What do breastfeeding nipples look like
8 ways your nipples can change when you breastfeed
Breastfeeding can be pretty hard on a woman's nipples. Here are the different things that nursing can do to your nipples, and what they mean.
After nine months of pregnancy, we don’t blame you for not recognizing your own body. But when it comes to your nipples specifically, certain changes could mean breastfeeding isn’t going that well, while others are just cosmetic. Here are eight things that breastfeeding can do to your nipples—and when you should worry.
Can nipple shields help with breastfeeding problems?
1. Nipples changing colourIf your nipple is white after feeding (known as blanching), it could be a sign your baby isn’t latching well and cutting off blood supply to your nipple. This is called vasospasm, and is often accompanied by burning, stinging or shooting pain. Fixing the latch usually fixes the problem, although vasospasm can also be a symptom of Raynaud’s disease, and unrelated to breastfeeding. Vasospasm is often misdiagnosed as thrush, because they have similar symptoms.
2. Sore, cracked or bleeding nipples
You may have heard that cracked and bleeding nipples are an unavoidable side effect of breastfeeding, but that’s not the case, says Taya Griffin, a lactation consultant in Toronto. “If a baby is latched on well, you shouldn’t have cracking or bleeding,” she says. If breastfeeding is painful, you may want to seek out a lactation consultant to help with your baby’s latch. Click here to learn more about preventing and treated sore, cracked nipples.
3. Lipstick
nippleIf your nipple comes out of your baby’s mouth flattened, or slanted like a new tube of lipstick, it’s a sign your baby’s latch when breastfeeding isn’t deep enough. You may not feel any pain, but this is still a cause for concern. “In the long term, the milk supply might suffer,” says Griffin.
You may not feel any pain, but this is still a cause for concern. “In the long term, the milk supply might suffer,” says Griffin.
4. Painful blisters on the nipple
Milk blisters, known as blebs, can be white, yellow or clear and look like a pimple on your nipple. They can be extremely painful, and are caused by milk getting backed up behind a milk duct opening, which can lead to blocked ducts and potentially mastitis, a breast infection. Blisters can often be treated at home with warm washcloths and saline solution but if it’s not going away, see your doctor or a lactation consultant.
5. Thrush
Thrush is a yeast infection that can be on your nipple, or in the baby’s mouth, or both. You may notice itchiness, pain or white flakes, and your baby may have white, cheese-curd like patches in his mouth. Griffin notes that thrush is actually rare, and often misdiagnosed. One sign you have thrush is that breastfeeding has been going smoothly and without pain or symptoms, and then symptoms suddenly develop.
6. Nipples appear bigger
Very few women have truly inverted nipples, but some do have fairly flat or slightly inverted nipples, which can get drawn out once your baby latches on and starts feeding. In this case, your nipples didn’t actually grow, but once they’ve been drawn out they will likely stay in their new position, given the appearance of getting bigger.
7. Dark or bumpy areolas
You may notice your areolas—the circular area of pigmented skin around your nipples—got darker and acquired small bumps, which are called Montgomery’s tubercules. These changes actually happened during pregnancy, but many women don’t notice until breastfeeding, when they are spending a good deal of time looking at their breasts.
8. Droopy nipples
One lasting effect of breastfeeding is that your nipples might look droopy, or settle lower than they were before, after you stop breastfeeding. While you may not be entirely pleased with your new look, remember: You birthed and fed a baby! Your body is pretty cool, regardless of how it’s changed.
