Mouth infections in babies
Oral thrush in babies | Pregnancy Birth and Baby
Oral thrush in babies | Pregnancy Birth and Baby beginning of content3-minute read
Listen
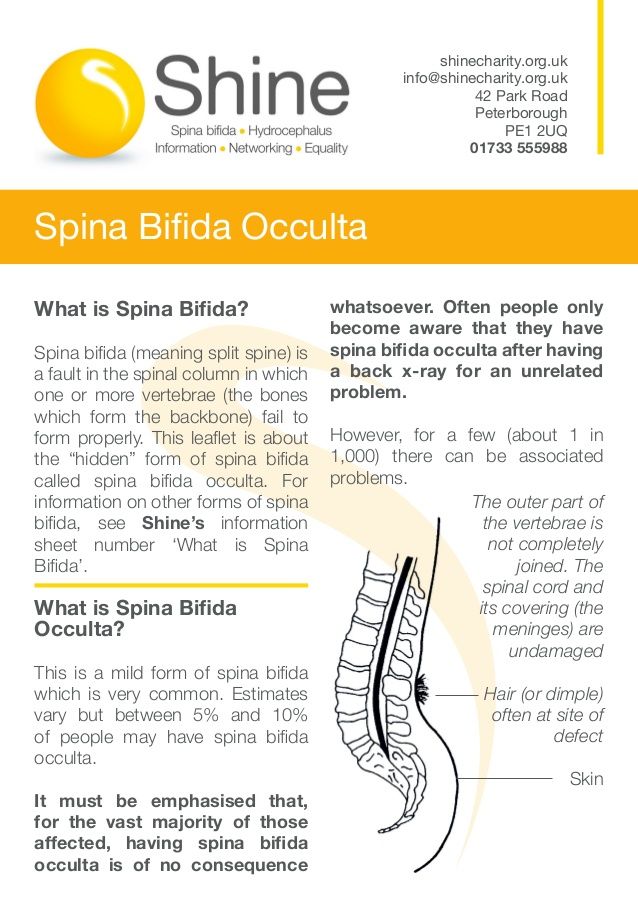
Oral thrush is a type of fungus infection, very common among babies. It appears as moist, milky-white patches in and around a child's mouth. Usually oral thrush is not serious and can sometimes even go unnoticed.
What causes oral thrush?
Oral thrush is a yeast infection caused by a fungus called Candida albicans. While around 1 in every 2 people live healthily with the fungus, at times it grows too quickly, causing a visible infection. If your child is on antibiotic treatment or taking inhaled corticosteroids (such as those in many commonly-used asthma puffers), they are more likely to have oral thrush. An immunocompromised child (a child with a weak immune system — either as a result of illness or a medical treatment), is also more likely to be infected.
What are the symptoms?
Oral thrush appears as milky, white patches on the insides of a child's cheeks, tongue or lips and cannot be wiped away easily, as the infection is under the skin. The patches might also appear red or inflamed. Usually, the infection doesn't cause irritation, however if the mouth area is very red and raw, it might be hard for your child to eat. Another sign that your child may have an oral thrush infection is drooling.
Thrush can also appear in the nappy area (nappy rash).
Is oral thrush contagious?
While the fungus is contagious, it doesn't transfer easily. The most common points of transfer include:
- teething toys
- dummies
- teats
- bottles
The yeast might transfer from one person to another, for example, when a child chews on an infected child's toy. Another common infection point for a baby is their mother's vagina (vaginal oral thrush) during birth, as the yeast often lives in small amounts in the vagina.
Another common infection point for a baby is their mother's vagina (vaginal oral thrush) during birth, as the yeast often lives in small amounts in the vagina.
Treating oral thrush
Your doctor can prescribe your child antifungal drops or gel to help manage the infection. If you are a breastfeeding mother with an infected child, your doctor might also prescribe an antifungal gel for your nipples. This is because you might be spreading the infection to your child when feeding. You can continue to breastfeed as usual if your baby has oral thrush.
