10 week blood test for down syndrome
Prenatal Testing for Down Syndrome | Patient Education
Down syndrome is a genetic condition caused by extra genes from the 21st chromosome. It results in certain characteristics, including some degree of cognitive disability and other developmental delays. Common physical traits include an upward slant of the eyes; flattened bridge of the nose; single, deep crease on the palm of the hand; and decreased muscle tone. A child with Down syndrome, however, may not have all these traits.
The incidence of Down syndrome in the United States is about 1 in 1,000 births. There is no association between Down syndrome and culture, ethnic group, socioeconomic status or geographic region.
Age-Related Risks
Generally, the chance of having a Down syndrome birth is related to the mother's age. Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350. At age 40, the odds are about 1 in 100.
Causes of Down Syndrome
There are three causes of Down syndrome:
Trisomy 21
An estimated 95 percent of people with Down syndrome have trisomy 21, meaning they have three number 21 chromosomes instead of two. We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
Translocation
Translocation occurs in about 3 to 4 percent of people with Down syndrome. In this type, an extra part of the 21st chromosome gets stuck onto another chromosome. In about half of these situations, one parent carries the extra 21st chromosome material in a "balanced" or hidden form.
Mosaicism
In mosaicism, the person with Down syndrome has an extra 21st chromosome in some of the cells but not all of them. The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
Prenatal Testing
Screening tests can identify women at increased risk of having a baby with Down syndrome.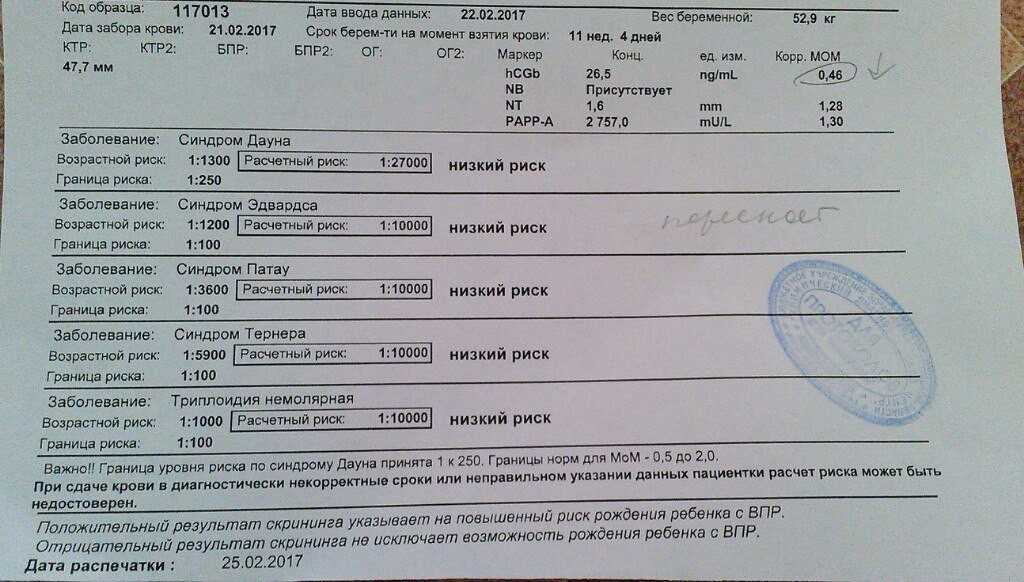 These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
Continue reading
Screening Tests
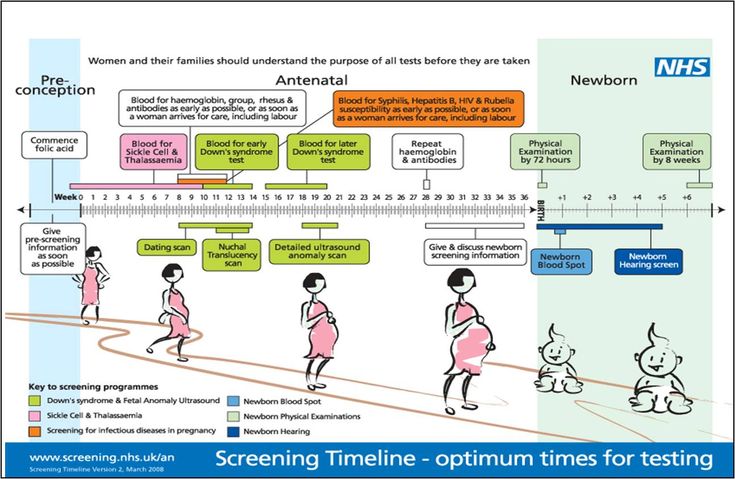
Sequential Integrated Screening — Sequential integrated screening is offered to all pregnant women by the state of California. This non-invasive screening is performed in two steps.
In the first step, which is performed between 10 and 14 weeks of pregnancy, a blood sample is taken from the mother and a nuchal translucency ultrasound is performed to measure the amount of fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.
The second step is a maternal blood test between 15 to 20 weeks of pregnancy. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome, an open neural tube defect or an abdominal wall defect.
Diagnostic Tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis — Amniocentesis is used most commonly to identify chromosomal problems such as Down syndrome. When the fetus is known to be at risk, it can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease.
An amniocentesis procedure for genetic testing is typically performed between 15 and 20 weeks of pregnancy. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small amount of amniotic fluid.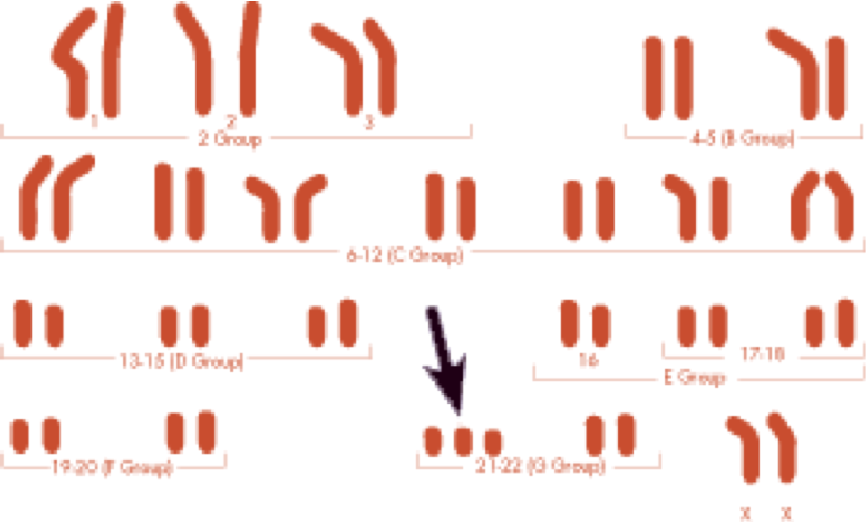 The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
Amniocentesis detects most chromosomal disorders, such as Down syndrome, with a high degree of accuracy. Testing for other genetic diseases, such as Tay-Sachs disease, is not routinely performed but can be detected through specialized testing if your fetus is known to be at risk. Testing for neural tube defects, such as spina bifida, also can be performed.
