7 months pregnant pain
7 Months Pregnant: Symptoms and Fetal Development
Now that you’re seven months pregnant, your little one is growing quickly and starting to look more and more like the baby you’ll soon meet. For example, she’s plumping up and her skin is becoming less transparent. Your belly is also growing, and you may face some physical challenges as a result. Try to keep in mind that every day that brings you back pain or tiredness also brings you one day closer to meeting your baby. Read on to find out what kinds of things may be in store this month from symptoms to baby development and more.
Common Pregnancy Symptoms at 7 Months Pregnant
You’re entering the third trimester — the home stretch! Around this time, it’s common to feel the effects of your growing tummy and progressing pregnancy. Symptoms at seven months pregnant can include:
Sciatica. As your uterus grows, it can put pressure on the sciatic nerve, which can then cause hip or lower back pain.
If the pain starts in your lower back or hip and travels down one leg, it could be sciatica, but only your healthcare provider can make a diagnosis. A hot or cold pack can help relieve the pain, and your provider can recommend stretches. If, at any time, you notice numbness in your legs or feet, let your provider know right away. Sciatica is likely to go away after your baby is born.
Pelvic pain. Pregnancy hormones do strange and unexpected things to your body. For example, they help loosen the joints that connect the two sides of your pelvis in preparation for labor and delivery. This can cause pelvic pain. If this strikes, try to stay off your feet as much as possible. Your healthcare provider can also give you stretches to do that may help ease your discomfort.
Constipation. Higher levels of the hormone progesterone and iron (if it’s in your prenatal vitamins) can slow digestion, making you feel blocked up. To help alleviate constipation, keep yourself hydrated (water and prune juice are great) and make sure you’re getting enough fiber in your diet.
 Good sources of fiber include beans, whole grains, fruits, and veggies.
Good sources of fiber include beans, whole grains, fruits, and veggies. Braxton Hicks contractions. Sometimes called practice contractions, Braxton Hicks contractions can begin in the second or third trimester. They sometimes feel like a slight tightening in your abdomen, and they usually go away when you move or change positions. They’re more likely to occur later in the day, and after physical activity like exercising or sex. Read up on Braxton Hicks contractions and speak to your healthcare provider if you’re unsure whether you’re experiencing practice or real contractions.
Fatigue. Some moms-to-be experience a boost of energy during the second trimester, but as you begin the third trimester, you may start to feel a little more tired. One reason for this is that by seven months pregnant your belly has grown quite a bit, and it may be more difficult to get a restful night’s sleep. Try to rest when you can — even if that means taking some time out during the day — and sleep on your side using a pillow to support your growing bump.
 Maintaining a healthy diet and moderate exercise routine can also help you sleep better and keep your energy levels up.
Maintaining a healthy diet and moderate exercise routine can also help you sleep better and keep your energy levels up. Bleeding or spotting. Some light bleeding or spotting can happen around this time. Although it may not be anything serious, check with your healthcare provider, just in case. Bleeding can sometimes be a sign of a problem, so consulting your provider can give you peace of mind.
How Is Your Baby Developing This Month?
When you’re seven months pregnant, your baby is busy developing those organs and systems that will help her survive outside the womb. For example, her lungs are starting to produce a substance called surfactant, which allows her lungs to expand and contract properly.
Other big news: your little one can now open and close his eyes! You’re probably eager to see those little peepers, and it won’t be long now! In the meantime, your baby may be able to sense changes in light and dark, and might respond to bright lights by moving or kicking. She’s also fattening up (becoming even more adorable), and this extra fat helps to smooth out the wrinkles in her skin. Her skin cells, meanwhile, are starting to produce melanin, which is a natural pigment that helps give skin its color.
She’s also fattening up (becoming even more adorable), and this extra fat helps to smooth out the wrinkles in her skin. Her skin cells, meanwhile, are starting to produce melanin, which is a natural pigment that helps give skin its color.
How Big Is Your Baby When You’re 7 Months Pregnant?
So, what’s your baby’s approximate size when you’re seven months pregnant? Your baby could weigh about 2.5 pounds and measure 14 inches at this time.
Related pregnancy tool
Fill out your details:
Pre-pregnancy weight (lbs.)
This is a mandatory field.
Height (ft.)
This is a mandatory field.
Height (in.)
Current week of pregnancy (1 to 40)
This is a mandatory field.
Tick the box
I'm expecting twins
What Does a Fetus Look Like at 7 Months?
Check out these illustrations for a glimpse at what your baby might look like when you’re seven months pregnant:
7 Months Pregnant: Your Body’s Changes
In your third trimester, you could gain as much as a pound a week. Using our Weight Gain Calculator, you can learn how to calculate your pre-pregnancy body mass index, or BMI (if you don't know that value already) and then get a basic overview of the weight gain ranges that might be acceptable for someone of your pre-pregnancy BMI. You can use the information you get to talk to your healthcare provider about the healthy pregnancy weight gain that’s right for you, and how to stay on track.
As your belly grows, and likely some time when you’re seven months pregnant, your healthcare provider will start to measure your fundal height. This is the distance between your pubic bone and the top of your uterus. This distance is measured in centimeters, and often corresponds closely to the week of your pregnancy. So, if you’re 28 weeks pregnant, it’s quite likely that your fundal height measurement will be something like 28 centimeters (11.02 inches), or very close to it. This measurement is just a tool to track your baby’s steady growth, and the measurements may not be exact for all moms-to-be.
