Umbilical cord in the womb
What happens if the umbilical cord is around my baby’s neck? | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
May 22, 2018
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
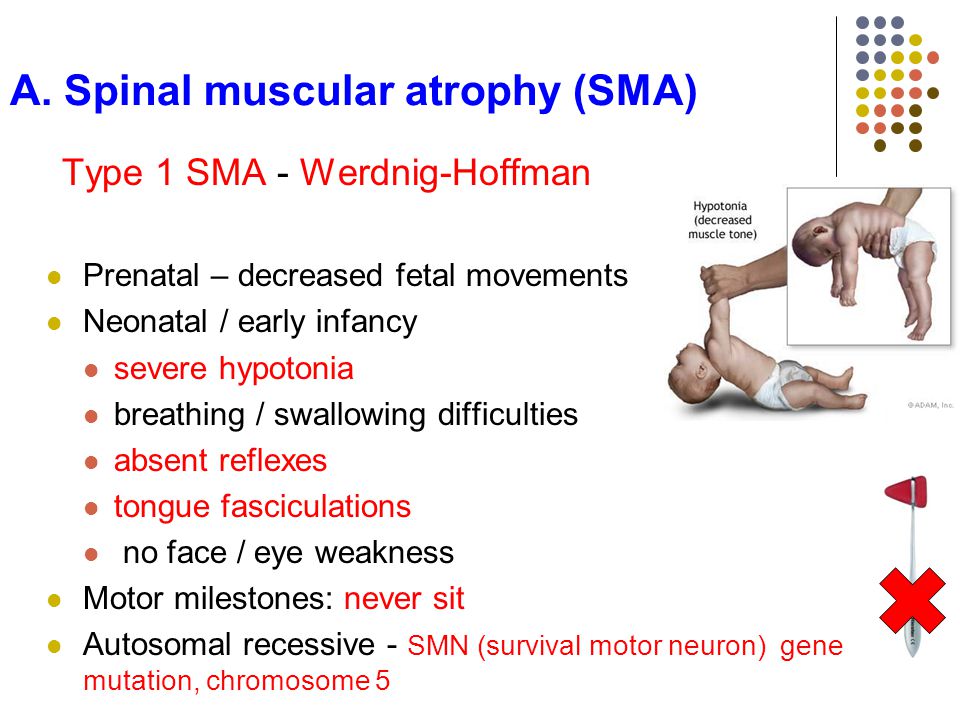
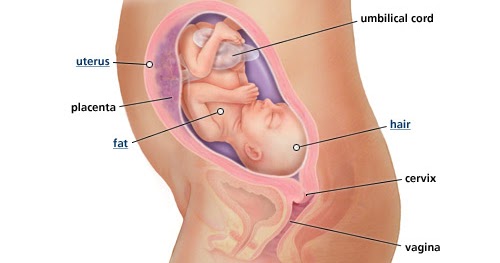
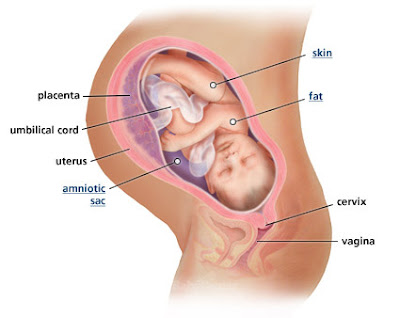
An umbilical cord is a lifeline for a baby in the womb. Running from the baby’s abdomen to the placenta, the umbilical cord usually contains three blood vessels and is about 21” long. It provides oxygen, blood, and nutrients to the developing fetus. However, later in pregnancy many women fear the thought of the umbilical cord wrapping around the baby’s neck and the possibility of problems during delivery or even a stillbirth.
Pregnant women: Breathe a sigh of relief. Nuchal cords are surprisingly common and unlikely to cause problems during pregnancy or at birth.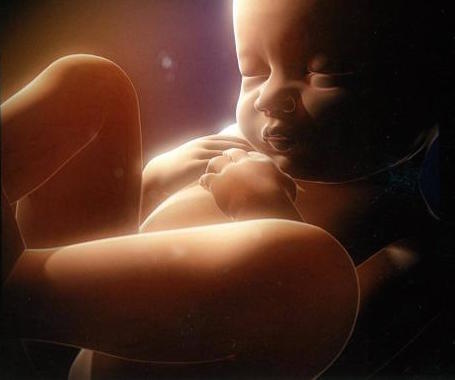 Estimates suggest that 20 to 30 percent of all deliveries involve a nuchal cord. And a 2018 study in the American Journal of Obstetrics and Gynecology reports that, the majority of time, babies do just fine when one is present.
Estimates suggest that 20 to 30 percent of all deliveries involve a nuchal cord. And a 2018 study in the American Journal of Obstetrics and Gynecology reports that, the majority of time, babies do just fine when one is present.