There is a small risk of miscarriage as a result of amniocentesis — about 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Chorionic Villus Sampling (CVS) — Like amniocentesis, chorionic villus sampling is used most commonly to identify chromosomal problems such as Down syndrome. It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses.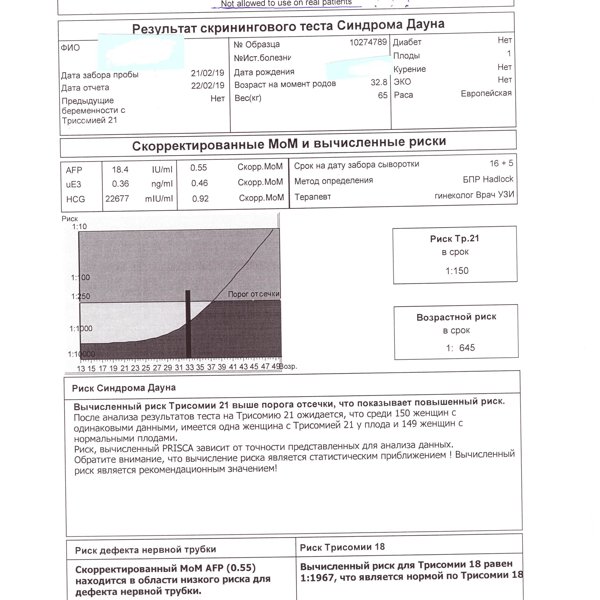 The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
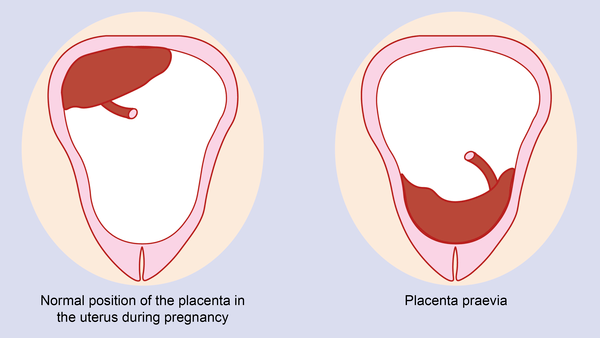
CVS involves removing a tiny piece of tissue from the placenta. Under ultrasound guidance, the tissue is obtained either with a needle inserted through the abdomen or a catheter inserted through the cervix. The tissue is then cultured and a karyotype analysis of the chromosomal make-up of the cells is performed. It takes about two weeks to receive the results.
The advantage of CVS over amniocentesis is that the test is performed much earlier in pregnancy, so results are typically available by the end of the third month. A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
There is a small risk of miscarriage as a result of CVS — 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.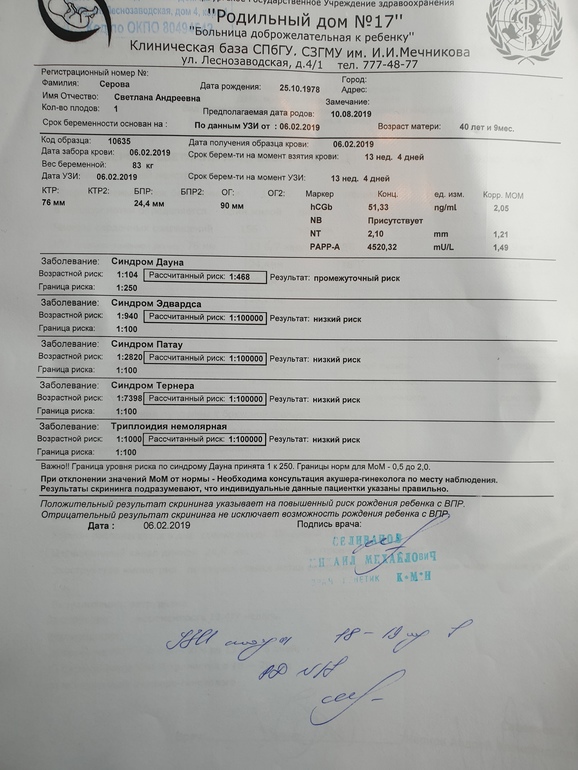
Ultrasound — The primary purpose of ultrasound is to determine the status of a pregnancy — the due date, size of the fetus and if the mother is carrying multiples. Ultrasound also can provide some information about possible birth defects in a fetus. All patients at UCSF Medical Center undergo a comprehensive ultrasound examination before any invasive tests are performed. Results of the ultrasound are explained at the time of the visit.
In some patients, an ultrasound raises concern of a possible abnormality in the fetus. We have extensive experience in performing and interpreting ultrasounds in pregnancy.
If You Receive a Positive Result
If you receive positive results on a screening test, we recommend that you discuss this with your doctor and a genetic counselor. Options for further diagnostic testing will be explained. The decision as to whether to have invasive genetic testing is up to you.
If a diagnostic test finds a genetic abnormality, the significance of such results should be discussed with experts familiar with the condition, including a medical geneticist and a genetic counselor, as well as your own doctor.
Gender blood test: What NIPT can tell you
- Pregnancy
- Health & Safety
By Karen Miles
|
|
March 16, 2022
The NIPT test is a noninvasive blood test that's available to all pregnant women beginning at 10 weeks of pregnancy. It screens for Down syndrome and some other chromosomal conditions, and it can tell you whether you're having a boy or a girl. NIPT is a screening test, so it's not definitive. If NIPT indicates a possible problem, experts recommend having CVS or amniocentesis to be sure.
Photo credit: iStock.com / chee gin tan
- What is NIPT?
