Allergic reaction pregnancy
Allergies During Pregnancy - North Shore Associates in Gynecology & Obstetrics
More than 50 million people suffer from allergies every year. So if you?re sneezing a little more than usual these days, you aren?t alone. Given how common allergies are, it?s not surprising that you might be experiencing symptoms during pregnancy. You might be sneezing or have a sore throat or itchy eyes.
You can manage allergy symptoms when you?re pregnant–and get back to enjoying the outdoors–but it does take a little extra thought and attention.
How Common Are Allergies During Pregnancy?
The true source of allergies resides with your immune system. Usually, when your body encounters a disease, your immune system launches into action. But that immune response can cause certain symptoms within your body. When you come down with a common cold, for example, it?s your immune response–not the virus–which causes your runny nose and cough.
When you have an allergic reaction to something, it?s because your body has identified that allergen as a hazard. So your immune system goes into defense mode. Allergic reactions can occur when the allergen is experienced through skin contact, ingestion, or inhalation. Common allergens include pollen, pet dander, shellfish, and bee stings.
For pregnant women, allergies during pregnancy are particularly common, even among individuals who have not suffered from long-term allergies in the past. In other words, you can sometimes develop new allergies during pregnancy. In other cases, allergies that were already present may become worse. Usually, the novel allergies will subside after your child is born, so most of these allergy-related changes are temporary. Conversely, some allergies improve with the reduced immune response.
Types of Allergies
Everybody is unique, and there?s no exception when it comes to allergies. While some types of reactions are more common than others, which allergies you experience (and how your immune response presents) will be unique to you. The most common types of allergies include:
- Pollen Allergies – Sometimes called Hay Fever, allergies to pollen in the air can produce symptoms akin to the common cold, including sneezing and coughing.
- Food Allergies – Food allergies can range from mild to severe. Additionally, not all food must be ingested to cause a reaction. In some cases, topical application of the food can cause reactions as well.
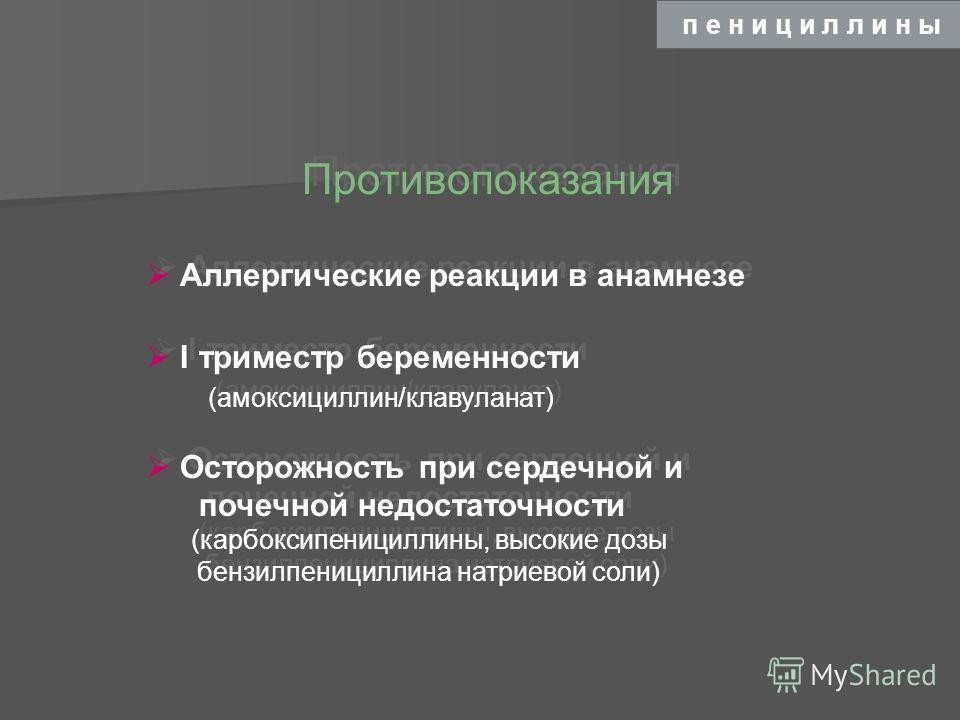
- Drug Allergies – Allergic reactions to drugs and pharmaceuticals can produce a wide range of impacts with varying severity.
- Pet Allergies – Pet dander is a leading cause of allergies. These allergies can sometimes intensify when you?re pregnant.
