Baby spinal problems
Spina Bifida (for Parents) - Nemours KidsHealth
What Is Spina Bifida?
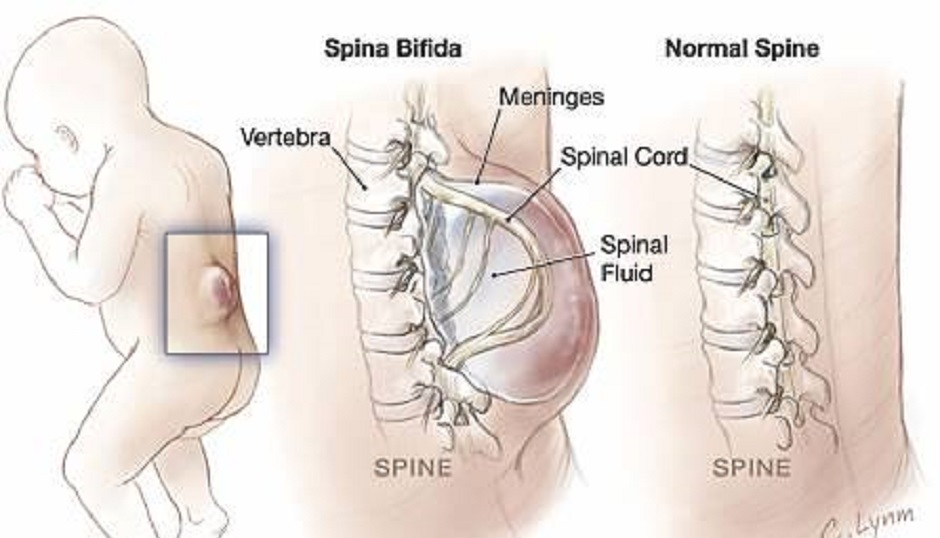
Spina bifida (SPY-nuh BIF-ih-duh) is when a baby's backbone (spine) does not form normally before birth.
The condition can be mild or severe. Treatments can help babies born with spina bifida.
What Are the Types of Spina Bifida?
All types of spina bifida cause an opening in the spine's bones:
- Spina bifida occulta: This is a gap in the bones in the spine but the spinal cord and meninges do not push through it. They are in their normal place inside the spinal canal, and there's no opening on the baby's back.
- Meningocele: This is when a sac that contains spinal fluid pushes through the gap in the spine. The spinal cord is in its normal place in the spinal canal. The skin over the meningocele often is open.
- Myelomeningocele: This is when a sac that contains the meninges, spinal fluid, and part of the spinal cord pushes through the gap in the spine and the skin.
You can see it on the baby's back.
What Are the Signs & Symptoms of Spina Bifida?
Symptoms depend on what kind of spina bifida a baby has and where it is on the spine. Some babies with spina bifida have few or no problems. But sometimes the condition can cause serious problems, including weakness, loss of bladder control, or paralysis.
What Causes Spina Bifida?
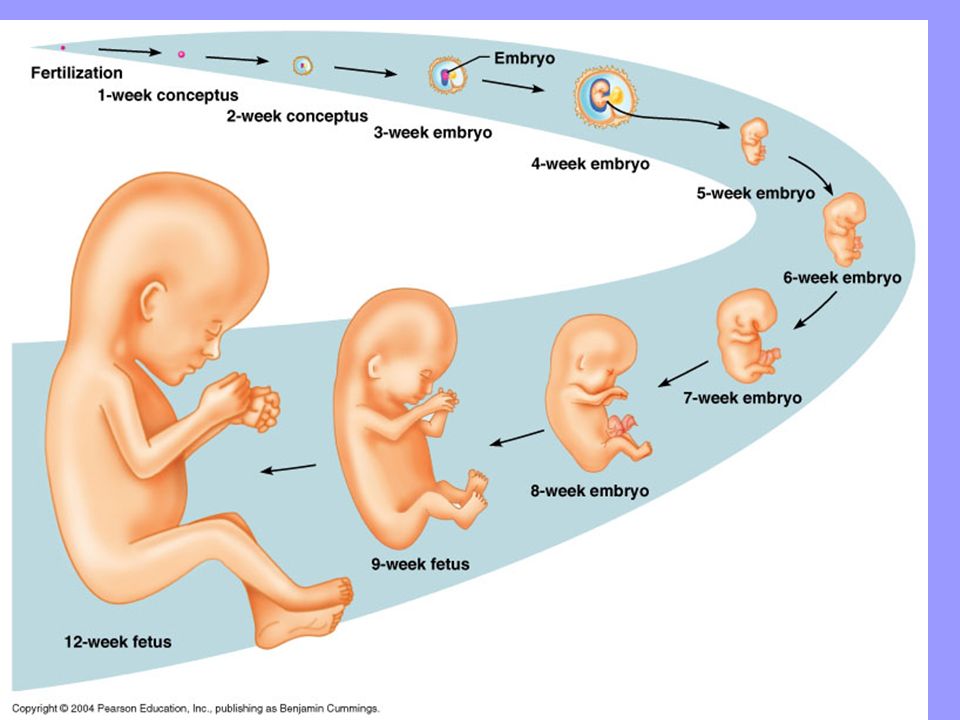
All types of spina bifida happen in the first month of pregnancy. At first, a fetus' spinal cord is flat. It then closes into a tube called a neural tube. If this tube does not fully close, the baby is born with spina bifida.
It’s not clear why some babies get spina bifida. The condition can happen if the mother doesn’t get enough of the vitamin folic acid early in their pregnancy, or:
- took some types of seizure medicines during pregnancy
- already has had a baby with spina bifida
- has diabetes
How Is Spina Bifida Diagnosed?
During pregnancy, a blood test called alpha-fetoprotein (AFP) can tell if a woman has a higher risk of having a baby with spina bifida.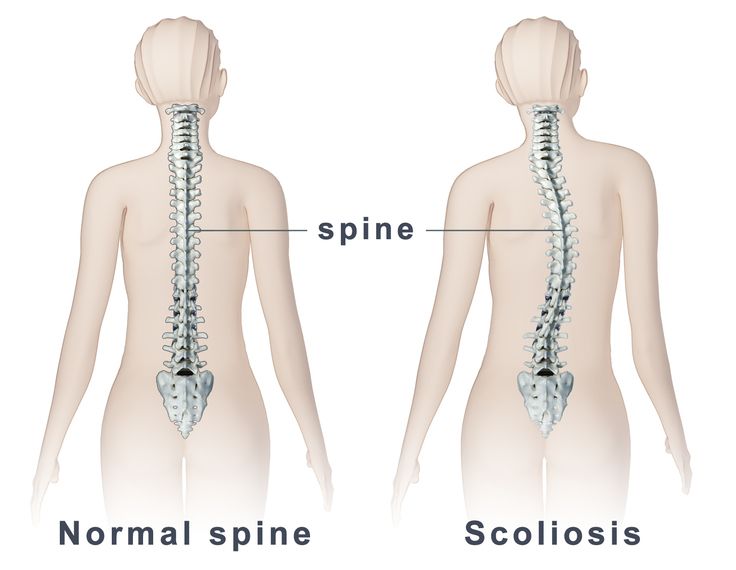 A prenatal ultrasound or fetal MRI can show whether a baby has it.
