When do you have a miscarriage
Miscarriage | NHS inform
A miscarriage is the loss of your baby before 24 weeks. Early miscarriages happen in the first 12 weeks of pregnancy. Late miscarriages happen between 12 and 24 weeks.
Most of the time there’s no clear reason why it happens, but it’s very unlikely to be caused by anything you did or didn’t do.
About 1 out of 5 pregnancies miscarry. Since many miscarriages aren't recorded the figure might be higher.
What causes a miscarriage?
Doctors think most miscarriages are caused when the building blocks controlling the development of a baby (the chromosomes) aren’t right. Babies with too many or not enough chromosomes won't develop properly. This leads to a miscarriage.
Miscarriages can also be caused by:
- issues with your placenta
- cervical weakness - when your cervix (neck of your womb) starts to open
Early miscarriages
An early miscarriage happens in the first 12 weeks of pregnancy. Most women who miscarry do so in the first 12 weeks of their pregnancy.
Many women have a miscarriage before they even know they’re pregnant. If this happens it can feel like a late period with heavy bleeding.
Symptoms of an early miscarriage
You might be having an early miscarriage if:
- you're bleeding from your vagina
- you've cramps in your lower abdomen – these can feel like bad period pains
- there's fluid or tissue coming from your vagina
- your breasts are no longer tender and any morning sickness has passed
Bleeding
Having some light bleeding's fairly common in the first 12 weeks of pregnancy and doesn't necessarily mean you're having a miscarriage.
If you start bleeding, you should always contact your GP or midwife and get advice about what to do.
What happens during an early miscarriage
If you’re in the early weeks of pregnancy:
- you’ll probably be asked to go to the early pregnancy unit at your local hospital straight away
- you’ll have some tests and usually an ultrasound scan
- your body usually completes the miscarriage naturally
Depending on your stage of pregnancy, you may deliver a small baby. That can be a shock and is an understandably upsetting time.
That can be a shock and is an understandably upsetting time.
Late miscarriages
A late miscarriage happens after 12 weeks and before 24 weeks.
For many parents who lose their baby after a late miscarriage, the word ‘miscarriage’ doesn't properly express the impact of their loss. The loss of a baby at any time's a terrible shock and a late miscarriage can be especially hard.
Symptoms of a late miscarriage
You might be having a late miscarriage if:
- you're bleeding from your vagina – this can be heavy and you might have blood clots
- you've strong, cramping pains
Always get medical help if:
- you're bleeding
- your baby’s movements have changed or you haven’t felt any movements for a while.
- your waters break and your baby's born very quickly
Contact your midwife or local maternity unit if you’re registered with them. If you’re not registered, contact your GP or phone the NHS 24 111 service.
What happens during a late miscarriage
If you’re later on in pregnancy:
- you may be asked to go to the maternity ward
- you’ll have some tests and usually an ultrasound scan
- you're likely to go through labour in hospital and might have your labour induced
While you deliver your baby you're likely to have heavier bleeding and labour-like pains.
Making difficult decisions
If you're having a miscarriage, your doctor or midwife will:
- talk to you about what will happen next
- help you, and your partner if you have one, decide what you’d like to do
You may have many difficult decisions to make at this time and will have overwhelming emotions. Take your time. Your midwife or doctor can help, and there are many organisations that can support you, your baby’s father and your family.
Get support from SANDS
Get support from SiMBA
After a miscarriage
Depending on your circumstances and stage of pregnancy, your midwife or doctor may ask if you'd like to see or hold your baby.
Some parents decide they don't want to see their baby, and others choose not to for faith or cultural reasons. This is a decision only you can make. It can be very hard when you're feeling overwhelmed. Whatever you decide is okay.
If you’re worried about what your baby looks like, your midwife or doctor can describe them to help you decide.
If your symptoms continue
You’ll probably have some bleeding for a week or two. If you continue to have symptoms after your miscarriage, it may mean that some of the pregnancy tissue's still in your womb.
Some women may need medicine or a short operation to treat this.
If you’re worried about seeking treatment, maybe a friend can come with you. Having support's really important at this difficult time.
Taking time off work
Many women will want to take time off work after having a miscarriage.
If you have a miscarriage before the end of the 24th week, you’re entitled to:
- take sick leave
- any sick pay you'd normally qualify for
If you lose your baby after the end of the 24th week, you’re entitled to:
- take maternity leave
- any maternity pay you qualify for
Speak to your employer about which choices may be right for you and your family.
