Anal pressure during pregnancy
Causes, in Pregnancy, Home Remedies, Treatment
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Overview
Anus pain is known as proctalgia and can have many causes. The anus is where your large intestine opens into your buttocks at the rectum. The anus is the last passageway of the gastrointestinal (GI) tract.
The anus is surrounded by muscles known as sphincter muscles. These tighten and relax the anus when you pass waste. Your tailbone (coccyx), the last bone in your spine, and many nerves are also near your anus.
Read on to learn what causes anus pain, how you can treat it at home, what medical treatments are available, and how you can help prevent this type of pain.
Anal pain can have a variety of causes.
1. Sitting for a long time
Sitting down for a long time, especially on a hard surface, can cause temporary anal pain by putting pressure on anal nerves and muscles. Even sitting for a short time on a hard surface can cause anal pain that lasts for hours after you get up.
You don’t need to see your doctor for this kind of pain.
If the pain persists for a few days after a long period of sitting, see your doctor.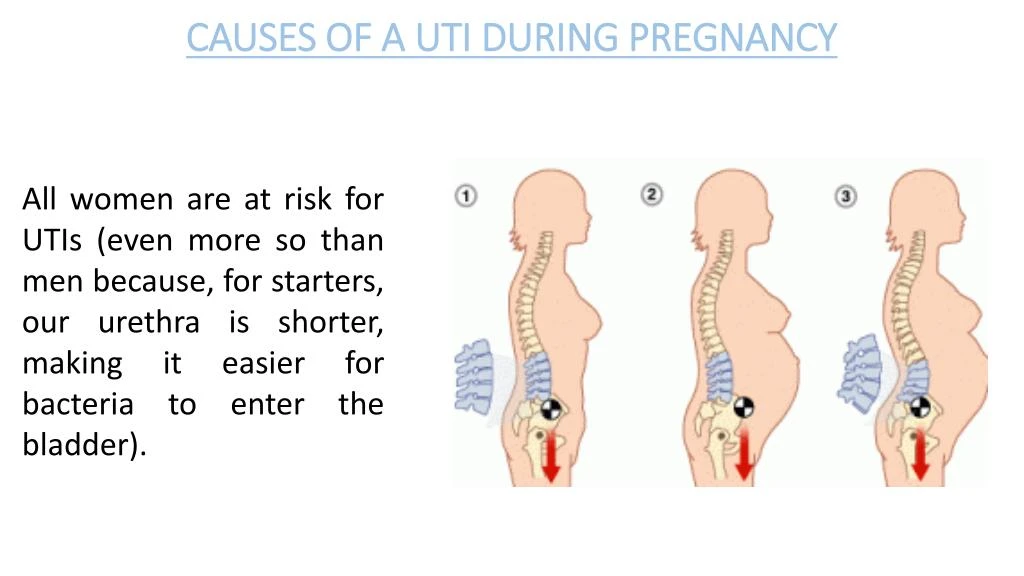 They can diagnose any injury to your anus muscles, tailbone, or the surrounding structures.
They can diagnose any injury to your anus muscles, tailbone, or the surrounding structures.
2. Diarrhea
Diarrhea happens when you pass watery, loose stool more than three times in a day. Diarrhea can have many causes, such as dietary changes (being dehydrated or not eating enough fiber), and infections like gastroenteritis, colitis, or diverticulitis.
Frequently passing stool can make your anus sore. This can get worse from wiping or cleaning. Your anal tissue can become raw and bleed, too.
Other diarrhea symptoms include:
- feeling bloated or gassy
- cramping in your lower abdomen
- feeling nauseous
- not being able to hold in your stool
Diarrhea often goes away on its own. Seek emergency medical attention if you have any of the following symptoms, though:
- diarrhea for more than two days
- fever
- blood in your stool
- black or discolored stool
- loss of consciousness
3. Injury
Falling on your butt can injure the muscles, bones, or nerves around the anus. The sudden impact of a hard surface can bruise or damage your skin, muscles, or nerve endings as well as potentially fracture bones.
The sudden impact of a hard surface can bruise or damage your skin, muscles, or nerve endings as well as potentially fracture bones.
This type of injury is most common during activities like contact sports, such as football and soccer, or activities like skateboarding, rollerblading, or gymnastics.
Depending on how severe the injury is, pain may radiate up from your anus to your lower back and feel like a constant ache or throb. You may notice bruises on your buttocks.
Seek immediate medical attention if:
- the pain is sharp and constant
- you can’t walk or get up without severe pain
- you lose sensation in your lower back or in one or both legs
4. Fissures
Anal fissures happen when your anal tissues tear. Passing especially hard or large stool is the most common culprit. The pain is often sudden and sharp at first. Your anus may ache for hours or days afterward until the fissure heals.
Symptoms of an anal fissure include:
- feeling sudden, unusual pain in or around your anus when you pass stool
- bleeding from your anus, especially when you wipe
- pain that lasts for hours after you pass stool
Fissures don’t always require immediate medical treatment.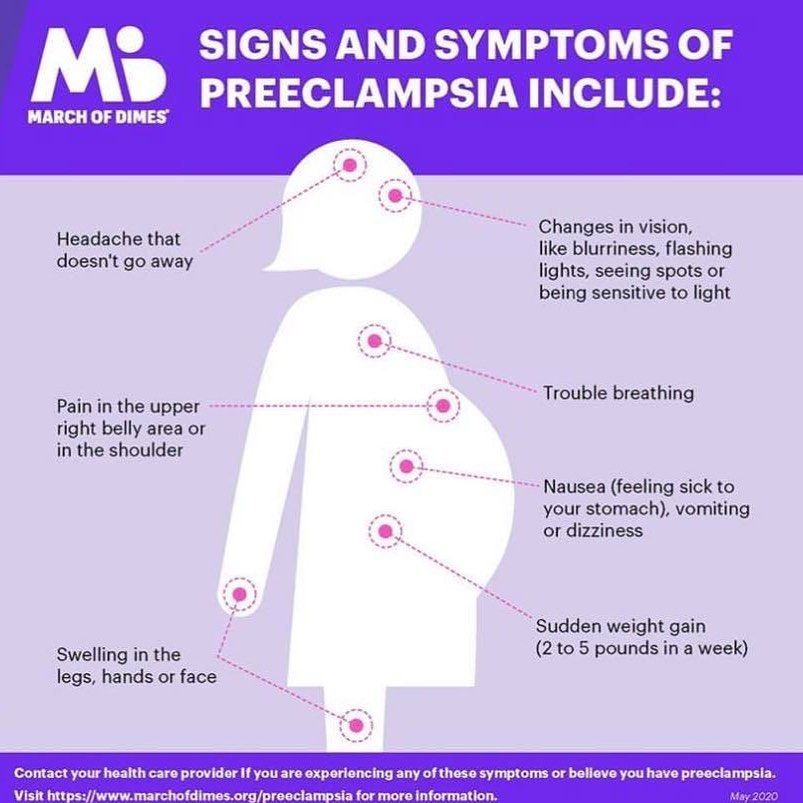 See your doctor if the pain persists or gets significantly worse when you sit down, pass stool, or walk.
See your doctor if the pain persists or gets significantly worse when you sit down, pass stool, or walk.
5. Hemorrhoids
Hemorrhoids happen when anal blood vessels are swollen. Straining to pass stool or being constipated are often the causes of hemorrhoids.
When you have a hemorrhoid, you may feel a lump near your anus. The pain may be generally dull but sharp when you sit down. You may not feel comfortable sitting without a special cushion or pillow. In some cases, you may not notice any symptoms.
Common symptoms of hemorrhoids include:
- constant pain, soreness, or itching around your anus
- bleeding from your anus when you pass stool
- sharp anal pain if blood in the hemorrhoid becomes clotted
Hemorrhoids can go away on their own, but severe hemorrhoids may require medical treatment. See your doctor right away if you:
- have trouble passing stool
- can’t sit without sharp or severe pain
- notice blood in your stool
6.
 Menstruation
MenstruationMenstruation can cause anal pain along with other symptoms related to your digestive tract.
Your rectum and anus may be more sensitive during this time. This can make your anus feel tender, sore, or uncomfortable. Common period symptoms, such as diarrhea and bloating, can make anal pain even more pronounced.
You don’t need to see your doctor to treat these symptoms. They usually go away once your period is over.
7. Anal spasms (proctalgia fugax)
Anal spasms happen when you get sharp, unexpected anal pain due to anal sphincter muscle contractions. It’s relatively common. A 2013 review estimates it affects between 8 and 18 percent of people.
The cause of this condition isn’t well known. It’s more likely to occur if you have irritable bowel syndrome (IBS) or anxiety as well as after hemorrhoid surgery or a hysterectomy.