This is the distance between your pubic bone and the top of your uterus. This distance is measured in centimeters, and often corresponds closely to the week of your pregnancy. So, if you’re 28 weeks pregnant, it’s quite likely that your fundal height measurement will be something like 28 centimeters (11.02 inches), or very close to it. This measurement is just a tool to track your baby’s steady growth, and the measurements may not be exact for all moms-to-be.
How Far Along Are You at 7 Months Pregnant?
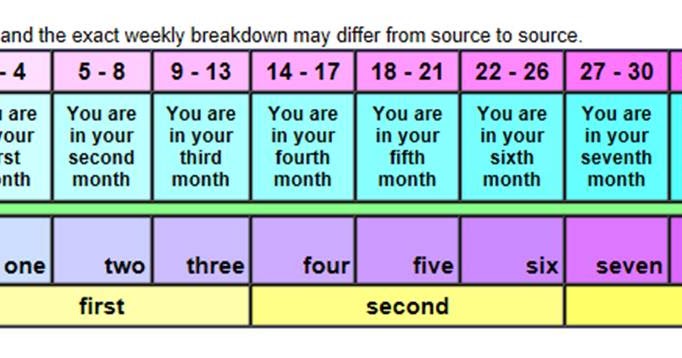
At seven months pregnant, it’s generally accepted that you’re at the very beginning of the third trimester. It's a little trickier to determine how many weeks seven months pregnant is. The weeks of pregnancy don’t fit neatly into months, so seven months can begin between 25 weeks and 27 weeks pregnant and extend up to 28 to 31 weeks.
Checklist for When You’re 7 Months Pregnant
If you have had a cesarean section before and would now like to try for a vaginal delivery, ask your healthcare provider whether you might be a good candidate for a VBAC (a vaginal birth after a cesarean delivery).

Consider whether you’d like to hire a labor support person called a doula and ask your healthcare provider or other moms in your area for recommendations.
Ask your healthcare provider about counting your baby’s movements at seven months pregnant. Download our Fetal Movement Tracker to help.
If you know and would like to share your baby’s gender before her birth, why not hold a gender reveal party this month? See our guide on planning a gender reveal party as well as our creative ideas for how to actually reveal your baby’s gender at the party.
If the search continues for the perfect baby name, try our Baby Name Generator for inspiration.
Download our Pampers Club app to learn how you can earn gifts and discounts on all those baby products you’ll soon be needing!
Put the finishing touches on your baby shower registry by checking our comprehensive list of registry must-haves to make sure you haven’t forgotten something important.

Consider whether you’ll store or donate your baby’s umbilical cord blood. Your provider can give you more information about your options.
If you are thinking of making a birth plan, download our Birth Plan Guide to help organize your thoughts.
If you’re starting to shop for baby gear items or would like more inspiration on what to add to your registry list, check out the best baby products as voted by Pampers Parents. We surveyed thousands of Pampers Parents to find out which specific items they love and recommend, and we reviewed all their favorites so you can make the right choice for you and your little one.
Sign up for even more weekly pregnancy tips here:
8 third trimester pains and how to deal with them | Your Pregnancy Matters
Congratulations! You’ve made it through the early pregnancy morning sickness and fatigue. Now it’s the third trimester and you’re so close to meeting baby. Unfortunately, there may be a few uncomfortable symptoms still in store for you.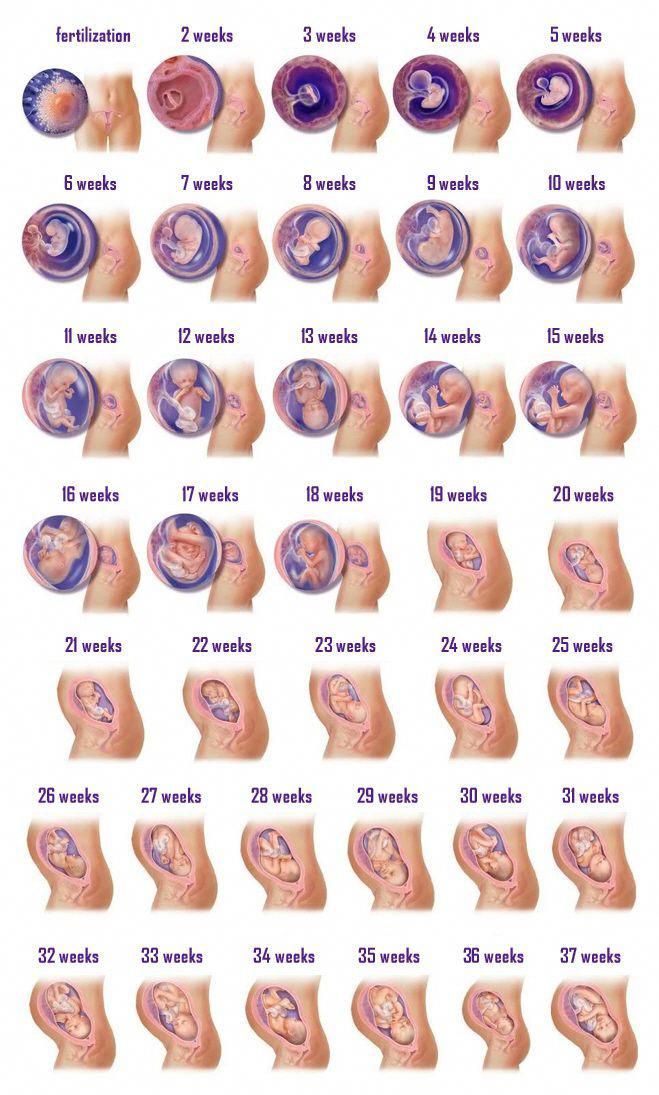
Swelling ankles, trouble sleeping, back pain, having to go to the bathroom every 20 minutes – these are all possibilities as you move into the pregnancy homestretch.
