Allergies during pregnancy first trimester
Pregnancy and Allergies | Allergy & Asthma Network
Table Contents
- 1 Pregnancy and Allergies
- 1.1 Do women develop allergies for the first time during pregnancy?
- 1.2 Do allergies get worse during pregnancy?
- 1.3 What are types of allergy symptoms during pregnancy?
- 1.4 Does a stuffy nose during pregnancy mean I have allergies?
- 1.5 What medicines can I take for allergies during pregnancy?
- 1.6 Can I use a nasal spray during pregnancy?
- 1.7 Can I get allergy shots during pregnancy?
- 1.8 If I experience anaphylaxis, can I use my epinephrine auto-injector during pregnancy?
- 1.8.1 Can I breastfeed if I take allergy medications?
- 1.9 If I have allergies during pregnancy, will the baby have allergies?
- 1.10 What can I do to reduce allergy symptoms during pregnancy without taking medications?
- 1.11 Are there certain foods that pregnant moms should avoid to reduce risk of the child developing allergic disease?
- 1.
12 See Related Pages
Do women develop allergies for the first time during pregnancy?
It is possible for a woman to develop allergies during pregnancy. It is more common for women to already have allergies before conception.
Do allergies get worse during pregnancy?
It depends on the woman and the severity of allergies during pregnancy. About one-third of moms-to-be find their allergy symptoms tend to worsen during pregnancy. Another one-third find their allergy symptoms stay the same. And another one-third find their allergy symptoms actually improve during pregnancy.
What are types of allergy symptoms during pregnancy?
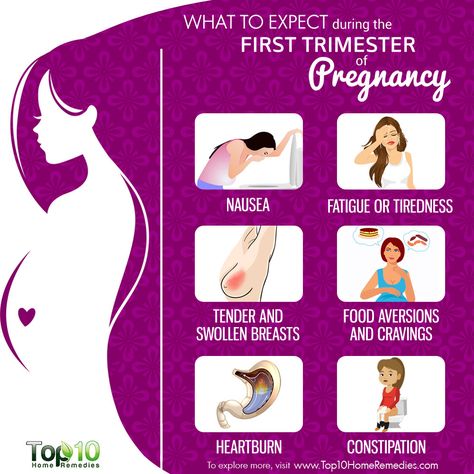
Symptoms are the same for pregnant women as they are for non-pregnant individuals. Common allergy symptoms during pregnancy include:
- itchy, watery eyes
- sneezing
- sore or itchy throat
- runny nose
- sinus congestion
Does a stuffy nose during pregnancy mean I have allergies?
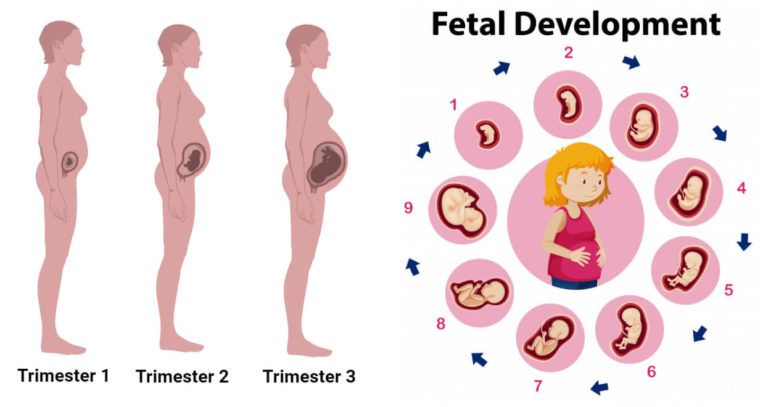
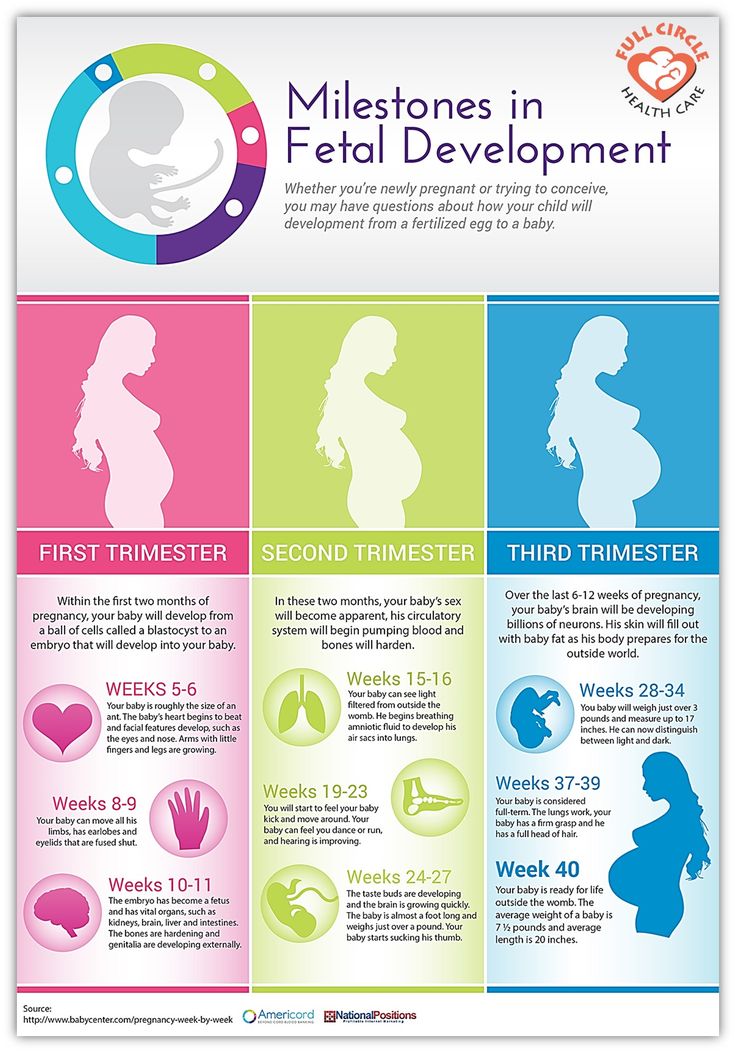
Pregnant women often develop stuffy noses.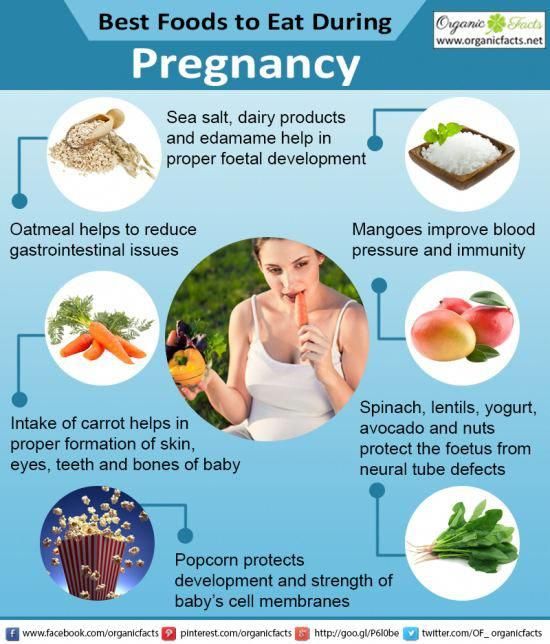 Nasal congestion usually starts sometime in the second trimester causing mucus membranes to swell and soften. Your doctor may refer to this as pregnancy rhinitis.
