What helps varicose veins during pregnancy
Treat Varicose Veins Naturally During Pregnancy
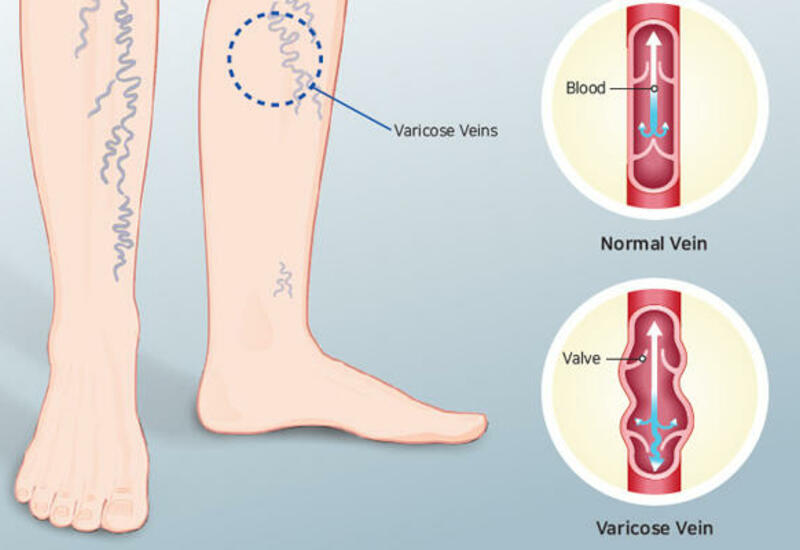
Varicose veins during pregnancy are caused by blood volume increases that put pressure on the veins. Varicose veins are enlarged veins that commonly occur in the legs, although during pregnancy they can also appear on the buttocks and vaginal area. Hormonal changes can also lead to varicose veins during pregnancy as increased progestin levels can dilate or open the veins. In addition, during pregnancy the uterus puts pressure on the inferior vena cava (the vein that carries blood from the legs and feet to the heart), further contributing to varicose veins.
Varicose veins are generally harmless, although they may become itchy and uncomfortable. The good news is they typically diminish within three months to a year after giving birth.
Hemorrhoids are another kind of varicose vein in the anus or rectum that occurs during pregnancy and is oftentimes a result of constipation.
While varicose veins can be hereditary, and you can’t prevent the circulatory changes that occur during pregnancy, there are some ways you can prevent or minimize varicose veins.
These preventative measures are ultimately your best treatment option during pregnancy:
- Avoid sitting or standing in the same position for long periods of time. Make sure to take breaks to change your position.
- Avoid wearing high heels. It is better to wear lower-heel or flat shoes as this works your calf muscles, fostering healthy circulation.
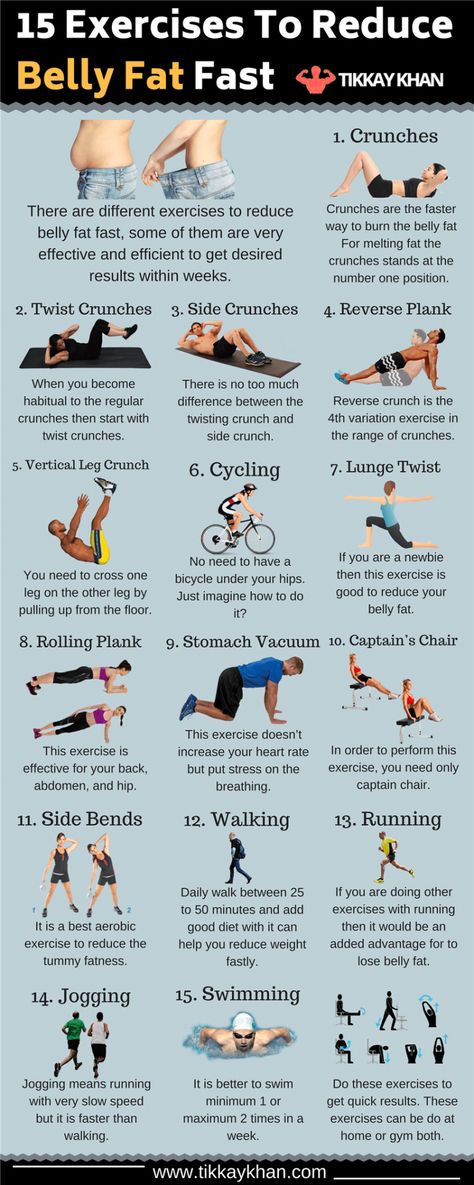
- Get regular exercise. Talk with your doctor to confirm if it is safe for you to exercise during pregnancy.