A prenatal ultrasound or fetal MRI can show whether a baby has it.
If it's not diagnosed during pregnancy, sometimes the condition is seen right away when the baby is born.
Spina bifida occulta, though, usually doesn't cause symptoms. Often, it's found when doctors do an X-ray or other imaging study of the spine for another reason. Sometimes doctors find spina bifida by doing an ultrasound after they notice a dimple, patch of hair, or red patch at the base of a baby's spine.
How Is Spina Bifida Treated?
Treatment for spina bifida depends on how severe it is. Many babies with spina bifida occulta do not need any treatment.
Babies with meningocele or myelomeningocele will need care from a team that can include a neurosurgeon, urologist, orthopedic surgeon, physical therapist, occupational therapist, and social worker.
Sometimes, doctors can treat spina bifida with surgery while the baby is still in the womb.
How Can Parents Help?
A child whose spina bifida is severe may need medical care for life.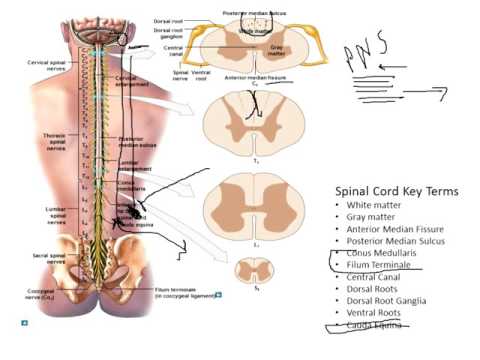 This can feel overwhelming for any family. But you're not alone, and many resources are available to help you and your family. Talk to anyone on the care team about ways to find support. You also can find more information online at:
This can feel overwhelming for any family. But you're not alone, and many resources are available to help you and your family. Talk to anyone on the care team about ways to find support. You also can find more information online at:
- Spina Bifida Association
- Centers for Disease Control and Prevention
Reviewed by: Amy W. Anzilotti, MD
Date reviewed: January 2022
Spina bifida - Symptoms and causes
Overview
Spina bifida is a birth defect that occurs when the spine and spinal cord don't form properly. It's a type of neural tube defect. The neural tube is the structure in a developing embryo that eventually becomes the baby's brain, spinal cord and the tissues that enclose them.
Typically, the neural tube forms early in pregnancy and it closes by the 28th day after conception. In babies with spina bifida, a portion of the neural tube doesn't close or develop properly, causing problems in the spinal cord and in the bones of the spine.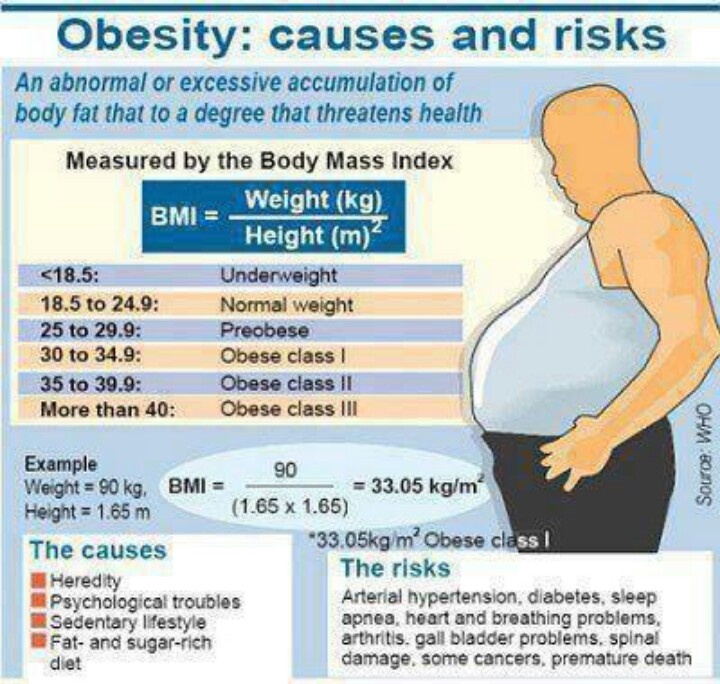
Spina bifida can range from mild to severe, depending on the type of defect, size, location and complications. When necessary, early treatment for spina bifida involves surgery — although such treatment doesn't always completely resolve the problem.
Types
Spina bifida (myelomeningocele)
Spina bifida (myelomeningocele)
Myelomeningocele is a severe type of spina bifida in which the membranes and the spinal nerves protrude at birth, forming a sac on the baby's back. The exposed nervous system may become infected, so prompt surgery is needed after birth.
Spina bifida can occur in different types: spina bifida occulta, myelomeningocele (my-uh-lo-muh-NING-go-seel) or the very rare type meningocele (muh-NING-go-seel).
Spina bifida occulta
Occulta means hidden. It's the mildest and most common type. Spina bifida occulta results in a small separation or gap in one or more of the bones of the spine (vertebrae). Many people who have spina bifida occulta don't even know it, unless the condition is discovered during an imaging test done for unrelated reasons.
Many people who have spina bifida occulta don't even know it, unless the condition is discovered during an imaging test done for unrelated reasons.
Myelomeningocele
Also known as open spina bifida, myelomeningocele is the most severe type. The spinal canal is open along several vertebrae in the lower or middle back. The membranes and spinal nerves push through this opening at birth, forming a sac on the baby's back, typically exposing tissues and nerves. This makes the baby prone to life-threatening infections and may also cause paralysis and bladder and bowel dysfunction.
Meningocele
This rare type of spina bifida is characterized by a sac of spinal fluid bulging through an opening in the spine. No nerves are affected in this type, and the spinal cord isn't in the fluid sac. Babies with meningocele may have some minor problems with functioning, including those affecting the bladder and bowels.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Signs and symptoms of spina bifida vary by type and severity, and also between individuals.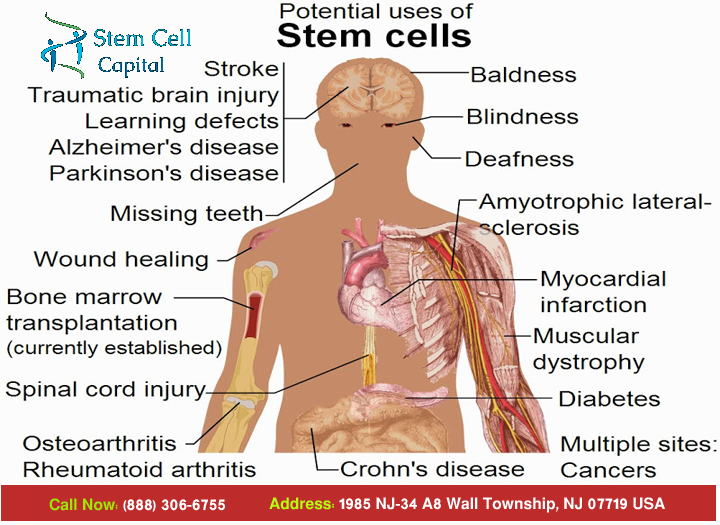
- Spina bifida occulta. Typically, there aren't any signs or symptoms because the spinal nerves aren't involved. But you can sometimes see signs on the newborn's skin above the spinal problem, including a tuft of hair, a small dimple or a birthmark. Sometimes, these skin marks can be signs of an underlying spinal cord issue that can be discovered with MRI or spinal ultrasound in a newborn.