Nasal congestion usually starts sometime in the second trimester causing mucus membranes to swell and soften. Your doctor may refer to this as pregnancy rhinitis.
Pregnancy rhinitis can make you as stuffed up as if you had a cold or an allergy. It can result in nosebleeds during pregnancy and/or post nasal drip that may make you cough or even gag at night.
The good news is that pregnancy rhinitis typically goes away soon after pregnancy ends.
How can you tell the difference between allergies and a bad case of pregnancy congestion? If you have allergies, you’ll most likely experience symptoms such as congestion, coughing, sneezing and itchy eyes. If noticeable itchiness and sneezing aren’t plaguing you, it could be hormone-related congestion of pregnancy. If you’re not sure, talk to your doctor.
What medicines can I take for allergies during pregnancy?
Women should be very cautious when taking medications during pregnancy, especially during the first trimester.
It’s important to talk with a doctor before using allergy medicine while pregnant. Work together to find an appropriate balance for the medication and symptom control.
Your doctor may first recommend ways to reduce symptoms that don’t involve medications. Strategies include allergy proofing your home, avoiding allergy triggers, or using a saline (saltwater) nasal spray, nasal irrigation or nasal strips.
- Oral antihistamines treat nasal and eye allergy symptoms of allergic rhinitis. It is best to take them after the first trimester.
- Loratadine and cetirizine are second-generation oral antihistamines. They are considered safe for pregnancy, according to multiple studies. They do not cause drowsiness unlike first-generation oral antihistamines (chlorpheniramine, diphenhydramine, tripelennamine).
Avoid using antihistamines combined with a decongestant during pregnancy. Research is ongoing on the impact of these medications to mom and baby.
Can I use a nasal spray during pregnancy?
Some nasal sprays are safer than others.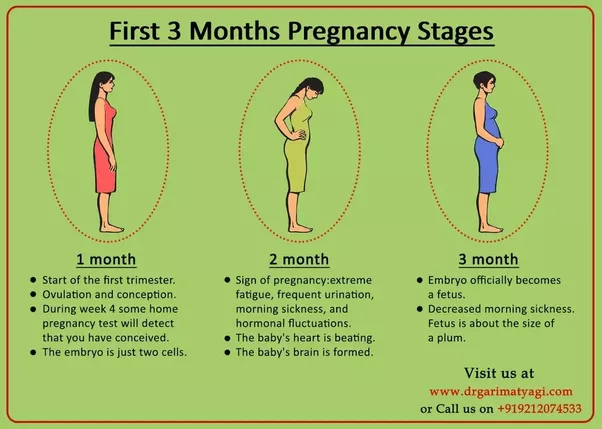 The good thing about nasal sprays is that the drug focuses primarily on the nose. It does not travel throughout the rest of the body.
The good thing about nasal sprays is that the drug focuses primarily on the nose. It does not travel throughout the rest of the body.
Corticosteroid nasal sprays are mostly safe. They are prescribed to pregnant women with moderate to severe allergy symptoms that last longer than a few days. Budesonide is considered the safest. Mometasone and fluticasone are also considered safe.
Decongestant nasal sprays are more problematic. Some studies point to a risk of birth defects when expectant moms use these products. They are not typically recommended during pregnancy, especially during the first trimester.
Pregnant women should avoid antihistamine nasal sprays, as there is not enough research to prove their safety.
Always talk with your doctor about which nasal spray medication is right for you, as well as any medication risks to you and your baby.
Can I get allergy shots during pregnancy?
Pregnant women can continue with allergy shots they started before they were pregnant. They should stay at the current dose through pregnancy — do not increase dosage. If there’s any reactivity, the doctor may reduce the dosage of the shot.
They should stay at the current dose through pregnancy — do not increase dosage. If there’s any reactivity, the doctor may reduce the dosage of the shot.
It’s not recommended to start allergy shots during pregnancy. This can trigger changes in an already-fluctuating immune system and may cause a systemic reaction.
If I experience anaphylaxis, can I use my epinephrine auto-injector during pregnancy?
Treatment of anaphylaxis during pregnancy is similar to treatment for non-pregnant women with food, insect venom or latex allergy. Use epinephrine at the first sign of symptoms.
Can I breastfeed if I take allergy medications?
Breastfeeding is a good way to increase your child’s immunity. It is strongly recommended. Medications recommended for use during pregnancy can be continued while nursing. (The baby gets less medicine through breast milk than in the womb.) Your allergist can discuss the best medications for you when nursing your baby.
If I have allergies during pregnancy, will the baby have allergies?
