White colour stool
Pale stool: causes, diagnosis, and treatment
Pale stools can result from dietary choices, an infection, or an underlying medical problem, such as gallbladder or liver disease. Anyone with persistently white or clay-colored stools should seek medical advice.
If pale stools occur once with no other symptoms, it is usually safe to wait and see if the stool returns to its usual color. A child or infant with pale or white poop should see a doctor as soon as possible to rule out any underlying conditions.
In this article, learn about the causes of pale stool and other symptoms that may occur with them.
Bile from the liver, known as bilirubin, creates the typical brown hue of a healthy bowel movement. When the stool is very pale, it often means that not enough bile is reaching the stool.
Stools may contain low bile levels if there is a problem with the gallbladder, pancreas, or liver. People with consistently pale stools may want to talk with a doctor about conditions that affect these organs.
The most common reasons for a pale stool color include:
1. Foods
Some foods, such as fatty foods, may cause stool color to become yellow.
The occasional pale bowel movement is unlikely to be a cause for concern. Changing the diet may cause poop to return to its usual color.
What should poop look like?
2. Giardiasis
Giardiasis, also known as beaver fever, is an infection that may turn the stool yellow. Symptoms can result from an infection with Giardia lamblia, an intestinal parasite. A person can contract this parasite by drinking contaminated water or coming into contact with soil or stool that contains the parasite.
Giardiasis is present around the world, including all parts of the United States, according to the Centers for Disease Control and Prevention (CDC).
Other symptoms of giardiasis include:
- headache
- abdominal pain
- vomiting
- fever
Symptoms start 1–2 weeks after infection and can 2–6 weeks to resolve, or longer in some cases. Prescription medicine can reduce the time symptoms last.
Prescription medicine can reduce the time symptoms last.
3. Medications
Many drugs and medications can damage the liver, especially with high doses.
Both prescription and over-the-counter (OTC) remedies, for example, ibuprofen and acetaminophen, can harm the liver.
Large amounts of aluminum hydroxide, present in antacids, can cause stool to lighten in color. Barium sulfate, a type of contrast used for certain X-ray tests, can also cause pale stools.
Pale stools may be a sign of liver damage in a person who:
- is taking a new drug
- has been taking medication for some time
- is taking high doses of a drug
With OTC drugs, it is best to stop taking the drug and see a doctor as soon as possible. For prescription drugs, people should speak with their doctor before stopping the drug.
Which drugs cause liver damage?
4. Gallbladder disease
The gallbladder holds bile and is located on the upper right side of the stomach, next to the liver. During digestion, the gallbladder releases bile into the intestines through the bile duct. Gallbladder diseases can change the color of stool.
During digestion, the gallbladder releases bile into the intestines through the bile duct. Gallbladder diseases can change the color of stool.
Gallstones, one of the most common gallbladder diseases, can block the bile duct.
As well as pale stool, it can cause:
- intense pain
- nausea
- vomiting
- fever and chills
- jaundice
Without treatment, gallstones can cause problems with other organs, such as the pancreas and liver.
Treatments for gallbladder problems depend on the cause. A doctor may have to remove gallstones, either surgically or with medication to dissolve them.
A person can live without a gallbladder, and so a doctor may remove it if gallstones keep returning. The person may need to change their diet after surgery.
What are the most common gallbladder problems?
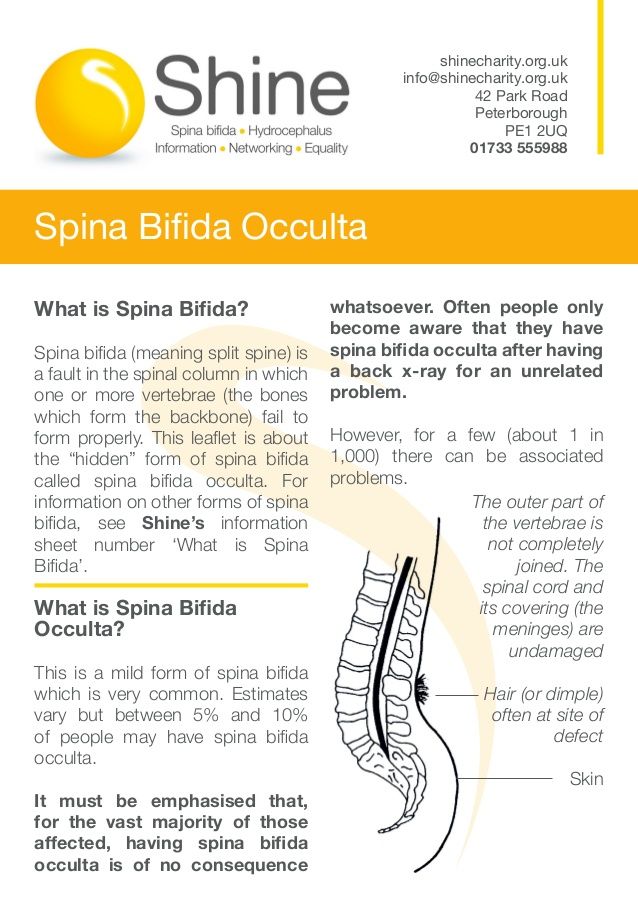
5. Liver problems
Problems with the liver or bile ducts can turn the stool pale.
There are two forms of bilirubin in the body. One type is passed in the urine or feces and the other type is bound to protein (albumin), which helps it stay in the blood vessels.
