Birth with an epidural
Epidural | Pregnancy Birth and Baby
beginning of content3-minute read
Listen
An epidural is a type of pain relief for women in labour or who are having a caesarean section.
What is an epidural?
An epidural is a procedure that injects a local anaesthetic in to the space around the spinal nerves in your lower back.
This anaesthetic usually blocks the pain from labour contractions and during the birth very effectively. With an epidural you can usually move and can push your baby out when you need to.
An epidural is usually done by an anaesthetist.
The procedure
Before an epidural, you will usually have a drip for fluids put into your arm.
You can sit up and bend forward over a pillow, or lie on your side curled up into a ball. This makes it easier for the needle to be inserted into the right place. You will be asked to stay still.
Your lower back will be washed with cold antiseptic. A small amount of local anaesthetic will be injected into the skin of your lower back. A needle will be inserted between the bones of your spine into the space around your spinal nerves. Your anaesthetist will insert the epidural needle when your contraction stops, so it is important that you tell them when you have a contraction.
A small soft plastic tube will be inserted and the needle will be removed. That tube delivers the anaesthetic that will numb your pain.
It usually takes between 5 and 30 minutes for your pain to be relieved by the epidural.
You usually only have an epidural during the first stage of labour — but it can be given at any stage of labour.
Advantages and disadvantages of an epidural
Epidurals are available at most hospitals but not in birth centres or for home births.
The advantages of an epidural are:
- it is usually very effective
- it is generally very safe
- you can often still move around in bed and push when you need to
- if you have a long labour, it allows you to sleep and recover your strength
- if you're having a caesarean, you can stay awake and your partner can be there
The disadvantages of an epidural are:
- for medical reasons, not everyone can have an epidural
- you might need to have fluids given to you through a tube in your arm, and will need to have your blood pressure monitored
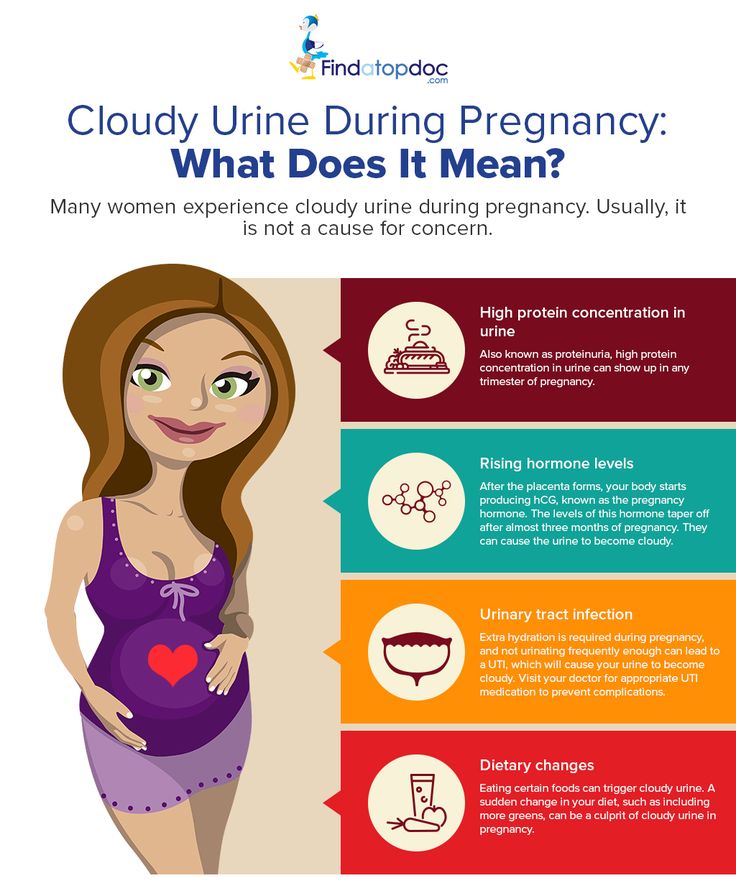
- you might lose feeling in your bladder and need a catheter (tube) in your bladder to help you pass urine
- you might lose feeling in your legs for a few hours
- it might slow down the second stage of labour
- you might not be able to push and need help to give birth
- your baby will need to be closely monitored during your labour
Whether you have an epidural or not makes no difference to the chance of you having a caesarean section.
Risks and side effects
An epidural is effective and fairly safe. But there are some risks.
- Some women feel cold or itchy.
- A small number of women get little or no pain relief.
- Some women get weakness in the legs; it wears off after a few hours.