Read more:
7 breastfeeding tips every nursing mom has to read
7 easy ways to treat mastitis
Stay in touch
Subscribe to Today's Parent's daily newsletter for our best parenting news, tips, essays and recipes.- Email*
- CAPTCHA
- Consent*
Yes, I would like to receive Today's Parent's newsletter. I understand I can unsubscribe at any time.**
FILED UNDER: Breastfeeding breastfeeding problems sore nipples
Inverted and Flat Nipples - La Leche League International
Inverted or Flat Nipples
Prepared by Mary Marine
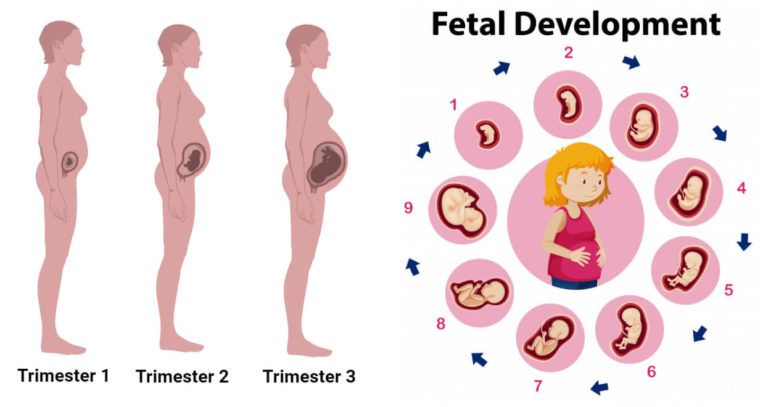
The size and shape of nipples and breasts vary from person to person and can change during the breastfeeding journey. It is common for nipples to gradually change shape, become more elastic and protrude more during pregnancy and while breastfeeding. When babies suck at the breast, they stretch the nipple and surrounding breast tissue into their mouth. The more elastic or stretchy the nipple, the easier it will be for your baby to latch. However, even if the nipples don’t protrude more during pregnancy, you can still breastfeed. These variations often have very little to do with the baby’s ability to breastfeed, because baby latches to the nipple and surrounding breast tissue.
When babies suck at the breast, they stretch the nipple and surrounding breast tissue into their mouth. The more elastic or stretchy the nipple, the easier it will be for your baby to latch. However, even if the nipples don’t protrude more during pregnancy, you can still breastfeed. These variations often have very little to do with the baby’s ability to breastfeed, because baby latches to the nipple and surrounding breast tissue.
If you have inverted or flat nipples, your baby may need more time and patience to breastfeed. A flat nipple is smooth next to the breast tissue. Inverted nipples withdraw below the surface of the nipple. If you think your nipple may be inverted, try placing your thumb and finger on opposite sides of the areola (the darker area of skin surrounding the nipple) and squeezing gently inwards. Sometimes nipples may be partly inverted, looking dimpled or folded. Severely inverted nipples retract deeply when compressed or stimulated. A nipple that stands out when stimulated is not inverted.
After your baby is born, your nipples may appear flatter than usual but babies often lick the nipple to stimulate it before latching on. Your nipples may also appear flatter if your breasts are very full or engorged.
A deep latch and comfortable position helps your baby latch and breastfeed effectively. In the beginning, the following techniques may help you initiate breastfeeding:
- Immediately after birth, place your baby in skin-to-skin contact on your chest. Continue to use skin to skin during early breastfeeding to soothe your baby and to ease frustrations during breastfeeding. Ideally, the breastfeeding dyad is kept together until both are discharged.
- Being with your baby helps you to recognize your infant’s hunger cues.
- Before breastfeeding, express several drops of milk, so the milk is immediately available when your baby latches.
- You may massage your breast while breastfeeding to assist your baby in receiving milk.
To help evert the nipple:
- Pull back on breast tissue so nipple will protrude more.

- Breastfeed in a laidback or side-lying position especially if you have large breasts.
- Breast engorgement can contribute to the nipple being less protruded. Massage the nipple and areolar area so milk will move back into the breast or will leak out, softening the areola and everting the nipple. Also try reverse nipple softening. Reverse pressure softening involves using gentle finger pressure around the base of the nipple to temporarily move some of the swelling slightly backward and upward into the breast.
- Roll the nipple between the thumb and index finger and immediately afterwards touch the nipple with a moist cold cloth. Avoid making the nipple too cold because it can result in the nipple being numb, and inhibit let down.