One type is passed in the urine or feces and the other type is bound to protein (albumin), which helps it stay in the blood vessels.
When a person has liver or biliary problems, bilirubin is unable to pass in the stool. This causes the stool to lose its color, giving it a paler or clay-colored appearance.
Conversely, the body excretes excess bilirubin in the urine, giving it a darker or amber-colored appearance.
There are many types of liver disease, including:
- infectious diseases, such as hepatitis A, B, and C
- liver damage from alcohol consumption
- fatty liver disease, most common in those with obesity or who eat a high-fat diet
- autoimmune diseases, when the body attacks the cells of the liver
- failure of other organs
- liver cancer
- liver cysts
- Wilson’s disease, a genetic condition where the body retains too much copper
In addition to pale stool, other symptoms of liver disease include:
- nausea and vomiting
- fatigue
- very dark urine
- fatty stool
- itching
- swelling in the ankles or legs
Anyone under a doctor’s care for liver disease should report any changes in stool color.
Treatment for liver disease depends on the cause and how far it has progressed.
For mild liver disease, a person may only need medication and lifestyle changes. Those with severe liver disease may need a liver transplant.
Sometimes problems with other organs — such as the gallbladder — lead to liver symptoms. In this case, a doctor must treat the underlying condition as well.
Examples of bile duct problems include bile duct obstruction, which may be due to bile duct stones.
What is cirrhosis?
6. Pancreatic problems
Diseases of the pancreas can make it hard for this organ to secrete pancreatic juices into the digestive system. This can lead to the food moving too quickly through the gut, resulting in a pale and fatty-looking stool.
Examples of problems with the pancreas include pancreatitis and pancreatic cancer.
Both can involve jaundice, with the following symptoms:
- pale and fatty stools
- dark urine
- yellowing of the whites of the eyes
Pancreatitis refers to swelling and inflammation of the pancreas.
It can result from various conditions, including:
- infections
- autoimmune pancreatitis
- gallstones
- high alcohol consumption
- the use of some drugs
Chronic pancreatitis can also increase the risk of pancreatic cancer.
Treatment for pancreatitis depends on the cause. The doctor may address an underlying issue, such as gallstones.
Some people need hospitalization, intravenous fluids, and pain management. If a bacterial infection is present, a doctor may prescribe antibiotics.
In some cases, surgery may be necessary.
What is the best diet for someone with pancreatitis?
Pale stools in children are not necessarily a medical emergency if they occur once and are pale but not white.
Breastfed babies often have light yellowish-brown stools. Once they start transitioning to solids, their stool usually becomes browner.
When the stool is white or very light brown, this can signal a more serious problem, such as cholestasis, a type of liver disease.
In newborns, cholestasis or any other problem with the liver, gallbladder, or pancreas may be a medical emergency. A caregiver should call their pediatrician right away.
If the baby has other symptoms, turns yellow, or appears to be in pain, they must go straight to the emergency room.
In older children who have no other symptoms, it is usually safe to wait for the next bowel movement.
What are the pros and cons of breastfeeding?
White or clay-colored stools during pregnancy usually indicate a problem with the gallbladder, liver, biliary ducts, or pancreas. Some people develop a pregnancy-related liver disease called cholestasis of pregnancy.
Symptoms of cholestasis include pale stool as well as:
- intense itchiness
- pain under the ribs on the upper right side of the stomach
- dark urine even when hydrated
- nausea
- exhaustion beyond that of a typical pregnancy
- jaundice, or yellowing of the eyes, fingernail beds, or skin
It is not clear precisely what causes cholestasis, but pregnancy hormones might affect liver functioning.
Treatment can include medication and frequent monitoring, including blood work and ultrasound scans. In some cases, an early deliver might be necessary.
How will pregnancy affect your body?
A doctor will ask some questions and may carry out a physical examination.
They may ask:
- When did you first notice this symptom?
- Are all your stools pale?
- What medications do you use?
- Do you have any other health conditions?
- Do you have any other symptoms?
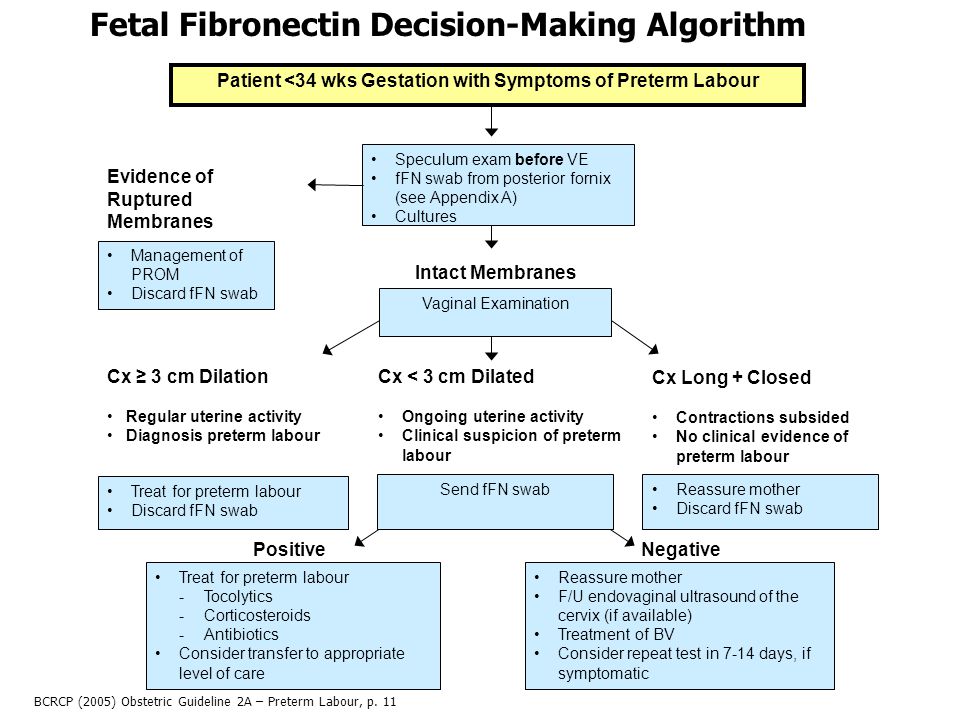
To investigate pale stools, a doctor may recommend the following tests:
- blood tests to assess liver function and look for signs of infection
- endoscopic retrograde cholangiopancreatography (ERCP)
- imaging studies, for instance, an abdominal ultrasound, a CT scan, or MRI of the liver and bile ducts
What are the symptoms of liver disease, and how do doctors diagnose it?
