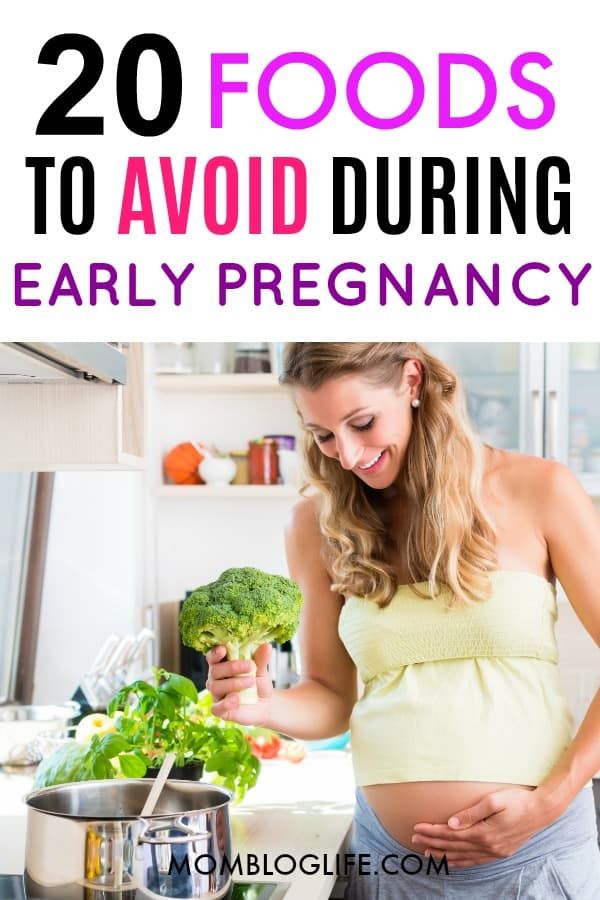
What foods to avoid in first trimester
11 Foods and Beverages to Avoid During Pregnancy
One of the first things people learn when they’re pregnant is what they can’t eat. It can be a real bummer if you’re a big sushi, coffee, or rare steak fan.
Thankfully, there’s more you can eat than what you can’t. You just have to learn how to navigate the waters (the low mercury waters, that is). You’ll want to pay close attention to what you eat and drink to stay healthy .
Certain foods should only be consumed rarely, while others should be avoided completely. Here are 11 foods and beverages to avoid or minimize while pregnant.
Mercury is a highly toxic element. It has no known safe level of exposure and is most commonly found in polluted water.
In higher amounts, it can be toxic to your nervous system, immune system, and kidneys. It may also cause serious developmental problems in children, with adverse effects even in lower amounts.
Since it’s found in polluted seas, large marine fish can accumulate high amounts of mercury. Therefore, it’s best to avoid high mercury fish while pregnant and breastfeeding.
High-mercury fish you want to avoid include:
- shark
- swordfish
- king mackerel
- tuna (especially bigeye tuna)
- marlin
- tilefish from the Gulf of Mexico
- orange roughy
However, it’s important to note that not all fish are high in mercury — just certain types.
Consuming low mercury fish during pregnancy is very healthy, and these fish can be eaten up to three times per week, according to the Food and Drug Administration (FDA).
Low mercury fish are plentiful and include:
- anchovies
- cod
- flounder
- haddock
- salmon
- tilapia
- trout (freshwater)
Fatty fish like salmon and anchovies are especially good options, as they are high in omega-3 fatty acids, which are important for your baby.
This one will be tough for you sushi fans, but it’s an important one. Raw fish, especially shellfish, can cause several infections. These can be viral, bacterial, or parasitic infections, such as norovirus, Vibrio, Salmonella, and Listeria.
These can be viral, bacterial, or parasitic infections, such as norovirus, Vibrio, Salmonella, and Listeria.
Some of these infections may only affect you, causing dehydration and weakness. Other infections may be passed on to your baby with serious, or even fatal, consequences.
Pregnant women are especially susceptible to listeria infections. In fact, according to the Centers for Disease Control and Prevention (CDC), pregnant women are up to 10 times more likely to get infected by Listeria than the general population. Pregnant Hispanic women are 24 times more at risk.
This bacteria can be found in soil and contaminated water or plants. Raw fish can become infected during processing, including smoking or drying.
Listeria bacteria can be passed to your baby through the placenta, even if you’re not showing any signs of illness. This can lead to premature delivery, miscarriage, stillbirth, and other serious health problems, according to the CDC.
It’s definitely advised to avoid raw fish and shellfish, including many sushi dishes. But don’t worry, you’ll enjoy it that much more after baby is born and it’s safer to eat again.
Some of the same issues with raw fish affect undercooked meat, too. Eating undercooked or raw meat increases your risk of infection from several bacteria or parasites, including Toxoplasma, E. coli, Listeria, and Salmonella.
Bacteria may threaten the health of your little one, possibly leading to stillbirth or severe neurological illnesses, including intellectual disability, blindness, and epilepsy.
While most bacteria are found on the surface of whole pieces of meat, other bacteria may linger inside the muscle fibers.
Some whole cuts of meat — such as tenderloins, sirloins, or ribeye from beef, lamb and veal — may be safe to consume when not cooked all the way through. However, this only applies when the piece of meat is whole or uncut, and completely cooked on the outside.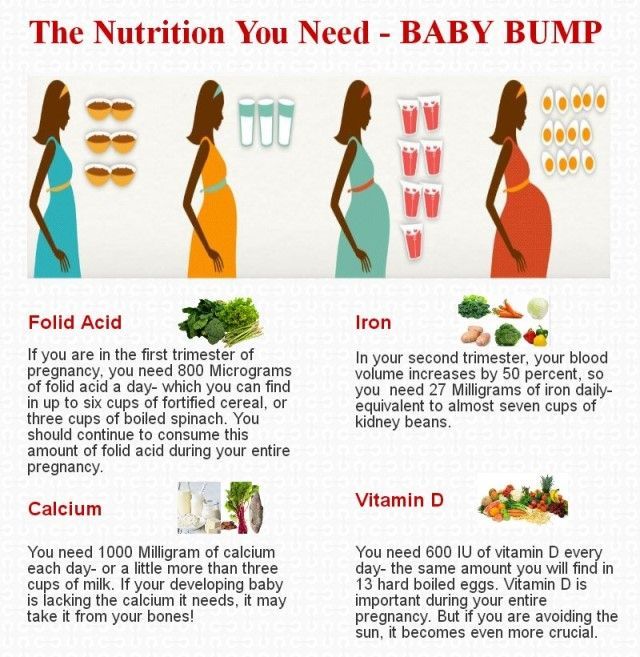
Cut meat, including meat patties, burgers, minced meat, pork, and poultry, should never be consumed raw or undercooked. So keep those burgers on the grill well done for now.
Hot dogs, lunch meat, and deli meat are also of concern, which is sometimes surprising to pregnant people. These types of meat may become infected with various bacteria during processing or storage.
Pregnant women should not consume processed meat products unless they’ve been reheated until steaming hot.
Raw eggs can be contaminated with the Salmonella bacteria.
Symptoms of salmonella infections include fever, nausea, vomiting, stomach cramps, and diarrhea.
However, in rare cases, the infection may cause cramps in the uterus, leading to premature birth or stillbirth.