What causes nuchal cords?
Random fetal movement is the primary cause of a nuchal cord. Other factors that might increase the risk of the umbilical cord wrapping around a baby’s neck include an extra-long umbilical cord or excess amniotic fluid that allows more fetal movement.
Nuchal cords typically are discovered at birth. Occasionally, patients ask if we can see them on ultrasound, which sometimes we can. There’s no way yet to prevent nuchal cords or unwind them from a baby’s neck in the womb. But when a baby is born with a nuchal cord, your doctor will know what to do because it happens so frequently.
The colored sections of the ultrasound show that the umbilical cord is under the baby’s chin.
When is a nuchal cord dangerous?
If the cord is looped around the neck or another body part, blood flow through the entangled cord may be decreased during contractions. This can cause the baby’s heart rate to fall during contractions. Prior to delivery, if blood flow is completely cut off, a stillbirth can occur.
In the 2018 study, 12 percent of deliveries had a nuchal cord. Most babies with a nuchal cord had just a single loop around the neck. Fortunately, there was no increased risk for growth problems, stillbirth, or lower Apgar scores in this group.
What happens during delivery?
Since the vast majority of time we don’t know if a baby will have a nuchal cord, it is routine that the doctor will check the baby’s neck for a nuchal cord after the baby’s head is delivered. Usually the cord is loose and can be slipped over the baby’s head. At times it might be too tight to easily slip over the head, and the doctor or midwife will clamp and cut the cord before the baby’s shoulders are delivered. This keeps the cord from tearing away from the placenta when the rest of the baby’s body is delivered.
This keeps the cord from tearing away from the placenta when the rest of the baby’s body is delivered.
Remember, a nuchal cord is common, and complications caused by the condition are rare. If you’ve been told your baby has a nuchal cord and you have questions, call us at 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.
 D.
D.
August 23, 2022
More Articles
What Are Signs of Umbilical Cord Problems?
Birth Injury Attorney (Home) / Traumatic Birth Injuries / What Are Signs of Umbilical Cord Problems?
An umbilical cord may become compressed or damaged before or during childbirth. Common signs of umbilical cord problems include an irregular fetal heartbeat and decreased or low fetal movement. Umbilical cord problems can be a serious threat to the child’s health and should be carefully monitored and treated as necessary.
The information in this post was compiled from government, educational non-profit, and medical expert sources.
Keep reading to learn about the signs of umbilical cord problems.
The Umbilical Cord Delivers Oxygen to the Baby
Before exploring the common problems with umbilical cords, we should first examine why the umbilical cord is so important.
The umbilical cord connects the mother to the baby as the baby develops in the womb. The umbilical cord starts at the mother’s placenta and connects to an opening in the baby’s stomach.
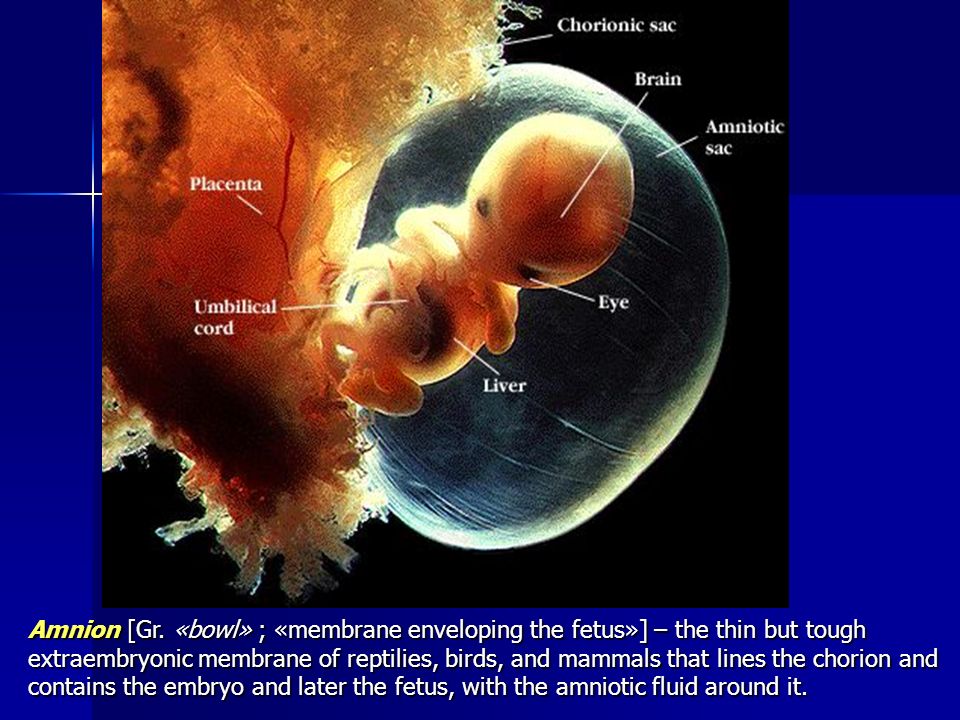
During pregnancy, the umbilical cord delivers vital nutrients and oxygen from the mother to the baby. The umbilical cord has one vein and two arteries surrounded by a protective layer. The protective layer is made up of a substance called Wharton’s jelly and wrapped in a membrane called the amnion.