- Insect Allergies – Insect bites and bee stings can cause severe allergic reactions in some individuals.
- Mold Allergies – Mold spores in the air are usually not uncommon, but some specific types can cause mild to severe allergic reactions.
- Latex Allergies – Some people are allergic to latex, which can then cause skin irritation or other reactions.
What causes one type of allergy or another isn?t particularly well understood. Scientists don?t have a good answer for why one person might develop a pollen allergy and another person might develop a latex allergy. These allergies may also change significantly through your life–or they may remain static.
Scientists don?t have a good answer for why one person might develop a pollen allergy and another person might develop a latex allergy. These allergies may also change significantly through your life–or they may remain static.
What Are the Risks of Allergies During Pregnancy?
If you’re pregnant, allergies will generally pose very little risk to you or to your baby. Severe allergic reactions, such as anaphylaxis, will generally pose the most significant and severe risk that expectant mothers may need to consider. Anaphylaxis can be treated with an injection of epinephrine (an epi-pen), so it?s usually recommended that you carry one with you should you have known severe allergic reactions.
The two other risks that allergies pose are secondary in nature. Allergies can interfere with your sleep, nutrition, and health. Over long enough periods of severity, such interruptions could start to pose some health challenges. Likewise, there are some allergy medications that can present risks for your infant.
These risks, however, tend to be quite minimal. So assessing these risks will usually be performed on an individual basis, in conversation with your OB GYN or midwife. You can talk about your allergies, how severe those allergies typically become, and what you can do to treat your symptoms. Often, allergies are treated with antihistamines or steroid nasal sprays; while these treatments are usually safe, it?s still recommended that you discuss brand, dosage, and frequency of use with your OB GYN or midwife.
Additionally, you should always communicate any and all allergies to your healthcare providers, especially any drug allergies that you are aware of.
How Do You Treat Allergies During Pregnancy?
Many expecting mothers understandably want to avoid taking any medications that they don?t have to. When you?re treating allergies, this isn?t always possible. For example, if you can?t stop sneezing or have frequent headaches because of your allergies, treatment is desirable. After consulting with youR provider, you may try one of the following:
After consulting with youR provider, you may try one of the following:
- Prevention: The easiest way to avoid allergies is to stay away from anything that might trigger a reaction–even a mild one. One example would be keeping your dog in another room if you develop an allergy to canine dander. You should also avoid foods or medications that might cause a reaction. If you?re allergic to pollen, you can stay inside and keep the air conditioning running.
- Antihistamines: One of the most common treatments for allergy symptoms–especially those symptoms which resemble cold symptoms. However, not all antihistamines are chemically identical. Some pose fewer risks than others, especially during the first trimester. If you need to take antihistamines to manage your symptoms, make sure you speak to your healthcare provider or OB GYN first.
- Nasal sprays: A common way to treat allergies, nasal sprays are usually quite low risk.
 If you want to use a saline-based nasal spray, for example, you can do so without reservations. Using a steroid-based spray in accordance with directions is also usually okay. However, as with any medication, it?s a good idea to check with your OB GYN before taking nasal sprays.
If you want to use a saline-based nasal spray, for example, you can do so without reservations. Using a steroid-based spray in accordance with directions is also usually okay. However, as with any medication, it?s a good idea to check with your OB GYN before taking nasal sprays.
In general, pregnant women should avoid the following treatments:
- Decongestants: As a general rule, it is recommended that women avoid taking decongestants while pregnant. Certain decongestants can restrict blood flow to the placenta, which can cause unwanted complications. If you have taken a decongestant already, that?s okay–just be sure to touch base, especially before you take any more.
- Allergy shots: Allergy shots are a common way of controlling allergy symptoms. If you?ve already been taking allergy shots before becoming pregnant, it?s perfectly safe to continue. However, it?s generally recommended that this process not start while you are pregnant–this way your immune system stays as predictable as possible throughout your pregnancy.

Allergies can be a pain, especially when you?re pregnant and your body is a little unpredictable. However, they can be safely treated, so you don?t necessarily have to suffer with your allergies during pregnancy.
At NSAGO we offer comprehensive obstetrics care with OBGYNs and Nurse MIdwives. If you have questions about how you can treat allergy flare ups while you?re pregnant, contact our Wilmette or Glenview offices to schedule an appointment with an OBGYN or midwife.
Hives During Pregnancy: Causes, Treatment & Prevention
About 1 in 5 pregnant women experience changes in their skin during pregnancy, including acne, skin darkening, and stretch marks. Although women may feel self-conscious about these new “beauty marks,” skin changes during pregnancy are a normal occurrence. Hives during pregnancy are less common, but they do happen frequently.