Working Families has more about your rights at work after a miscarriage
Repeated miscarriages
Most women go on to have a successful pregnancy and a healthy baby after a miscarriage. But unfortunately, some women have repeated miscarriages.
If you've had:
- 1 or 2 miscarriages - you're not more likely than anyone else to have another one
- 3 or more miscarriages - your GP can refer you to a specialist to see whether there’s a specific cause
Causes, Symptoms, Risks, Treatment & Prevention
Overview
What is a miscarriage?
A miscarriage (also called a spontaneous abortion) is the unexpected ending of a pregnancy in the first 20 weeks of gestation. Just because it’s called a “miscarriage” doesn’t mean you did something wrong in carrying the pregnancy. Most miscarriages are beyond your control and occur because the fetus stops growing.
Types of miscarriage
Your pregnancy care provider may diagnose you with the following types of miscarriage:
- Missed miscarriage: You’ve lost the pregnancy but are unaware it’s happened.
 There are no symptoms of miscarriage, but an ultrasound confirms the fetus has no heartbeat.
There are no symptoms of miscarriage, but an ultrasound confirms the fetus has no heartbeat. - Complete miscarriage: You’ve lost the pregnancy and your uterus is empty. You’ve experienced bleeding and passed fetal tissue. Your provider can confirm a complete miscarriage with an ultrasound.
- Recurrent miscarriage: Three consecutive miscarriages. It affects about 1% of couples.
- Threatened miscarriage: Your cervix stays closed, but you’re bleeding and experiencing pelvic cramping. The pregnancy typically continues with no further issues. Your pregnancy care provider may monitor you more closely for the rest of your pregnancy.
- Inevitable miscarriage: You’re bleeding, cramping and your cervix has started to open (dilate). You may leak amniotic fluid. A complete miscarriage is likely.
How do I know if I’m having a miscarriage?
You may not be aware you’re having a miscarriage.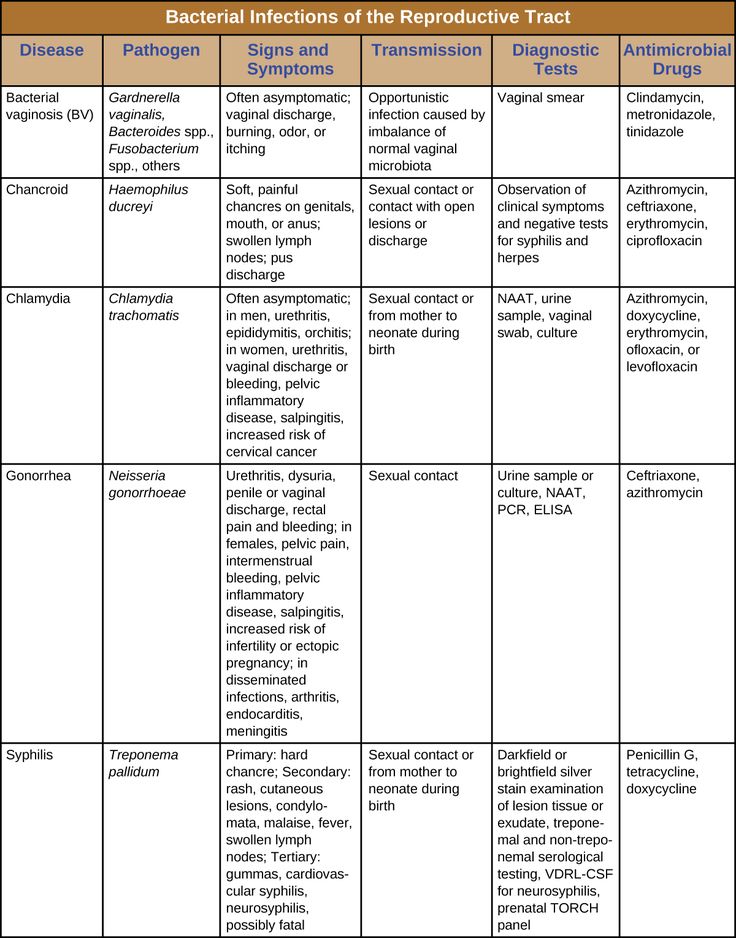 In people who have symptoms of a miscarriage, the most common signs are:
In people who have symptoms of a miscarriage, the most common signs are:
- Bleeding that progresses from light to heavy. You may also pass grayish tissue or blood clots.
- Cramps and abdominal pain (usually worse than menstrual cramps).
- Low back ache that may range from mild to severe.
