Anemia caused by pregnancy
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
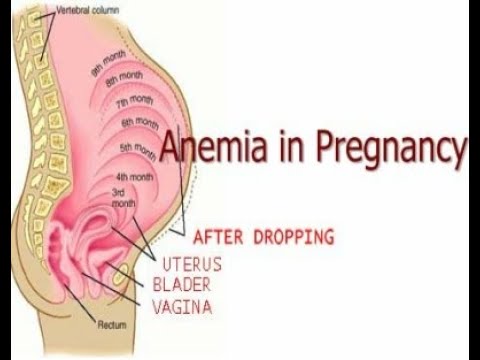
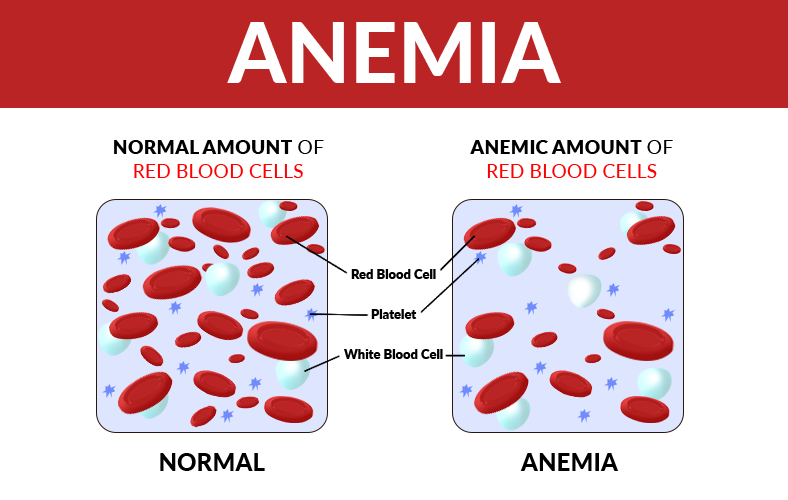
When you're pregnant, you may develop anemia. When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
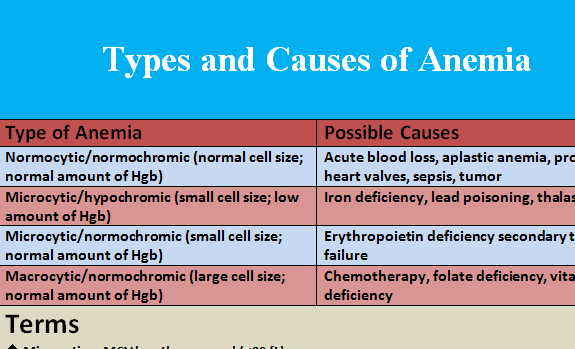
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia. This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.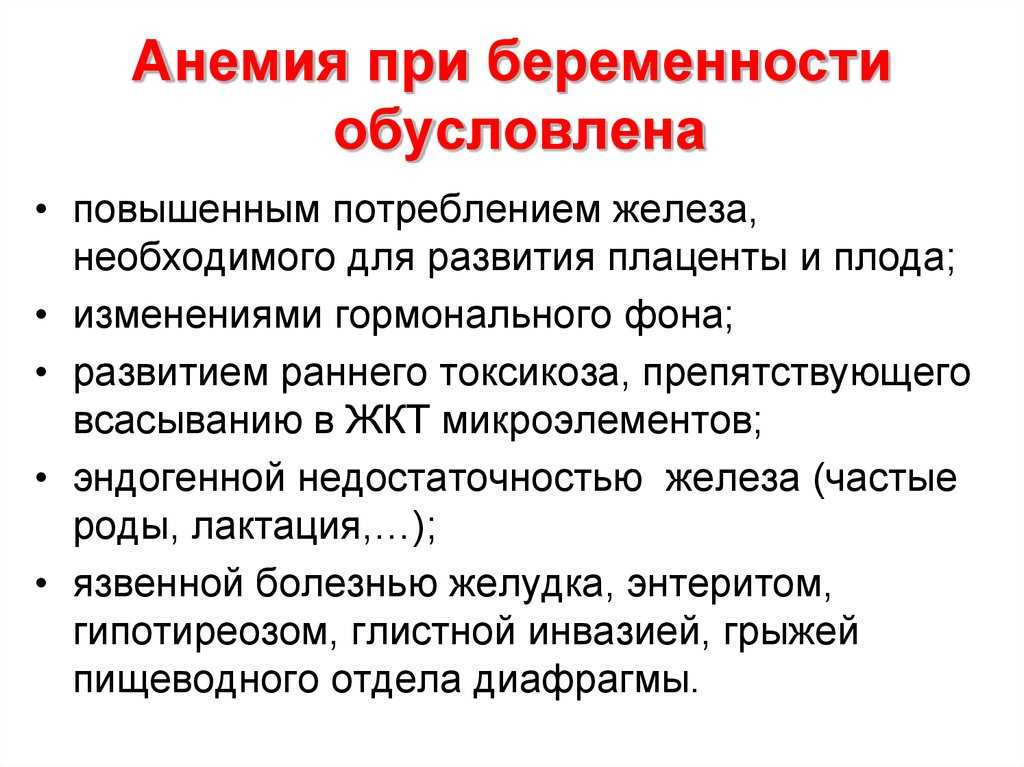
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic.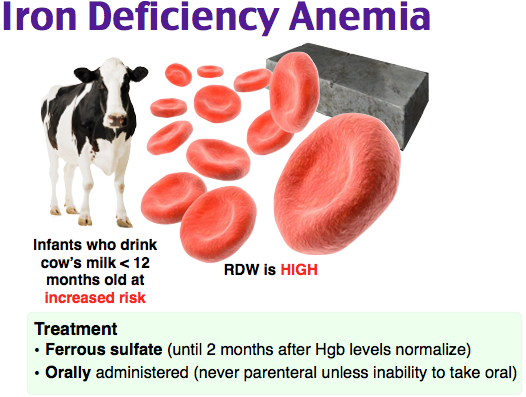 That's because they need more iron and folic acid than usual. But the risk is higher if you:
That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
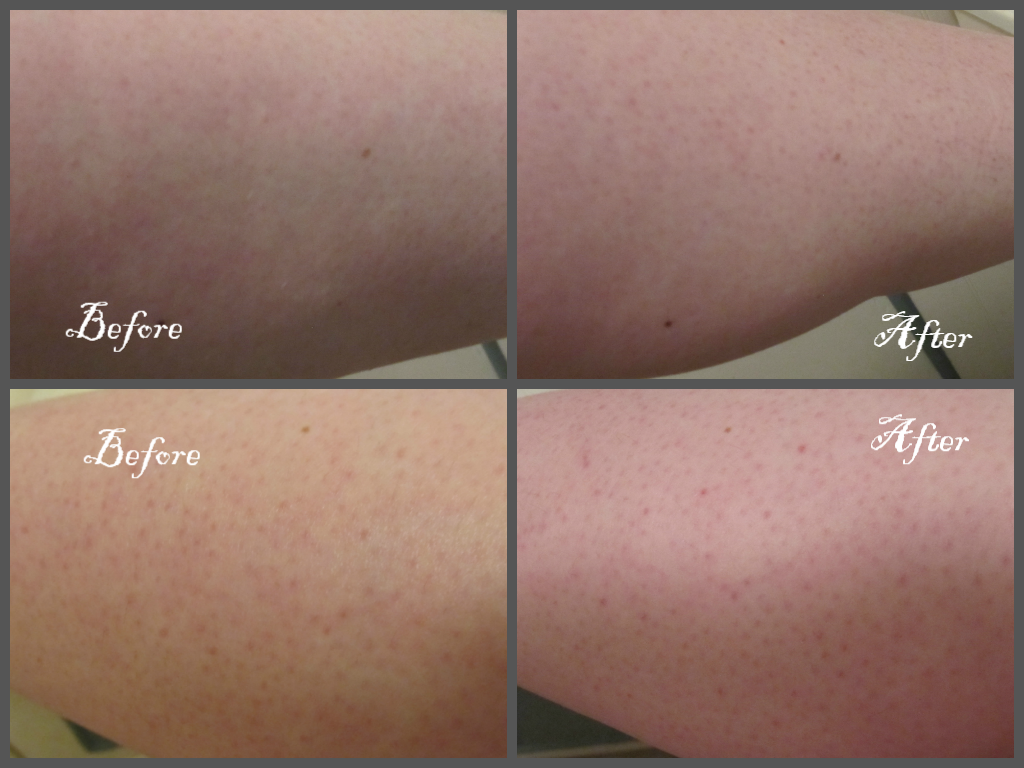
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms. And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.