- Wear maternity support hosiery. These put pressure on the legs, stimulating blood flow up the leg towards the heart. However, avoid wearing tight hose that cut off circulation.
- Avoid crossing your legs while sitting.
- Elevate your legs periodically to improve circulation.
- Sleep on your left side. This will help relieve pressure on the inferior vena cava.
- Reduce sodium intake to minimize swelling of the veins.
- Drink plenty of water and eat enough fiber to prevent constipation.
Warning: Some have used horse chestnut seed extract (with the poisonous esculin removed) to treat varicose veins. However, consuming the raw bark, flower, seed, or leaf of this plant is poisonous and can cause death. The safety of using horse chestnut extract with the esculin removed during pregnancy remains unknown.
Therefore, it is best to avoid using it if you are pregnant or breastfeeding.
How to Treat Varicose Veins Naturally During Pregnancy When Naturally Does Not Work
Varicose vein surgery is not recommend during pregnancy as varicose veins generally improve after giving birth. Contact your doctor if the veins become swollen, warm, tender, or red, if they bleed, if you have a rash on your leg or ankle, or if the skin on leg changes color or thickens.
- Skin Changes During Pregnancy
Compiled using information from the following sources:
1. Aetna Inc. (2015). Clinical policy bulletin: Varicose veins, Number 0050.
Aetna Inc. (2015). Clinical policy bulletin: Varicose veins, Number 0050.
2. Mayo Clinic Staff. (2013, January 31). Varicose veins.
https://www.mayoclinic.org/diseases-conditions/varicose-veins/basics/definition/con-20043474
3. MedlinePlus. (2014) Horse chestnut.
https://www.nlm.nih.gov
4. Murry, M. M. (2013, April 10. Varicose veins and pregnancy: Legs and more.
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-blog/varicose-veins-and-pregnancy/bgp-20055799
5. Nemours. (2013). Why do some pregnant women get varicose veins?
https://kidshealth.org/parent/question/infants/veins.html
6. Office on Women’s Health, U.S. Department of Health and Human Services. (2012). Varicose veins and spider veins fact sheet.
Varicose veins during pregnancy | BabyCenter
- Pregnancy
- Your Body
By Eva Dasher
|
|
December 30, 2020
Many women first develop varicose veins – or find that they get worse – during pregnancy. You're more likely to get varicose veins if other members of your family have had them. The good news for some women is that varicose veins may improve or disappear after you give birth, especially if you didn't have any before you got pregnant.
You're more likely to get varicose veins if other members of your family have had them. The good news for some women is that varicose veins may improve or disappear after you give birth, especially if you didn't have any before you got pregnant.
Photo credit: Thinkstock
- What are varicose veins?
- What causes varicose veins during pregnancy?
- How can I prevent varicose veins in pregnancy?
- Can compression stockings help prevent varicose veins?
- Are varicose veins in pregnancy ever serious?
- How should I treat my varicose veins after pregnancy?
What are varicose veins?
Varicose veins are unusually swollen veins that may bulge near the surface of the skin. These blue, red, or purple veins sometimes look squiggly or ropelike and are most likely to show up on your legs, though in pregnancy it's possible to get them on your lower pelvic area, buttocks, or elsewhere. (Hemorrhoids are just varicose veins in the rectal area. )
)
Many women first develop varicose veins – or find that they get worse – during pregnancy. You may have little or no discomfort from varicose veins, or they may make your legs feel heavy and achy. The skin around a varicose vein may also itch, throb, or feel like it's burning. The symptoms tend to be worse at the end of the day, especially if you've been on your feet a lot.