Patients often ask me how to make the third trimester a little more comfortable. This topic has been on my mind more in the last few months as my sister, Toral Patel, who is a neurosurgeon at UT Southwestern Medical Center, entered her third trimester and began dealing with some of these discomforts.
Let’s take a look at eight common symptoms during the third trimester of pregnancy: What causes them, how to help relieve them, and when you should call your doctor.
1. Swelling
Why it happens: When you hit 30 weeks of pregnancy, it may not just be your belly that’s swelling. You also may notice swelling (edema) in other parts of your body, especially in your lower extremities, such as your feet and ankles.
During pregnancy, your body produces about 60 percent more blood volume. Meanwhile, your growing uterus is putting pressure on the large veins that return blood to your heart, leaving all the extra fluid to pool in your lower limbs.
This pressure also may cause some veins to become swollen or look purple or blue. These are called varicose veins, and they should go back to normal after the birth of the baby.
What you can do: The best thing you can do to avoid or reduce swelling is to reduce how long you’re on your feet. If you have to stand for a long period of time, take a break every couple hours to sit down and put your feet up for 10 minutes. This helps gravity pull fluids from the legs back into your circulatory system.
One of the best times to put your feet up is after dinner. While you don’t have to have them straight up, get them as high as you can. I often tell patients to prop their feet up on a few pillows on the coffee table. I recommend doing this a few hours before bed because all those fluids that you’re helping return to the heart will be filtered by the kidneys and you’ll have to pee it all out. If you elevate your feet right before bed, you’ll likely have to get up right as you’re falling into a deep sleep to use the bathroom!
When you need to be on your feet for a long time, wear compression stockings, or TED hose. These can go from your feet up to your knees or mid-calves. They help move fluids up to the heart and keep them from pooling in your legs. If you’re picturing your grandma’s stockings, don’t worry. Many manufacturers are making much more stylish versions these days. You wouldn’t even know some of them are compression stockings!
These can go from your feet up to your knees or mid-calves. They help move fluids up to the heart and keep them from pooling in your legs. If you’re picturing your grandma’s stockings, don’t worry. Many manufacturers are making much more stylish versions these days. You wouldn’t even know some of them are compression stockings!
If your shoes are starting to feel tight, wear shoes with straps you can loosen. Or if it’s nice out, throw on some flip flops.
When to be concerned: If you notice sudden swelling, asymmetric swelling – such as one leg being larger than the other – or one calf being warm or tender to the touch, see your physician right away. These could be signs of a blood clot. Swelling in non-dependent parts of your body like hands and fingers may suggest the development of preeclampsia.
2. Insomnia
Why it happens: Insomnia – trouble falling asleep or staying asleep – often occurs in the first and third trimesters, although for different reasons. In the first trimester, it’s a result of hormonal changes, specifically due to a surge of progesterone. However, your progesterone levels off in the second trimester, returning you to peaceful slumber.
In the first trimester, it’s a result of hormonal changes, specifically due to a surge of progesterone. However, your progesterone levels off in the second trimester, returning you to peaceful slumber.
In your third trimester, sleep becomes more elusive because it’s difficult to get comfortable due to your growing belly.
What you can do: Find the position that’s most comfortable for you to sleep in, whether it’s your left or right side. It doesn’t matter which side you pick. Sleeping on your back is likely not comfortable, but if you want to sleep this way, it helps to shift your hips just a little to keep all the weight from being on your back.
There are a variety of body pillows you can try. My sister particularly liked the Snoogle pillow, which is C-shaped and goes up under the neck, around the shoulders, and between the legs.
Practice good sleep hygiene, such as not watching TV or looking at your phone right before you go to sleep. Other things you can try before going to bed are sipping warm milk or tea, taking a warm bath, or using lavender scents in your bath or lotion.
When to be concerned: If you’ve tried all of these things and you still can’t sleep, talk to your physician about which over-the-counter medications may be safe to take.
3. Reflux and feeling full faster
Why it happens: You may find that you can’t eat as much as you used to or that you’re experiencing reflux. As your uterus gets bigger, it begins to push up on your stomach. This means there just isn’t as much space for food. Also, the sphincter between your stomach and esophagus doesn’t work as well during pregnancy.
What you can do: Eat five small meals each day instead of three larger meals. Find foods that make you feel less full without lowering your caloric intake. For example, try a protein shake instead of a big sandwich.
If you’re having problems with reflux, avoid foods that are spicy or acidic. Instead, choose foods that are creamy, such as yogurt. Don’t eat within two hours of going to bed to allow foods time to leave your stomach prior to going to bed. Elevating your head and not lying flat also helps to avoid reflux.
Elevating your head and not lying flat also helps to avoid reflux.
When to be concerned: If you continue to have problems with reflux, talk to your doctor about an over-the-counter medication. If you are having reflux that is not related to something you ate, or you are experiencing heartburn or abdominal pain that doesn’t go away with medications such as Tums or Maalox, see your doctor. This could be an indication of a serious problem, such as preeclampsia.
4. Restless leg syndrome
Why it happens: Restless leg syndrome is a sensation of needing to move your legs. This can manifest in many ways, from a general feeling of discomfort to a burning or throbbing sensation. My sister said it made her feel like she needed someone to pull on her legs.
Restless leg syndrome is more common in the evening, making it impossible to fall asleep. While there are theories out there, we’re not 100 percent sure why restless leg syndrome affects so many pregnant women.