Hives during pregnancy represent an allergic reaction to food, insect bites, medicine, chemicals, etc. With the increase in hormones and changes that happen in your body, it is possible that you become more sensitive to pathogens and experience hives while pregnant.
With the increase in hormones and changes that happen in your body, it is possible that you become more sensitive to pathogens and experience hives while pregnant.
What Causes Hives During Pregnancy?
As your belly grows to keep up with your growing baby, skin discomfort in the form of itchiness and dryness can occur. Pregnant women can face more serious bouts of itchiness, hives or rashes, and 1 in 150 pregnant women will develop a more serious skin condition known as PUPP.
Hives are caused by allergic reactions. The dryness and stretching of your skin along with other changes can make you more susceptible to experiencing hives during pregnancy. Hives can be caused by an allergic reaction to almost anything.
Some common causes of hives during pregnancy are noted below:
- Medicine
- insect bites
- chemicals
- pollen
- animal dander
- foods (i.e. dairy, nuts, shellfish)
Hives can be triggered or brought on by scratching stress, or pressure on the skin. It is important to take great care of your skin as to not aggravate or worsen the hives you experience.
It is important to take great care of your skin as to not aggravate or worsen the hives you experience.
Another condition that affects 1 in 50 women is cholestasis of pregnancy. This is a condition where intense itching is also accompanied by nausea, vomiting, and potentially jaundice. This condition can indicate there are problems with your liver. Should you see these signs or symptoms, it is important to contact your doctor immediately.
What is PUPP?
PUPP stands for pruritic urticarial papules and plaques of pregnancy. Women that develop PUPP will see outbreaks of red, raised patches on their skin.
The first site of the outbreak is generally the abdomen, but women with PUPP can see the condition spread to the arms and legs as well. Women with PUPP sometimes report extreme itching with these outbreaks.
Some research points to PUPP being linked to a genetic condition, as it seems to run in families, but ultimately, the cause of PUPP is still unknown. Generally, PUPP happens more often in a woman’s first pregnancy and is rarely seen in subsequent pregnancies.
Generally, PUPP happens more often in a woman’s first pregnancy and is rarely seen in subsequent pregnancies.
How Can I Treat Hives During Pregnancy?
Minor rashes can have a tendency to go away on their own. However, it is important not to scrub the affected area. Soap can aggravate the condition, so cutting back on the amount of soap you use can be beneficial.
One technique that could reduce the itchiness is taking an oatmeal bath or using baking soda in your bath. Keeping your skin well-moisturized can also help with the itching and dryness.
There are several antihistamines that are considered safe to take during pregnancy such as Allegra, Benadryl, and Chlor-Trimeton, Claritin and Zyrtec. It is important to review the warnings on any medication and consult your pharmacist and healthcare provider before taking any medication.
For more serious skin conditions like PUPP, doctors may prescribe oral medications or a variety of anti-itch creams.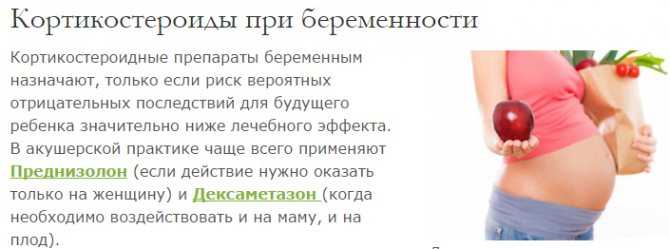
How Can I Prevent Hives During Pregnancy?
You might be someone who is more susceptible to hives in general. If that is the case, more than likely you know what foods or pathogens to avoid from previous experience.
Because you might be more susceptible and pregnancy tends to bring on dry and itchy skin, it is important to know steps you can take to prevent hives while pregnant. You at least want to know how you can minimize the hives you experience during pregnancy.
Here are some tips for minimizing or preventing hives during pregnancy:
- Avoid hot showers and hot baths (at least lower the temperatures)
- Avoid wearing tight fitted clothing
- Try not to scratch your skin as it itches
- Keep pressure off your skin
- Avoid stress and practice relaxation techniques
The above may not prevent all cases of hives, but it usually makes the cases of hives less severe and go away quicker.
Want to Know More?