Allergy symptoms during pregnancy are not believed to have any impact on whether your baby develops allergies.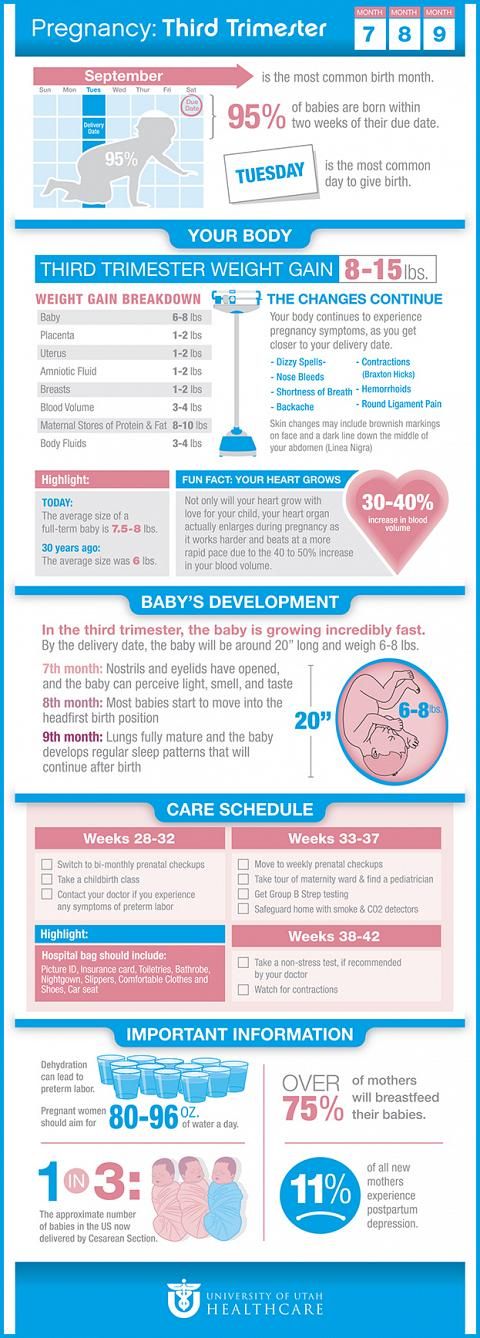 Genetics, however, are a major factor in the development of allergies in children. If a child has a parent or a sibling with allergies, then they are at increased risk of getting allergies, too.
Genetics, however, are a major factor in the development of allergies in children. If a child has a parent or a sibling with allergies, then they are at increased risk of getting allergies, too.
An expectant mother’s diet during pregnancy may be a factor in whether a child develops allergic rhinitis, food allergies, asthma or eczema. One study found that expectant moms who ate plenty of food-based vitamin D reduced their child’s risk of getting allergic rhinitis. Foods with a lot of vitamin D include dairy products, cereals, fish, eggs and mushrooms. Learn more about the allergic march.
What can I do to reduce allergy symptoms during pregnancy without taking medications?
Stay away from people who are smoking. Smoke can make allergies worse. Exposure to secondhand smoke during pregnancy isn’t good for you or your baby.
If you’re allergic to pollen, try to stay inside as much as possible. If you do go outside, try wearing wraparound sunglasses to keep pollen out of your eyes. When you come back inside, take off your shoes, wash your hands and face, and change clothes so the pollen doesn’t stay with you. Then put your clothes in the wash. Shower and wash your hair before you go to sleep to help relieve nighttime symptoms.
If you do go outside, try wearing wraparound sunglasses to keep pollen out of your eyes. When you come back inside, take off your shoes, wash your hands and face, and change clothes so the pollen doesn’t stay with you. Then put your clothes in the wash. Shower and wash your hair before you go to sleep to help relieve nighttime symptoms.
If you’re allergic to dust, make sure your house is cleaned regularly or hire someone to clean for you. Use a vacuum with a HEPA filter, a wet mop or a sweeper to avoid stirring up dust. A microfiber cloth is better than a traditional feather duster. Try to keep away from attics, basements and other musty places.
If you’re allergic to pets, let your dog- and cat-owning friends know of your allergy before you drop by so they have time to make arrangements. If you’re suddenly allergic to your own pet, try to make at least one room in your house pet-free.
Are there certain foods that pregnant moms should avoid to reduce risk of the child developing allergic disease?
Avoidance diets during pregnancy do not prevent allergic disease, according to the American Academy of Pediatrics.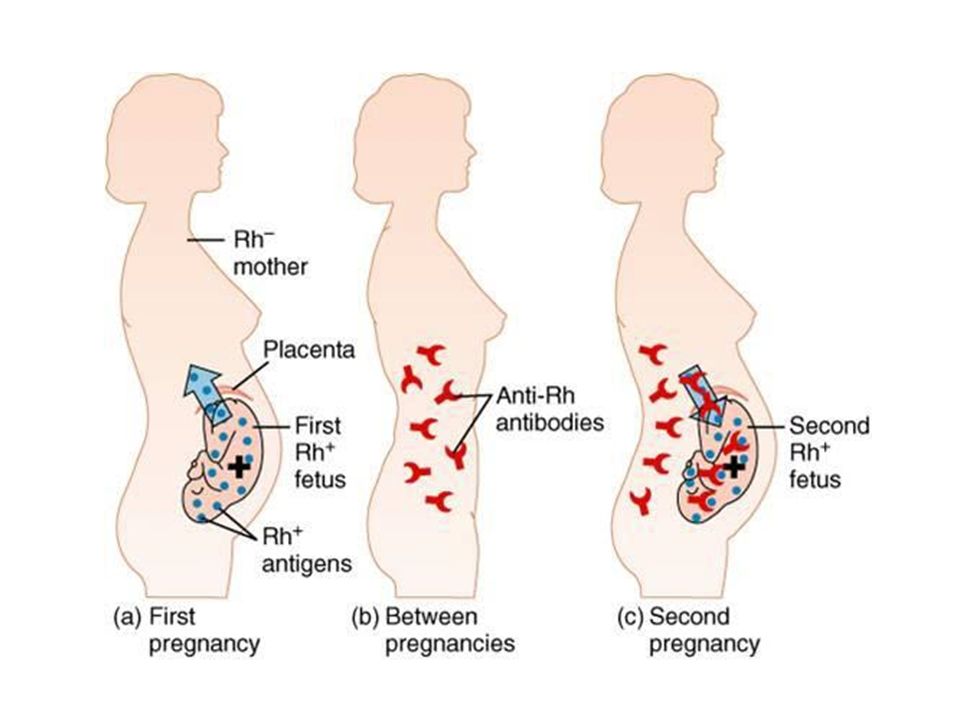 That means pregnant women don’t need to avoid common food allergens such as peanuts, tree nuts, milk or wheat.