When you’re pregnant, your uterus becomes enlarged, which puts pressure on your anus. That can lead to discomfort or pain. This extra pressure can also cause hemorrhoids, which can make your anus uncomfortable.
This extra pressure can also cause hemorrhoids, which can make your anus uncomfortable.
Anal pain during pregnancy is most common during the third trimester, when your baby is larger and may put more pressure on your anal nerves. Contractions during labor can also cause pain in your anus.
In many cases, you should be able to treat anal pain at home. Here are some home remedies to try:
- Take a sitz bath. Buy a sitz bath at your local drugstore or online and mount it in your toilet bowl. Fill it with warm water and Epsom salt, then sit on top of the sitz bath with the water immersing your anus. Soak for 15 to 20 minutes.
- Use over-the-counter (OTC) creams or ointments. Apply a small amount of cream or ointment, such as lidocaine or cortisone, to reduce pain and speed up the healing process of irritated skin.
- Use a cold compress. You can make your own cold compress at home by wrapping an ice pack or bag of frozen vegetables in a towel.
 Press it against your anal area to help relieve pain. Do this 20 minutes at a time, three to four times daily.
Press it against your anal area to help relieve pain. Do this 20 minutes at a time, three to four times daily. - Take OTC pain medicine for pain relief. Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) can temporarily relieve anal pain until any cuts or injuries heal.
Seek emergency medical treatment if:
- Your anal pain makes you unable to walk, pass waste, stand, or sit.
- You notice blood in your stool.
- You have a fever.
- You’re severely dehydrated.
- You can’t eat or pass stool.
Medical treatment depends on the cause of pain and the severity of your symptoms.
Treatment for injuries
You may need X-rays or other imaging tests to see the extent of any damage to your tailbone or spine. Severe spinal injuries may require surgery or long-term rehabilitation to restore any lost mobility.
Treatment for diarrhea
If you’re severely dehydrated, you may need intravenous fluids (IV) to replenish your body fluids.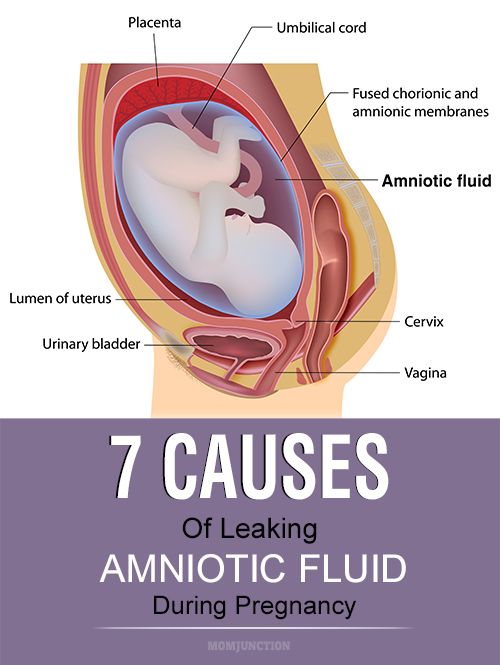 If a bowel disorder is causing diarrhea, such as IBS or Crohn’s disease, your doctor may prescribe you medication or a treatment plan to help reduce symptoms.
If a bowel disorder is causing diarrhea, such as IBS or Crohn’s disease, your doctor may prescribe you medication or a treatment plan to help reduce symptoms.
Treatment for a fissures
Chronic anal fissures may require surgery so that you can pass stool without injuring your sphincter muscles. Your doctor may also recommend adding fiber to your diet to help you pass stool more easily.
Treatment for hemorrhoids
Your doctor may wrap the hemorrhoid with a rubber band until it shrinks. Surgery to cut or freeze the hemorrhoid are also possible treatment options. In severe cases, your doctor may need to remove the hemorrhoid tissues and blood vessels in a hemorrhoidectomy procedure.
It may not always be possible to prevent anal pain. But there are things you can do to reduce your risk:
- Stay hydrated. Drink at least 64 ounces of water per day to make your stool easier to pass.
- Sit with good posture.
 When sitting,straighten your back and keep your knees bent at a 90-degree angle.
When sitting,straighten your back and keep your knees bent at a 90-degree angle. - Get up and walk around at least once every 30 to 50 minutes. This reduces long-term pressure on muscles and nerves in your anus and lower spine.
- Don’t strain when you pass stool. Straining can cause discomfort, hemorrhoids, and anal fissures.
- Eat a healthy diet. Eat plenty of fiber so that you regularly pass stool and prevent constipation.
- Wear loose, breathable underwear. Wear 100 percent cotton underwear to prevent your anus from becoming moist with sweat, which could lead to irritation.
- Consider using moist wipes or jets of water instead of toilet paper. Toilet paper can scratch and cut your anal skin, making you more prone to infections. Moist wipes and bidets are gentler on your skin.
- Don’t eat raw, uncooked, or untrustworthy food.
 Food and unfiltered water can contain bacteria or other microbes that can lead to diarrhea. Make sure your food is properly cooked and that your water is clean.
Food and unfiltered water can contain bacteria or other microbes that can lead to diarrhea. Make sure your food is properly cooked and that your water is clean.
Many things can lead to anal pain, some serious and others not.
If the pain is bearable and starts to fade quickly after it starts, there’s no need for concern. If pain persists for more than a few days and accompanies other painful or disruptive symptoms, see your doctor for immediate treatment.
Butt Pain During Pregnancy: How to Cope
Butt Pain During Pregnancy: How to Cope- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
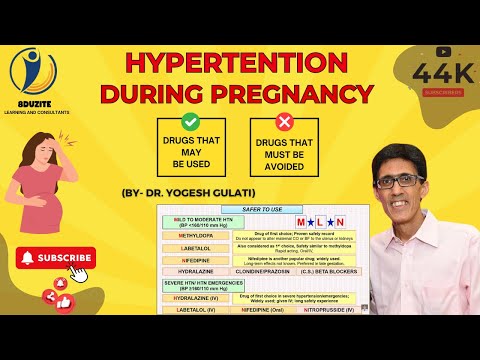
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Janine Kelbach, RNC-OB — By Rachel Nall, MSN, CRNA on November 6, 2018
We include products we think are useful for our readers.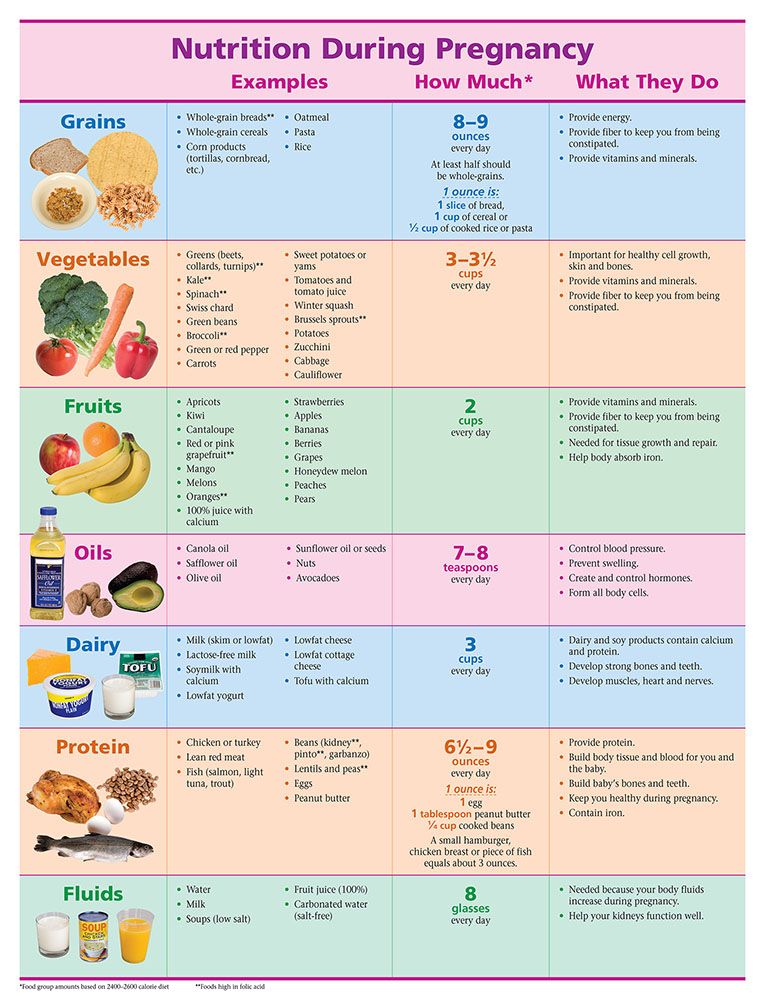 If you buy through links on this page, we may earn a small commission. Here’s our process.
