Abdominal tearing during pregnancy
Abdominal separation (diastasis recti) | Pregnancy Birth and Baby
Abdominal separation (diastasis recti) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is abdominal separation?
Some women find their stomach muscles weaken and separate during and after pregnancy. This is known as abdominal separation, ‘diastasis recti’ or ‘recti divarication’. It is a common condition and often gets better in the first 8 weeks after having your baby.
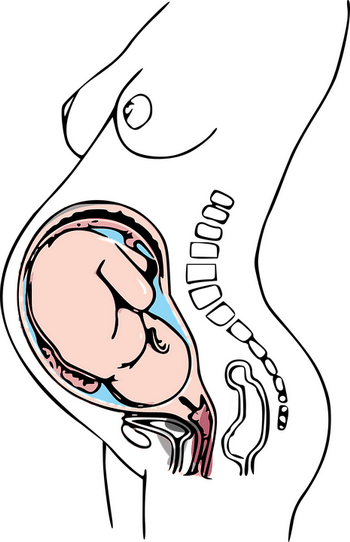
Abdominal separation occurs when the growing uterus causes the 2 long, parallel muscles of your stomach to separate from each other. These muscles run from your chest to your pelvis, just under the skin, down the middle of your belly.
Abdominal separation is partly due to the pressure of your growing baby, and partly due to the hormonal changes that take place during pregnancy. It usually starts in the second half of pregnancy.
Abdominal separation is more common in women who have had more than 1 child, are aged over 35 or who are having twins or triplets (or more). It can also occur in a small-statured woman who is having a larger-than-average baby.
It is sometimes known as ‘DRAM’ (diastasis of rectus abdominis muscle).
What are the signs and symptoms of abdominal separation?
If you have abdominal separation after the birth of your baby, you may be able to see a gap between the two bands of abdominal muscles. You can see this gap more clearly if you lie flat on your back and lift your head up.
You might also notice a physical canoe-shaped bulge in the middle of your stomach, especially when your abdominal muscles are active.
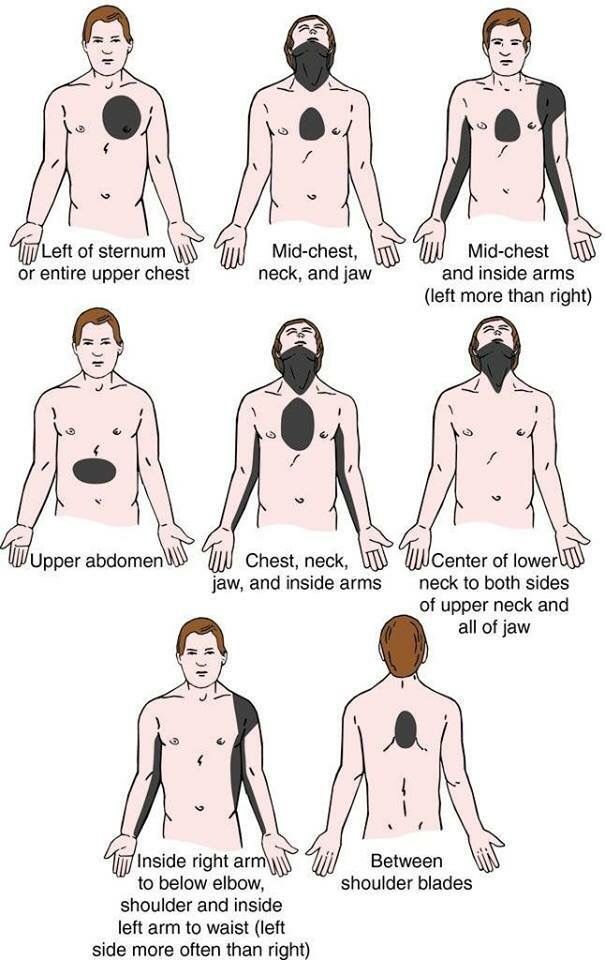
Some women with abdominal separation also get lower back pain, as the separation prevents the stomach muscles from supporting the back.
How is abdominal separation diagnosed?
Your GP, midwife or physiotherapist can check how big your abdominal separation is by measuring it with their fingers or a measuring tape, or by doing an ultrasound.