What you can do: There’s no real cure for restless leg syndrome, but there are lifestyle changes you can make to relieve the symptoms, including staying hydrated. We recommend pregnant women drink 80 to 100 ounces of water each day. Calcium and vitamin D supplements also may help.
Take a 20- to 30-minute walk around the time your legs are most restless to relieve the sensation. You also can try massaging the legs or using heat or ice packs.
When to be concerned: If these tricks don’t relieve your symptoms and your sleep is affected, talk to your doctor about medication.
5. Back and hip pain
Why it happens: Increased levels of progesterone during pregnancy relax the joints and muscles to accommodate the growing uterus and enhance flexibility in your pelvis so the baby can pass through the birth canal more easily. However, this also can cause pain.
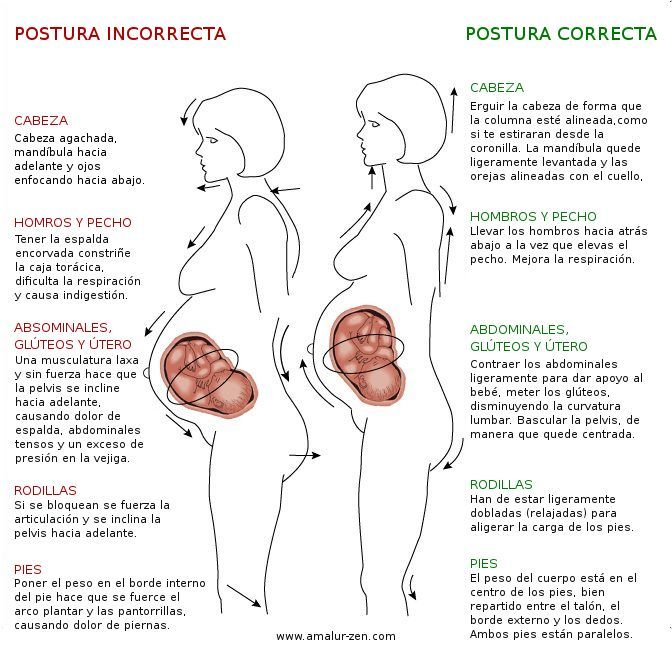
Your posture may change due to carrying extra weight around. You may find yourself leaning more to one side or another, which can lead to lower back or hip pain.
What you can do: Wear a support belt under and over the belly to take some of the weight off the hips and back. There are a wide variety of types and brands to choose from. This won’t hurt your baby, so tighten it enough to get the support you need.
When you sit down, place pillows under your hips or try sitting on a balance or yoga ball instead of a chair. Take a warm bath or use a heating pad on your hips or back to help relieve the pain.
Remember, thanks to your growing belly, your center of gravity is much different these days. Skip the stilettos until after you give birth.
When to be concerned: If you have unrelenting pain, a deep and sharp pain, or have become unable to walk or get up, see your doctor. Also, if you are experiencing a rhythmic pain in your low back every few minutes, it may be contractions, which sometimes present as low back pain.
6. Breast pain
Why it happens: Sore breasts are common during pregnancy. Hormonal changes are preparing them to feed your baby, and you may find you go up a few cup sizes.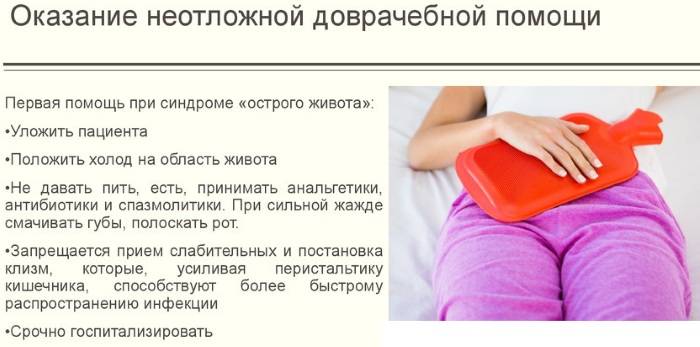 Women with smaller breasts may find they have more pain than women with larger breasts.
Women with smaller breasts may find they have more pain than women with larger breasts.
What you can do: I see too many women in their third trimester try to wear the same bras they did before pregnancy. Plan to buy new bras a couple times as your breasts grow throughout pregnancy – your breasts and back will thank you.
When to be concerned: Sports bras may be comfortable during and right after pregnancy, but if they are too tight, they can inhibit milk production. We advise women who don’t want to breastfeed to wear a sports bra to help dry up their milk. If you plan to breastfeed, make sure your bra has good support, but don’t let it get too tight.