The outlook will depend on the cause of pale stools.
If a person’s stools are pale because of certain foods or supplements, changing the diet or regime will usually help.
The outlook for pancreatitis varies. In around 2% of cases, it can be fatal. It can also increase the risk of other conditions, such as pancreatic cancer.
For people with pancreatic cancer, the chance of surviving 5 years or longer after diagnosis is around 42%, if it is still limited to the pancreas. If cancer has spread to other parts of the body, the 5-year survival rate is about 3%.
Gallstones can be life threatening, especially if a person needs emergency surgery, as is a risk of complications.
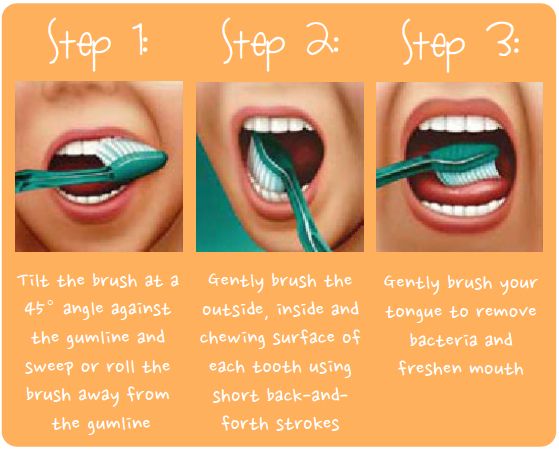
Various factors can lead to pale stools. It is not always possible to prevent pale stools, but people can lower the risk of developing certain diseases, such as pancreatitis and pancreatic cancer.
Some ways to prevent pancreatitis include:
- following a low fat diet
- avoiding smoking
- limiting alcohol consumption
- maintaining a moderate weight
Similar measures may also help prevent pancreatic cancer.
To reduce the risk of liver disease, a person can:
- limit alcohol intake
- maintain a moderate weight
- eat a balanced diet
- follow all instructions when taking medications
- having hepatitis A and hepatitis B vaccinations, if a doctor recommends them
Which foods protect the liver?
Diseases of the liver, gallbladder, and pancreas can quickly become life threatening, but they are usually treatable.
If symptoms arise, such as pale stools, it is best to seek help as soon as possible, as leaving them can lead to lasting damage and complications.
Sometimes a person passes one pale stool, and then the usual color returns. If pale stools persist, it is best to seek medical advice promptly, especially if there are other symptoms, such as pain, dark urine, vomiting, or a fever.
Here are some answers to questions people often ask about pale stool.
What does pale stool mean?
Pale stools can indicate problems in the liver, bile ducts, gallbladder, or pancreas. Dietary factors can also play a role. Giardiasis, a parasitic infection, can cause yellow stools.
Is it serious?
Without treatment, the conditions underlying pale stools can be serious or lead to severe complications. Anyone with persistently pale stools should seek medical advice.
Bowel movements reveal important information about a person’s health. One pale stool is not usually a matter for concern, but frequent pale stools can indicate diseases of the liver, pancreas, or gallbladder.
In some cases, treatment can help a person feel better within a few days or weeks. Other underlying conditions require long-term management.
Read this article in Spanish.
Yellow stool: 8 causes
Normal stool is brown due to healthy levels of excreted bilirubin and bile. Sometimes, a person may notice their stool is a different color, including yellow.
Stools may change color for various reasons, including a person’s diet and various underlying medical conditions. Yellow is a normal variation of stool color in infants.
Changes in stool color are also normal. Watch for consistent changes over time and consult with a doctor if other symptoms are present.
This article will outline the causes of yellow stool in adults and infants, complications, and when to see a doctor.
A person’s diet and the level of bile present in the stool directly influence a person’s stool color. Bile is yellow-green, and as it travels through the gastrointestinal (GI) tract, enzymes cause changes that turn it brown.
All shades of brown-colored stool are normal. If a person’s stool is red or black, or other changes remain longer than 2 weeks or come with other symptoms, they should consult a doctor.
Stools can be other colors, including:
- Green: Eating leafy green vegetables, green food coloring, iron supplements, or diarrhea moving food through the intestine too quickly may cause this color.
- Yellow, pale brown, or gray: Giardiasis can cause bright yellow diarrhea. Pale yellow or gray stool can result from problems in the liver or gallbladder.
