only symptom before a child’s asthma diagnosis. You may find that coughing fits follow a pattern, such as during or after vigorous play, at night, or during cold weather. The cough may exist before your child has a cold or flu, and the respiratory infection makes the cough worse.
Persistent cough is often the first and only symptom before a child’s asthma diagnosis. You may find that coughing fits follow a pattern, such as during or after vigorous play, at night, or during cold weather. The cough may exist before your child has a cold or flu, and the respiratory infection makes the cough worse.
Children’s behavior may reveal asthma, too. They could display less energy or a tendency to avoid physical activity. Stopping to catch their breath after light activity could also be suspicious, and coughing may disrupt their sleep.
Wheezing is the classic symptom of asthma in children and when it’s combined with other symptoms, it’s time to bring your child in for diagnosis and treatment.
The differences with adult-onset asthma
Childhood asthma symptoms are typically intermittent, emerging as asthma attacks, while adults tend to show persistent symptoms. Asthma that first shows in older patients may require daily control treatments, such as medications and inhalers.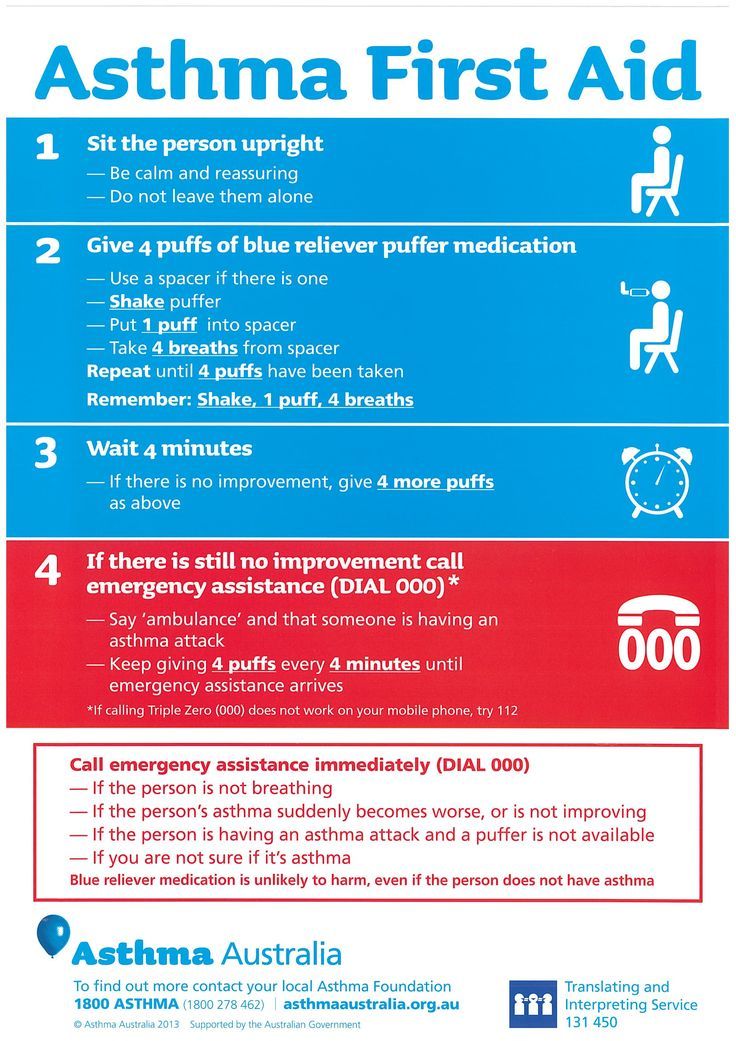
Unlike childhood asthma, which affects more boys than girls, asthma starting after the age of 20 is more common in women than in men. About 30% of adults with asthma have the condition because of related allergies, and being obese increases your risk of developing asthma later in life. Asthma attacks are rarely fatal, but people over 65 are at greater risk.