7. Frequent urination
Why it happens: Needing to run to the bathroom frequently may be the most annoying part of the third trimester. The volume of fluids running through your kidneys doubles during pregnancy, meaning you will need to pee twice as much. As your baby grows, he or she also may press on your bladder.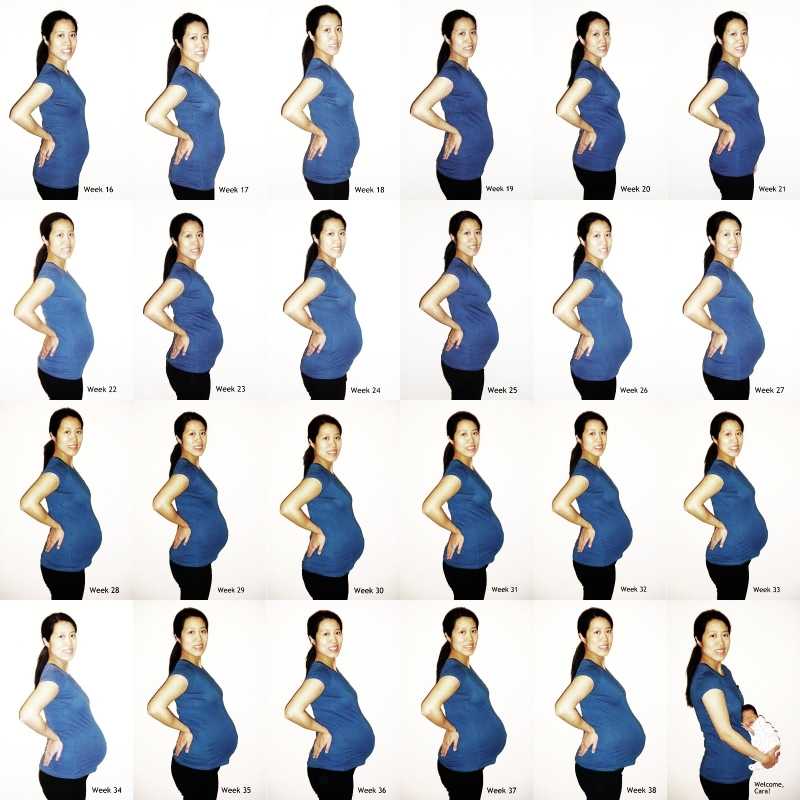
What you can do: Unfortunately, there’s not much you can do about this. Don’t stop drinking liquids in order to avoid frequent urination. You need to stay hydrated. Dehydration can cause contractions, dizziness, and lightheadedness.
Know you’re going to need to pee more often and prepare for it. For example, sit on the aisle or near the exit when at an event.
When to be concerned: Sudden changes in urination may be cause for concern, such as if you’re peeing far more today than you were yesterday. Also, if you experience pain or burning when you urinate, or if there is blood in your urine, see your doctor right away.
8. Lightheadedness and dizziness
Why it happens: Along with swelling, fluid pooling in your legs instead of circulating throughout the body can cause dizziness or lightheadedness. You may notice this more when you have been standing for a prolonged period of time or when you get up too quickly.
What you can do: Again, compression stockings can help by pushing blood out of the legs and to the heart. If you have to stand for a long time, keep moving to increase circulation – shuffle your feet or bend your knees by bringing your lower leg up toward your rear end a few times.
If you have to stand for a long time, keep moving to increase circulation – shuffle your feet or bend your knees by bringing your lower leg up toward your rear end a few times.
Avoid getting up too quickly from sitting and lying positions. When you’re ready to get out of bed in the morning, sit up, put your feet on the floor, and wait a minute before you stand up and go. This will give your body time to adjust. This is another instance in which staying properly hydrated will help.
When to be concerned: If you are constantly feeling lightheaded or dizzy, if it happens even after a short period of standing, or if it’s accompanied by a racing heartbeat, call your doctor.
The upside to dealing with all of these issues? You are getting close to the end of the pregnancy! We understand these problems can make the third trimester feel like it will never end. However, a few simple changes can make it a little more comfortable. And remember, it’s worth it. Just ask my sister, who gave birth May 6, 2016, to a perfect little boy, Elliott.
If you have questions about any third-trimester symptoms you are experiencing, request an appointment online or call 214-645-8300.
Abdominal pain during pregnancy
Abdominal pain in a pregnant woman can be felt for various reasons. In some cases, this is a natural reaction of the body to changes occurring in the body. In some - an alarming symptom that requires urgent medical intervention.
Consider the most common causes of abdominal pain in pregnant women.
Fatigue
The most obvious cause of pulling pains in the abdomen, especially in the later stages. Due to the weight of a growing belly, the body gets tired faster, and even habitual physical activity can cause fatigue, shortness of breath and pain. Naturally, this pain goes away during rest.
Ectopic pregnancy
If the fetal egg is not fixed in the uterus, but outside it, the pregnancy is called ectopic. After 2-3 weeks, the growing embryo begins to damage the surrounding tissues and organs - for example, a rupture of the fallopian tube often occurs. With this dangerous pathology, a woman's life is in danger, urgent hospitalization and surgical intervention are necessary. Therefore, it is very important to visit the antenatal clinic, where the doctor will determine whether the fetal egg is fixed in the uterus.
With this dangerous pathology, a woman's life is in danger, urgent hospitalization and surgical intervention are necessary. Therefore, it is very important to visit the antenatal clinic, where the doctor will determine whether the fetal egg is fixed in the uterus.
Growing pain
As the baby grows in the uterus, the uterus stretches. Most often, a woman does not notice this. But in some cases, the stretching of the uterus is felt and causes pain. Often this happens when the uterus is in hypertonicity. This reason is natural and practically not dangerous.
Compression of internal organs
A growing baby not only stretches the uterus, but also gains weight. In some positions, the uterus presses on adjacent organs, which also causes pain, especially when the child moves. Sometimes it is enough just to move, change the position of the body, so that the squeezed organ is released and the pain is gone.
Constipation
Due to changes in metabolism, as well as the weight of a growing belly, the intestines may not be active enough to perform their functions, and the pregnant woman suffers from constipation. A mild laxative will help ease the bowel and relieve pain.
A mild laxative will help ease the bowel and relieve pain.
Read in our media center: "What is the luteal phase." Find out why it is so important, what happens to a woman's body during the luteal phase and how it affects the skin.