- Benefits of NIPT
- Is the NIPT test conclusive?
- How does the NIPT test work?
- What does NIPT screen for?
- What does NIPT not screen for?
What is NIPT?
NIPT (noninvasive prenatal testing) is a blood test used to screen for Down syndrome and a few other chromosomal conditions.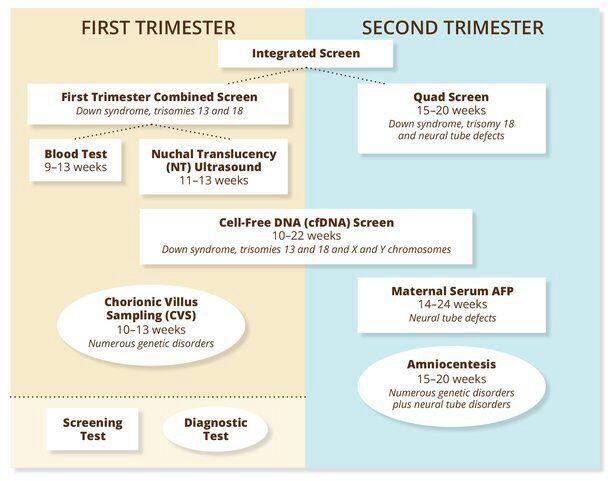 (It doesn't test for all chromosomal disorders.) NIPT is also known as cell-free DNA screening (cfDNA). Or you may have heard it called MaterniT21, a brand name.
(It doesn't test for all chromosomal disorders.) NIPT is also known as cell-free DNA screening (cfDNA). Or you may have heard it called MaterniT21, a brand name.
The test is available to all pregnant women, and some healthcare providers offer it to all of their patients. The cost varies widely, but most insurance plans cover at least a portion of the fee.
Some labs will use the NIPT to screen for additional conditions. Work with your provider or a genetic counselor to decide which conditions you want your baby to be screened for. While NIPT screening for some conditions is very accurate – and very helpful for many families – some of these added tests have high inaccuracy rates.
Benefits of NIPT
NIPT is a simple procedure that provides a lot of useful information. There are some good reasons why it's such a popular test:
- It's not invasive. A simple blood draw taken at a regular prenatal checkup is all you need. There's no need to schedule and take the time for an invasive procedure, like amniocentesis or CVS.
- It's perfectly safe for you and your baby and carries none of the potential risks of some other testing. (Amniocentesis and CVS carry a small risk of miscarriage, for example.)
- While you'll need follow-up diagnostic testing to confirm results, negative results provide a high degree of accuracy – and reassurance – for a number of conditions.
- It's available very early in pregnancy, at 9 to 10 weeks or later.
- Results are provided fairly quickly (within a couple of weeks, often sooner).
- If you want to know, the test can tell you if you're having a girl or a boy.
Is the NIPT test conclusive?
No, NIPT is a screening test, not a diagnostic test. That means the results don't indicate for sure whether your baby has a chromosomal condition. So, a "normal" NIPT result doesn't guarantee a healthy baby, and an "abnormal" result doesn't mean your baby definitely has a certain condition.
That said, when testing for the major conditions (see below), the NIPT test is very accurate – especially if you get a negative result.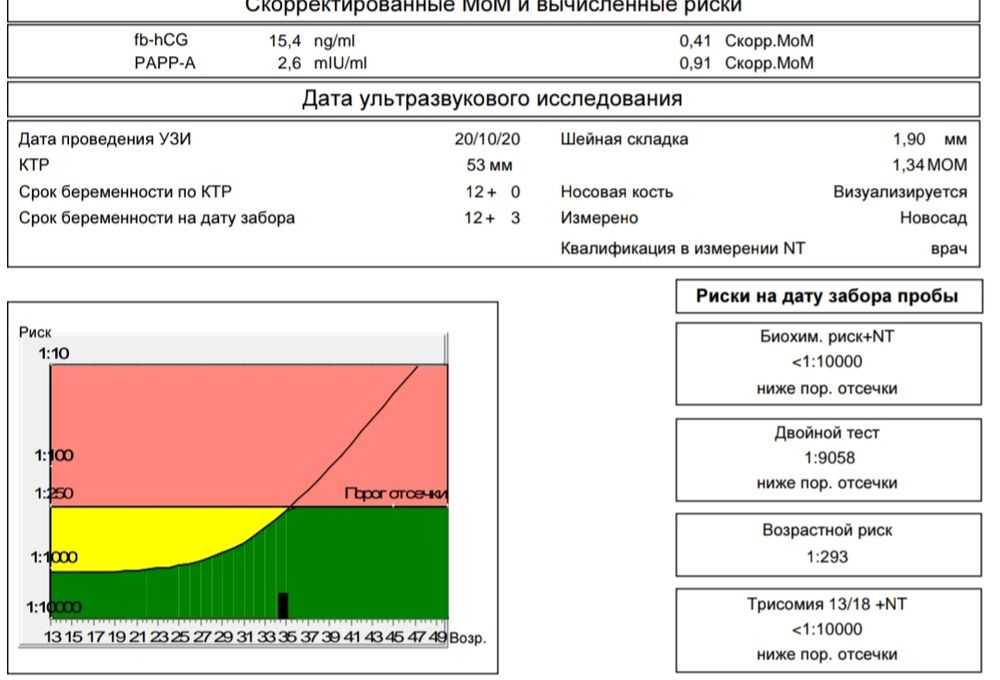
For example, when testing for Trisomy 21 (Down Syndrome), the negative result accuracy of the test is 99.5 percent. If you get a negative result, there's less than a 1 percent chance that it's incorrect. For Trisomy 18, the negative result accuracy is 97.7 percent, and for Trisomy 13 it's 96.1 percent. If you get a negative result for these conditions, there's a high likelihood that the test is correct and you can feel fairly confident that you don't need any further testing.