Foods that commonly contain raw eggs include:
- lightly scrambled eggs
- poached eggs
- hollandaise sauce
- homemade mayonnaise
- some homemade salad dressings
- homemade ice cream
- homemade cake icings
Most commercial products that contain raw eggs are made with pasteurized eggs and are safe to consume.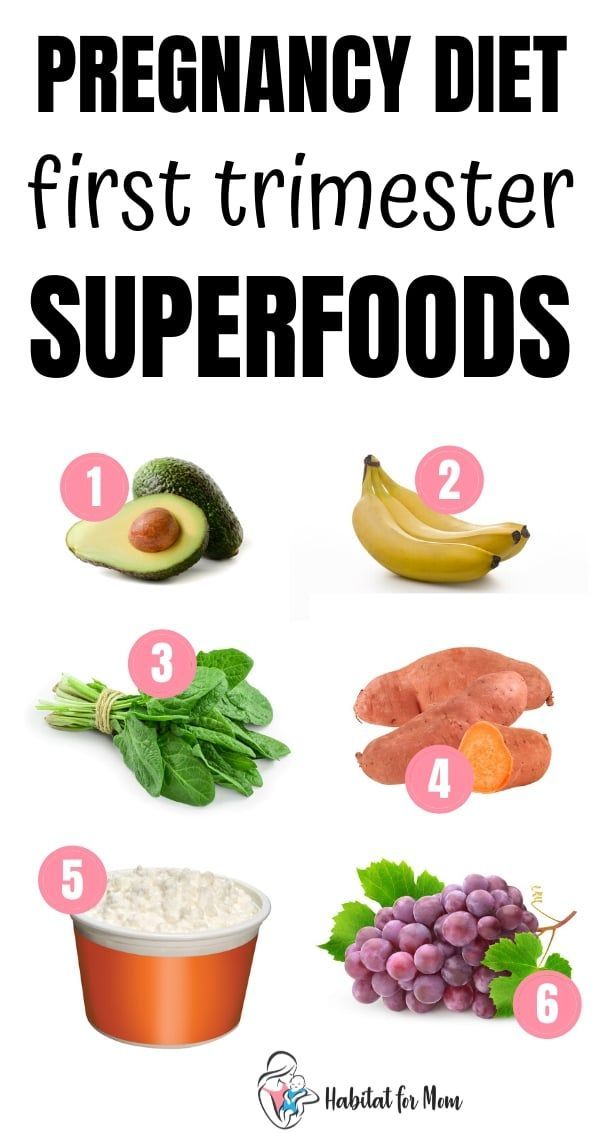 However, you should always read the label to make sure.
However, you should always read the label to make sure.
To be on the safe side, make sure to always cook eggs thoroughly or use pasteurized eggs. Save those super runny yolks and homemade mayo until after baby makes their debut.
Organ meat is a great source of a variety of nutrients.
These include iron, vitamin B12, vitamin A, zinc, selenium, and copper — all of which are good for you and baby. However, eating too much animal-based vitamin A (preformed vitamin A) is not recommended during pregnancy.
Consuming too much preformed vitamin A, especially in the first trimester of pregnancy, can lead to congenital malformations and miscarriage.
Although this is mostly associated with vitamin A supplements, it’s best to keep your consumption of organ meats like liver to just a few ounces once per week.
You may be one of the millions of folks who love their daily cups of coffee, tea, soft drinks, or cocoa. You’re definitely not alone when it comes to our love of caffeine.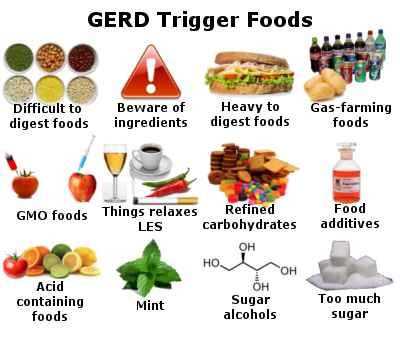
Pregnant people are generally advised to limit their caffeine intake to less than 200 milligrams (mg) per day, according to the American College of Obstetricians and Gynecologists (ACOG).
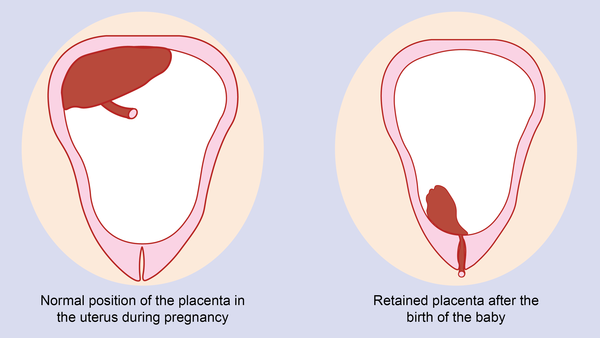
Caffeine is absorbed very quickly and passes easily into the placenta. Because babies and their placentas don’t have the main enzyme needed to metabolize caffeine, high levels can build up.
High caffeine intake during pregnancy has been shown to restrict fetal growth and increase the risk of low birth weight at delivery.
Low birth weight — defined as less than 5 lbs., 8 oz. (or 2.5 kg) — is associated with an increased risk of infant death and a higher risk of chronic diseases in adulthood.
So keep an eye on your daily cup of joe or soda to make sure baby doesn’t have exposure to too much caffeine.
Your healthy salad choice may not be free from rogue ingredients, either. Raw sprouts, including alfalfa, clover, radish, and mung bean sprouts, may be contaminated with Salmonella.
The humid environment required by seeds to start sprouting is ideal for these kinds of bacteria, and they’re almost impossible to wash off.
For this reason, you’re advised to avoid raw sprouts altogether. However, sprouts are safe to consume after they have been cooked, according to the FDA.
The surface of unwashed or unpeeled fruits and vegetables may be contaminated with several bacteria and parasites.
These include Toxoplasma, E. coli, Salmonella, and Listeria, which can be acquired from the soil or through handling.
Contamination can occur at any time during production, harvest, processing, storage, transportation, or retail. One dangerous parasite that may linger on fruits and vegetables is called Toxoplasma.
The majority of people who get toxoplasmosis have no symptoms, while others may feel like they have the flu for a month or more.
Most infants who are infected with the Toxoplasma bacteria while still in the womb have no symptoms at birth.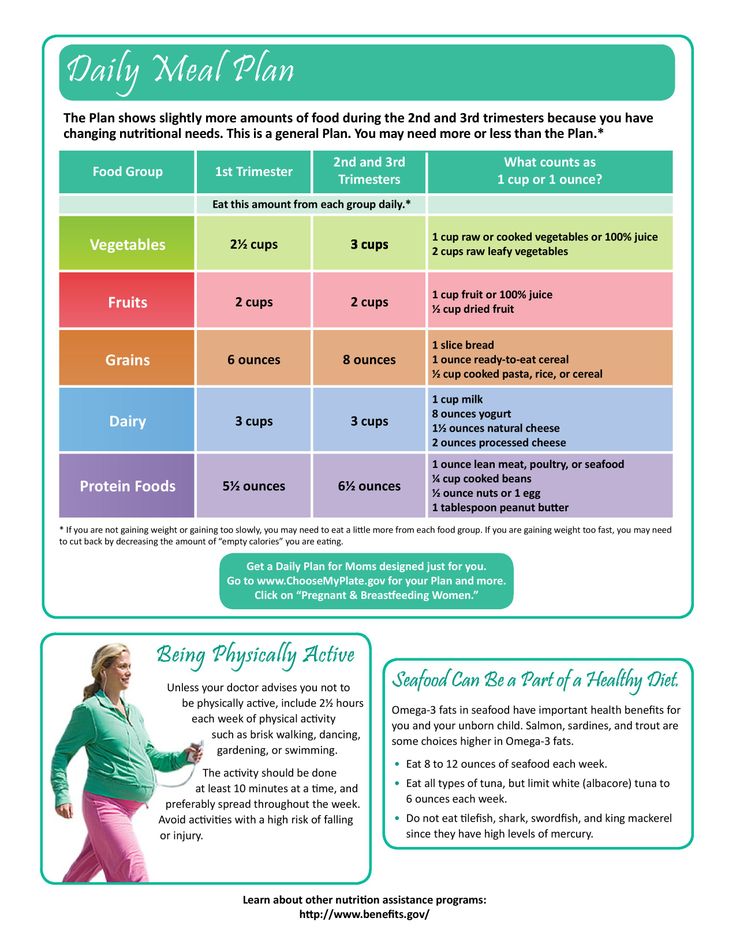 However, symptoms such as blindness or intellectual disabilities may develop later in life.
However, symptoms such as blindness or intellectual disabilities may develop later in life.
What’s more, a small percentage of infected newborns have serious eye or brain damage at birth.