Asthma treatment
There’s little difference between treatment of asthma in children and adults. Most asthmatics have a two-step plan. Effective control medications, combined with asthma trigger avoidance, help to prevent asthma attacks in the first place, while reducing attack severity when they happen. Combined with this long-term treatment strategy are quick-relief solutions, usually in the form of inhalers.
Devising an effective asthma control plan is crucial, no matter what the age of the patient. This may involve keeping a log of asthma attacks to identify possible triggers, factors that cause attacks, as well as pinpointing effective treatments, what to take, and when to take them.
Contact Alpha Internal Medicine to get the medical assistance you need to create your asthma plan. Call the office directly or request an appointment using the link on this page. Asthma relief is close at hand, so book your consultation now.
Reasons to Consider Sculptra
Dermal fillers are one of the most popular minimally invasive cosmetic treatments in use today, able to fill in lines and wrinkles while adding volume. While Sculptra has much in common with other fillers, it also offers unique advantages.
I'm a Diabetic: What Should I Be Most Concerned About?
The effects of diabetes on your body are widespread. You can suffer problems with your heart and blood circulation, kidneys, eyes, feet, and more. To minimize all problems, your primary concern is control over your blood sugar levels.
5 Benefits of Dysport
Injectable treatments using variations of the botulinum toxin type A are the most requested cosmetic procedure on the market today. Dysport has a unique formulation with its own characteristics that provide natural, long-lasting effects.
Dysport has a unique formulation with its own characteristics that provide natural, long-lasting effects.
The Link Between Drinking Alcohol and Having High Blood Pressure
High blood pressure is a silent killer, compromising your health without signs or symptoms, so understanding its contributing factors helps you avoid the risk. More than moderate use of alcohol raises your blood pressure level.
Can Strep Throat Heal on Its Own?
A common bacterial infection that favors children but can hit you at any age, strep throat usually lasts about a week when left untreated. However, it can be responsible for some serious complications in rare cases.
Understanding the Difference Between Acute and Chronic Bronchitis
What some people think of as a chest cold is actually acute bronchitis, a common condition that develops from a respiratory infection.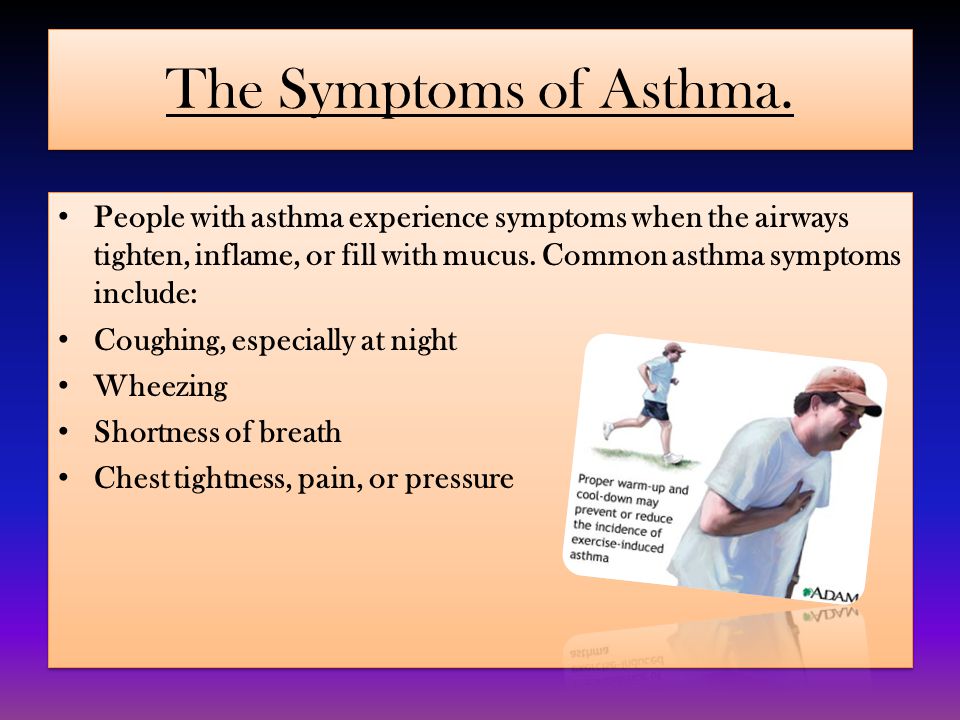 Chronic bronchitis is more serious, lasts longer, or occurs more frequently, and requires medical care.