What causes varicose veins during pregnancy?
As your uterus grows, it puts pressure on the large vein on the right side of your body (the inferior vena cava), which increases pressure in your leg veins.
Veins are the blood vessels that return blood from your extremities to your heart, so the blood in your leg veins is already working against gravity. And when you're pregnant, the amount of blood in your body increases, adding to the burden on your veins. Your progesterone level also rises, relaxing the walls of your blood vessels.
You're more likely to get varicose veins if other members of your family have had them.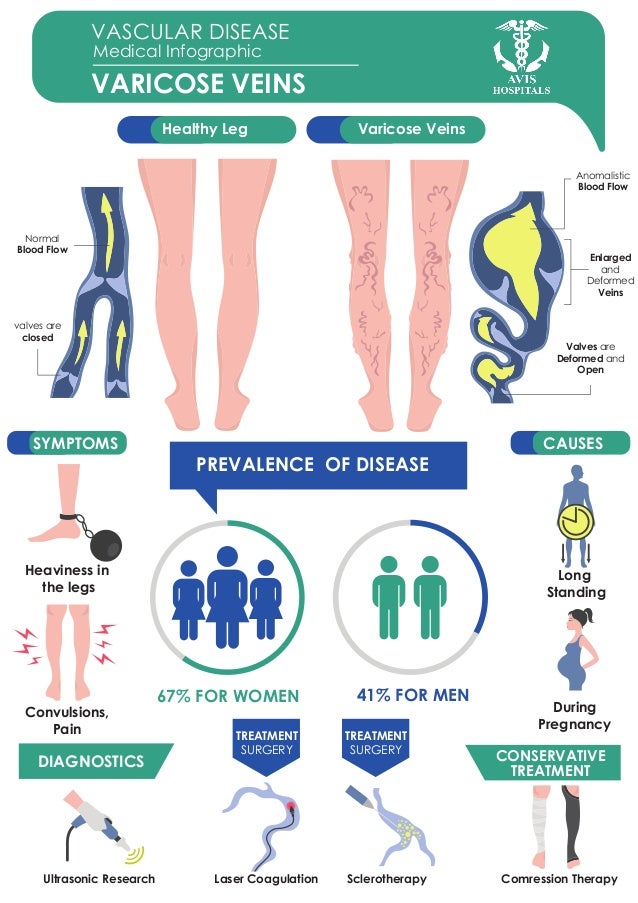 They're more common in women than men, and if you have them, they tend to get worse with each successive pregnancy and as you get older. Being overweight, carrying twins or other multiples, and standing for long periods can also make you more likely to get them.
They're more common in women than men, and if you have them, they tend to get worse with each successive pregnancy and as you get older. Being overweight, carrying twins or other multiples, and standing for long periods can also make you more likely to get them.
The good news for some women is that varicose veins may improve or disappear after you give birth, especially if you didn't have any before you got pregnant. And if they don't get better, you can look into various treatment options after your baby is born.