While you’re pregnant, it’s very important to minimize the risk of infection by thoroughly washing with water, peeling, or cooking fruits and vegetables. Keep it up as a good habit after baby arrives, too.
Raw milk, unpasteurized cheese, and soft-ripened cheeses can contain an array of harmful bacteria, including Listeria, Salmonella, E. coli, and Campylobacter. (These are probably sounding familiar by now.)
The same goes for unpasteurized juice, which is also prone to bacterial contamination. These infections can all have life-threatening consequences for an unborn baby.
The bacteria can be naturally occurring or caused by contamination during collection or storage. Pasteurization is the most effective way to kill any harmful bacteria, without changing the nutritional value of the products.
To minimize the risk of infections, eat only pasteurized milk, cheese, and fruit juice.
It’s advised to completely avoid drinking alcohol when pregnant, as it increases the risk of miscarriage and stillbirth. Even a small amount can negatively impact your baby’s brain development.
Drinking alcohol during pregnancy can also cause fetal alcohol syndrome, which involves facial deformities, heart defects and intellectual disability.
Since no level of alcohol has been proven to be safe during pregnancy, it’s recommended to avoid it altogether.
There’s no better time than pregnancy to start eating nutrient-dense foods to help both you and your growing little one. You’ll need increased amounts of many essential nutrients, including protein, folate, choline, and iron.
It’s also a myth that you’re “eating for two.” You can eat as you normally do during the first semester, then increase by about 350 calories per day in your second trimester, and about 450 calories per day in your third trimester.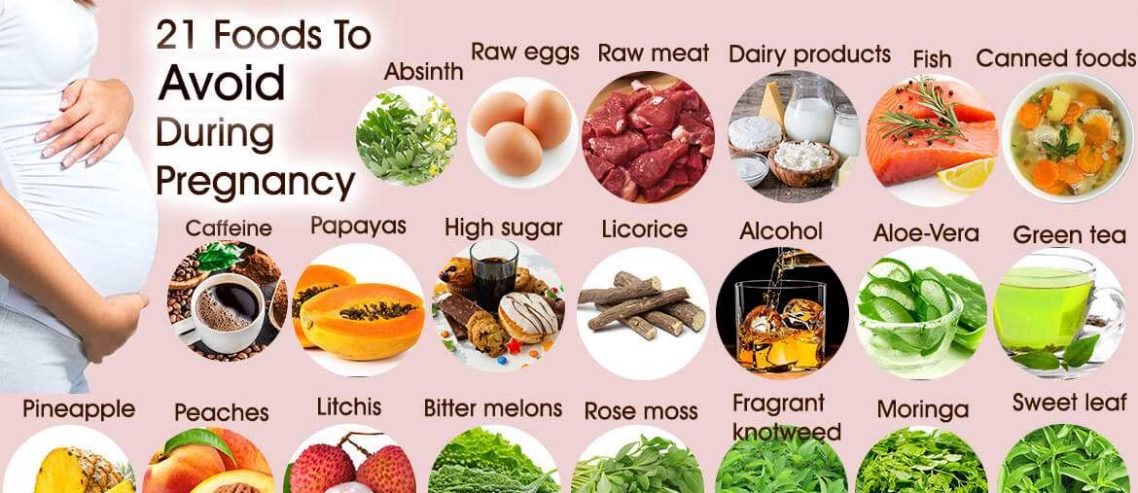
An optimal pregnancy eating plan should mainly consist of whole foods, with plenty of nutrients to fulfill yours and baby’s needs. Processed junk food is generally low in nutrients and high in calories, sugar, and added fats.
While some weight gain is necessary during pregnancy, excess weight gain has been linked to many complications and diseases. These include an increased risk of gestational diabetes, as well as pregnancy or birth complications.
Stick to meals and snacks that focus on protein, vegetables and fruits, healthy fats, and fiber-rich carbohydrates like whole grains, beans, and starchy vegetables. Don’t worry, there are lots of ways to sneak veggies into your meals without sacrificing taste.
When you’re pregnant, it’s essential to avoid foods and beverages that may put you and your baby at risk.
Although most foods and beverages are perfectly safe to enjoy, some, like raw fish, unpasteurized dairy, alcohol, and high mercury fish, should be avoided.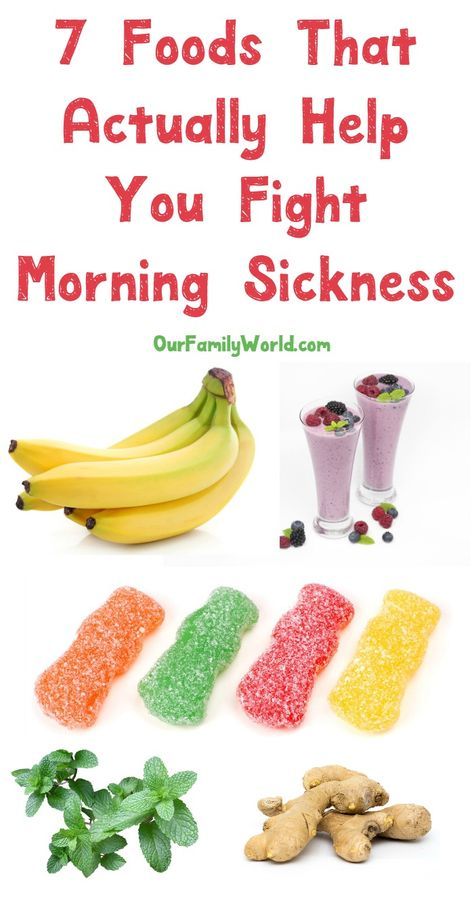
Plus, some foods and beverages like coffee and foods high in added sugar, should be limited in order to promote a healthy pregnancy.
If you want to learn more about what foods you should eat during pregnancy, check out this article: Healthy Eating During Pregnancy.
Quick tips for foods to avoid when pregnant
- Avoid high-mercury fish including shark, swordfish, tuna, and marlin.
- Raw fish and shellfish can be contaminated with bacteria and parasites. Some of these can cause adverse health effects and harm both you and baby.
- Raw or undercooked meat may contain harmful bacteria. As a general rule, meat should be cooked all the way through.
- Raw eggs may be contaminated with Salmonella, and may put you and your baby at risk. Be sure to thoroughly cook eggs before eating.
- Organ meat is a great source of iron, vitamin B12, vitamin A, and copper. To prevent consuming too much vitamin A limit your intake of organ meat to a few ounces once a week.
- Limit caffeine intake to under 200 mg per day, which is about 2 to 3 cups of coffee. High caffeine intake during pregnancy may limit baby’s growth and cause low birth weight.
- Raw sprouts may be contaminated with bacteria. Only eat them thoroughly cooked.
- Fruits and vegetables may be contaminated with harmful bacteria, including Toxoplasma. It’s important to thoroughly wash all fruits and vegetables with plenty of clean water.
- Don’t consume unpasteurized milk, cheese, or fruit juice, as these foods increase the risk of bacterial infections.
- Avoid all alcohol. Drinking alcohol can increase the risk of miscarriage, stillbirth, and fetal alcohol syndrome.
- Eating processed foods during pregnancy can increase your risk of excess weight gain, gestational diabetes, and complications. This can have long-term health implications for you and your child.
Healthy Diet During Pregnancy
If you’re concerned about what foods to eat to keep you and your baby healthy while you’re pregnant, that’s totally normal. Don’t worry — it’s easier than you think once you know which foods to prioritize.
Don’t worry — it’s easier than you think once you know which foods to prioritize.
Good nutrition during pregnancy can help ensure that your baby gets the best start possible. The meal plan is a balanced one that provides lots of:
- protein
- complex carbohydrates
- healthy types of fat
- vitamins and minerals
- fiber and fluids
A healthy pregnancy eating pattern contains much of the same balance of vitamins, minerals, and nutrients as healthy eating patterns in general.
The difference is that you need higher amounts to compensate for all the work your body is doing and baby’s additional needs.
If you already have healthy eating habits, it shouldn’t be too hard to make slight adjustments to ensure a healthy pregnancy. And if you’re starting from scratch on healthy eating? Not to worry — there are lots of healthy and yummy options.
