Baby with watery eye and discharge
Is it normal and how to treat it?
Eye discharge is common in newborns and typically occurs due to a blocked tear duct. However, parents and caregivers can often treat this at home.
Eye discharge is typically harmless and self-resolving. However, discharge that occurs alongside other symptoms in the eye area, such as swelling or tenderness, could indicate an infection or another eye problem. A parent or caregiver of a newborn with these symptoms will need to consult a doctor.
This article discusses how common eye discharge is and explains how to treat it at home. We also cover medical treatment, other causes, complications, and when to contact a doctor.
Eye discharge in newborns is common and rarely a cause for concern. A common cause of eye discharge is a blocked tear duct.
According to the American Academy of Ophthalmology, almost 20% of newborns have a blocked tear duct. This condition can occur because the end of the tear duct does not open properly when the baby is born.
Tears form in the lacrimal gland, which sits just above the eye. Tear fluid helps clean and lubricate the surface of the eye. When a person blinks, the eyelids sweep the tear fluid into these ducts, which drain it into the nose.
If something blocks a tear duct, fluid may no longer be able to drain away from the eye’s surface. Blockages can cause very watery eyes, and sticky discharge may form in the corners.
Learn more about blocked tear ducts.
Blocked tear ducts are a common cause of eye discharge in infants. However, other conditions and factors can also cause discharge.
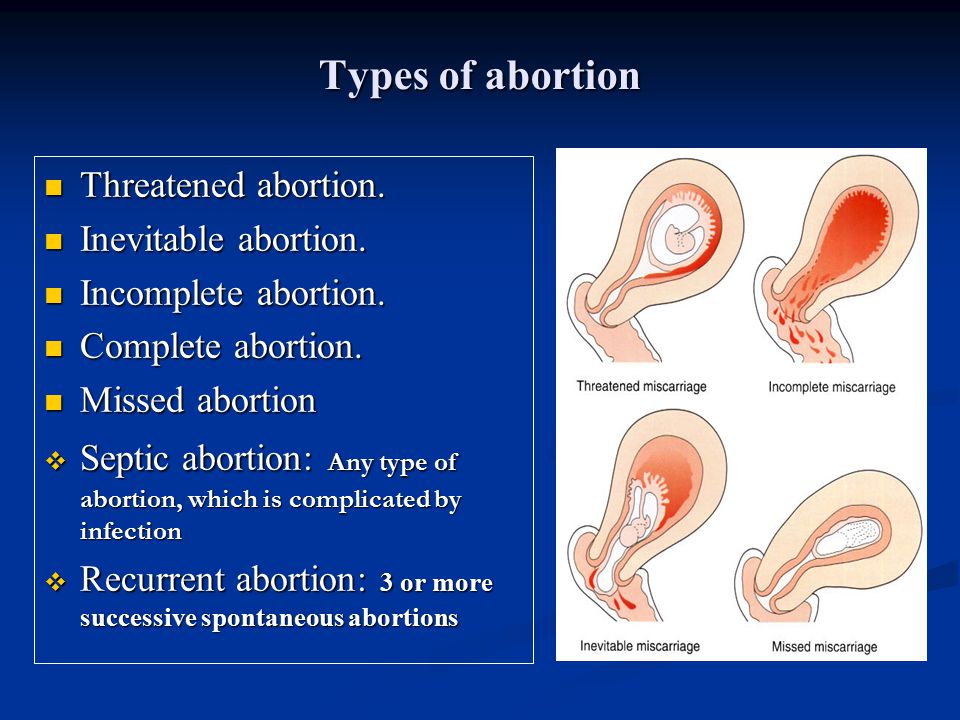
Conjunctivitis
Eye discharge in newborns can also be a sign of conjunctivitis or pinkeye. Conjunctivitis is an inflammation of the conjunctiva, a thin membrane that protects the front of the eye. Unlike a blocked tear duct, conjunctivitis often causes the white part of the eye to appear red.
Symptoms of conjunctivitis in newborns can include:
- drainage or discharge that develops between 5 and 12 days after birth
- puffy or tender eyelids, often with skin discoloration
- red, irritated eyes
Conjunctivitis in newborns can sometimes occur alongside a blocked tear duct. However, a pregnant person can also pass on a bacterial or viral infection to their baby when giving birth, leading to conjunctivitis.