The vein delivers blood full of nutrients and oxygen to the baby, while the arteries remove deoxygenated blood and waste from the baby back to the placenta.
After the baby is born, the umbilical cord is clamped and cut. There are no nerves within an umbilical cord, so this is not painful for the baby or for the mother. Within a couple of weeks, the clamped stump of the umbilical cord will eventually fall off, leaving behind the baby’s belly button.
In summary: if the proper function of the baby’s umbilical cord is vital to deliver nutrients and oxygen to the baby.

Most Common Umbilical Cord Problems
Here are some of the most common umbilical cord issues that can interfere with the health of the baby:
- Umbilical cord compression
- Nuchal cords
- True knots
- Umbilical cord prolapse
- Short umbilical cords
- Vasa previa
- Umbilical cord infection
In the next sections, we will learn about the signs of each problem and what each problem means for the baby.
Umbilical Cord Compression
One common umbilical cord problem is due to compression. Compression occurs when pressure partially or completely stops the flow of blood through the umbilical cord. Babies can survive short periods of umbilical cord compression, but if an adequate flow of blood to the baby is not re-established, the baby may suffer serious birth injuries. As we covered in the previous sections, this condition is dangerous because babies need nutrients and oxygen to remain healthy during development.
As we covered in the previous sections, this condition is dangerous because babies need nutrients and oxygen to remain healthy during development.
Signs of umbilical cord compression may include less activity from the baby, observed as a decrease in movement, or an irregular heart beat, which can be observed by fetal heart monitoring.
Common causes of umbilical cord compression include: nuchal cords, true knots, and umbilical cord prolapse.
Nuchal Cords
Nuchal cord is the medical term for when an umbilical cord becomes wrapped once or more times around the baby’s neck within the womb. Nuchal cord with one loop of cord around the baby’s neck may occur in approximately 20% of deliveries.
Nuchal cord is usually caused by the baby’s movement through a loop of the umbilical cord. Nuchal cord may be detectable by electronic fetal heart monitoring. Certain patterns of the baby’s heart rate, like “variable decelerations” of the heart rate, are often associated with nuchal cord.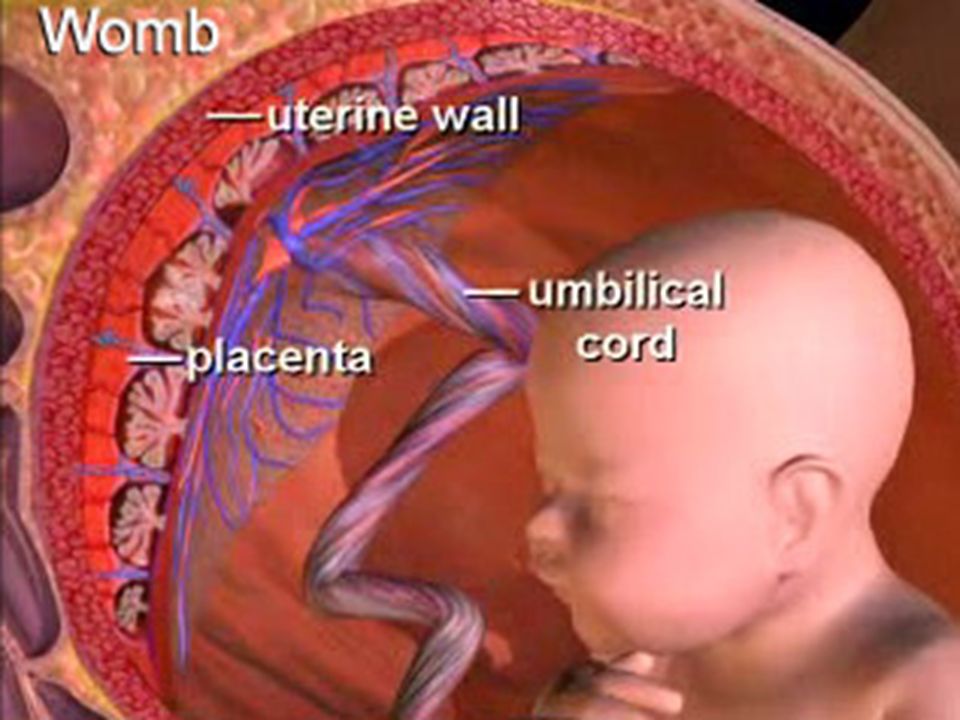 Nuchal cord may sometimes be visualized on color Doppler ultrasound.