If you’re pregnant, you only need to consume about 300 calories more per day.
The old adage that you need to “eat for two” doesn’t mean that you double your intake: The key is moderation and working with your healthcare team to find the right calorie and nutrition goals for you.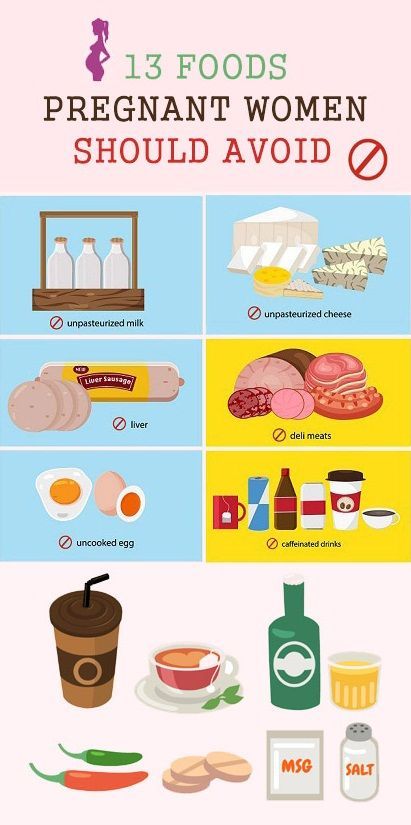
Complex carbs
Whenever possible, eat complex carbohydrates, such as:
- whole grain breads and pastas
- vegetables
- beans
- legumes
Limiting their tempting but lower fiber, nutritionally deficient cousins, the simple carbs:
- white bread
- cookies
- pretzels
- chips
- excess added sugar
Protein
Your protein needs increase considerably during pregnancy and peak during your third trimester.
To ensure you’re getting enough protein throughout your pregnancy, be sure to add a protein-rich food source to every meal and snack.
Examples of good, protein-rich foods include:
- eggs
- nuts and nut butters
- seeds
- fish
- chicken or turkey
- beans
- Greek yogurt and cheese
- tofu
- lean beef or pork
Try preparing some easy, protein-rich portable snacks for when you’re on the go. And talk to your doctor if you have questions regarding your specific protein needs.
Vegetables and fruits
Vegetables contain loads of nutrients you and your growing baby need such as:
- vitamins A and C
- beta-carotene
- fiber
- vitamin E
- riboflavin
- folic acid
- B vitamins
- calcium
- trace minerals
Here are some tips for getting more veggies into your meals without going full-on rabbit. Try making veggie-based sauces and adding vegetables to smoothies, soups, casseroles, lasagnas, and guacamole.
Grains and legumes
Whole grains and legumes, such as dried peas and beans, and other healthy carbs like fruit and starchy vegetables should make regular appearances on your plate.
They provide B vitamins and trace minerals, such as zinc selenium and magnesium. Grains and legumes are full of nutrients, including iron and the various B vitamins: thiamin (vitamin B-1), riboflavin (vitamin B-2), folate, and niacin.
Your little one needs these for the development of just about every part of their body. For instance, folate intake significantly reduces the risk of having a baby with spina bifida.
For instance, folate intake significantly reduces the risk of having a baby with spina bifida.
These foods supply energy for your baby’s development and help build the placenta and other tissues in your body. It’s all about teamwork when it comes to fueling both you and baby.
Fiber
Think of fiber as your body’s plumber, keeping constipation and hemorrhoids at bay. Try to eat 20 to 35 grams of fiber per day from whole grains, veggies, legumes, and fruit. Be sure to increase your intake of fluids along with fiber for best results.
Some fun options to toss into recipes include:
- oats
- nuts
- avocados
- chia seeds
- berries
Remember to check the nutrition panel and choose products made with whole grains that contain the most fiber per serving.
Fat
Remember those trendy low fat diets from the ’90s? Long gone are the days of avoiding fat. While you don’t want to consume excessive amounts of fats, it’s also dangerous to eliminate all fat from your meals. A healthy balance is recommended.
A healthy balance is recommended.
High fat foods to limit include fried foods and packaged products containing trans fats. Greasy meals tend to make any nausea or heartburn worse.
Essential fatty acids are important, including omega-3 fatty acids. Even saturated fats, once considered a fat to avoid, are now known to be important for fetal development.
Follow the same guidelines as the general public when it comes to choosing healthy fats. Include more plant-based fat sources like canola, olive, and soybean oil, and limit trans fats.
Some sources of healthy fats include:
- walnuts
- avocado
- pumpkin and sunflower seeds
- chia seeds
- flaxseed
- fatty fish
- olive oil
These foods provide the right types of fats to fuel your baby’s brain development.
Salt
Salt intake is important during pregnancy, and limiting it usually isn’t necessary, even if you already have high blood pressure. In fact, pregnant people often need more salt in their food to compensate for the growing baby, and restricting your intake could be harmful.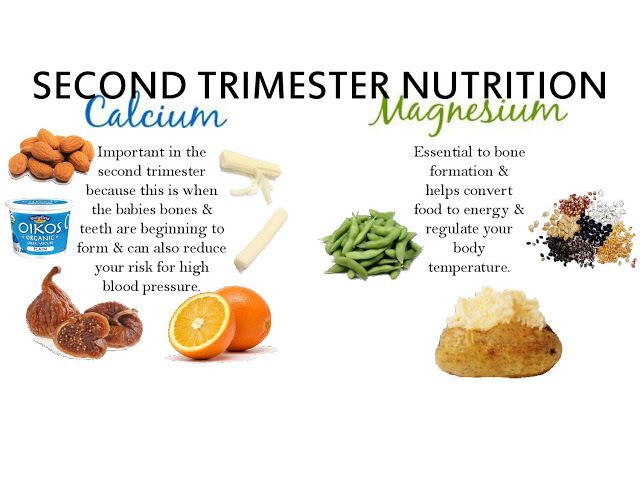
However, you don’t need to limit salt while pregnant, it’s important to limit unhealthy, processed salty foods such as fast food and processed meats.
Speak to your healthcare provider if you have questions about your salt intake during pregnancy.
Fluids
Fluids are an important part of any healthy eating plan. You should consume at least 80 ounces (2.4 liters) per day, and more is better to avoid dehydration. Pregnant people need the extra fluid to support the extra blood and amniotic fluid produced.
If you’re a coffee fan, you should limit caffeinated drinks while pregnant to not exceed 200 milligrams (mg) of caffeine per day, according to the American College of Obstetrics and Gynecology (ACOG).
Water also reduces your chance of constipation and the subsequent hemorrhoids that can develop from straining while you go.
The increased flow of urine also reduces your risk of developing a urinary tract infection, which can be dangerous for you and your baby.
If you choose to take supplements during your pregnancy, make sure you read the labels of every bottle and work with your healthcare providers. It’s important to stay within the daily allowance.
Keep in mind that a complete prenatal vitamin should have a balance of the nutrients that you need, and taking additional supplements may give you more than the recommended daily dosing in total.
Always discuss any supplements or over-the-counter medications you wish to take with your doctor for individual advice.
Choline
Choline is a vital nutrient during pregnancy and plays an important role in baby’s brain development. Choline helps to prevent developmental abnormalities of the brain and spine.
Some research suggests that the current choline recommended dietary allowance (RDA) for pregnancy (450 mg per day) is inadequate and that a choline intake closer to 930 mg per day is optimal while you’re pregnant.
Keep in mind that most prenatal vitamins don’t contain choline, so look for one that does or take a separate choline supplement. Check with your healthcare provider to make sure the amount is right for you.
Check with your healthcare provider to make sure the amount is right for you.
Here are some foods high in choline:
- beef liver provides 356 mg per 3-ounce serving.
- eggs — just two egg yolks provide nearly 300 mg of choline
- mushrooms
- soybeans
- kidney beans
Folic acid
Folic acid is the synthetic form of folate found in supplements. It’s an important vitamin that stimulates red blood cell formation and the production of important chemical signals in the nervous system. It’s also important in the process of making DNA.