If you get a positive result, however, the accuracy is less reliable. That means you could get a "false positive" result that would be concerning and might lead you to have additional testing. For Trisomy 21, the chance of a positive result being correct ranges from 33 percent to 83 percent. (The accuracy range is a bit lower for Trisomy 18 and Trisomy 13.) Your more likely to get a false positive if you're at low risk of having a baby with a chromosomal condition. (Risk depends on factors such as your age and whether you have another child with the condition.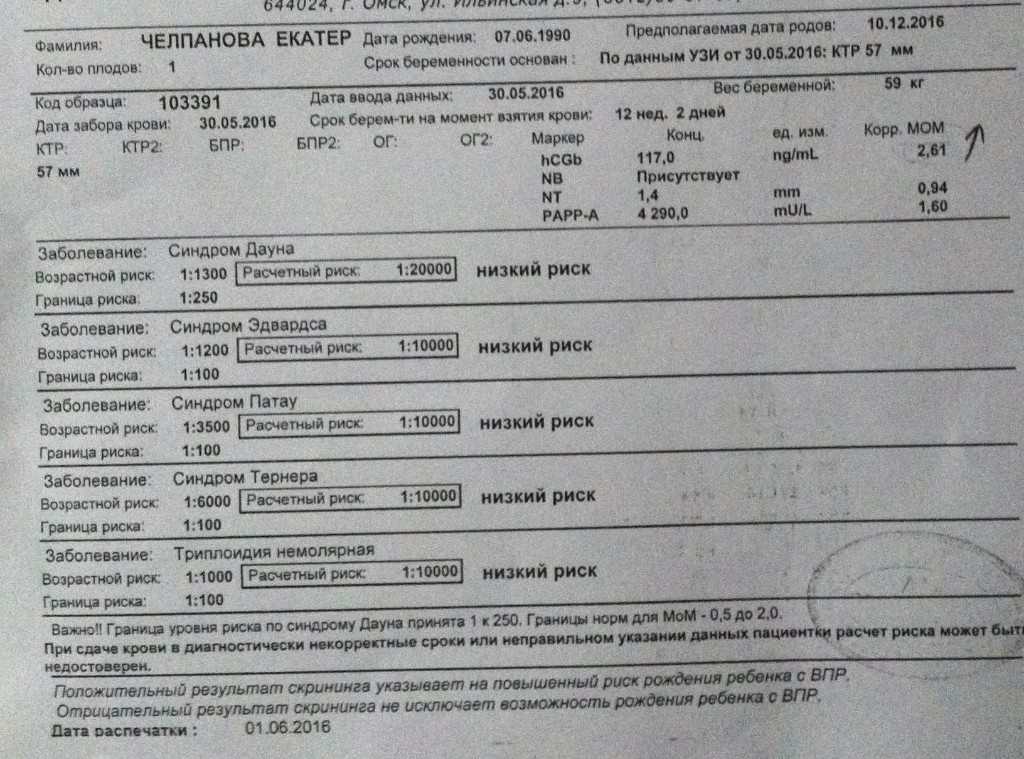 )
)
Occasionally (from 1 to 5 percent of the time) a test doesn't yield a result, perhaps because of insufficient fetal DNA in the sample taken. Your provider can review your options with you if this happens.
The NIPT may be less accurate for you if you:
- Are obese (have a BMI of 30 or higher)
- Are pregnant with multiples
- Are pregnant as a result of IVF
- Are taking certain blood thinners
Currently CVS and amniocentesis are the only two tests used to diagnose Down syndrome and other chromosomal conditions prenatally, so if NIPT indicates a possible problem, experts recommend having CVS or amniocentesis for a definitive diagnosis.
How does the NIPT test work?
You have a simple blood draw, and your blood sample is sent to a lab for analysis. The test counts fragments of DNA from your placenta that's circulating in your blood, so it contains cells from both you and your pregnancy. These fragments are free-floating rather than within cells, so they're called cell-free DNA.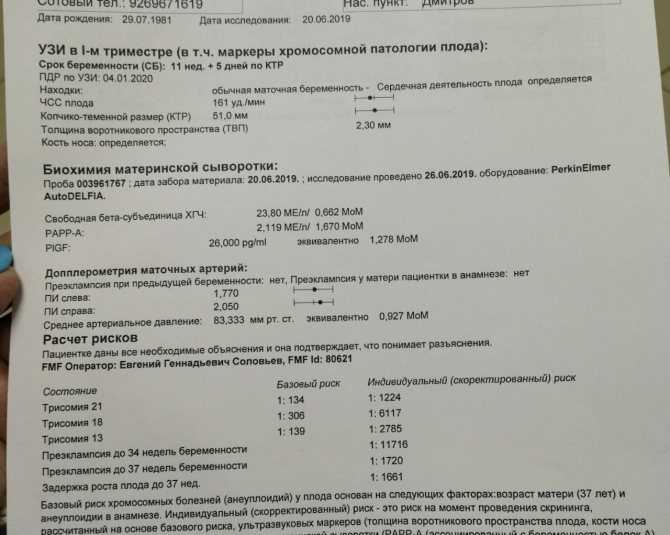
By examining the chromosomes (the part of cells that contain genes), doctors can tell if your baby is more likely to have certain disorders. There are normally two copies of a chromosome. If one of the pairs has an extra chromosome, it's called a trisomy. Down syndrome is also called trisomy 21 because there's an extra copy of chromosome 21, for example.
With all this examining of chromosomes, NIPT can also tell you what sex your baby is. Make it clear to your provider whether or not you want this information revealed to you when you get your results.
What does NIPT screen for?
The major conditions NIPT screens for are:
- Trisomy 21 (Down syndrome)
- Trisomy 18 (Edwards syndrome)
- Trisomy 13 (Patau syndrome)
- Common sex chromosome conditions, such as Klinefelter syndrome and Turner syndrome
Some labs may screen for a few other conditions as well, if you choose.
In many cases, the results of these tests are much less accurate than those for the conditions listed above – so if you're concerned about these, you may prefer to have definitive testing (an amnio or CVS).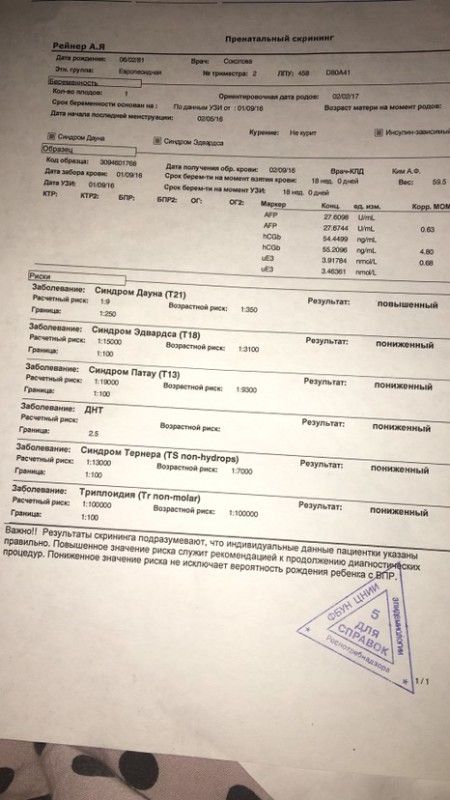
Added tests may include:
- Trisomy 16
- Trisomy 22
- Triploidy
- Sex chromosome aneuploidy
- Certain disorders caused by a small chromosomal deletion (microdeletion syndrome)
- Certain single-gene disorders
What does NIPT not screen for?
