Yeast infection while pregnant discharge
Answers to 6 burning questions about yeast infection during pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
September 20, 2022
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
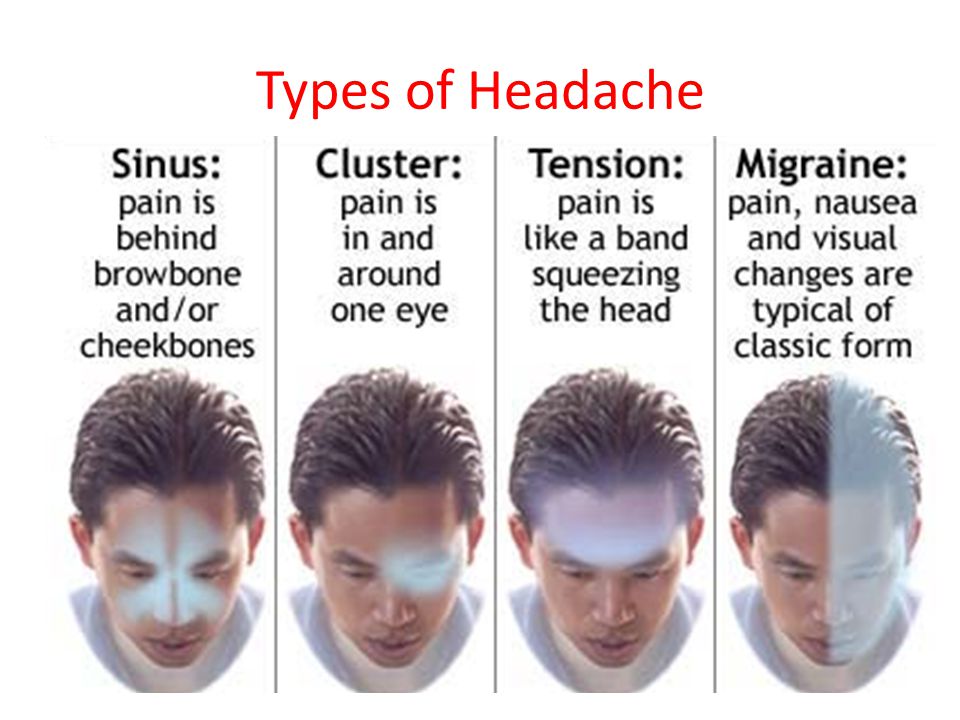
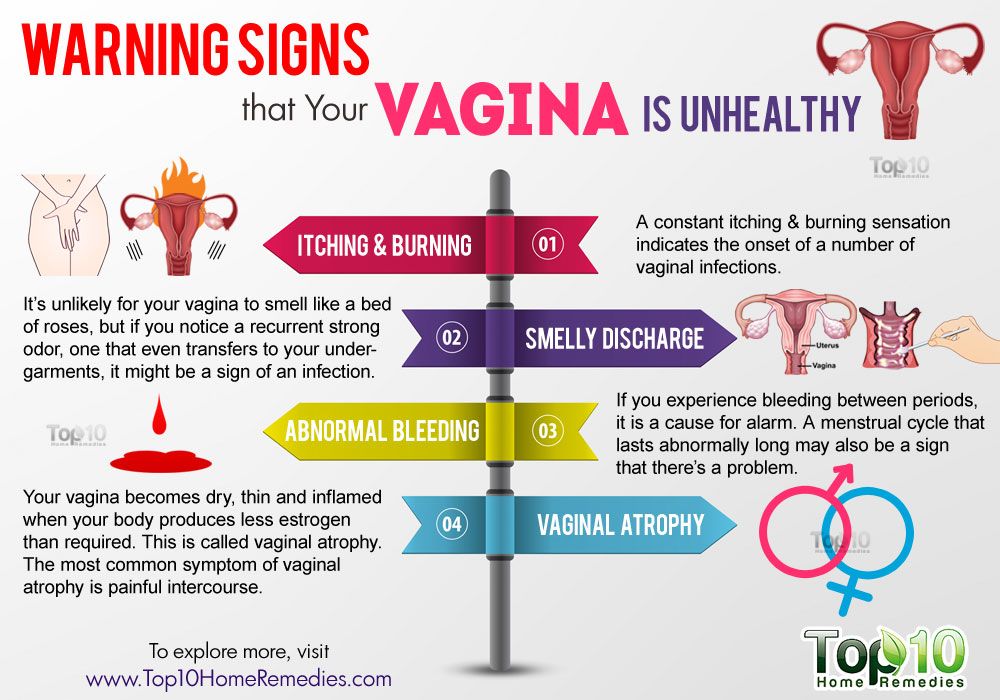
Vaginal candidiasis, also known as a yeast infection, can be a real pain. The itching, burning, and discharge can be especially worrisome during pregnancy.
In most cases, though, vaginal yeast infections and most treatment options pose minimal risk to the patient or pregnancy.