Tests for Anemia
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia. Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron. These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
When you're pregnant, you may develop anemia.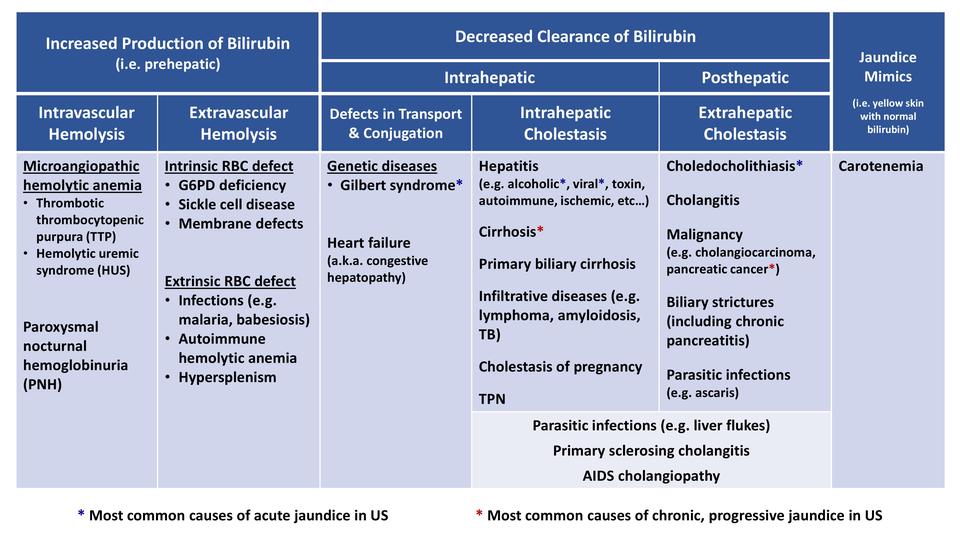 When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia.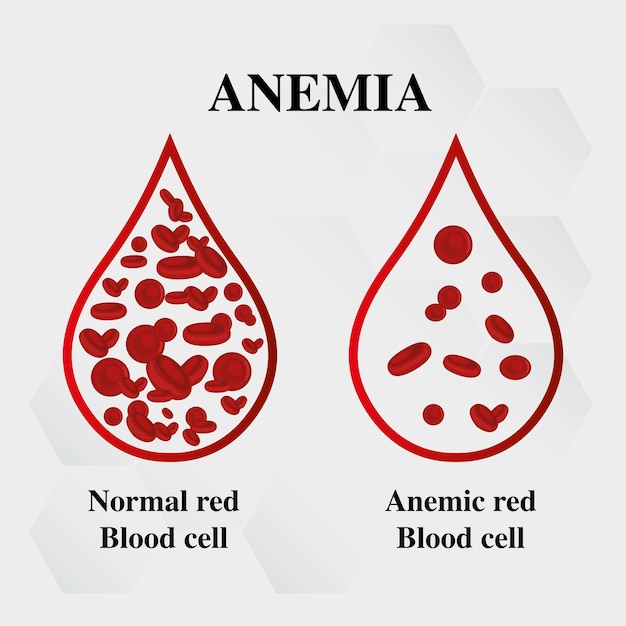 This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic. That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms.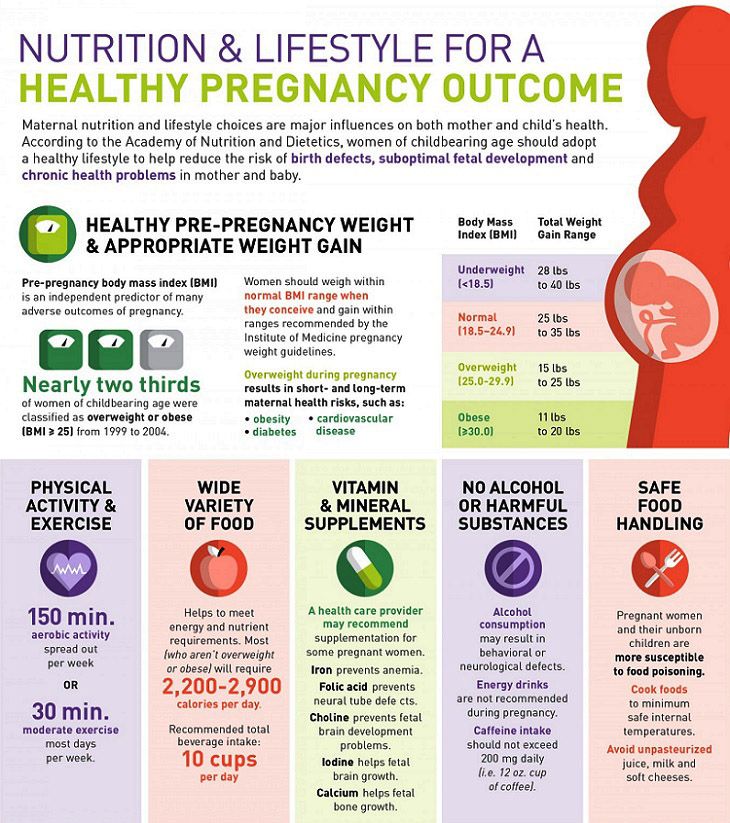 And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.
