Blood pressure medication safe during pregnancy
High blood pressure treatment in pregnancy is safe, prevents maternal heart risks
Statement Highlights:
- High blood pressure during pregnancy remains a major cause of maternal and fetal pregnancy-related complications and death, and it increases women’s short- and long-term risks for cardiovascular disease.
- Emerging data from clinical trials and observational research support the benefits and safety of blood pressure treatment during pregnancy.
- Continued investigation is critical to determine which blood pressure levels, during- and post-pregnancy, both for starting therapy and as treatment goals, are beneficial for the mother and safe and beneficial for the fetus.
- The statement advises multidisciplinary, team-based personalized care where clinicians partner with the patient to determine preferred treatment and consider the risks for hypertension-related adverse outcomes
Embargoed until 4 a. m. CT / 5 a.m. ET Wednesday, Dec. 15, 2021
DALLAS, Dec. 15, 2021 — Treatment for high blood pressure during pregnancy appears safe for many women and may reduce maternal risk for severe hypertension without increasing fetal and neonatal risks, according to a new American Heart Association scientific statement published today in the Association’s journal Hypertension.
A scientific statement is an expert analysis of current research and may inform future clinical practice guidelines. In this statement, “Hypertension in Pregnancy: Diagnosis, Blood Pressure Goals, and Pharmacotherapy,” experts in obstetrics and gynecology, maternal-fetal medicine, cardiology, nephrology, hypertension and internal medicine reviewed and analyzed quality studies focusing on high blood pressure during pregnancy including gestational hypertension and preeclampsia/eclampsia.
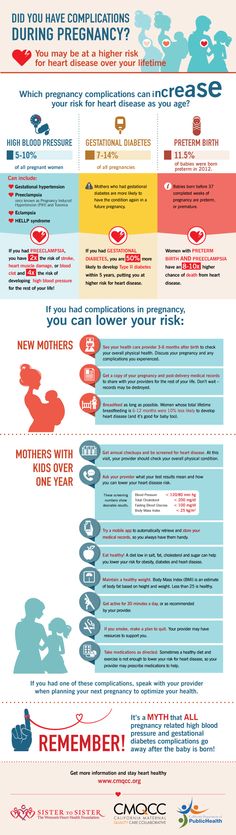
The latest American Heart Association statistics indicate hypertension during pregnancy, defined as a systolic pressure (the top number in a blood pressure reading) of 140 mm Hg or higher, is the second leading cause of maternal death worldwide. Severe cases are associated with increased risks of cardiovascular complications for mothers immediately or soon after delivery, and for years after pregnancy. Hypertension during pregnancy increased the risks for complications for the offspring such as preterm delivery, small for gestational age and low birthweight. Rates of hypertension during pregnancy are increasing globally, and the data indicate that it disproportionately affects women who are from diverse racial and ethnic backgrounds in the U.S., particularly those who are Black, American Indian or Alaskan Native.
Severe cases are associated with increased risks of cardiovascular complications for mothers immediately or soon after delivery, and for years after pregnancy. Hypertension during pregnancy increased the risks for complications for the offspring such as preterm delivery, small for gestational age and low birthweight. Rates of hypertension during pregnancy are increasing globally, and the data indicate that it disproportionately affects women who are from diverse racial and ethnic backgrounds in the U.S., particularly those who are Black, American Indian or Alaskan Native.
The goals of treatment during pregnancy include preventing severe hypertension and preventing early delivery to allow the fetus time to mature before delivery.
“For decades, the benefits of blood pressure treatment for pregnant women were unclear. And there were concerns about fetal well-being from exposure to antihypertensive medications,” said Chair of the statement writing group Vesna D. Garovic, M.D., Ph. D., a professor of medicine, chair of the division of nephrology and hypertension with a joint appointment in the department of obstetrics and gynecology at Mayo Clinic in Rochester, Minnesota. “Through our comprehensive review of the existing literature, it is reassuring to see emerging evidence that treating high blood pressure during pregnancy is safe and effective and may be beneficial at lower thresholds than previously thought. Now, we have the current statement focused on hypertension during pregnancy to help inform optimal treatment and future research.”
D., a professor of medicine, chair of the division of nephrology and hypertension with a joint appointment in the department of obstetrics and gynecology at Mayo Clinic in Rochester, Minnesota. “Through our comprehensive review of the existing literature, it is reassuring to see emerging evidence that treating high blood pressure during pregnancy is safe and effective and may be beneficial at lower thresholds than previously thought. Now, we have the current statement focused on hypertension during pregnancy to help inform optimal treatment and future research.”