Preventing oral thrush
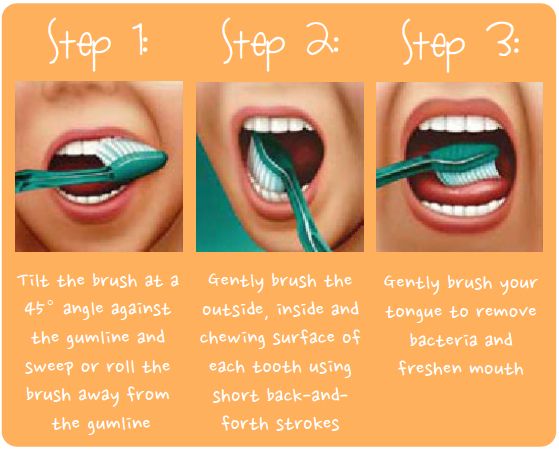
Maintaining a high level of oral (mouth) and personal hygiene is a good way to prevent the spread of the infection. If your child has teeth, this includes brushing twice a day and taking them to the dentist for check-ups and treatments. It is important to sterilise items that come into contact with your child's mouth, including teething toys, dummies, and bottles. Clean teats well in between feeds to ensure that your child doesn't become reinfected.
Does my child need to see a doctor?
If you think your child may have oral thrush, it's a good idea to take your child to see a doctor to get a diagnosis. Most cases are very mild, and will quickly clear up with prescription gel or drops.
Be sure to take your child to the doctor if:
- white patches appear in their mouth
- the rash keeps on coming back after treatment
- they have a fever or are feeling generally unwell
- you are concerned about your child’s health
Sources:
Raising Children Network (Oral thrush in babies and children), DermNet NZ (Oral candidiasis), Better Health Channel (Oral conditions - young children)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2020
Back To Top
Related pages
- Regular health checks for babies
Need more information?
Oral thrush in babies and children | Raising Children Network
Oral thrush is a fungal infection in and around babies’ mouths. It’s common and isn’t usually anything to worry about. Read about oral thrush treatment.
It’s common and isn’t usually anything to worry about. Read about oral thrush treatment.
Read more on raisingchildren.net.au website
Dental health - Diabetes Australia
The mouth is often overlooked as an area of the body with complications associated with diabetes.
Read more on Diabetes Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Oral Thrush (for Parents) - Nemours KidsHealth
Reviewed by: Michelle P. Tellado, MD
en español Muguet (candidiasis oral)
What Is Oral Thrush?
Oral thrush is a very common yeast infection in babies. It causes irritation in and around a baby's mouth.
What Are the Signs and Symptoms of Oral Thrush?
Oral thrush (also called oral candidiasis) can affect anyone, but is most common in babies younger than 6 months old and in older adults.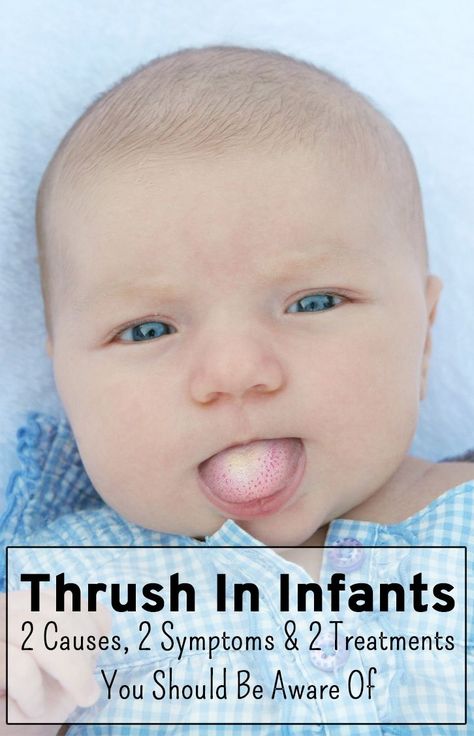
A baby with oral thrush might have cracked skin in the corners of the mouth or white patches on the lips, tongue, or inside the cheeks that look a little like cottage cheese but can't be wiped away.