However, a pregnant person can also pass on a bacterial or viral infection to their baby when giving birth, leading to conjunctivitis.
Learn more about the symptoms of eye infections.
Chemical irritation
Chemical irritation can also cause conjunctivitis in newborns. Healthcare professionals often give antibacterial eye drops to newborns to prevent infections. These eye drops can sometimes cause irritation that can result in conjunctivitis symptoms.
Learn more about eye irritation.
If the eye discharge is due to a blocked tear duct, it will usually resolve without treatment within 4–6 months.
However, wind, cold weather, and strong sunlight can also worsen symptoms, so a parent or caregiver should aim to protect a newborn’s eyes from these elements.
Clearing discharge
A parent or caregiver can often treat a newborn with a blocked tear duct at home. Before touching the area close to the child’s eyes, it is essential to wash the hands with soap and warm water to prevent infections. A person should also take care to rinse the hands thoroughly after cleaning them to avoid getting soap in the baby’s eye.
A person should also take care to rinse the hands thoroughly after cleaning them to avoid getting soap in the baby’s eye.
To clear away discharge, dip a clean piece of gauze or soft cloth in some lukewarm water, then gently wipe the corner of the eye. If a blocked tear duct affects both eyes, always use a new area of the cloth or gauze to clean the other eye.
Tearduct massage
A doctor may also recommend gently massaging the blocked tear duct to help it open, and they will demonstrate how to do this safely.
To massage the tear duct:
- Lightly press the tip of the index finger against the inside bridge of the newborn’s nose, on the side of the blocked tear duct.
- Make 2 or 3 short downward strokes with the finger along the side of the nose. These should be gentle but firm.
- Perform the massage twice a day — once in the morning and once in the evening.
If the side of the newborn’s nose becomes red or swollen, stop the massage immediately and contact a doctor.
In newborns, blocked tear ducts tend to open up within several months of birth. However, medical intervention may be necessary in some cases.
Surgery
If the blockage has not gone away by the baby is 1 year of age, a doctor may recommend a medical treatment called a nasolacrimal duct probing.
This procedure involves inserting a small probe into the infant’s tear duct. By using probes that gradually increase in size, a doctor will be able to open up the tear duct. They will then use a saline solution to flush out any remaining debris.
Sometimes, the doctor may also insert a small tube, or stent, into the duct to keep it open.
Probing is usually successful in opening the tear duct. For children with a severe blockage, a doctor may recommend a more complicated surgical procedure called a dacryocystorhinostomy to clear out and open the tear duct.
Antibiotics
If an infection is causing eye discharge, the newborn will need prompt medical attention. To treat cases of infectious discharge, a doctor may prescribe topical, oral, or intravenous antibiotics.
To treat cases of infectious discharge, a doctor may prescribe topical, oral, or intravenous antibiotics.
Blocked tear ducts can sometimes lead to an infection called dacryocystitis. Symptoms of this condition may include:
- excessive thick discharge from the eye
- redness in the corner of the eye
- a tender bump or swelling at the side of the nose
- fever
If a newborn has any of these symptoms, a parent or caregiver should consult a doctor.
Newborns with eye discharge or very watery eyes should speak with a pediatrician or an eye doctor specializing in children, called a pediatric ophthalmologist. These healthcare professionals can diagnose the cause of the discharge and check for signs of infection.
Parents or caregivers should seek medical attention if an infant’s eye discharge persists for more than 6 months.