Does abdominal separation go away by itself?
Abdominal separation usually goes away after the birth of the baby. That said, up to 1 in 3 women still report problems with abdominal separation 12 months after the birth.
How can abdominal separation be prevented during pregnancy?
Strengthening your core muscles before you get pregnant or in the early stages of pregnancy might help prevent abdominal separation.
It’s best to avoid putting excess strain on your abdominal muscles while pregnant. Avoid sit-ups or planks. Try to avoid constipation and if you have a cough, get it treated.
How is abdominal separation after the birth treated?
It’s important to stop the separation from getting worse. Try these tips:
- Avoid lifting anything heavier than your baby.
- Roll onto your side when getting out of bed or sitting up.
- Choose gentle exercises (rather than intense ones) that strengthen the deeper stomach muscles.
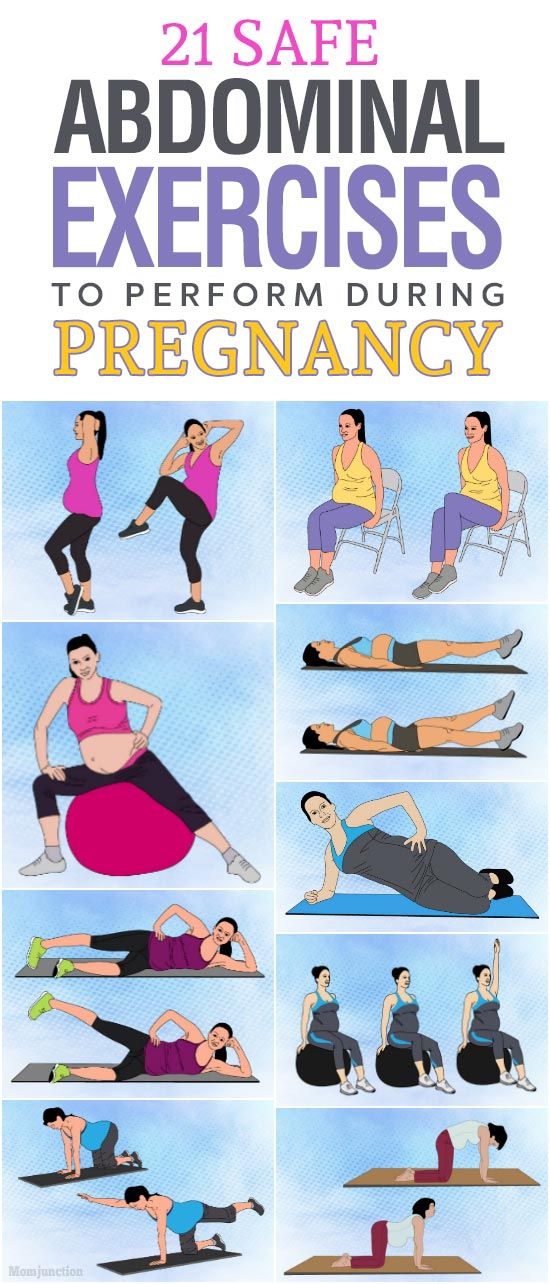
- Skip activities and movements that can make abdominal separation worse, such as sit-ups (crunches), oblique curls and some yoga poses (ask your GP, midwife or physiotherapist for advice).
You can also wear a supportive brace or compression underwear to help support your back and resolve the muscle separation.
There is a good chance that with time and care, the muscles will come back together. If that doesn’t work as well as you’d like, surgery after you’ve had your baby is an option.
Surgery often involves using stitches to repair the abdominal wall and reduce the gap between the muscles. This can improve quality of life and muscle strength, especially when separation is wider than 3cm.
Where to get help
If you notice anything unusual about your stomach muscles or experience any symptoms, see your GP, midwife or physiotherapist. You can find a physiotherapist near you using the healthdirect service finder.
You can also contact Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse.