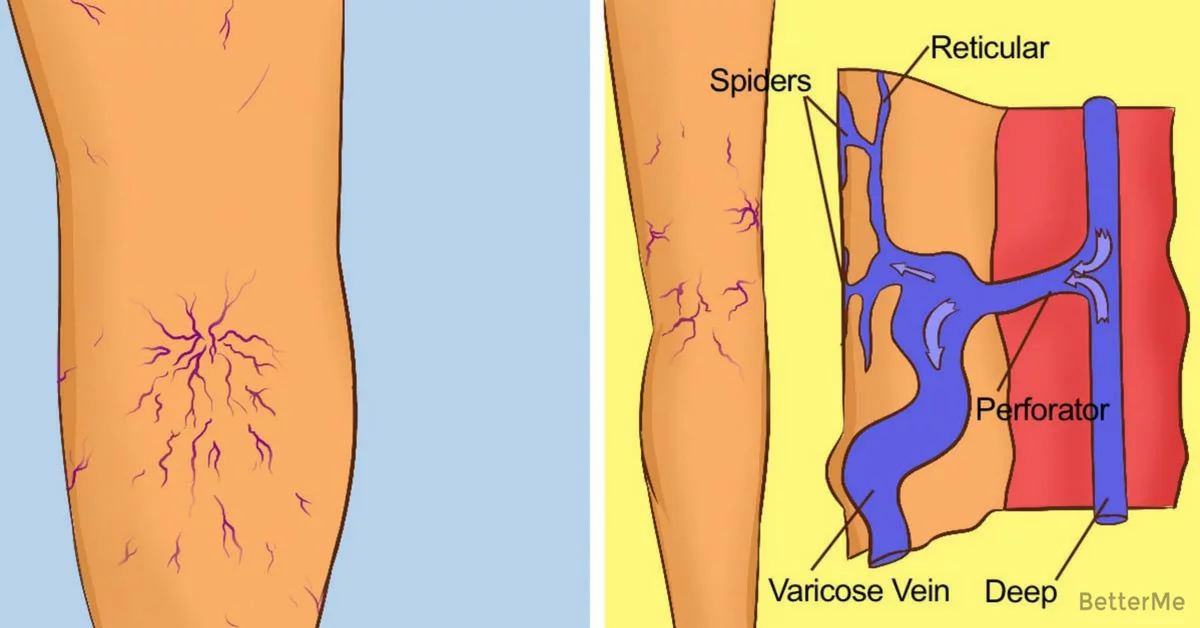
You may have also noticed tiny blood vessels near the surface of the skin, especially on your ankles, legs, or face. These are called spider veins because they often appear in a spider-like pattern, with little branches radiating out from the center. (Though sometimes they may look more like the branches of a tree or separate thin lines with no specific pattern.)
These don't cause discomfort, and they typically disappear after delivery.
How can I prevent varicose veins in pregnancy?
You may be able to prevent, or at least minimize, varicose veins while you're pregnant if you:
- Exercise daily.
 Even just a brisk walk around the block can improve your circulation.
Even just a brisk walk around the block can improve your circulation. - Stay within the recommended weight range for your stage of pregnancy.
- Elevate your feet and legs to the level of your heart or higher whenever possible. Rest your legs on a tall stool or box when you're sitting and elevate your feet and legs with pillows when you're lying down.
- Don't cross your legs or ankles when sitting.
- Don't sit or stand for long periods of time. Take frequent breaks to move around.
Can compression stockings help prevent varicose veins?
Yes. Compression stockings put pressure on your veins and increase the blood flow from your legs. There are three kinds of compression stockings:
- Support pantyhose: These can be found online or in most stores and will provide the least amount of pressure.
- Over-the-counter gradient compression hose: Tighter at the feet and ankles and looser as they go up your legs, these make it easier for blood to flow back up toward your heart.
 As a result, they help prevent swelling and may keep your varicose veins from getting worse. They’re available online or at pharmacies and medical supply stores. You can ask your doctor or midwife to help you make sure yours fit properly. (Morning is the best time to check for a proper fit because that's when you have the least swelling.)
As a result, they help prevent swelling and may keep your varicose veins from getting worse. They’re available online or at pharmacies and medical supply stores. You can ask your doctor or midwife to help you make sure yours fit properly. (Morning is the best time to check for a proper fit because that's when you have the least swelling.) - Prescription-strength gradient pressure hose: These will offer the greatest amount of pressure at your feet, ankles, and lower legs. You may need a prescription from your doctor or midwife to buy them and your medical insurance may cover the cost. You’ll need to be fitted by a professional and can buy them at some drugstores and medical supply stores.
Put on the stockings before you get out of bed in the morning (while you're still lying down) and keep them on all day to prevent blood from pooling in your legs.