If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Overview
If you’re pregnant, you probably expected to experience some back pain and abdominal discomfort. But what you didn’t count on was butt pain.
As your pregnancy progresses, there are common conditions like sciatica that can cause you a great deal of discomfort. You might feel pain in the buttocks area as a result.
Luckily, as you continue to wait for your little one to enter the world, there are several steps you can take to reduce butt pain.
Here’s how to make the next few months more comfortable before your baby makes their arrival.
Causes of butt pain during pregnancy
Butt pain during pregnancy can be pain caused by an abnormality on the buttocks itself (like hemorrhoids). It can also be referred pain that radiates from the lower back to the buttocks.
Some common causes of butt pain during pregnancy include the following.
Hemorrhoids
Hemorrhoids are enlarged, swollen veins in the anus or rectum. Pregnant women are more likely to experience hemorrhoids because the uterus creates extra pressure on the anus and rectum.
If you have to stand for long periods of time because of your job or hobbies, the pain may get worse.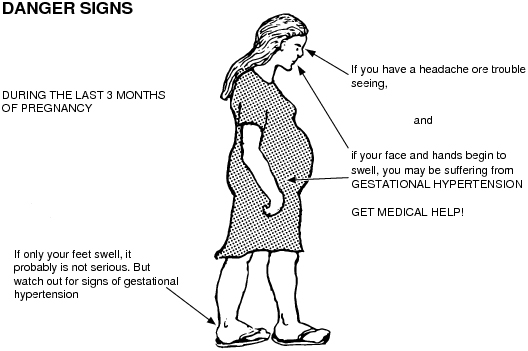
Labor pains/Contractions
Women experience contractions differently. Some have abdominal cramping and back cramping that can extend to the buttocks. The nature of the pain can vary, too. Some people feel a cramping sensation while others may feel pressure, throbbing, or shooting pain.
Braxton-Hicks contractions may cause discomfort, but they aren’t usually painful. If the contractions are causing your buttocks pain, call your doctor.
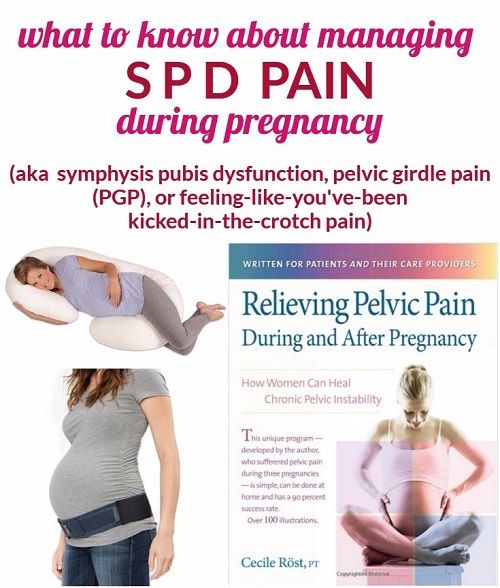
Pelvic girdle pain
Pelvic girdle pain affects 1 in 5 pregnant woman. This pain occurs when the extra weight of the baby and pregnancy-related movements in the pelvis start to add up and cause pelvic pain.
Many women also experience this pain in their buttocks. Other symptoms can include feeling a grinding or clicking in the pelvic area, and pain that gets worse with movement.
Although pelvic girdle pain is very uncomfortable, it isn’t harmful to your baby. It won’t keep you from having a vaginal birth.
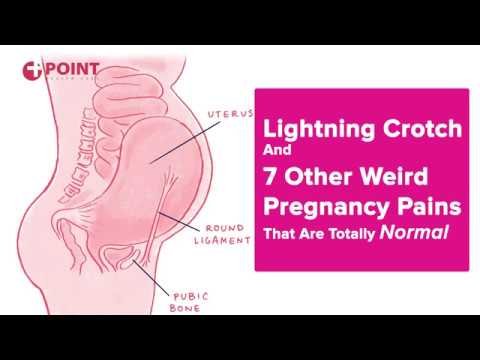
Sciatica
Sciatica is a condition that happens when there’s pressure on the sciatic nerve that runs from the buttocks down the leg. Pregnancy can cause the nerve to become irritated or inflamed. Your expanding uterus can place extra pressure on the sciatic nerve.
Pregnancy can cause the nerve to become irritated or inflamed. Your expanding uterus can place extra pressure on the sciatic nerve.
As you reach your third trimester, your baby’s change in positioning can rest on the nerve directly in your buttocks area. This can cause butt pain.
You also might feel a burning sensation in your back, buttocks, and leg. Some women also report shooting pain that extends down the leg.
When to call your doctor
Whatever the cause, butt pain can make it difficult to complete your daily activities comfortably. (As if it wasn’t hard enough already with your pregnancy!)
If you experience the following symptoms, it’s time to call your doctor:
- the pain is so severe that it is making you feel ill
- you are experiencing a significant amount of blood loss (bigger than typical hemorrhoids, which may cause only a smear of blood)
- you have experienced a rush of fluid from your vagina or your “water breaking”
- you lose control of your bladder/bowels
- the pain never subsides
Medical treatments
An estimated 14 percent of pregnant women take an opioid pain medication while they’re pregnant. Examples of these prescription medications include oxycodone and hydrocodone.
Examples of these prescription medications include oxycodone and hydrocodone.
Typically, women take them for a week or less. Back pain’s the most common reason doctors prescribe these medications.
If your buttocks pain does not respond to over-the-counter and at-home treatments, your doctor may consider prescribing a pain medicine.
But the fewer medications you can take during pregnancy, the better. This will reduce the likelihood the medications could affect your baby’s growth and/or development.
At-home treatments
If your pain is the result of hemorrhoids, you can try the following at-home treatments to reduce discomfort:
- Soak in a warm water bath or a sitz bath. A sitz bath is a plastic bath that can fit over your toilet. You can fill it with warm water, sit, and soak without having to draw a bath. Shop for sitz baths.
- Try witch hazel. Place a few drops of witch hazel on a sanitary pad that you can wear to reduce inflammation.
 You can change the witch hazel pads throughout the day to reduce inflammation. Also try freezing them for more relief. Shop for witch hazel.
You can change the witch hazel pads throughout the day to reduce inflammation. Also try freezing them for more relief. Shop for witch hazel. - Don’t sit or stand too long. Refrain from sitting or standing for extended time periods. This puts extra pressure on your anus. Lying on your side can reduce pressure.
- Drink up. Drink plenty of fluids each day. This can help reduce your risk for constipation, which makes your stool harder to pass.
- Eat fiber. Eat a diet that has plenty of fiber with whole-grain foods, fruits, and vegetables.
You can also ask your doctor if there are creams and/or stool softeners you could take to reduce hemorrhoid-related pain and strain.
Shop for stool softeners.
Sciatica treatments
For pain related to sciatica and/or pelvic pain, you can take the following steps:
- Take an over-the-counter pain reliever like acetaminophen to reduce discomfort.
- Take a warm bath and/or shower to soothe tight muscles.
- Wear a supportive pelvic belt (also called a girdle) to reduce the pressure on your lower back and pelvis. Shop for pelvic belts.
- Avoid performing activities that aggravate your pain, like lifting heavy objects, standing on only one leg at a time, and keeping your legs together when you turn in bed and/or get out of the car.
- Place a pillow under your belly and one between your legs when you sleep. This can help promote proper body positioning.
You can also ask your doctor if you can apply cold and/or heat packs to painful areas.
The takeaway
Pregnancy-related butt pain will typically resolve after you deliver. But some women may continue to experience hemorrhoids post-delivery. You can ask your doctor if there are other treatments you can use to reduce the frequency of butt pain.