Some babies may not feed well or are uncomfortable when sucking because their mouth feels sore, but many babies don't feel any pain or discomfort.
What Causes Oral Thrush?
Oral thrush is caused by the overgrowth of a yeast (a type of fungus) called Candida albicans.
Most people (including infants) naturally have Candida in their mouths and digestive tracts, which is considered normal growth. Usually, a healthy immune system and some "good" bacteria control the amount of this fungus in the body.
But if the immune system is weakened (from an illness or medicines like chemotherapy) or not fully developed (as in babies), Candida in the digestive tract can overgrow and lead to an infection. Candida overgrowth also causes diaper rash and vaginal yeast infections. Babies can have oral thrush and a diaper rash at the same time.
Babies can have oral thrush and a diaper rash at the same time.
Candida overgrowth also can happen after a baby has been given antibiotics for a bacterial infection because antibiotics can kill off the "good" bacteria that keep the Candida from growing. Oral thrush also can happen after the use of steroid medicines.
How Is Oral Thrush Treated?
See your doctor if you think your baby may have thrush. Some cases go away without medical treatment within a week or two, but the doctor may prescribe an antifungal solution for your baby's mouth. This medicine is usually applied several times a day by "painting" it on the inside of the mouth and tongue with a sponge applicator.
Depending on your baby's age, the doctor also might suggest adding yogurt with lactobacilli to your baby's diet. The lactobacilli are "good" bacteria that can help get rid of the yeast in your child's mouth.
If your baby keeps getting oral thrush, especially if he or she is older than 9 months old, talk with your doctor because this might be a sign of another health issue.
Can Oral Thrush Be Prevented?
Oral thrush is a common infection in babies, but you can help prevent it:
- If you formula-feed your baby or use a pacifier, thoroughly clean the nipples and pacifiers in hot water or a dishwasher after each use. That way, if there's yeast on the bottle nipple or pacifier, your baby won't be reinfected. Store milk and prepared bottles in the refrigerator to prevent yeast from growing.
- If you breastfeed and your nipples are red and sore, you might have a yeast infection on your nipples, which you and your baby can pass back and forth. Talk to your doctor, who might recommend using an antifungal ointment on your nipples while your baby is treated with the antifungal solution.
To prevent diaper rash, change diapers often.
Reviewed by: Michelle P. Tellado, MD
Date reviewed: September 2019
What are the diseases of the oral cavity and gums - dentistry DS
Stomatitis
This is a group of diseases characterized by inflammation of the oral mucosa with hyperemia, swelling, and an increase in the amount of mucus in the oral cavity. Depending on the severity and depth of the lesion, even sores or foci of necrosis can form in the oral cavity, which sharply disrupt the general condition - fever, weakness, anxiety, refusal to eat.
Depending on the severity and depth of the lesion, even sores or foci of necrosis can form in the oral cavity, which sharply disrupt the general condition - fever, weakness, anxiety, refusal to eat.
There are many causes of the disease: mechanical, chemical, thermal, bacterial factors. Often the cause of the disease in infancy is contaminated nipples, toys and other objects that enter the child's mouth. Often stomatitis develops in infectious diseases (measles, scarlet fever, influenza, whooping cough, etc.). The mucous membrane of the oral cavity acquires a bright red color, becomes swollen, teeth marks are visible on the mucous membrane of the cheeks and tongue. Saliva becomes viscous, viscous. The mucous membrane is covered with a whitish coating. The tongue is dry, swollen, often with a brown tinge, chewing is painful. The duration of the disease is from 1 to 3 weeks, the prognosis is favorable.
A general preventive rule for children and adults is good oral hygiene.
Gingivitis
Inflammatory process that causes swelling and tenderness of soft tissues. With untimely treatment, the problem worsens and becomes chronic.