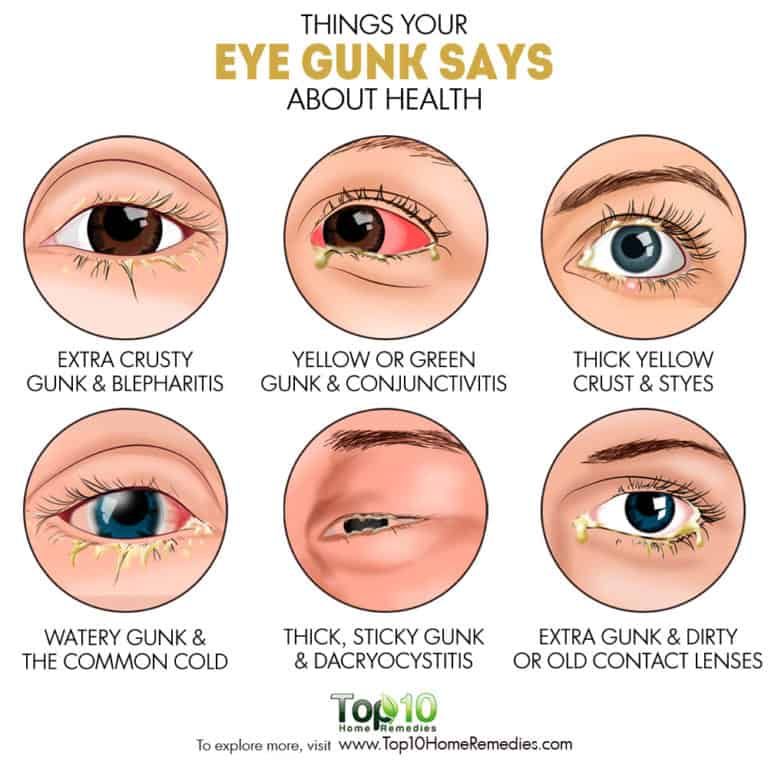
Newborns with signs of an eye infection require immediate medical attention. Signs of an eye infection can include:
- sore or puffy eyes
- swollen eyelids
- yellow or green pus or discharge
- a bump or swelling on the inside corner of the eye
If a parent or caregiver notices any of these symptoms, they should contact a doctor immediately.
Eye discharge in newborns is common and often results from a blocked tear duct. The blockage will usually clear up by itself within 4 to 6 months.
However, newborns with eye redness, eye discharge, or excessive watering of the eyes should speak with a doctor to diagnose the cause and rule out an eye infection.
Parents and caregivers can treat a baby with a blocked tear duct at home by wiping away any discharge and gently massaging the area twice a day. A doctor can demonstrate how to do this.
Discoloration, swelling, or soreness in the eye can indicate an eye infection. Speak with a doctor immediately if an infant has these signs.
Eye - Pus or Discharge
Is this your child's symptom?
- Yellow or green discharge (pus) in the eye
- The eyelids are stuck (matted) together with pus after sleep
- After being wiped away, the pus comes back during the day
- Often caused by a bacterial eye infection
Causes of Eye with Pus
- Bacterial Conjunctivitis.
 This is a bacterial infection of the eye. The main symptom is eyelids stuck together with pus after sleep. Can be present in 1 or both eyes. A few viruses can cause pus in the eyes, but most don't.
This is a bacterial infection of the eye. The main symptom is eyelids stuck together with pus after sleep. Can be present in 1 or both eyes. A few viruses can cause pus in the eyes, but most don't. - Viral Conjunctivitis. This is a viral infection of the eyes. Main symptom is pinkness of the white parts of the eyes. The eyes are also watery. Most often, there is no pus. Usually on both sides.
- Normal Discharge. A small amount of dried mucus only in the corner of the eye. It may not even be pus. A collection of mucus can be cream colored. Often due to an irritant that got in the eye from dirty hands. Needs no treatment except wiping it away with warm water.
- Blocked Tear Duct. Present in 10% of newborns. Main symptom is a constant watery eye. Tears fill the eye and run down the face. This happens even when not crying. The eye is not red and the eyelid is not swollen. The wet eye may get secondary infections.
 This will cause the eyelids to become matted with pus.
This will cause the eyelids to become matted with pus. - Foreign Object in Eye (Serious). Small particles such as sand, dirt or sawdust can be blown into the eyes. The grit often gets stuck under the upper eyelid. If not removed, the eye reacts by producing pus. The main clue is an eye infection that does not respond to antibiotic eyedrops. Older children complain of feeling something in the eye.
- Eyelid Cellulitis (Serious). This is a deep infection of the eyelid and tissues around it. The main symptom is a red, swollen, very tender eyelid. The eye can be swollen shut. Usually only on one side. This can be a problem caused by bacterial conjunctivitis. The eye infection spreads inward. More commonly this is caused by an ethmoid sinus infection. That type occurs without any pus in the eye.