Appendicitis
Not very often - about 1 in 10,000 pregnancies - the weight of the growing belly leads to inflammation of the appendix. Sometimes this inflammation goes away on its own, the woman does not even have time to understand what is the cause of the pain. But if the inflammation progresses, surgery may be needed. As with any inflammatory process, body temperature rises with appendicitis. In combination with the characteristic pains, the temperature gives a clinical picture that will allow the doctor to make a correct diagnosis.
Training contractions
In the third semester, pregnant women often experience rhythmic uterine contractions, which can be quite painful.![]() As a rule, they are safe. But if the contractions are strong, frequent and do not stop, you should call an ambulance.
As a rule, they are safe. But if the contractions are strong, frequent and do not stop, you should call an ambulance.
Placental abruption
This is an alarming symptom that is fraught with abortion. For various reasons, the placenta begins to exfoliate from the walls of the uterus. This is fraught with metabolic disorders of the fetus and spontaneous abortion. Usually, a woman notices spotting from the vagina. It is recommended to go to the hospital.
Miscarriage
Of all the listed causes of abdominal pain, this is one of the most dangerous. Spontaneous abortion can occur at any time, although in the first half it is called autoabortion, and in the later stages - premature birth. The fact that this is the cause of the pain can be recognized by a combination of several signs: pulling pains in the lower abdomen, spotting, preliminary contractions. Without medical assistance, the life of both the fetus and the mother is at risk.
What to do if you experience lower abdominal pain during pregnancy:
- Change body position: stand up or lie down, find a comfortable position.
- Remember what and when you last ate, when you emptied your bowels.
- Measure the temperature.
- Check for bloody or other discharge from the genitals.
- Determine if there are contractions.
If the pain is severe, accompanied by discharge, contractions and fever, call an ambulance.
If the pain is tolerable, disappears rather quickly, there is no discharge, it is worth telling the doctor about this at the next visit to the antenatal clinic.
Sign up for an appointment with a gynecologist
Familiarize the prices and services of
early stages and in the second trimester
from the moment the woman’s organism is rebuilt.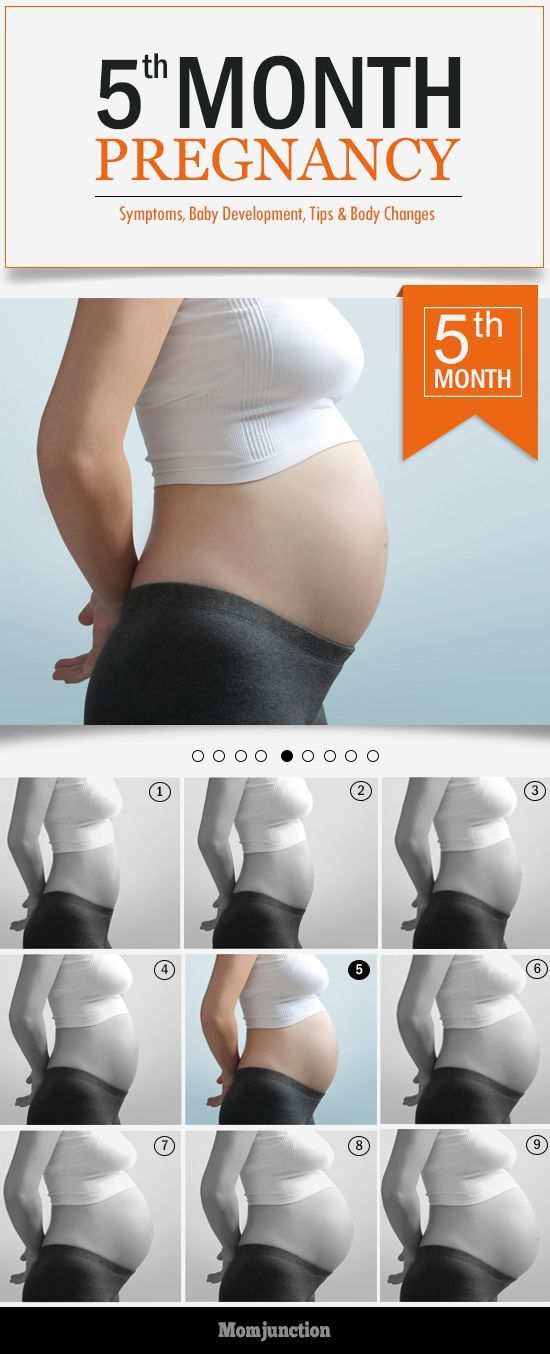 The composition of the produced hormones changes, nutrients are distributed between the mother and the fetus. At an early stage, these changes are invisible to others. But the woman notices that menstruation did not begin at the appointed time. Taste preferences change, nausea appears in the morning, fatigue, drowsiness, irritability or unusual peace. If you notice signs of pregnancy, you need to see a doctor. A few days after the delay in menstruation, pregnancy can be confirmed by laboratory tests. The doctor will give advice on how to prevent the development of pathologies and bear a healthy child.
The composition of the produced hormones changes, nutrients are distributed between the mother and the fetus. At an early stage, these changes are invisible to others. But the woman notices that menstruation did not begin at the appointed time. Taste preferences change, nausea appears in the morning, fatigue, drowsiness, irritability or unusual peace. If you notice signs of pregnancy, you need to see a doctor. A few days after the delay in menstruation, pregnancy can be confirmed by laboratory tests. The doctor will give advice on how to prevent the development of pathologies and bear a healthy child.