- Orange: Eating carrots, winter squash, antibiotics, or antacids could cause this color.
- Blue: Usually the result of eating artificially blue foods or drinking blue beverages.
- Black, tarry: Eating black licorice or taking iron supplements, and bleeding in the upper GI tract, cirrhosis, or colorectal cancer can also cause black stool.
 Medication containing bismuth subsalicylate, better known as Pepto Bismol or Kaopectate, can also cause black, tarry stools.
Medication containing bismuth subsalicylate, better known as Pepto Bismol or Kaopectate, can also cause black, tarry stools. - Bright red: Eating or drinking red, artificially colored food or drinks can cause this. Certain conditions can cause bleeding in the upper GI tract, such as cirrhosis or GI tumors. Hemorrhoids can cause bleeding in the lower GI tract and cause stool to be red.
Possible causes of yellow stool include:
Diet
Since the GI tract processes food for elimination, what a person eats can affect the color of their stool.
Carrots, sweet potatoes, turmeric, and foods that contain yellow food coloring may cause stool to become yellow.
A diet high in fat or gluten can also lead to yellow stool.
If a person regularly has yellow stools, they should try avoiding fatty, processed foods, gluten, or anything that causes an upset stomach.
Stress
Stress and anxiety can have many physical effects on the body, including speeding up the digestive process.
As a result, the body may not be able to absorb all of the nutrients in food, which may lead to diarrhea or yellow stool.
Taking steps to relieve stress by reducing commitments, practicing yoga, or seeing a therapist may help reduce physical symptoms.
Celiac disease
If people with celiac disease eat gluten, a protein in wheat, rye, and barley, their immune system responds by attacking the tissues of their small intestine.
This immune response causes tissue damage and compromises the intestines’ ability to absorb nutrients.
In addition to yellow stool, symptoms of celiac disease include:
- diarrhea
- constipation
- nausea
- bloating
- fatigue
- headaches
- depression
There is no cure for celiac disease, but a person can effectively manage the condition by avoiding gluten.
Disorders of the pancreas
Disorders of the pancreas can cause yellow or pale stool. Some of these disorders include:
- chronic pancreatitis
- cystic fibrosis
- pancreatic cancer
- blockage of the pancreatic duct
In people with these conditions, the pancreas cannot provide enough enzymes for the intestines to digest food. Undigested fat can lead to yellow stool that also appears greasy or frothy.
Undigested fat can lead to yellow stool that also appears greasy or frothy.
Liver disorders
Disorders of the liver, such as cirrhosis and hepatitis, can lower or eliminate bile salts in the body.
Bile salts are essential for the digestion of food and absorption of nutrients. The removal of these salts can result in yellow stools.
Gallbladder disorders
Gallbladder problems and gallstones can also reduce the level of bile salts in the body. This reduction can lead to a variety of symptoms, including:
- abdominal pain
- a fast heartbeat
- an abrupt drop in blood pressure
- jaundice, the yellowing of the skin and the whites of the eyes
- pale stool
Treatment will depend on the specific gallbladder issue. The treatment for gallstones, for example, may include medication to dissolve the stones. In some cases, a person may need surgery.
Gilbert syndrome
Gilbert syndrome is a genetic liver disorder that affects 3–7% of Americans.
People with Gilbert syndrome have periods when their bilirubin levels are too high. Symptoms include mild jaundice and yellow stool. However, the symptoms can be so mild that most people do not notice them or know they have the condition.
Giardiasis
Giardiasis is a common intestinal infection caused by a microscopic parasite. A person can contract the Giardia parasite by ingesting Giardia cysts, usually through contaminated food or water.
Symptoms of giardiasis include:
- stomach cramps
- foul-smelling diarrhea
- yellow diarrhea
- nausea
- fever
- headaches
- weight loss
A doctor can diagnose giardiasis by testing a person’s stool samples. Treatment involves antibiotics, and the symptoms can last for up to a few weeks. In rare cases, the infection can be long term.
In infants, shades of yellow, brown, and green are all common stool colors. Babies fed formula may have thicker and darker stools, similar to mustard or soft play dough.
In the first week after birth, babies fed human milk will have three or four mustard-yellow, loose stools every 24 hours.
Speak with a doctor if an infant has red, black, or white poop, as this can indicate a problem.
An older adults’ diet or an underlying medical condition may cause yellow stools.
Liver or gallbladder disorders can reduce the production of bile salts, resulting in pale or yellow-colored stools.
If accompanied by diarrhea, older adults should avoid dehydration by drinking water or using oral rehydration solutions.
Yellow stool by itself does not lead to complications, but the underlying cause of it might.
Yellow stool may indicate a malabsorption disorder caused by a parasite, illness, or disease.
Malabsorption of fat can lead to an increased fat content in stools, which can be pale, large, foul-smelling, and loose. This is known as steatorrhea, and complications may include:
- malnutrition
- weight loss
- vitamin deficiencies
- iron deficiency anemia
- poor bone health
Yellow stool is usually due to dietary changes or food colors. However, if the color change continues for several days or other symptoms are present, it is best to contact a doctor.
However, if the color change continues for several days or other symptoms are present, it is best to contact a doctor.
A person should see a doctor if they experience any of the following symptoms with yellow stool:
- a fever
- vomiting
- abdominal pain
- pus-filled stool
- inability to urinate
- trouble breathing
- fainting
- a lack of awareness
- confusion or mental changes
The cause of yellow stool is usually related to a person’s diet, but it can also result from underlying health problems.