The main causes of gingivitis:
- poor oral hygiene;
- thermal or chemical burns;
- use of certain drugs;
- unbalanced diet (insufficient amount of vitamins in food)
- smoking;
- certain infectious diseases;
- gastritis;
- ulcerative processes in the digestive system;
- caries.
Forms and varieties of gingivitis
Depending on the clinical situation and the nature of the development of the disease, acute and chronic gingivitis are distinguished.
Acute gingivitis manifests itself in the form of classic signs of the disease: redness, swelling and bleeding of the gums.
Chronic gingivitis develops more calmly, without pronounced signs, but gradually leads to the growth of gum tissues (hyperplasia), which entails partial and complete coverage of the surface of the tooth crown by the gum.
Preventive measures
By following simple rules, you can reduce the likelihood of serious oral diseases:
- Brushing teeth at least 2 times a day after meals;
- Use of dental floss and rinses;
- Rational nutrition;
- Refusal of bad habits;
- Visiting the dentist at least once every six months.
Periodontitis
Periodontitis is an inflammation of the periodontal tissues, which includes the teeth, ligaments, cementum and gums. Periodontitis as a disease is a consequence of gingivitis - a slight inflammation of the gums, the main cause of which is the neglect of oral hygiene. If with gingivitis inflammation spreads exclusively to soft mucous membranes, then with periodontitis, the ligaments that hold the teeth in the holes suffer. That is why at 9In 0% of cases, when diagnosing this disease, tooth mobility is observed, which eventually leads to their loss.
The most common causes of the disease are the following:
1. Improper or irregular oral care . Plaque, which is present on the surface of the teeth and in the interdental spaces, is not as safe a substance as it might seem at first glance. Soft and easily removed at the beginning, it goes through certain cycles of "development". The result is the mineralization of plaque and its transformation into hard tartar. This process in most cases is observed in those who neglect their daily oral care or use the wrong toothbrush, toothpaste and rinse.
Improper or irregular oral care . Plaque, which is present on the surface of the teeth and in the interdental spaces, is not as safe a substance as it might seem at first glance. Soft and easily removed at the beginning, it goes through certain cycles of "development". The result is the mineralization of plaque and its transformation into hard tartar. This process in most cases is observed in those who neglect their daily oral care or use the wrong toothbrush, toothpaste and rinse.
2. Poor blood supply to the gums . Periodontitis is one of the most common problems among smokers. Substances contained in tobacco smoke lead to narrowing of the vessels of the oral mucosa and their fragility, which impairs the blood supply to the tissues of the gums and the supporting apparatus of the teeth. The slowdown in blood circulation and, as a result, the development of periodontitis is also facilitated by the lack of chewing load caused by eating habits (for example, the predominance of soft foods in the diet).
3. Nutritional deficiency . The lack of fresh vegetables, fruits, greens in the diet, a sufficient amount of fish, meat and dairy products quickly leads to a lack of essential substances in the gum tissues. If malnutrition is in the nature of a permanent habit, then over time, metabolic processes in the gums are disturbed, which creates the basis for inflammation and periodontitis. Deficiency of vitamins A, C and group B can lead to negative consequences.
Treatment of periodontitis
Professional teeth cleaning is an essential step in the treatment of periodontitis. This procedure removes physical obstacles (plaque and calculus) that prevent the gums from restoring their original position and tightly covering the teeth.
Medical treatment - use of topical antiseptics. This need is due to the high risk of spreading inflammation and infection to other tissues.
Surgical treatment
In the advanced stage of periodontitis, when the inflammation has spread deep into the bone tissue, surgical intervention becomes necessary. Such manipulations include partial excision of the gums (gingivectomy), washing of periodontal pockets with medicinal solutions, removal of stones, patchwork operations. In some cases, surgical treatment of periodontitis involves the implantation of bone tissue substitutes or the application of collagen or artificial membranes to restore the supporting apparatus of the tooth.