- 7 Common Discomforts of Pregnancy
- How to Treat Itchy Skin Naturally During Pregnancy
Compiled from the following Sources
American Academy of Dermatology, (Accessed Oct 2014), Hives: Who Gets and Causes
National Institute of Health (access Oct 2014), Hives
Harms, R. (2004). Mayo Clinic guide to a healthy pregnancy (1st ed., pp. 480-481). New York: HarperResource.
(2004). Mayo Clinic guide to a healthy pregnancy (1st ed., pp. 480-481). New York: HarperResource.
Johnson, R. (1994). Mayo Clinic complete book of pregnancy & baby’s first year (1st ed., p. 17). New York: W. Morrow and Co.
| When an allergic girl prepares to become a mother, or when an allergy begins during pregnancy, the happy moments of waiting cease to bring joy. At such moments, expectant mothers face a difficult choice. On the one hand, you need to be especially careful in the use of drugs, but, on the other hand, you should not leave allergic reactions unattended. Can pregnancy cause allergies? Pregnancy itself cannot cause allergies. However, allergies, as in other stressful situations, may first appear during pregnancy. How complex biological changes during pregnancy affect the onset and course of allergies is not fully understood scientifically. Allergies: Hay fever. Almost one in five women suffer from hay fever during pregnancy. Since often the nose in pregnant women is blocked due to increased levels of estrogen, therefore, hay fever is exacerbated. Asthma. In 20% of women, asthma worsens during pregnancy. Good treatment of asthmatics is especially important, since this allergy can affect the lack of oxygen in a child. Eczema. Women who suffer from atopic dermatitis often experience an improvement in symptoms during pregnancy. But, for some women, pregnancy only exacerbates the symptoms. Rash (urticaria). Often occurs in pregnant women on a nervous basis. Sometimes you need to calm down and put your thoughts in order so that the allergy goes away. Anaphylactic shock. The immune system during pregnancy is prone to anaphylactic shock. Therefore, you should avoid possible allergens and consult a specialist at the first sign of an allergy. How does pregnancy affect allergies? In order for pregnancy not to be additionally aggravated by allergy symptoms, you need to contact a specialist. Pregnant women should try to avoid contact with allergic agents. Then it is possible to reduce medications or completely refuse them. Due to changes in hormone levels in the body of a pregnant woman, allergic rhinitis may increase throughout the period. Especially at the beginning of the second trimester of pregnancy, many women suffer from nasal congestion. More fresh air, sleeping with an elevated upper body, and a saline nasal spray can help. What are the treatment options for allergies during pregnancy? Despite certain limitations during pregnancy, methods for diagnosing and treating allergies are available. Skin tests should not be performed at this time, as the risk of anaphylactic shock, although minimal, is present. Instead, a blood test is preferred. Hay fever during pregnancy can be treated with nasal sprays. Immunotherapy or desensitization is a good way to treat the causes of allergies, that is, it is not only a way to remove the symptoms, but also to combat the causative agents of the allergy. Allergies should be especially carefully monitored and treated during pregnancy. To minimize the burden on the mother and her unborn child. At the first signs of an allergy, pregnant women should definitely contact an allergist. If anaphylactic shock is suspected, an ambulance should be called immediately. « Back |
Allergies in Pregnancy: Allergies in Pregnancy
Allergies are on the rise due to the increased prevalence and use of cosmetics, synthetics, disinfectants, and changing food and human diets.