Chronic bronchitis is more serious, lasts longer, or occurs more frequently, and requires medical care.
Bronchial asthma
Bronchial asthma is a very common disease. Epidemiological studies of recent years indicate that from 4 to 10% of the world's population suffer from bronchial asthma of varying severity.
Bronchial asthma
Bronchial asthma is a very common disease. Epidemiological studies of recent years indicate that from 4 to 10% of the world's population suffer from bronchial asthma of varying severity. In children, this figure is even higher - 15%. We talked with EvroMed Clinic pulmonologist Evgenia Nikolaevna SELIVANOVOY about methods of diagnosing and treating this pathology.
Bronchial asthma is an infectious-allergic disease is a chronic lung disease in which bronchial obstruction occurs. The disease has a hereditary genetic character.
Symptoms of bronchial asthma
Cough. If you suffer from a chronic cough (lasting more than 8 weeks), be sure to consult a pulmonologist! Against the background of a prolonged cough, the risk of developing bronchial asthma is high.
If you suffer from a chronic cough (lasting more than 8 weeks), be sure to consult a pulmonologist! Against the background of a prolonged cough, the risk of developing bronchial asthma is high.
Feeling of tightness in the chest, "congestion", lack of air, as if something is preventing you from breathing.
Shortness of breath, wheezing in the chest, which may increase in a horizontal position.
Frequent colds. Often, when examined by a doctor, it turns out that the patient does not suffer from acute respiratory infections, but from asthma in combination with an allergic reaction. Asthma gives a cough, and allergies give a runny nose.
Any of the above symptoms can signal the onset of bronchial asthma. Therefore, at the slightest doubt, we recommend consulting a pulmonologist, because only a doctor can objectively assess the patient's condition and make a diagnosis.
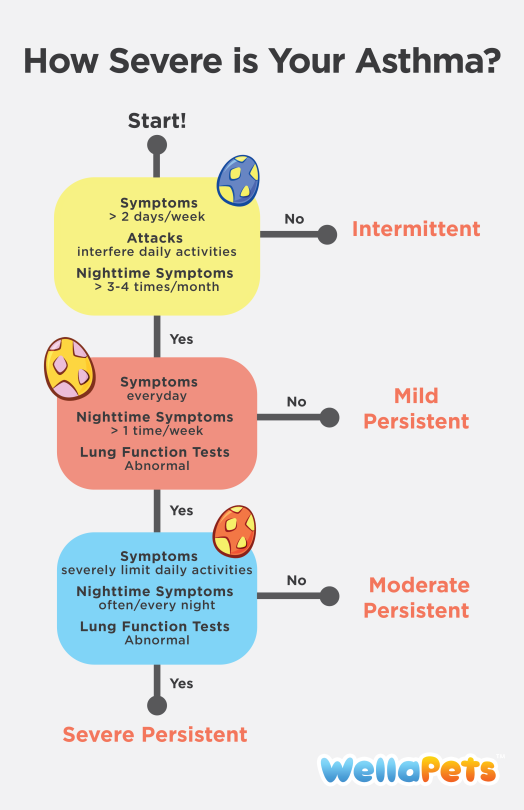
There are 4 degrees of severity of bronchial asthma: intermittent, mild persistent, moderate persistent, severe persistent.
Mild persistent asthma
Symptoms occur once a week or more often, but less than 1 time per day. Exacerbations of the disease can interfere with activity and sleep. Night symptoms occur more often than 2 times a month.
Bronchial asthma of moderate severity
daily symptoms. Exacerbations disrupt activity and sleep. Nocturnal symptoms occur more than once a week.