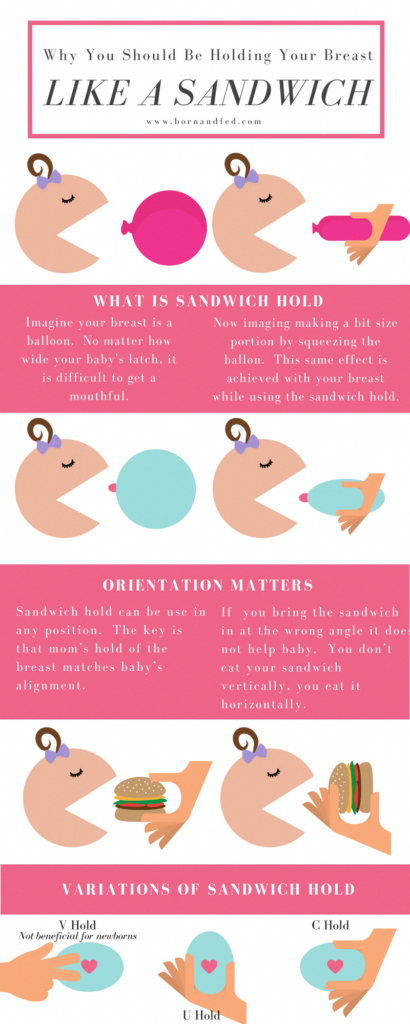
- Use nipple and breast support to help protrude the nipple. Use both hands on each side of breast to make a “sandwich”, to squeeze nipple and areola. Use hands to press in on breast like the way you hold a big sandwich to put in the mouth.

- Use a breast pump for several minutes to draw out the nipple. The suction from a pump will often cause the nipple to protrude more.
- If you have had assistance with latch and tried the tips in this article and your nipples are still sore, consider trying a nipple shield. The nipple shield is a thin silicone devise that goes on top of your nipple and areola while breastfeeding. It looks like a brimmed hat. The nipple shield is a commercially made product. A nipple shield can be used temporarily to help establish breastfeeding or in some cases to help ensure that breastfeeding continues. A shield provides a firm stimulus at the roof of a baby’s mouth where the soft and hard palate meet. This may help your baby suckle more effectively.
- Commercial products that are intended to assist in drawing out inverted nipples such as breast shells or everters are best used only with the guidance of a trained lactation consultant.
If Nipple Soreness Occurs
- You may experience nipple soreness for about the first two weeks of nursing while your flat or inverted nipple is gradually drawn out by baby’s suckling.
 This discomfort is generally the result of adhesions or skin binding to underlying breast tissue. If the soreness is severe, or continues past the initial two weeks, consult your health professional.
This discomfort is generally the result of adhesions or skin binding to underlying breast tissue. If the soreness is severe, or continues past the initial two weeks, consult your health professional. - If your nipple retracts after feedings, that skin may remain moist, leading to chapping of the skin. After feeding, pat your nipples dry and apply a moisturizer safe for breastfeeding. You may also want to wear breast shells or other devices to keep your nipple out between feedings so the skin can dry.
When Nipple Soreness is Prolonged
Rarely, sore nipples may persist for a longer period because instead of stretching, the adhesions remain tight. This can create a stress point which may lead to cracks or blisters.
- If one breast is easier for your baby to grasp and he nurses well from that breast, you can continue to feed on that side. You can pump the breast with the deeply inverted nipple until the adhesions loosen and the nipple is drawn out.
 Your baby will get all the milk he needs from one breast if allowed unlimited and unrestricted time at the breast.
Your baby will get all the milk he needs from one breast if allowed unlimited and unrestricted time at the breast. - If both nipples are deeply inverted, you can pump both breasts simultaneously for 15-20 minutes 8 or more times in 24 hours. You can feed your baby with an alternative feeding device until she is able to latch on effectively and comfortably.
- How long you will need to pump in order to draw out your nipples depends upon the strength of the adhesions and the degree of inversion. One pumping may be enough to completely draw out the nipple. If the nipple continues to deeply invert, you may need to continue pumping. When your nipple stays out after pumping, you can resume breastfeeding immediately.
- Once your nipple can be drawn into the baby’s mouth correctly and the baby can breastfeed effectively, you should be able to discontinue pumping and breastfeed without discomfort.
- On rare occasions you may continue to feel some discomfort even after your nipple has been drawn out.
 This could be due to the correction to the nipple.
This could be due to the correction to the nipple. - The nipple may invert again as your baby pauses during a feeding. In this case, you may need to stop breastfeeding and pump again for a few minutes before putting baby back to the breast.
- As a temporary transition to exclusive breastfeeding, breast compressions or the use of a nursing supplementer might help to encourage continuous sucking and swallowing so that the nipple won’t be as likely to invert during feeding.