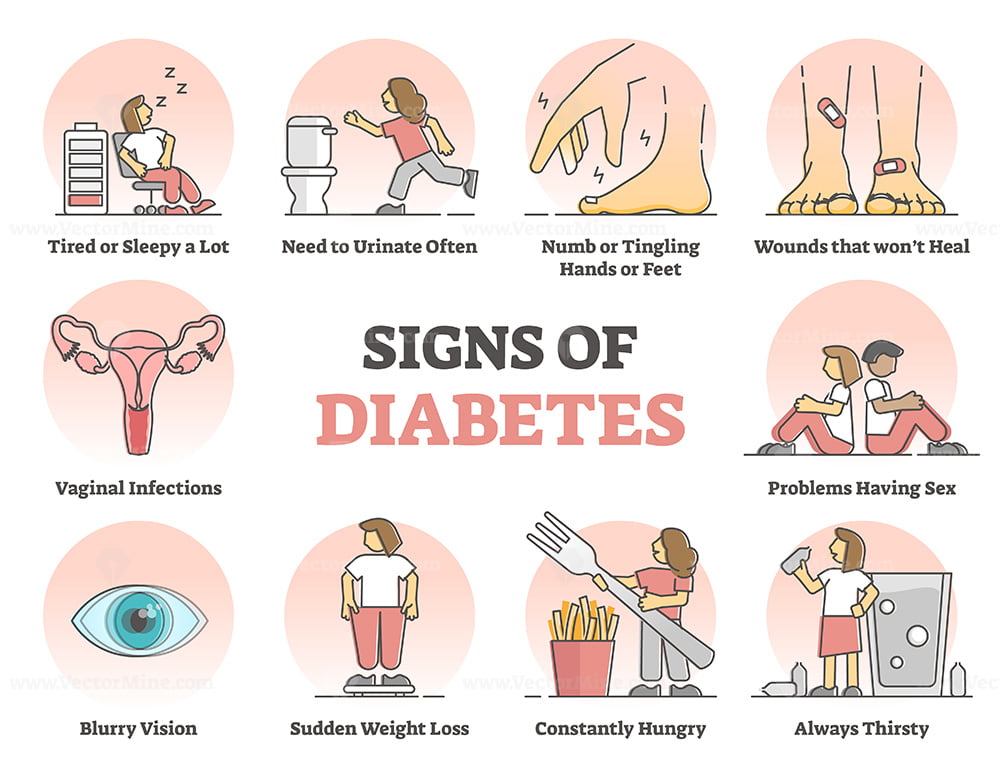
After bacterial vaginal infections, yeast infections are the second most common cause of vaginal inflammation, and 75% of women will have at least one in their lifetime. Common symptoms can include redness, itching, or irritation on the external genital area (vulva), an increase in white or tan vaginal discharge, and a burning sensation during urination or intercourse.
There are a range of over-the-counter and prescription treatments, and an Ob/Gyn or gynecologist can help you choose the safest, most effective option during pregnancy.
I’ve invited Meredith McClure, M.D., a UT Southwestern gynecologist, to answer the top questions pregnant and breastfeeding patients ask about yeast infection treatment and prevention.
Meredith McClure, M.D.Q: How common are yeast infections during pregnancy?
A: Studies have found that 20%-30% of women develop a yeast infection during pregnancy. An increase in the hormone estrogen creates a more hospitable climate for yeast to colonize the vagina because it binds to the protein factor H on the surface of the cells that cause vulvovaginal candidiasis.
Some women are more likely to develop yeast infections due to their genetics. Mutations of several genes can interfere with the immune system’s ability to defend against candida yeast, resulting in recurring infections for some people. This inherited predisposition is called familial candidiasis.
This inherited predisposition is called familial candidiasis.
Q: Can a yeast infection harm my pregnancy?
A: No. A yeast infection won’t affect your developing baby – that’s why we don’t treat yeast infections that don’t have symptoms. However, most symptomatic yeast infections get worse when left untreated. This means more itching, redness, and inflammation. If the skin becomes cracked or torn from repeated scratching, a skin infection can result. In rare cases, an untreated yeast infection can lead to fatigue, oral thrush, or digestive problems.
Q: Do yeast infections appear throughout pregnancy?