Severe bronchial asthma
Persistent symptoms, frequent flare-ups, frequent nocturnal symptoms, physical activity limited to asthma symptoms.
Asthma therapy is selected individually, there are no universal treatment regimens. The doctor evaluates many parameters, the form, the severity of the pathology, the individual characteristics of the patient and the presence of concomitant diseases. You can’t prescribe treatment yourself on the principle of “helped by a friend” or “recommended on the Internet”! But the good news is that modern drugs are very effective, and with well-chosen therapy, you can live a full life, forgetting about seizures.
QUESTIONS TO THE DOCTOR
Is it possible to cure bronchial asthma with psychotherapy?
In some types of bronchial asthma, psychogenic mechanisms are involved, and psychotherapy is really needed for effective treatment. But not as monotherapy, but in combination with treatment by a pulmonologist!
Usually, the doctor determines the presence of a psychogenic connection by what the patient himself tells. If asthma attacks are associated with excitement, anxiety, emotional state, then the doctor may recommend a consultation with a psychoneurologist or psychotherapist.
How are asthma and allergies related?
Asthma is an infectious-allergic disease. As is clear from the definition, there is a connection with allergies. One of the most common forms of bronchial asthma is allergic. Allergies can cause the development of bronchial asthma. Also, allergens can be a trigger, a trigger for an asthma attack.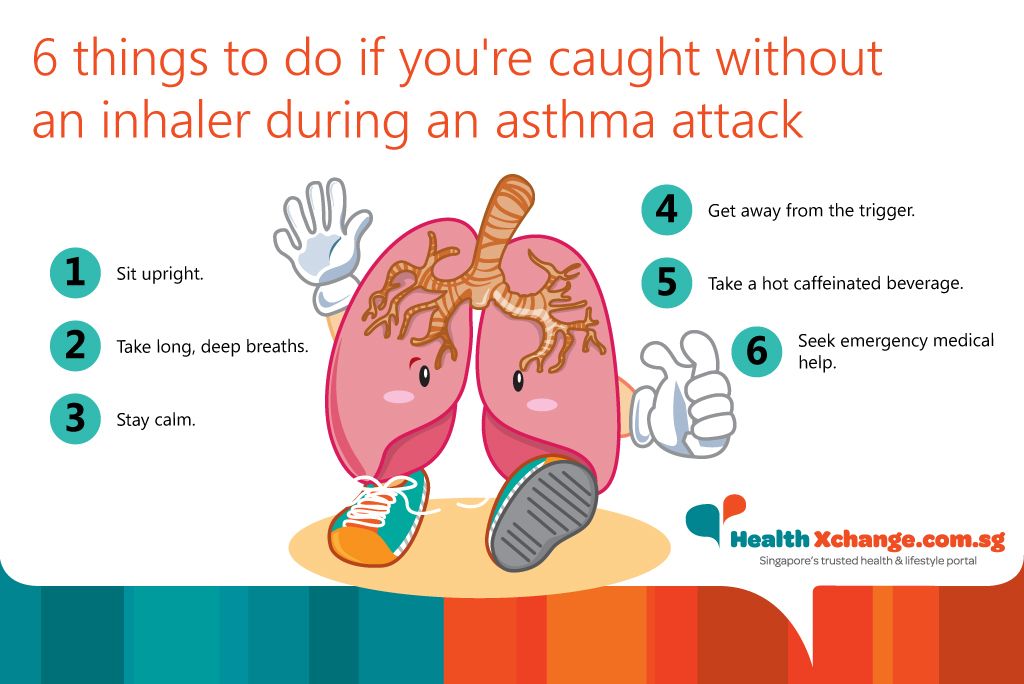 Most often, bronchial asthma is associated with pollinosis (a reaction to the flowering of certain plants), with an allergy to dust and animal hair.
Most often, bronchial asthma is associated with pollinosis (a reaction to the flowering of certain plants), with an allergy to dust and animal hair.