- Meningocele. This type may cause problems with bladder and bowel function.
- Myelomeningocele. In this severe type of spina bifida:
- The spinal canal remains open along several vertebrae in the lower or middle back
- Both the membranes and the spinal cord or nerves protrude at birth, forming a sac
- Tissues and nerves usually are exposed, though sometimes skin covers the sac
When to see a doctor
Typically, myelomeningocele is diagnosed before or right after birth, when medical care is available. Children diagnosed with this condition should be followed by a specialized team of health care providers throughout their lives. Families should be educated on the different complications to watch for.
Children diagnosed with this condition should be followed by a specialized team of health care providers throughout their lives. Families should be educated on the different complications to watch for.
Children with spina bifida occulta typically don't have any symptoms or complications, so usually only routine pediatric care is needed.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information.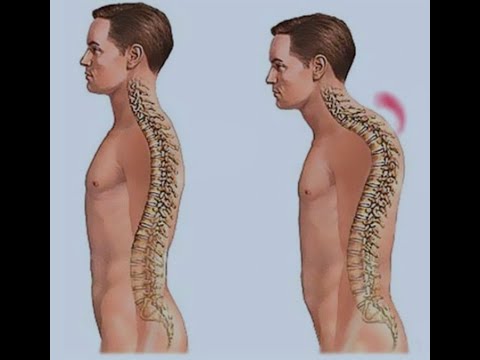 If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Doctors aren't certain what causes spina bifida. It's thought to result from a combination of genetic, nutritional and environmental risk factors, such as a family history of neural tube defects and folate (vitamin B-9) deficiency.
Risk factors
Spina bifida is more common among white people and Hispanics, and females are affected more often than males. Although doctors and researchers don't know for sure why spina bifida occurs, they have identified some risk factors:
- Folate deficiency.
 Folate, the natural form of vitamin B-9, is important to the development of a healthy baby. The synthetic form, found in supplements and fortified foods, is called folic acid. A folate deficiency increases the risk of spina bifida and other neural tube defects.
Folate, the natural form of vitamin B-9, is important to the development of a healthy baby. The synthetic form, found in supplements and fortified foods, is called folic acid. A folate deficiency increases the risk of spina bifida and other neural tube defects. - Family history of neural tube defects. Couples who've had one child with a neural tube defect have a slightly higher chance of having another baby with the same defect. That risk increases if two previous children have been affected by the condition. In addition, women who were born with a neural tube defect have a greater chance of giving birth to a child with spina bifida than someone who doesn't have a neural tube defect. However, most babies with spina bifida are born to parents with no known family history of the condition.
- Some medications. For example, anti-seizure medications, such as valproic acid seem to cause neural tube defects when taken during pregnancy.
 This might happen because they interfere with the body's ability to use folate and folic acid.
This might happen because they interfere with the body's ability to use folate and folic acid. - Diabetes. Women with diabetes who don't have well-controlled blood sugar have a higher risk of having a baby with spina bifida.
- Obesity. Pre-pregnancy obesity is associated with an increased risk of neural tube birth defects, including spina bifida.
- Increased body temperature. Some evidence suggests that increased body temperature (hyperthermia) in the early weeks of pregnancy may increase the risk of spina bifida. Increases in core body temperature, due to fever or use of a sauna or hot tub, have been associated with a slightly increased risk of spina bifida.
If you have known risk factors for spina bifida, talk with your doctor to determine if you need a larger dose or prescription dose of folic acid, even before a pregnancy begins.
If you take medications, tell your doctor. If you plan ahead, some medications can be adjusted to diminish the potential risk of spina bifida.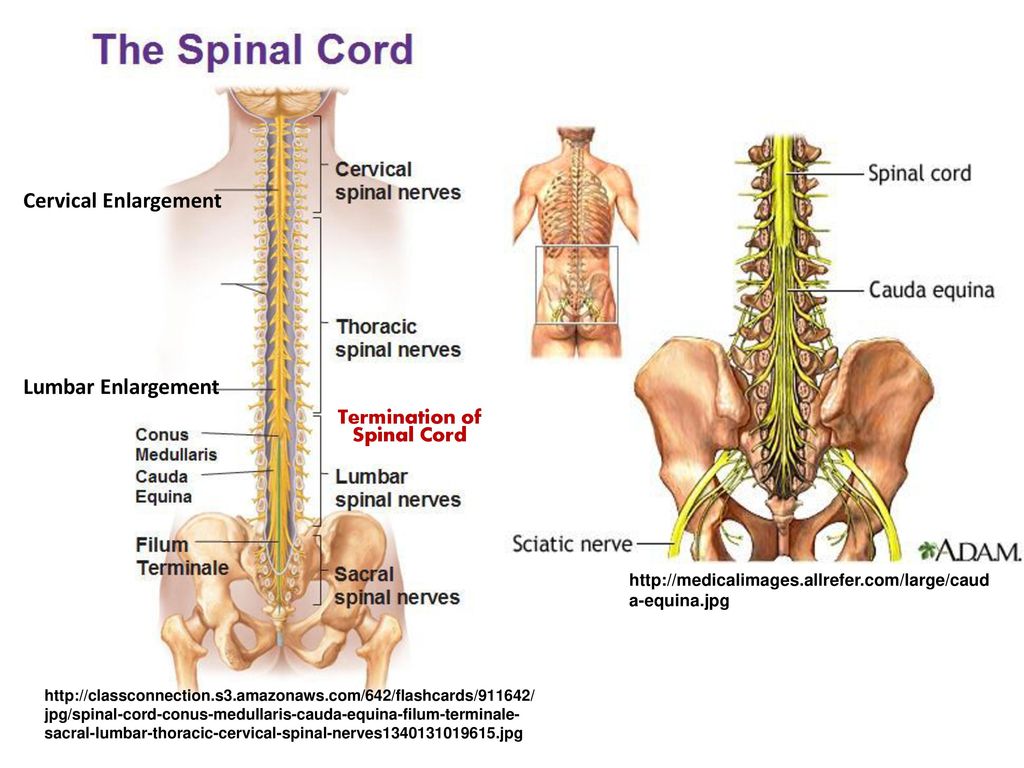
Complications
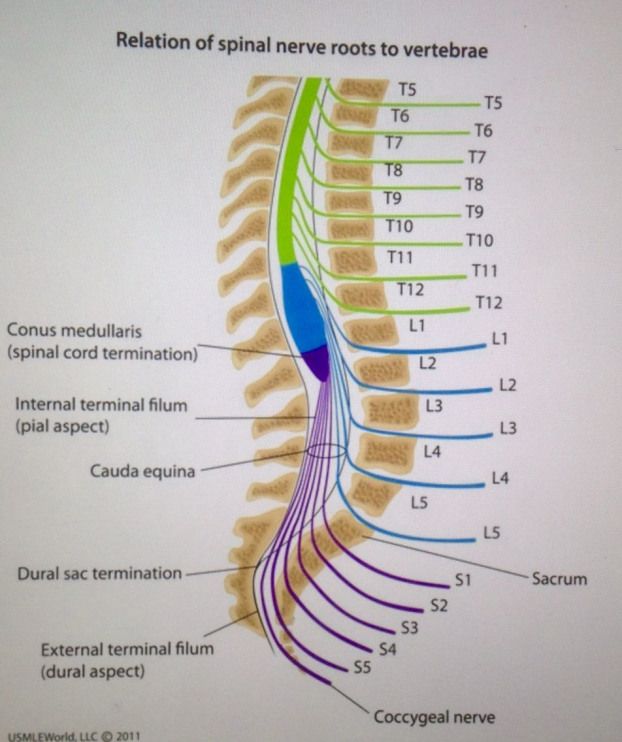
Spina bifida may cause minimal symptoms or minor physical problems. But severe spina bifida can lead to more significant physical conditions. Severity is affected by:
- The size and location of the neural tube defect
- Whether skin covers the affected area
- Which spinal nerves come out of the affected area of the spinal cord
This list of possible complications may seem overwhelming, but not all children with spina bifida get all of these complications. Many of these complications can be treated.