Some health problems can lead to malabsorption and malnutrition which can cause a loss of important vitamins and nutrients.
It is essential to look out for additional symptoms and see a doctor if the yellow color persists. The treatment will depend on the underlying cause.
Read the article in Spanish.
Grayish-white stools - causes, diagnosis and treatment
Grayish-white stools is a discoloration of stools, often accompanied by a violation of the consistency and frequency of stools. A change in the color of feces is characteristic of dysbacteriosis, diseases of the liver and gallbladder, and damage to the pancreas. To determine the cause of the appearance of gray or white feces, a coprogram, ultrasound and radiography of the gastrointestinal tract, endoscopy are prescribed. To eliminate the symptom, probiotics, enzyme preparations, specific antiviral and detoxifying agents are used.
A change in the color of feces is characteristic of dysbacteriosis, diseases of the liver and gallbladder, and damage to the pancreas. To determine the cause of the appearance of gray or white feces, a coprogram, ultrasound and radiography of the gastrointestinal tract, endoscopy are prescribed. To eliminate the symptom, probiotics, enzyme preparations, specific antiviral and detoxifying agents are used.
Causes of grayish-white feces
Errors in diet
Passage of gray feces in an adult is observed after the abuse of fatty foods. An excess amount of neutral fats accumulates in the intestine, due to the increased load on the pancreas, lipids are not digested and are excreted in the stool. The consistency changes - the feces become soft, “fat”, leave marks on the walls of the toilet bowl. Typically, stools increase up to 3-4 times a day.
Usually the symptoms disappear on their own, normalization of stool color occurs the next day. The reasons that provoke the discharge of grayish-white stools in infants are the incorrect introduction of complementary foods, the use of unbalanced milk formulas. A change in the color of feces occurs against the background of general weakness and lethargy of the child, constant crying and refusal to feed. These symptoms are an indication for consulting a pediatrician.
The reasons that provoke the discharge of grayish-white stools in infants are the incorrect introduction of complementary foods, the use of unbalanced milk formulas. A change in the color of feces occurs against the background of general weakness and lethargy of the child, constant crying and refusal to feed. These symptoms are an indication for consulting a pediatrician.
Dysbacteriosis
Violation of the composition of the intestinal microflora causes digestive disorders, insufficient digestion of incoming food. The feces become liquid, grayish-white or dark gray in color. The frequency of stool with dysbacteriosis increases up to 5-7 times a day, defecation is preceded by cramps and discomfort in the left abdomen. The stools have a fetid odor, a light gray coating can be seen on the surface.
Hepatitis
Infectious causes cause destruction of liver cells and disorders of bilirubin metabolism, due to which the supply of stercobilin to the intestine decreases, which stains feces in a brown hue. Gray feces appear at the height of hepatitis, the symptom is combined with a sharp darkening of the urine and yellowing of the skin. Characterized by an increase in stool and a change in its consistency, before defecation, patients feel rumbling and "seething" in the abdomen.
Gray feces appear at the height of hepatitis, the symptom is combined with a sharp darkening of the urine and yellowing of the skin. Characterized by an increase in stool and a change in its consistency, before defecation, patients feel rumbling and "seething" in the abdomen.
The duration of the symptom depends on the type of liver inflammation. In non-severe forms of viral hepatitis A and E, grayish-white feces persist for 2-3 weeks. With hepatitis B, the color of feces returns to normal after 1-2 months, in case of severe damage to the hepatic parenchyma, dark gray stools are excreted up to six months. Alcoholic hepatitis, complicated by damage to the pancreas, often cause persistent lightening of the feces.
Cholelithiasis
Isolation of grayish-white stool indicates an exacerbation of cholelithiasis and blockage of the bile duct by a calculus. In this case, bile does not enter the intestines, symptoms of obstructive jaundice develop. A person notices that the stool becomes light, almost white, the consistency of the stool often remains normal. Discoloration of the stool occurs simultaneously with severe pain in the right hypochondrium, nausea, bitterness in the mouth.
A person notices that the stool becomes light, almost white, the consistency of the stool often remains normal. Discoloration of the stool occurs simultaneously with severe pain in the right hypochondrium, nausea, bitterness in the mouth.
Pancreatitis
A change in the color of feces to white in adults occurs in chronic pancreatitis, which is characterized by pancreatic enzyme deficiency. The light color is due to the accumulation of undigested food in the stool. Fecal masses are abundant, grayish-white in color, with a sharp fetid odor. There is an increase in stool, during defecation, patients experience diffuse pain in the abdomen.
Disorders of the pancreas function are often irreversible, therefore, without the appointment of replacement therapy, the restoration of normal stool color is impossible. The patient's condition worsens under the influence of external causes - with the abuse of heavy food, alcohol intake, the disease worsens. During this period, diarrhea is disturbing with the release of a large amount of light feces, accompanied by intense pain in the left hypochondrium and epigastrium.
During this period, diarrhea is disturbing with the release of a large amount of light feces, accompanied by intense pain in the left hypochondrium and epigastrium.
Other pathologies of the liver
Damage to liver cells of various etiologies is accompanied by parenchymal jaundice, which is typically characterized by the appearance of a grayish-white stool. Such changes persist for a long time, for several months. Violation of the chair is combined with dull pain and heaviness in the right hypochondrium, nausea and vomiting with bile. Most often, discoloration of feces is caused by such reasons as:
- Cirrhosis : alcoholic, postnecrotic, biliary.