- A decrease in pregnancy symptoms.
Contact your pregnancy care provider right away if you’re experiencing any of these symptoms. They will tell you to come into the office or go to the emergency room.
Symptoms and Causes
What causes miscarriage?
Chromosomal abnormalities cause about 50% of all miscarriages in the first trimester (up to 13 weeks) of pregnancy. Chromosomes are tiny structures inside the cells of your body that carry your genes. Genes determine all of a person’s physical attributes, such as assigned sex, hair and eye color and blood type.
During fertilization, when the egg and sperm join, two sets of chromosomes come together. If an egg or sperm has more or fewer chromosomes than normal, the fetus will have an abnormal number. As a fertilized egg grows into a fetus, its cells divide and multiply several times. Abnormalities during this process also leads to miscarriage.
If an egg or sperm has more or fewer chromosomes than normal, the fetus will have an abnormal number. As a fertilized egg grows into a fetus, its cells divide and multiply several times. Abnormalities during this process also leads to miscarriage.
Most chromosomal problems occur by chance. It’s not completely known why this happens.
Several factors may cause miscarriage:
- Infection.
- Exposure to TORCH diseases.
- Hormonal imbalances.
- Improper implantation of fertilized egg in your uterine lining.
- How old you are.
- Uterine abnormalities.
- Incompetent cervix (your cervix begins to open too early in pregnancy).
- Lifestyle factors such as smoking, drinking alcohol or using recreational drugs.
- Disorders of the immune system like lupus.
- Severe kidney disease.
- Congenital heart disease.
- Diabetes that isn't managed.
- Thyroid disease.
- Radiation.
- Certain medicines, such as the acne drug isotretinoin (Accutane®).

- Severe malnutrition.
There is no scientific proof that stress, exercise, sexual activity or prolonged use of birth control pills cause miscarriage. Whatever your situation is, it’s important to not blame yourself for having a miscarriage. Most miscarriages have nothing to do with something you did or didn’t do.
How painful is a miscarriage?
Miscarriages are different for every person. Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
What happens first during a miscarriage?
It’s hard to say what happens first during a miscarriage because everyone’s symptoms are different. Sometimes there are no signs of miscarriage, and you find out at a prenatal ultrasound that you’ve lost the pregnancy. Most people will experience some degree of cramping and bleeding, but what happens first varies.
Most people will experience some degree of cramping and bleeding, but what happens first varies.
How long does a miscarriage take?
It depends. Some people have painful cramping and heavy bleeding longer than others. Your pregnancy care provider can tell you what to expect and give you advice on how to manage pain and cramps during your miscarriage.
What are the risk factors for a miscarriage?
A risk factor is a trait or behavior that increases a person’s chance of developing a disease or condition. Risk factors for miscarriage include:
- Your age: Studies show that the risk of miscarriage is 12% to 15% for people in their 20s and rises to about 25% for people by age 40. Most age-related miscarriages happen because of a chromosomal abnormality (the fetus has missing or extra chromosomes).
- Previous miscarriage: You have a 25% chance of having another miscarriage (only slightly higher than someone who hasn’t had a miscarriage) if you’ve already had one.

- Health conditions: Certain health conditions like unmanaged diabetes, infections or issues with your uterus or cervix increase your chance of miscarriage.
Talk to your pregnancy care provider about the risk factors for miscarriage. They can discuss your risk after they’ve reviewed your medical history.
How many people have miscarriages?
Between 10% and 20% of all known pregnancies end in miscarriage. Most miscarriages (80%) happen within the first three months of pregnancy (up to 13 weeks of pregnancy). Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
What is my risk of miscarriage by week?
Your risk of pregnancy loss declines each week you’re pregnant. Around 15% of pregnancies end in miscarriage. Miscarriage risk in the second trimester (13 to 19 weeks) is between 1% and 5%. Many factors affect your risk of miscarriage such as your age and health. However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
Miscarriage risk in the second trimester (13 to 19 weeks) is between 1% and 5%. Many factors affect your risk of miscarriage such as your age and health. However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
Diagnosis and Tests
How is a miscarriage diagnosed?
Your pregnancy care provider will perform an ultrasound test to confirm a miscarriage. These tests check for fetal heartbeat or the presence of a yolk sac (one of the first fetal structures your provider can see on ultrasound).
You may also have a blood test to measure human chorionic gonadotropin (hCG), a hormone produced by the placenta. A low hCG level can confirm a miscarriage.
Finally, your provider may perform a pelvic exam to check if your cervix has opened.