Such bronchial asthma can have a mild intermittent course, and disturb a person only due to the presence of an allergen. That is, only during the flowering period of a certain plant (with hay fever) or when interacting with a dog or cat (with an allergy to wool).
By the way, if you perform ASIT (allregen-specific immunotherapy) and get rid of allergies, then asthma attacks will also pass.
Do I need to change drugs for treatment?
This question has two aspects.
The first is addictive. The answer is: no, properly selected drugs can be taken constantly, they are not addictive. Bronchial receptors, which are affected by an inhalation agent, remain sensitive throughout life.
The second point is related to the fact that in recent years there has been a breakthrough in modern pharmaceuticals in terms of treating bronchial asthma, and many more effective and safe drugs have appeared. Some patients continue treatment, as they were prescribed 30 years ago, with systemic hormones, preparations of the methylxanthines group: aminophylline, theophylline, which today is considered irrelevant and ineffective.
Some patients continue treatment, as they were prescribed 30 years ago, with systemic hormones, preparations of the methylxanthines group: aminophylline, theophylline, which today is considered irrelevant and ineffective.
Therefore, I would like to emphasize once again - if you have been diagnosed with the disease "bronchial asthma", be sure to periodically visit a pulmonologist to control treatment and monitor your condition. In the first year after the diagnosis, it is recommended to visit the doctor every three months so that the doctor can choose the minimum maintenance dose of the drug. Thereafter, at least once a year.
Can asthma be cured?
It is impossible to completely cure bronchial asthma. It always remains as a chronic disease, the symptoms of which are controlled with the right therapy. The only time asthma can go away is during adolescence. During this period, a rapid hormonal restructuring of the body occurs, and a change in the hormonal background can lead to the fact that the child will have a stable remission.
By the way, in connection with a change in the hormonal background, the opposite can also happen - in people of mature age, against the background of a decrease in hormonal levels, bronchial asthma may begin.
symptoms, treatment and prevention
Bronchial asthma (BA)
- All types of examinations, personalized therapy according to modern international protocols, teaching the patient to live with the disease.
- An integrated approach with the participation of doctors of related specialties (pulmonologist, general practitioner, otolaryngologist, rehabilitation specialist, psychotherapist, etc.).
- Modern and effective methods of treatment, including allergen-specific immunotherapy (ASIT).
- 24-hour emergency and ambulance service in the clinic for adults and children: all the necessary tests (spirometry, pulse oximetry), removal of an acute condition.
- Many years of expert experience of EMC allergists allows each patient to successfully fight the disease and maintain quality of life.

Bronchial asthma (BA) has become one of the most common respiratory diseases, and its prevalence in all countries is increasing every year. This led to the creation of a joint report by the World Health Organization and the National Heart, Lung and Blood Institute (USA) called the Global Strategy for the Treatment and Prevention of Bronchial Asthma (GINA). The report is updated annually and its main goal is to translate scientifically proven research results into improved standards of asthma care.
Asthma is a heterogeneous disease characterized by chronic inflammation of the airways, the presence of respiratory symptoms such as wheezing, dyspnoea, chest congestion, and cough that vary in time and intensity and present with variable airway obstruction. This definition of this disease is accepted throughout the world. It most accurately reflects the changes occurring in the patient's body.
The goal of therapy is to achieve stable remission and a high quality of life in all patients, regardless of the severity of the disease.
The stepwise approach to asthma therapy clearly defines which drugs can be selected for a particular patient, taking into account age, frequency of attacks, timing of diagnosis, and previous treatment. The volume of basic therapy is determined by the severity and level of control of bronchial asthma, the age of patients, and the nature of comorbidity. The severity of the course of the disease varies from mild to severe, and the degree of control from complete, in which there are no symptoms, to its absence.
Good asthma control can be achieved in most patients with deliberate pharmaceutical intervention, which is one of the important components of an asthma therapy strategy that also includes inhaler skills, adherence to therapy, as well as non-pharmacological components (regular monitoring, creation of a hypoallergenic environment) and allergen management. -specific immunotherapy.