Tests for Anemia
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia.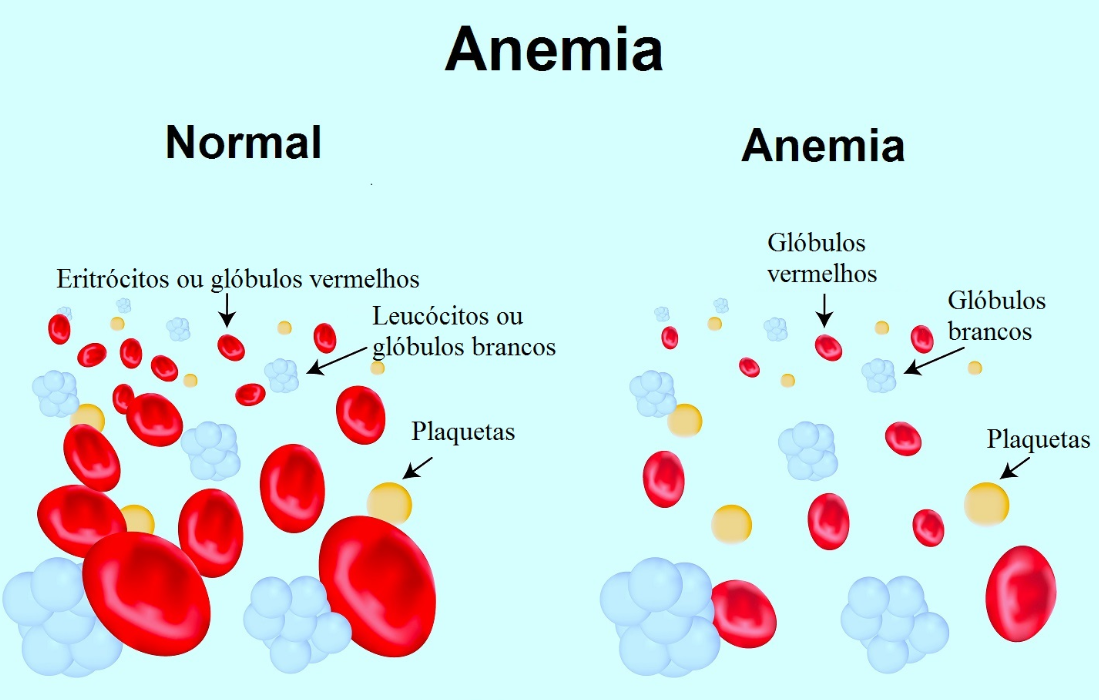 Blood tests typically include:
Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.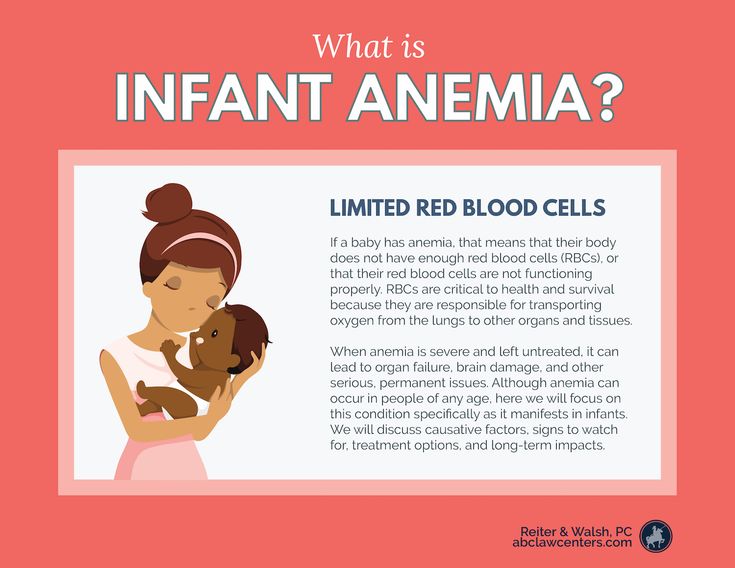
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron. These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Anemia during pregnancy.
 What is Anemia in Pregnancy?
What is Anemia in Pregnancy? IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Anemia during pregnancy is a decrease in hemoglobin levels that occurs during gestation and is pathogenetically associated with it. Manifested by weakness, fatigue, dizziness, perversion of taste and olfactory preferences, cardiac pain, muscle weakness, paresthesia, mucosal lesions, changes in the skin, nails, hair. It is diagnosed using a general clinical blood test and a laboratory study of iron metabolism. For treatment, iron-containing preparations, folic acid, cyanocobalamin are used, according to indications, complex antihypoxic therapy is carried out.
ICD-10
O99.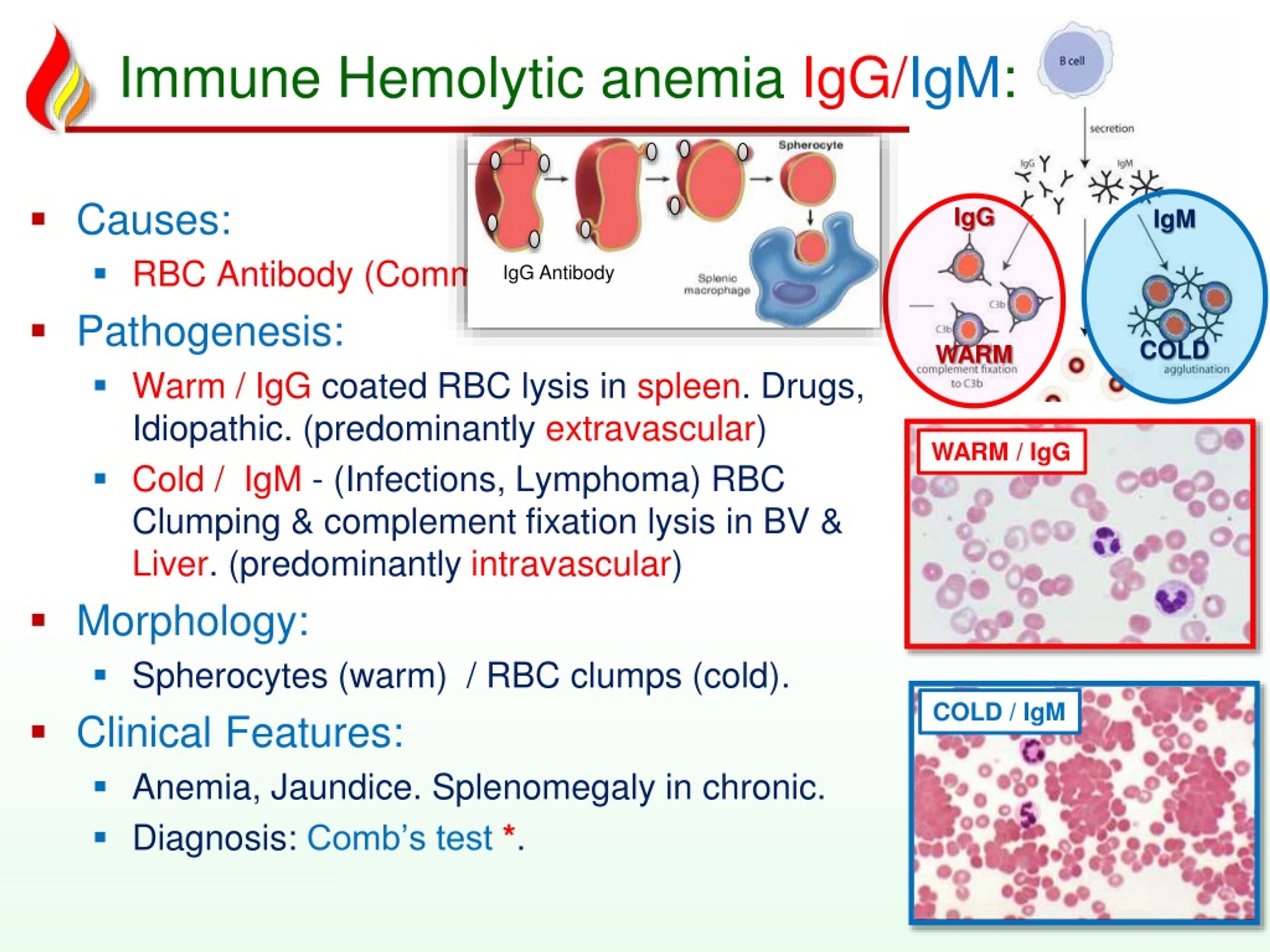 0 Anemia complicating pregnancy, childbirth and the puerperium
0 Anemia complicating pregnancy, childbirth and the puerperium
- Causes of anemia during pregnancy
- Pathogenesis
- Classification
- Symptoms of anemia in pregnancy
- Complications
- Diagnostics
- Treatment of anemia in pregnancy
- Prognosis and prevention
- Prices for treatment
General
The existence of physiological prerequisites for the occurrence of gestational anemia (hydremia) makes this disease one of the most common types of pathology during pregnancy. Manifest forms of the disease with clinically pronounced symptoms in economically developed countries occur in 16-21% of patients, in developing countries their prevalence reaches 80%. At the same time, latent (latent) iron deficiency, taking into account the usefulness of the diet by the end of pregnancy, is observed in 50-100% of women. The predominant form of gestational anemia is iron deficiency, diagnosed at 75-95% of cases.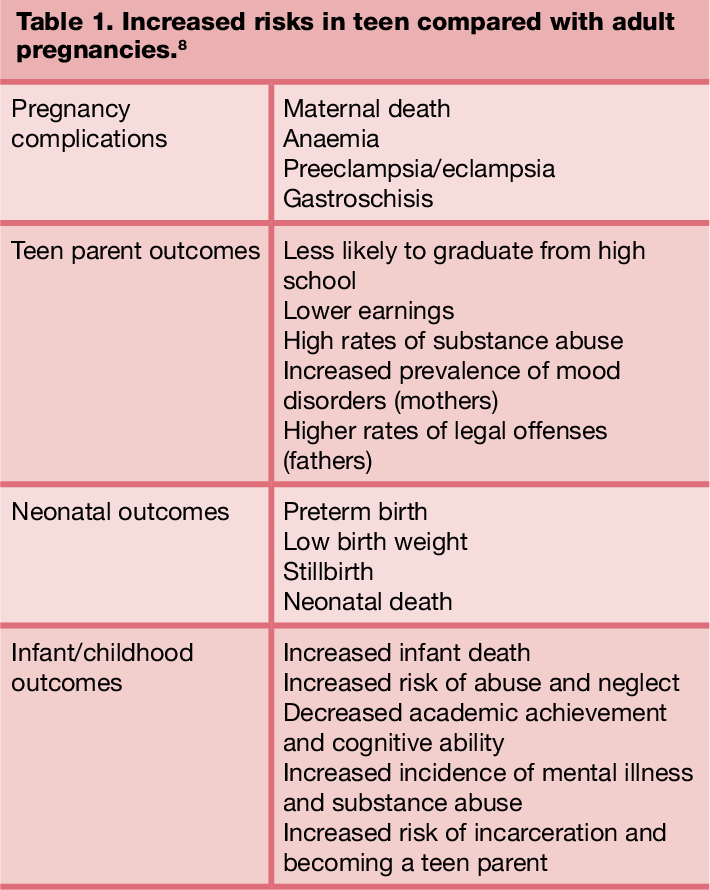 The relevance of timely detection of pathology is associated with a high probability of a complicated course of pregnancy and the occurrence of hypoxic conditions against the background of a physiological increase in oxygen demand by 15-33%.
The relevance of timely detection of pathology is associated with a high probability of a complicated course of pregnancy and the occurrence of hypoxic conditions against the background of a physiological increase in oxygen demand by 15-33%.