According to the statement, among high-income countries, the United States has one of the highest hypertensive-related maternal mortality rates. Cardiovascular disease, which includes stroke and heart failure, now accounts for up to half of all maternal deaths in the U. S, and pregnancy-related stroke hospitalizations increased more than 60% from 1994 to 2011. Preeclampsia, which occurs when hypertension during pregnancy is accompanied by signs of liver or kidney problems such as protein in the urine, affects 5% to 7% of pregnancies and is responsible for more than 70,000 maternal deaths and 500,000 fetal deaths worldwide every year, according to the American Heart Association.
“Given the rising number of cases of hypertension during pregnancy, together with hypertension-related complications, the problem has become a public health crisis, particularly among women from racially and ethnically diverse backgrounds,” Garovic said.
While the definition of hypertension for the general population is established at 130/80 mm Hg according to the 2017 in the American College of Cardiology (ACC)/ American Heart Association (AHA) Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults, most guidelines worldwide define hypertension during pregnancy as 140/90 mm Hg.
There is a lack of consensus about when to start hypertension treatment during pregnancy because of concerns about how medications may impact the fetus. Several health advocacy groups recommend beginning treatment when blood pressure measures during pregnancy are from 140/90 mm Hg (Canadian guidelines) to 160/110 mm Hg (U.S. guidelines).
The new statement points to evidence that blood pressure-lowering therapy for pregnancy hypertension significantly reduces the incidence of severe hypertension.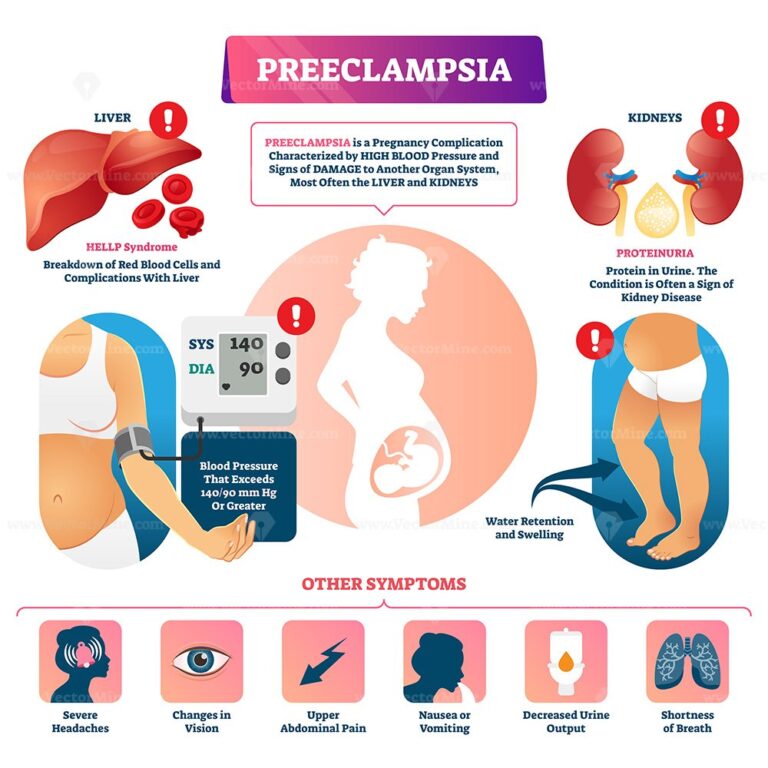 Additional research is needed to determine the extent to which treating hypertension at a lower threshold may decrease serious hypertensive complications, namely organ damage and hypertensive emergencies. Reducing severe hypertension may be particularly important in communities that lack resources and expertise to respond to hypertension emergencies, the statement authors write.
Additional research is needed to determine the extent to which treating hypertension at a lower threshold may decrease serious hypertensive complications, namely organ damage and hypertensive emergencies. Reducing severe hypertension may be particularly important in communities that lack resources and expertise to respond to hypertension emergencies, the statement authors write.
“Future studies should address whether lowering the threshold for treating hypertension during pregnancy might allow for safe and timely blood pressure control and avoid a rushed delivery because of uncontrolled hypertension,” said Garovic.
So far, the latest research indicates that treating hypertension during pregnancy with blood pressure-lowering medicine does not appear to negatively impact fetal growth or development. Preventing hypertension during pregnancy supports maternal health both during and after pregnancy. It is well known that those who have hypertension during pregnancy are more likely to develop sustained hypertension after pregnancy at a higher rate compared to those whose blood pressure was normal during pregnancy. The statement reinforces recent research that suggests lifestyle changes before and during pregnancy have the potential to improve maternal and fetal outcomes:
The statement reinforces recent research that suggests lifestyle changes before and during pregnancy have the potential to improve maternal and fetal outcomes:
- Dietary changes before and during pregnancy can limit weight gain and improve pregnancy outcomes.