Nuchal cord may sometimes be visualized on color Doppler ultrasound.
Nuchal cords are a surprisingly common condition, occurring in as many as 35% of pregnancies. A nuchal cord becomes dangerous when the cord wraps tightly around the baby’s neck, often during labor and delivery, and the flow of blood to the baby is interrupted.
In a dangerous situation caused by a nuchal cord, a c-section delivery may be necessary to quickly deliver the baby before the lack of blood flow causes the baby to suffer a permanent brain injury. Common injuries that can be caused by nuchal cords include birth asphyxiation, HIE, and Cerebral Palsy.
If you believe that the umbilical cord was wrapped around your baby’s neck and your baby has suffered an injury, we are happy to talk with you to determine whether or not the injury could have been prevented.
True Knots
True knots are the medical term for when the umbilical cord gets twisted like a rope into a knot. True knots can form simply by the baby’s movement within the mother’s womb. Other causes can include monoamniotic twins (when twins share the same amniotic sac), polyhydramnios (excessive amounts of amniotic fluid), overly long umbilical cords, smaller than normal fetuses, gestational diabetes, and amniocentesis (a procedure to test the amniotic fluid). True knots also can form more often in male fetuses or when the mother has had several previous pregnancies.
Other causes can include monoamniotic twins (when twins share the same amniotic sac), polyhydramnios (excessive amounts of amniotic fluid), overly long umbilical cords, smaller than normal fetuses, gestational diabetes, and amniocentesis (a procedure to test the amniotic fluid). True knots also can form more often in male fetuses or when the mother has had several previous pregnancies.
If a baby’s activity decreases after 37 weeks, that is a common sign of a true knot. Medical professionals should remain alert for decreased activity and should test for umbilical cord problems as needed.
Medical professionals can check for a reassuring heartbeat from the baby and monitor the baby’s activity to determine whether further intervention is required. More on True & False Knots
Umbilical Cord Prolapse
A prolapse means that the umbilical cord has moved down the birth canal before or along side of the baby. Ideally, the umbilical cord should follow the baby out through the birth canal. If the cord gets ahead of the baby or moves along side the baby, a dangerous situation can develop leading to birth asphyxia, HIE, and other birth injuries.
If the cord gets ahead of the baby or moves along side the baby, a dangerous situation can develop leading to birth asphyxia, HIE, and other birth injuries.
If a mother or a medical professional becomes aware of a possible cord prolapse, the medical professionals should take immediate steps to monitor and intervene as necessary–particularly if the prolapse occurs within the third trimester. By carefully monitoring the situation and by delivering the baby by c-section, potential serious injuries may be avoided.
In summary: umbilical cord compression can be caused by nuchal cords, true knots, and umbilical cord prolapse. In all of these circumstances, medical professionals must carefully monitor the baby’s health. If necessary, the medical professionals should consider ordering an emergency c-section to prevent further injury.
Learn more about prolapsed umbilical cord
Short Umbilical Cords
If the baby’s umbilical cord is short the baby’s movements may stretch and tear either the umbilical cord or the mother’s placenta (known as placental abruption). Ideally, an umbilical cord should be long enough for the baby to move without stretching the cord, but not so long as to easily get knotted or tangled.
Ideally, an umbilical cord should be long enough for the baby to move without stretching the cord, but not so long as to easily get knotted or tangled.
If a short umbilical cord causes placental abruption, the mother may hemorrhage a lot of blood, which can be harmful to both the baby and the mother. Medical professionals should be prepared to perform a c-section or an operative delivery with forceps or a vacuum extractor if necessary (although forceps and vacuum extractor methods can also be dangerous and should not be attempted if the medical professional is not well trained and experienced with these methods).