Perhaps more importantly, folic acid, like folate, has been identified as a critical vitamin to prevent neural tube defects in your baby, such as spina bifida.
ACOG recommends taking 400 micrograms (mcg) a day before you conceive, and receiving at least 600 mcg a day from all sources, including meals, during pregnancy.
Good sources of folic acid include:
- cooked green leafy vegetables
- beef liver, cooked
- great northern beans
- fortified cereal
- avocado
- asparagus
- citrus fruits and juices
Pantothenic acid (B-5)
This vitamin (B-5) is involved in many of the body’s regulatory and metabolic activities. The RDA for the average person is 4 to 7 mg.
The RDA for the average person is 4 to 7 mg.
Pantothenic acid is present in:
- meats, including chicken and beef
- potatoes
- whole grains
- broccoli
- egg yolks
Riboflavin (B-2)
Riboflavin is important for baby’s development and growth. The RDA for pregnant people is 1.4 mg and 1.6 mg for those who are breastfeeding.
A prenatal vitamin may be your most consistent source, but B-2 can be found in milk and dairy products, with smaller amounts present in soybeans, grains, and pork.
Thiamine (B-1)
Thiamine is important for metabolism and development of the brain, nervous system, and heart. When you’re pregnant, you need increased amounts of many vitamins, including B-1.
The RDA for pregnant people is about 1.4 mg.
Vitamin A
Vitamin A is critical for proper cell growth and the development of the eyes, skin, and blood, as well as immunity and resistance to infection.
Vitamin B-6 (pyridoxine)
Vitamin B-6 is important for your body’s metabolism and for the development of the fetal brain and nervous systems.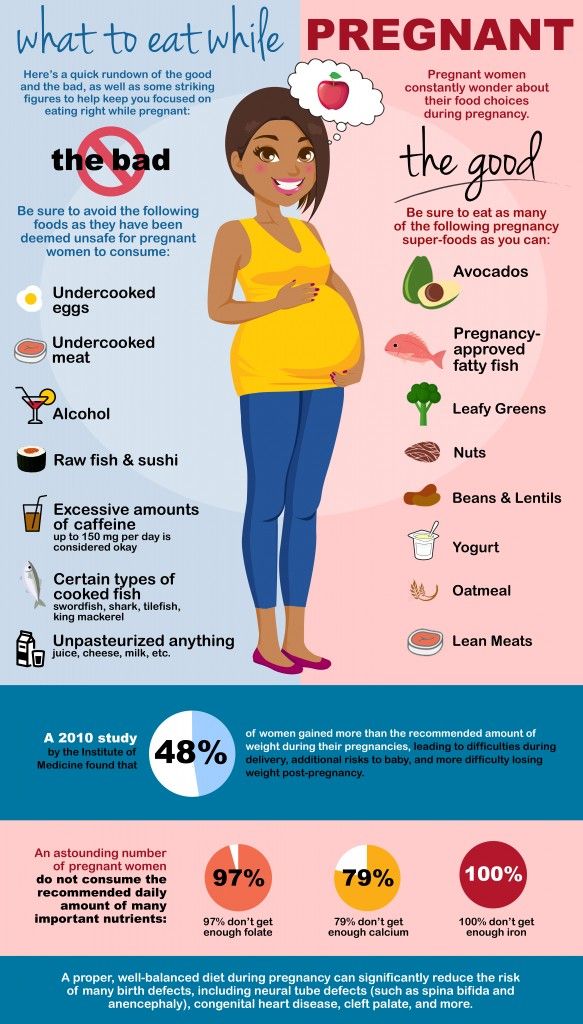 The RDA for pregnant people is 1.9 mg.
The RDA for pregnant people is 1.9 mg.
Vitamin B-12
Vitamin B-12 is found mainly in meats and dairy products. So it can be a problem for vegans or strict vegetarians. If you have dietary restrictions, make sure that your vitamin supplement has adequate B-12.
Nutritional yeast, fortified with B-12, is a great staple for vegetarians. It has a salty and savory flavor and tastes similar to Parmesan cheese. Here’s why “the nooch” is so popular for its health benefits.
Vitamin C (ascorbic acid)
The body does not stockpile vitamin C, so you need regular sources to fulfill your daily requirement. The RDA for pregnant people is 85 mg.
You can reach your goal through daily intake with these foods:
- citrus fruits (add fresh lemon or lime juice to your water!)
- berries
- bell peppers
- broccoli
- lots of other fruits and veggies
Vitamin D
Humans produce vitamin D in response to sunlight. Vitamin D itself is found naturally only in some fish liver oils.
Since exposure to sunlight is variable and this vitamin is so important for pregnant people and growing children, all milk is now fortified with vitamin D per quart as regulated by the U.S. government.
Vitamin D supplements are especially important if you don’t drink milk. Your doctor can check vitamin D levels to guide supplementation if you are taking a supplement.
And if you are deficient in vitamin D? You’re not alone: About 40 percent of people in the United States are too.
Calcium
Calcium, vitamin D’s life partner, is important for strong bones and teeth, of course. But it’s also critical for proper development and function of the heart and other muscles, as well as for the blood clotting system.
Your baby demands a huge supply of calcium during development. Pregnant people need 1,000 mg of calcium, preferably in two doses of 500 mg, per day.
Calcium-rich foods include:
- milk and dairy products
- calcium-fortified orange juice and bread
- canned fish with bones
- calcium-set tofu
- cooked beans
- cooked dark leafy greens
Prenatal supplements usually contain only 150 to 200 mg of calcium. So, prenatal vitamins alone won’t provide sufficient calcium for you.
So, prenatal vitamins alone won’t provide sufficient calcium for you.
Iodine
Iodine is critical for the development and functioning of the thyroid gland and regulation of metabolism. The RDA for pregnant people is 220 mcg per day.
You can get iodine from:
- fluoridated drinking water
- iodized (table) salt
- eggs
- milk
- brewer’s yeast
Iron
Make sure to eat iron-rich foods daily. Since many people, especially women, don’t get enough iron in their meals, iron is an important part of prenatal supplements.
Iron is often poorly absorbed from plant foods, which is why it’s difficult to reach the proper requirement. Talk to your doctor if you are prone to iron-deficiency anemia. They may recommend a supplement.
Iron-rich foods include:
- spinach
- lentils
- fortified cereals
- red meats such as beef and lamb
- kidney, lima, and navy beans
To improve the absorption of plant (or non-heme) iron, pair iron-rich food with a vitamin-C-rich source.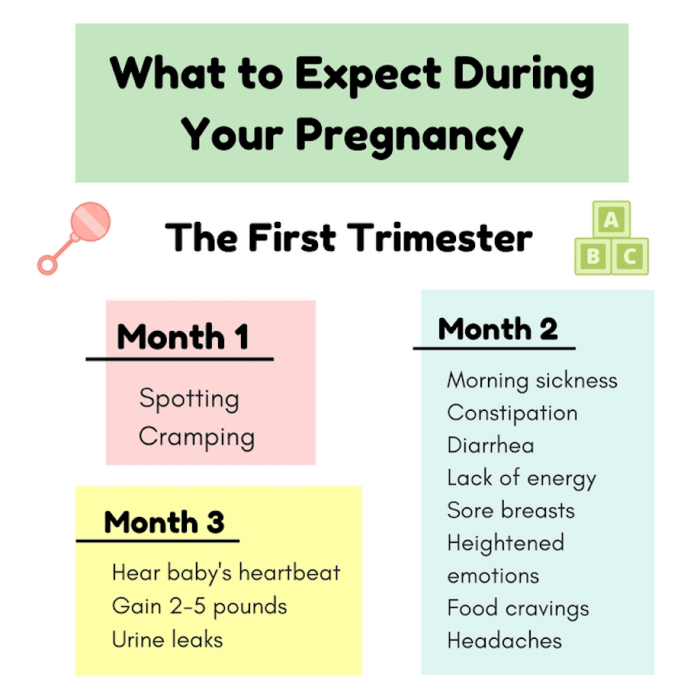 For example, add fresh sliced bell peppers or strawberries to your spinach salad.