That means pregnant women don’t need to avoid common food allergens such as peanuts, tree nuts, milk or wheat.
While no specific diet or food can prevent allergic diseases, studies have shown that consuming peanuts, milk and wheat in the first and second trimesters can reduce the risk of a child developing peanut allergy, allergic rhinitis and asthma.
Doctors say the most important thing expectant moms can do is eat a healthy diet rich in fruits and vegetables, fish and vitamin D. Consuming these foods may reduce the risk of a child developing allergic diseases.
Talk with your doctor before considering any changes involving diet during pregnancy.
See Related Pages
Allergies During Pregnancy: Treatments
Overview
If you can’t step outside without sneezing, chances are seasonal allergies are to blame. Pregnancy can cause enough symptoms as it is. But adding an itchy nose to an itchy belly can make for a long trimester.
Pregnancy can cause enough symptoms as it is. But adding an itchy nose to an itchy belly can make for a long trimester.
Seasonal allergies cause symptoms, including:
- coughing
- sneezing
- itching
- runny nose
The condition can affect your breathing. So can pregnancy. Fortunately, there are many safe treatments you can use to relieve seasonal allergy symptoms.
You need to be careful of the medications you take and other treatments during pregnancy. Here’s what you need to know about treating seasonal allergies.
What causes seasonal allergies?
Your body’s immune system ideally fights against “bad guys” like flu viruses, colds, and other infection-causing organisms that seek to make you sick. But sometimes, your immune system reacts to things that really aren’t all that harmful to you. This is the case with seasonal allergies. Seasonal allergies occur when your body reacts to allergens that tend to show up in a certain season. Seasonal allergies are usually your body’s reaction to pollen. Pollen is a powdery substance that forms the male sperms cells that fertilize plants so they can reproduce. Common culprits of seasonal allergies include:
Seasonal allergies are usually your body’s reaction to pollen. Pollen is a powdery substance that forms the male sperms cells that fertilize plants so they can reproduce. Common culprits of seasonal allergies include:
- cocklebur
- grasses
- molds
- pigweed
- ragweed
- trees
- tumbleweed
Depending on where you live, spring allergies can pop up around February and end in early summer. Fall allergies can take place in late summer and continue until late fall. Pregnancy can make seasonal allergies worse. Also, a condition called “rhinitis of pregnancy” can cause similar symptoms to seasonal allergies. This usually occurs in the last trimester. But the cause of rhinitis of pregnancy is extra hormones, not allergens.
At-home treatments for seasonal allergies
Moms-to-be with seasonal allergies can use several at-home treatments to relieve their symptoms. Some examples include:
- Creating a saline nasal spray by combining 8 ounces of warm water with 1/4 salt to the water.
 You can add this to a spray or squeeze bottle to irrigate and soothe irritated nasal passages. Neti pots are another option.
You can add this to a spray or squeeze bottle to irrigate and soothe irritated nasal passages. Neti pots are another option. - Watching news reports and checking pollen counts daily. During episodes of large pollen counts, pregnant women can avoid too much time outdoors to keep exposure down.
- Avoiding going outdoors between 5 a.m. and 10 a.m., the times when pollen counts are usually the highest.
- Taking showers and changing clothing after being outside. This can help remove pollen that builds up on hair and clothing.
- Wearing a protective filter mask when doing outdoor activities like mowing the lawn or gardening.
- Wearing over-the-counter nasal strips at night. These position the nasal passages so they’re more open. This reduces a person’s symptoms.
If you can avoid whatever’s causing your seasonal allergies, you can often keep your symptoms at bay.
Medications for seasonal allergies during pregnancy
Most pregnant women can safely take over-the-counter allergy medications. Examples of medications that have research to support that they’re safe for pregnant women to take (as of currently available data) include:
Examples of medications that have research to support that they’re safe for pregnant women to take (as of currently available data) include:
- cetirizine (Zyrtec)
- chlorpheniramine (ChlorTrimeton)
- diphenhydramine (Benadryl)
- loratadine (Claritin)
There are always risks when taking any medication during pregnancy. Women should talk with their doctors before taking allergy medicines to make sure they aren’t potentially harmful. While doctors consider many oral over-the-counter medications safe for seasonal allergies, using both oral and nasal spray decongestants isn’t as studied or well-known. Use of nasal sprays may be safer than oral decongestants. That’s because nasal sprays aren’t as likely to be absorbed into the bloodstream. An example is oxymetazoline, an ingredient in brands like Afrin and Neo-Synephrine. Women should exercise caution when using nasal sprays for more than three days. This is because using decongestants for longer can make allergy symptoms worse by causing nasal swelling. Some women also get allergy shots. These are compounds of allergens that are injected as a means to desensitize a person to an allergen. If a woman becomes pregnant while she is in the course of her allergy shots, she can usually keep getting them. Pregnancy isn’t a good time to start getting allergy shots. It’s possible they can cause strong allergic reactions. Without knowing a woman’s reaction, it’s best to delay starting allergy shots until after giving birth.
Some women also get allergy shots. These are compounds of allergens that are injected as a means to desensitize a person to an allergen. If a woman becomes pregnant while she is in the course of her allergy shots, she can usually keep getting them. Pregnancy isn’t a good time to start getting allergy shots. It’s possible they can cause strong allergic reactions. Without knowing a woman’s reaction, it’s best to delay starting allergy shots until after giving birth.