Vasa Previa
Vasa (from the latin for vessels) previa (from the latin for before) is a condition where the fetal blood vessels move out of the umbilical cord and into the amniotic sac membranes across the birth canal. In this position, the vessels are at risk for rupture during labor and delivery, which can lead to massive blood loss and permanent injury of the baby.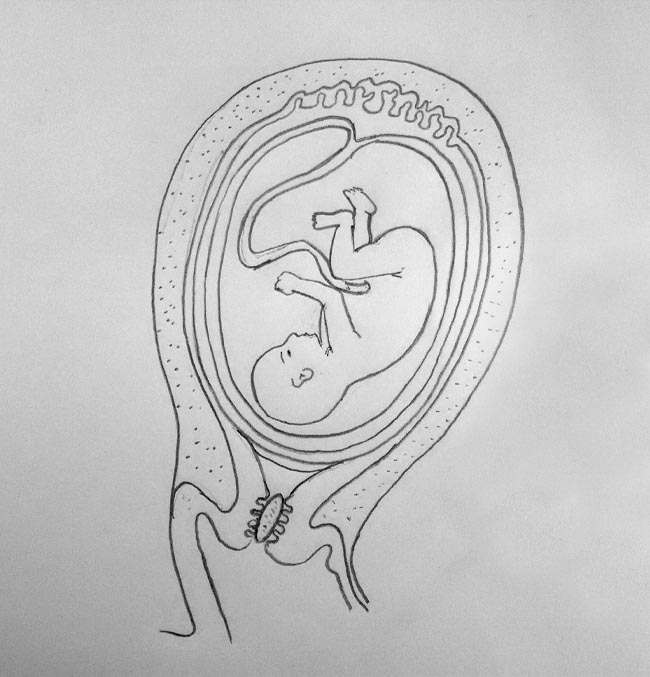
If vasa previa is detected, medical professionals should consider an early c-section to prevent potential birth injuries. If the blood vessels are ruptured during delivery, a blood transfusion may be necessary immediately after birth.
Umbilical Cord Infection
When the fetal membranes become infected, that infection can spread to the umbilical cord, the placenta, the fetus, and the amniotic fluid. This is called an intra-amniotic infection, or an IAI.
An IAI or an infection of the umbilical cord is called funisitis. An infection of the umbilical cord can potentially lead to fetal inflammatory response syndrome, or FIRS, and can cause pre-term birth, neonatal sepsis, periventricular leukomalacia, and Cerebral Palsy.
Antibiotics can potentially prevent a serious birth injury from occurring.
Treatment for Umbilical Cord Based Injuries
As we’ve already discussed in this article, careful monitoring, an early c-section or operative delivery, along with blood transfusions are all potential treatment strategies to prevent injuries caused by umbilical cord problems.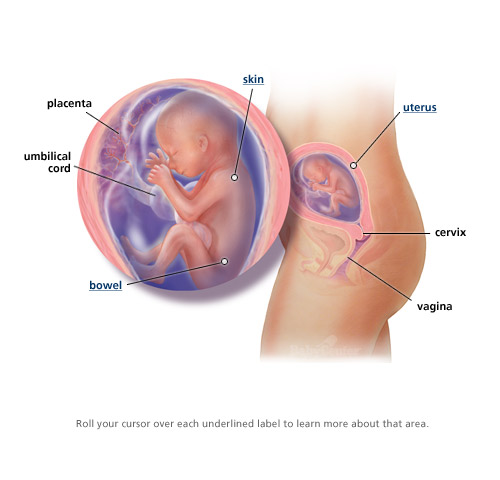
An additional treatment strategy that becomes available once the child has been delivered is cooling therapy. Cooling therapy can be used shortly after birth to try and slow or stop permanent injuries caused by lack of blood flow to the brain.
Use this infographic on your site
<a href="https://browntrialfirm.com/" target="blank"><img src="https://browntrialfirm.com/infographics/infant-cooling-therapy-btf.jpg" alt="Cooling Therapy Infographic" title="" /></a>
Infant Cooling Therapy
How does it work?
6-24 hour window
Infant cooling therapy is typically applied within six hours of birth. Some new studies suggest it may be effective up to 24 hours after birth.
Blanket or cap
Cooling therapy is applied by either placing the baby on a cooling blanket or by placing a cooling cap on the baby’s head.
33 C / 91.
 4 F
4 FThe baby’s body temperature is cooled down to 33c or 91.4f in an effort to slow down or prevent potential brain injuries.
2 – 3 days
Although treatment may vary from case to case depending on severity, two to three days is a typical length for cooling therapy to be applied.
Sources:
What is the umbilical cord?. (2018). nhs.uk. Retrieved 17 February 2020, from https://www.nhs.uk/common-health-questions/pregnancy/what-is-the-umbilical-cord/
Umbilical cord conditions. (2020). Marchofdimes.org. Retrieved 17 February 2020, from https://www.marchofdimes.org/complications/umbilical-cord-conditions.aspx
What happens if the umbilical cord is around my baby’s neck? | Your Pregnancy Matters | UT Southwestern Medical Center. (2020). Utswmed.org. Retrieved 17 February 2020, from https://utswmed.org/medblog/nuchal-cord-during-pregnancy/
Contact a Cerebral Palsy and Birth Injury Attorney
Getting help for a child with a birth injury can make a big difference. Early intervention and early treatment is often key to helping improve a child’s wellbeing. You must act quickly.
Early intervention and early treatment is often key to helping improve a child’s wellbeing. You must act quickly.