Sources:
Royal Women’s Hospital (Abdominal muscle separation), Surgical Endoscopy (The general surgeon’s perspective of rectus diastasis), King Edward Memorial Hospital (Physiotherapy after childbirth), Pelvic Floor First (Re-thinking abdominal training in pregnant and postnatal women)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2020
Back To Top
Related pages
- Yoga and Pilates during pregnancy
- Looking after your body after having a baby
- Pelvic floor exercises
- Safe return to exercise after pregnancy
- Exercising during pregnancy
- Physiotherapy advice after pregnancy
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Why Ab Separation Happens and How It's Treated
Written by Stephanie Siegel
In this Article
- Dos and Don'ts
- Treatment
“Diastasis recti” means your belly sticks out because the space between your left and right belly muscles has widened. You might call it a “pooch.”
It's very common among pregnant women. About two-thirds of pregnant women have it.
Newborn babies also can have this belly spread, and it should go away on its own. Men can get it, possibly from yo-yo dieting, from doing sit-ups or weightlifting the wrong way, or from other causes.
Having more than one child makes this condition more likely, especially if they’re close in age. You’re also more likely to get it if you’re over 35 when pregnant, or if you’re having a heavy baby or twins, triplets, or more.
You’re also more likely to get it if you’re over 35 when pregnant, or if you’re having a heavy baby or twins, triplets, or more.
Pregnancy puts so much pressure on the belly that sometimes the muscles in front can’t keep their shape. "Diastasis" means separation. "Recti" refers to your ab muscles called the "rectus abdominis."
When the ab muscles move aside like this, the uterus, bowels, and other organs have only a thin band of connective tissue in front to hold them in place. Without the needed muscle support, a vaginal delivery could be more difficult.
The condition also can cause lower back pain, constipation, and urine leaking. It can even make it harder to breathe and to move normally. It's rare, but in extreme cases, the tissue may tear, and organs may poke out of the opening -- that’s called a hernia.
The muscle opening often shrinks after giving birth, but in some studies of women with diastasis recti, the muscle wasn't back to normal even a year later.
Dos and Don'ts
Don't strain. It can make matters worse. Constipation and lifting heavy things, including your kids, strain that connective tissue. Standing up and sitting down also count as heavy lifting in this case, because you’re lifting your body weight.
You push down when giving birth, but if done wrong, this action puts big pressure on the weak belly tissue.
Do be careful with exercise. Some routine fitness moves, including crunches, sit-ups, pushups, press-ups, and front planks, make abdominal separation worse. So can swimming, some yoga poses (like downward dog), and doing anything on your hands and knees. Some trainers may suggest those exercises for women with abdominal separation, not knowing what could happen.
Do heal your belly. Physical therapists don’t have one standard guideline on what moves will bring the belly muscles back into line. Some research found success with the Tupler technique. It involves certain exercises done while wearing a belly splint, which protects and holds the ab muscles together.
When the connective tissue has healed, some Pilates or other exercises may help you strengthen and rely more on your transverse (deep core) belly muscles instead of the outer ones. Not all Pilates or strengthening moves are good during pregnancy, though, so make sure you're working with a trainer who knows what "diastasis recti" means.
The best time to begin core strengthening is before you get pregnant, if you don’t already have an abdominal separation.
Before starting any exercises during or after pregnancy, be sure to ask your doctor what's OK for you to do and what's off-limits for now.
Treatment
If your abdominal separation is not too big, you may decide to live with it. But you should bring those muscles back together before you have another pregnancy.
Your doctor can measure how far apart your muscles are using finger widths, a measuring tape or instrument, or ultrasound. Then they can see whether it's getting better or worse.
Many women can close their belly gap by learning gentle movements to use while the abs are supported. Ask your doctor for advice. They may refer you to a physical therapist.
Ask your doctor for advice. They may refer you to a physical therapist.
If that rehab won’t work for you, maybe surgery will. An operation to correct diastasis may be called "abdominoplasty" or "a tummy tuck." The surgeon folds and sews together the weak central ridge.
It might be possible to get laparoscopy, which is surgery done with only small cuts instead of one large one. Scarring, infection, and other side effects are possible with any operation.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Diastasis of the rectus abdominis muscles and diastasis of the womb. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
— What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of connective tissue collagen. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
- The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and cartilage that connect the pubic bones suffer. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, this patient may experience rupture of the pubic symphysis and may require surgery to repair it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
The choice of method depends on the size and localization of the defect.