- Exercise during pregnancy may reduce gestational hypertension risk by about 30% and preeclampsia risk by about 40%.
The statement also highlights these areas of concern:
- There is emerging evidence that hypertension after delivery (postpartum) may be associated with significant maternal health problems.
- The current science suggests physicians should individualize treatment decisions, considering risk factors and patient preferences.
- The care of women with hypertension during pregnancy is often complex, and a multispecialty team of health care professionals may be beneficial.
“Future clinical trials are needed to address questions about when to begin treatment for high blood pressure during pregnancy,” Garovic said.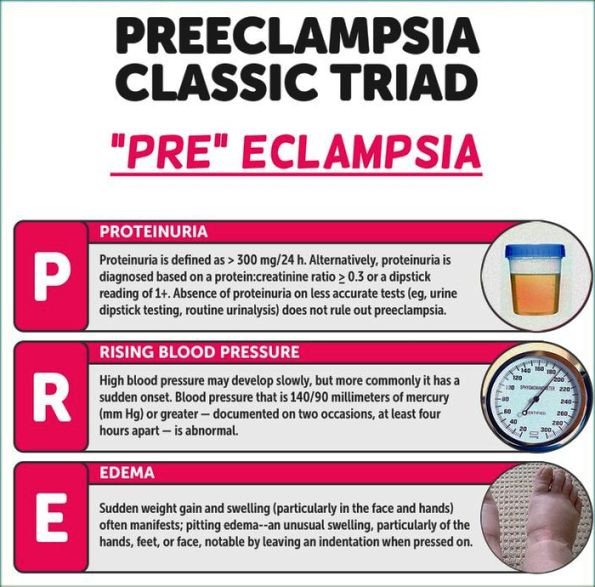 “Also, close collaboration between the American Heart Association and American College of Obstetricians and Gynecologists will be instrumental in optimizing diagnosis and treatment of hypertension during pregnancy and in improving immediate and long-term outcomes for many women who develop hypertension during pregnancy.”
“Also, close collaboration between the American Heart Association and American College of Obstetricians and Gynecologists will be instrumental in optimizing diagnosis and treatment of hypertension during pregnancy and in improving immediate and long-term outcomes for many women who develop hypertension during pregnancy.”
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension; the Council on the Kidney in Cardiovascular Disease Science Subcommittee; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Lifestyle and Cardiometabolic Health; the Council on Peripheral Vascular Disease; and the Stroke Council. American Heart Association scientific statements promote greater awareness about cardiovascular diseases and stroke issues and help facilitate informed healthcare decisions. Scientific Statements outline what is currently known about a topic, and what areas need additional research. While scientific statements inform the development of guidelines, they do not make treatment recommendations. American Heart Association guidelines provide the Association’s official clinical practice recommendations.
While scientific statements inform the development of guidelines, they do not make treatment recommendations. American Heart Association guidelines provide the Association’s official clinical practice recommendations.
Co-authors are Vice Chair Phyllis August, M.D., M.P.H.; Ralf Dechend, M.D.; S. Ananth Karumanchi, M.D.; Suzanne McMurtry Baird, D.N.P., R.N.; Thomas Easterling, M.D.; Laura A. Magee, M.D.; Sarosh Rana, M.D., M.P.H.; and Jane V. Vermunt, M.B.Ch.B., M.Sc. Authors’ disclosures are listed in the manuscript.
The Association receives funding primarily from individuals. Foundations and corporations (including pharmaceutical, device manufacturers and other companies) also make donations and fund specific Association programs and events. The Association has strict policies to prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers and health insurance providers and the Association’s overall financial information are available here.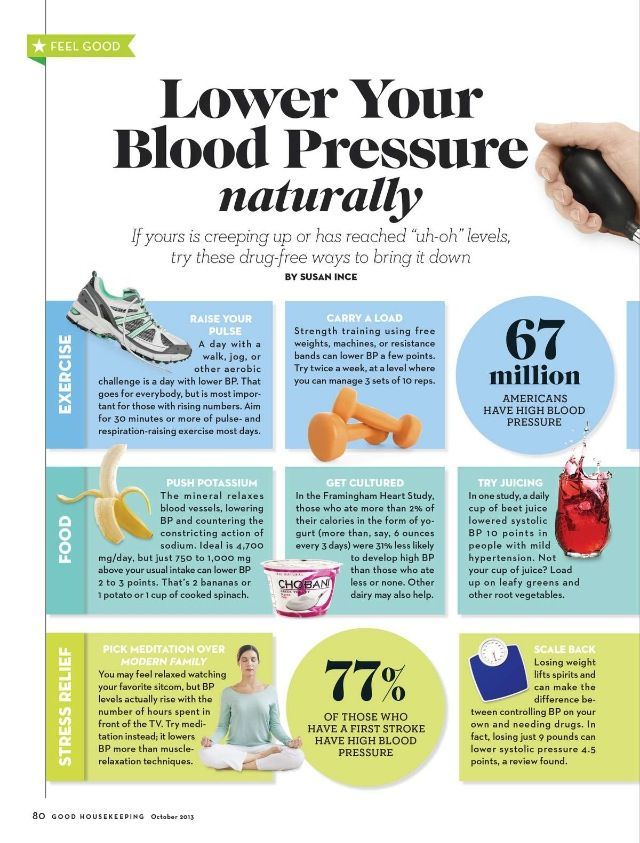
Additional Resources:
- Available multimedia is on right column of release link: https://newsroom.heart.org/news/high-blood-pressure-treatment-in-pregnancy-is-safe-prevents-maternal-heart-risks?preview=975db88ec84a385b9413dcded11b99bd
- After Dec. 15, view the manuscript online.