- There is an increased risk of needing forceps or a vacuum to help with the birth.
- Some women develop a bad headache 24 to 48 hours after an epidural.
- There is a small chance of developing a skin infection.
- Very rarely a few women get permanent nerve damage.
What to discuss with your doctor or midwife
You can check:
- if you can have an epidural at your chosen hospital or birth centre
- what their epidural procedures are
- the type of pain relief that might suit you best
Sources:
Australia and New Zealand College of Anaesthetists (Epidurals and childbirth), Government of Western Australia Department of Health (Epidurals for childbirth), Mater Mothers' Hospital (Epidural), They Royal Women's Hospital (Epidural information), Royal Australian College of Obstetricians and Gynaecologists (Pain relief in labour and childbirth), Queensland Health (Epidural analgesia in labour - clinical guidelines)Learn more here about the development and quality assurance of healthdirect content.:strip_icc():format(jpeg)/kly-media-production/medias/3299137/original/005536400_1605658939-pexels-jonathan-borba-3259628.jpg)
Last reviewed: January 2020
Back To Top
Related pages
- TENS (Transcutaneous electrical nerve stimulation)
- Gas (Entonox)
- Non-medical pain relief during labour
- Pain relief during labour
- Making a birth plan
- Giving birth - stages of labour
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Natural Birth vs. Epidural: What to Expect
Giving birth can and should be a beautiful experience. But the prospect of delivery may give some women anxiety because of the anticipated pain and discomfort.
But the prospect of delivery may give some women anxiety because of the anticipated pain and discomfort.
While many women opt to receive epidurals (medication for pain relief) to have a more comfortable labor, many more are choosing “natural” or unmedicated births. There is growing fear about the side effects of medicated births and epidurals.
Discuss the options with your doctor or midwife to determine which method is best for you and your child. In the meantime, here are some of the most important points to consider.
An epidural decreases pain in a specific area — in this case, the lower part of the body. Women often choose to have one. It’s also sometimes a medical necessity if there are complications, such as those resulting in a cesarean delivery (C-section).
An epidural takes about 10 minutes to place and an additional 10 to 15 minutes to work. It’s delivered through a tube via the spine.
Benefits
The greatest benefit of an epidural is the potential for a painless delivery. While you may still feel contractions, the pain is decreased significantly. During a vaginal delivery, you’re still aware of the birth and can move around.
While you may still feel contractions, the pain is decreased significantly. During a vaginal delivery, you’re still aware of the birth and can move around.
An epidural is also required in a cesarean delivery to ease pain from surgically removing a baby from the womb. General anesthesia is used in some cases as well, where the mother isn’t awake during the procedure.
The National Institutes of Health (NIH) report a 72 percent increase in the number of cesarean deliveries from 1997 through 2008, which might also explain the enduring popularity of epidurals.
While some cesarean deliveries are elective, most are required if vaginal delivery can’t be accomplished. Vaginal birth after cesarean section is possible, but not for all women.
Risks
Some risk factors of an epidural include:
- back pain and soreness
- headaches
- persistent bleeding (from puncture site)
- fever
- breathing difficulties
- drop in blood pressure, which can slow down the baby’s heart rate
It’s important to note that, while such risks exist, they’re considered rare.
The fact that mothers can’t feel all of the elements of delivery with an epidural can also lead to a host of other problems, such as increased risk of tearing during vaginal delivery.
Risks with cesarean deliveries aren’t necessarily related to the epidural. Unlike vaginal births, these are surgeries, so recovery times are longer and there’s a risk of infection.
Cesarean deliveries have also been linked to greater risk of childhood chronic diseases (including type 1 diabetes, asthma, and obesity). More research is needed.
The term “natural birth” is usually used to describe a vaginal delivery performed without medication. It’s also sometimes used to distinguish between a vaginal delivery and a cesarean delivery.
Benefits
Unmedicated births have increased in popularity due to concerns that epidurals can interfere with natural body responses to labor and delivery. Ashley Shea, a birth doula, yoga teacher, student midwife, and founder of Organic Birth, has also witnessed this trend.
“Women want to be able to move around untethered to machines, they want to stay home as long as possible before heading to the hospital, they don’t want to be disturbed or excessively monitored, or have too many cervical checks (if at all), and they want to have immediate and uninterrupted skin-to-skin contact with their newborn and wait until the cord stops pulsating to clamp and cut the cord,” said Shea.
As she pointed out, “If you found out you could have a baby in a warm, deep pool of water compared to flat on your back with people yelling at you to push, what would you choose?”