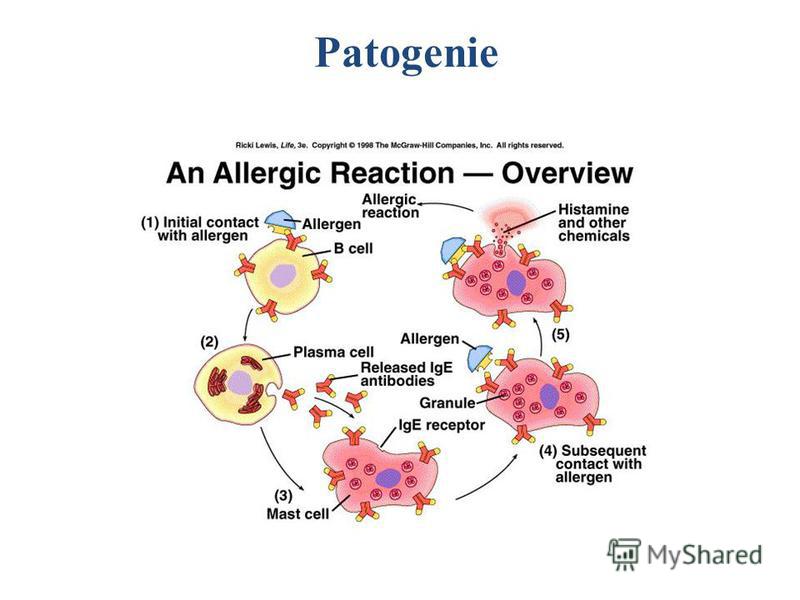
Allergic disease occurs when the body's immune system reacts to allergens when it comes into contact with them.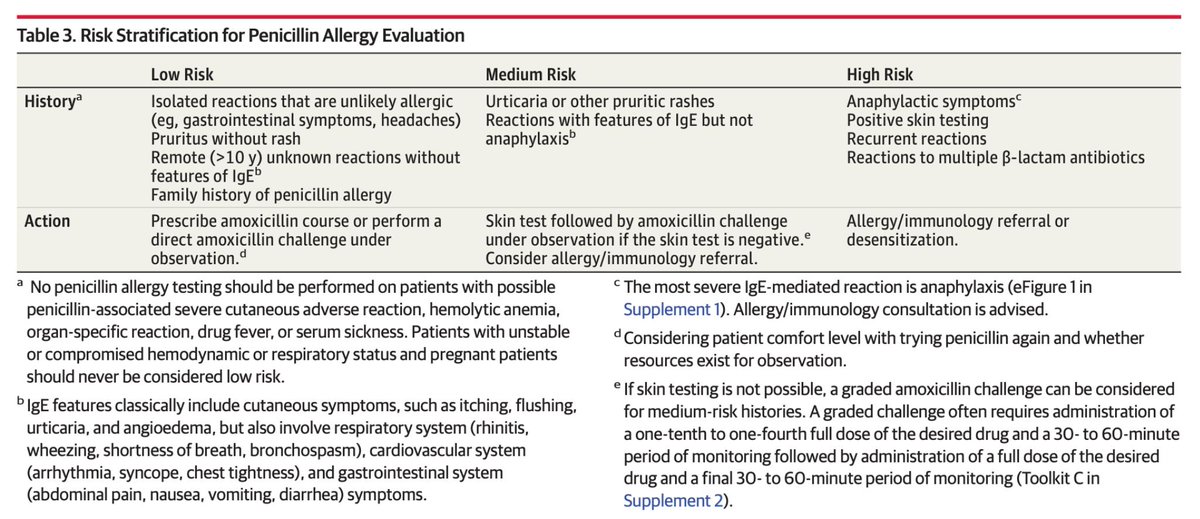 Allergic diseases also include acute allergies.
Allergic diseases also include acute allergies.
Among people susceptible to acute allergosis, from 5 to 20% of cases are pregnant. Pregnant women are most susceptible to this disease between the ages of 18 and 24.
Allergies in pregnancy - effects on the baby
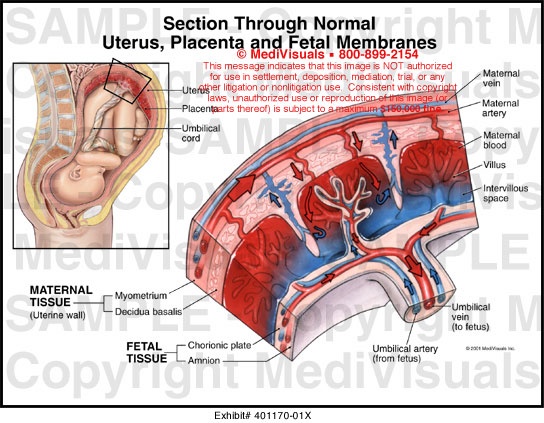
When allergies develop in pregnant women, they do not affect the fetus. This is due to the fact that immunocomplexes that react to an allergen that irritates the body cannot reach the fetus due to the placenta. Despite this, the fetus that is in the womb can be negatively affected by the disease due to three main reasons:
- When the mother's health condition changes.
- Medicines needed to treat when allergies occur during pregnancy may affect the reduction in uteroplacental blood flow. The process of supplying blood to the fetus is deteriorating.
- Drugs, other than the above effects, can have a bad effect on the fetus as a whole.
Treatment of allergies during pregnancy
Treatment should be started immediately, because only in this case the allergy does not have time to affect the fetus. Also, a very important task, which must be taken into account before starting treatment, is the maximum avoidance of harm that can be caused to an unborn child by drugs.
Also, a very important task, which must be taken into account before starting treatment, is the maximum avoidance of harm that can be caused to an unborn child by drugs.