Such manipulations include partial excision of the gums (gingivectomy), washing of periodontal pockets with medicinal solutions, removal of stones, patchwork operations. In some cases, surgical treatment of periodontitis involves the implantation of bone tissue substitutes or the application of collagen or artificial membranes to restore the supporting apparatus of the tooth.
Good oral hygiene
Without regular plaque removal and oral bacterial protection, periodontitis treatment cannot achieve sustainable results. Hygiene procedures twice a day with properly selected products, the use of dental floss and rinses will help make recovery faster.
Periodontal disease
Periodontal disease is a serious disease in which the last stage of gum inflammation occurs. Often this is the cause of the development of infectious diseases, gastritis, stomach ulcers or cirrhosis of the liver. Even more often, the patient's teeth simply fall out, and he cannot lead his usual way of life, eat his favorite food.
How to recognize periodontal disease
The signs of this dental disease are fuzzy and blurred. The patient is most often concerned about:
- exposure of the necks of the teeth;
- the presence of tartar;
- burning gums;
- discomfort when eating.
There are 3 stages of periodontal disease:
- Light. The patient has no complaints, very rarely there is a reaction to cold or hot food. The presence of periodontal disease can be established during the examination at the dentist. The mild stage of the disease is best treated.
- Medium. The roots of the teeth are exposed on average by 4-6 mm. The patient begins to worry about burning in the mouth, there is an acute reaction to the intake of hot, cold or sour foods.
- Heavy. The roots of the teeth are exposed by 8-10 mm. Chewing food causes severe pain.
Methods of treatment
Diagnosis
Before starting the treatment of periodontal disease, the dentist conducts an initial examination, which determines the degree of damage to the teeth and gums: which teeth are to be restored and which will have to be removed. This is necessary in order to draw up an algorithm for further actions. Then the patient is sent to the diagnostic room in order to make sighting and panoramic x-rays. According to them, the periodontist determines the depth of the pockets and the condition of the bone tissue.
This is necessary in order to draw up an algorithm for further actions. Then the patient is sent to the diagnostic room in order to make sighting and panoramic x-rays. According to them, the periodontist determines the depth of the pockets and the condition of the bone tissue.
Removal of plaque and calculus
Inflammation of the gums, which is always observed in periodontal disease, is mainly due to soft plaque, subgingival and supragingival calculus. The main reason for their appearance is poor oral hygiene. Therefore, the task of a specialist is not only to treat the disease, but also to educate the patient in proper hygiene.
General and local therapy
To improve immunity, the patient is prescribed a complex of vitamins and anti-inflammatory drugs. If the inflammation is insignificant, the dentist prescribes a course of local therapy, which can be carried out independently at home.
Splinting of teeth
Increased mobility of teeth indicates that the jawbone and soft tissues around them began to rapidly deteriorate. To avoid changing the position of the teeth and their falling out (for example, they can diverge fan-shaped), they are fastened with fiberglass tape and filling material. It is also necessary before surgical treatment.
To avoid changing the position of the teeth and their falling out (for example, they can diverge fan-shaped), they are fastened with fiberglass tape and filling material. It is also necessary before surgical treatment.
Surgery
If periodontal pockets reach 5-10 mm, it is impossible to prevent the progression of the disease without surgery. First, the pockets are cleaned of granulations and food plaque. This procedure is called curettage. It is of two types - open and closed.
Closed by special instruments, curettes. It is carried out only with periodontal disease at the initial stage (pockets reach 3 mm), when there is a slight inflammation of the gums.
Open curettage is required at an advanced stage of periodontal disease. With its help, all granulations and food deposits are completely removed. This operation is more difficult to perform. To completely clean the pockets, incisions are made on the gum. Mucosal flaps are exfoliated from the bone and the root surface is cleaned with curettes and an ultrasonic scaler. To restore the bone tissue, the periodontist implants a synthetic bone.
To restore the bone tissue, the periodontist implants a synthetic bone.
The patient then undergoes flap surgery to prevent receding gums. The doctor removes a 1.5 mm marginal strip of gums, because after prolonged inflammation, the gums are modified in such a way that they can no longer fit normally to the tooth. After that, the mucosal flaps are pulled to the neck of the tooth.