A: Yeast infections can occur any time, but they are most common during the second trimester. Talk with your doctor if you notice signs of a yeast infection while pregnant, even if you have had one before. Some more serious infections have similar symptoms, so your doctor will perform a simple fungal culture swap in the office to check for the presence of yeast.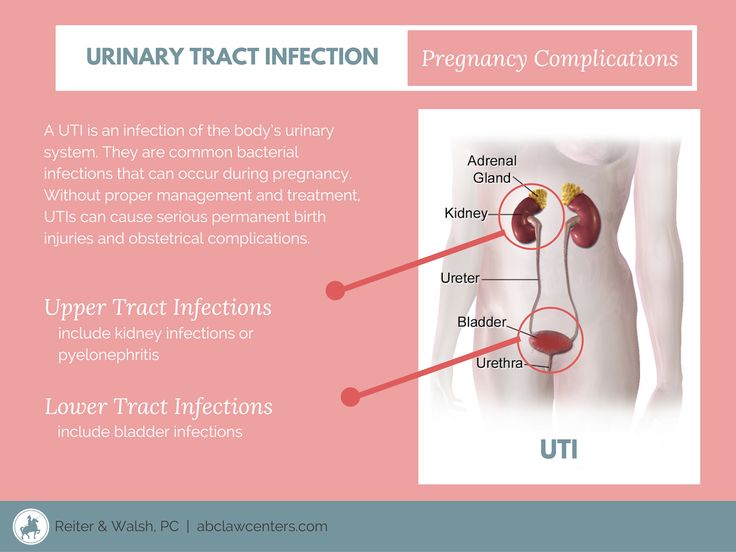
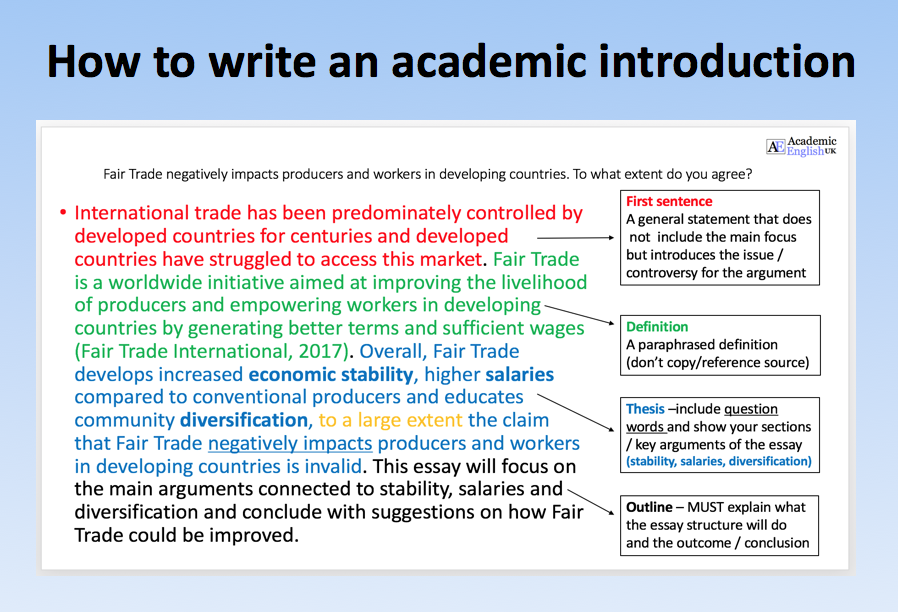
Q: What treatment options are available?
Talk with your doctor about the safest and most effective options for treating yeast infections during pregnancy.A: Topical creams or vaginal suppositories are the recommended yeast infection treatment options during pregnancy or while breastfeeding. Over-the-counter medications such as Miconazole, Clotrimazole, and Terconazole have been shown to eliminate a yeast infection safely and effectively. They are usually applied for three to seven days. It is important to finish the entire course of medication to prevent the infection from coming back. Studies have demonstrated these medications are safe to use during pregnancy.
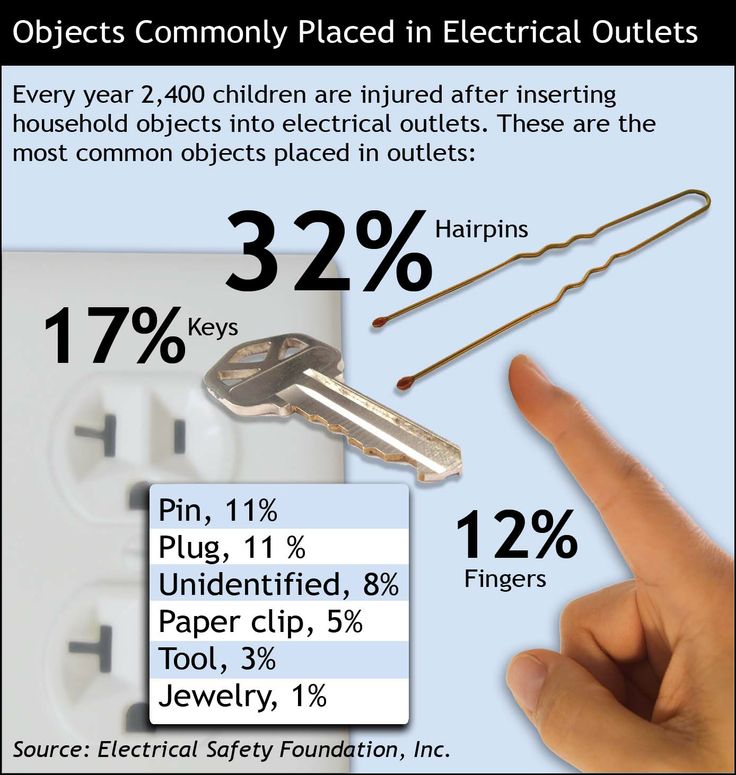
The oral medication Diflucan (fluconazole) is not recommended for most patients during pregnancy. Though taking a single pill is simpler, quicker, and less messy, some studies suggest fluconazole carries a slightly increased risk of miscarriage, birth defects, or stillbirth, especially at high doses taken over long periods of time.
While the increase is small – approximately 12 incidents per 10,000 births – the convenience of single-pill treatment might not outweigh the risk. However, in the event you have already taken or need to take fluconazole while pregnant, the additional risk at a normal dose is unlikely to pose any problems for your baby.
Q: Are yeast infection treatments safe while breastfeeding?