And in case you didn’t already know, mothers do have the right to elect unmedicated births at hospitals.
Risks
There are a few serious risks associated with unmedicated births. Risks often arise if there is a medical problem with the mother or if an issue prevents the baby from naturally moving through the birth canal.
Other concerns surrounding a vaginal birth include:
- tears in the perineum (area behind the vaginal wall)
- increased pain
- hemorrhoids
- bowel issues
- urinary incontinence
- psychological trauma
Preparation
Preparing for the risks of an unmedicated birth is important. Mothers might consider having a midwife come to their home or perhaps complete the delivery process at the hospital.
Mothers might consider having a midwife come to their home or perhaps complete the delivery process at the hospital.
Childbirth education classes help prepare you for what to expect. This provides a safety net should any complications arise.
Nonmedication methods used to ease labor and delivery can include:
- massages
- acupressure
- taking a warm bath or using a hot pack
- breathing techniques
- frequent changes in position to compensate for changes in the pelvis
Due to the complexity of labor, there is no one-size-fits-all method when it comes to birthing. According to the Office on Women’s Health, these are just some of the factors doctors and midwives consider when making a recommendation:
- overall health and emotional well-being of the mother
- the size of the mother’s pelvis
- the mother’s pain tolerance level
- the intensity level of contractions
- size or position of the baby
It’s best to understand all of your options and to know when you might need medication to make sure your baby can enter the world without complications.
Position of women in the second stage of labor with epidural anesthesia
What is the problem?
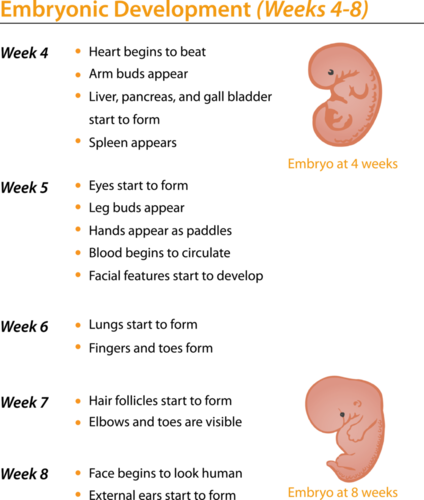
The second stage of labor consists of a latent or passive phase, when the cervix is fully dilated and the baby's head descends without mother's effort, and an active phase, when the mother tries to push the baby out and he is born.
We wanted to find out whether different positions (vertical or horizontal) in the second stage of labor can change the outcomes of labor in women who received epidural anesthesia and their children. Outcomes included caesarean section, instrumental delivery, major bleeding, or suturing following vaginal lacerations during labor. As for children, we looked at whether they tolerated childbirth well and whether they needed hospitalization for special care. We also wanted to determine women's views on the experience of childbirth and their satisfaction with childbirth. This is an update of a review first published in 2013.
Why is this important?
Epidural anesthesia is the most effective method of pain relief during childbirth. It is common, although it can increase the duration of labor and the need for forceps and a vacuum extractor. Instrumental labor can lead to prolapse, urinary incontinence, or painful intercourse. In recent years, the introduction of low doses of anesthetics, known as "mobile" epidural anesthesia, has become popular. Low doses allow women to be more mobile during childbirth and make it easier to get upright. It has been suggested that the upright position may make childbirth easier.
What evidence did we find?
We looked for evidence in randomized controlled trials in June 2018. This updated review now includes 8 studies involving 4,464 women and their children. One of the new studies was very well done; three-quarters of all women in the survey participated in it. 5 trials were conducted in the UK, 1 in France, and 2 in Spain.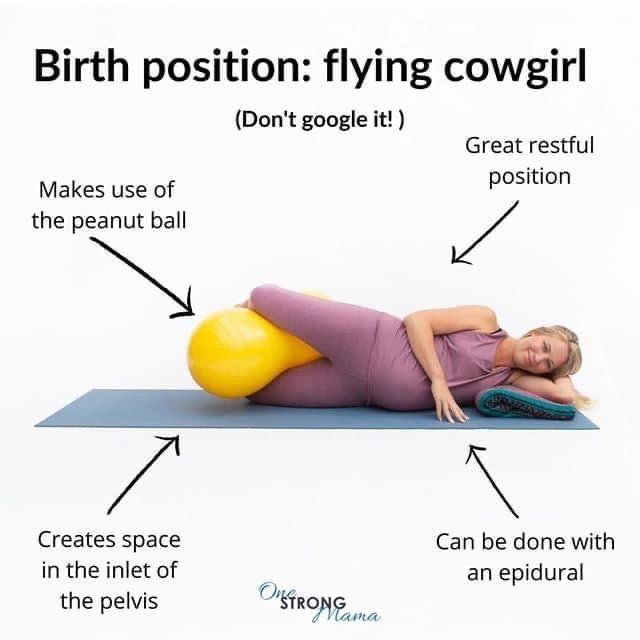 They compared different versions of the vertical and horizontal (lying) positions.