When prescribing a course of treatment, a doctor should take into account the fact that the number of pregnant women who have diseases of the internal organs, according to statistics, reaches 45%. In addition, the proportion of women taking medication during pregnancy ranges from 60% to 80%. The average number of medications a woman takes during the entire pregnancy process is 4 different types. And this is without taking into account various vitamin complexes, dietary supplements and minerals. That is why a pregnant woman should never engage in self-treatment after discovering the first signs of an allergy in herself. You must immediately go to an appointment with a doctor who will provide qualified assistance and prescribe the correct course of treatment, as harmless as possible to the fetus.
The search for an allergy medicine in pharmacies, if necessary, after a doctor's prescription, can be done on our portal. There is all the information about each of them, and it is also possible to compare their cost.
There is all the information about each of them, and it is also possible to compare their cost.
When contacting an allergist for a consultation, a woman, in order to correctly diagnose and identify the allergen, will be subject to a special examination. A similar test involves preparing a solution that is made from the irritants that are believed to have caused the allergy. After that, a similar solution is injected into the skin of a pregnant woman in a small amount. If she is allergic to one of the irritants present in the solution, the area around the injection site will become swollen.
Where to get skin tests for allergies, as well as a laboratory blood test, you can find on our website. Here you can choose a profitable and convenient location option for yourself.
There are three stages in the development of allergies during pregnancy. The first entry of the allergen into the body. Immunity cells recognize the "enemy" and mechanisms for the formation of antibodies begin to work in the body. Second allergen exposure. The body is again exposed to allergens. There are processes that stimulate the production of histamine, which causes allergic symptoms. Third stage. Vessels expand, tissue permeability increases. This results in swelling and inflammation. A strong vasodilation is also possible, causing a sharp drop in blood pressure, i.e. anaphylactic shock occurs.
Second allergen exposure. The body is again exposed to allergens. There are processes that stimulate the production of histamine, which causes allergic symptoms. Third stage. Vessels expand, tissue permeability increases. This results in swelling and inflammation. A strong vasodilation is also possible, causing a sharp drop in blood pressure, i.e. anaphylactic shock occurs.
The result is an acute allergic reaction.
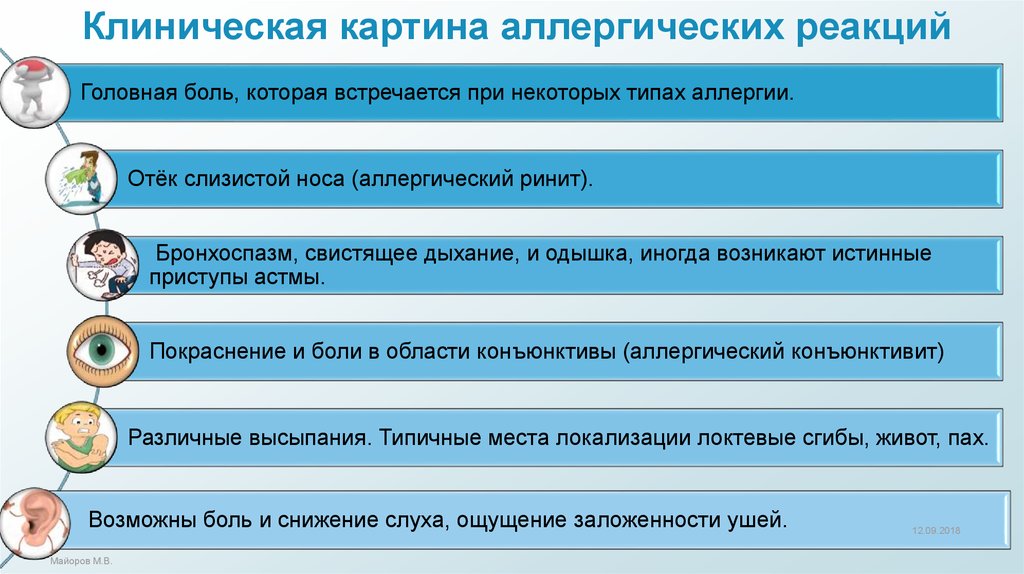
Acute allergosis:
- allergic rhinitis. Complication of breathing through the nose, its congestion, the mucous membranes of the nose swell, and an abundant secretion of mucous secretion appears, sneezing and burning in the throat occur;
- urticaria. Damage to a certain area of \u200b\u200bthe skin - the appearance of sharply defined blisters, accompanied by itching;
- redness, swelling, conjunctiva, itchy eyes, lacrimation, narrowing of the palpebral fissure.