Allergy medications to avoid during pregnancy
Doctors haven’t widely studied some medicines regarding their safety in pregnancy. This is because it isn’t ethical to perform testing on pregnant women. As a result, most information about medications is due to reports and knowledge about general medication safety. According to the American College of Allergy, Asthma, & Immunology (ACAAI), several medications aren’t considered safe. During the first trimester, it’s especially important to consider the potential risks and benefits because the baby is developing the most then.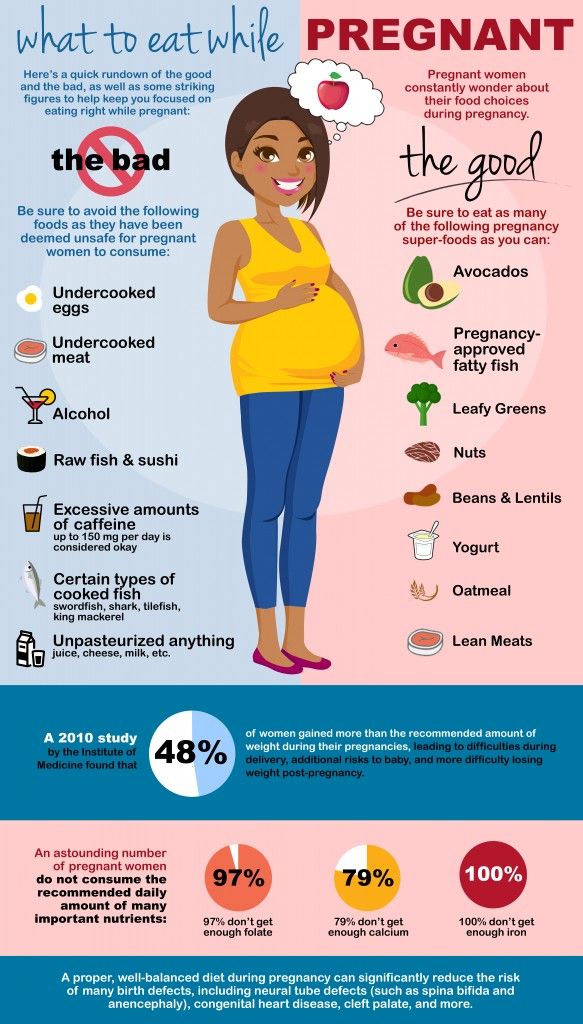 Unsafe treatments during pregnancy include:
Unsafe treatments during pregnancy include:
- Pseudoephedrine (Sudafed): While some studies found that pseudoephedrine is safe in pregnancy, there have been reports of an increase in abdominal wall defects in the babies of mothers who used the medication during pregnancy, according to the ACAAI.
- Phenylephrine and phenylpropanolamine: These decongestants are considered “less desirable” than taking pseudoephedrine, according to the ACAAI.
Next steps
If your seasonal allergy symptoms have made sleep evasive or are interfering with your daily activities, treatments are available that are likely safe for you and baby. Always talk to your doctor about any concerns you have regarding medications. You can also read medication labels carefully to ensure your medicines don’t have a warning for pregnant women (manufacturers are legally required to list their pregnancy safety information). If you have questions on specific allergy medicines, visit the website MotherToBaby. org. This site is operated by the Organization of Teratology Information Specialists, whose members study medication safety for pregnant and breast-feeding moms. Pregnancy and seasonal allergies are self-limiting conditions. Your due date will come and blooming season will end. It’s important you stay as comfortable as possible while you navigate both.
org. This site is operated by the Organization of Teratology Information Specialists, whose members study medication safety for pregnant and breast-feeding moms. Pregnancy and seasonal allergies are self-limiting conditions. Your due date will come and blooming season will end. It’s important you stay as comfortable as possible while you navigate both.
Q:
What remedies are helpful for allergies during pregnancy? Anonymous patient
A:
The safest methods are taking simple steps such as trying to avoid known allergens and saline nose drops. When this doesn’t work, over-the-counter antihistamines such as Claritin, Zyrtec, and Tavist are acceptable. Sudafed can be used after the first trimester with caution if other methods fail. Almost all of these medications are category C which means there aren’t sufficient studies available to assure safety, yet there are no significant known problems with these drugs. If the problem is severe or is not responding to home remedies, seek the advice of a doctor.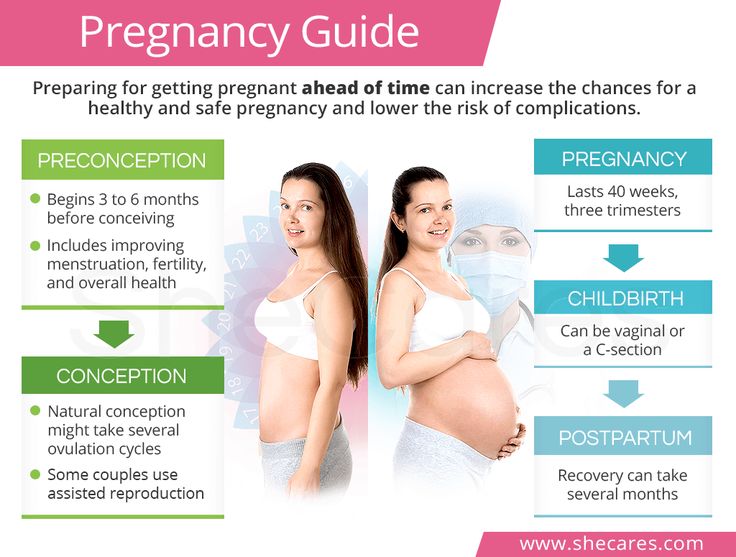 Michael Weber, MD
Michael Weber, MD
Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
Share on Pinterest
Allergies in Pregnancy: Allergies in Pregnancy
Increased prevalence and use of cosmetics, synthetics, disinfectants, and changing food and human diets are contributing to the increase in allergies.
Allergic disease occurs when the body's immune system reacts to allergens when it comes into contact with them. Allergic diseases also include acute allergies.
Among people susceptible to acute allergosis, from 5 to 20% of cases are pregnant. Pregnant women are most susceptible to this disease between the ages of 18 and 24.