With symphysiopathy, therapeutic exercises reduce lumbar and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment of pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence.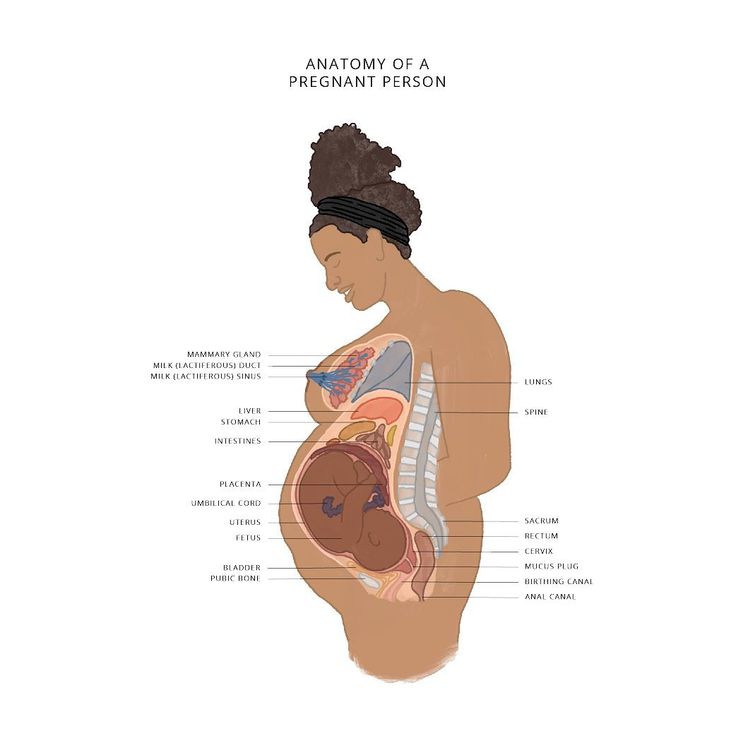 Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
The best advice for prevention, diagnosis and treatment: ask a competent doctor all the questions that worry you. Only the joint efforts of the doctor and the patient can overcome all problems and find the best solutions.
separation of abdominal muscles after childbirth
Almost every woman is faced with a divergence of the abdominal muscles after childbirth. Stretching occurs as early as the third trimester of pregnancy. And normally goes away on its own some time after the birth of the child. We understand why this happens, how to fix it and understand on our own that the muscles have dispersed.
What is diastasis rectus abdominis?
The muscular corset of the abdomen consists of rectus, oblique and transverse muscles, which are interconnected by tendons and a white line. The main function of the muscular corset is to support the abdominal organs, participate in some physiological processes, for example, in breathing, defecation and urination, and the work of the spine.
The linea alba is a large vertical tendon that connects the rectus abdominis muscles. Due to the large amount of dense collagen, it has a white color, because of which it got its name.
It has a maximum width (about 15 mm) in the upper abdomen and gradually narrows downward. Its main function is to provide movement and maintain the stability of the peritoneum.
If the white line loses elasticity and stretches, it can no longer perform its function and hold the rectus muscles together securely. This condition is called diastasis. Most often it develops for the following reasons:
- overweight;
- sharp weight loss;
- significant physical activity;
- prolonged cough;
- frequent constipation;
- connective tissue dysplasia.
However, most often diastasis occurs during pregnancy. According to statistics, from 70 to 100% of women face it in the later stages. Stretching of the white line during this period is considered a normal physiological state, which passes on its own some time after childbirth.
Stretching of the white line during this period is considered a normal physiological state, which passes on its own some time after childbirth.
What causes diastasis of the abdomen after childbirth?
Several factors influence the change in the abdominal muscles during pregnancy. Usually changes occur in the second half of this period and persist for several months after childbirth. As a rule, it does not require correction and goes away on its own when the muscles recover.
What affects the formation of diastasis during pregnancy?
| Type of change | Description |
| Hormonal changes | Hormones affect the elasticity of connective tissues and lead to their stretching. |
| Fetal growth | The volume of the uterus increases 500 times, which leads to weakening of the muscles and tendons. |
| Change in the load on the abdominal muscles | The growing fetus, firstly, affects intra-abdominal pressure. Secondly, it changes the load on the muscles themselves |
| Method of delivery | After natural childbirth, the body starts processes that shrink the uterus and reduce its volume. After a caesarean section, these processes are slower, which leads to a greater load on the muscles of the peritoneum. |
Most often, diastasis of pregnant women disappears on its own within a year after delivery. If the problem persists longer, consultation with specialists is necessary.