Severe allergy:
- generalized urticaria.
 Involvement of all areas of the skin with symptoms of simple urticaria;
Involvement of all areas of the skin with symptoms of simple urticaria; - Quincke's edema. Edema of the skin, mucous membranes, and subcutaneous tissue. Basically, in the area of lips, cheeks, forehead, eyelids, hands, feet. Swelling of the larynx. Swelling of the gastrointestinal mucosa, accompanied by pain;
- anaphylactic shock. Arterial hypotension. Loss of consciousness, respiratory failure, swelling of the respiratory tract, urticaria, itching.
Quincke's edema, urticaria and rhinitis are most common in pregnant women.
What causes allergic reactions? Conventionally, three stages can be distinguished in their development. When a mother has allergic reactions, the fetus does not show any signs of allergy, because specific immunocomplexes that react to an allergen-irritant are not able to penetrate the placenta. However, in spite of this, a child in the womb may be affected by allergies for the following reasons:
- the mother's condition changes due to the onset of the disease;
- the influence of certain drugs that can cause a decrease in uteroplacental blood flow, which ensures the life of the fetus;
- the negative effect of drugs directly on the fetus.
So how to treat allergies in pregnant women? The most basic goal of treatment is the painless elimination of symptoms of pregnancy allergy without the risk of negative effects on the fetus. The reaction of the human body to taking various drugs largely depends on the general vitality, the type of therapy it undergoes, and the nature of the symptoms of the disease.
Pregnancy is a special, complex state of the body, because up to 45% of pregnant women can have diseases of the internal organs, and from 60 to 80% of expectant mothers who regularly take certain drugs in general. During the course of pregnancy, on average, according to surveys and observations, a woman can take up to four different medications, and this does not include vitamins, various nutritional supplements and minerals.
Habitual allergy pills, during pregnancy, for the most part, are contraindicated:
- Diphenhydramine taken late in pregnancy may cause uterine excitability or contractions when taken in doses greater than 50 mg;
- Terfenadine often causes weight loss in neonates;
- Astemizole has a strong toxic effect on the fetus;
- Suprastin (chloropyramine), cetirizine (Alleprtec), claritin (loratadine) and fexadine (fexofenadine) are acceptable during pregnancy, but only if the effect of treatment outweighs the potential risk to the child;
- Tavegil (clemastine) should never be used throughout pregnancy, except in cases of direct threat to the life of the pregnant woman;
- Pipolfen (piperacillin) is strongly discouraged during pregnancy and lactation.

If an allergy in pregnant women occurs for the first time, it is necessary to urgently contact an allergist. Separately, it is worth noting that during pregnancy, the primary task is to eliminate contact with the allergen, and not the symptoms of allergies.
To find out what may be an allergen in a particular case, a special examination is carried out.
What should be done in case of manifestation of OAS, and what drugs can be used:
- if the allergen is known, it must be eliminated immediately;
- consult a doctor;
- In the absence of the possibility of consulting a doctor, the following list of recommended drugs should be used.
1st generation of H2 blockers:
- Pipolfen (piperacillin) - not recommended during pregnancy or breastfeeding;
- Suprastin (chlorpyramidine) - can only be prescribed for acute allergic reactions during pregnancy;
- Allertec (cyterizine) - the drug can be taken in late pregnancy;
- Tavegil (clemastine) - during pregnancy is prescribed only in cases where an allergic reaction threatens the life of a pregnant woman, and for some reason there is no possibility of using other drugs.
 This is due to the negative effect of the drug on the fetus.
This is due to the negative effect of the drug on the fetus.
2nd generation H2-histamine blockers:
Claritin (loratadine) - during pregnancy, the use is allowed only if the expected effect of the treatment outweighs the potential risk to the child. The drug can be used only in cases where the disease state of the mother threatens the fetus more than taking this drug. This risk in each case must be assessed by a doctor.
3rd generation H2-histamine blockers:
Fexadine (fexofenadine) - during pregnancy, you can use it only in cases where the expected positive effect of therapy outweighs the potential risk to the child.
Prevention of allergic disease during pregnancy
Prevention of allergies is important, as it will help to avoid allergic disease and the effects on the fetus of drugs for its treatment. In order to prevent, it is necessary, first of all, to remove from the woman's food products that are characterized as highly allergic. This is primarily due to the fact that irritants most often enter through the gastrointestinal tract, and then penetrate to the fetus. Until about the 22nd week of intrauterine development in the fetus, the immune system completes its formation. It is after it becomes mature that hypersensitivity begins to develop. This means that after the 22nd week of pregnancy, a pregnant woman should review her diet and exclude from it foods that may be allergens for her.