Allergies in pregnancy - effects on the baby
When allergies develop in pregnant women, they do not affect the fetus. This is due to the fact that immunocomplexes that react to an allergen that irritates the body cannot reach the fetus due to the placenta. Despite this, the fetus that is in the womb can be negatively affected by the disease due to three main reasons:
Despite this, the fetus that is in the womb can be negatively affected by the disease due to three main reasons:
- When the mother's health condition changes.
- Medicines needed to treat when allergies occur during pregnancy may affect the reduction in uteroplacental blood flow. The process of supplying blood to the fetus is deteriorating.
- Drugs other than the above effects may have a bad effect on the fetus as a whole.
Treatment of allergies during pregnancy
Treatment should be started immediately, because only in this case the allergy will not have time to affect the fetus. Also, a very important task, which must be taken into account before starting treatment, is the maximum avoidance of harm that can be caused to an unborn child by drugs.
When prescribing a course of treatment, a doctor should take into account the fact that the number of pregnant women who have diseases of the internal organs, according to statistics, reaches 45%.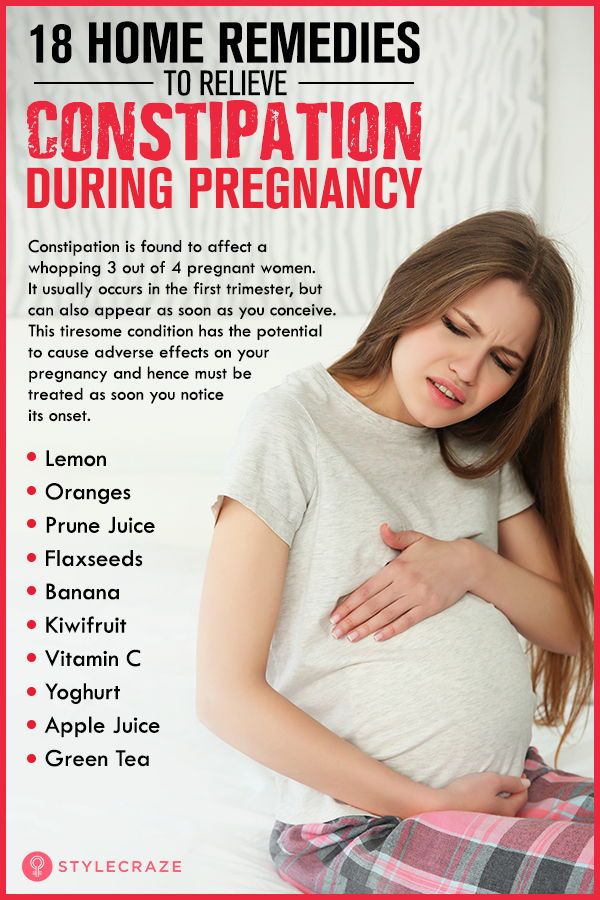 In addition, the proportion of women taking medication during pregnancy ranges from 60% to 80%. The average number of medications a woman takes during the entire pregnancy process is 4 different types. And this is without taking into account various vitamin complexes, dietary supplements and minerals. That is why a pregnant woman should never engage in self-treatment after discovering the first signs of an allergy in herself. You must immediately go to an appointment with a doctor who will provide qualified assistance and prescribe the correct course of treatment, as harmless as possible to the fetus.
In addition, the proportion of women taking medication during pregnancy ranges from 60% to 80%. The average number of medications a woman takes during the entire pregnancy process is 4 different types. And this is without taking into account various vitamin complexes, dietary supplements and minerals. That is why a pregnant woman should never engage in self-treatment after discovering the first signs of an allergy in herself. You must immediately go to an appointment with a doctor who will provide qualified assistance and prescribe the correct course of treatment, as harmless as possible to the fetus.
The search for an allergy medicine in pharmacies, if necessary, after a doctor's prescription, can be done on our portal. There is all the information about each of them, and it is also possible to compare their cost.
When contacting an allergist for a consultation, a woman, in order to correctly diagnose and identify the allergen, will be subject to a special examination. A similar test involves preparing a solution that is made from the irritants that are believed to have caused the allergy. After that, a similar solution is injected into the skin of a pregnant woman in a small amount. If she is allergic to one of the irritants present in the solution, the area around the injection site will become swollen.
A similar test involves preparing a solution that is made from the irritants that are believed to have caused the allergy. After that, a similar solution is injected into the skin of a pregnant woman in a small amount. If she is allergic to one of the irritants present in the solution, the area around the injection site will become swollen.
Where to get skin tests for allergies, as well as a laboratory blood test, you can find on our website. Here you can choose a profitable and convenient location option for yourself.
There are three stages in the development of allergies during pregnancy. The first entry of the allergen into the body. Immunity cells recognize the "enemy" and mechanisms for the formation of antibodies begin to work in the body. Second allergen exposure. The body is again exposed to allergens. There are processes that stimulate the production of histamine, which causes allergic symptoms. Third stage. Vessels expand, tissue permeability increases. This results in swelling and inflammation. A strong vasodilation is also possible, causing a sharp drop in blood pressure, i.e. anaphylactic shock occurs.
This results in swelling and inflammation. A strong vasodilation is also possible, causing a sharp drop in blood pressure, i.e. anaphylactic shock occurs.
The result is an acute allergic reaction.