If you have questions about whether your child’s birth injury was caused by a preventable medical error, then our attorneys at Brown Trial Firm may be able to help.
Case Review at No Cost or Obligation
If you would like help investigating your child’s birth injury, please contact us. Our birth injury attorneys will be happy to give you a free case evaluation. We can also point you to great non-legal resources that can help you figure out your next steps.
Many birth injuries that cause cerebral palsy could have been prevented. Don’t wait, get help today. Call +1 (866) 393-2611, email us at [email protected], or use the live chat button for 24/7 assistance.
Our birth injury attorneys represent clients in all types of cases including:
Brain Damage and Birth Injuries
- Cerebral Palsy
- Caput Succedaneum and Cephalohematoma
- Neonatal Intracranial Hemorrhage (Childbirth Brain Bleeds)
- Hydrocephalus (Extra Fluid in the Brain Cavity)
- Cervical Dystonia
- Hemiplegia (Brain or Spinal Cord Injury)
- Hemorrhagic Stroke
- Neonatal Stroke
- HIE
- Periventricular Leukomalacia (PVL) Brain Injury
- Infant Seizures
- Spastic Diplegia (Spasticity in the Legs)
- Top Risks for Birth Injuries
Nerve and Spinal Cord Birth Injuries
- Facial Paralysis
- Spinal Cord Injuries
- Bell’s Palsy
- Brachial Plexus Nerves & Erb’s Palsy
Bone Birth Injuries
- Fractures and Broken Bones At Birth
- Baby’s Skull Not Fused at Birth
Birth Injuries from Medications or Procedures
Procedures
- G-Tubes for Newborns
- Medical Errors
- Cesarean Section & Birth Injury
- Negligence in Brain Cooling Treatment
- Craniosacral Therapy
Medications
- Zofran Birth Injury
- Pitocin Birth Injuries
- Medication Side Effects
- Uterine Hyperstimulation
Labor and Delivery Complications
Birth injuries from failure to diagnose or provide appropriate treatment
- Fetal Intolerance to Labor
- Jaundice (Kernicterus)
- Breech Position
- Placental Complications
- Placental Problems
- Umbilical Cord Problems
- Uterine Rupture
- Cervical Incompetence (Insufficiency)
- Blighted Ovum
- Necrotizing Enterocolitis (NEC) - Intestinal Inflammation
- Cephalopelvic Disproportion
- Meconium Aspiration Syndrome
- Amniotic Fluid Embolism
- Birth Injury from Premature Delivery
- Developmental Delays
- Abnormal Cord Insertion
- Infections at Birth
- Chorioamnionitis Bacterial Infection
- Premature birth
- Oxygen Deprivation
- Listeria
Pregnancy Complications
- Obesity Related Birth Injuries
- Intrauterine Growth Restriction
- Blood Clots During Pregnancy
- Ectopic Pregnancy Misdiagnosis
- Myths & Facts About Birth Injuries
- Bacterial Vaginosis
- Gestational Diabetes
- Maternal Mortality Risk
Traumatic Birth Injury Attorneys & the Law
- Statute of Limitations
- How to Find the Best Birth Injury Attorney
- Determining Fault in Birth Injury Trials
Umbilical cord: everything you need to know.

06/29/2022
Future parents often know about the umbilical cord (umbilical cord) only that it is clamped after the birth of a child. Meanwhile, the umbilical cord plays an important role in the course of a healthy pregnancy, and the blood and tissues of the umbilical cord are a kind of bio-insurance for the health of your family for many years and even decades in the future.
So, what are the functions of the umbilical cord?
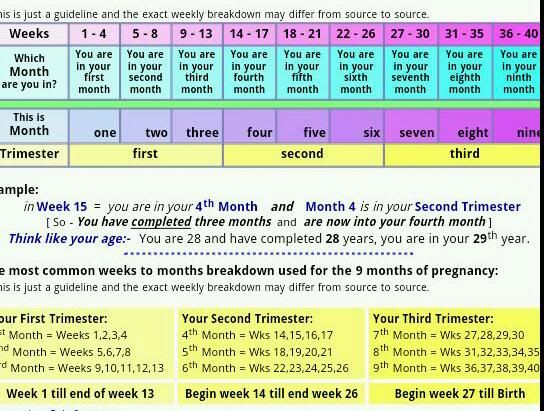
The umbilical cord is a wonderful thread that connects mother and child for 9months of pregnancy. A narrow, tube-like structure, the umbilical cord runs from the belly of the developing embryo to the placenta, delivering oxygen and nutrient-rich blood and removing the baby's waste products. It begins to develop about 5 weeks after conception. As the baby grows, the umbilical cord gets longer and longer, forming a neat coil in the womb, until it reaches its full length (50-60 cm) at about 28 weeks.