At the first appointment, the doctor will warn you about early symptoms that indicate a threat of miscarriage:
Lower back pain may occur during the first trimester of pregnancy. It is often encountered by women in the later stages.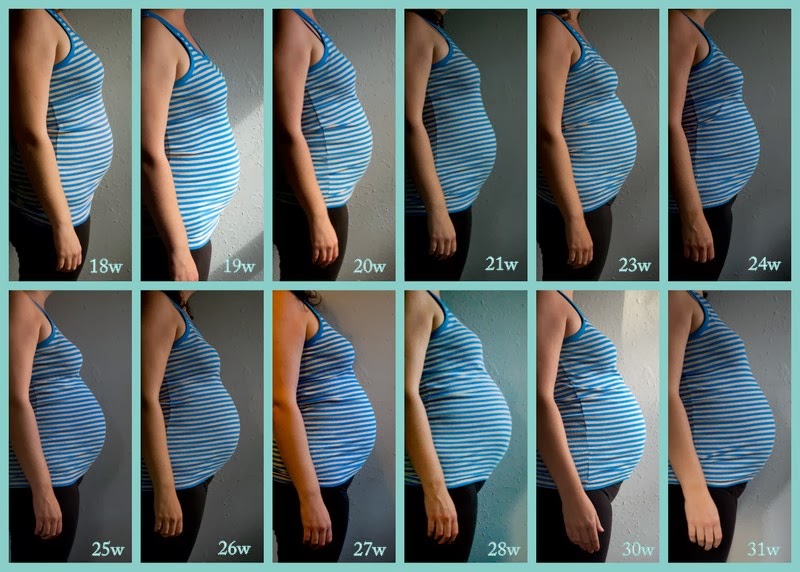 It arises due to increased weight and a shift in the center of gravity. But in the first trimester, the weight and size of the abdomen change slightly. You need to analyze your condition and understand if there is a danger.
It arises due to increased weight and a shift in the center of gravity. But in the first trimester, the weight and size of the abdomen change slightly. You need to analyze your condition and understand if there is a danger.
Causes that do not cause concern
Pulling the lower back during pregnancy can be due to various processes occurring in the body. Some of them create inconvenience, but do not pose a threat.
Attachment of the ovum to the uterus
Attachment of the ovum to the uterine wall occurs 5-7 days after fertilization, even before the woman notices a delay in menstruation and thinks about a possible pregnancy. The process may be accompanied by an increase in vaginal discharge. They are not white, but pink. Women often believe that menstruation begins. Due to the production of various hormones, a few days can pull the lower back. These sensations are caused by natural, not pathological changes in the body. They are harmless, do not require treatment and disappear after 5-6 days.
Changes in the circulatory system
After the attachment of the fetal egg in the uterus, the fetus begins to grow. He needs more nutrients and oxygen every day. To deliver them, the circulatory system begins to work differently, directing more blood to the uterus. Vessels from the pelvic area overflow, increase in volume and come into contact with the nerve endings in the lumbar region. There is a pulling pain. It is felt at 5-7 weeks of pregnancy. If the pain symptoms are not very pronounced, you can not worry. The body will rebuild, and the pain will pass without treatment.
Softening of joints, ligaments
During childbirth, the joints and ligaments in the spine and pelvis should be well stretched. The body prepares in advance for the upcoming work. He already at an early stage begins to produce the hormone relaxin, which softens the joints and ligaments. Due to a change in their density, it can pull the lower back.
Uterine growth
At 9-10 weeks of gestation, the volume of the uterus already noticeably increases. The woman feels that the lower abdomen has become more firm and convex. The growing uterus begins to come into contact with other organs. With increased sensitivity, its pressure can be felt at an early stage. But more often women experience discomfort, mild pressing back pain in the second trimester.
The woman feels that the lower abdomen has become more firm and convex. The growing uterus begins to come into contact with other organs. With increased sensitivity, its pressure can be felt at an early stage. But more often women experience discomfort, mild pressing back pain in the second trimester.
Braxton-Higgs contractions
At the end of the first and beginning of the second trimester, spontaneous uterine contractions may occur, resembling labor pains, but less intense. Drawing cramping pain is given in the lower back. They can periodically disturb 2-3 weeks. If there are no other dangerous symptoms, medication, restriction of motor activity is not required.
Drawing back pain in pregnant women often occurs from natural causes. They do not pose a threat to the health of the expectant mother and the development of the fetus, do not require treatment. But it is necessary to tell the doctor about them in the antenatal clinic. He correlates them with other symptoms and will not miss the signs of an incipient miscarriage, other pathologies.
Dangerous conditions
Drawing pain in the lower back is often one of the signs of dangerous conditions:
- missed pregnancy, threatened miscarriage;
- diseases of the genitourinary system;
- osteochondrosis;
- symphysite;
- colds.
Missed pregnancy, threatened miscarriage
In case of missed pregnancy, threatened miscarriage, lower back pain is accompanied by bloody discharge from the vagina, cramping or constant aching pain in the lower abdomen. This is a dangerous condition. You need to immediately go to the hospital or call an ambulance. Do not refuse if the doctor suggests treatment in a hospital. To stop an incipient miscarriage, you need to administer drugs intravenously, limit physical activity, and constantly monitor the condition of the woman and fetus.
In a miscarriage, tests should be done to make sure there are no fetal particles left in the uterus. This can cause a life-threatening inflammatory process or further infertility. Requires the introduction of drugs that enhance uterine contraction, relieve inflammation, or surgical intervention.
Requires the introduction of drugs that enhance uterine contraction, relieve inflammation, or surgical intervention.