When prescribing treatment, general and individual questions should be answered: which drug is preferred to achieve control; How is this particular patient different from the “average” AD patient? This is especially important when basic therapy is prescribed for children, since the right tactics can significantly change the long-term prognosis of the disease.
Symptoms of bronchial asthma
Characteristic signs of bronchial asthma:
- wheezing;
- shortness of breath;
- chest tightness;
- cough.
Symptoms are variable in time and intensity and often worse at night or early in the morning. The attack and clinical manifestations of asthma can provoke respiratory viral infections, exercise, weather changes, contact with allergens and non-specific irritants.
In children, the typical clinical symptoms are wheezing, coughing, and dyspnea, often worse at night or on awakening. With the development of an exacerbation of bronchial asthma in children, an obsessive dry or unproductive cough (sometimes to vomiting), noisy wheezing may appear.
Diagnosis of bronchial asthma
The diagnosis of asthma is established on the basis of complaints and data from the patient's medical history, the results of functional examination methods, a specific allergological examination and the exclusion of other diseases.
EMC allergists conduct the necessary examination at the consultation - an important part of it is the collection of anamnesis. In a patient with suspected bronchial asthma, it is necessary to find out the causes of occurrence, the duration of clinical manifestations and resolution of symptoms, the presence of allergic reactions in the patient himself and his close relatives, the causal features of the occurrence of signs of the disease and its exacerbations. In addition, spirometry is performed at the consultation as an initial study to identify and assess the severity of airway obstruction.
All patients with suspected asthma are given a bronchodilator test. The study is necessary to determine the degree of obstruction reversibility under the influence of bronchodilator drugs.
EMC allergists perform peak expiratory flow monitoring. Peak flowmetry is used as an additional diagnostic test. Multiple peak expiratory flow (PEF) measurements performed for at least 2 weeks at home to confirm airflow variability help establish the correct diagnosis.
Laboratory tests include: CBC, total IgE, sputum, chemistry, allergology - skin prick testing and serum total and specific IgE, eosinophilic cationic protein, blood gas.
Instrumental studies: spirometry, peak flowmetry, bronchoscopy, radiography or computed tomography of the lungs, electrocardiography, ultrasound of the heart.
Treatment of bronchial asthma
Therapy includes two main schemes - basic therapy and therapy for exacerbations of bronchial asthma.
The goal of treating exacerbations is to eliminate bronchial obstruction as quickly as possible and prevent further relapses (attacks). In some cases, with severe exacerbations, such assistance is possible only in a hospital setting. In the EMC clinic, such therapy can be carried out at any time of the day.
Basic therapy, according to the Global Strategy for the Treatment and Prevention of Bronchial Asthma, is prescribed using the principle of a stepwise approach to the treatment of this disease.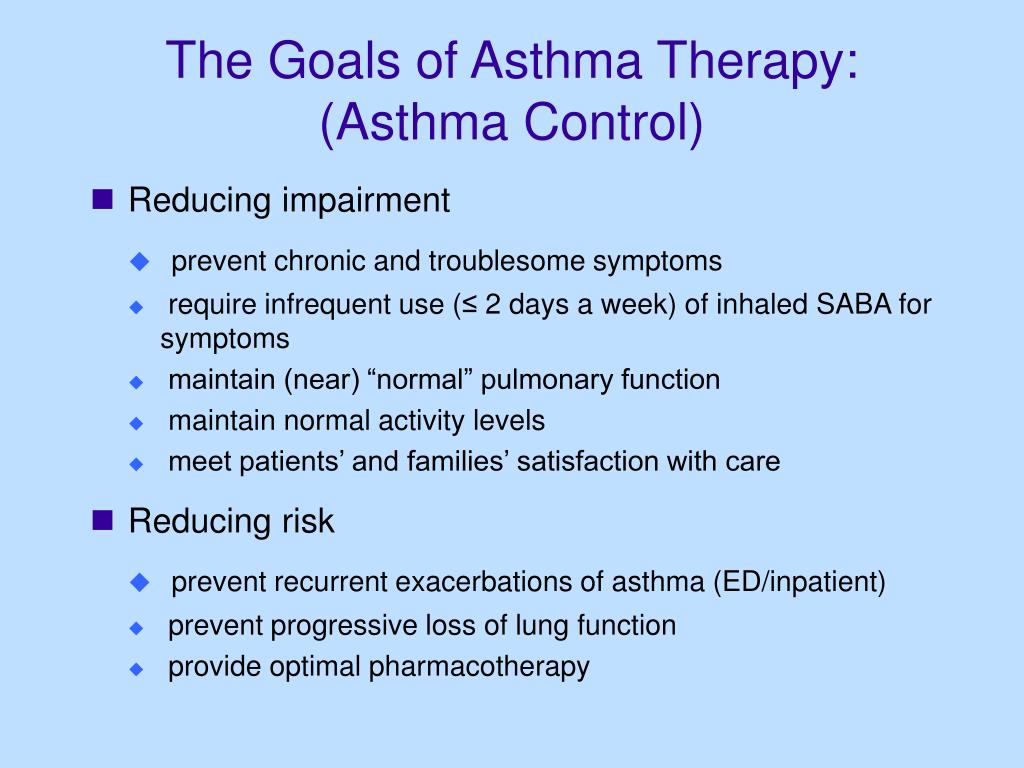 The higher the stage of therapy, the more control drugs that the patient receives and / or the higher their dosages. Inhalation administration of drugs is the main method of treating bronchial asthma.