There are blood vessels inside the umbilical cord: two arteries and one vein. The vessels are located in the thickness of a powerful connective tissue that protects them from possible compression. The vein delivers fresh oxygen and nutrients to the baby through the placenta, which in turn is connected to the mother's bloodstream. The arteries transport the waste products of the child. The path is the same: through the placenta, they enter the mother's bloodstream and are filtered through her kidneys.
The blood that flows through the umbilical cord is called cord blood. It is a rich source of hematopoietic stem cells. These cells can be harvested and stored for use in more than 80 treatments for diseases including leukemia, lymphomas, metabolic disorders, various anemias, and more.
The connective tissue that protects the vessels in the umbilical cord is called Wharton's jelly. It is a gelatinous substance composed mainly of collagen. It is Wharton's jelly that allows the umbilical cord to do its job throughout pregnancy, preventing it from contracting or bending. In addition, it is in the connective tissue of the umbilical cord that mesenchymal stem cells (MSCs) are located, which are currently being actively explored as a potential treatment for a wide range of serious diseases. Like cord blood, cord tissue and MSCs can be banked.
In addition, it is in the connective tissue of the umbilical cord that mesenchymal stem cells (MSCs) are located, which are currently being actively explored as a potential treatment for a wide range of serious diseases. Like cord blood, cord tissue and MSCs can be banked.
What happens to the umbilical cord after the baby is born?
When a baby is born, the umbilical cord is no longer needed, so it is cut. This process is quick and painless; since the umbilical cord contains no nerves, the baby will not feel anything.
Cords are usually discarded unless the family decides to collect and store cord blood and/or cord tissue from their child. The collection of these biomaterials is quick, easy and low risk, however, the collection needs to be planned in advance for the family: biobanks must be notified of the intention to save blood and tissue, and parents will need to have a cord blood and / or tissue collection kit (most banks recommend purchasing set at least six weeks before the due date).
CryoCentre LLC works on an all-inclusive basis: when concluding a Contract for stem cell collection, we form and send a set to the maternity hospital specified by the clients. If the place of future birth is not determined, the set is kept at the parents' home in the appropriate conditions determined by the bank.
About the pulsation of the umbilical cord.
Delayed cord clamping is 30-60 seconds after the baby is born. This practice is recommended by major medical organizations, including the World Health Organization (WHO). Delayed cord clamping allows more fetal red blood cells from the placenta to pass through the cord into the baby's body, as recommended. This maintains iron stores during the first months of life, reducing the risk of developing iron deficiency anemia. This practice is also believed to promote healthy brain development in the first few years of life. Delayed cord clamping can be performed for both vaginal delivery and caesarean delivery, and is suitable for term and premature babies. It is also fully compatible with newborn cord blood banking.
It is also fully compatible with newborn cord blood banking.
There is an Indonesian form of childbirth, the so-called "lotus birth". In this case, the umbilical cord is not cut and the baby remains attached to the placenta until two weeks after birth. This practice is not generally accepted and has not been shown to provide any health benefits to infants. The vast majority of medical practitioners advise against doing this, arguing that lotus childbirth is deadly for newborns, as it seriously increases the risk of bacterial infections.
If you have questions about cord blood and/or cord storage, talk to your doctor, call CryoCentre LLC to make an informed decision for your family's bioinsurance health.
Umbilical cord - norm and pathology
The umbilical cord is a spiral tube that connects the fetus to the placenta. Outside, the umbilical cord is covered with fetal membranes. It contains two arteries and one vein.
Arterial blood flows through the vein of the umbilical cord, carrying oxygen to the organs of the fetus. The umbilical arteries carry venous blood from the fetus to the placenta, this blood contains the metabolic products of the fetus. The vessels of the umbilical cord are in a special gelatinous substance that fixes them and protects them from injury, and also exchanges substances between the fetal blood and amniotic fluid. The umbilical cord begins to form from 2-3 weeks of pregnancy and grows with the baby. By the time of birth, its length is 45–60 cm (the length of the umbilical cord, on average, corresponds to the height of the child), and its diameter is 1.5–2 cm.
The umbilical cord can attach to the placenta in different ways. In some cases, attachment occurs in the center of the placenta (central attachment), in others - on the side (lateral attachment). Sometimes the umbilical cord is attached to the membranes, not reaching the placenta itself (shell attachment). In these cases, the vessels of the umbilical cord approach the placenta between the membranes. Such attachment of the placenta is a risk factor for the occurrence of fetal placental insufficiency.
In these cases, the vessels of the umbilical cord approach the placenta between the membranes. Such attachment of the placenta is a risk factor for the occurrence of fetal placental insufficiency.