Share on Pinterest
Last medically reviewed on November 7, 2018
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.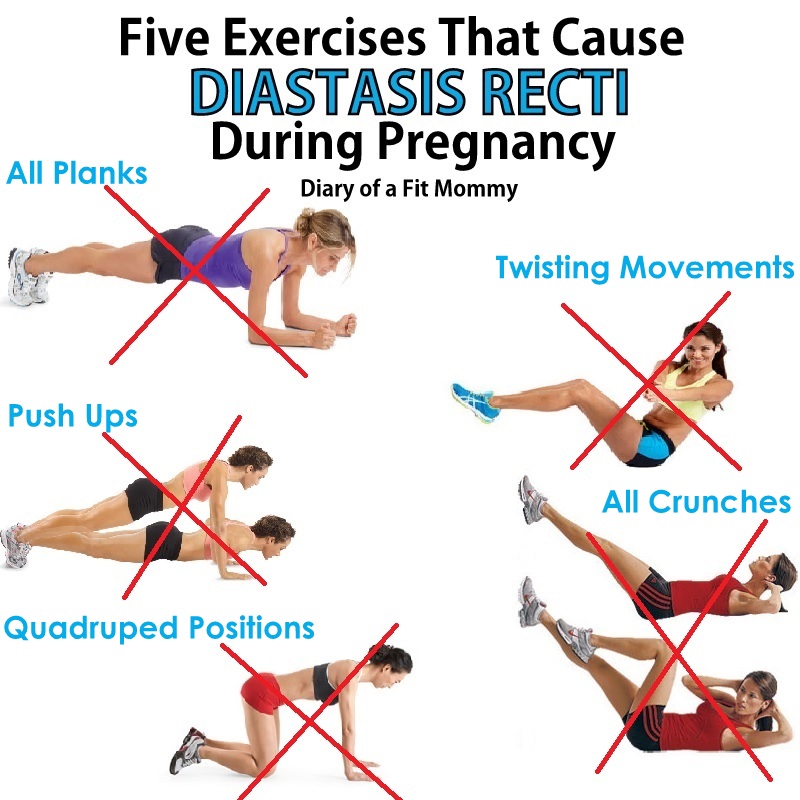 We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Giannoudis, P. V., Kanakaris, N. K., & Roberts, C. S. (2011, February 15)
ncbi.nlm.nih.gov/pmc/articles/PMC3050758/ - Hemorrhoids. (2009, August)
marchofdimes.org/pregnancy/hemorrhoids.aspx - How do you treat pregnancy hemorrhoids and constipation. (2013, January)
kidshealth.org/parent/pregnancy_center/q_a/piles.html - How to handle sciatica during your pregnancy. (2014, December 17)
health.clevelandclinic.org/2014/12/how-to-handle-sciatica-during-your-pregnancy/ - More than 14 percent of pregnant women prescribed opioids, study says. (2014, February 12)
asahq.org/about-asa/newsroom/news-releases/2014/02/opioids-in-pregnancy - Pelvic girdle pain and pregnancy. (2015)
rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy. pdf
pdf - Types of back pain in pregnancy. (2009, December 3)
spine-health.com/conditions/pregnancy-and-back-pain/types-back-pain-pregnancy - What can I do to treat hemorrhoids during pregnancy? (2014, November 11)
mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/hemorrhoids-during-pregnancy/faq-20058149
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Nov 7, 2018
Written By
Rachel Nall, MSN, CRNA
Edited By
Frank Crooks
Medically Reviewed By
Janine Kelbach, RNC-OB
Share this article
Medically reviewed by Janine Kelbach, RNC-OB — By Rachel Nall, MSN, CRNA on November 6, 2018
related stories
How to Identify Lightning Crotch Pain During Pregnancy
How to Manage Back Spasms During Pregnancy
First Trimester Pregnancy Back Pain: Causes and Treatments
Sciatica During Pregnancy: Symptoms, Causes, Treatments
13 Home Remedies for Swollen Feet During Pregnancy
Read this next
How to Identify Lightning Crotch Pain During Pregnancy
Medically reviewed by Deborah Weatherspoon, Ph.
 D., MSN
D., MSNIn your third trimester and having some shooting pain “down there”? In general, lightning crotch pain is a normal part of pregnancy and nothing to get…
READ MORE
How to Manage Back Spasms During Pregnancy
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
One of the most common complaints during pregnancy is back pain and, specifically, back spasms. Learn why this happens and how you can treat it.
READ MORE
First Trimester Pregnancy Back Pain: Causes and Treatments
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
Back pain during the first trimester might be one of the first pregnancy symptoms you experience. Here’s what’s causing it and how to treat it safely.
READ MORE
Sciatica During Pregnancy: Symptoms, Causes, Treatments
Medically reviewed by Beth Holloway, RN, MEd
Many pregnant women experience sciatic pain.
 Here's a look at the causes, symptoms, and ways to find relief.
Here's a look at the causes, symptoms, and ways to find relief. READ MORE
13 Home Remedies for Swollen Feet During Pregnancy
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
Swollen feet during pregnancy is very common, but that doesn't mean you have to be uncomfortable. We'll cover some effective ways to deal with the…
READ MORE
Causes of Hemorrhoids and Tips for Prevention
Medically reviewed by Lauren Castiello, MS, AGNP-C
Hemorrhoids, also known as piles, are swollen veins located around the anus or in the lower rectum.
READ MORE
The Best Pregnancy Apps of 2020
These are the best iPhone and Android apps to find information, answers, tools, and tracking during your pregnancy. From scheduling doctor’s visits…
READ MORE
14 Recipes to Ease Morning Sickness
Medically reviewed by Natalie Butler, R.
 D., L.D.
D., L.D.Morning sickness got you down? Get over your nausea with one of these 14 delicious, easy recipes.
READ MORE
Hemorrhoid Surgery Types: Outpatient and Inpatient
Medically reviewed by Saurabh Sethi, M.D., MPH
Hemorrhoids are swollen veins that appear near the rectum. If you have a severe case that doesn't resolve with home treatment, there are a number of…
READ MORE
7 Books That Shine a Light on Pregnancy
For everything from what to eat during pregnancy to how to plan for birth and what comes after, check out these best pregnancy books!
READ MORE
Signs, symptoms and causes of hemorrhoids in pregnant women - NEARMEDIC network of clinics
The main causes of hemorrhoids in pregnant women can be as follows:
- Chronic constipation.
 In this case, the stretching and tension of the walls of the rectum increases during defecation, which leads to the formation of hemorrhoids. In pregnant women, constipation occurs much more often due to a decrease in intestinal tone.
In this case, the stretching and tension of the walls of the rectum increases during defecation, which leads to the formation of hemorrhoids. In pregnant women, constipation occurs much more often due to a decrease in intestinal tone. - Inactive lifestyle. With hypodynamia, blood stagnation occurs in the venous plexus of the rectum, which eventually leads to vein thrombosis and the formation of hemorrhoids. Features of the condition do not always allow pregnant women to be mobile, therefore they have a high risk of developing this disease. nine0006
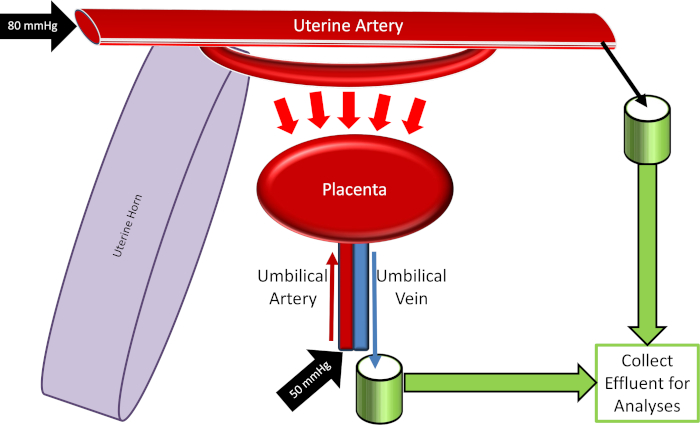
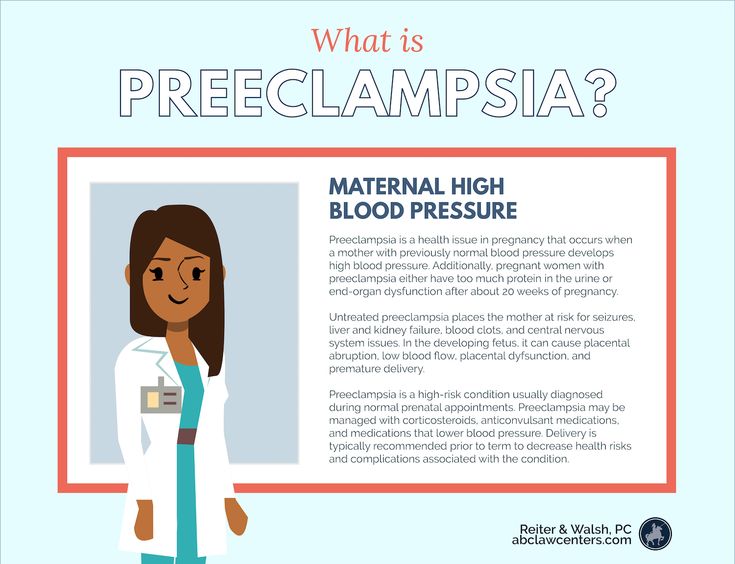
- Disturbance of blood circulation in the lower half of the body. During pregnancy, the uterus grows and compresses the inferior vena cava. This leads to stagnation of blood in the veins of the legs and rectum. During childbirth, a woman's intra-abdominal pressure rises greatly - this can cause hemorrhoids after pregnancy.