- Call to Action: Maternal Health and Saving Mothers: A Policy Statement from the American Heart Association
- Promoting Risk Identification and Reduction of Cardiovascular Disease in Women Through Collaboration With Obstetricians and Gynecologists: A Presidential Advisory From the American Heart Association and the American College of Obstetricians and Gynecologists
- Hypertension Disorders in Pregnancy and the Effects on Offspring
- First-time pregnancy complications could mean high blood pressure later
- Follow AHA/ASA news on Twitter @HeartNews
About the American Heart Association
The American Heart Association is a relentless force for a world of longer, healthier lives. We are dedicated to ensuring equitable health in all communities. Through collaboration with numerous organizations, and powered by millions of volunteers, we fund innovative research, advocate for the public’s health and share lifesaving resources. The Dallas-based organization has been a leading source of health information for nearly a century. Connect with us on heart.org, Facebook, Twitter or by calling 1-800-AHA-USA1.
We are dedicated to ensuring equitable health in all communities. Through collaboration with numerous organizations, and powered by millions of volunteers, we fund innovative research, advocate for the public’s health and share lifesaving resources. The Dallas-based organization has been a leading source of health information for nearly a century. Connect with us on heart.org, Facebook, Twitter or by calling 1-800-AHA-USA1.
###
For Media Inquiries: 214-706-1173
Michelle Kirkwood: 703-457-7838; [email protected]
Maggie Francis: 214-706-1382; [email protected]
For Public Inquiries: 1-800-AHA-USA1 (242-8721)
heart.org and stroke.org
Blood pressure treatment changes for pregnant women
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
April 12, 2022
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
Traditionally, Ob/Gyns have prescribed blood pressure medications only to patients with very high blood pressure – 160/90 or higher – to reduce risks such as maternal stroke or preterm delivery. Older data suggested that antihypertensive drugs might reduce blood flow to the uterus, causing fetal growth restriction.
But new research has shown that treating non-severe hypertension is safe for pregnant patients and their babies.
Chronic Hypertension and Pregnancy (CHAP), a randomized clinical study, demonstrated a 20% overall reduction of a composite measure of severe preeclampsia and related risks in patients who were actively managed to control mild hypertension, compared with a control group.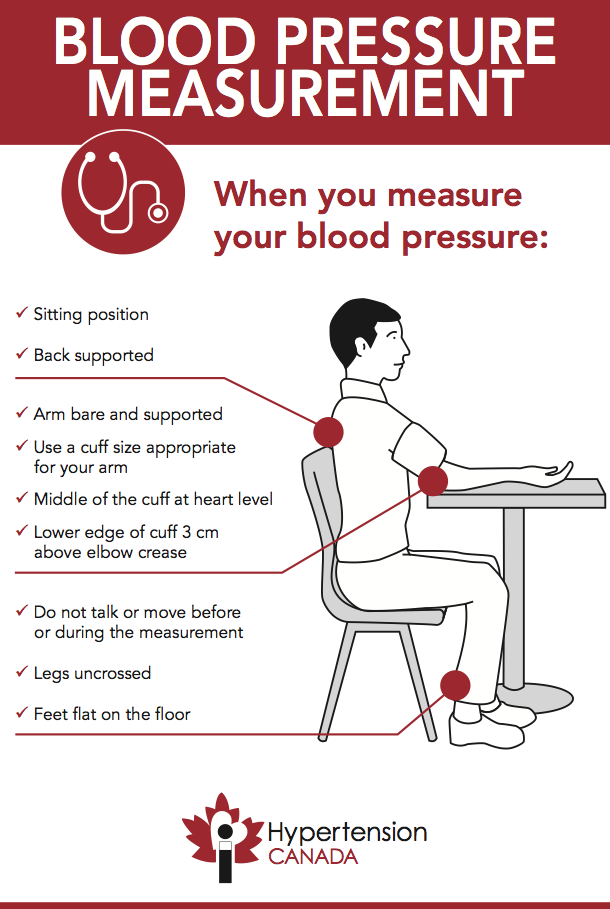
Importantly, adherence to the therapy was 86%. Women welcomed the opportunity to improve their health, and this gives me hope that more providers will be willing to prescribe antihypertensives during pregnancy.