Important! A muscle strain of 20 mm or more is considered pathological and requiring intervention. If the changes are not so significant, doctors suggest monitoring the condition of the white line.
Is it possible to determine the pathology yourself?
The divergence of the rectus abdominis muscles does not have pronounced symptoms. However, you can see the manifestation of diastasis on your own with the naked eye. To do this, you need to tighten your stomach and see if there are protrusions or depressions in the middle of the abdomen.
Another self-diagnosis method that can be done at home. For this you need:
- Lie on your back.
- Bend your knees.
- Put one hand under the head, and the other on the stomach.
- Raise your upper body.
- Feel the middle of the abdomen for disappearances.
In rare cases, with a strong discrepancy, muscle support changes. Because of this, there are pulling pains in the lower back or heaviness in the lower abdomen. If these symptoms appear, you must definitely try to determine diastasis yourself. And if that doesn't work, see a doctor.
This disease is treated by a surgeon. He will conduct a visual inspection and manual diagnosis of muscle divergence. To confirm the diagnosis and determine the degree of discrepancy, he may prescribe computed tomography, x-rays and ultrasound of the abdominal organs.
He will conduct a visual inspection and manual diagnosis of muscle divergence. To confirm the diagnosis and determine the degree of discrepancy, he may prescribe computed tomography, x-rays and ultrasound of the abdominal organs.
If diastasis does not go away on its own, it is necessary to consult a doctor in order to choose a treatment and avoid the development of complications. Do not hesitate to contact our doctors with such a problem - they are in touch with you around the clock, which means they will tell you at any time what actions can be taken to eliminate muscle pathology.
What are the consequences of muscle separation?
Muscle divergence is not at all a harmless pathology or a cosmetic defect. The stretching of the white line affects the entire muscular corset of the abdomen and peritoneum. This leads to a variety of consequences. The main ones are:
- hernia of the umbilical ring and white line;
- frequent constipation;
- increased gas formation;
- nausea;
- disruption of the muscles of the diaphragm;
- urinary incontinence when coughing and sneezing;
- atrophy of the abdominal muscles;
- stagnant processes in the veins of the lower extremities;
- prolapse of internal organs;
- excessive stress on the spine.

Complications often occur with severe sprains of the white line and the divergence of the rectus muscles by more than 5 centimeters. In addition, in the absence of proper treatment, pathological processes can intensify, and muscle divergence increases.
Pay attention! Incorrect physical activity can increase stretching of the white line and divergence of the rectus muscles. This load includes almost any exercise on the press, so after childbirth they should be done with caution.
How to get rid of diastasis?
Normally, muscle discrepancy after childbirth is up to 25 mm. Such diastasis does not require treatment or correction and usually resolves on its own one year after delivery. However, in women who were born by caesarean section, this recovery process may take longer.
However, there are some ways to improve the condition of the white line and help the body recover faster. What can be done?
- Normal and varied food.

- Avoid foods that cause constipation.
- Exclude exercises on the press (lifting the body, twisting, bar).
- Add exercises to strengthen the abdominal muscles (vacuum, Kegel exercises, and so on).
- Wear a muscle-supporting bandage in the postpartum period.
With severe diastasis, a surgical operation to suture the white line is recommended. Abdominoplasty is performed according to indications. With its help, muscles are strengthened and the distance between them is reduced. With moderate stretching (up to 50 mm), minimally invasive methods are recommended through incisions and punctures of the white line, rather than abdominal surgery.
The operation is performed at least 12 months after childbirth and only if conservative methods have not helped to improve the condition of the rectus muscles and white line. It is better to plan the next pregnancy not earlier than one year after abdominoplasty.
In order not to miss the moment when normal recovery processes turn into pathological ones, it is better to constantly contact the doctor and consult with him about any changes in the condition of the abdomen. Our doctors will consult both by phone and by video link and will tell you about the methods of treatment and measures that will help to cope with diastasis.