Acute allergosis:
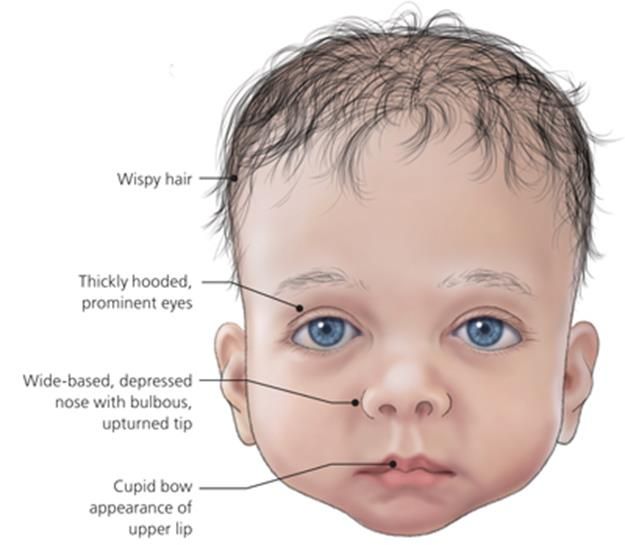
- allergic rhinitis. Complication of breathing through the nose, its congestion, the mucous membranes of the nose swell, and an abundant secretion of mucous secretion appears, sneezing and burning in the throat occur;
- urticaria. Damage to a certain area of \u200b\u200bthe skin - the appearance of sharply defined blisters, accompanied by itching;
- redness, swelling, conjunctiva, itching of the eyes, lacrimation, narrowing of the palpebral fissure.
Severe allergy:
- generalized urticaria. Involvement of all areas of the skin with symptoms of simple urticaria;
- angioedema. Edema of the skin, mucous membranes, and subcutaneous tissue. Basically, in the area of lips, cheeks, forehead, eyelids, hands, feet.
 Swelling of the larynx. Swelling of the gastrointestinal mucosa, accompanied by pain;
Swelling of the larynx. Swelling of the gastrointestinal mucosa, accompanied by pain; - anaphylactic shock. Arterial hypotension. Loss of consciousness, respiratory failure, swelling of the respiratory tract, urticaria, itching.
Quincke's edema, urticaria and rhinitis are most common in pregnant women.
What causes allergic reactions? Conventionally, three stages can be distinguished in their development. When a mother has allergic reactions, the fetus does not show any signs of allergy, because specific immunocomplexes that react to an allergen-irritant are not able to penetrate the placenta. However, in spite of this, a child in the womb may be affected by allergies for the following reasons:
- the mother's condition changes due to the onset of the disease;
- the influence of certain drugs that can cause a decrease in uteroplacental blood flow, which ensures the life of the fetus;
- the negative effect of drugs directly on the fetus.

So how do you treat allergies in pregnant women? The most basic goal of treatment is the painless elimination of symptoms of pregnancy allergy without the risk of negative effects on the fetus. The reaction of the human body to taking various drugs largely depends on the general vitality, the type of therapy it undergoes, and the nature of the symptoms of the disease.
Pregnancy is a special, complex state of the body, because up to 45% of pregnant women can have diseases of the internal organs, and from 60 to 80% of expectant mothers who regularly take certain drugs in general. During the course of pregnancy, on average, according to surveys and observations, a woman can take up to four different medications, and this does not include vitamins, various nutritional supplements and minerals.
Habitual allergy pills, during pregnancy, for the most part, are contraindicated:
- Diphenhydramine taken late in pregnancy may cause uterine excitability or contractions when taken in doses greater than 50 mg;
- Terfenadine frequently causes weight loss in neonates;
- Astemizole has a strong toxic effect on the fetus;
- Suprastin (chloropyramine), cetirizine (Alleprtec), claritin (loratadine) and fexadine (fexofenadine) are acceptable during pregnancy, but only if the effect of treatment outweighs the potential risk to the child;
- Tavegil (clemastine) should never be used throughout pregnancy, except in cases of direct threat to the life of the pregnant woman;
- Pipolfen (piperacillin) is strongly discouraged during pregnancy and lactation.
If an allergy occurs in pregnant women for the first time, it is necessary to urgently contact an allergist. Separately, it is worth noting that during pregnancy, the primary task is to eliminate contact with the allergen, and not the symptoms of allergies.
To find out what may be an allergen in a particular case, a special examination is carried out.
What should be done in case of manifestation of OAS, and what drugs can be used:
- if the allergen is known, it must be eliminated immediately;
- consult a doctor;
- In the absence of the possibility of consulting a doctor, the following list of recommended drugs should be used.
1st generation of H2 blockers:
- Pipolfen (piperacillin) - not recommended during pregnancy or breastfeeding;
- Suprastin (chlorpyramidine) - can be prescribed only for acute allergic reactions during pregnancy;
- Allertec (cyterizine) - the drug can be taken in late pregnancy;
- Tavegil (clemastine) - during pregnancy is prescribed only in cases where an allergic reaction threatens the life of a pregnant woman, and for some reason there is no possibility of using other drugs.
 This is due to the negative effect of the drug on the fetus.
This is due to the negative effect of the drug on the fetus.
2nd generation H2-histamine blockers:
Claritin (loratadine) - during pregnancy, the use is allowed only if the expected effect of the treatment outweighs the potential risk to the child. The drug can be used only in cases where the disease state of the mother threatens the fetus more than taking this drug. This risk in each case must be assessed by a doctor.
3rd generation H2-histamine blockers:
Fexadine (fexofenadine) - during pregnancy, you can use it only in cases where the expected positive effect of therapy outweighs the potential risk to the child.
Prevention of allergic disease during pregnancy
Prevention of allergies is important, as it will help to avoid allergic disease and the consequences of exposure to drugs for its treatment on the fetus. In order to prevent, it is necessary, first of all, to remove from the woman's food products that are characterized as highly allergic. This is primarily due to the fact that irritants most often enter through the gastrointestinal tract, and then penetrate to the fetus. Until about the 22nd week of intrauterine development in the fetus, the immune system completes its formation. It is after it becomes mature that hypersensitivity begins to develop. This means that after the 22nd week of pregnancy, a pregnant woman should review her diet and exclude from it foods that may be allergens for her.
This is primarily due to the fact that irritants most often enter through the gastrointestinal tract, and then penetrate to the fetus. Until about the 22nd week of intrauterine development in the fetus, the immune system completes its formation. It is after it becomes mature that hypersensitivity begins to develop. This means that after the 22nd week of pregnancy, a pregnant woman should review her diet and exclude from it foods that may be allergens for her.
Also, for the prevention of an allergic disease, one should not have much contact with recently appeared products from the field of cosmetics and household chemicals.