- Walking and mobility problems. The nerves that control the leg muscles don't work properly below the area of the spina bifida defect. This can cause muscle weakness of the legs and sometimes paralysis. Whether a child can walk typically depends on where the defect is, its size, and the care received before and after birth.
- Orthopedic complications. Children with myelomeningocele can have a variety of problems in the legs and spine because of weak muscles in the legs and back.
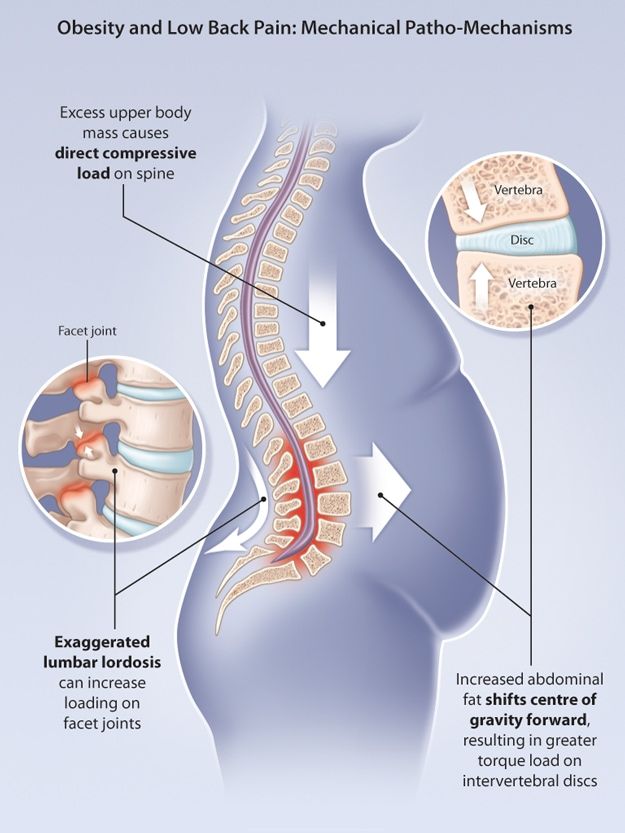 The types of problems depend on the location of the defect. Possible problems include orthopedic issues such as:
The types of problems depend on the location of the defect. Possible problems include orthopedic issues such as: - Curved spine (scoliosis)
- Abnormal growth
- Dislocation of the hip
- Bone and joint deformities
- Muscle contractures
- Bowel and bladder problems. Nerves that supply the bladder and bowels usually don't work properly when children have myelomeningocele. This is because the nerves that supply the bowel and bladder come from the lowest level of the spinal cord.
- Accumulation of fluid in the brain (hydrocephalus). Babies born with myelomeningocele commonly experience accumulation of fluid in the brain, a condition known as hydrocephalus.
- Shunt malfunction. Shunts placed in the brain to treat hydrocephalus can stop working or become infected. Warning signs may vary. Some of the warning signs of a shunt that isn't working include:
- Headaches
- Vomiting
- Sleepiness
- Irritability
- Swelling or redness along the shunt
- Confusion
- Changes in the eyes (fixed downward gaze)
- Trouble feeding
- Seizures
- Chiari malformation type II.
 Chiari malformation (kee-AH-ree mal-for-MAY-shun) type 2 is a common problem with the brain in children who have the myelomeningocele type of spina bifida. The brainstem is the lowest part of the brain above the spinal cord. In Chiari malformation type 2, the brainstem is elongated and positioned lower than usual. This can cause problems with breathing and swallowing. Rarely, compression on this area of the brain occurs and surgery is needed to relieve the pressure.
Chiari malformation (kee-AH-ree mal-for-MAY-shun) type 2 is a common problem with the brain in children who have the myelomeningocele type of spina bifida. The brainstem is the lowest part of the brain above the spinal cord. In Chiari malformation type 2, the brainstem is elongated and positioned lower than usual. This can cause problems with breathing and swallowing. Rarely, compression on this area of the brain occurs and surgery is needed to relieve the pressure. - Infection in the tissues surrounding the brain (meningitis). Some babies with myelomeningocele may develop meningitis, an infection in the tissues surrounding the brain. This potentially life-threatening infection may cause brain injury.
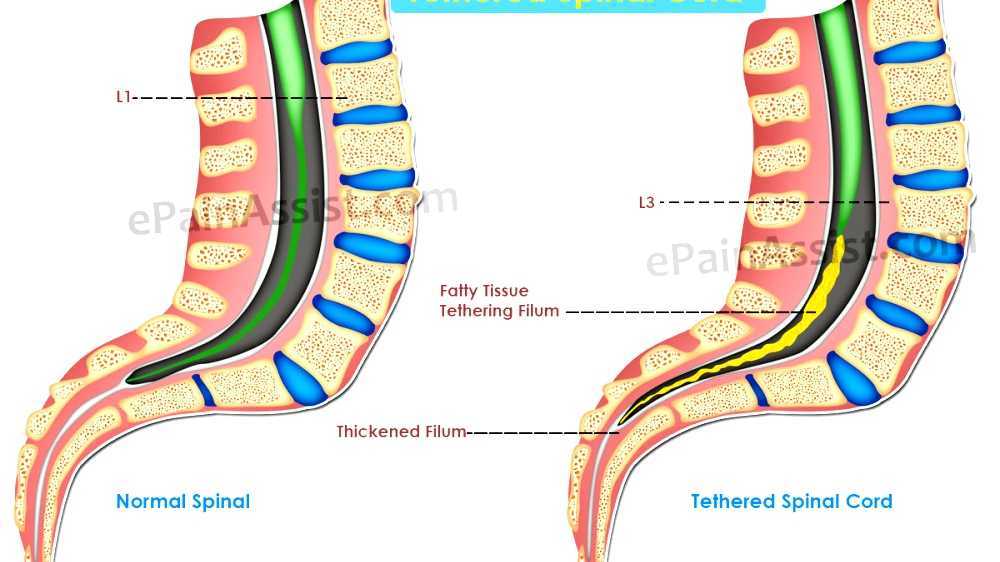
- Tethered spinal cord. Tethered spinal cord results when the spinal nerves bind to the scar where the defect was closed surgically. The spinal cord is less able to grow as the child grows. This progressive tethering can cause loss of muscle function to the legs, bowel or bladder.