Signs of hemorrhoids in pregnant women
The longer the period, the higher the likelihood of developing the disease. Most often, hemorrhoids appear in the 3rd trimester or after childbirth. nine0003
Most often, hemorrhoids appear in the 3rd trimester or after childbirth. nine0003
The blood vessels of the hemorrhoidal plexus of the rectum gradually dilate. Over longer periods, the stretching of the veins becomes even stronger. With the expansion of the walls of the veins of the rectum, they lose their elasticity. This provokes protrusion of the veins under the mucous membrane.
If hemorrhoids protrude only into the lumen of the rectum and do not come out of the anus, then we are talking about the treatment of hemorrhoids of the 1st stage. The farther, the larger the knots become and the more they sag from the anus. In the second stage of hemorrhoids, the nodes sag from the anus, but are easily set back on their own. The third stage occurs when the nodes can no longer cope back. nine0003
The symptoms of the disease depend on its stage.
- Internal hemorrhoids. Symptoms are mild, there is no sagging of hemorrhoids from the anus. At this stage, women may experience pain during bowel movements, slight bleeding or fresh blood in the stool, and itching and discomfort in the anus.
- External hemorrhoids. The main symptom is the sagging of one or more purple-red nodes from the anus. This manifestation is the main sign of what is required, and not of another disease, such as anal fissure. Walking, sitting and defecation in this case become extremely painful. nine0006
Urgent medical attention is required in case of infringement of the hemorrhoid - a pregnant woman experiences very severe pain in the anus with fever.
Treatment of hemorrhoids during pregnancy
If a woman already has any symptoms of hemorrhoids - itching, pain in the anus, bleeding from the anus, etc. - professional treatment is required.
At NEARMEDIC, the first stage of treatment is the preventive measures described above, which stop the progression of the disease. Then the woman is prescribed drugs, both local and systemic. But due to pregnancy, local therapy is preferable, as this reduces the risk of side effects, increases the effectiveness of treatment and reduces the negative effects of drugs on the child.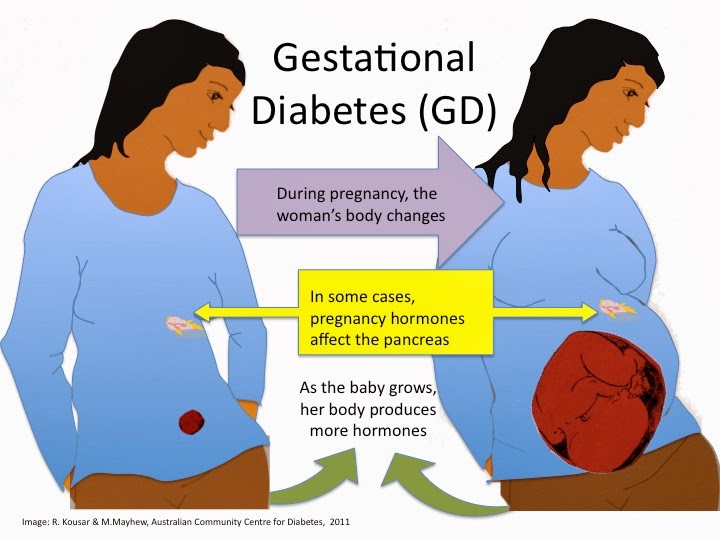 In any case, the medicine is prescribed only by the attending physician who observes the woman during pregnancy. nine0003
In any case, the medicine is prescribed only by the attending physician who observes the woman during pregnancy. nine0003
In the case when a woman already has prolapsed nodes that cannot be set, an operation is prescribed. Other indications for surgical intervention are infringement or necrosis of the hemorrhoid, as well as acute inflammation. Most often, in NEARMEDIC surgery is postponed until the postpartum period, and during pregnancy they are limited to conservative treatment.
Prevention of hemorrhoids during pregnancy
Due to the fact that all pregnant women are at high risk of developing hemorrhoids, NEARMEDIC clinic doctors strongly recommend that preventive measures be taken throughout pregnancy, without waiting for symptoms to appear. nine0003
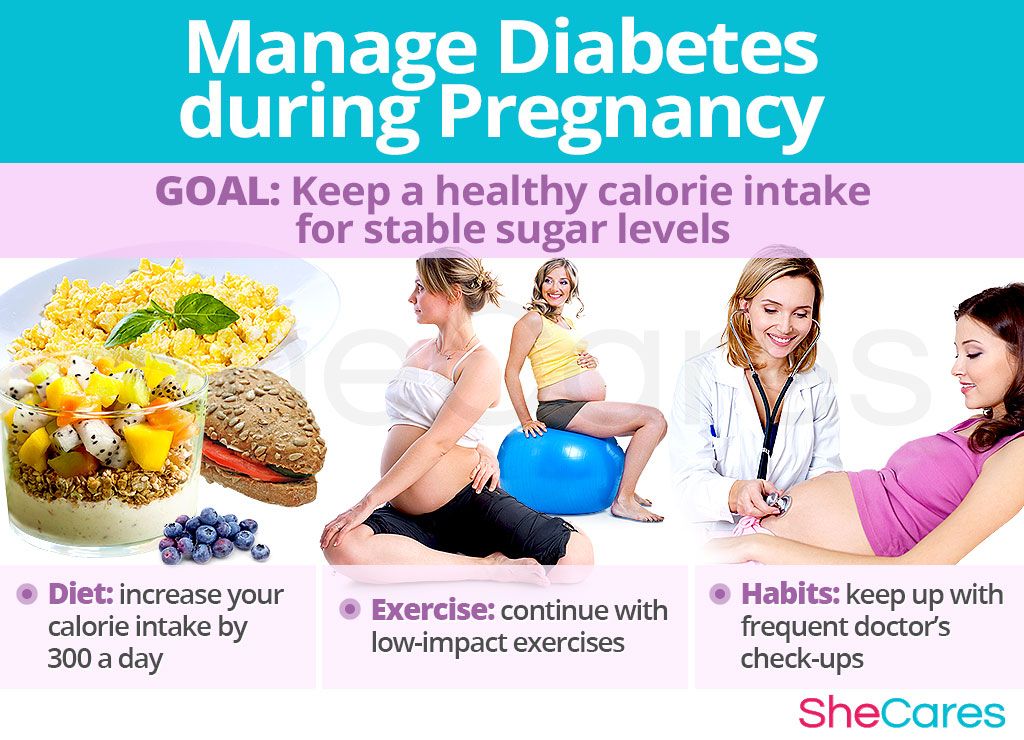
- Relief of constipation. To do this, you need to adjust your diet: eat more foods that contain coarse vegetable fiber - vegetables, fruits, cereals, cereals, prunes. Dairy products also have a beneficial effect on digestion.
 On the contrary, it is better to refuse meat and other foods rich in protein. As well as from an excess of fat, coffee and hot spices.