Anemia during pregnancy
Causes of anemia during pregnancy
The insufficient content of hemoglobin and red blood cells in the blood of a pregnant woman is due to both factors directly related to gestation and previous diseases. According to the observations of specialists in the field of obstetrics, in most patients, gestational hydremia has such easily explained physiological causes as:
- Increased need for iron. Starting from the second trimester of pregnancy, more iron is required for adequate maintenance of the fetoplacental complex. This trace element is rapidly consumed by the growing fetus, enters the placenta, and is used to increase the total number of red blood cells circulating in the woman's blood.
 By the beginning of the third trimester, the daily requirement of a pregnant woman for iron is at least 4-6 mg, and at 32-34 weeks it requires at least 10 mg / day.
By the beginning of the third trimester, the daily requirement of a pregnant woman for iron is at least 4-6 mg, and at 32-34 weeks it requires at least 10 mg / day. - Physiological hemodilution. During pregnancy, the volume of circulating plasma increases by 40-50%, and the volume of erythrocyte mass only by 20-35%. This is due to the increased need of the body for iron and plastic substances, with insufficient intake of which, the rate of erythropoiesis does not correspond to the rate of increase in BCC. According to WHO recommendations, the permissible level of hemoglobin in pregnant women is reduced to 110.0 g / l, and hematocrit - to 33%.
A factor aggravating anemia in the postpartum period is the physiological loss of up to 150 ml of blood during childbirth, each 2.0-2.5 ml of which contains up to 1 mg of iron. Specialists also identify a number of pathological causes that cause the disease. A decrease in the volume of red blood cells (microcytic variant of anemia) with a corresponding drop in hemoglobin levels is observed in case of poisoning with industrial poisons (for example, lead), many chronic diseases (rheumatism, diabetes, peptic ulcer, gastritis, chronic infectious processes), sideroblastic anemia, thalassemia.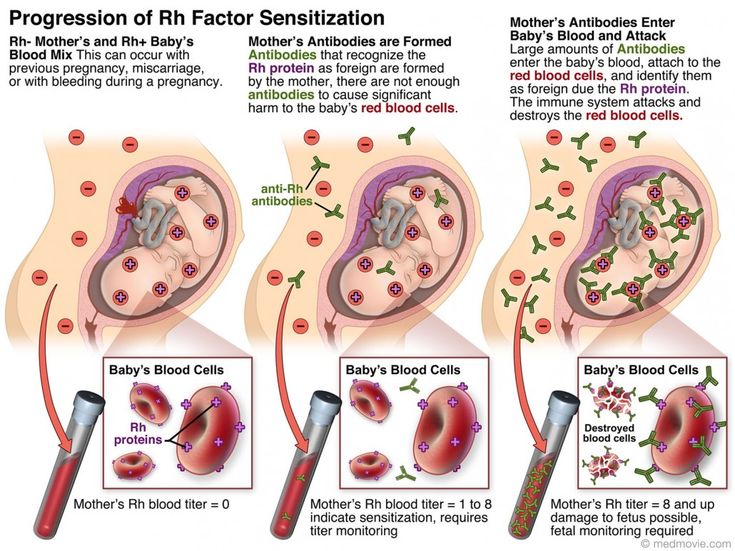 This condition also occurs with iron deficiency due to a lack of meat in the diet and the consumption of products containing non-heme forms of the trace element (plant foods, milk and dairy products).