 Surgery can limit the degree of disability.
Surgery can limit the degree of disability. - Sleep-disordered breathing. Both children and adults with spina bifida, particularly myelomeningocele, may have sleep apnea or other sleep disorders. Assessment for a sleep disorder in those with myelomeningocele helps detect sleep-disordered breathing, such as sleep apnea, which warrants treatment to improve health and quality of life.
- Skin problems. Children with spina bifida may get wounds on their feet, legs, buttocks or back. They can't feel when they get a blister or sore. Sores or blisters can turn into deep wounds or foot infections that are hard to treat. Children with myelomeningocele have a higher risk of wound problems in casts.
- Latex allergy. Children with spina bifida have a higher risk of latex allergy, an allergic reaction to natural rubber or latex products. Latex allergy may cause rash, sneezing, itching, watery eyes and a runny nose. It can also cause anaphylaxis, a potentially life-threatening condition in which swelling of the face and airways can make breathing difficult.
 So it's best to use latex-free gloves and equipment at delivery time and when caring for a child with spina bifida.
So it's best to use latex-free gloves and equipment at delivery time and when caring for a child with spina bifida. - Other complications. More problems may arise as children with spina bifida get older, such as urinary tract infections, gastrointestinal (GI) disorders and depression. Children with myelomeningocele may develop learning disorders, such as problems paying attention, and difficulty learning reading and math.
Prevention
Folic acid, taken in supplement form starting at least one month before conception and continuing through the first trimester of pregnancy, greatly reduces the risk of spina bifida and other neural tube defects.
Get folic acid first
Having enough folic acid in your system by the early weeks of pregnancy is critical to prevent spina bifida. Because many women don't discover that they're pregnant until this time, experts recommend that all women of childbearing age take a daily supplement of 400 micrograms (mcg) of folic acid.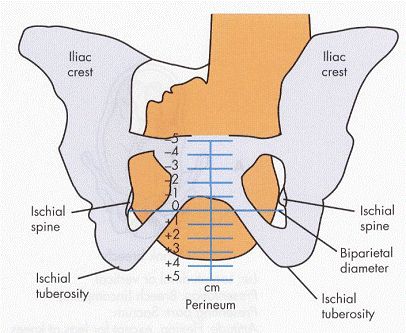
Several foods are fortified with 400 mcg of folic acid per serving, including:
- Enriched bread
- Pasta
- Rice
- Some breakfast cereals
Folic acid may be listed on food packages as folate, which is the natural form of folic acid found in foods.
Planning pregnancy
Adult women who are planning pregnancy or who could become pregnant should be advised to get 400 to 800 mcg of folic acid a day.
Your body doesn't absorb folate as easily as it absorbs synthetic folic acid, and most people don't get the recommended amount of folate through diet alone, so vitamin supplements are necessary to prevent spina bifida. And it's possible that folic acid will also help reduce the risk of other birth defects, including cleft lip, cleft palate and some congenital heart defects.
It's also a good idea to eat a healthy diet, including foods rich in folate or enriched with folic acid. This vitamin is present naturally in many foods, including:
This vitamin is present naturally in many foods, including:
- Beans and peas
- Citrus fruits and juices
- Egg yolks
- Milk
- Avocados
- Dark green vegetables, such as broccoli and spinach
When higher doses are needed
If you have spina bifida or if you've previously given birth to a child with spina bifida, you'll need extra folic acid before you become pregnant. If you're taking anti-seizure medications or you have diabetes, you may also benefit from a higher dose of this B vitamin. Check with your doctor before taking additional folic acid supplements.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Scoliosis of the spine in children and adolescents - how to treat?
With scoliosis, the spine deviates to the side, and the displaced vertebrae change their shape. The problem is not limited to an aesthetic defect and can have serious consequences for the whole organism.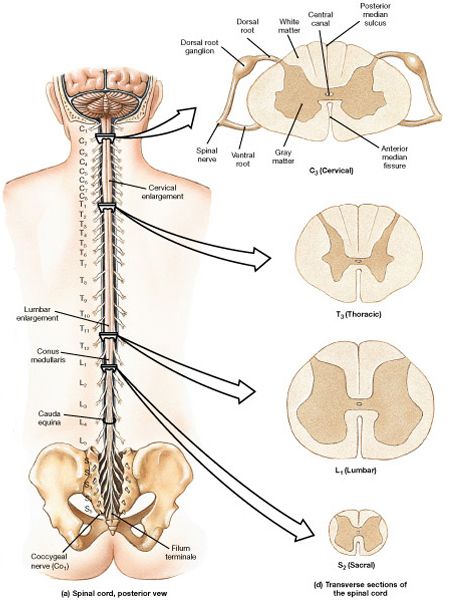
It is very important to identify the deformity in time and start treatment in childhood, since the spinal column of an adult is difficult to correct.
Curvature of the spine in children causes pathological changes in itself and surrounding tissues. These changes lead to a turn (torsion) of the vertebral bodies and a violation of the motor stereotype, and also negatively affect the state of the intracavitary organs. nine0003
Scoliosis is widespread among children and is found in approximately 7% of children, more often in girls. The progress of the disease can lead to displacement, compression and deterioration of the functioning of the organs of the chest cavity and small pelvis.
Species
Scoliosis of the spine in adolescents can take different forms, which have letter designations:
- C - with one scoliotic curve;
- S - 2 arcs; nine0017 Z - 3 arcs.
The curvature of the spine has several degrees, on which the severity of symptoms and methods of orthopedic correction depend.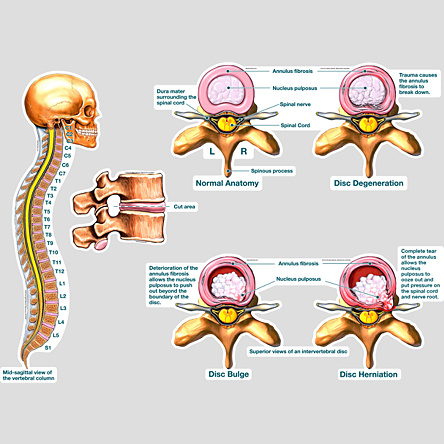 The degrees are determined by the magnitude of the angle of deviation by radiography:
The degrees are determined by the magnitude of the angle of deviation by radiography:
- 1 degree. The spine deviates no more than 10°, the rotation of the vertebrae is small;
- 2nd degree. The angle of the arc is 10–25°, the vertebrae at the maximum point of curvature are turned relative to the axis and moderately deformed; nine0018
- 3 degree. Deviation 25–50°, pronounced rotation of the vertebrae, the presence of a costal hump, persistent deformity of the spinal column;
- 4 degree. The angle is more than 50°, strong curvature causes a significant distortion of the whole body and a shift of the internal organs with a violation of their functioning.
Causes
In the vast majority of cases, the cause remains unidentified, and scoliosis is recognized as idiopathic. Increased risk factors are: nine0003
- asthenia;
- sedentary lifestyle;
- severe stress on the spine, exceeding its capacity;
- bad posture.