On the contrary, it is better to refuse meat and other foods rich in protein. As well as from an excess of fat, coffee and hot spices. - Hygiene. It is recommended to wash the perineum and anus after each act of defecation. In addition, once a day you can take sitz baths with antiseptics: chamomile infusion, a weak solution of potassium permanganate, etc. nine0006
Doctors
Who treat hemorrhoids during pregnancy
More doctorsClinics in Moscow
For all questions, you can contact the single contact center: +7 (495) 6-171-171
Hemorrhoids during pregnancy - symptoms, diagnosis, treatment methods
Contents
1. Introduction 2. Diagnostics 2.1. Diagnosis of anal fissure 2.2. Digital rectal examination 2.3. Instrumental diagnostics 2.4. Laboratory diagnostics 3. Features of the treatment of hemorrhoids in pregnant women 3.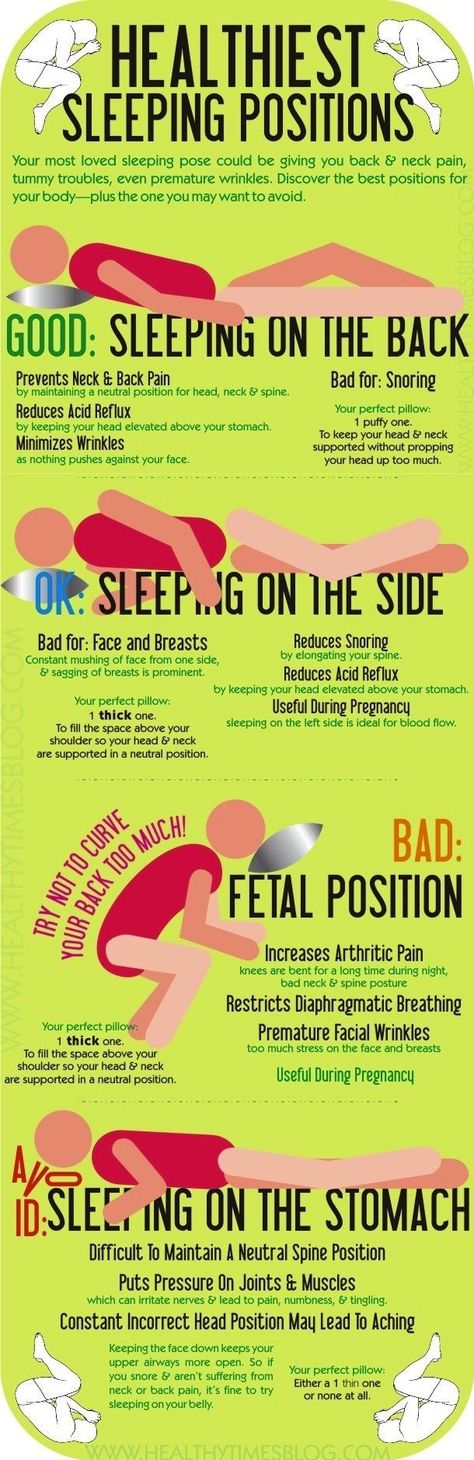 1. Lifestyle change 3.2. Medical therapy 3.3. Surgical intervention 4. Complications 5. Prevention 5.1. Nutrition and drinking regimen 5.2. Personal hygiene 5.3. Physical activity nine0003
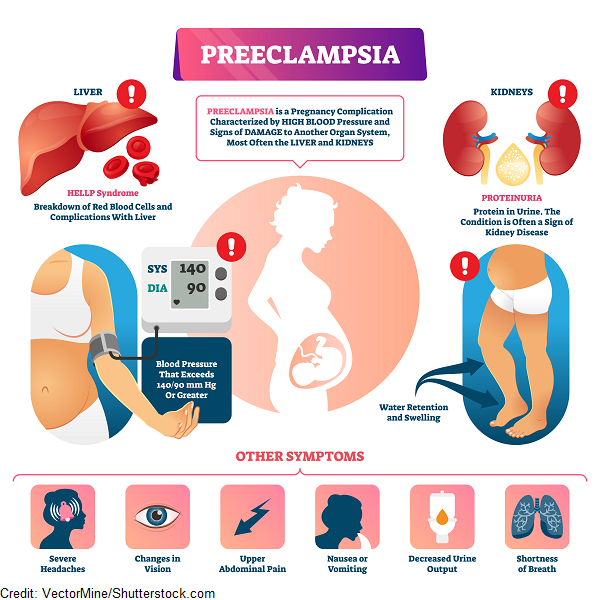
1. Lifestyle change 3.2. Medical therapy 3.3. Surgical intervention 4. Complications 5. Prevention 5.1. Nutrition and drinking regimen 5.2. Personal hygiene 5.3. Physical activity nine0003 According to statistics, hemorrhoids during pregnancy occur in 40% of cases. Most often in the II - III trimesters.
In the initial stages, the disease does not pose a danger to either the patient or the fetus. But it negatively affects the psycho-emotional state of the pregnant woman and causes a lot of discomfort.
The problem is complicated by limitations in the patient's treatment methods - not all drugs and procedures can be used during gestation and lactation without a threat to the child. nine0003
If hemorrhoids occur during pregnancy and do not progress, then after childbirth, the nodes, most often, retract on their own.
Causes
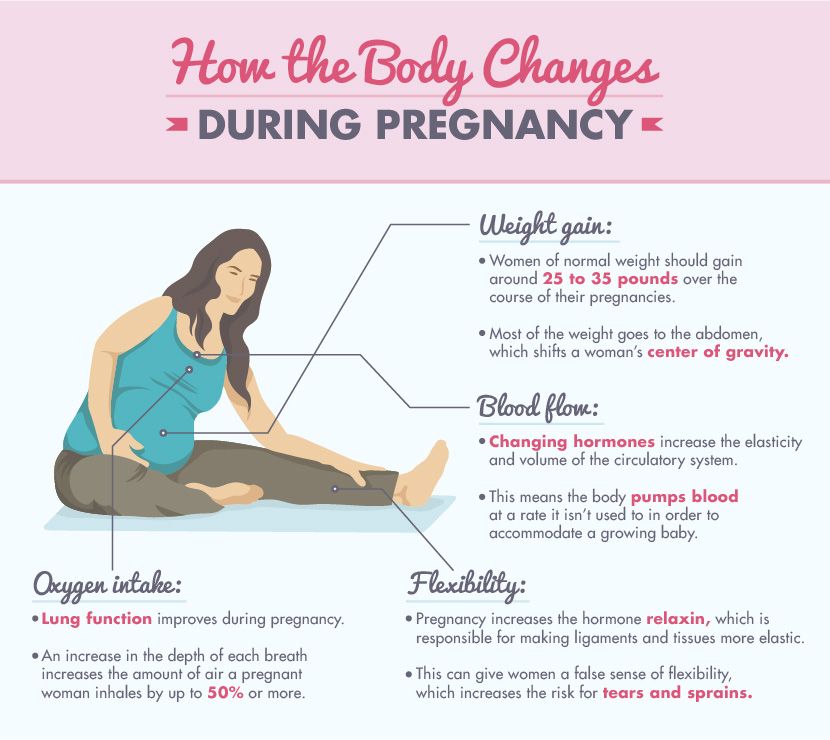
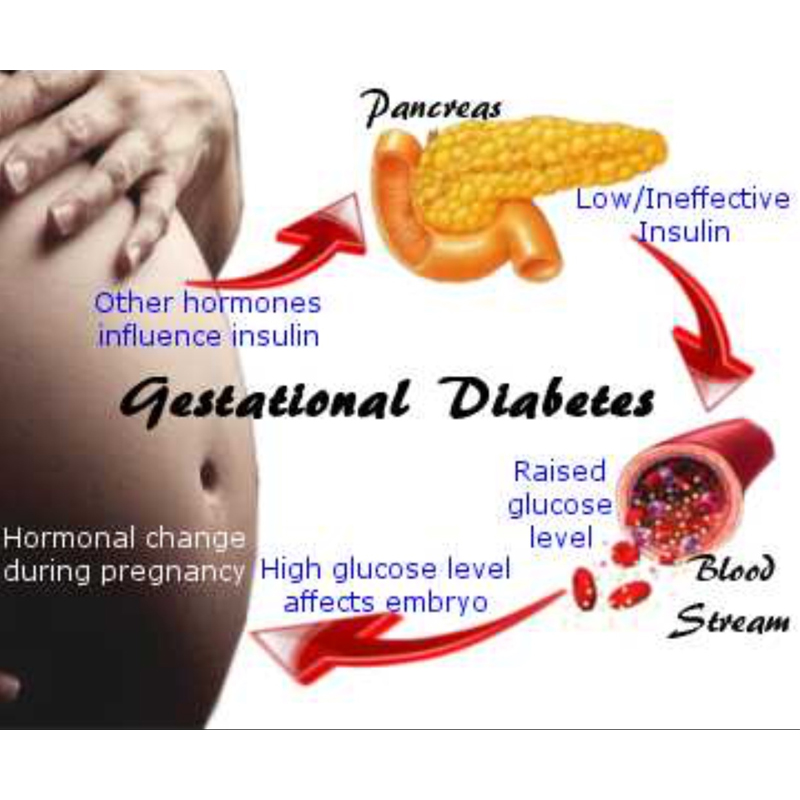
The main reason for the development of hemorrhoids during gestation is physiological changes in the functioning of the whole organism.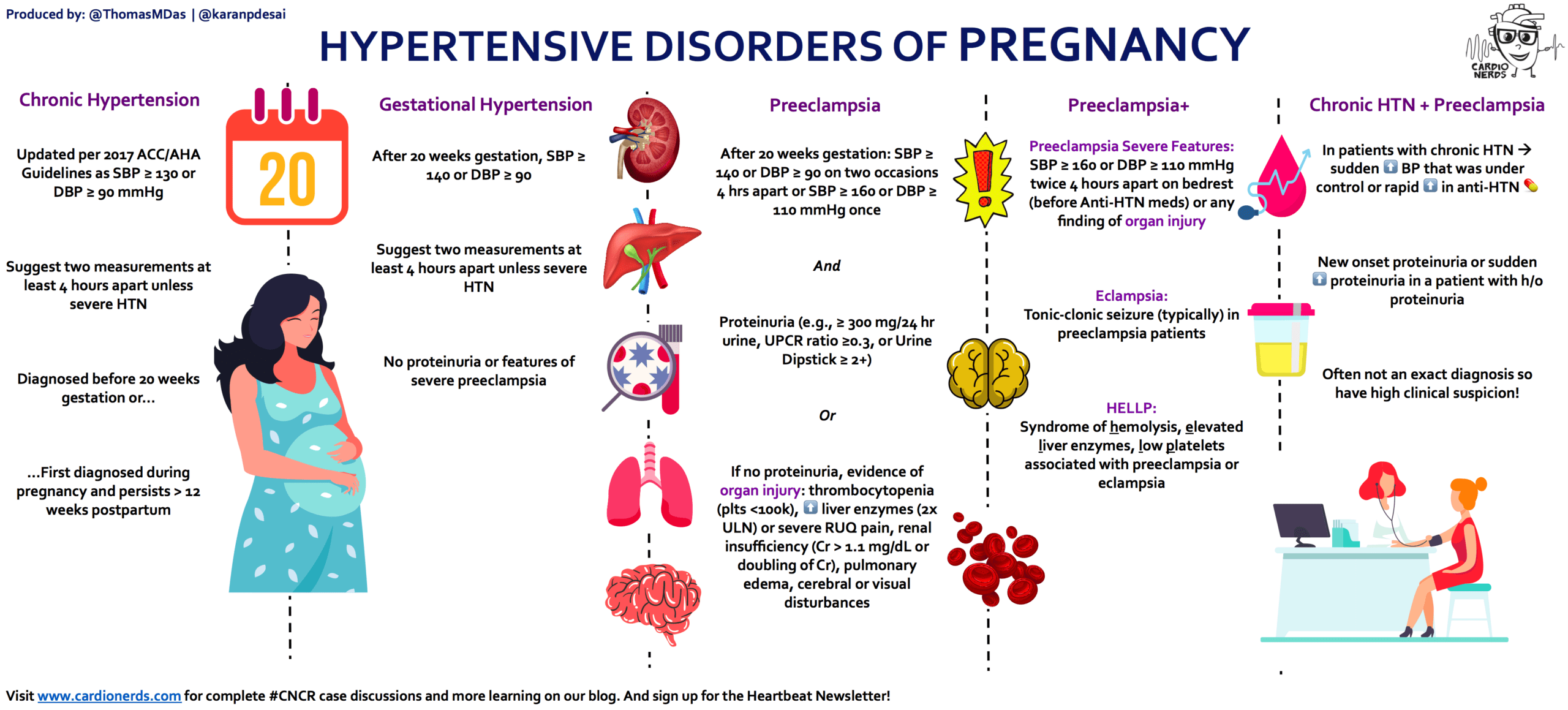
During this period, both chronic pathologies can become aggravated, and new ones can appear. The development of nodes during pregnancy is facilitated by: nine0003
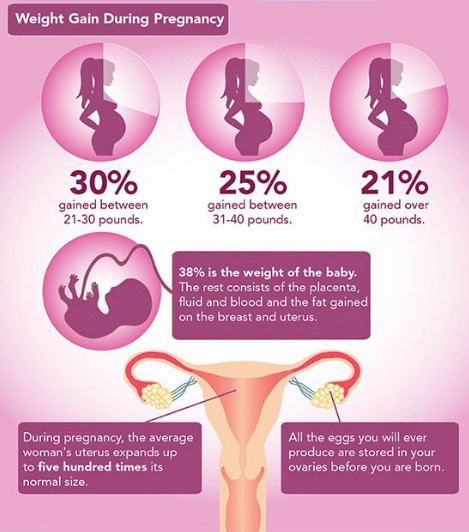
- Lifestyle. Some women begin to neglect physical exercises or, due to poor health, severely limit themselves in them. Against the background of physical inactivity and actively produced progesterone, intestinal motility worsens. With improper nutrition and fluid deficiency, an increase in progesterone synthesis leads to constipation. An enlarged uterus puts extra pressure on the rectum. When straining during bowel movements, intra-abdominal pressure rises even more, which causes overflow of blood into the cavernous sinuses of the rectum. nine0006
- Stagnation. An enlarged uterus leads to compression of the inferior vena cava. Blood circulation in the pelvic organs and the digestive system worsens. This provokes a poor outflow of blood from the lower extremities and the formation of congestion.
 Due to the increased pressure on the walls of the vessels, they do not withstand and are deformed.
Due to the increased pressure on the walls of the vessels, they do not withstand and are deformed. - Childbirth. When pushing, the body is put under enormous stress. Especially strongly the pressure rises in the intra-abdominal space. When the child's head descends into the small pelvis, the rectal vein is compressed. During this period, hemorrhoids may be displaced and ruptured, which leads to additional hemorrhage. nine0006
- Effect of progesterone on the body. Under the influence of the hormone, loosening of the connective tissue and a decrease in the tone of smooth muscle fibers occur. As a result, blood is deposited in the hemorrhoidal plexuses and typical cavernous bodies are formed.
- Improper nutrition and non-compliance with the drinking regimen. Deficiencies of fiber and fluid lead to compaction of feces, which increases the need for straining during the act of defecation. Overeating and plentiful rare meals are also considered harmful. In such a situation, the feces are unevenly distributed throughout the intestines, which leads to their tamping and complications during the act of defecation.