Pregnancy itself taxes the cardiovascular system. Women who have been pregnant face a greater lifetime risk of heart problems than peers who haven’t. And patients with even mild hypertension in pregnancy are at increased risk of complications. Getting ahead of those risks could be key to better heart health later in life.
In April 2022, the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) announced their support of treating mild to moderate hypertension in pregnancy, with a starting point for treatment of 140/90 mm Hg.
CHAP showed immediate positive results – and time will tell whether treating mild to moderate hypertension can improve women’s lifelong cardiovascular health.
Related reading: When a new mom's blood pressure is too high
Inside the numbers: Data from the CHAP study
CHAP included 2,408 patients who enrolled in the trial before 23 weeks of pregnancy. Of these, 48% were non-Hispanic Black, 20% were Hispanic, and 28% were non-Hispanic white. All had elevated blood pressure readings between 140/90 and 160/105 (severe hypertension), and some had been previously diagnosed with high blood pressure.
Of these, 48% were non-Hispanic Black, 20% were Hispanic, and 28% were non-Hispanic white. All had elevated blood pressure readings between 140/90 and 160/105 (severe hypertension), and some had been previously diagnosed with high blood pressure.
During the trial, half the patients received standard prenatal hypertension care – monitoring for signs of preeclampsia (severe high blood pressure in pregnancy) such as persistent headache, shortness of breath, vision changes, or swelling in the hands and face. The other half received common blood pressure medication, such as labetalol or nifedipine.
Researchers compiled the data and found a composite risk reduction of 20% for:
- Fetal or newborn death
- Preterm delivery before 35 weeks of gestation
- Placental abruption – separation of the placenta from the uterine wall
There was no significant difference in fetal weight below the 10th percentile for gestational age: 11.2% in the control group and 10. 4% in the medication group. CHAP showed that treatment of mild to moderate hypertension was safe and beneficial for pregnancy outcomes.
4% in the medication group. CHAP showed that treatment of mild to moderate hypertension was safe and beneficial for pregnancy outcomes.
Related reading: Preeclampsia can strike suddenly during pregnancy
Optimizing blood pressure before or during pregnancy
For most women, blood pressure doesn't rise during pregnancy. In fact, it falls gradually until around 20 weeks, then rises closer to baseline toward the end of pregnancy. Most patients should fall below 120/80 on average and start thinking about treatment at 140/90 or higher, according to ACOG.
If you start pregnancy with elevated blood pressure (130/80 or higher) you may have chronic hypertension that has not yet been diagnosed. So, it makes sense to discuss treatment options with your provider, working together to manage blood pressure early and reduce the risk of maternal or fetal complications.
In general, blood pressure medications are inexpensive and accessible under most types of health insurance. However, it sometimes takes a bit of time for new data to trickle into the clinical setting – and replace outdated information online.
However, it sometimes takes a bit of time for new data to trickle into the clinical setting – and replace outdated information online.
If you know you have high blood pressure, talk with your doctor about whether taking antihypertensive medication is right for your pregnancy. If you are already on medications, plan to review those with your provider as there are some that are not appropriate to take during pregnancy. Don’t assume you should just stop taking the medication to avoid exposure to your unborn baby. It is your right to bring up any care you think could benefit your health.
The risk of pregnancy complications is never zero. But taking small steps to improve your health – such as managing your blood pressure – can make a big impact on your outcomes, potentially long after delivery.
To talk with a doctor about blood pressure management and pregnancy, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.
 D.
D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
Your Pregnancy Matters
- Emily Adhikari, M.D.
August 2, 2022
Your Pregnancy Matters
- Abey Eapen, M.
 D., Ph.D.
D., Ph.D.
July 26, 2022
More Articles
what means can be taken without harming the fetus?
Hypertension is a frequent companion of women during childbearing, when metabolic processes in the body increase and intra-abdominal pressure increases. High blood pressure in pregnant women threatens with the development of serious consequences, among which are premature births, miscarriages and even death. Therefore, it is important to have an idea about which antihypertensive drugs are most effective during pregnancy, whether concomitant treatment is necessary, and about many other features of hypertension in women during this remarkable and crucial period.
Physicians at the Yusupov Hospital will help you choose a drug for the treatment of hypertension that is both highly effective and has minimal side effects.