Management and Treatment
What are the treatments for a miscarriage?
If you experience the loss of a pregnancy, the fetus must be removed from your uterus. If any parts of the pregnancy are left inside your body, you could experience infection, bleeding or other complications.
If any parts of the pregnancy are left inside your body, you could experience infection, bleeding or other complications.
If the miscarriage is complete and your uterus expels all the fetal tissue, then no further treatment is usually needed. Your pregnancy care provider will conduct an ultrasound to make sure there’s nothing left in your uterus.
If your body doesn’t remove all the tissue on its own or you haven’t started to bleed, your pregnancy care provider will recommend removing the tissue with medication or surgery.
Nonsurgical treatment
Your pregnancy care provider may recommend waiting to see if you pass the pregnancy on your own. This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
If a miscarriage wasn’t confirmed, but you had symptoms of a miscarriage, your provider may prescribe bed rest for several days. You might be admitted to the hospital overnight for observation. When the bleeding stops, you may be able to continue with your normal activities. If your cervix is dilated, they may diagnose you with an incompetent cervix, and they may perform a procedure to close your cervix (cervical cerclage).
Surgical treatment
Your provider may perform a dilation and curettage (D&C) or dilation and evacuation (D&E) if your uterus hasn’t passed the pregnancy or if you’re bleeding heavily. Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
What are some of the symptoms after a miscarriage?
Spotting and mild discomfort are common symptoms after a miscarriage.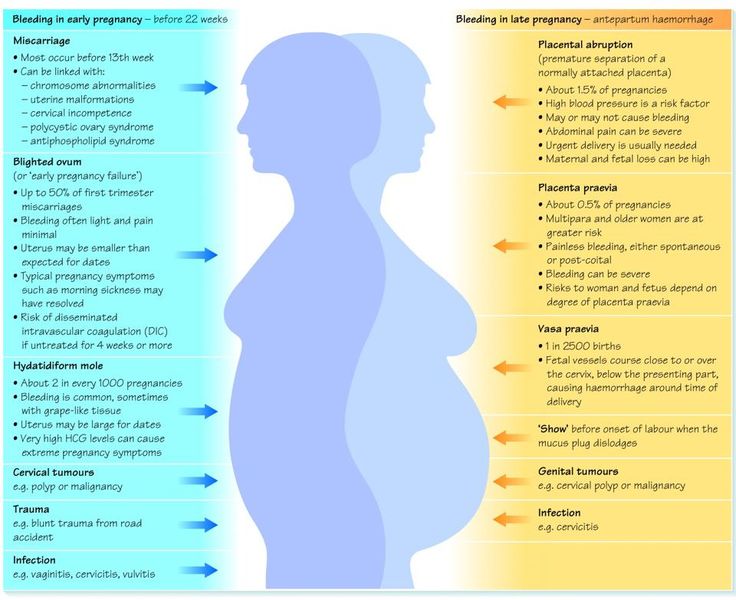
Contact your healthcare provider immediately if you have any of these symptoms as it could be signs of an infection:
- Heavy bleeding or worsening bleeding.
- Fever.
- Chills.
- Intense pain.
Don’t put anything inside your vagina for at least two weeks after a miscarriage. This includes tampons, sexual intercourse and fingers or sex toys. Your provider will schedule a follow-up appointment with you to discuss your recovery and any complications.
What tests should I have after repeat miscarriages?
Blood tests or genetic tests might be necessary if you’ve more than three miscarriages in a row (called repeated miscarriage). These include:
- Genetic tests: You and your partner can have blood tests, like karyotyping, to check for chromosome abnormalities. If tissue from the miscarriage is available, your provider may be able to test it for chromosome irregularities.
- Blood tests: You may have a blood test to check for autoimmune or hormone conditions that could be causing miscarriages.
Your provider may also look at your uterus using one of the following procedures:
- Hysterosalpingogram (an X-ray dye test of your uterus and fallopian tubes).
- Hysteroscopy (a test during which your provider views the inside of your uterus with a thin, telescope-like device).
- Laparoscopy (a procedure during which your provider views the pelvic organs with a lighted device).
Prevention
How can I prevent another miscarriage?
It’s usually not possible to prevent a miscarriage. If you have a miscarriage, it’s not because you did something to cause it. Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
- Attending all your prenatal care appointments.
- Maintaining a weight that's healthy for you.
- Avoiding risk factors for miscarriage like drinking alcohol and smoking cigarettes.
- Taking a prenatal vitamin.