The higher the stage of therapy, the more control drugs that the patient receives and / or the higher their dosages. Inhalation administration of drugs is the main method of treating bronchial asthma.
For all inhalation preparations, one of the essential components of success is the device with which the preparation reaches its target. Selection of the optimal inhalation device for each individual patient is the task of the doctor prescribing basic therapy.
Basic therapy is an important component in achieving control over the symptoms of bronchial asthma. The drug treatment regimen is reviewed at least once every 3 months, this allows you to achieve control over the disease without using unnecessary drugs.
Successful asthma management requires close collaboration between the patient and the physicians providing care. The patient must be sure that his participation plays one of the main roles in the treatment process. Patient education in the field of bronchial asthma can also help - it allows you to recognize the symptoms of the disease, complications, seek medical help in time and strictly follow the doctor's instructions.
Allergen-specific immunotherapy (ASIT) plays an important role in the treatment of allergic bronchial asthma. An allergist conducts a comprehensive examination, identifies the allergen, the interaction with which leads to an exacerbation of the disease, and draws up the most optimal scheme for allergen-specific immunotherapy. Then increasing doses of the allergen are sequentially introduced into the body. Over time, the immune system becomes resistant to allergens. Successfully performed ASIT allows maintaining a long-term remission of the disease or significantly reducing the amount of basic therapy.
Rehabilitation
For asthma, it is recommended that physical rehabilitation education and methods be included in the rehabilitation program for all patients. The patient education program should include the provision of information about the disease, the development of an individual treatment plan for the patient, and training in the technique of controlled self-management of bronchial asthma.
Physical rehabilitation improves cardiopulmonary function. As a result of training during exercise, the maximum oxygen consumption increases and the maximum ventilation of the lungs increases. According to the available observations, training with aerobic exercise, swimming, training of the inspiratory muscles with a threshold dosed load improve the course of BA. EMC rehabilitation physicians will help to create an individual training plan taking into account the patient's health status, and will teach breathing exercises.
Prevention of exacerbations of bronchial asthma
The key to the success of asthma treatment is disciplined compliance with the doctor's recommendations in full. General health promotion measures are also important - the fight against smoking, overweight, nasal diseases, physical training, and influenza vaccination.
The main advantage of bronchial asthma therapy at EMC is the possibility of remote patient support in any situation using the most modern technologies, training in the use of modern inhalation devices, and ASIT.