Causes of high blood pressure during pregnancy
Hypertension syndrome in women during pregnancy can be triggered by several factors. Blood pressure in pregnant women increases due to the following changes:
- the location of the heart changes;
- hormonal changes occur - blood levels of progesterone and estrogen increase;
- increases placental circulation;
- body weight increases;
- diaphragm movement is limited.
The development of all hemodynamic changes during pregnancy leads to a complex of problems that trigger arterial hypertension syndrome.
Treatment and hospitalization of pregnant women with hypertension
Pregnant women with hypertension syndrome must be hospitalized three times in order to confirm the diagnosis and find adequate treatment. Antihypertensive drugs during pregnancy are prescribed strictly by the attending physician, who takes into account the duration of pregnancy and possible complications of intrauterine development of the fetus.
- the first hospitalization is carried out in the early stages (up to 12 weeks) - in order to diagnose hypertension;
- a second hospitalization is planned between weeks 26 and 30 to change therapy;
- the third hospitalization is prescribed a couple of weeks before the birth - to prepare for them.
With the development of preeclampsia on the background of arterial hypertension, a woman needs immediate hospitalization, regardless of how pregnant she is at that moment.
Arterial hypertension in pregnant women requires constant medical support. Women are prescribed medications, and not only antihypertensives. In pregnancy complicated by high blood pressure, it is recommended to take sedatives, calcium antagonists, beta-blockers, alpha-blockers. In addition, symptomatic therapy is carried out.
In addition to drug therapy, a woman is advised to follow a special regimen and diet throughout the entire period of pregnancy.
There are a number of recommendations for pregnant women suffering from arterial hypertension:
- Observance of the correct sleep and rest regimen helps to normalize the emotional state - it is necessary to sleep at least 9 hours a day;
- any physical activity should be avoided;
- A pregnant woman with arterial hypertension syndrome needs to constantly measure her blood pressure.

Nutrition of a pregnant woman, even in spite of toxicosis, should be complete and high-calorie, with enough vitamins, microelements, proteins and antioxidants. It is recommended to include seafood and other foods containing polyunsaturated acids in the diet.
Antihypertensive drugs during pregnancy
Antihypertensive drugs during pregnancy must be used very carefully, strictly following the dosage and duration of the course prescribed by the attending physician, in order to avoid a negative effect on the fetus caused by insufficient blood flow to the placenta due to a decrease in blood pressure.
Alpha- and beta-blockers in pregnancy
Beta-blockers are prescribed to prevent premature termination of pregnancy.
There are good reasons to take these drugs:
- beta blockers lower blood pressure quickly and effectively;
- the risk of side effects when taking this group of drugs for pregnant women is minimal;
- the simultaneous use of alpha and beta blockers increases the effectiveness of therapy.

These drugs are not recommended if the blood pressure is unstable because they cause a sharp decrease in blood pressure.
Calcium antagonists in pregnancy
In the treatment of arterial hypertension syndrome, pregnant women are prescribed drugs - potassium antagonists, which improve microcirculation and permeability of the heart muscle. These drugs can be used no earlier than in the second trimester of pregnancy.
Calcium antagonists have a number of advantages: they minimize the likelihood of giving birth to children with insufficient body weight, are absolutely not toxic to the child, and also reduce the frequency of preeclampsia in early pregnancy.
However, this group of antihypertensive drugs also has a number of disadvantages: blood pressure decreases too quickly, which threatens to circulate in the placenta, edema of the extremities, allergic reactions and dyspeptic disorders.
Diuretics in pregnancy
Diuretics (diuretics) in the treatment of hypertension in pregnant women help reduce pressure and eliminate edema. However, like all drugs, diuretics also have side effects associated with a deterioration in blood flow to the placenta due to a decrease in fluid volume, additionally due to early and late preeclampsia. In addition, while taking diuretics, the electrolyte balance may be disturbed, the concentration of uric acid may increase, which has a negative effect on the state of the placenta during preeclampsia.
However, like all drugs, diuretics also have side effects associated with a deterioration in blood flow to the placenta due to a decrease in fluid volume, additionally due to early and late preeclampsia. In addition, while taking diuretics, the electrolyte balance may be disturbed, the concentration of uric acid may increase, which has a negative effect on the state of the placenta during preeclampsia.
Complications of arterial hypertension syndrome in pregnant women
The main danger of arterial hypertension syndrome during pregnancy is a hypertensive crisis. In addition, women are threatened by other conditions that are dangerous to their health:
- plaques form on the walls of blood vessels, which leads to a significant disruption of the already disturbed blood circulation and the supply of necessary substances to the placenta;
- high blood pressure can lead to myocardial infarction, resulting in death of the child. This is due to the narrowing of the coronary arteries and insufficient blood flow to the heart;
- arterial hypertension can cause pathological processes in the kidneys, there may be a development of renal failure resulting from impaired blood circulation in the kidneys;
- due to impaired blood circulation, pathologies of the central nervous system may occur: possible development of a stroke, chronic failure of brain circulation;
- In addition, pregnant women with arterial hypertension often develop endocrine diseases, visual impairment, metabolic syndrome, and many other serious complications.