This is primarily due to the fact that irritants most often enter through the gastrointestinal tract, and then penetrate to the fetus. Until about the 22nd week of intrauterine development in the fetus, the immune system completes its formation. It is after it becomes mature that hypersensitivity begins to develop. This means that after the 22nd week of pregnancy, a pregnant woman should review her diet and exclude from it foods that may be allergens for her.
Also, for the prevention of an allergic disease, one should not contact much with recently appeared products from the field of cosmetics and household chemicals.
Expectant mothers who have ever been exposed to an allergic disease should completely exclude the possibility of contact with those allergens that have caused an allergic reaction at least once before. In addition, it is recommended not to have pets, to clean the house, preferably wet and daily, to carry out a complete house cleaning weekly, which should include airing rooms, vacuuming carpets and beating, drying pillows.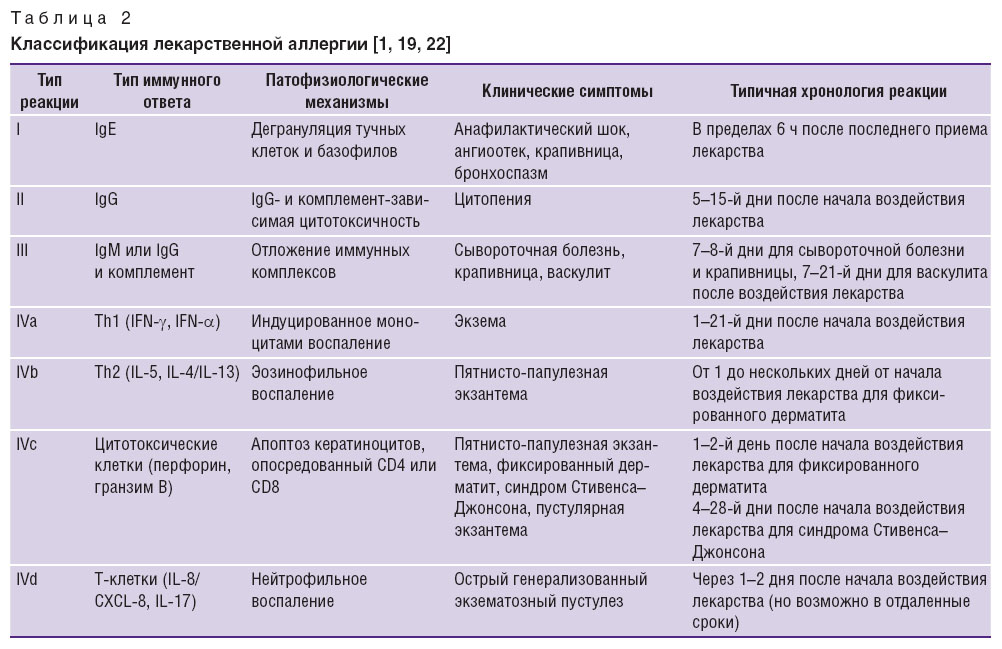
An important aspect of allergy prevention is fetal prevention. First of all, this is the restriction or refusal of the mother from highly allergenic foods. But since the child's immune system is not formed immediately, but only by the 22nd week of pregnancy, then, accordingly, the restriction in the use of highly allergenic foods makes sense from this period. Also, during the entire period of pregnancy, contact with household chemicals and new cosmetics should be limited.
If the expectant mother has never had allergies before, then she can consume risky foods, in small quantities, and not every day, of course. Otherwise, you will have to abandon entire product groups.
Separately, it should be noted that smoking for the expectant mother during pregnancy and lactation is strictly prohibited, because it affects the development of the respiratory tract and lungs of the fetus, and can cause intrauterine growth retardation. It is also known that after smoking just one cigarette, a spasm of the uterus occurs, which leads to a violation of the supply of nutrients and oxygen to the fetus, and this can last 20-30 minutes.
 An experienced doctor diagnoses the disease and prescribes treatment. Many allergy medications are not recommended for pregnant or breastfeeding mothers.
An experienced doctor diagnoses the disease and prescribes treatment. Many allergy medications are not recommended for pregnant or breastfeeding mothers.  Studies so far have not revealed the potential harm to the child from the use of such funds.
Studies so far have not revealed the potential harm to the child from the use of such funds.