- Getting regular exercise and eating a healthy diet.

Outlook / Prognosis
Can I get pregnant after I’ve had a miscarriage?
Yes. Most people (87%) who have miscarriages have subsequent normal pregnancies and births. Having a miscarriage doesn’t necessarily mean you have a fertility problem. Remember, most miscarriages occur because of a chromosomal abnormality, not because of something you did.
How soon can I get pregnant after a miscarriage?
The decision on when you should begin trying to get pregnant again is between you and your pregnancy care provider. Most people can get pregnant again after they’ve had one “normal” menstrual period.
Taking time to heal both physically and emotionally after a miscarriage is important. Counseling is available to help you cope with your loss. A pregnancy loss support group might also be a valuable resource to you and your partner. Ask your healthcare provider for more information about counseling and support groups. Above all, don’t blame yourself for the miscarriage. Take the time you need to grieve.
Take the time you need to grieve.
If you’ve had three miscarriages in a row, ask your provider about performing tests to figure out an underlying cause. You should use birth control until you receive the results. After your provider reviews the test results, they may suggest going off birth control and trying to conceive again.
Living With
How can I cope with my miscarriage?
Losing a pregnancy can be devastating and leave you with a range of emotions and lots of questions. Healing emotionally from a miscarriage is often harder and longer than the physical healing. Take the time you need to grieve your loss. Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
A note from Cleveland Clinic
A miscarriage is a very emotional moment for expectant parents and it’s natural to grieve the loss. Remember that a miscarriage can’t be prevented, and it’s not caused by something you did wrong. It doesn’t mean that you can’t have children or that you’ll have another miscarriage. If you’re planning to become pregnant, reach out to your healthcare provider to discuss the timing of your next pregnancy and ask any questions you have. It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
Remember that a miscarriage can’t be prevented, and it’s not caused by something you did wrong. It doesn’t mean that you can’t have children or that you’ll have another miscarriage. If you’re planning to become pregnant, reach out to your healthcare provider to discuss the timing of your next pregnancy and ask any questions you have. It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
Early miscarriage - symptoms and how to prevent it
The term "early miscarriage" refers to a spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body.
In addition, a curious pattern was revealed: more often than a natural one, a pregnancy induced artificially ends in a miscarriage. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
Why can an early miscarriage occur?
Here are the most common causes, each of which significantly increases the risk of miscarriage:
- the expectant mother has certain infectious diseases, as well as STDs;
- intoxication of a woman's body for various reasons, including as a result of her living in an ecologically unfavorable region;
- all kinds of metabolic disorders in the body;
- hormonal disruptions, including those caused by a malfunction of the thyroid gland;
- various neoplasms in the uterus and others, as well as the cervix, pathologies;
- maintenance by the future mother of a life far from a healthy lifestyle. May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition;
- obesity;
- immune status disorders;
- cardiac diseases;
- diabetes mellitus;
- too early for pregnancy or, conversely, the patient's overly mature age at times increases the risk of miscarriage;
- all kinds of pathologies of chromosomes and genes;
- prolonged exposure to stress or severe psycho-emotional trauma in a woman.

The timing of a miscarriage may depend, among other things, on the patient's genetic predisposition to miscarriage. Finally, often its specific cause remains unexplained to the end.
Symptoms of miscarriage
A pregnant woman should urgently seek medical help if she has the following warning signs:
- bleeding from the vagina;
- spotting discharge from the genital tract. They can have both light pink and intense red or brownish tint;
- convulsions;
- severe pain in the lumbar region;
- abdominal pain, etc.
All of the above signs can be symptoms of a miscarriage. Timely provision of qualified medical care is the key to maintaining pregnancy.
Life after miscarriage
If a woman could not bear the pregnancy - an early miscarriage crossed out all her plans - then she needs to calm down and take all measures to prevent such complications in the future. Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment.
Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment.
Gynecologists of the corresponding department of our private clinic in Ryazan will help you find out what could have caused the miscarriage, as well as make recommendations on how to prepare for pregnancy. They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped!
miscarriage, symptoms - Health Clinic 365 G.
 Yekaterinburg
Yekaterinburg Causes of miscarriage
Questions to the doctor about miscarriages
Diagnostics of miscarriage
Treatment and prevention of miscarriage
Pereki - this is spontaneous termination of pregnancy up to 20 weeks. According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Symptoms of miscarriage .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Call your doctor if:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can place a piece of tissue to be isolated in a clean container and take it to your doctor for examination.