A: Yeast infections are less common among breastfeeding patients because estrogen levels drop dramatically in the postpartum period, making it hard for yeast to thrive. But if they occur, fluconazole may be taken by women who are breastfeeding as the levels secreted into breast milk are small.
It is possible for a breastfeeding mother and baby to pass thrush, a fungal infection that typically grows in the mouth and throat, back and forth between nipple and mouth. If that happens, both must be treated to stop the infection. Thrush is usually minor and is often caused by the same fungus – and treated with a 7- to 14-day course of the same antifungal medicines – as a yeast infection in the vagina.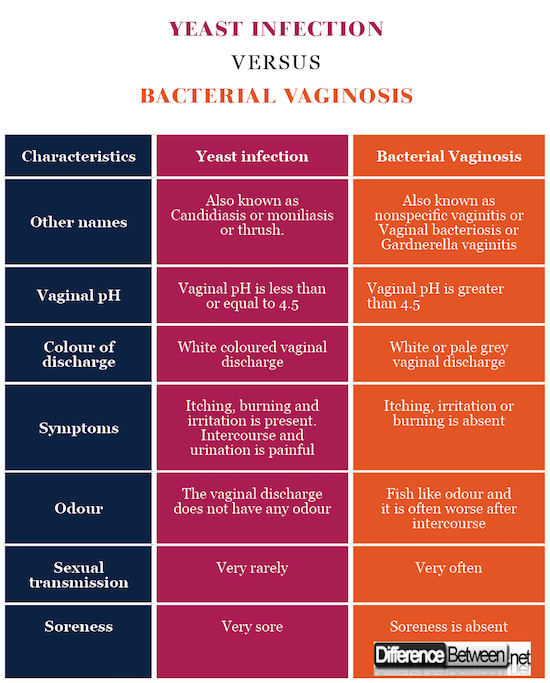
Q: What steps can reduce the risk of yeast infection?
A: During pregnancy and otherwise, take the following precautions:
- Wipe front to back after using the toilet.
- Avoid using scented tampons, pads, and pantyliners.
- Change tampons, pads, and pantyliners often.
- Avoid very hot baths and hot tubs.
- Wear underwear with a cotton lining to promote airflow.
- Do not douche, which removes healthy vaginal bacteria that prevent infection.
- Wear loose fitting clothing.
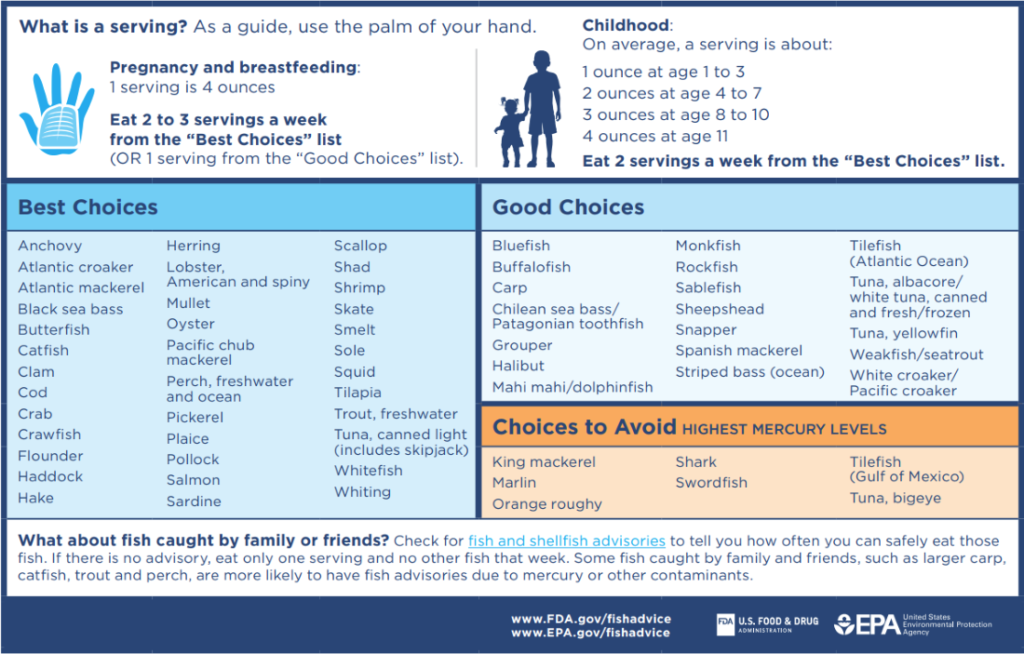
- Manage your blood sugar if you have diabetes or gestational diabetes.
- Remove wet workout clothes and swimsuits as soon as possible after activities.
If you’re pregnant and notice signs of a yeast infection, discuss treatment options with your doctor so you can eliminate these disruptive symptoms. To request an appointment, call 214-645-8300 or request online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
December 13, 2022
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.D.
December 6, 2022
Your Pregnancy Matters
- Shivani Patel, M.
 D.
D.