The curvature is congenital when a child is born with various anomalies of the vertebrae, spinous processes and ribs. They can be underdeveloped (hemivertebrae), grow together, which is more often observed in the lumbar region and is detected in the form of lumbarization or sacralization. nine0003
Acquired scoliosis often occurs with traumatic injuries, including congenital dislocations of the hip, different leg lengths, and problems with flexion-extension of large joints of the lower extremities.
The curvature of the spine can be of neurogenic, metabolic, rheumatic origin and develop against the background of such diseases as:
- poliomyelitis, Friedreich's ataxia, cerebral palsy, syringomyelia;
- myopathy, muscular dystrophy; nine0017 rickets, cystinosis, bone formation disorders, Hunter's syndrome;
- rheumatoid arthritis;
- osteochondrosis, neurofibromatosis.
Symptoms
Most often, scoliotic disease is detected in schoolchildren and almost never manifests itself in the early stages.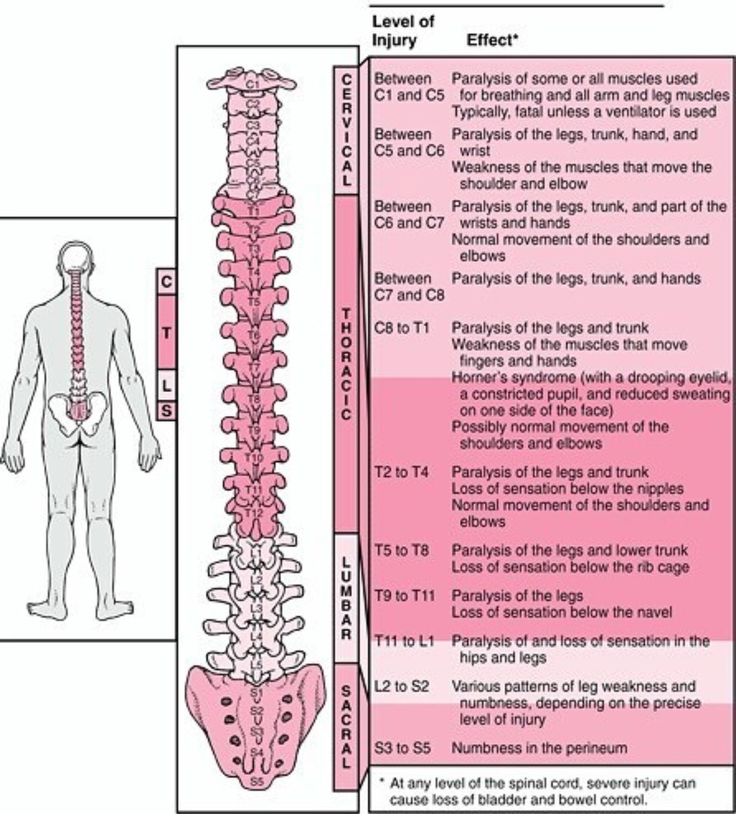 It can be recognized only by some asymmetry of the shoulders and scapular bones.
It can be recognized only by some asymmetry of the shoulders and scapular bones.
Later stages may be characterized by marked deformity of the spine and chest, especially when the body is tilted forward. In the lumbar region, a solid roller appears from the muscles that perform a compensatory function. nine0003
Over time, the ribs begin to protrude, and one side of the body rises above the other. Muscle tone becomes uneven - some muscle groups are constantly tense, while others are practically out of work.
Scoliosis is manifested not only by external signs. The clinical picture usually includes general symptoms, including:
- fatigue;
- poor exercise tolerance; nine0017 back pain of varying intensity;
- disorders of the monthly cycle in girls.
Diagnosis
First, a physical examination. The doctor looks at the level of the shoulders, shoulder blades, pelvic bones, paying attention to the presence of the costal hump, the asymmetry of the skin folds on the back.
The angle of curvature is measured with a scoliometer: a deviation of more than 5–7° is an indication for an x-ray. Pictures are taken in a standing and lying position, according to the results, the spine stability index is evaluated. nine0003
If it is necessary to detail the state of the tissues, MRI, CT, myelography, optical tomography (without radiation exposure) can be prescribed. A prerequisite for the examination is photographing the child from different positions, which is repeated during treatment to monitor the dynamics.
Important! Additional examination may include ultrasound of the abdominal organs, electrocardiogram, etc.
Scoliosis in school-age children: treatment
The main goal of therapy is to prevent the progression of the curvature. To achieve this, methods such as:
- exercise therapy - therapeutic exercises;
- manual therapy;
- orthopedic massage;
- physiotherapy;
- corseting (with incomplete growth of the skeleton).
Effective correction of scoliosis in children is impossible without the systematic implementation of a special set of exercises, which is selected individually. A very important event is also massage, especially with the use of soft manual techniques. nine0003
Keep your back straight!
A detailed plan of how to treat scoliosis of the spine in a teenager is issued by the attending physician. For each child, his points will differ depending on the age, degree of scoliosis and the symptoms present.
If you already have such a plan, or you suspect possible back problems in your child, call and sign up to our center for a consultation. Here you will undergo diagnostics, a course of treatment and receive personal recommendations to maintain the achieved effect. nine0003
All procedures are performed by experienced doctors with deep knowledge in the field of orthopedics and vertebrology. A comfortable stay is also ensured thanks to the latest equipment, which allows you to perform even complex manipulations without causing inconvenience to the patient.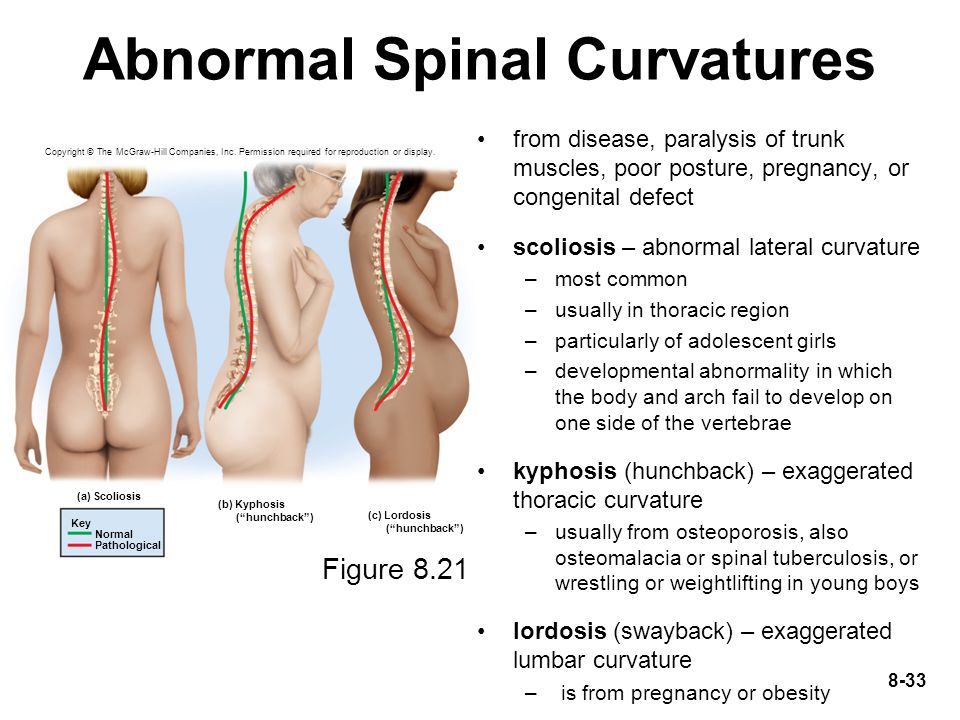
Make an appointment by calling +375 29 628 85 82
Attention, the child's spine!