Symptoms of Bacterial Eye Infection
- Yellow or green discharge or pus in the eye
- Dried pus on the eyelids and eyelashes
- The eyelashes are more likely to be stuck together after sleep
- The whites of the eye may or may not be red or pink
- The eyelids are often puffy
When to Call for Eye - Pus or Discharge
Call Doctor or Seek Care Now
- Eyelid is very red or very swollen
- Vision is blurred
- Eye pain or discomfort is more than mild
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old.
 Caution: do NOT give your baby any fever medicine before being seen.
Caution: do NOT give your baby any fever medicine before being seen. - Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Pus in the eye, but none of the symptoms above. Reason: you may need antibiotic eyedrops to treat it.
- Using antibiotic eye drops more than 3 days and pus is still there
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Pus In the Eye
- What You Should Know About Bacterial Eye Infections:
- Bacterial eye infections are common with colds.
- They respond to home treatment with antibiotic eye drops which need a prescription.
- They are not harmful to vision.
- Until you get some antibiotic eye drops, here is some advice that should help.
- Bacterial eye infections are common with colds.
- Remove Pus:
- Remove all the dried and liquid pus from the eyelids. Use warm water and wet cotton balls to do this.
- Do this whenever pus is seen on the eyelids.
- Also, remove the pus before the antibiotic eye drops are put in. Reason: they will not work if you don't.
- The pus can spread infection to others. So, dispose of it carefully.
- Wash your hands well after any contact with the pus.
- Antibiotic Eye Drops: How to Use
- For a cooperative child, gently pull down on the lower lid. Put 1 drop inside the lower lid. Then ask your child to close the eye for 2 minutes. Reason: so the medicine will get into the tissues.
- For a child who won't open his eye, have him lie down.
 Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
- Contact Lenses:
- Children who wear contact lenses need to switch to glasses until the infection is gone.
- Reason: to prevent damage to the cornea.
- Disinfect the contacts before wearing them again.
- Discard them if they are disposable.
- Return to School:
- Your child can return to school when the pus is a small amount.
- Antibiotic eye drops should be used for 24 hours before going back.
- What to Expect:
- With treatment, the pus discharge should clear up in 3 days.
- The red eyes may last up to a week.
- Call Your Doctor If:
- Eyelid gets red or swollen
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/23/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Festering eyes in a child, causes, treatment, prevention.
Suppurating eyes in a child
Suppurating eyes in children means the presence of mucous discharge from the eyes of yellow or yellow-green color.
Symptoms of conjunctivitis in a child
In addition to discharge from the eyes, other symptoms appear, which include:0012
Causes of purulent discharge from the eyes in children
Eye diseases that can cause purulent discharge from the eyes in newborns and infants:
Neonatal dacryocystitis
Many children are born with poorly developed tear ducts. This means that the tear cannot flow properly into the nasal cavity. Because of this, a secret from the eyes accumulates in the lacrimal sac and inflammation begins. At the same time, the baby has watery and festering, as a rule, only one eye.
Treatment in the first 3 months of the child is carried out with medication. Anti-inflammatory drops are instilled and lacrimal sac massage is applied. In most cases, dacryocystitis resolves. Sometimes probing of the lacrimal ducts is necessary.
Neonatal conjunctivitis
Inflammation of the mucous membrane of the eye within 28 days after birth is called neonatal conjunctivitis.
Bacteria that cause inflammation: Staphylococcus aureus, chlamydia, streptococcus, etc.
Gonococcal infection of newborns
With gonococcal infection in newborns, very abundant purulent discharge, with severe swelling of the eyelids. Possible damage to the cornea and the development of corneal ulcers.