November 22, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
More Articles
Yeast Infections During Pregnancy - American Pregnancy Association
Yeast infections during pregnancy are more common than any other time in a woman’s life, especially during the second trimester of pregnancy.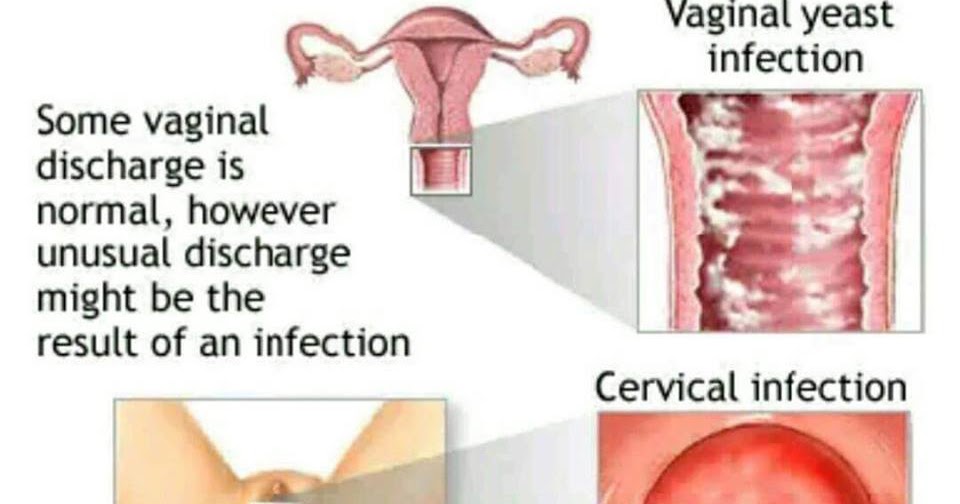 You may be noticing an increase in the amount of thin, white, odd smelling discharge. This is common and a normal symptom in the second trimester.
You may be noticing an increase in the amount of thin, white, odd smelling discharge. This is common and a normal symptom in the second trimester.
If you think you may be experiencing a yeast infection, the following information will prepare you to discuss the possibility with your doctor. Though yeast infections have no major negative effect on pregnancy, they are often more difficult to control during pregnancy, causing significant discomfort for you. Don’t wait to seek treatment!
What is a yeast infection?
Yeast infection occurs when the normal levels of acid and yeast in the vagina are out of balance, which allows the yeast to overgrow causing an uncomfortable, but not serious, a condition called a yeast infection.
If you have never been diagnosed or treated by a physician for a yeast infection and have some of the symptoms, you should see your physician first for accurate diagnosis and treatment. Other infections have similar symptoms, so you want to make sure that you are treating the infection correctly. There are also treatments that are not appropriate during pregnancy.
There are also treatments that are not appropriate during pregnancy.
What causes yeast infections during pregnancy?
A yeast infection can be caused by one or more of the following:
- Hormonal changes that come with pregnancy or before your period
- Taking hormones or birth control pills
- Taking antibiotics or steroids
- High blood sugar, as in diabetes
- Vaginal intercourse
- Douching
- Blood or semen
Why are yeast infections more common during pregnancy?
Your body is going through so many changes right now, and it is difficult for your body to keep up with the chemical changes in the vagina. There is more sugar in vaginal secretions on which the yeast can feed, causing an imbalance which results in too much yeast.
What are the symptoms of yeast infections?
The symptoms of a yeast infection may include one or more of the following:
- Discharge that is usually white/tan in color, similar to cottage cheese and may smell like yeast/bread
- Other discharge may be greenish or yellowish, also similar to cottage cheese and may smell like yeast/bread
- An increase in discharge
- Redness, itching, or irritation of the lips of the vagina
- Burning sensation during urination or intercourse
What else could I be experiencing?
If you are experiencing symptoms similar to a yeast infection, but a physician has ruled this diagnosis out, you may have one of the following:
- Sexually Transmitted Diseases (STDs) like Chlamydia, Gonorrhea, & Trichomoniasis
- A vaginal infection called bacterial vaginosis
How do I know for sure if I have a yeast infection?
At your doctor’s office or medical clinic, a clinician will use a simple, painless swab to remove the discharge or vaginal secretions and examine it through a microscope.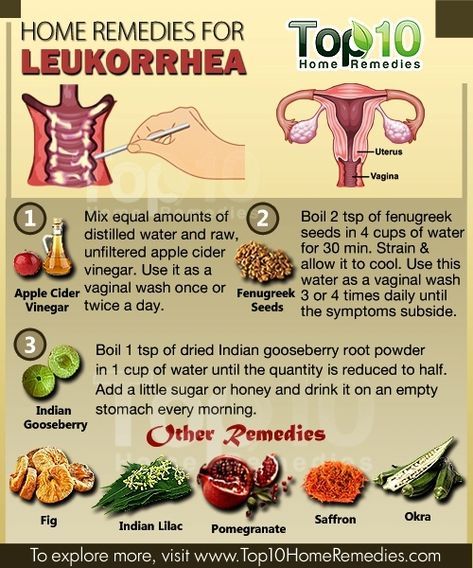 Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
How are yeast infections treated during pregnancy?
During pregnancy, physicians recommend vaginal creams and suppositories only. The oral medication, Diflucan (a single-dose medication), has not been proven safe during pregnancy and lactation. Not all vaginal creams and suppositories are okay to use during pregnancy, so it is best to consult your doctor or pharmacist to get the right one. If left untreated, yeast infections can pass to your baby’s mouth during delivery. This is called “thrush” and is effectively treated with Nystatin.