 nine0006
nine0006
Additional factors in the development of hemorrhoids are: chronic constipation or diarrhea, heredity, changes in blood volume, coagulation process, intensive synthesis of mediators, long stay in the toilet, excessive straining, weight gain.
Diagnostics
At the slightest suspicion of pathology, it is urgent to contact a proctologist. The most competent treatment is to prevent the development of the disease. nine0003
Diagnosis consists of several stages: a survey, examination, instrumental and laboratory examination.
Poll
The proctologist asks a number of questions in order to clarify the lifestyle, nutrition, genetic predisposition to the patient's varicose veins. The doctor is also interested in the frequency and nature of the symptoms that provoke them.
An important role is played by concomitant diseases, occupation, allergies, etc. nine0003
After collecting an anamnesis, the doctor makes a preliminary diagnosis. It is possible to confirm or refute it according to the results of further examinations.
It is possible to confirm or refute it according to the results of further examinations.
Digital rectal examination
With hemorrhoids in a mild form, the examination is painless. The proctologist studies the structure of the anus (closeness, symmetry of the valves, deformities), the condition of the mucous membranes and the adjacent dermis, the presence of inflammation and discharge, etc. If the procedure is painful for the patient, then the question of transferring it is raised. nine0003
Examination is necessary to make a differential diagnosis. Symptoms similar to hemorrhoids appear with anal fissures, condyloma, oncology, benign neoplasms, rectal prolapse.
In addition to visiting the proctologist, the patient is examined by a gynecologist. The doctor evaluates the condition of the vagina, rectovaginal septum and tissues adjacent to the anus.
Instrumentation
If your doctor suspects other bowel disease, an anoscopy may be done. This is a technique in which a tube with a flashlight is inserted into the rectum. If necessary, during the procedure, tissues of the intestinal mucosa are taken for a biopsy.
This is a technique in which a tube with a flashlight is inserted into the rectum. If necessary, during the procedure, tissues of the intestinal mucosa are taken for a biopsy.
Anoscopy during pregnancy is possible, since it does not require anesthesia. It does not cause pain to the patient, only a slight discomfort during the introduction of the instrument and the sampling of the biomaterial. nine0003
Before carrying out instrumental diagnostics by the method under consideration, cleaning of the lower intestine with microclysters is required.
If oncology or intestinal bleeding is suspected, a colonoscopy is performed. In other cases, during the period of preeclampsia, colonoscopy is strictly not recommended, as it can cause the onset of premature birth.
Laboratory diagnostics
nine0002 Due to the fact that during pregnancy a woman systematically donates biomaterials for research, when examining hemorrhoids, they can not be taken additionally.
However, this rule applies to cases where the clinical picture is clear and there are no reasons for additional laboratory diagnostics.
If there is anal bleeding, especially in the postpartum period, then the patient must donate blood for hemoglobin and feces to determine the latent blood in it. nine0003
Features of the treatment of hemorrhoids in pregnant women
Treatment of hemorrhoids in pregnant women consists of several stages. First of all, the patient is prescribed a lifestyle change and drug therapy. If necessary, it is possible to carry out minimally invasive techniques to remove the hemorrhoid.
Lifestyle change
After collecting information about the patient and her habits, the doctor may recommend: nine0003
1. Stick to a diet:
- avoid spicy and salty foods;
- eat foods rich in fiber;
- if there are no diseases of the cardiovascular system and kidneys, then drink at least 1.