Conditions not screened for include:
- Neural tube defects
- Heart defects
- Abdominal wall defects
- Many other chromosomal and genetic disorders
NIPT only screens for some chromosomal conditions. CVS and amnio, on the other hand, can diagnose almost all chromosomal abnormalities. They can also be used to check for any of several hundred genetic disorders, such as cystic fibrosis, if you ask for these extra tests.
If you're feeling like there are a lot of testing options for you during pregnancy, you're right. Throughout pregnancy, you'll be offered tests to check on you and your growing baby. Our prenatal testing article provides a good rundown of those tests.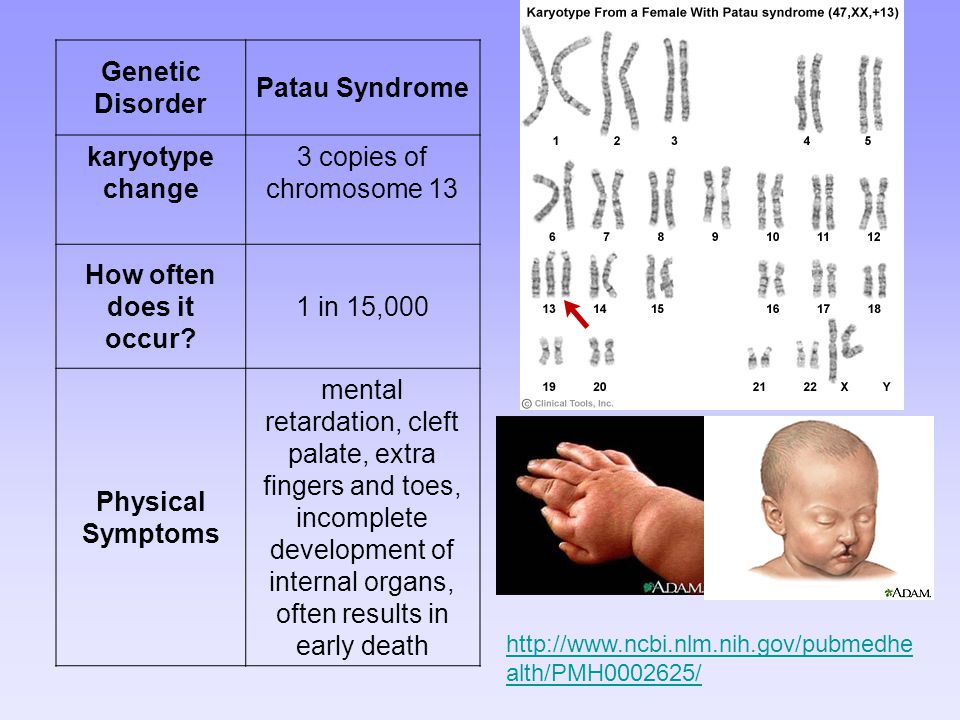
Learn more:
- Your pregnancy week by week
- When will my pregnancy start to show?
- How to have a healthy pregnancy and baby
Sources
BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies.
ACOG. 2019. Cell-free DNA prenatal screening test. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/infographics/cell-free-dna-prenatal-screening-test [Accessed March 2022]
ACOG. Reaffirmed 2021. Cell-free DNA to screen for single-gene disorders. The American College of Obstetricians and Gynecologists.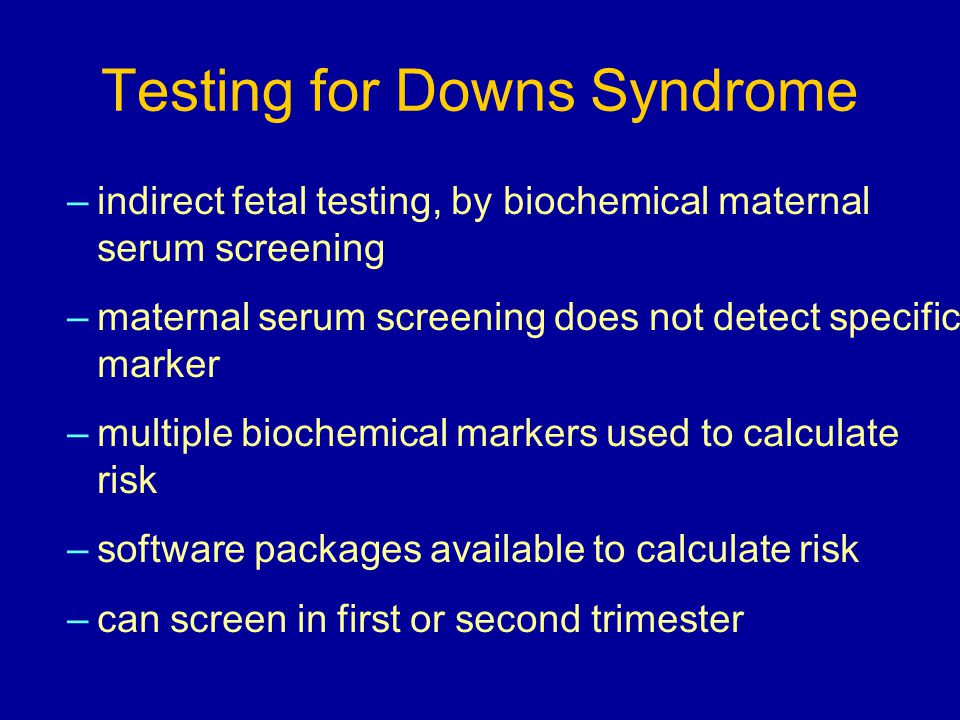 https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2019/02/cell-free-dna-to-screen-for-single-gene-disorders [Accessed March 2022]
https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2019/02/cell-free-dna-to-screen-for-single-gene-disorders [Accessed March 2022]
ACOG. 2021. Prenatal genetic screening tests. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/prenatal-genetic-screening-tests [Accessed March 2022]
Mackie FL et al. 2016. The accuracy of cell-free fetal DNA-based non-invasive prenatal testing in singleton pregnancies: A systematic review and bivariate meta-analysis. BJOG 124 (1): 32-46. https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/1471-0528.14050 [Accessed March 2022]
Mayo Clinic. 2020. Prenatal cell-free DNA screening. https://www.mayoclinic.org/tests-procedures/noninvasive-prenatal-testing/about/pac-20384574 [Accessed March 2022]
MedlinePlus. 2021. Prenatal cell-free DNA screening. https://medlineplus.gov/lab-tests/prenatal-cell-free-dna-screening/ [Accessed March 2022]