It may take 10-14 days to find relief or completely clear up the infection while you are pregnant. After the infection has cleared up and any sores have healed, it may be helpful to use a starch-free drying powder, or Nystatin powder to prevent a recurring infection.
How can I prevent a yeast infection or recurring yeast infections?
Most yeast infections can usually be avoided by doing the following:
- Wear loose, breathable cotton clothing and cotton underwear.

- After regular, thorough washing (using unscented, hypoallergenic or gentle soap), use your blow dryer on a low, cool setting to help dry the outside of your genital area.
- Always wipe from front to back after using the restroom.
- Shower immediately after you swim. Change out of your swimsuit, workout clothes, or other damp clothes as soon as possible.
- Do NOT:
- douche
- use feminine hygiene sprays
- use sanitary pads and tampons that contain deodorant
- take a bubble bath/use scented soaps
- use colored or perfumed toilet paper
- Include yogurt with “lactobacillus acidophilus” in your diet.
- Limit sugar intake, as sugar promotes the growth of yeast.
- Get plenty of rest to make it easier for your body to fight infections.
When should I contact my doctor?
If you are experiencing the symptoms described in this article, call your doctor now. Yeast infections have similar symptoms of other infections, such as STDs. Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
If you see no improvement within three days, or if symptoms worsen or come back after treatment, you should contact your healthcare provider again.
Want to Know More?
- Pregnancy Nutrition
- Medication and Pregnancy
Compiled using information from the following sources:
1. American Academy of Family Physicians
https://familydoctor.org
1. Mayo Clinic Complete Book of Pregnancy & Babys First Year. Johnson, Robert V., M.D., et al, Ch. 11.
Ecofucin for the treatment of thrush during pregnancy.
Thrush is a disease of the vaginal and vulvar mucosa caused by yeast-like fungi of the genus Candida, which affects 35% of women during pregnancy 1 .
At risk for the occurrence of a recurrent form of thrush are those pregnant women who have already had episodes of thrush in their anamnesis the level of estrogens rises, in connection with which glycogen accumulates in the vaginal mucosa - a nutrient medium for yeast-like fungi of the genus Candida. nine0005
nine0005
Lactobacilli are the predominant microorganisms in the vaginal microflora of a healthy woman. A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli also participate in the formation of local immunity
In addition, during thrush, the vaginal microflora is disturbed - the number of lactobacilli decreases sharply. These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush. nine0005
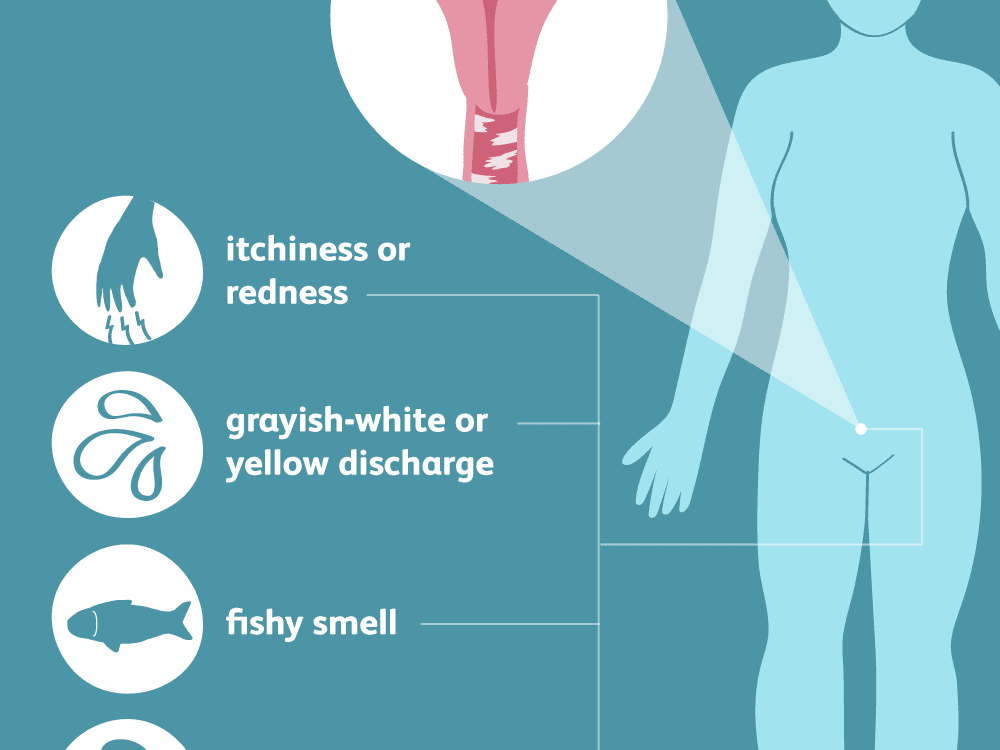
Symptoms of thrush in a pregnant woman:
- itching and burning in the vulva and/or vagina, swelling and irritation in the vulva
- vaginal discharge with a "curdled character" and occasional foul odor
- pain during and after intercourse
- urination disorder and pain
The appearance of at least one of the symptoms is a reason for an unscheduled visit to the doctor. nine0005
nine0005
Why is it important to diagnose and treat thrush in a pregnant woman in time?