For example, add fresh sliced bell peppers or strawberries to your spinach salad.
Magnesium
Magnesium is an important element for teeth and bones, regulation of blood-sugar levels, and the proper functioning of body proteins. It’s also important for tissue growth and repair, and may play a role in reducing preterm delivery.
The recommended upper limit for magnesium for pregnant people is around 300 mg. A good eating plan usually provides enough magnesium, so it’s not present in most prenatal vitamins.
The best food sources of magnesium are:
- seeds such as sunflower and pumpkin
- wheat germ
- tofu
- almonds
- yogurt
Chromium
Chromium is important for your baby’s development. You should get about 30 mcg per day. Foods that contain significant amounts of chromium include:
- whole wheat bread
- peanut butter
- asparagus
- spinach
- wheat germ
Copper
Copper stimulates the growth of cells and tissues, hair growth, and general metabolism. It’s a critical component of baby’s major systems: The heart and circulatory system, the skeleton, and the nervous system.
It’s a critical component of baby’s major systems: The heart and circulatory system, the skeleton, and the nervous system.
One mg of copper is recommended daily.
Zinc
It’s recommended pregnant people take in 11 mg of zinc, while breastfeeding women need a bit more: 12 mg. You can buy prenatal vitamins that contain zinc.
Zinc sources include:
- red meat
- seeds
- nuts
- beans
Potassium
Potassium is a mineral that affects cellular function, fluid balance, and blood pressure regulation, as well as proper nerve and muscle function.
Research from 2017 revised potassium intake recommendations to 4,000 mg daily for adults and pregnant people (slightly higher for people who are breastfeeding).
Prenatal vitamins can provide potassium, but potassium is present at high levels in foods such as:
- bananas
- avocados
- cantaloupes
- oranges
- watermelons
- dark leafy greens
- meats
- milk
- grains
- legumes
- squashes
Phosphorus
Phosphorus is an important part of the development of the muscular, circulatory, and skeletal systems. The RDA is 700 mg for pregnant and breastfeeding people.
The RDA is 700 mg for pregnant and breastfeeding people.
Sources include:
- milk
- yogurt
- beans
- seafood
- nuts
Taking prenatal multivitamins will ensure that you get the basic requirements. But vitamin-packed, fresh foods will help your baby get the best start in life and keep you going strong.
You should always talk to your healthcare provider or dietitian if you are concerned about your eating plan. They can help you determine if you are getting enough nutrients.
Nutrition of a pregnant woman
So, your plans and decisions to give birth to a child have come true - you are pregnant! But this news causes you a double feeling: - on the one hand, a feeling of joy, and on the other hand, a feeling of certain fear and even fear of unknown trials for your life and the fate of the unborn baby. What will he be like? - healthy, beautiful, happy?...
And this largely depends on the woman herself, on what lifestyle she will lead during pregnancy and, most importantly, how she will eat. nine0003
nine0003
Nutrition of a woman in different periods of pregnancy
The main thing in the menu of a future mother is variety. She should consume foods from all food groups: meat, fish, vegetables and fruits, dairy products, bread and cereals.
A woman's nutrition during pregnancy can be roughly divided into three periods (trimesters).
If before pregnancy a woman ate normally, felt comfortable, did not experience allergies to any products, then it is not worth changing her diet at an early stage of the first trimester of pregnancy. nine0003
During this period, all organs and systems in the child's body are formed, tissues are formed. The body needs complete proteins and vitamins: lean meat (rabbit, chicken, turkey), fish and seafood, dairy products. Be sure to eat rice, fresh or frozen vegetables, seasonal fruits. In the first trimester, many expectant mothers are still working. No matter how difficult it is to control your diet in the workplace, you need to do it - find time for a full breakfast and lunch. nine0003
nine0003
In the first trimester of pregnancy, there is an active restructuring of the body and adaptation to a new state. During this period, it is recommended to switch to a low-calorie diet, which includes more fruits, juices, decoctions of dried fruits, including rose hips. At the very beginning of pregnancy, especially if toxicosis torments, more frequent, but less plentiful meals are recommended.
Always keep a hematogen, a bag of nuts or dried fruit in your pocket to have a snack on the street. If your condition does not allow you to eat regular food, you should pay attention to baby food. Baby products literally save expectant mothers suffering from severe toxicosis. These are boxed cereals, children's curds, cookies and fruit purees. nine0003
In the first trimester, special attention must be paid to the quality of products. Gradually abandon sauces, semi-finished products and canned food containing harmful chemical additives. Do not forget that the placenta freely accumulates and passes chemistry.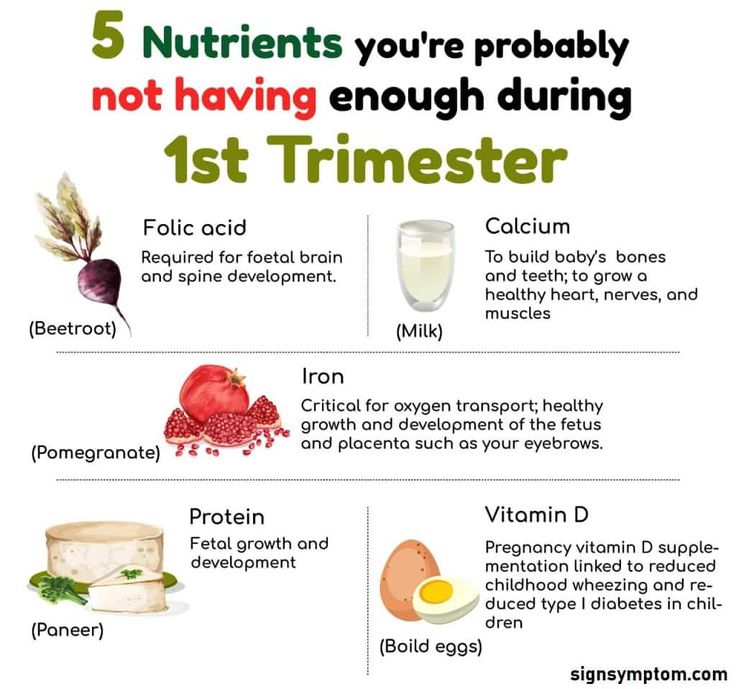 The importance of products containing folic acid is great, without it intensive metabolism is impossible, its deficiency can cause developmental abnormalities. Folic acid is found in greens, nuts, white cabbage and broccoli, beets, legumes, and eggs. nine0003
The importance of products containing folic acid is great, without it intensive metabolism is impossible, its deficiency can cause developmental abnormalities. Folic acid is found in greens, nuts, white cabbage and broccoli, beets, legumes, and eggs. nine0003
According to nutritionists, the diet of pregnant women should be 300 kcal / day higher than that of non-pregnant women, but in the first trimester there is no need to increase the energy value of the diet at all; in the second trimester, an additional 340 kcal / day is required; in the third trimester - 452 kcal / day. Pregnant women generally get enough calories, and more than 80% of women achieve and even exceed the required weight gain. These extra calories benefit the fetus. An underweight woman should gain 16–20 kg during her entire pregnancy, an overweight woman about 7 kg, and a normal body weight of 11–12 kg. nine0003
In the second trimester there are active jumps in the height and weight of the baby and uterus, so the caloric content of the diet needs to be increased. It is desirable to eat more and better. At this time, the need for trace elements increases: iron, magnesium, zinc, selenium, calcium, potassium. The child creates his own "reserve" of trace elements using the mother's resource, which means that the mother should have enough of them for two.
It is desirable to eat more and better. At this time, the need for trace elements increases: iron, magnesium, zinc, selenium, calcium, potassium. The child creates his own "reserve" of trace elements using the mother's resource, which means that the mother should have enough of them for two.