This condition also occurs with iron deficiency due to a lack of meat in the diet and the consumption of products containing non-heme forms of the trace element (plant foods, milk and dairy products).
Normocytic anemia with a reduced content of normal erythrocytes is more often observed with blood loss due to placental pathology, chronic renal failure, hypothyroidism, hypopituitarism, an autoimmune hemolytic form of the disease, and inhibition of erythropoiesis in the bone marrow. The macrocytic type of anemia with an increase in the volume of erythrocytes is characteristic of a deficiency of folic acid and vitamin B12, acute myelodysplastic syndrome, hepatic pathology (hepatitis, cirrhosis), alcohol dependence, reticulocytosis. Additional risk factors are the low material standard of living of a pregnant woman, frequent childbirth, multiple pregnancy, long-term breastfeeding with a short interbirth period, complicated course of this pregnancy (pronounced early toxicosis with repeated vomiting, gestosis).
Pathogenesis
The mechanism of anemia formation during pregnancy is usually associated with an imbalance between the intake of iron in the body, especially in combination with a deficiency of protein, folic acid, vitamin B12, and their high consumption for plastic purposes. An additional link in the pathogenesis is the inhibition of erythropoiesis due to an increase in the concentration of estradiol and the accumulation of metabolites that have a toxic effect on the bone marrow. The situation is aggravated by immunological changes associated with the constant stimulation of the mother's body with fetal antigens, which increases anti-tissue sensitization. The results of pathophysiological processes are tissue, hemic and circulatory hypoxia with metabolic disorders and further accumulation of harmful metabolic products.
Classification
The optimal criteria for systematizing the forms of anemia in pregnant women are the concentration of hemoglobin in the blood and the element or substance, the deficiency of which led to the onset of the disease. This approach to classification makes it possible to more accurately predict possible complications and select a scheme for managing pregnancy. Modern obstetricians and gynecologists distinguish the following forms of gestational anemia:
This approach to classification makes it possible to more accurately predict possible complications and select a scheme for managing pregnancy. Modern obstetricians and gynecologists distinguish the following forms of gestational anemia:
- By severity: according to the WHO classification, taking into account the level of hemoglobin, the disease is mild (90-109 g/l), moderate (70-89 g/l), severe (less than 70 g/l).
- By type of deficiency: the most common is iron deficiency anemia (in the structure of morbidity it occupies about 95%), folic acid deficiency and B12-deficiency forms of the disease are less common.
Symptoms of anemia during pregnancy
Mild degree usually proceeds latently. With a decrease in the concentration of iron less than 90 g / l, signs of hemic hypoxia (actually anemic syndrome) and iron deficiency in tissues (sideropenic syndrome) become noticeable. The possible development of oxygen starvation is indicated by general weakness, dizziness, tinnitus, discomfort and pain in the precordial region, complaints of increased heart rate, shortness of breath during exercise. The mucous membranes and skin appear pale. A woman becomes irritable, nervous, inattentive, her memory decreases, her appetite worsens.
The mucous membranes and skin appear pale. A woman becomes irritable, nervous, inattentive, her memory decreases, her appetite worsens.
Tissue iron deficiency is manifested by fatigue, perverted taste (desire to eat plaster, chalk, clay, sand, minced meat, raw meat), thickening and brittleness of the nail plates, dryness and hair loss, muscle weakness, urinary incontinence due to weakening of the sphincter apparatus. In some patients, the epithelial membranes are affected: cracks (“seizes”) appear in the corners of the mouth, the oral mucosa becomes inflamed, there are complaints of itching, burning in the vulva. With moderately severe and severe anemia, there is often a slight yellowness of the palms and nasolabial triangle, associated with impaired carotene metabolism in iron deficiency, and a "blue" sclera caused by dystrophic processes.
Complications
The likelihood of pregnancy complications directly depends on the severity of the violations and the time of occurrence of the disease.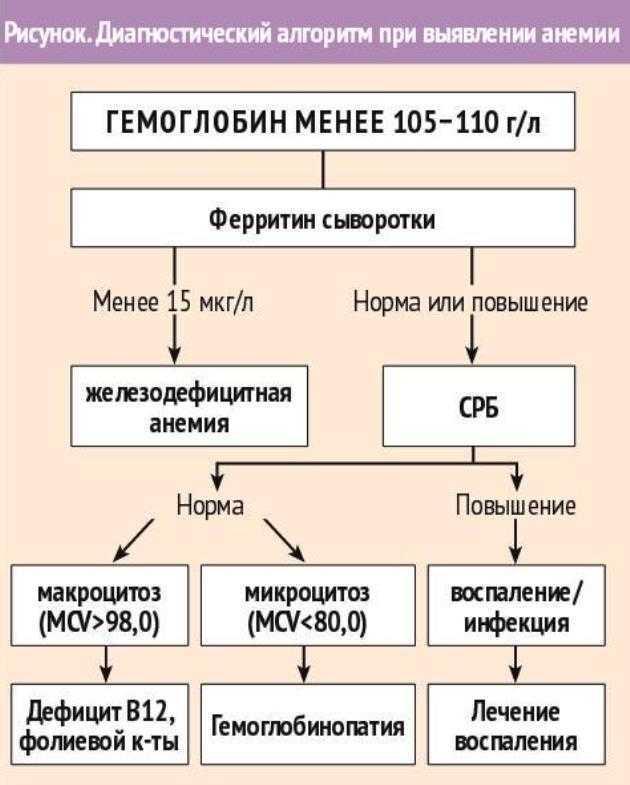 Anemia that developed before conception is especially unfavorable. In such cases, primary placental insufficiency, hypoplasia of the fetal membranes, low location of the placenta and its presentation, early miscarriage, non-developing pregnancy are possible. With the appearance of an anemic symptom complex in the II-III trimesters, the risk of preeclampsia, late miscarriages and premature births, premature detachment of a normally located placenta increases.
Anemia that developed before conception is especially unfavorable. In such cases, primary placental insufficiency, hypoplasia of the fetal membranes, low location of the placenta and its presentation, early miscarriage, non-developing pregnancy are possible. With the appearance of an anemic symptom complex in the II-III trimesters, the risk of preeclampsia, late miscarriages and premature births, premature detachment of a normally located placenta increases.