MedlinePlus. 2021.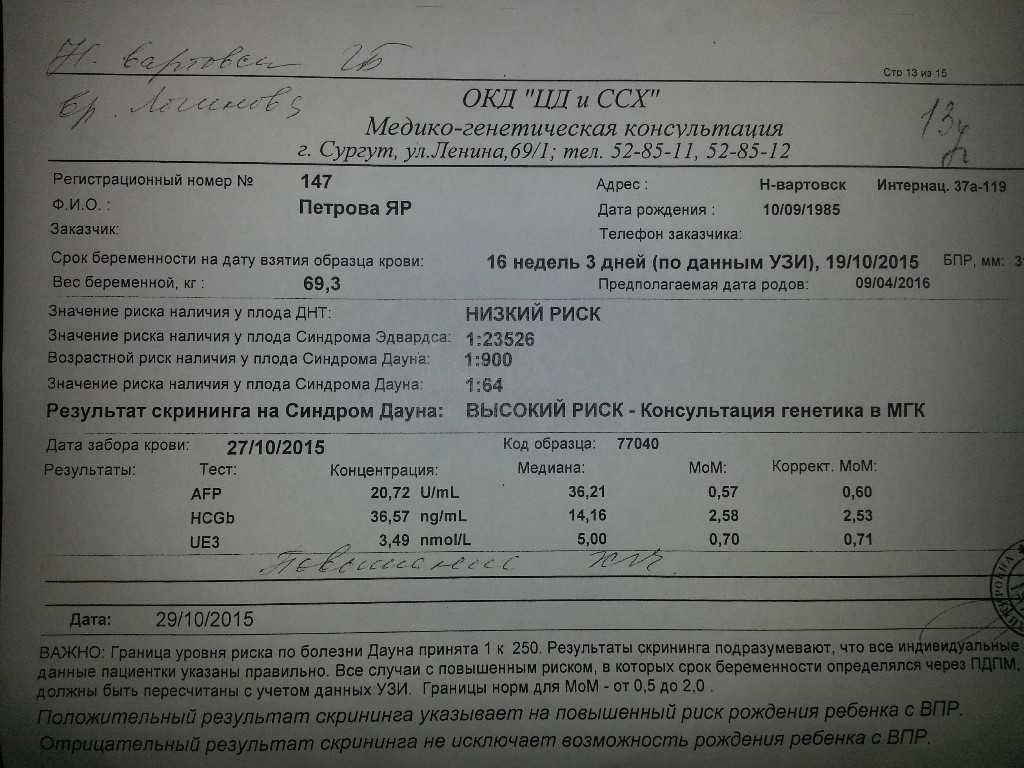 What is noninvasive prenatal testing (NIPT) and what disorders can it screen for? https://medlineplus.gov/genetics/understanding/testing/nipt/ [Accessed March 2022]
What is noninvasive prenatal testing (NIPT) and what disorders can it screen for? https://medlineplus.gov/genetics/understanding/testing/nipt/ [Accessed March 2022]
SMFM. Undated. Cell free DNA screening is not a simple blood test. https://www.smfm.org/publications/183-cell-free-dna-screening-is-not-a-simple-blood-test [Accessed March 2022]
SMFM. Undated. SMFM statement: Maternal serum cell-free DNA screening in low risk women. https://www.smfm.org/publications/157-smfm-statement-maternal-serum-cell-free-dna-screening-in-low-risk-women [Accessed March 2022]
Soukkhaphone B et al. 2021. Non-invasive prenatal testing for the prenatal screening of sex chromosome aneuploideies: A systematic review and meta-analysis of diagnostic test accuracy studies Molecular Genetics & Genomic Medicine 9 (5): e1654. https://onlinelibrary.wiley.com/doi/full/10.1002/mgg3.1654 [Accessed March 2022]
Show more
advertisement | page continues below
advertisement
Featured video
All pregnancy, parenting, and birth videos >
Screening tests for Down syndrome in the first 24 weeks of pregnancy
Relevance
Down's syndrome (also known as Down's disease or Trisomy 21) is an incurable genetic disorder that causes significant physical and mental health problems and disability. However, Down syndrome affects people in completely different ways. Some have significant symptoms, while others have minor health problems and are able to lead relatively normal lives. There is no way to predict how badly a child might be affected.
However, Down syndrome affects people in completely different ways. Some have significant symptoms, while others have minor health problems and are able to lead relatively normal lives. There is no way to predict how badly a child might be affected.
Expectant parents during pregnancy are given the opportunity to have a screening test for Down syndrome in their baby to help them make a decision. If a mother is carrying a child with Down syndrome, then a decision should be made whether to terminate the pregnancy or keep it. The information gives parents the opportunity to plan life with a child with Down syndrome.