You may have heard advice that sleeping on your left side can help prevent varicose veins. The theory goes that because the inferior vena cava is on the right side of your body, lying on your left side takes the weight of your uterus off the vein, relieving the pressure on the veins in your legs and feet. Although providers sometimes recommend it anyway, there's no proof to support the claim that sleeping this way prevents varicose veins.
Although providers sometimes recommend it anyway, there's no proof to support the claim that sleeping this way prevents varicose veins.
Are varicose veins in pregnancy ever serious?
Varicose veins may itch or hurt, and they can be unsightly, but they're generally harmless in the short term. Treatment, if needed, can usually be postponed until after you have your baby.
However, a small percentage of people who have varicose veins develop small blood clots near the skin's surface (superficial venous thrombosis). When this kind of clot develops, the vein may feel hard and cord-like, and the area around it may become red, hot, tender, or painful.
Call your doctor or midwife if you think you have one of these clots because they can be serious. During pregnancy, they can be treated with warm compresses and will usually subside in a few days or weeks. Occasionally the area surrounding a clot becomes infected. You may develop a fever or chills in that case, and you'll need to be treated promptly with antibiotics.
Also, call your provider right away if:
- Either leg becomes severely swollen.
- You develop sores on your leg.
- The skin near the veins changes color.
In rare cases, superficial venous thrombosis can progress to deep vein thrombosis (DVT), a more serious condition in which a clot develops in deep veins, usually in the legs, and could become inflamed or travel to the lungs and be life-threatening.
Pregnancy makes DVT more likely whether or not you have varicose veins, but DVT isn't common: Your chance of developing it – either during pregnancy or in the weeks after you give birth – is about 1 in 1,600. (Women with blood clotting disorders, obesity, multiple gestation or who are on prolonged bedrest have a higher risk.)
If you develop DVT, you may have no symptoms, or you may have sudden, painful swelling in your ankle, leg, and thigh. It may hurt more when your foot is flexed or when you're standing, and you may have a slight fever as well. If you notice any of these symptoms, call your provider immediately.
If you notice any of these symptoms, call your provider immediately.
You may need to have an ultrasound exam of the affected area. And if you do have one of these clots, you'll need to be hospitalized and treated with blood-thinning medication.
Left untreated, the clot could break away and travel to the lungs, resulting in a life-threatening condition called a pulmonary embolism. Signs of a pulmonary embolism include shortness of breath, painful breathing, a cough (or coughing up blood), a panicky feeling, and a rapid heartbeat. If you have any of these symptoms, call 911.
How should I treat my varicose veins after pregnancy?
After you give birth, it's a good idea to continue to wear compression stockings, exercise regularly, don't sit or stand for long periods of time, and elevate your legs whenever possible.
Varicose veins often improve within three to four months after giving birth, though sometimes it takes even longer – and sometimes they don't improve much at all. (This is more likely if you've had multiple pregnancies.)
(This is more likely if you've had multiple pregnancies.)
If your varicose veins persist and become too uncomfortable to live with, or even if you're just unhappy with how they look, ask your provider to refer you to a specialist to find out about other treatment options.
Learn more:
- Swollen feet, ankles, and hands (edema) during pregnancy
- Itching during pregnancy
- Help for common pregnancy skin problems
Sources
BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies.
AAFP. 2020. Deep vein thrombosis. American Academy of Family Physicians. https://familydoctor.org/condition/deep-vein-thrombosis/ [Accessed November 2020]
American Academy of Family Physicians. https://familydoctor.org/condition/deep-vein-thrombosis/ [Accessed November 2020]
ACOG. 2011. FAQ 174: Preventing deep vein thrombosis. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/preventing-deep-vein-thrombosis [Accessed November 2020]
NIH. 2020. Varicose veins. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/001109.htm [Accessed November 2020]
OWH. 2019. Varicose veins and spider veins. Office on Women’s Health. https://www.womenshealth.gov/a-z-topics/varicose-veins-and-spider-veins [Accessed November 2020]
Show more
advertisement | page continues below
advertisement
Featured video
All pregnancy, parenting, and birth videos >
Varicose veins during pregnancy - what to do and how to treat varicose veins in the legs
Varicose veins are persistent and irreversible enlargement resulting from pathological changes in the walls and valves of blood vessels. The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
Causes
The following reasons contribute to the occurrence of varicose veins during pregnancy:
- Violation of the outflow of blood from the veins of the lower extremities. This is because the growing uterus presses on the inferior vena cava - a large abdominal vein that collects blood from the lower half of the trunk and lower extremities.