In severe cases of the disease, myocardial dystrophy occurs, the contractility of the heart muscle worsens. As a result, hemic and tissue hypoxia are aggravated by circulatory one, as a result, the parenchymal organs of the pregnant woman suffer, and decompensation of their function is observed. In childbirth, 10-15% of women in labor show weakness of the labor forces, and abundant bleeding of the hypotonic type is often observed. After childbirth, 10-12% of puerperas and 35-37% of newborns develop various purulent-septic processes. 4 out of 10 nursing mothers have hypogalactia.
4 out of 10 nursing mothers have hypogalactia.
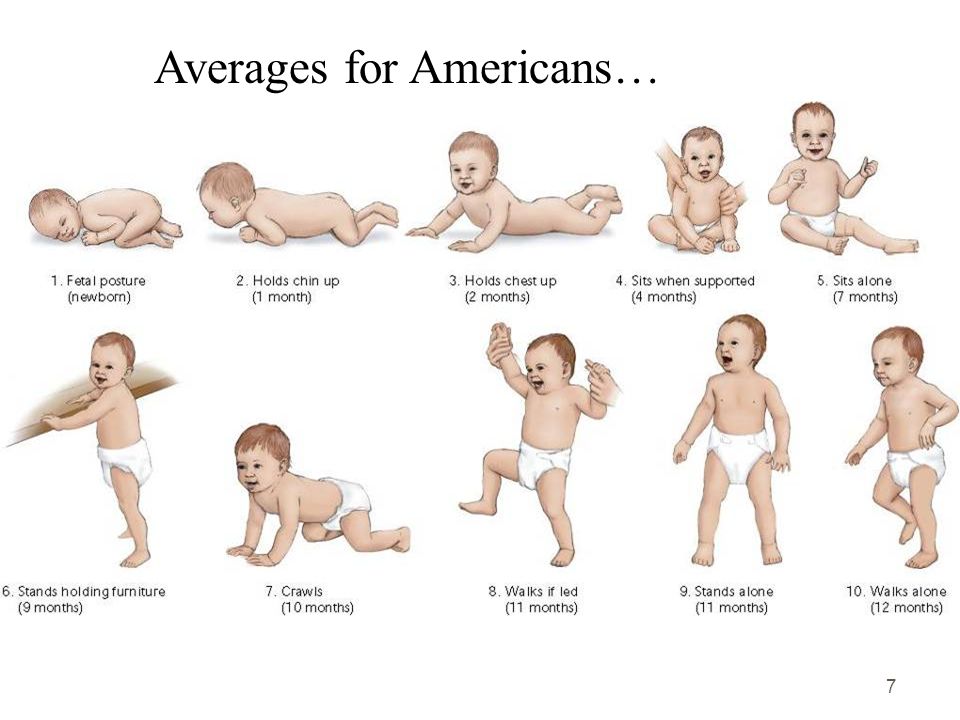
The presence of anemia in a pregnant woman poses a direct threat to the child. Perinatal morbidity with this pathology can increase up to 100%, and mortality - up to 14-15%. Due to fetoplacental insufficiency, fetal hypoxia is noted in 63% of cases, hypoxic brain injury in 40%, and developmental delay in 32%. Almost a third of newborns are born in asphyxia. Deficiency of vitamin B12, folic acid causes anomalies in the development of the spine and nervous system (spina bifida, etc.). In children whose mothers suffered from severe or severe anemia during pregnancy, the function of external respiration is worse established. In the postnatal period, they often lag behind in height and body weight, and are more prone to the occurrence of infectious diseases.
Diagnostics
The key tasks of a diagnostic search for suspected anemia during pregnancy are the assessment of the severity of the disorder and the timely detection of complications.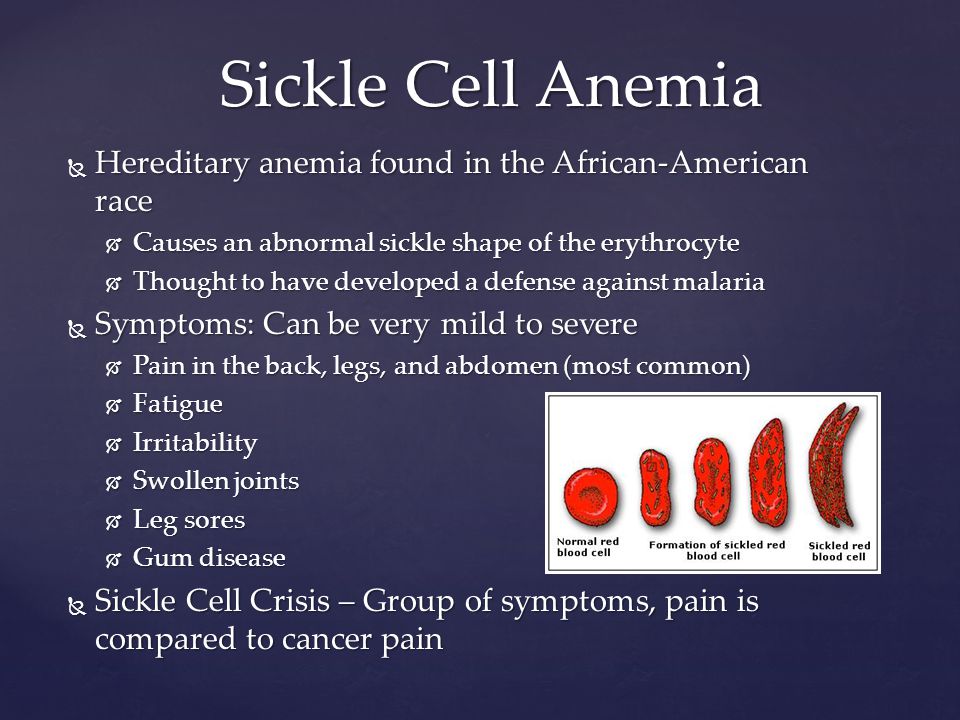 Since in most cases anemia is iron-deficient, laboratory methods for determining the level of iron and hemoglobin are most informative for making a diagnosis:
Since in most cases anemia is iron-deficient, laboratory methods for determining the level of iron and hemoglobin are most informative for making a diagnosis:
- Complete blood count. The hemoglobin content is less than 110 g/l. The color index is reduced to 0.85. The number of erythrocytes is below 3.5x1012 cells/l. There are signs of microcytosis (decrease in the diameter of erythrocytes less than 6.5 microns). In the morphological picture of erythrocytes, poikilocytosis, anisocytosis are possible.
- Study of iron metabolism. The serum iron level is less than 12 µmol/L. The total iron-binding capacity of serum (IBC) increased to 85 µmol/l or more. Reduced ferritin concentration (less than 15 mcg/l) and iron saturation of transferrin (less than 16%). Increased latent iron-binding capacity of blood (LZhSS).