Timely diagnosis and choosing the right treatment will help stop periodontal disease and keep healthy teeth!
Stomatitis in a child - what is it? . Official site of KGAUZ "Norilsk GSP"
Stomatitis is an inflammation of the oral mucosa. The name comes from the Latin word “stoma” (mouth). Stomatitis occurs in both children and adults, but most often it appears in infants and preschoolers. This is because the mucosa at this age is thinner and more tender. It’s more common for everyone to say “stomatitis”, but it would be more correct to say “stomatitis”, since this is a generalizing concept for a whole group of diseases.
Causes of stomatitis in children
The causes of stomatitis in a child are different. These are dirty hands, and fragile children's immunity, and the features of thermoregulation, on which the respiratory system directly depends. You need to understand that the children's mucosa, unlike the adult one, is a very thin and vulnerable substance, so the attachment of any infection occurs very quickly. At an early age, salivation is not yet fully formed in a child, and saliva enzymes play a very important role in protecting the body. As a result, the mucous membrane often dries up, cracks appear, an infection occurs, and stomatitis follows it. It is impossible not to take into account the long-term use of medications, such as antibiotics, as well as neuropsychiatric disorders, unfavorable living conditions, poor child care and inadequate oral hygiene by the parents themselves.
It is often the parents who help the doctor to find out the cause of the disease. Only they can try to analyze what caused the appearance of a bubble, sore or plaque. For example, the child ate something wrong, bought a new toothpaste or toothbrush, or maybe the baby suffered a temperature drop.
For example, the child ate something wrong, bought a new toothpaste or toothbrush, or maybe the baby suffered a temperature drop.
Depending on the causes of occurrence, stomatitis can be divided into several types, each of which has a number of features.
Viral, herpes, or herpetic stomatitis in children is one of the most common types of childhood stomatitis. Usually a child becomes infected with it by airborne droplets. The virus is also transmitted through dishes, toys, household items. Most often, herpetic stomatitis in a child appears at the age of one to 4 years. The disease begins as a cold and is accompanied by a rash on the lips, lethargy, and fever. Sometimes there is a runny nose and cough. Around the second day, aphthae appear on the lips, tongue, and inside of the cheeks - small round or oval sores of light yellow color with a bright red border. They exude an unpleasant odor, are easily torn off and then bleed. These ulcers are the main symptom of this type of stomatitis. Therefore, such stomatitis in children is also called aphthous, or ulcerative. This is a particularly unpleasant type of disease, as it can be severe and accompanied by severe intoxication. Viral stomatitis in children also often occurs against the background of other viral diseases, such as influenza, chickenpox or measles.
Therefore, such stomatitis in children is also called aphthous, or ulcerative. This is a particularly unpleasant type of disease, as it can be severe and accompanied by severe intoxication. Viral stomatitis in children also often occurs against the background of other viral diseases, such as influenza, chickenpox or measles.
Infectious stomatitis occurs in children of both school and preschool age. Most often they occur with tonsillitis, sinusitis, pneumonia. The main symptom is a thick yellow crust on the lips. At the same time, the lips stick together, the mouth opens with difficulty. The temperature usually rises. Bacterial stomatitis in a child most often occurs due to weakened immunity in the autumn-winter period.
Traumatic stomatitis in a child is caused by mechanical trauma to the oral cavity. For example, burns from hot food, a too hard nipple, the habit of chewing on a pencil. Also, traumatic stomatitis often occurs in children with malocclusion due to frequent biting of the cheeks and tongue.
Candidal stomatitis occurs in children under one year old. The cause is Candida fungus. The milk left in the baby's mouth after breastfeeding is an excellent breeding ground for them. Therefore, parents call candidal stomatitis in children thrush. The main symptom is the appearance of white plaque in the baby's mouth. It is worth noting that this plaque should not be confused with the usual plaque after feeding. A cause for alarm is if the plaque does not go away, and the child refuses to eat.