April 09, 2015
Everyone knows that the spinal column is one of the most important structures of the human body. In Eastern medicine, there is a fair opinion that a healthy spine is the key to the health of the whole organism. Keeping the youth and health of the spine, a person does not age. Already in childhood, the foundations are laid for the health of the spine in adulthood, or the prerequisites for the appearance of the vast majority of problems with it appear. At the same time, diseases and deformities of the spine are the most common orthopedic pathology in children and adolescents today. It should be noted that under the wording "diseases and deformities of the spine" there is a large number of completely different nosological forms. These can be both minor deviations from the norm, and serious problems leading to disability. Therefore, it is not surprising that in adults, problems with the spine are very common. Take, for example, such a common disease of modern man as osteochondrosis. nine0003
Take, for example, such a common disease of modern man as osteochondrosis. nine0003
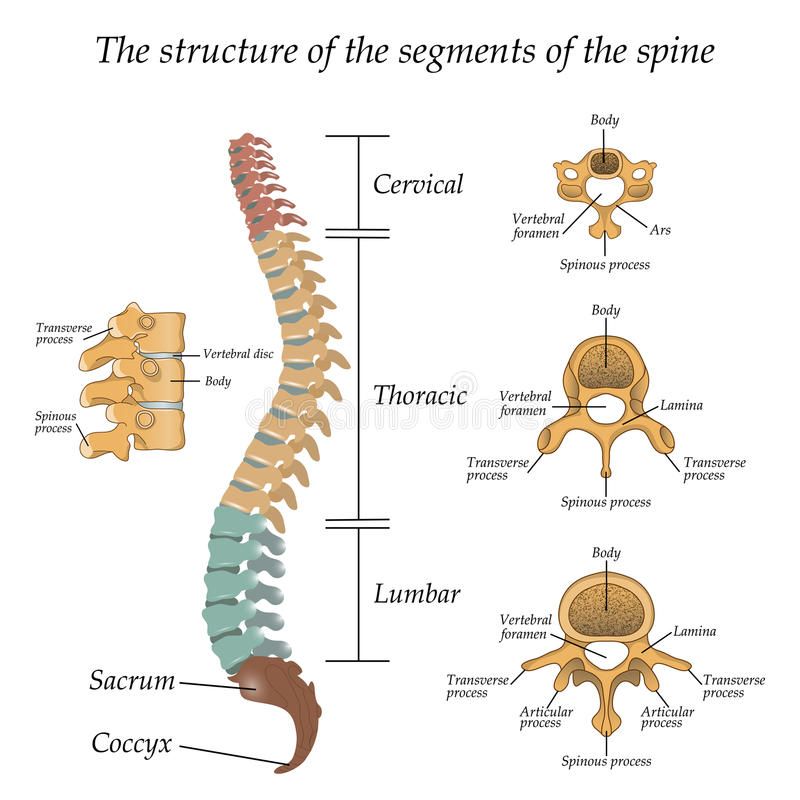
To understand the reason for this situation, it is necessary to remind the reader, what is our spine? The spine, as a key "detail" of the skeleton of the human musculoskeletal system, is a complex and unique structure. Its main functions are protective, supporting and motor. Nature is wise and rational, therefore, its anatomical structure contributes to the qualitative performance of all the functions assigned to the spinal column.
The spinal column consists of 33-34 vertebrae. There are cervical, thoracic, lumbar, sacral and coccygeal regions. The cervical region consists of seven vertebrae, the thoracic - twelve, the lumbar - five, the sacral also has five vertebrae, and the coccyx may consist of four or five vertebrae. 24 vertebrae are interconnected by intervertebral discs, due to which these sections of the spine are mobile. They provide flexibility to the body and allow movement in all three planes.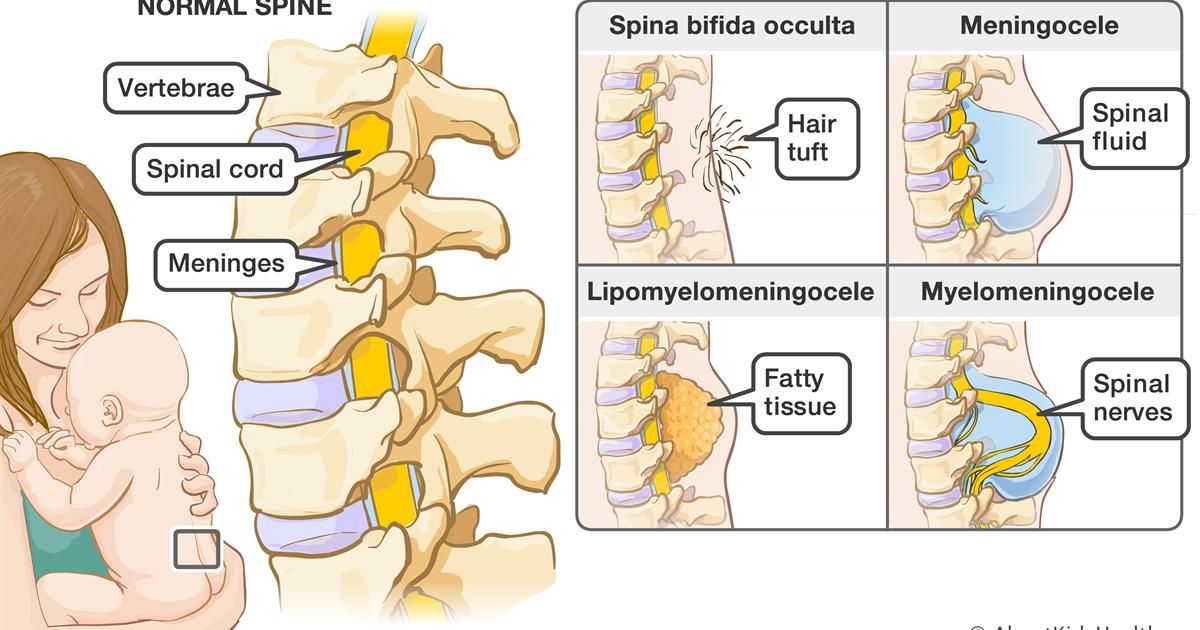 The remaining ten vertebrae do not have the ability to move. This is due to the fact that five sacral vertebrae have fused into one bone, which is called the sacrum. The coccygeal department is rudimentary in nature. nine0003
The remaining ten vertebrae do not have the ability to move. This is due to the fact that five sacral vertebrae have fused into one bone, which is called the sacrum. The coccygeal department is rudimentary in nature. nine0003
All vertebrae are connected to each other by ligaments, consisting of dense connective tissue. Interestingly, this fabric is able to withstand the most extreme loads. Therefore, in case of injuries, a bone rupture often occurs at the site of attachment of the connective tissue, while the ligaments remain intact. Numerous muscles of the back, neck and pelvis provide movement of the spinal column. It is logical to assume that the more complex the structure, the more “weak spots” it has during its growth and formation. This is exactly the case with the growth and functional development of the spinal column. This is an extremely long and dynamic process, which is characterized by a certain phasing. The beginning of the formation of the spine falls on the 16th day of intrauterine development, when its rudiments are formed, and completely ends only by the age of 20-22.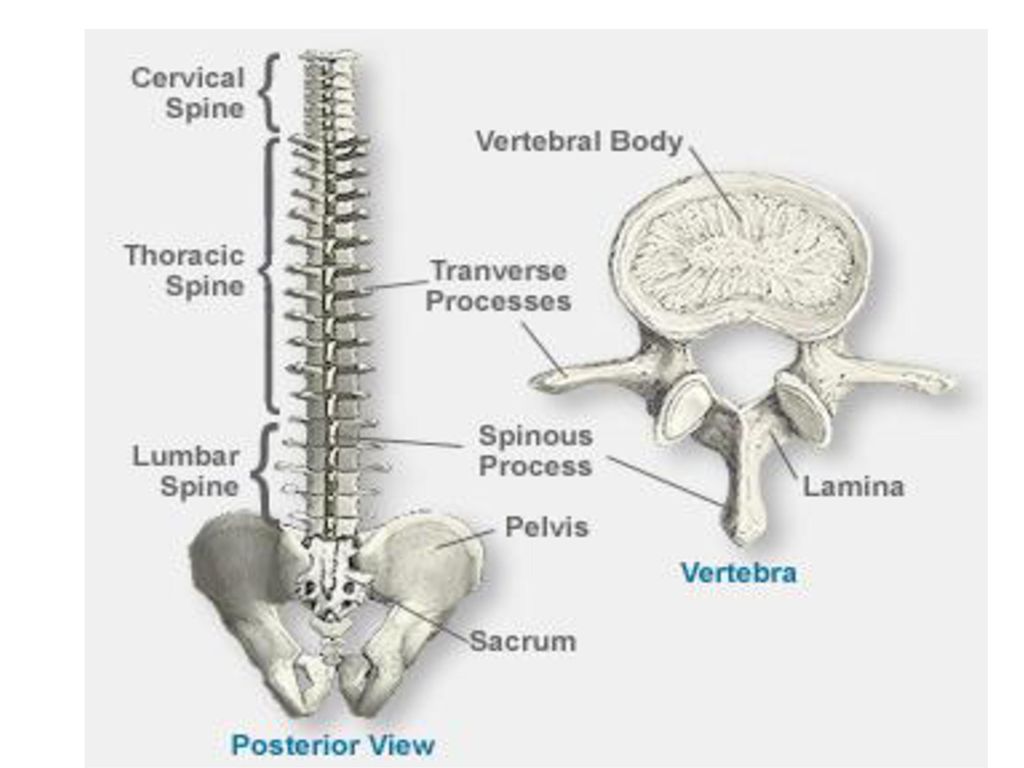 It should be noted that adverse effects on the child's body throughout the entire specified period can lead to certain deviations in the development of the spinal column. nine0003
It should be noted that adverse effects on the child's body throughout the entire specified period can lead to certain deviations in the development of the spinal column. nine0003
Growth and functional development of the spine in time proceeds unevenly. There are physiological fluctuations in the intensity of growth and related features of the development of the spinal column. In the period of intrauterine life, when the child has not yet been born, his spine is already formed and is actively growing. Moreover, it does not just grow, but grows at a "frantic" pace, for example, from the fourth to the sixth months of pregnancy, the length of the fetus increases by 2.5 cm per week, which would correspond to a growth rate of up to 130 cm per year! After the sixth month, the growth rate gradually slows down to 0.5 cm per week. It becomes obvious that the impact on the body of a pregnant woman of any adverse factors (infectious diseases, taking medications, and much more) can lead to various malformations of the spine in the fetus. At the same time, depending on the "aggressiveness" and the timing of the impact of these factors, the degree of severity of anomalies in the development of the spine can vary from gross to barely noticeable. That is why the period of intrauterine life can be designated as the first "dangerous" period in the development of the spine. nine0003