To exclude B12-deficient and folate-deficient variants of anemia that occurred during pregnancy, the serum level of cyanocobalamin and folic acid is determined.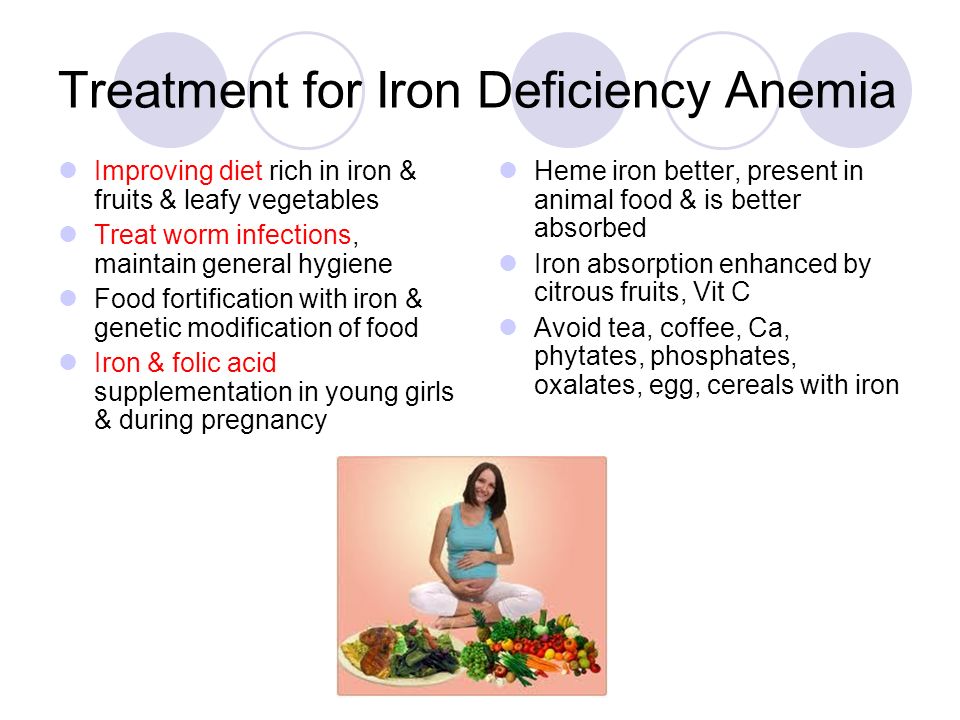 Taking into account possible complications on the part of the fetus, it is recommended to assess its condition in dynamics with fetometry, cardiotocography, and phonocardiography. Differential diagnosis is carried out between different forms of the disease, hemoglobinopathies, anemia syndrome caused by pregnancy complications, and extragenital pathology.
Taking into account possible complications on the part of the fetus, it is recommended to assess its condition in dynamics with fetometry, cardiotocography, and phonocardiography. Differential diagnosis is carried out between different forms of the disease, hemoglobinopathies, anemia syndrome caused by pregnancy complications, and extragenital pathology.
Treatment of anemia in pregnancy
The main objectives of therapy in pregnant women with reduced hemoglobin are the correction of iron deficiency, the elimination of manifestations of hypoxia, and the stabilization of hemodynamics and metabolism. In moderate and severe anemia, special attention is paid to supporting the adequate functioning of the fetoplacental complex. The treatment regimen includes drugs that allow:
- Restore hemoglobin content. In iron deficiency anemia, oral intake of optimally high doses of iron in a convenient for assimilation bivalent form is recommended. It is preferable to use depot preparations with a slow release of the element.
 Parenteral correction of anemia is carried out with intolerance to ferrous iron taken orally, impaired absorption of the gastrointestinal mucosa, exacerbated peptic ulcer of the stomach or duodenum. For more effective assimilation of the microelement, ascorbic acid is prescribed. WHO experts recommend supplementing the intake of iron-containing preparations with folic acid, which prevents the development of folic acid deficiency anemia. Cyanocobalamin deficiency is the basis for parenteral administration of vitamin B12.
Parenteral correction of anemia is carried out with intolerance to ferrous iron taken orally, impaired absorption of the gastrointestinal mucosa, exacerbated peptic ulcer of the stomach or duodenum. For more effective assimilation of the microelement, ascorbic acid is prescribed. WHO experts recommend supplementing the intake of iron-containing preparations with folic acid, which prevents the development of folic acid deficiency anemia. Cyanocobalamin deficiency is the basis for parenteral administration of vitamin B12. - Eliminate the effects of hypoxia. To ensure an adequate supply of the fetus with oxygen and nutrients, they comprehensively affect various elements of the uteroplacental blood flow system. To increase blood flow to the placenta, tocolytics are used, which relax the uterine wall. Microcirculation can be improved with the help of angioprotectors and drugs that affect blood rheology. The appointment of membrane stabilizers, antioxidants, actovegin can increase the resistance of the fetus to hypoxia.
 Antihypoxic therapy is usually used for II-III degrees of anemia, complicated by placental insufficiency. If necessary, drugs are used to correct metabolic acidosis and improve the cardiac activity of a pregnant woman.
Antihypoxic therapy is usually used for II-III degrees of anemia, complicated by placental insufficiency. If necessary, drugs are used to correct metabolic acidosis and improve the cardiac activity of a pregnant woman.
Antianemic therapy is usually long-term, allowing complete normalization of red blood counts only at 5-8 weeks of treatment. To increase the effectiveness of drugs, a dietary adjustment is required. It is recommended to supplement the diet with iron-rich foods: beef, veal, lean ham, pork, beef, chicken liver, fish. It is necessary to reduce the amount of food that impairs the absorption of iron: cereals, bran, soybeans, corn, tea, coffee, milk, carbonate, hydrocarbonate, phosphate mineral water. Almagel, tetracyclines, magnesium and calcium salts, which can aggravate anemia, are prescribed with caution.
Prognosis and prevention
Mild anemia, diagnosed in most pregnant women with low hemoglobin levels, does not pose a threat to the life of the mother and fetus. Timely correction of moderate and severe forms of the disease can significantly improve blood counts and prevent the development of complications. To prevent perinatal and maternal complications, a balanced diet, early administration of iron preparations to patients with a history of menorrhagia, a short interval between births, prolonged lactation after previous births, and multiple pregnancies are recommended. Women with anemia should be given increased attention during childbirth to quickly identify and correct possible violations of labor, postpartum hemorrhage.
Timely correction of moderate and severe forms of the disease can significantly improve blood counts and prevent the development of complications. To prevent perinatal and maternal complications, a balanced diet, early administration of iron preparations to patients with a history of menorrhagia, a short interval between births, prolonged lactation after previous births, and multiple pregnancies are recommended. Women with anemia should be given increased attention during childbirth to quickly identify and correct possible violations of labor, postpartum hemorrhage.
You can share your medical history, what helped you in the treatment of anemia during pregnancy.
Sources
- Anemia in pregnancy: textbook / Khitrov M.V., Okhapkin M.B., Ilyashenko I.N. – 2002.
- Anemia in pregnancy. Principles of modern therapy/ Korotkova N.A., Prilepskaya V.N.// Medical Council. – 2015.
- Iron deficiency in pregnant women, ways of prevention/ Yakunina N.
 A., Zaidieva Z.S.// medical advice. – 2014.