- During pregnancy, the blood is more viscous, flows more slowly, this also contributes to venous congestion.
- The increase in body weight during gestation increases the load on the legs.
The development of varicose veins is promoted by wearing high-heeled shoes, prolonged work in a standing position, lifting weights, and overweight.
Symptoms
The first symptom is a visible increase in the vessels of the lower extremities. The veins are blue or purple, tortuous, protrude above the surface of the skin, may be serpentine or knobby (nodular) in shape. At the initial stage of the disease, a woman is only concerned about a cosmetic defect.
Other complaints follow. Edema appears, increasing in the evening and decreasing or completely disappearing after rest and a night's sleep. At night, convulsions may disturb. When walking, rapid fatigue is observed, there may be a feeling of fullness and pain.
Varicose veins of the lower extremities are observed in 50% of pregnant women, but not all of them suffer from true varicose veins, when irreversible changes appear in the venous wall. For most, the disease is functional in nature, that is, it is temporary, and after childbirth, when the factors that prevent normal venous outflow are eliminated, the tubes return to normal. This usually happens within a year.
Regression does not occur if the predisposition is independent of pregnancy. In this case, close relatives usually have varicose veins, or the woman herself had some symptoms even before conception.
Diagnostics
As you know, the “gold standard” for diagnosing pathology is ultrasound duplex scanning (USDS) of the veins of the lower extremities. This is a safe procedure for the expectant mother. Experienced obstetricians and gynecologists strongly recommend that pregnant women visit a phlebologist in the early stages of pregnancy, which contributes to the early prevention of complications of varicose veins in the postpartum period.
Stockings for varicose veins during pregnancy
During pregnancy, it is recommended to wear special compression (anti-varicose) tights and stockings. They need to be put on in a prone position, slightly lifting the leg up. There are 4 compression classes (pressure levels):
- 18-21 mmHg
- 23-32 mmHg
- 33-48 mmHg
- over 49 mmHg
During pregnancy, it is recommended to use compression class 1-2. The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
Tights should be specially designed for expectant mothers so that they do not put pressure on the growing belly, but support it.
How much to wear?
After 20 weeks, you need to wear a bandage. It supports the uterus and reduces pressure on the large vessels of the abdominal cavity, thereby improving the outflow of blood from the lower half of the body.
Compression underwear and a bandage should be bought in pharmacies, it is important to choose the right size for them.
Exercise
It is recommended to attend gymnastics for pregnant women or do exercises at home. Particularly good prevention of varicose veins are classes in the pool. Sports strengthen the walls of blood vessels and improve blood flow. In addition, gymnastics is the prevention of overweight.
A contrast shower on the calf muscles is useful.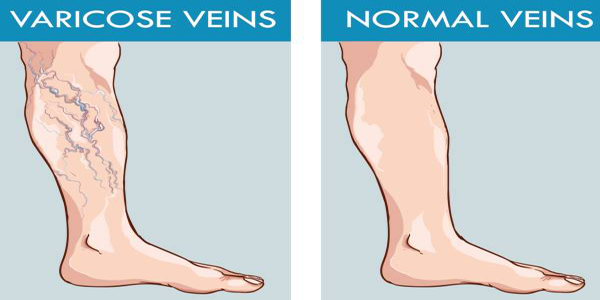
If you think you have a predisposition to varicose veins, you should avoid saunas and thermal treatments.
As often as possible, try to give your legs an elevated position. Don't sit cross-legged for long periods of time.
Wear comfortable shoes with small heels.