Some women are asymptomatic carriers of yeast-like fungi of the genus Candida and experience neither discomfort nor manifestations of the disease throughout the entire period of pregnancy 2
A pregnant woman with thrush (including an asymptomatic carrier) is a source of infection for her unborn child. Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with fungi of the genus Candida is especially dangerous 2 .
Timely and effective treatment of thrush in a pregnant woman is an important task
Treatment of thrush
Safety and efficacy are the main criteria for choosing a drug in the treatment of thrush in pregnant women
The earlier a pregnant woman is diagnosed and treated for thrush, the less the risk of negative consequences and complications for the course of pregnancy and for the health of the mother and her unborn child.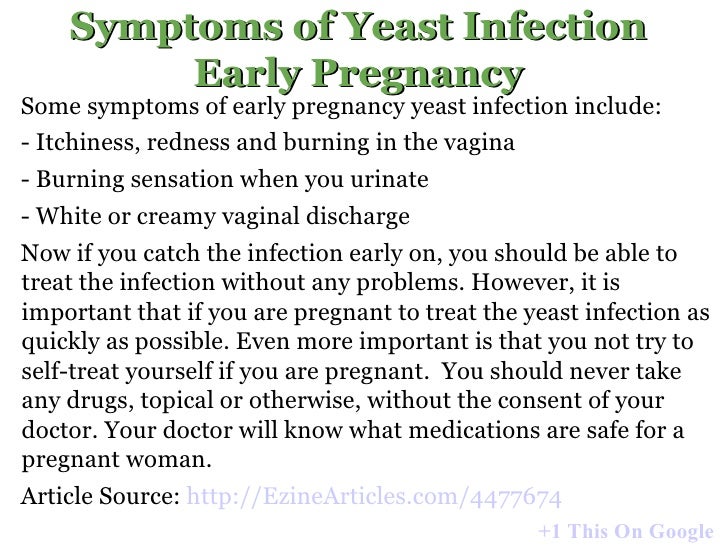 In the treatment of thrush, experts recommend an integrated approach to therapy.
In the treatment of thrush, experts recommend an integrated approach to therapy.
It is important to follow the recommendations of a specialist, following the prescribed dosage and regimen. nine0005
Comprehensive treatment should be aimed at solving two problems: eliminating the cause of thrush (fungi of the genus Candida) and restoring the vaginal microflora. It is important to know that not all drugs are approved for use during pregnancy. For example, most oral (systemic) drugs and some topical drugs for treating thrush are contraindicated during pregnancy.
Ecofucin
® in the treatment of thrush in pregnancyEcofucin
® is allowed at all stages of pregnancy and lactation 4
Natamycin
- practically not absorbed into the blood and has no systemic effect
- has a fungicidal effect - causes fungal cell death
- resistance to it does not develop
- does not inhibit the growth of natural microflora
+
Prebiotic 5
- actively fermented by the normal microflora of the vagina, stimulating the growth of lactobacilli 6
- causes restoration of the vaginal microflora, stimulates local immunity 6
The active substance 7 of Ecofucin ® eliminates the cause of thrush, and the prebiotic 5 in Ecofucin ® promotes the restoration of the vaginal microflora and strengthens local immunity 6 .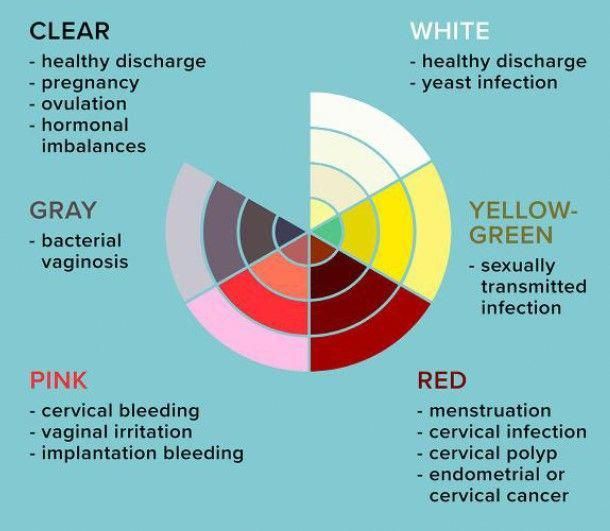
Efficacy and safety of the drug Ecofucin has been proven by clinical studies
Ecofucin promotes faster recovery of patients with thrush. nine0005
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Ecofucin helps to increase the number of own lactobacilli in the vagina and reduce the risk of recurrence of thrush. nine0005
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Dosage and Administration
The regimen for the use of Ecofucin ® in a pregnant woman is prescribed by the attending physician individually.
Additional conditions for effective treatment of thrush are: giving up bad habits, a carbohydrate-restricted diet, wearing underwear made from natural fabrics, etc.
It is important to consult a gynecologist in a timely manner and exclude self-medication.
1. Tikhomirov A.L., Sarsania S.I. Features of candidal vulvovaginitis in pregnant women at the present stage. // Farmateka No. 9, 2009, p. 64-70.
2. Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bairamova G.R. Federal clinical guidelines "Urogenital candidiasis". // 2013.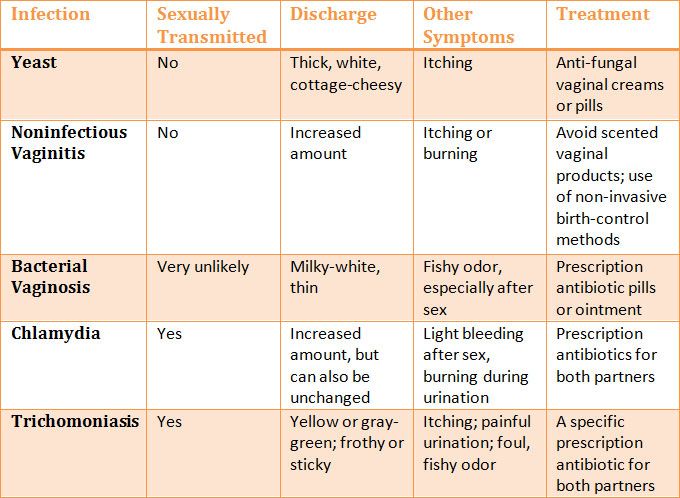
3. Kupert A.F., Akudovich N.V., Khoroshikh O.V., Vereshchagina S.A., Khmel T.V. Features of the clinic and treatment of vaginal candidiasis in pregnant women, depending on the type of fungi of the genus Candida. // Gynecology. v. 05, N 5b, 2003.
4. Instructions for use of the drug Ecofucin ® .
5. Excipient, lactulose.
6. Dikovskiy A.V., Dorozhko O.V., Rudoy B.A. Pharmaceutical composition of antimycotics and prebiotics and a method for the treatment of candidal vaginitis. // International publication WO 2010/039054 A1.
7. Active ingredient, natamycin.
What is thrush during pregnancy - Omega-Kyiv guide
In preparation for pregnancy, a woman undergoes a comprehensive examination by a gynecologist in a private clinic, and passes all the necessary tests. But this does not protect her from all the dangers that surround weakened by pregnancy immunity. Quite often, in an absolutely healthy woman, the onset of pregnancy is accompanied by thrush.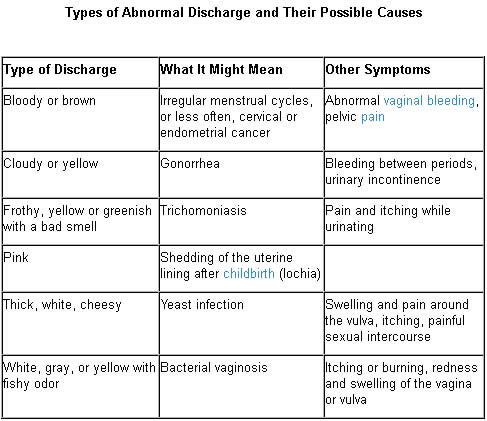 Thrush - (scientific name "candidiasis") is an infectious disease caused by a fungus of the genus Candida. The disease is accompanied by white curdled discharge from the vagina, which is not typical for a healthy woman. nine0005
Thrush - (scientific name "candidiasis") is an infectious disease caused by a fungus of the genus Candida. The disease is accompanied by white curdled discharge from the vagina, which is not typical for a healthy woman. nine0005
Why is thrush dangerous during pregnancy?
If you start treatment in a timely manner, then thrush during pregnancy is not dangerous. Some believe that it is pointless to treat thrush, because this phenomenon occurs against the background of hormonal changes during pregnancy. But this opinion is erroneous and can lead to infection of the baby with stomatitis, which will lead to problems with feeding. Also, thrush can cause erosion of the uterus, which subsequently leads to a loss of elasticity of the vagina and ruptures during childbirth. nine0005
What are the symptoms of thrush during pregnancy?
The symptomatology of the disease during pregnancy does not differ much from the usual signs of thrush.
Symptoms of candidiasis during pregnancy:
- White or white-yellow vaginal discharge.
 By consistency, the discharge can be liquid or cheesy;
By consistency, the discharge can be liquid or cheesy; - Discharge may have a sour, offensive odor;
- Discomfort caused by severe itching inside the vagina. The most severe itching occurs at night, after taking a hot bath or after sexual intercourse; Pain when urinating. nine0018
The treatment of thrush during pregnancy must be treated with particular importance. You should forget all the ways of “self-treatment at home”, and immediately consult a doctor. This action is primarily due to the fact that during pregnancy, many medicines are prohibited and can harm the baby. The gynecologist will help you choose drugs that do not harm the child. The most effective and safe methods of treatment will be suppositories and topical ointments. Also, based on the recommendations of the doctor, you can apply folk methods of dealing with the disease. nine0005
Concerning methods of preventing thrush during pregnancy, gynecologists give the following recommendations:
- Replace synthetic and uncomfortable underwear with cotton;
- Daily maintain vaginal hygiene, avoid excessive dampness, because a humid environment contributes to the growth and reproduction of the fungus;
- Exclude from the diet alcohol, high-calorie and junk food that contains preservatives.