A., Zaidieva Z.S.// medical advice. – 2014. - Iron deficiency anemia during pregnancy/ Peresada O.A., Kotova G.S., Solonko I.I.// Medical news. – 2013.
- This article was prepared based on the materials of the site: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Anemia during pregnancy: consequences
10/12/2022
Anemia during pregnancy is common and to some extent this is a physiological phenomenon. Anemia is otherwise called anemia. This disease consists in a decrease in the concentration of hemoglobin and the number of red blood cells (erythrocytes) in blood . It appears in the case when the production of red blood cells is not enough, or if there is a risk, or the destruction of a significant number of them.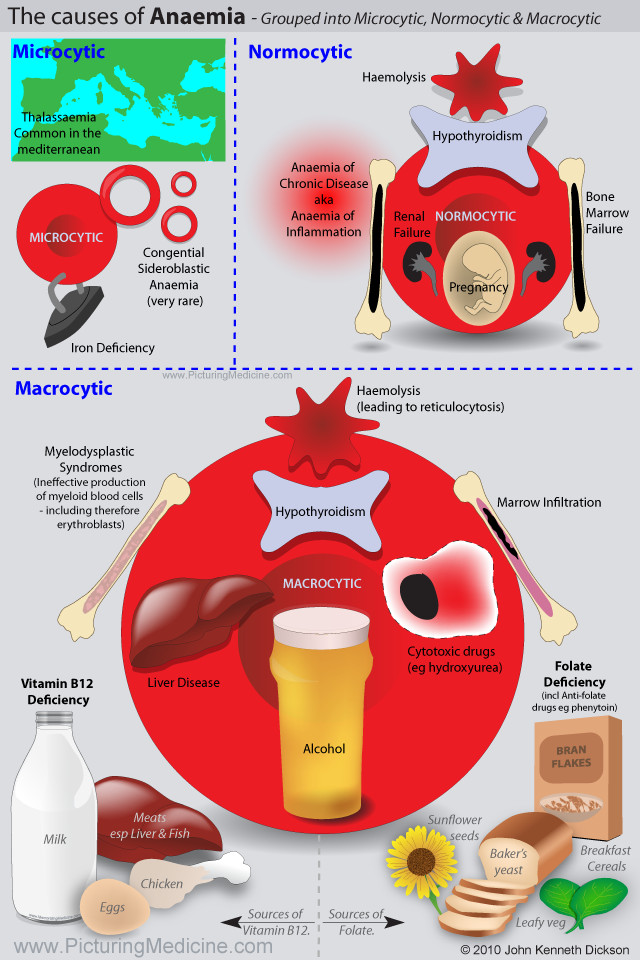 If anemia is diagnosed in women at pregnancy , then it can be dangerous for the baby?
If anemia is diagnosed in women at pregnancy , then it can be dangerous for the baby?
Anemia during pregnancy - symptoms
The main and most common symptoms of anemia:
- pallor of the skin;
- increased heart rate and respiration;
- fatigue;
- headaches and dizziness ;
- tinnitus ;
- scotoma in front of eyes ;
- muscle weakness;
- difficulty concentrating and concentrating;
- irritability;
- drowsiness;
- subfebrile temperature.
Anemia may be due to iron, folic acid or vitamin B12 deficiency.
Anemia of pregnancy - diagnosis
Anemia is a problem for many expectant mothers - it usually occurs at the beginning of the third trimester of pregnancy . During pregnancy most often occurs anemia caused by iron deficiency. This is because at this time, the need for iron in the expectant mother increases by at least 30 mg per day, and its reserves are quickly consumed.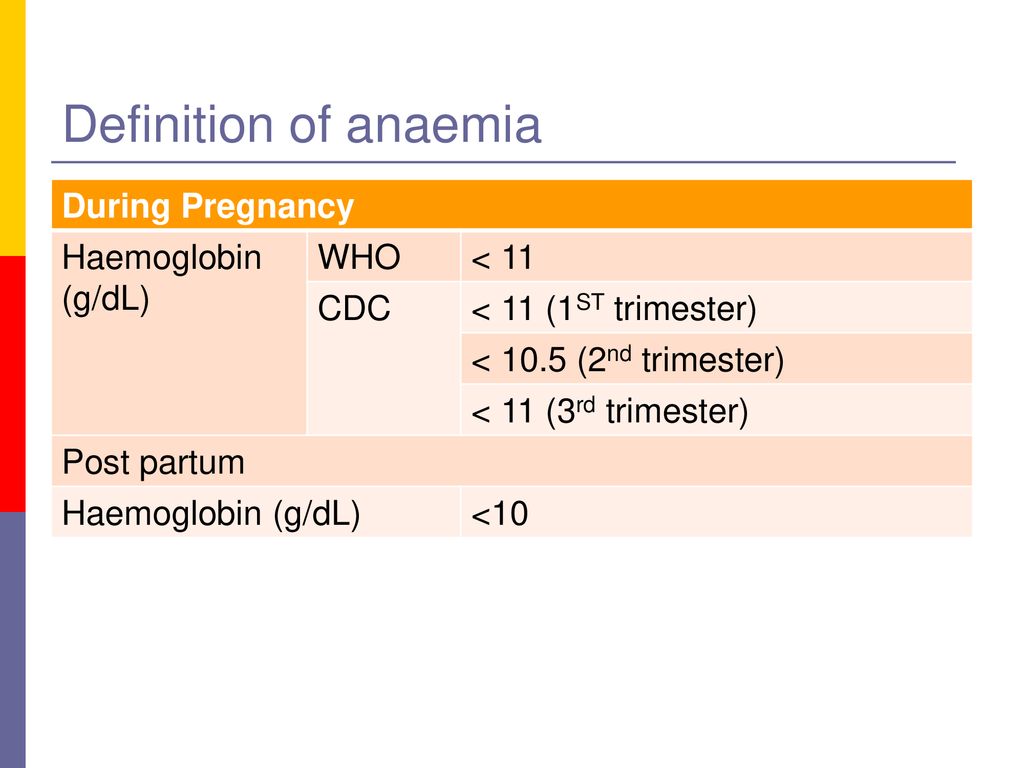 About anemia at pregnancy is usually said to occur when the hemoglobin level falls below 11 g/dL. The doctor leading the pregnancy decides whether an additional intake of iron-containing preparations is needed or it is enough to change the diet . However, it is worth knowing that thanks to the iron-rich diet, it is possible to control anemia during pregnancy .
About anemia at pregnancy is usually said to occur when the hemoglobin level falls below 11 g/dL. The doctor leading the pregnancy decides whether an additional intake of iron-containing preparations is needed or it is enough to change the diet . However, it is worth knowing that thanks to the iron-rich diet, it is possible to control anemia during pregnancy .
Other symptoms of anemia in pregnant women:
- weakness
- shortness of breath
- pale skin
- palpitations
- syncope
Anemia during pregnancy - consequences
As soon as the expectant mother notices any of the listed symptoms of anemia, you should consult a doctor as soon as possible . If anemia is not treated during pregnancy , then complications may develop, for example, premature delivery or a small child.