The most accurate screening tests for Down syndrome include amniotic fluid (amniocentesis) or placental tissue (chorionic villus biopsy (CVS)) to identify abnormal chromosomes associated with Down syndrome. Both of these tests involve inserting a needle into the mother's abdomen, which is known to increase the risk of miscarriage. Thus, screening tests are not suitable for all pregnant women.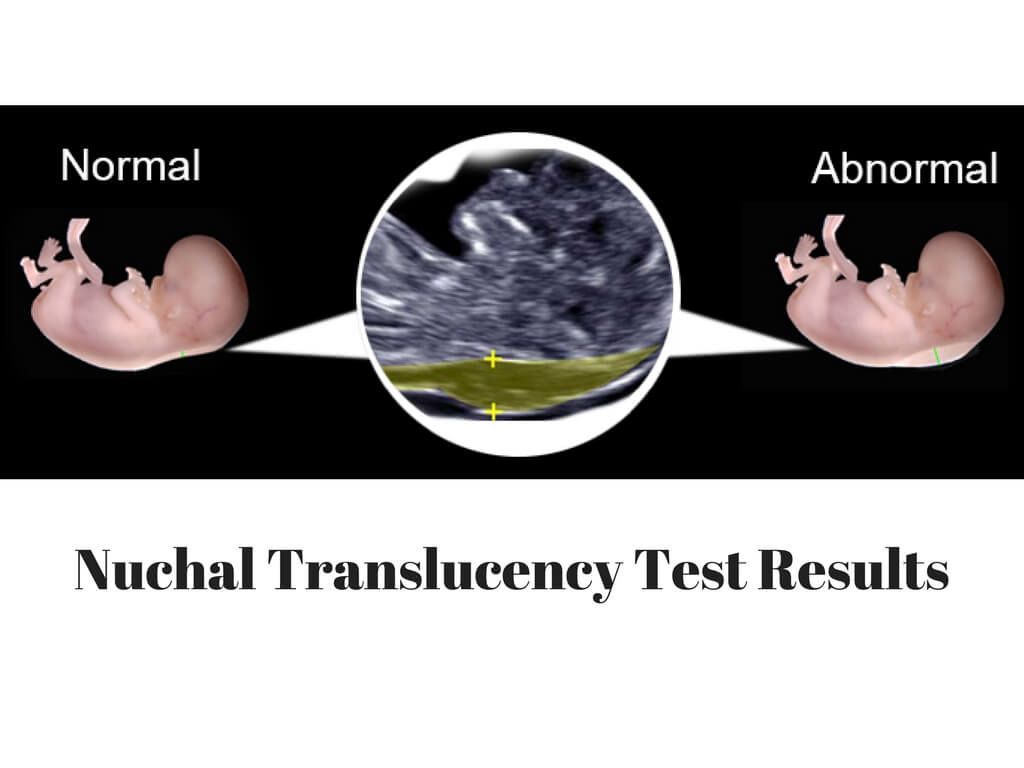 Therefore, more often take blood and urine tests of the mother, and also conduct an ultrasound examination of the child. These screening tests are not perfect because they can miss cases of Down syndrome and are also at high risk of being positive when the child does not have Down syndrome. Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome.
Therefore, more often take blood and urine tests of the mother, and also conduct an ultrasound examination of the child. These screening tests are not perfect because they can miss cases of Down syndrome and are also at high risk of being positive when the child does not have Down syndrome. Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome.
What we did
We analyzed combinations of serum screening tests in the first (up to 14 weeks) and second (up to 24 weeks) trimesters of pregnancy with or without ultrasound screening in the first trimester. Our goal was to identify the most accurate tests for predicting the risk of Down syndrome during pregnancy. One ultrasound index (neckfold thickness) and seven different serological indexes (PAPP-A, total hCG, free beta-hCG, unbound estriol, alpha-fetoprotein, inhibin A, ADAM 12) were studied, which can be used separately, in ratios or in combination with each other, obtained before 24 weeks of gestation, thereby obtaining 32 screening tests for the detection of Down's syndrome.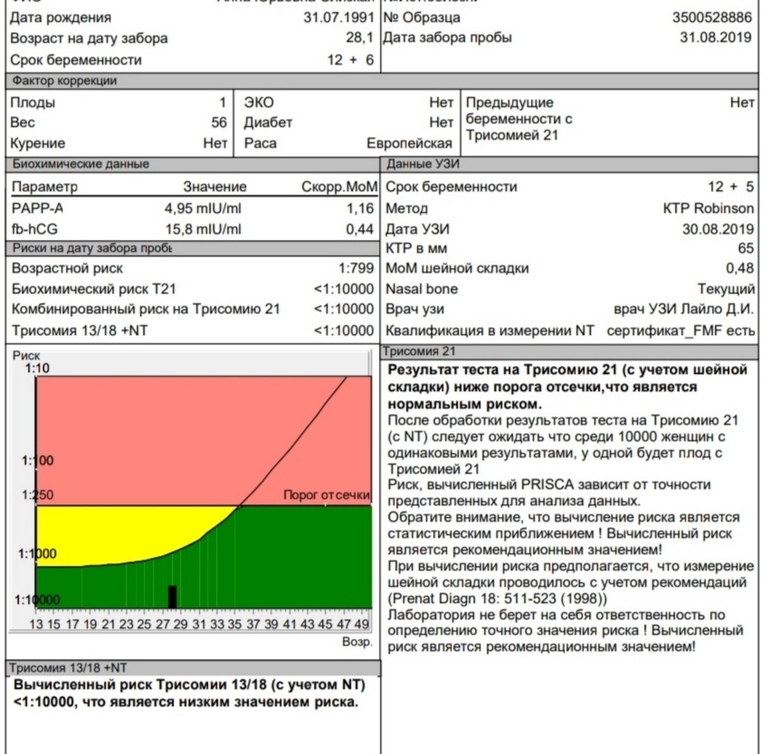 We found 22 studies involving 228615 pregnant women (including 1067 fetuses with Down syndrome).
We found 22 studies involving 228615 pregnant women (including 1067 fetuses with Down syndrome).
What we found
During Down Syndrome screening, which included tests during the first and second trimesters that combined to determine overall risk, we found that a test that included neckfold measurement and PAPP- A in the first trimester, as well as the determination of total hCG, unbound estriol, alpha-fetoprotein and inhibin A in the second trimester, turned out to be the most sensitive, as it allowed to determine 9out of 10 pregnancies associated with Down syndrome. Five percent of pregnant women who were determined to be at high risk on this combination of tests would not have a child with Down syndrome. There have been relatively few studies evaluating these tests, so we cannot draw firm conclusions or recommendations about which test is best.