- Massive lesions : hepatocellular carcinoma, echinococcal cyst, polycystic liver.
- Functional disorders : Gilbert's syndrome, Crigler-Najjar syndrome, cholestasis of pregnancy.
Complications of pharmacotherapy
A short-term change in the color of stools to grayish-white is a natural reaction after oral administration of barium sulfate for x-ray of the digestive tract. Light fecal masses depart 10-12 hours after the study, atypical coloring of fecal masses persists for 2-3 days. Normally, these changes are not accompanied by dyspeptic disorders or abdominal pain.
Light fecal masses depart 10-12 hours after the study, atypical coloring of fecal masses persists for 2-3 days. Normally, these changes are not accompanied by dyspeptic disorders or abdominal pain.
Other reasons also provoke gray feces: taking antacids, iron. Trace elements, which are found in large quantities in these drugs, accumulate in the feces and cause the appearance of a characteristic grayish-white color. With the use of iron preparations, the color is darker up to black. Discoloration of feces is possible with prolonged use of antibiotics, anti-tuberculosis drugs.
Rare causes
- Inflammatory bowel disease : Crohn's disease, ulcerative colitis, chronic enteritis.
- Celiac disease .
- Malignant tumors : pancreatic head cancer, duodenal cancer.
- Bile duct atresia .
Diagnosis
A gastroenterologist is in charge of identifying the cause of gray stool. The specialist collects an anamnesis and complaints to establish why dyspeptic disorders appeared. Diagnostics includes instrumental imaging methods, which, according to indications, are supplemented with invasive techniques. To clarify the diagnosis, laboratory tests are prescribed. Most informative methods:
The specialist collects an anamnesis and complaints to establish why dyspeptic disorders appeared. Diagnostics includes instrumental imaging methods, which, according to indications, are supplemented with invasive techniques. To clarify the diagnosis, laboratory tests are prescribed. Most informative methods:
- Coprogram . Microscopic analysis of grayish-white feces reveals the remains of undigested food, muscle fibers, starch grains. The absence of stercobilin is pathognomonic. To confirm the diagnosis of pancreatitis, a study of the level of fecal elastase is done. Bacteriological analysis is necessary to detect dysbacteriosis and bacterial overgrowth syndrome.
- Biochemical blood test . With obstructive jaundice, cholestasis syndrome is determined - an increase in the amount of cholesterol and the enzyme alkaline phosphatase. An increase in the level of ALT and AST indicates cytolysis and parenchymal jaundice. To check the exocrine function of the pancreas, the concentration of pancreatic lipase and amylase is measured.

- Ultrasound . In order to detect the organic cause of the grayish-white hue of feces, a survey ultrasound of the abdominal cavity is performed with targeted scanning of the organs of the hepatobiliary zone. The study allows you to visualize signs of the inflammatory process of the gallbladder, heterogeneous echogenicity of the liver parenchyma, rounded volumetric neoplasms.
- Duodenal sounding . To assess the flow of bile into the intestine, several portions of bile are sequentially taken after stimulation with secretory drugs. Typically, slow bile flow or its complete absence in case of blockage of the common bile duct. The collected material is sent to the laboratory for bacteriological analysis.
- Cholangiopancreatography . White feces usually appear when the biliary tract is affected, so ERCP is required. The method involves examining the Vater papilla and bile ducts using endoscopic technologies. The study reveals stones in the bile ducts, signs of inflammatory and tumor pathologies.

Treatment
Help before diagnosis
Grayish-white stools caused by dietary errors do not need to be treated. The patient is advised to consume easily digestible foods (stewed vegetables, soups, lean meat) for several days, to reduce the amount of portions. You can't take alcohol. If during this time the stool has not returned to normal, it is necessary to consult a doctor to determine the cause of the disorder.
To avoid diarrhea and stool discoloration when taking antibiotics and other toxic drugs, it is advisable to drink natural kefir and yogurt, which are rich in beneficial bifidus and lactobacilli. Self-administration of enzyme preparations to improve digestion is not recommended, as this can provoke violations of the pancreas.
Conservative therapy
Treatment of dyspeptic disorders, including grayish-white stool, is mainly aimed at eliminating the cause of the symptoms, after which the color and consistency of the stool normalizes. Medications must be supplemented with a special therapeutic diet, which is selected depending on the disease. In clinical practice, drugs such as:
Medications must be supplemented with a special therapeutic diet, which is selected depending on the disease. In clinical practice, drugs such as:
- Enzyme preparations . Medicines containing pancreatic extract improve the processes of parietal and abdominal digestion in the small intestine. Gray feces disappear a few days after the start of medication, the severity of other dyspeptic disorders decreases.
- Probiotics . They are a mixture of beneficial bacteria that inhabit the colon and prevent the reproduction of pathogenic microflora. In adults, they are prescribed for long-term antibiotic therapy, combined with prebiotics, which stimulate the growth of bifidobacteria.
- Cholagogues . They increase the contractility of the gallbladder and expand the ducts, improve the colloidal properties of bile, so that it is released into the intestine in the right quantities. Additionally, hepatoprotectors are recommended, which protect cells from the toxic effects of bile acids.

- Antivirals . In chronic hepatitis of viral etiology, special treatment regimens are used with interferons, RNA polymerase inhibitors. Medicines reduce the viral load in the blood, inhibit the replication of the virus in the liver cells. They are combined with detoxifying agents.