Drug-induced or allergic stomatitis in children is caused by some type of allergy or drug reaction. In case of suspicion of this type of disease, the allergen should be identified and removed, otherwise there is a risk of getting unpleasant consequences, up to anaphylactic shock.
Symptoms of stomatitis in children
For all types of stomatitis, inflammation of the oral mucosa and the appearance of various formations in the form of sores, vesicles, characteristic plaque, vesicles (blistering rashes) and in cases of traumatic stomatitis - burns, bites, injuries. It is important to understand that stomatitis is not one acute or chronic disease with certain classic symptoms, each type has its own special cause, and they manifest themselves in the oral cavity in different ways, therefore, they need to be treated differently.
It is important to understand that stomatitis is not one acute or chronic disease with certain classic symptoms, each type has its own special cause, and they manifest themselves in the oral cavity in different ways, therefore, they need to be treated differently.
Treatment of stomatitis in children
There is no single algorithm for the treatment of stomatitis in children. Each case is individual in its own way. It often happens when a mother comes in the hope that the doctor will prescribe an ointment, and she will immediately cure her child with it. This does not happen! It is necessary to understand what preceded the inflammation, taking into account the age of the child, the stage and severity of the disease. Treatment is carried out both locally and symptomatically, i.e. symptoms are relieved. Doctors dentist-therapist and pediatrician give their recommendations, it is possible to involve highly specialized specialists, such as ENT, mycologist, dermatologist. Of course, there are some textbook principles that guide specialists in order to relieve or relieve pain or prevent complications. We are talking about compliance with the rules of oral hygiene, diet and sleep, treatment of the mucous membrane with special gels, solutions and applications. For example, with allergic stomatitis in children, antihistamines are recommended, with herpetic forms - antiviral, if there is a temperature - it is antipyretic. It is important that when you find a problem, contact a specialist without delay.
We are talking about compliance with the rules of oral hygiene, diet and sleep, treatment of the mucous membrane with special gels, solutions and applications. For example, with allergic stomatitis in children, antihistamines are recommended, with herpetic forms - antiviral, if there is a temperature - it is antipyretic. It is important that when you find a problem, contact a specialist without delay.
Caring for a child with stomatitis
Parental involvement in the treatment and proper care of the child are not only important - they are decisive. With stomatitis, it is necessary to strictly follow the treatment plan, which is often very laborious, so the result depends on parental care and control. The oral cavity is a kind of epicenter of pain, so it is not surprising that the child will be capricious a lot. Therefore, it is important for parents to stock up on patience and perseverance.
Most moms and dads are concerned about how to feed a child with stomatitis. Firstly, it is necessary to consume only soft, warm (not hotter than 30 degrees) and mushy food, for example, in the form of mashed potatoes. The main thing is that the food is high-calorie and positive, because the child's immunity is already weakened. After eating, it is imperative to rinse your mouth so as not to provoke the development of stomatitis and not to attach any additional infection. A diet for stomatitis in a child should be with the exclusion from the diet of spicy, sour, sweet foods and citrus fruits.
Firstly, it is necessary to consume only soft, warm (not hotter than 30 degrees) and mushy food, for example, in the form of mashed potatoes. The main thing is that the food is high-calorie and positive, because the child's immunity is already weakened. After eating, it is imperative to rinse your mouth so as not to provoke the development of stomatitis and not to attach any additional infection. A diet for stomatitis in a child should be with the exclusion from the diet of spicy, sour, sweet foods and citrus fruits.
Children with stomatitis need to be anesthetized. It is carried out with the help of various medications in order to avoid refusal of food and deterioration of sleep. In addition, with stomatitis in children, proper treatment of the oral cavity is very important. How to handle and rinse the child's mouth should be recommended by the doctor.
Prevention of stomatitis in children
If a person has had stomatitis at least once in his life, there will always be a risk of its recurrence, so prevention comes to the fore - in general, strengthening immunity in order to prevent the disease from returning.