If you do encounter challenges during your breastfeeding journey, support from a La Leche League Leader and other participants in Group meetings may help you to overcome the challenges. (Find a Leader or meeting.)
Additional Resources
Cotterman, Jean K., Reverse Pressure Softening, http://breastfeedingmadesimple.com/wp-content/uploads/2016/02/SimplerRPSsheet2.pdf
Cotterman, Jean K., Reverse Pressure Softening, http://www.breastfeedingonline.com/rps.shtml#sthash. 2MPE4KHE.T3v63FBt.dpbs
2MPE4KHE.T3v63FBt.dpbs
Cotterman, Jean K., Engorgement Help: Reverse Pressure Softening
… a technique to aid latching when a mother is engorged, https://kellymom.com/bf/concerns/mother/rev_pressure_soft_cotterman/
Cotterman, Jean K. Reverse Pressure Softening, http://www.health-e-learning.com/articles/RPS_JCotterman_ver2005.htm
Genna, Catherine Watson, Supporting Sucking Skills in Breastfeeding Infants, C. Burlington, MA: Jones & Bartlett, 2012.
La Leche League Great Britain, Nursing Supplementers, https://www.laleche.org.uk/nursing-supplementers/
Mohrbacher, N. Breastfeeding Answers: A guide to helping Families, 2nd edition
(Revised February 2022)
Breastfeeding with pierced, flat or inverted nipples
The shape and size of nipples can vary greatly from woman to woman. Our practical tips will help you make breastfeeding easier, no matter what your nipples are.
Share this information
Most women's nipples protrude, enlarge and swell when touched, but some have flat or even inward nipples. In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
“Don't panic if you have flat or inverted nipples. As a rule, this does not interfere with breastfeeding in any way,” says Shawnad Hilton, a lactation consultant, health visitor and newborn care specialist who has worked with Medela in the UK for more than a decade. “Remember that your baby takes into his mouth not only the nipple, but also part of the breast.”
However, in the early days, when the baby's mouth is still very small and suckling skills have not developed, inverted or flat nipples can make feeding difficult, especially if the baby is unwell or born prematurely.
“Flat or inverted nipples may not reach the baby's palate and therefore not trigger the sucking reflex,” Schoned explains. “That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk. ”
”
How to tell if you have flat or inverted nipples
Flat nipples 1 do not protrude much from the areola (the darker
area surrounding the nipple) even when stimulated.
Inverted nipples seem to be recessed in the center. They may look like this all the time or only if they are stimulated. Sometimes inverted nipples are on the same level with the areola, and sometimes even sink deep into the breast tissue.
This feature may occur on one or both nipples. It is estimated that approximately 10% of nulliparous women have at least one retracted nipple. 2 If you're not sure what type of nipples you have, try a simple pinch test: Gently squeeze your breast with your thumb and forefinger on both sides of the areola. The nipple should come forward. If your nipple hides inside, creating a depression, then it is retracted.
Preparing inverted and flat nipples during pregnancy
You may have noticed that during pregnancy your breasts have changed and your nipples have become more protruding. If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
“In a normal pregnancy, nipple formers can be worn from 32 weeks,” advises Schoned. - Start wearing them for an hour a day, gradually increasing the time to eight hours. If you have an incompetent (weakened) cervix or are at risk of preterm labor, check with your healthcare provider about when you can start using shapers, as nipple stimulation can trigger contractions.”
“Nipple formers can continue to be worn after childbirth,” adds Schoned. “Try to put them in a bra 30 to 60 minutes before feeding.”
“I have inverted nipples, and after two or three weeks of constantly trying to latch on, I almost switched to formula,” recalls Nina, a mother from Germany. “I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.”
“I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.”
How to help your baby latch on to flat or inverted nipples
If your baby enjoys sucking on your thumb but isn't as interested in your breast, chances are your nipple isn't reaching the palate. The baby may become nervous, push off the breast and cry or even fall asleep on your chest. If this happens, ask a lactation consultant or healthcare professional to check the grip.
There are several tricks you can use before every feed to make your nipples more comfortable to latch on to. Schoned recommends the following:
- twist the nipple between thumb and forefinger so that it protrudes better;
- place fingers in a "V" or "C" shape and squeeze the breast just behind the areola to push out the nipple;
- apply a cold compress or ice cube to the nipple to push it forward;
- Express milk manually or with a breast pump for a couple of minutes before feeding so that the nipple comes out more.