When a hypertensive crisis occurs, a woman needs immediate treatment.
How to prevent a hypertensive crisis
The risk of developing this severe complication exists in any trimester of pregnancy. A hypertensive crisis, along with an increase in pressure, leads to damage to the renal system, the appearance of edema, obesity and numbness of the lower extremities.
For preventive purposes, a pregnant woman should strictly follow the recommendations of her doctor. In addition, she is prescribed additional drugs:
- diuretic: indapamide, triamterene;
- antispasmodics, stopping hypertensive crisis;
- calcium antagonists: norvasca, foridone.
Women with hypertension should not have a caesarean section during pregnancy because it is not safe in this situation. Painkillers, drugs that improve blood circulation and normalize the emotional state can be prescribed.
During labor, women with hypertension may develop severe bleeding, which should be considered in planned treatment throughout pregnancy.
In the therapy clinic of the Yusupov Hospital you will receive qualified assistance from the best physicians in Moscow, who have significant experience in treating hypertension in various categories of patients, including pregnant women. Our experts will tell you in detail which antihypertensive drugs can be taken by women during pregnancy, and which of them are strictly contraindicated.
You can make an appointment for a consultation by phone or on the website of the Yusupov Hospital by contacting the coordinating doctor.
Pregnancy and medicines / Obstetrics and gynecology, reprodoctology / Articles about health / Articles and encyclopedia / madez.ru
We have been actively planning for a baby for a long time, but we never think about the dangers of drugs during pregnancy!
Gynecologist, gynecologist endocrinologist Popova Natalya Vladimirovna will tell you which medicines can be taken during pregnancy, and which are categorically not recommended.
One of the most important periods in a woman's life is the period of bearing a child. And in these few months, the expectant mother must do everything in her power to give birth to a healthy baby. But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
If it is necessary to use any drug during pregnancy, the mother-to-be should remember:
- Any drug during pregnancy (at any stage) can be used only in accordance with the indications and only as prescribed by the attending physician;
- When choosing a medicinal product, preference should be given only to those medicinal products that have proven efficacy;
- Prefer monotherapy, i.e. treatment with only one drug if possible; combined treatment during this period is undesirable;
- Topical treatment is more desirable than systemic (oral, intravenous, intramuscular) administration of the drug.
- A pregnant woman should remember that completely safe and absolutely harmless drugs do not exist.
The most dangerous period for the use of any drugs, both of chemical and natural origin, is considered the first trimester of pregnancy (the first 12 gestational weeks), when all organs and systems are laid in the fetus, which will only develop and form the placenta in the future. It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
Pronounced mutagenic hazard:
1. in industry - asbestos, acetaldehyde, vinyl chloride, dimethyl sulfate; factors of metallurgical and rubber industries;
Metals: copper, nickel, lead, zinc, cadmium, mercury, chromium, arsenic, styrene, formaldehyde, chloroprene, epichlorohydrin, ethylene oxide.
2. agriculture - a mixture of defoliants, pesticides, insectiosides, repellents, fungicides, pesticides, methylpartion, phthalaphos, chlorophos, gardona, DDT, contan.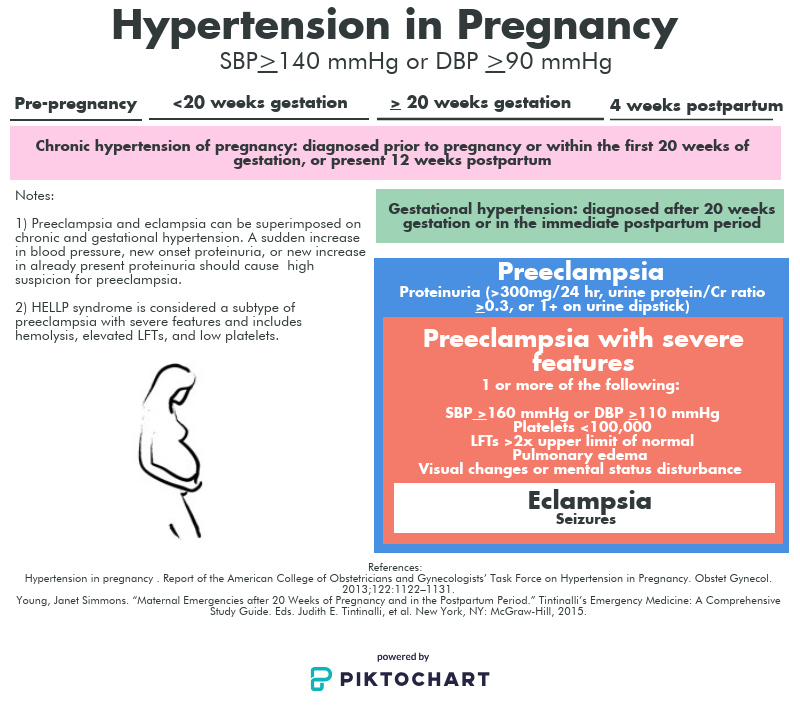
If you work in a hazardous industry and come into contact with these chemicals, from early pregnancy, switch to "light work".