Very often in pregnant women in the second trimester hemoglobin drops, this is a normal physiological phenomenon, if it is not threatening to health. You can increase hemoglobin by eating red meat, chicken, fish, dried fruits, pomegranates, green vegetables and fresh herbs, buckwheat, citrus fruits (oranges, grapefruits, pomelo, lemons), rosehip and berry infusions. nine0003
In the second trimester, a pregnant woman should limit the intake of smoked and fried foods, as well as salt in her diet. In no case should you limit the liquid. Pure water is the best drink for a pregnant woman, and water should be consumed up to 2-2.5 liters per day. Water is a natural drink for the body, it does not cause complications and has no contraindications. Edema is caused not by water, but by salt, which we not only add in its pure form, but also consume with canned food, mayonnaise, cheese, and sausage. The absence of salt is not harmful, it is naturally found in many products: vegetables, bread, so the diet will not remain completely without it. Excess salt disrupts metabolism. nine0003
Edema is caused not by water, but by salt, which we not only add in its pure form, but also consume with canned food, mayonnaise, cheese, and sausage. The absence of salt is not harmful, it is naturally found in many products: vegetables, bread, so the diet will not remain completely without it. Excess salt disrupts metabolism. nine0003
During this period, you can increase the calorie content of food. Childbirth must be approached physically strong. It is better to eat meat and fish in the morning, for breakfast and lunch, and for dinner, prepare dairy and vegetable dishes: cheesecakes, stewed vegetables, cottage cheese and vegetable casseroles. It is necessary to minimize the intake of canned food, smoked meats, pickles and marinades, hot spices and fatty foods. Frequent walks in the air, physical activity are recommended.
In the third trimester, it is necessary to reduce the calorie content of foods at the expense of confectionery and flour products, eat less fatty meat, as well as cheese and sour cream.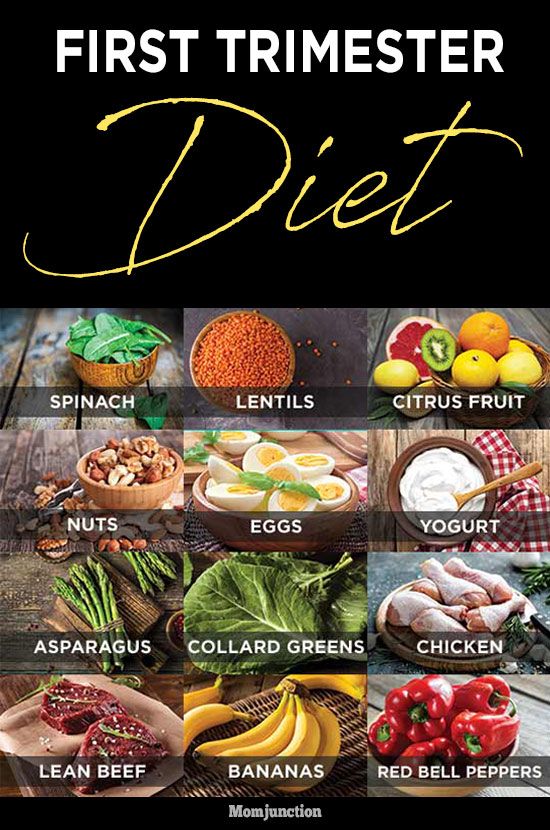 nine0003
nine0003
By the end of this period, many experts advise pregnant women to give up meat altogether in order to increase tissue elasticity and prevent ruptures.
During the entire period of pregnancy, special attention should be paid to the combination of products. If you combine foods wisely, you can ensure more efficient absorption of food. If the food is digested poorly, then this can lead to rotting and fermentation of products and the formation of substances harmful to the body of the mother and child. In addition, the fermentation process is accompanied by gas formation, which can lead to flatulence (bloating) and discomfort. This is especially harmful in the last stages of pregnancy. nine0003
Try not to take the first, second and third course at the same time; this overflows the stomach and presses on the fetus, the food is poorly digested and poorly absorbed. Eat little and often. It is not recommended to eat immediately before starting work, a long walk, before charging and immediately after it; it is advisable to rest for 10 minutes before eating.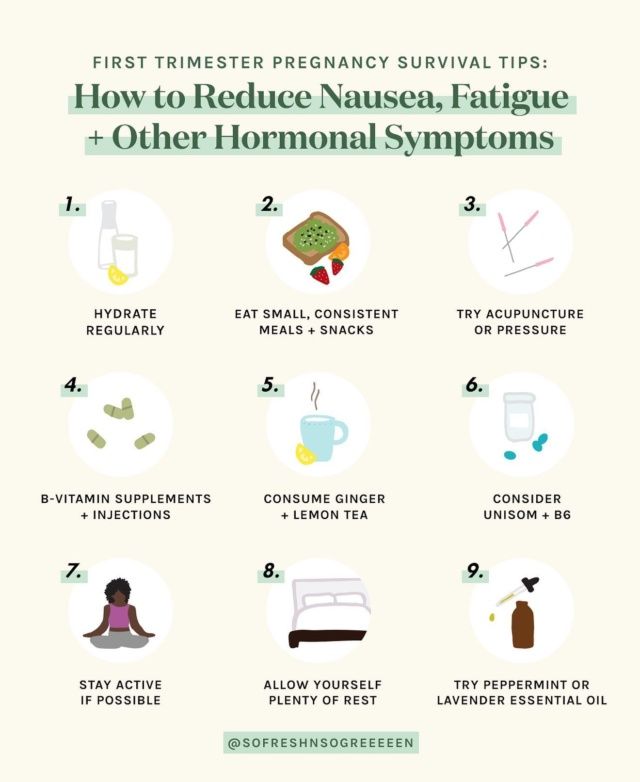
Eat only when you are hungry, try not to snack on the go. Follow the diet, eat at about the same time. nine0003
Proper preparation of food will help to maximize the useful substances contained in the products. Do not overcook food, try not to reheat the same dish several times, it is better to set aside only the portion that will be used. Cook in the most gentle way: baking, steaming, stewing. Avoid frying, boiling in large amounts of water, with this method of processing products, many useful substances are lost. If possible, do not cook for several days at once. Do not use aluminum cookware when cooking. Remember that for a pregnant woman, it is not calories that are important, but the quality of food, its naturalness, primarily a “living cell” (whole cereals, raw vegetables and fruits, fresh meat and dairy products). nine0003
What can harm the pregnant woman and the fetus
Smoking and alcohol – quit smoking from the first days of pregnancy, if you have smoked before, avoid "passive" smoking, and do not consume alcoholic beverages in any doses.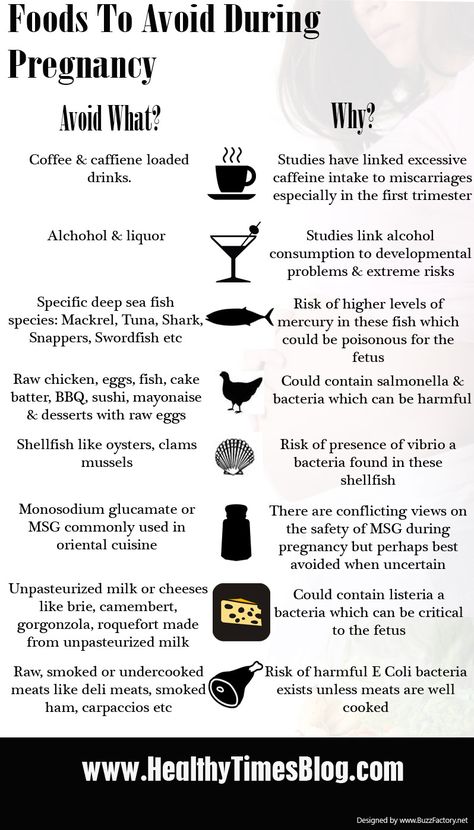
Lack of vitamins and microelements in the body - their absence or deficiency can lead to irreparable consequences. So, for example, iodine deficiency can lead to mental retardation of a child, folic acid deficiency - to severe fetal deformities, calcium deficiency - to a violation of the formation of the child's skeleton, iron deficiency - to anemia and a delay in the physical and neuropsychic development of the child. It is necessary to consult a doctor, perhaps he will recommend switching to iodized salt, as well as supplementing your diet with a vitamin-mineral complex and folic acid. nine0003
Excess weight is the risk of having a large child, which means the risk of complications during childbirth and the child's tendency to become obese at an older age.