Surgical treatment
Complicated cholelithiasis, which is accompanied by grayish-white stool, requires surgical intervention. Removal of small calculi is carried out during therapeutic and diagnostic ERCP, and the method of extracorporeal shock wave lithotripsy is also used. With pronounced changes in the biliary tract, drainage according to Kerr or Halstead or the formation of a choledochodigestive anastomosis is indicated.
Grayish-white feces - causes, diagnosis and treatment
Grayish-white feces is a discoloration of the stool, often accompanied by a violation of the consistency and frequency of the stool. A change in the color of feces is characteristic of dysbacteriosis, diseases of the liver and gallbladder, and damage to the pancreas. To find out the cause of the appearance of gray or white feces, a coprogram, ultrasound and radiography of the gastrointestinal tract, endoscopy are prescribed. To eliminate the symptom, probiotics, enzyme preparations, specific antiviral and detoxifying agents are used.
A change in the color of feces is characteristic of dysbacteriosis, diseases of the liver and gallbladder, and damage to the pancreas. To find out the cause of the appearance of gray or white feces, a coprogram, ultrasound and radiography of the gastrointestinal tract, endoscopy are prescribed. To eliminate the symptom, probiotics, enzyme preparations, specific antiviral and detoxifying agents are used.
Causes of grayish-white feces
Errors in diet
Passage of gray feces in an adult is observed after the abuse of fatty foods. An excess amount of neutral fats accumulates in the intestine, due to the increased load on the pancreas, lipids are not digested and are excreted in the stool. The consistency changes - the feces become soft, “fat”, leave marks on the walls of the toilet bowl. Typically, stools increase up to 3-4 times a day.
Usually the symptoms disappear on their own, normalization of stool color occurs the next day. The reasons that provoke the discharge of grayish-white stools in infants are the incorrect introduction of complementary foods, the use of unbalanced milk formulas. A change in the color of feces occurs against the background of general weakness and lethargy of the child, constant crying and refusal to feed. These symptoms are an indication for consulting a pediatrician.
The reasons that provoke the discharge of grayish-white stools in infants are the incorrect introduction of complementary foods, the use of unbalanced milk formulas. A change in the color of feces occurs against the background of general weakness and lethargy of the child, constant crying and refusal to feed. These symptoms are an indication for consulting a pediatrician.
Dysbacteriosis
Violation of the composition of the intestinal microflora causes digestive disorders, insufficient digestion of incoming food. The feces become liquid, grayish-white or dark gray in color. The frequency of stool with dysbacteriosis increases up to 5-7 times a day, defecation is preceded by cramps and discomfort in the left abdomen. The stools have a fetid odor, a light gray coating can be seen on the surface.
Hepatitis
Infectious causes cause destruction of liver cells and disorders of bilirubin metabolism, due to which the supply of stercobilin to the intestine decreases, which stains feces in a brown hue. Gray feces appear at the height of hepatitis, the symptom is combined with a sharp darkening of the urine and yellowing of the skin. Characterized by an increase in stool and a change in its consistency, before defecation, patients feel rumbling and "seething" in the abdomen.
Gray feces appear at the height of hepatitis, the symptom is combined with a sharp darkening of the urine and yellowing of the skin. Characterized by an increase in stool and a change in its consistency, before defecation, patients feel rumbling and "seething" in the abdomen.
The duration of the symptom depends on the type of liver inflammation. In non-severe forms of viral hepatitis A and E, grayish-white feces persist for 2-3 weeks. With hepatitis B, the color of feces returns to normal after 1-2 months, in case of severe damage to the hepatic parenchyma, dark gray stools are excreted up to six months. Alcoholic hepatitis, complicated by damage to the pancreas, often cause persistent lightening of the feces.
Cholelithiasis
Isolation of grayish-white stool indicates an exacerbation of cholelithiasis and blockage of the bile duct by a calculus. In this case, bile does not enter the intestines, symptoms of obstructive jaundice develop. A person notices that the stool becomes light, almost white, the consistency of the stool often remains normal. Discoloration of the stool occurs simultaneously with severe pain in the right hypochondrium, nausea, bitterness in the mouth.
A person notices that the stool becomes light, almost white, the consistency of the stool often remains normal. Discoloration of the stool occurs simultaneously with severe pain in the right hypochondrium, nausea, bitterness in the mouth.
Pancreatitis
A change in the color of feces to white in adults occurs in chronic pancreatitis, which is characterized by pancreatic enzyme deficiency. The light color is due to the accumulation of undigested food in the stool. Fecal masses are abundant, grayish-white in color, with a sharp fetid odor. There is an increase in stool, during defecation, patients experience diffuse pain in the abdomen.
Disorders of the pancreas function are often irreversible, therefore, without the appointment of replacement therapy, the restoration of normal stool color is impossible. The patient's condition worsens under the influence of external causes - with the abuse of heavy food, alcohol intake, the disease worsens. During this period, diarrhea is disturbing with the release of a large amount of light feces, accompanied by intense pain in the left hypochondrium and epigastrium.
During this period, diarrhea is disturbing with the release of a large amount of light feces, accompanied by intense pain in the left hypochondrium and epigastrium.