Eye trauma during childbirth
In case of pathological childbirth, damage to the eyes and infection of the eye is possible.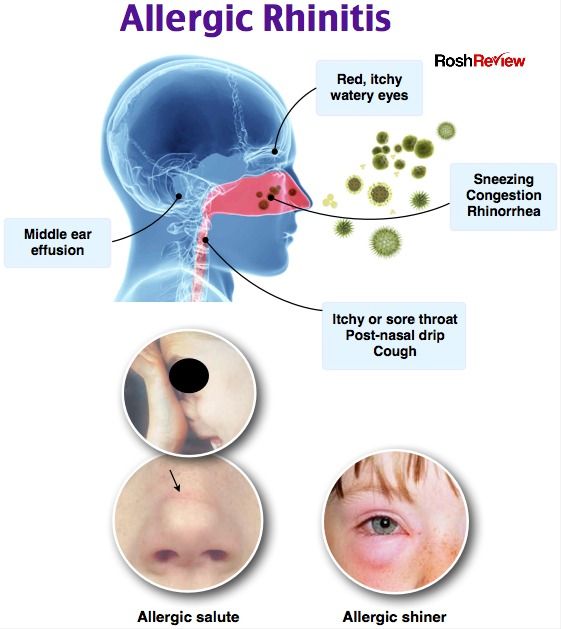
Inadequate eye prophylaxis immediately after birth
Newborns are given special antiseptic drops for prophylaxis immediately after birth. In the case when drops are not used, the risk of developing neonatal conjunctivitis is increased.
Inflammation of the maternal genital tract
Inflammation of the maternal genital tract leads to infection of the child and signs of inflammation of the eyes.
Causes of purulent discharge from the eyes in pregnant women and children older than one year
SARS and influenza
The pus that may be present in your child's eyes may be due to a viral infection. Knowing the causative factors, as well as how to deal with them, can prevent the development of purulent discharge from the eyes in an infant.
Sinusitis
If your baby has a cold, they may develop sinusitis (inflammation of the sinuses). Important symptoms: fever, pain in the forehead and eyes, lacrimation and suppuration of the eyes.
Allergies
If your baby has a runny nose and you notice redness and small mucous yellow discharge, it may be an allergy.
Conjunctivitis
The eyes of a child and pregnant women often fester due to infectious inflammation. Inflammation can be caused by both bacteria and viruses. The symptoms of conjunctivitis begin in one eye and then spread to the other eye.
Festering eyes during pregnancy
In a pregnant woman, due to hormonal changes, the conjunctiva becomes loose and there is more mucous discharge from the eyes. This can cause some discomfort when wearing contact lenses.
If you are pregnant and wear contact lenses, look out for discharge from the eyes. If a yellow discharge occurs, remove the lenses and consult a doctor.
Festering eye in a child treatment
Situations that require immediate attention and medical attention include the following symptoms:
- severe swelling of the eyelids and very profuse purulent discharge
- fever
- the child complains of decreased vision and pain in the eyes
- the child rubs the eye
- redness eyes and lacrimation
It is important to know that the spread of infection in children is very fast and rapid. Therefore, it is necessary to seek medical help in a timely manner.
Therefore, it is necessary to seek medical help in a timely manner.
During treatment, when using eye ointments and drops, it is necessary to first remove pus from the eye. Any types of medicines (drops and ointments) are effective only after washing the eye.
Lachrymation in children: causes, diagnosis, treatment
Children's clinic JSC "Medicina"
(clinic of Academician Roitberg)
Sign up for doctor
What should I do if my child's eyes start to water heavily? How dangerous can it be? Should I pay attention to this or is it a temporary phenomenon that will pass by itself? The answer is unequivocal: parents need to pay attention to this and find out the cause of lacrimation. Often, tearing from one eye in a child is a sign of the development of an infectious disease, a cold, or a manifestation of an allergic reaction.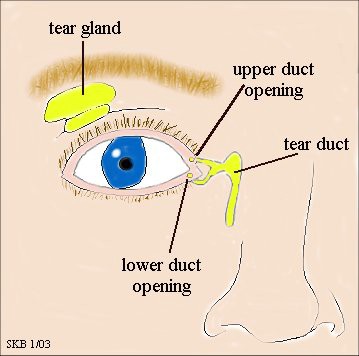 Moreover, such a manifestation may be the result of an injury, and it is important to prevent deterioration of vision. But in order to take effective measures to eliminate the problem, you must absolutely know the cause. Therefore, in most cases, an appeal to a specialist is required, and sometimes not to one.