At the same time, depending on the "aggressiveness" and the timing of the impact of these factors, the degree of severity of anomalies in the development of the spine can vary from gross to barely noticeable. That is why the period of intrauterine life can be designated as the first "dangerous" period in the development of the spine. nine0003
After birth, the overall growth of the child is up to 24 cm in the first year of life. And by 3-4 years there is a decrease in the intensity of growth with the transition to the so-called "growth plateau". It should be noted that it is in the first years of a child's life that the formation of normal (physiological) curves of the spinal column occurs. And this age can be justifiably considered the second "dangerous" period in the development of the spine. For example, the well-known rickets can lead to so-called rachitic deformities of the spinal column (especially in the first two years of life). Diseases of other organs and systems, inadequate nutrition, irrational physical activity can also have a significant impact on the formation of posture and even serve as an impetus for the occurrence of serious spinal deformities. nine0003
nine0003
At the age from 4-5 to 10-12 years of life, there is a period characterized by an average annual increase of 4-5 cm. Despite the relatively monotonous growth, one more, already the third "dangerous" period in development spine. It coincides with the beginning of schooling. The emergence of new loads, a fairly long stay in a "forced" position sitting at a desk (it's no secret that modern times dictate the conditions for maximum assimilation of large amounts of information already in the primary grades), especially when a small student is physically unprepared for such loads, often leads to the appearance of various deviations from the side of posture. nine0003
After 10 years, the intensity of growth increases significantly. The duration of the "growth spurt" is 2-4 years, its beginning corresponds to prepubertal age in girls (10.5-13.5 years), and in boys to puberty (12.5-15.5 years). During this period, the maximum growth rate reaches 10 cm (and sometimes more) per year. This period is the fourth "dangerous" period in the development of the spinal column. And it is at this age that such formidable deformities of the spinal column appear as scoliosis, pathological kyphosis. And not only appear, but also progress quite quickly. nine0003
This period is the fourth "dangerous" period in the development of the spinal column. And it is at this age that such formidable deformities of the spinal column appear as scoliosis, pathological kyphosis. And not only appear, but also progress quite quickly. nine0003
Growth rates decrease in girls by the age of 16, in boys - by 18 years, after which a slight increase in body length continues. Slowdown, and then complete cessation of the growth of the spinal column occurs by the age of 16-22. Thus, we considered four potentially dangerous periods in the formation of the spinal column: intrauterine development, the first years of life, 7-8 years, 10-15 years.
Timely detection of problems of the spinal column, the beginning of qualified treatment under the supervision of a pediatric orthopedist is the key to success in treatment. In connection with the above, a healthy child should be examined by a pediatric orthopedist according to the scheme:
- After birth
- 3 months life
- 6 months life
- 1 year
- 1.
 5 years
5 years - 2 years
- From 2 to 7 years Once a year
- From 7 to 8 years old 2 times a year
- From 8 to 10 years Once a year
- From 10 to 15 years old 2 times a year
How can I detect scoliosis in my child? Recommendations to parents. See video:
In the presence of any deviations from the spinal column, treatment and dynamic observation are prescribed individually.
Why shouldn't sunbathing be given to a child who has initial signs of scoliosis? Watch video
Separately, I would like to mention the role of sports and physical education in the formation of a healthy spine.