Our doctors will consult both by phone and by video link and will tell you about the methods of treatment and measures that will help to cope with diastasis.
Are there ways to prevent diastasis after childbirth?
The stretching of the white line and the divergence of the rectus muscles is a normal physiological process, due to which pregnancy can develop normally and correctly. Therefore, it is impossible to prevent the development of these processes by 100%.
However, without preventive measures, there is a risk of a serious discrepancy (more than 50 mm) and the development of such unpleasant symptoms as pain and heaviness in the lower abdomen, incontinence, prolapse of organs.
The following measures will help reduce the severity of diastasis:
- Normalization of nutrition and avoidance of constipating foods.
- Refusal to lift weights during pregnancy.
- Physical education, which strengthens the muscles of the pelvic floor and the press.

- Wearing a special bandage that supports the abdomen after the 25th week of pregnancy;
- Weight control during pregnancy.
Any physical activity and diet should be discussed with your doctor. Some exercises can cause uterine spasm and adversely affect the fetus, so it is better not to self-medicate, but to discuss these issues with a gynecologist.
FAQ
Why does diastasis develop after caesarean section?
+
After a caesarean section, the hormonal processes that trigger uterine contractions are not as intense as after a natural birth. This leads to the fact that the muscles do not contract as actively, and recovery is slower. To speed up these processes after removing the stitches, it is recommended to wear a support bandage and refuse to lift weights.
Why is the divergence of the rectus muscles dangerous?
+
The rectus muscles provide the muscular corset of the peritoneum and are involved in many physiological processes (contraction of the diaphragm, urination, defecation, rotation of the body, and so on). When the white line is stretched, these processes are disrupted, which leads to pain, incontinence, prolapse of the internal organs, sagging and atrophy of the abdominal muscles.
When the white line is stretched, these processes are disrupted, which leads to pain, incontinence, prolapse of the internal organs, sagging and atrophy of the abdominal muscles.
Can diastasis go away on its own?
+
Yes, in most cases, diastasis does not require special treatment and resolves on its own a year after childbirth. However, in any case, a woman needs the supervision of a surgeon in the postpartum period, so as not to miss the moment when normal processes turn into pathological ones.
How to remove diastasis?
+
Treatment is required only in cases where the divergence of the muscles becomes more than 50 mm or the woman has complications that impair her quality of life. In this case, abdominal or laparoscopic surgery is recommended, during which the doctor stitches the rectus muscles and reduces the gap between them.
When can I download the press after childbirth?
+
Abdominal exercises - lifting the body, bending over, squatting, twisting - can increase postpartum muscle divergence. If the recovery is going well, then you can start the exercises already 6 months after the birth. If the diastasis does not decrease, it is better to wait up to 12 months or consult a doctor so that he can help you choose exercises to strengthen the abdominal muscles.
If the recovery is going well, then you can start the exercises already 6 months after the birth. If the diastasis does not decrease, it is better to wait up to 12 months or consult a doctor so that he can help you choose exercises to strengthen the abdominal muscles.
How to help the body recover faster after childbirth?
+
To strengthen the muscles of the press, special exercises of physiotherapy exercises (vacuum, cat, Kegel exercises and others) are recommended. In addition, it is recommended to choose a diet that normalizes the functioning of the gastrointestinal tract, prevents the development of constipation and contains a large amount of protein.
Can muscle divergence be prevented?
+
Divergence of the rectus muscles and stretching of the white line is a normal process that occurs during any pregnancy. The divergence rate is up to 25 mm. It becomes pathological in cases where the stretching is greater and leads to complications. For prevention, it is recommended to monitor weight, eat normally, not lift weights and wear a special supporting bandage.
For prevention, it is recommended to monitor weight, eat normally, not lift weights and wear a special supporting bandage.
Expert opinion
Diastasis, that is, the divergence of the abdominal muscles, is a physiological process that women experience during pregnancy. Normally, the abdominal muscles should recover on their own after childbirth. If the discrepancy persists for a long time, the woman is recommended corrective surgery. But as a rule, surgical intervention to get rid of diastasis is not required.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Art.
 If this did not happen, the growing fetus and uterus would not be able to fit in the abdominal cavity.
If this did not happen, the growing fetus and uterus would not be able to fit in the abdominal cavity.