You can use creams for pregnant women "to relieve fatigue from the legs", such creams usually contain plant substances that, with regular use, strengthen the walls of superficial veins.
Treatment
Treatment of true varicose veins is surgical. During pregnancy, surgical treatment is carried out only for emergency indications, in view of the development of complications (thrombophlebitis).
A modern method of treatment is sclerotherapy, when a chemical substance is injected into the lumen of the vein, which leads to sclerosis and closure of its lumen. Endovasal methods are also minimally invasive methods of treatment performed on an outpatient basis (described in the relevant sections of our website). They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
All other methods are aimed only at preventing the disease from developing and temporarily reducing symptoms.
Most often, various ointments and gels are used, which are applied to the affected limb. For example, heparin-containing ointments reduce blood clotting and prevent the formation of blood clots. Venotonics (allowed only from the second trimester of pregnancy) have a decongestant and anti-inflammatory effect and strengthen the walls of blood vessels.
The diagnostic equipment used in our center has been tested in ROSTEST and has an appropriate conclusion about the absence of contraindications for use in pregnant women and children.
In the medical center "Yuzhny" they are very kind to expectant mothers and experienced phlebologists are well versed in the methods of diagnosing CVI and the secrets of preserving your beautiful legs after childbirth.
Varicose veins during pregnancy - what to do and how to treat
Veins are actively involved in the complex 9-month pregnancy process, and their changes are significant. Even with complete medical supervision, there is a risk of developing venous insufficiency.
Pregnancy is accompanied by profound changes throughout the female body. One of the first effects of pregnancy is an increase in the load on the veins of the pelvis and lower extremities. Therefore, many pregnant women develop varicose veins, which sometimes disappear after childbirth. This varicose vein is accompanied by discomfort, a feeling of heaviness, pain when walking, but women are mainly concerned with noticeable skin changes and varicose coloration of the legs and ankles, which remain after pregnancy.
From sickness to sickness
Many pregnant women are familiar with the feeling of malaise, accompanied by discomfort in the lower extremities. Functional chronic venous insufficiency is the first stage of venous disease with a feeling of heaviness in the lower extremities, sometimes with itching, paresthesias and, in some cases, convulsions, often nocturnal.
The possibility of thrombosis in pregnant women is 3-5 times higher than in other women. Sometimes blockage of the veins leads to their inflammation - thrombophlebitis. Blood clots that form in this case in the veins can cause a serious and dangerous disease - pulmonary embolism. In addition, the risk of developing thrombosis remains for another 1.5 months after childbirth, especially if they are severe.
Should I go to the doctor?
There are five groups of factors that affect the body of a pregnant woman, which explain the need for observation by a phlebologist.
Mechanical factor
An enlarged uterus is a barrier to blood circulation, as it compresses the inferior vena cava, pressing it against the spinal column and iliac muscle. This is of particular importance at rest, when a sharp decrease in venous outflow can lead to postural shock, well known to gynecologists. The anatomical structure of the iliac vein, which crosses the right iliac artery, explains the high incidence of thrombosis of the left limb (Cocket's syndrome).
Circulatory factor
An increase in blood volume and outflow of blood from the heart leads to an increase in the load on the vessels, especially veins, and their expansion. This is especially important for the veins of the lower extremities and the vaginal area.
Hormonal factors
Progesterone, due to its relaxing effect on smooth muscle fibers, leads not only to a decrease in the tone of the venous wall, but also to a decrease in the tone of the urethra, bladder and small intestine.
Hemostatic factors
Changes in the hemostasis system always occur in the direction of increased coagulability (increased fibrinogen and factor III levels, increased platelet activity and decreased fibrinolytic activity).
Hemorheological factors
Blood viscosity increases despite a decrease in hematocrit.
Other contributing factors
In addition to the above factors associated with pregnancy, there are other contributing factors such as a family history, sedentary lifestyle, immobile posture while working, driving, too low or high thin heels, obesity, underfloor heating, hot baths, and multiple pregnancies with short intervals between them.