Global trends in early pregnancy from the point of view of evidence-based medicine are unambiguous: the need for rational diet therapy , taking at least 400 mcg/day of folic acid and potassium iodide 200 mg/day has been recognized.After 12-14 weeks of pregnancy, with an inadequate diet, the use of vitamin preparations during pregnancy and lactation is recommended as a way to improve the health of the mother and fetus . Vitamin complexes intended for other groups of the population (including children) are contraindicated for pregnant women!
Medicines during pregnancy
In existing classifications, it is customary to subdivide drugs during pregnancy into groups - safe, relatively safe, relatively unsafe and dangerous. Moreover, the list of drugs is periodically updated.
Moreover, the list of drugs is periodically updated.
- Category A - safe drugs. Controlled trials have shown no risk to the fetus for the first 12 weeks of pregnancy. Regarding them, there is no evidence of a harmful effect on the fetus in late pregnancy. These are folic acid, levothyroxine sodium, paracetamol, magnesium sulfate.
- Category B - relatively safe drugs. Experimental studies have generally not shown their teratogenic effects in animals and children whose mothers took such drugs. These are amoxicillin, heparin, insulin, aspirin, metronidazole (except first trimester)
- Category C - relatively unsafe drugs. When testing these drugs on animals, their teratogenic or embryotoxic effects were revealed. Controlled trials have not been conducted or the effect of the drug has not been studied (isoniazid, fluoroquinolones, gentamicin, antidepressants, antiparkinsonian drugs).
 These drugs should only be used if the potential benefit outweighs the potential risk.
These drugs should only be used if the potential benefit outweighs the potential risk. - Caregory D - dangerous drugs. The use of drugs in this group is associated with a certain risk to the fetus, but despite this, it is possible to use the drug for health reasons (anticonvulsants, doxycycline, kanamycin, diclofenac).
- Category X - dangerous drugs that are contraindicated for use.
The teratogenic effect of drugs in this group has been proven, their use is contraindicated during pregnancy, as well as when planning a pregnancy.
Although almost 1000 chemicals are known to be teratogenic in animals, only a few chemicals have been proven to be permanently teratogenic in humans. These include a number of narcotic analgesics, chemotherapeutic drugs (antimetabolites, alkylating agents), anticonvulsants (trimethadione, valproic acid, fenithione, carbamazepine), androgens, warfarin, danazol, lithium, retinoids, thalidomide.
The safest drugs
(Larimore W.L., Petrie K.A., 2000)
| Drug groups | The safest drugs |
| Analgesics | Paracetamol, narcotic analgesics (short courses), NSAIDs (other than term) |
| Antibiotics | Aminopenicillins, macrolides (Vilprafen), azithromycin, cephalosporins, clindamycin, erythromycin, metronidazole (except 1st trimester), penicillins, trimethoprim (except 1st trimester) |
| Antidepressants | Venlafaxine, fluoxetine, trazodone |
| Antidiarrheals | Loperamide |
| Antiemetics | Andacids, doxylamine, prochlorperazine, promethazine, vitamin B |
| Antihypertensives | B-blockers, hydralazine, methyldopa, prazosin |
| Antiparasitics | Permethrin |
| Antituberculous drugs | Ethambutol, isoniazid |
| Antivirals | Amantadine, acyclovir |
| Antihistamines | Cetirizine, loratadine |
| Anti-asthma/anti-allergy means | Epinephrine, inhaled bronchodilators, theophylline |
| Cardiovascular medicines | B-blockers, calcium channel blockers, digoxin, nitroglycerin |
| Constipation products | Bisacodyl, methylcellulose |
| Antidiabetics | Insulin |
| Gastrointestinal drugs | Sucralfate, metoclopramide |
| Thyroid hormones | Levothyroxine, liothyronine |
Pins
It is very important that every pregnant woman remember that any drug during pregnancy can bring not only benefits, but also considerable harm, therefore, any self-administration during this period is not permissible, since their consequences are unpredictable and in many cases can cause irreparable harm to the developing fetus.