Diseases of the genitourinary system
Immunity in pregnant women is weakened. Hypothermia, malnutrition, increased stress can cause kidney disease. If the lower back is pulled during pregnancy on one side, on the right or on the left, check the functioning of the genitourinary system. Additional symptoms indicate problems with the kidneys: legs and arms swell, pressure and temperature rise, and pain occurs when urinating. Women with chronic kidney disease should be especially careful. They can worsen when the load on the diseased organ increases - in the second or third trimester, with a cold or eating salty, spicy, smoked, fatty foods. You cannot self-medicate. Taking the usual antibacterial drugs (Canephron, Levofloxacin, Furadonin) is undesirable for pregnant women. You need to see a nephrologist. He will prescribe a safe treatment.
Osteochondrosis
Starting from 7-8 weeks, the hormone relaxin begins to be produced, softening the joints and ligaments. If before conception a woman suffered from osteochondrosis, scoliosis, kyphosis, an exacerbation of diseases is possible even in the first or second trimester. An additional risk factor is rapid weight gain.
If before conception a woman suffered from osteochondrosis, scoliosis, kyphosis, an exacerbation of diseases is possible even in the first or second trimester. An additional risk factor is rapid weight gain.
In women who have not previously suffered from osteochondrosis, it can develop in the later stages, when the spine is under a lot of stress due to a significant increase in body weight, a shift in the center of gravity, uterine pressure and softening of the joints and ligaments. The pain is pulling, exhausting, aggravated after a long stay in one position. With dystrophic tissue lesions, it can be felt on one side, left or right. Spinal problems can complicate childbirth. If you do not start treatment in a timely manner, do not engage in prevention, they will continue to progress after childbirth.
Symphysitis
If the production of the hormone relaxin is strongly activated, premature softening of the joints occurs, which can cause the pubic bones to diverge. This increases the risk of preterm birth. With the divergence of the pubic bones, the pain is shooting, sharp. She gives to the lower abdomen and lower back. There are swelling in the pubic area. To diagnose symphysitis, the doctor examines blood and urine tests, conducts an additional ultrasound examination, observes the dynamics of the development of the disease and decides on the possibility of natural childbirth or the need for a planned caesarean section. In the later stages, motor activity may be limited, strict bed rest is recommended.
This increases the risk of preterm birth. With the divergence of the pubic bones, the pain is shooting, sharp. She gives to the lower abdomen and lower back. There are swelling in the pubic area. To diagnose symphysitis, the doctor examines blood and urine tests, conducts an additional ultrasound examination, observes the dynamics of the development of the disease and decides on the possibility of natural childbirth or the need for a planned caesarean section. In the later stages, motor activity may be limited, strict bed rest is recommended.
Colds
Pregnancy increases the risk of complications from colds. Especially dangerous is the early period when the organs of the fetus are formed. A significant increase in temperature, infection, uncontrolled use of antibiotics can provoke serious pathologies.
Consult your doctor and start treatment at the first symptoms of a cold. Lower back pain and body aches can occur when the temperature rises. It passes if it is knocked down using traditional medicine recommended by a doctor. But if it hurts in the lower back on the right or left, the temperature rises to 39degrees, there was a strong cough, shortness of breath - pneumonia is possible. You need to call a doctor at home or an ambulance.
But if it hurts in the lower back on the right or left, the temperature rises to 39degrees, there was a strong cough, shortness of breath - pneumonia is possible. You need to call a doctor at home or an ambulance.
Prevention and treatment
If during pregnancy pulls the lower back, do not take painkillers. If the pain is severe, but examinations have not shown dangerous pathologies, consult a doctor. After studying the causes and symptoms of pain, he will choose safe ways to alleviate the condition.
In the first trimester, you need to be especially careful. A woman may still not know about pregnancy, but pain is already appearing. With a delay in menstruation, even for 2-3 days, you need to coordinate drug treatment with your doctor.
The second trimester is the time when a woman intensively gains weight and the load on the musculoskeletal system increases, pressure on the internal organs. The doctor will advise you to wear a bandage for pregnant women and other non-drug ways to relieve and prevent pain.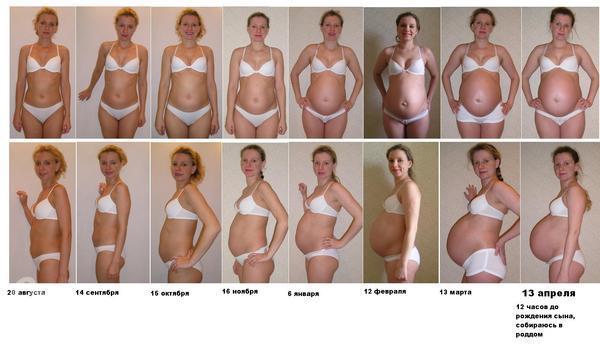
The third trimester - the body prepares for childbirth, the joints soften, the bones in the pelvic area diverge. If it pulls the lower back, the lower abdomen hurts, you need to lie down. If the pain intensifies, becomes cramping, childbirth may begin. If the period is less than 38 weeks, call the doctor who manages the pregnancy and describe the symptoms.
Prevention of pain in the lower back
To reduce the risk of lower back pain, the development of diseases of the musculoskeletal system:
- do not lift heavy loads, in the early term, power loads can provoke a miscarriage, in the late term - premature birth;
- do not wear tight shoes, shoes and boots with high heels, they create an additional load on the spine;
- watch your weight, no need to eat "for two";
- Eat more foods containing calcium, a mineral-vitamin complex recommended by your doctor;
- consult a doctor and start herbal medicine at the first sign of a cold, avoiding a significant increase in temperature;
- do not slouch, keep your back straight so that the load is distributed evenly;
- do not overwork, do not work for a long time in one position.