Moreover, such a manifestation may be the result of an injury, and it is important to prevent deterioration of vision. But in order to take effective measures to eliminate the problem, you must absolutely know the cause. Therefore, in most cases, an appeal to a specialist is required, and sometimes not to one.
Causes of lacrimation in children
Experts identify several main causes of lacrimation from the eyes of a child. At the same time, the symptoms and the nature of the course in them differ significantly. Therefore, we propose to consider each group of reasons in detail.
Conjunctivitis is a fairly common infectious disease that often occurs in children. Inflammation develops as a result of infection in the body. And she can get there in various ways, even with a speck of dust in her eye. The inflammatory process is accompanied by profuse lacrimation and redness of the white of the eye. Also, concomitant symptoms with various types of conjunctivitis can be swelling and swelling of the eyelids, unpleasant painful sensations. As with any other problem, it is best to start treatment as soon as possible, then it will be most effective and least long-lasting.
As with any other problem, it is best to start treatment as soon as possible, then it will be most effective and least long-lasting.
The main types of conjunctivitis:
- adenovirus - accompanies various viral diseases (for example, SARS, influenza, etc.). As a result, the child has a strong irritation of the cornea of the eye, lacrimation and redness of the proteins;
- bacterial - caused by the penetration of bacteria into the eye. The risk of infection is present when debris accidentally enters the eye or rubbing the eyes with contaminated hands. As a result of the introduction of pathogens, an inflammatory process begins, which is accompanied by profuse lacrimation and painful sensations, with an advanced degree, copious discharge of pus is possible;
- allergic - caused by contact with the corresponding allergen irritant. Symptoms appear immediately after contact and, as a rule, are pronounced.
Barley. It looks like a seal with localization on the eyelid. Seal tends to rapidly increase in size. At the same time, an inflammatory process occurs inside the seal and a barley sac is formed, in which pus accumulates. As the stye sac grows, so does the discomfort it creates for the eye. Irritation is accompanied by a strong release of lacrimal fluid. The cause of barley may be the hypothermia of the child or the ingress of debris and dust into the eye.
Seal tends to rapidly increase in size. At the same time, an inflammatory process occurs inside the seal and a barley sac is formed, in which pus accumulates. As the stye sac grows, so does the discomfort it creates for the eye. Irritation is accompanied by a strong release of lacrimal fluid. The cause of barley may be the hypothermia of the child or the ingress of debris and dust into the eye.
Dacryocystitis of the newborn. Can be diagnosed in infants in the first weeks of life. The fact is that immediately after birth, the nasolacrimal canal, through which, in fact, the lacrimal fluid passes, may not yet be open, that is, there is a congenital obstruction. As a result, the baby's tear fluid is removed from the eyes, and it looks like profuse lacrimation. The channel will gradually open, and with its opening, the tearing from the eyes of the child will also stop.
Foreign body entry. It is no secret that the eye is a very vulnerable organ. The ingress of foreign objects into it is of a percussive nature and can injure the protein. Even if the blow was not strong, it causes a defensive reaction - an abundant release of lacrimal fluid. It actively wets the injured area and thus helps to remove the foreign body from the eye.
Even if the blow was not strong, it causes a defensive reaction - an abundant release of lacrimal fluid. It actively wets the injured area and thus helps to remove the foreign body from the eye.
Exposure to a computer or other modern gadgets. Prolonged use of computers and smartphones without rest for the eyes leads to drying out of the cornea, as the number of blinks decreases. Due to drying, the cornea is irritated, which causes active lacrimation in children. And this once again demonstrates that the use of computer technology by a child and adults should be correct.
Diagnosis of lacrimation in children
Since the causes of lacrimation in children differ significantly, it is very important to accurately diagnose them. It is necessary for choosing a method of treatment.
Let's outline the main diagnostic methods that parents can perform in order to decide which doctor to contact.
- A visual examination of a child's eyes to determine if tearing is caused by injury or contamination.
 In the event of an injury, the help of an ophthalmologist and traumatologist may be required.
In the event of an injury, the help of an ophthalmologist and traumatologist may be required. - Measurement of body temperature and examination of the throat for redness. Fever and the presence of redness are signs of SARS or influenza. In this case, a consultation with a therapist is necessary.