Other pathologies of the liver
Damage to liver cells of various etiologies is accompanied by parenchymal jaundice, which is typically characterized by the appearance of a grayish-white stool. Such changes persist for a long time, for several months. Violation of the chair is combined with dull pain and heaviness in the right hypochondrium, nausea and vomiting with bile. Most often, discoloration of feces is caused by such reasons as:
- Cirrhosis : alcoholic, postnecrotic, biliary.
- Massive lesions : hepatocellular carcinoma, echinococcal cyst, polycystic liver.
- Functional disorders : Gilbert's syndrome, Crigler-Najjar syndrome, cholestasis of pregnancy.
Complications of pharmacotherapy
A short-term change in the color of stools to grayish-white is a natural reaction after oral administration of barium sulfate for x-ray of the digestive tract. Light fecal masses depart 10-12 hours after the study, atypical coloring of fecal masses persists for 2-3 days. Normally, these changes are not accompanied by dyspeptic disorders or abdominal pain.
Light fecal masses depart 10-12 hours after the study, atypical coloring of fecal masses persists for 2-3 days. Normally, these changes are not accompanied by dyspeptic disorders or abdominal pain.
Other reasons also provoke gray feces: taking antacids, iron. Trace elements, which are found in large quantities in these drugs, accumulate in the feces and cause the appearance of a characteristic grayish-white color. With the use of iron preparations, the color is darker up to black. Discoloration of feces is possible with prolonged use of antibiotics, anti-tuberculosis drugs.
Rare causes
- Inflammatory bowel disease : Crohn's disease, ulcerative colitis, chronic enteritis.
- Celiac disease .
- Malignant tumors : pancreatic head cancer, duodenal cancer.
- Bile duct atresia .
Diagnosis
A gastroenterologist is in charge of identifying the cause of gray stool. The specialist collects an anamnesis and complaints to establish why dyspeptic disorders appeared. Diagnostics includes instrumental imaging methods, which, according to indications, are supplemented with invasive techniques. To clarify the diagnosis, laboratory tests are prescribed. Most informative methods:
The specialist collects an anamnesis and complaints to establish why dyspeptic disorders appeared. Diagnostics includes instrumental imaging methods, which, according to indications, are supplemented with invasive techniques. To clarify the diagnosis, laboratory tests are prescribed. Most informative methods:
- Coprogram . Microscopic analysis of grayish-white feces reveals the remains of undigested food, muscle fibers, starch grains. The absence of stercobilin is pathognomonic. To confirm the diagnosis of pancreatitis, a study of the level of fecal elastase is done. Bacteriological analysis is necessary to detect dysbacteriosis and bacterial overgrowth syndrome.
- Biochemical blood test . With obstructive jaundice, cholestasis syndrome is determined - an increase in the amount of cholesterol and the enzyme alkaline phosphatase. An increase in the level of ALT and AST indicates cytolysis and parenchymal jaundice. To check the exocrine function of the pancreas, the concentration of pancreatic lipase and amylase is measured.

- Ultrasound . In order to detect the organic cause of the grayish-white hue of feces, a survey ultrasound of the abdominal cavity is performed with targeted scanning of the organs of the hepatobiliary zone. The study allows you to visualize signs of the inflammatory process of the gallbladder, heterogeneous echogenicity of the liver parenchyma, rounded volumetric neoplasms.
- Duodenal sounding . To assess the flow of bile into the intestine, several portions of bile are sequentially taken after stimulation with secretory drugs. Typically, slow bile flow or its complete absence in case of blockage of the common bile duct. The collected material is sent to the laboratory for bacteriological analysis.
- Cholangiopancreatography . White feces usually appear when the biliary tract is affected, so ERCP is required. The method involves examining the Vater papilla and bile ducts using endoscopic technologies. The study reveals stones in the bile ducts, signs of inflammatory and tumor pathologies.

Treatment
Help before diagnosis
Grayish-white stools caused by dietary errors do not need to be treated. The patient is advised to consume easily digestible foods (stewed vegetables, soups, lean meat) for several days, to reduce the amount of portions. You can't take alcohol. If during this time the stool has not returned to normal, it is necessary to consult a doctor to determine the cause of the disorder.
To avoid diarrhea and stool discoloration when taking antibiotics and other toxic drugs, it is advisable to drink natural kefir and yogurt, which are rich in beneficial bifidus and lactobacilli. Self-administration of enzyme preparations to improve digestion is not recommended, as this can provoke violations of the pancreas.
Conservative therapy
Treatment of dyspeptic disorders, including grayish-white stool, is mainly aimed at eliminating the cause of the symptoms, after which the color and consistency of the stool normalizes. Medications must be supplemented with a special therapeutic diet, which is selected depending on the disease. In clinical practice, drugs such as:
Medications must be supplemented with a special therapeutic diet, which is selected depending on the disease. In clinical practice, drugs such as:
- Enzyme preparations . Medicines containing pancreatic extract improve the processes of parietal and abdominal digestion in the small intestine. Gray feces disappear a few days after the start of medication, the severity of other dyspeptic disorders decreases.
- Probiotics . They are a mixture of beneficial bacteria that inhabit the colon and prevent the reproduction of pathogenic microflora. In adults, they are prescribed for long-term antibiotic therapy, combined with prebiotics, which stimulate the growth of bifidobacteria.
- Cholagogues . They increase the contractility of the gallbladder and expand the ducts, improve the colloidal properties of bile, so that it is released into the intestine in the right quantities. Additionally, hepatoprotectors are recommended, which protect cells from the toxic effects of bile acids.