They compared different versions of the vertical and horizontal (lying) positions.
Overall, there was little or no difference between upright and horizontal positions for caesarean section or instrumental vaginal (surgical) delivery (8 trials, 4316 women; low-quality evidence). The results of the studies differed significantly. However, when we looked only at high-quality studies, we found clear harm from standing upright (3 trials, 3,609 women). There is evidence of an increased risk of operative delivery (both instrumental and caesarean sections) and an increase in the number of caesarean sections.
There was no difference in the number of women with tears requiring sutures (3 trials, 3266 women; low-quality evidence) or major bleeding (1 trial; 3093 women; moderate-quality evidence). It is unclear whether standing has any effect on instrumental vaginal delivery or duration of the second stage of labor, as the quality of the evidence for these outcomes was very low.
Mothers reported slightly greater satisfaction with horizontal positions (1 trial, 2,373 women). Despite the fact that after birth in the supine position, a higher number of children had high cord blood acidity (2 trials, 3159children; moderate-quality evidence), there was no other evidence of harm to children. Comfortable were horizontal positions on the left or right side, but not on the back and not with legs raised in the stands.
Despite the fact that after birth in the supine position, a higher number of children had high cord blood acidity (2 trials, 3159children; moderate-quality evidence), there was no other evidence of harm to children. Comfortable were horizontal positions on the left or right side, but not on the back and not with legs raised in the stands.
What does this mean?
Overall, the evidence did not show a clear difference in operative delivery in women who received epidural anesthesia in the second stage of labor. This may be due to differences in the design and conduct of studies and the different positions studied. However, high-quality evidence showed better outcomes for women who shifted between side lying positions and avoided lying on their back. These positions result in a more normal birth, are better tolerated, and do not cause harm to the mother or baby compared to the upright position.
Translation notes:
Translation: Tashtanbekova Cholpon Bolotbekovna. Editing: Kukushkin Mikhail Evgenievich. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
Editing: Kukushkin Mikhail Evgenievich. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
Not Found (#404)
Paracelsus Medical Center
Page not found.
The above error occurred while the Web server was processing your request.
Please contact us if you think this is a server error. thank you.
Please wait, download may take time
Loading...
You know which doctor you want to book
You know the service you want to book
Service selection
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
The choice of a specialist
Service selected:
Choosing a specialist service
A second consultation is considered to be a consultation of one specialist within 30 days from the date of the previous appointment. On the 31st day from the previous visit to a specialist of this profile, the consultation will be primary.
Address selection:
st. Vikulova, 33, building 2 st. Bolshakova, d. 68
Vikulova, 33, building 2 st. Bolshakova, d. 68
Date selection:
Time of receipt:
Password
Password
Register Can't login? account activation
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for password recovery
To gain access to your personal account, enter the e-mail that was specified during registration, we will send instructions for reactivating your account
Your application has been accepted, our specialists will answer your question as soon as possible!
Telephone
Comment
Dear patients!
Multidisciplinary Clinic and Maternity Hospital "Paracelsus" informs you, according to the Letter of the Ministry of Finance of the Russian Federation to the Federal Tax Service dated March 25, 2022. N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
N BS-4-11 / 3605, that subparagraph 3 of paragraph 1 of Article 219The Tax Code of the Russian Federation provides for the right of a taxpayer to receive a social tax deduction in the amount paid by him in the tax period for medical services provided by medical organizations engaged in medical activities to him, his spouse, parents, children (including adopted children) in under the age of 18, wards under the age of 18 (in accordance with the list of medical services approved by the Government of the Russian Federation).
Joint order of the Ministry of Taxation of Russia and the Ministry of Health of Russia dated July 25, 2001 N 289 / BG-3-04 / 256 (hereinafter - the order of July 25, 2001) approved the form of the Certificate of payment for medical services for submission to the tax authorities of the Russian Federation (hereinafter - the Certificate payment for medical services).
This certificate certifies the fact of receiving a medical service and its payment through the cash desk of a healthcare institution at the expense of the taxpayer.