- The formation of pus and severe redness of the eyelids may indicate a viral eye infection. In this case, you need to contact an ophthalmologist.
If parents find it difficult to determine the cause of lacrimation, then a visit to the general practitioner is recommended, who will redirect to a specialist.
When to see a doctor
Seeing a doctor for watery eyes in children is not always necessary. If the reason was a long stay at the computer, then rest from this type of activity will solve the problem. The eyes will stop straining, there will be normal hydration of the cornea and tearing will stop.
Things are different when the causes of lacrimation are different and certain symptoms are present.
- The child has watery eyes and a severe runny nose - these symptoms are typical for both allergic reactions and colds and viral diseases. It is noteworthy that the redness of the proteins is also characteristic in both cases. Allergic reactions are characterized by pronounced swelling and swelling not only of the eyelids, but also of the bridge of the nose. But this cannot be a decisive factor for independent determination of the cause of lacrimation in a child by parents. Therefore, you need to contact a specialist. If the child had no previous allergic reactions, then the likelihood of an infectious disease is high. But a specialist can accurately diagnose the cause using additional research methods.
- The child has watery eyes and an elevated body temperature - this combination of symptoms often indicates a viral infection (ARI, tonsillitis, influenza, etc.). At elevated temperatures, redness of the proteins is always noted, the eyes are irritated, and lacrimation increases.
 This is a normal protective reaction during the course of infectious diseases.
This is a normal protective reaction during the course of infectious diseases.
So, we conclude that if lacrimation is combined with other symptoms, it is necessary to consult an appropriate doctor. With lacrimation, runny nose and fever, the help of a pediatric therapist may be required, as these are symptoms of colds and viral diseases. If the lacrimation and runny nose are allergic in nature, a consultation with a pediatric allergist is required. With a combination of lacrimation with swelling and the appearance of pus, it is necessary to contact a pediatric ophthalmologist to prevent the spread of infection in the eye.
Treatment
The choice of treatment method depends on the established cause. For each case - whether it is an infectious disease, an allergic reaction or a cold, there is a different treatment protocol.
The specialist also takes into account the individual characteristics of the child, the presence of concomitant or chronic diseases, the general condition of the patient. With a simple ingress of dust and debris, it may be sufficient to simply wash the eyes with a decoction of chamomile or sage to relieve irritation.
With a simple ingress of dust and debris, it may be sufficient to simply wash the eyes with a decoction of chamomile or sage to relieve irritation.
For a cold that is accompanied by conjunctivitis and watery eyes, the focus is on treating the cold itself and treating the eyes to relieve irritation and symptoms. Treatment of infectious diseases may require the use of antibiotics.
If the problem is of an allergic nature, contact with the allergen must first be eliminated, and in the future, try to exclude the possibility of such contact.
Prevention of lacrimation in children
Experts recommend the following as preventive measures.
- Regular outdoor walks. Staying in the fresh air contributes to the saturation of the eyes with oxygen, which in turn strengthens it and contributes to the proper development of this organ.
- Taking special vitamin complexes aimed at improving vision. Proper nutrition is also an important point - the diet should include the nutrients necessary for the eyes.

- Eye exercises recommended. It should be done daily. A set of special exercises helps to strengthen the muscles of the eyes, relieve tension and ultimately maintain healthy vision.
- Children must adhere to the mode of work at the computer and other types of gadgets. Every hour should take breaks of 10-15 minutes.
How to make an appointment with a specialist
To determine the causes of watery eyes in a child, you need to make an appointment with a doctor.
You can make an appointment by calling +7 (495) 775-73-60 (around the clock), as well as on the website using the online form. Clinic address: Moscow, 2nd Tverskoy-Yamskoy per., 10 (metro stations Mayakovskaya, Tverskaya, Belorusskaya, Novoslobodskaya).
Make an appointment
Leave your phone number and we will help you.
12:3013:0013:3014:0014:3015:0015:3016:00
I consent to the processing of the personal data specified by me for the purpose of processing applications (appointments) on the terms of processing personal data in accordance with "Personal data processing policy in JSC "Medicina".