Expectant mothers who have ever been exposed to an allergic disease should completely exclude the possibility of contact with those allergens that have caused an allergic reaction at least once before. In addition, it is recommended not to have pets, to clean the house, preferably wet and daily, to carry out a complete house cleaning weekly, which should include airing rooms, vacuuming carpets and beating, drying pillows.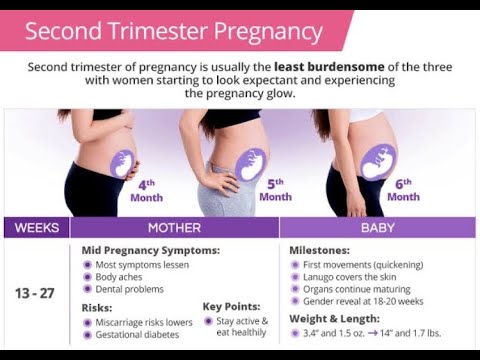
An important aspect of allergy prevention is fetal prevention. First of all, this is the restriction or refusal of the mother from highly allergenic foods. But since the child's immune system is not formed immediately, but only by the 22nd week of pregnancy, then, accordingly, the restriction in the use of highly allergenic foods makes sense from this period. Also, during the entire period of pregnancy, contact with household chemicals and new cosmetics should be limited.
If the expectant mother has never had allergies before, then she can consume risky foods, in small quantities, and not every day, of course. Otherwise, you will have to abandon entire product groups.
Separately, it should be noted that smoking for a future mother during pregnancy and lactation is strictly prohibited, because it affects the development of the respiratory tract and lungs of the fetus, and can cause intrauterine growth retardation. It is also known that after smoking just one cigarette, a spasm of the uterus occurs, which leads to a violation of the supply of nutrients and oxygen to the fetus, and this can last 20-30 minutes.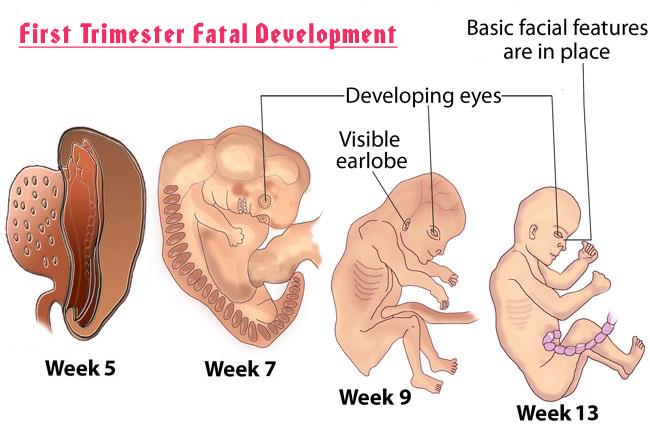 It is also worth refraining from having pets, vacuuming the room as often as possible, carrying out wet cleaning and knocking out and drying pillows weekly.
It is also worth refraining from having pets, vacuuming the room as often as possible, carrying out wet cleaning and knocking out and drying pillows weekly.
And of course, a pregnant woman needs to remember about a healthy lifestyle and the dangers of self-treatment and stress, because an unborn child requires no less care, and in some ways even more than a child who has already been born.
If the allergy nevertheless manifested itself and the doctor prescribed medication, you can search for medications through our website with catalogs of pharmacies in Kyiv.
| When an allergic girl prepares to become a mother, or when an allergy begins during pregnancy, the happy moments of waiting cease to bring joy. At such moments, expectant mothers face a difficult choice. On the one hand, you need to be especially careful in the use of drugs, but, on the other hand, you should not leave allergic reactions unattended. Can pregnancy cause allergies? Pregnancy itself cannot cause allergies. However, allergies, as in other stressful situations, may first appear during pregnancy. How complex biological changes during pregnancy affect the onset and course of allergies is not fully understood scientifically. Allergies: Hay fever. Almost one in five women suffer from hay fever during pregnancy. Since often the nose in pregnant women is blocked due to increased levels of estrogen, therefore, hay fever is exacerbated. Asthma. In 20% of women, asthma worsens during pregnancy. Good treatment of asthmatics is especially important, since this allergy can affect the lack of oxygen in a child. Eczema. Women who suffer from atopic dermatitis often experience an improvement in symptoms during pregnancy. But, for some women, pregnancy only exacerbates the symptoms. Rash (urticaria). Often occurs in pregnant women on a nervous basis. Anaphylactic shock. The immune system during pregnancy is prone to anaphylactic shock. Therefore, you should avoid possible allergens and consult a specialist at the first sign of an allergy. How does pregnancy affect allergies? In order for pregnancy not to be further aggravated by allergy symptoms, you need to contact a specialist. An experienced doctor diagnoses the disease and prescribes treatment. Many allergy medications are not recommended for pregnant or breastfeeding mothers. Pregnant women should try to avoid contact with allergic agents. Then it is possible to reduce medications or completely refuse them. Due to changes in hormone levels in the body of a pregnant woman, allergic rhinitis may increase throughout the period. Especially at the beginning of the second trimester of pregnancy, many women suffer from nasal congestion. What are the treatment options for allergies during pregnancy? Despite certain limitations during pregnancy, methods for diagnosing and treating allergies are available. Skin tests should not be performed at this time, as the risk of anaphylactic shock, although minimal, is present. Instead, a blood test is preferred. Hay fever during pregnancy can be treated with nasal sprays. Studies so far have not revealed the potential harm to the child from the use of such products. Immunotherapy or desensitization is a good way to treat the causes of allergies, that is, it is not only a way to remove the symptoms, but also to combat the causative agents of the allergy. Allergies should be especially carefully monitored and treated during pregnancy. To minimize the burden on the mother and her unborn child. At the first signs of an allergy, pregnant women should definitely contact an allergist. |

 Sometimes you need to calm down and put your thoughts in order so that the allergy goes away.
Sometimes you need to calm down and put your thoughts in order so that the allergy goes away.  More fresh air, sleeping with an elevated upper body, and a saline nasal spray can help.
More fresh air, sleeping with an elevated upper body, and a saline nasal spray can help.