The umbilical cord may also have features such as true and false nodes. False nodes are local thickening of the umbilical cord due to varicose veins of the umbilical cord or accumulation of Wharton's jelly. They do not affect the development of the fetus and the process of childbirth. True umbilical cord knots form early in pregnancy, when the fetus is still small, allowing it to slip through the umbilical cord loop. True umbilical cord knots can affect the outcome of labor. When the umbilical cord is pulled, the knot is tightened, the flow and outflow of blood through the vessels stop. In this case, acute fetal hypoxia occurs.
The pathology of the development of the umbilical cord is also a condition in which only one umbilical artery is formed instead of two; in some fetuses with one umbilical artery, various malformations are observed. The reason for this formation of the umbilical cord can be factors that cause fetal malformations - the so-called teratogenic factors (chemicals, certain drugs, ionizing radiation, genetic diseases of the parents).
The reason for this formation of the umbilical cord can be factors that cause fetal malformations - the so-called teratogenic factors (chemicals, certain drugs, ionizing radiation, genetic diseases of the parents).
Some problems may arise in connection with the shortening of the umbilical cord. Shortening of the umbilical cord can be divided into absolute and relative. With an absolute shortening of the umbilical cord, the length of the umbilical cord is less than 45 cm. During pregnancy, this condition does not affect the development of the baby. During childbirth, both with relative and absolute shortness of the umbilical cord, due to its tension, the placenta can prematurely exfoliate, which the umbilical cord pulls along, which creates a direct threat to the life of the fetus.
False shortening of the umbilical cord occurs when the umbilical cord is wrapped around the neck and torso of the fetus. The cause of umbilical cord entanglement may be its excessively long length (more than 70 cm), as well as increased fetal motor activity, which may be associated with chronic intrauterine fetal hypoxia. The causes of chronic lack of oxygen are different - these are maternal diseases, fetal diseases, and placental pathology. The entanglement of the umbilical cord can be single, double or even triple. During pregnancy, this condition usually does not affect the fetus, but problems can occur during childbirth. Tension or clamping of the vessels of the umbilical cord leads to disruption of blood flow.
The causes of chronic lack of oxygen are different - these are maternal diseases, fetal diseases, and placental pathology. The entanglement of the umbilical cord can be single, double or even triple. During pregnancy, this condition usually does not affect the fetus, but problems can occur during childbirth. Tension or clamping of the vessels of the umbilical cord leads to disruption of blood flow.
Conditions such as shortening of the umbilical cord (absolute and relative) and true knots of the umbilical cord during childbirth can lead to acute intrauterine fetal hypoxia. It is manifested by a change in the number of heartbeats. (The normal fetal heart rate is 120-160 beats per minute.) When acute intrauterine fetal hypoxia occurs, primordial feces (meconium) appears in the amniotic fluid, the water turns green. The appearance of all these symptoms requires emergency treatment. First of all, it is necessary to eliminate the cause of hypoxia, which is achieved by early delivery. The method of delivery depends on the period of labor and how far the presenting part of the fetus (head or pelvic end) has advanced along the birth canal. If acute hypoxia occurs during pregnancy or in the first stage of childbirth, the woman is given a caesarean section. In the second stage of labor, when the head or pelvic end is already close to the exit from the small pelvis, various obstetric aids are used to speed up the completion of the second stage of labor.
The method of delivery depends on the period of labor and how far the presenting part of the fetus (head or pelvic end) has advanced along the birth canal. If acute hypoxia occurs during pregnancy or in the first stage of childbirth, the woman is given a caesarean section. In the second stage of labor, when the head or pelvic end is already close to the exit from the small pelvis, various obstetric aids are used to speed up the completion of the second stage of labor.
Fortunately, this condition does not occur often. Therefore, entanglement of the umbilical cord and knots of the umbilical cord are not an absolute indication for a planned caesarean section (it is impossible to diagnose the absolute shortness of the umbilical cord before delivery). These states are relative indications for surgery, i.e. caesarean section is done only in cases where, in addition to them, there are also other relative indications for surgery (the age of the woman is over 30 years old, mild forms of preeclampsia, etc. ).
).
The only method that allows us to assume the pathology of the umbilical cord is an ultrasound scan. With the help of ultrasound, abnormalities of the umbilical cord can be detected, such as abnormal development of blood vessels (the only artery of the umbilical cord), true and false knots of the umbilical cord, entanglement of the umbilical cord. But the length of the umbilical cord during pregnancy is almost impossible to determine.
Special mention should be made of the diagnosis of entanglement of the umbilical cord. Sometimes, during examination, only loops of the umbilical cord in the neck are visible, but it is impossible to determine whether they wrap around the neck. In these cases, a Doppler study helps, during which it is possible to study the movement of blood through the vessels, including the umbilical cord. In addition, during childbirth, the cardiotocography method is used, which allows you to monitor the number of heartbeats, or listen to the fetal heartbeat with a stethoscope.