 5 liters of water per day.
5 liters of water per day.
2. Carry out the act of defecation correctly:
- do not push;
- sit no longer than 5 minutes, even if it was not possible to defecate; nine0006
- use microclysters.
3. Moderate physical activity. It can be a complex of exercise therapy, light physical exercises without weights, long walks at a calm pace.
If it is necessary to use laxatives, castor oil is recommended to be replaced with medicines allowed during gestation. Preparations containing magnesium can lead to premature stimulation of the uterus. It is better to give preference to vaseline oil, preparations with lactulose or foods rich in dietary fiber (plums, prunes, for example). The introduction of drugs in any trimester is permissible only after agreement with the supervising physician. nine0003
Compliance with simple rules allows you to eliminate the disease completely or significantly reduce its manifestations in 70% of cases.
Medical therapy
Due to the limited list of permitted medications, the scheme and course of taking medications should be developed by a doctor.
As a general rule, patients in position are prohibited from taking analgesics. However, there are a number of drugs, which include local anesthetics. They are not absorbed into the bloodstream, so they are absolutely safe for the fetus. These can be: suppositories, ointments and gels with benzocaine and lidocaine. nine0003
To eliminate the processes of thrombus formation in the hemorrhoid, let's take drugs with diosmin. They relieve swelling and inflammation in the “bump” and tissues adjacent to the anus. But during lactation, this group of drugs is prohibited, since proper clinical studies in the field of the effect of diosmin on the development of a child during breastfeeding have not been conducted. During lactation, local hormonal rectal suppositories and ointments are prescribed to relieve swelling, inflammation and itching.
When self-medicating, it should be remembered that even the safest medicines for an adult can be extremely dangerous for the fetus and newborn. Therefore, the appointment of drugs should be handled by a doctor.
Surgery
Milligan-Morgan operations or Ferguson hemorrhoidectomy during pregnancy are used extremely rarely and in situations that threaten the life and health of the patient. They can be carried out after childbirth, when the hemorrhoids have not returned to normal on their own or there is no effect from drug therapy or minimally invasive techniques. nine0003
Pregnant women may be offered a thrombectomy. This is a minimally invasive procedure that uses a local anesthetic. It takes only 10 minutes and does not require a long rehabilitation. The operation is painless.
For recurrent bleeding, the method of ligation with latex rings is used. The essence of the method is to pinch the leg of the hemorrhoid and stop the flow of blood into it. Over time, the knot dries out and falls off on its own. It is used only for internal hemorrhoids using local anesthesia. nine0003
Over time, the knot dries out and falls off on its own. It is used only for internal hemorrhoids using local anesthesia. nine0003
Complications
Not running hemorrhoids does not affect the course of gestation. It only causes discomfort to the pregnant woman and worsens the quality of life of the patient.
In advanced situations, it can cause the development of anemia, anal bleeding with attempts, paraproctitis, thrombophlebitis of the rectal veins, pinching. Complications lead to the launch of necrotic processes and infection of the patient's tissues, as well as intrauterine infection of the fetus. nine0003
There is an opinion that hemorrhoids lead to oncology. However, it is not. It can affect the quality of sleep, cause an increase in blood pressure and cause anxiety, thereby worsening the physical and psycho-emotional state of the patient.
Prophylaxis
Timely diagnosis and therapy can slow down the development of pathology in the early stages or eliminate it completely. With surgery, the problem can be completely eliminated. However, minimally invasive techniques used during pregnancy do not exclude relapses. nine0003
With surgery, the problem can be completely eliminated. However, minimally invasive techniques used during pregnancy do not exclude relapses. nine0003
To avoid the re-development of hemorrhoids or prevent its occurrence during gestation, experts recommend following simple rules.
Nutrition and drinking regimen
Patients are advised:
- eat often and in small portions;
- , depending on the trimester and the state of the body, consume the amount of calories recommended by the doctor;
- consume enough water, fiber and dietary fiber; nine0006
- Eliminate alcohol completely.
Depending on the type of constipation, a diet may be suggested.
So, with spastic constipation caused by irritation of the intestinal receptors, onions, legumes, mustard, unripe berries and fruits, black bread should be excluded from the diet. Add broccoli, honey (if there is no allergy), raisins, ripe apples, corn, potatoes, carrots, cauliflower, dried apricots, cereals (oatmeal and pearl barley), sour-milk products, vegetable fats to the diet.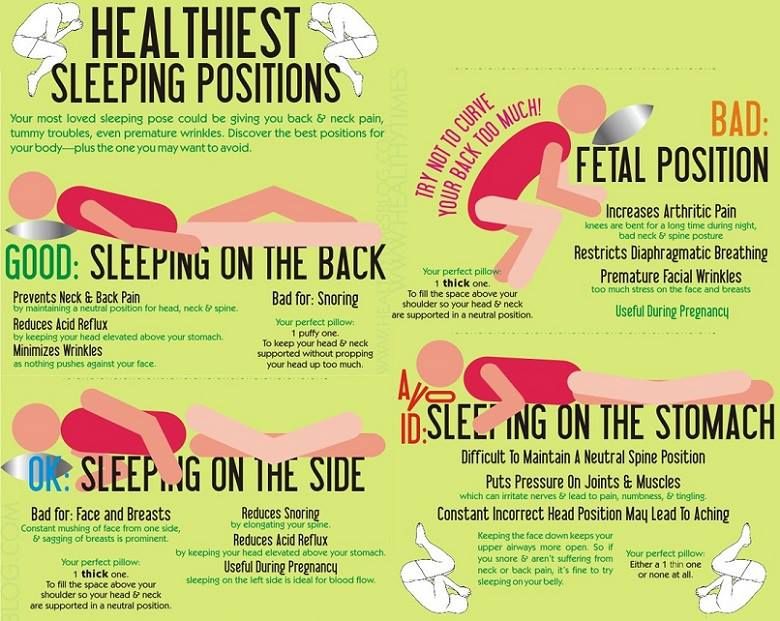 Vegetables and fruits need to be boiled, steamed or baked, they can be mashed. nine0003
Vegetables and fruits need to be boiled, steamed or baked, they can be mashed. nine0003
With atonic constipation, on the contrary, it is necessary to increase intestinal motility. The patient is recommended to diversify the menu with beets, prunes, berry and fruit decoctions, fresh salads, fresh fruits, juices and compotes.
An indicator of the correctness of the action is the normalization of the stool and a comfortable bowel movement.
Personal care
In addition to morning and evening hygiene, patients are advised to carry out additional procedures after each act of defecation. To do this, you can use wet wipes without alcohol, as well as a cool hygienic shower. nine0003
If hemorrhoids still appear, you should abandon toilet paper, even the softest, and give preference to a hygienic shower with soap. For a hygienic shower, you can use herbal infusions and decoctions, a weak solution of potassium permanganate or other available antiseptic.
Physical activity
During pregnancy, moderate gentle physical activity is extremely important to normalize blood circulation in the lower extremities and pelvic organs. nine0003
Pregnant women benefit from gymnastics (for example, according to Kegel), an individual set of exercises, exercise therapy, yoga (for pregnant women). A set of exercises designed for 10 - 15 minutes a day is enough.
Recently, hygienic gymnastics has been gaining popularity. The essence of the exercise is to lie on your back with a raised pelvis. For convenience, a pillow can be placed under the pelvis. For the day you need to do 3 sets of 15 minutes.
Pregnant women are also advised to avoid prolonged static standing and sitting. It is strongly not recommended to supercool and walk for a long time in wet weather. nine0003
Running hemorrhoids during pregnancy is a danger not only to the mother, but also to the fetus. Complications can force doctors to resort to radical measures to stop bleeding, which is fraught with premature birth with all the ensuing consequences for the child.
Like any disease, hemorrhoids are easier to prevent by using prevention recommendations and consulting a doctor in a timely manner. Call +7 (4842) 20-70-20!
FAQ
Of course NO! Hemorrhoids are not a tumor, as many people think, it is associated with deformation of the vessels of the lower rectum.
The danger of late treatment for hemorrhoids lies in the risk of bleeding. But discomfort and bruising also occur with rectal cancer.
As soon as there is discomfort in the anus, you should immediately contact a proctologist for an examination.
You can't say yes or no. In the large intestine, the processes of fecal formation take place. Further movement of feces is facilitated by wave-like contractions of the walls of the rectum, which depend on our nutrition and activity. These contractions are called peristalsis. The walls of the large intestine simultaneously absorb minerals and water. If there is no proper level of peristalsis, even with the consumption of large amounts of water, pathology can develop! nine0003
Hemorrhoids are considered a chronic disease.