Other important information to consider
Ultrasounds by themselves have no adverse effects on women, and blood tests can cause discomfort, bruising, and, in rare cases, infection.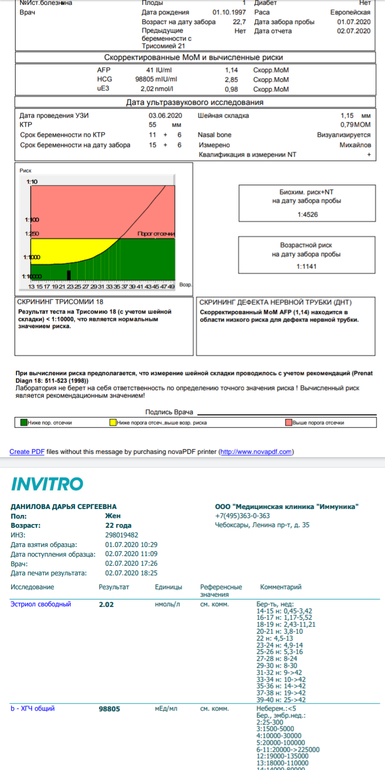 However, some women who have a high-risk Down syndrome baby on screening and who have had an amniocentesis or CVS are at risk of miscarriage of a non-Down syndrome baby. Parents will need to weigh this risk when deciding whether to perform amniocentesis or CVS after a "high risk" screening test is identified.
However, some women who have a high-risk Down syndrome baby on screening and who have had an amniocentesis or CVS are at risk of miscarriage of a non-Down syndrome baby. Parents will need to weigh this risk when deciding whether to perform amniocentesis or CVS after a "high risk" screening test is identified.
Translation notes:
Translation: Abuzyarova Daria Leonidovna. Editing: Prosyukova Ksenia Olegovna, Yudina Ekaterina Viktorovna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
Down Syndrome Screening - Bahçeci IVF Clinic
The desire of every parent-to-be is to have a healthy child. During pregnancy, various tests are used to assess the health of the unborn baby. Tests such as ultrasounds and blood tests are used during pregnancy for screening purposes.
What is Screening?
Tests called screening tests are used to detect a specific disease in healthy people. Thanks to these tests, it is possible to intervene during the course of the disease, either before it occurs or at an early stage. The main screening tests for women's health are breast ultrasound for breast cancer and the PAP smear test for cervical cancer. But screening is not a diagnostic test. Additional tests are needed to confirm the diagnosis in patients at high risk of developing the disease. For example, taking a tissue sample (biopsy) from a suspicious area. These tests are called "diagnostic" tests.
Why Are Diagnostic Tests Not Used Right Away?
Screening tests are tests that can be applied to all people, are inexpensive, and cause the least discomfort to patients. Diagnostic tests are expensive operations that require special interventions, knowledge and equipment. For example, to diagnose Down's syndrome, it is necessary to perform an amniocentesis (analysis of the amniotic fluid in which the baby is located). This procedure requires an experienced doctor, ultrasound, as well as a genetic laboratory and a specialist geneticist for chromosome analysis. Because of the risks and costs associated with them, diagnostic tests are only performed on pregnant women who have been identified as “high risk” of the disease.
This procedure requires an experienced doctor, ultrasound, as well as a genetic laboratory and a specialist geneticist for chromosome analysis. Because of the risks and costs associated with them, diagnostic tests are only performed on pregnant women who have been identified as “high risk” of the disease.
What is a Chromosome?
Chromosomal cells are the building blocks that contain the genetic information that makes us who we are and passes that information on to our children. Humans have 23 pairs of chromosomes. The pair of these chromosomes are the sex chromosomes (XY in males; XX in females).
What is Down Syndrome?
Down syndrome (trisomy 21) is a genetic disorder caused by an excess of part or all of chromosome 21. Children with Down syndrome have mild or severe mental retardation, learning difficulties, and physical retardation. They are also at high risk for heart abnormalities, reflux, recurrent ear infections, sleep disturbances, and thyroid disease.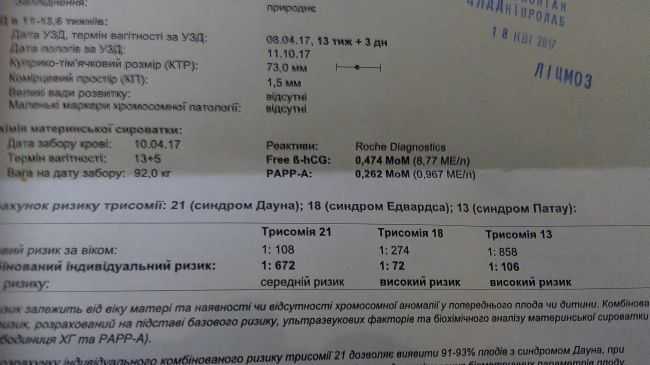 One child with Down syndrome is born in 800-1000 children.
One child with Down syndrome is born in 800-1000 children.
How is Down Syndrome screened during pregnancy?
At 10-14 and 16-18 weeks of pregnancy, biochemical tests of the mother's blood are performed. At weeks 10-14, free beta hCG and PAPP-A tests are done, and at weeks 16-18, alpha-fetoprotein, beta-hCG and estriol levels are checked. These tests are not "intelligence tests". As you know, IQ tests are written and oral exams, not blood tests. Therefore, the definition of "intellectual test" is used incorrectly.
First Trimester Screening
Obstetricians describe the pregnancy process by dividing it into three periods (trimesters). The first 14 weeks are called the first trimester. Between 10 and 14 weeks of pregnancy, your doctor will use ultrasound to measure your baby's age, heart rate, and nasal bone. Also at this time, the child's collar zone (NT) is measured.
Second Trimester Screening
In the second trimester of pregnancy, between 16 and 18 weeks, the next screening is done. A blood sample is taken from the expectant mother and examined for alpha-fetoprotein, beta hCG and estriol. The risk is calculated from the results of these tests.
A blood sample is taken from the expectant mother and examined for alpha-fetoprotein, beta hCG and estriol. The risk is calculated from the results of these tests.
What are the Risks?
So what does high risk and low risk mean?
The screening test is not a diagnostic test. Its goal is to refer only pregnant women at high risk of having a baby with Down's syndrome for further, more serious investigations (chromosomal analysis and amniocentesis).
A “high risk” or “positive” test result does not mean your child has Down syndrome. On the other hand, "low risk" or "negative" does not mean that your child will not have Down syndrome either. According to statistics, out of 10 children with Down syndrome, screening reveals 9, but one baby with this diagnosis is born into the world.
Is screening done for multiple pregnancies?
In multiple pregnancies, maternal blood counts are not used for screening purposes. Between 10 and 14 weeks of pregnancy, measurements of the collar zone and nasal bone are taken, and ultrasound is done in the second trimester.