The use of food additives (sauces, seasonings such as vegeta, bouillon cubes), exotic fruits, semi-finished products, carbonated drinks - the risk of allergies and anomalies in a child, unfortunately, increases.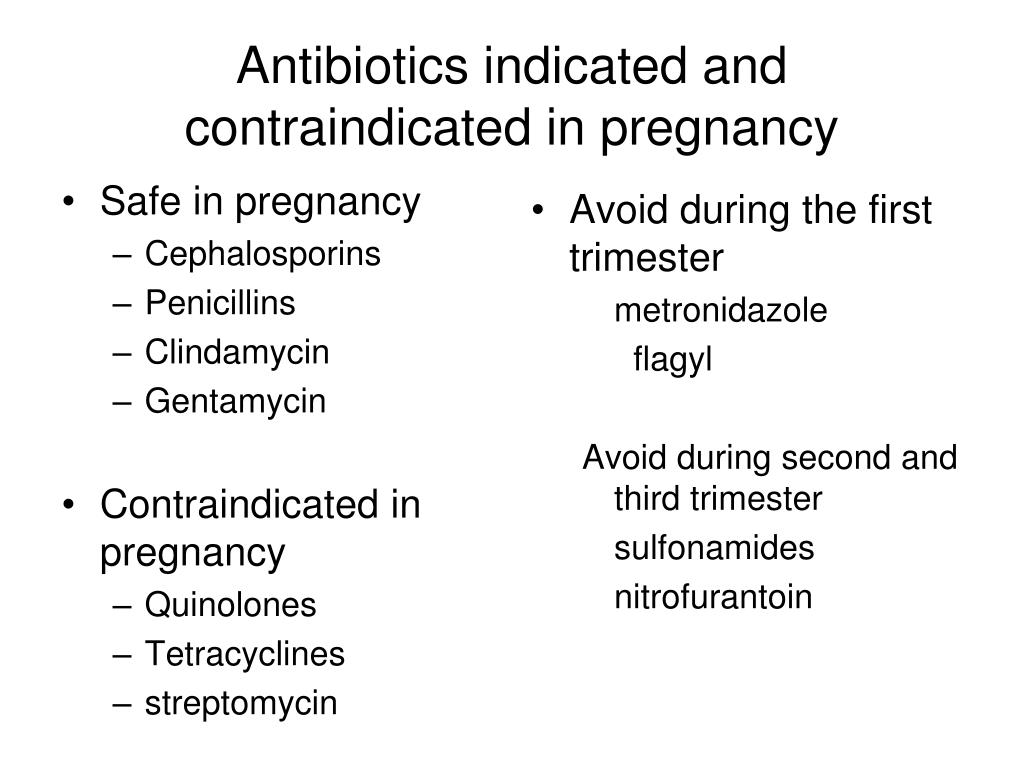
Recommended for pregnant women:
- Do not eat hot dogs and other snacks containing meat that has not been heated on fire or boiled in boiling water. nine0058
- Avoid soft cheeses. Hard cheeses are safe.
- Do not eat raw frozen pies and meat pastes, seafood. Canned analogues are safe.
- Do not consume raw vegetables, unpasteurized juices, liver, meat, poultry and eggs that have not been sufficiently cooked. These products may contain Salmonella taxins.
- Limit sweets.
- In no case do not resort to starvation and various diets. nine0058
- Regularly monitor blood pressure and do not miss visits to the gynecologist.
Remember!
Your child's development and health depend on your diet and lifestyle during pregnancy!
Nutrition in the 1st trimester of pregnancy
In the first trimester of pregnancy, the fetus is actively developing, so it needs a lot of vitamins and nutrients.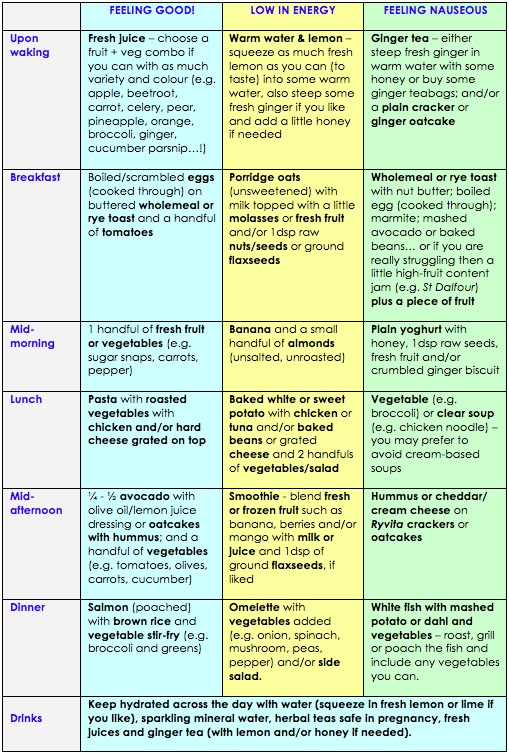 This must be taken into account when compiling a menu for a woman during this period. We will talk about what else to take into account and what should be the menu in the first trimester in this article. nine0003
This must be taken into account when compiling a menu for a woman during this period. We will talk about what else to take into account and what should be the menu in the first trimester in this article. nine0003
Meals for pregnant women: things to remember
You can often hear something like “you need to eat for two” addressed to a pregnant woman. However, this statement is not entirely true, because for development and formation, the child needs not so much calories as vitamins and microelements. It is because of their lack at the very beginning of pregnancy that pathologies can occur in the development of the fetus. As for calories, they should be distributed approximately as follows: 100-120 g of protein, up to 350 g of carbohydrates and only 75 g of fat. The total daily calorie intake should be within 2700 Kcal. nine0003
The second point is toxicosis, which accompanies the first stage of pregnancy in many women. Fortunately, by choosing the right foods and preparing them, you can keep discomfort to a minimum. To avoid unnecessary stress on the gastrointestinal tract and alleviate the symptoms of toxicosis, it is better to limit the use of fried, spicy and salt, not to mention coffee and alcohol. It is permissible for a pregnant woman to consume no more than 5-6 g of salt per day per day.
To avoid unnecessary stress on the gastrointestinal tract and alleviate the symptoms of toxicosis, it is better to limit the use of fried, spicy and salt, not to mention coffee and alcohol. It is permissible for a pregnant woman to consume no more than 5-6 g of salt per day per day.
The third point is the power frequency. In the first trimester, it is better to eat in small portions, but often - 5-6 times a day. At the same time, one should not neglect a full breakfast, because its absence can provoke fainting and weakness. The last meal should be no later than 2-3 hours before bedtime. nine0003
What should be in the diet?
In short, products that will provide the developing fetus with essential vitamins and microelements. So, literally from the moment of fertilization, folic acid is necessary for the proper development of the fetus. Therefore, you need to eat foods with a high content of iron, such as liver, eggs, bananas, Brussels sprouts, spinach, etc.
To avoid anemia in the mother and fetus, foods high in iron are needed. These are red meat, liver, nuts and pastries made from coarse flour. nine0003
These are red meat, liver, nuts and pastries made from coarse flour. nine0003
Foods containing magnesium can help to avoid complications and problems with low weight in a baby. It must be taken daily in an amount of at least 300 mg. Avoid coffee and foods containing artificial sweeteners to avoid magnesium deficiency.
For the proper development of the skeletal system, the fetus needs calcium. During the day, the mother needs to receive about 1200 mg of calcium. They are rich in sea fish, eggs and dairy products. And for calcium to be absorbed, it must be taken along with vitamin D.
Among other things, the expectant mother should eat foods rich in Omega-3 complex.
It is possible to minimize problems and errors in nutrition if you think through everything in advance. It is optimal to make a menu for a week, taking into account the necessary calories and trace elements and buy food in advance (except perishable ones). During the period of toxicosis, it is better to prepare a morning snack in the evening so as not to skip breakfast due to poor health.