“I had a flat nipple, but I only found out about it when I noticed Austin was having trouble suckling on that side,” says Jennifer, mother of two in the UK. “From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.”
Using nursing pads
If none of the above work and your baby still has difficulty latch-on, your lactation consultant or healthcare professional may recommend that you breastfeed with a nursing pad*. They are thin and flexible nipple-shaped silicone funnels with holes at the tip through which milk will flow.
It is easier for the baby to put the feeding pad in his mouth, as it is larger and more rigid. In addition, such an overlay will reach him to the sky, causing a sucking reflex. Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
Over time, as your baby learns to suckle properly and your nipples get used to breastfeeding, you will be able to breastfeed without breast pads.
“My nipples are rather flat. The doctor advised me nursing pads, and I was successfully able to feed my two babies,” says Ann-Sophie, mother of two from Sweden. “My secret is to make them adhere better to the skin, I lightly wet the edges before use.”
Breastfeeding with pierced nipples
Many women with pierced nipples find it does not affect their ability to breastfeed. However, jewelry must be removed before feeding, as the child may choke on them or injure their tongue, gums or palate.
“I had a nipple piercing, but I got it off a year later when I got pregnant because my breasts were very sensitive,” says Kelly, mother of three from the UK. “I breastfed my daughter exclusively, and then her two younger brothers, and never had any problems. And the pierced nipple was my favorite!”
Some women report that milk can leak from piercings, while others believe that piercing scars reduce milk production 4 - but this has not been well researched.
“You can't predict how a piercing will affect breastfeeding until milk production begins,” Schoned explains. - If you are concerned, talk to a lactation consultant or healthcare professional. And remember that one breast may be enough for babies to get the nutrition they need if there are problems with the second. ”
What to do if you can't breastfeed with flat or inverted nipples
If you've tried all the options and still can't breastfeed, you still shouldn't deprive your baby of breastmilk.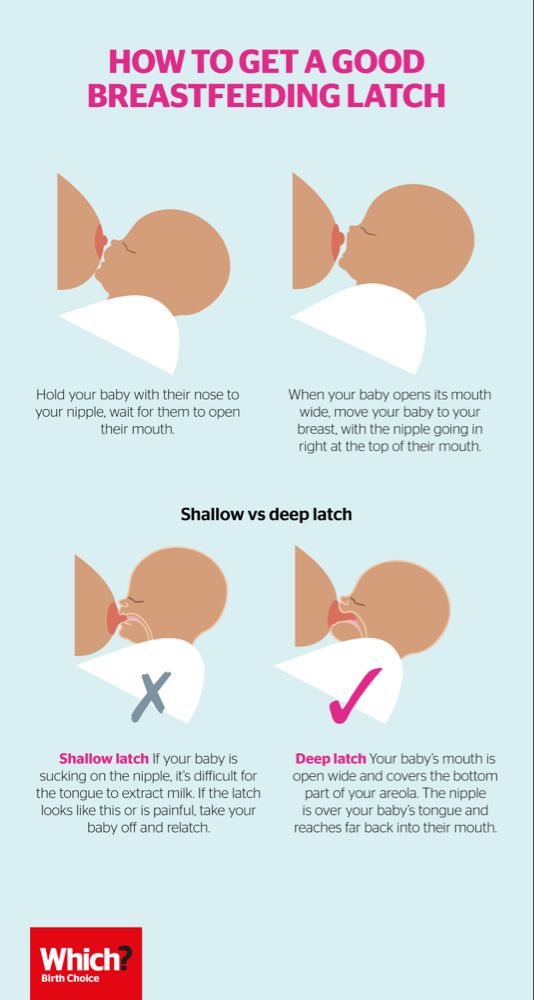
“Mom and baby's health is the most important thing,” says Schoned. “Maybe you should switch to full pumping and feed your baby only expressed milk. You can also try the supplementary feeding system** where the baby continues to feed at the breast while receiving additional expressed milk through a tube. That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more.
“I have inverted nipples. After the disastrous experience of breastfeeding my first son with my second, I decided to get my way after all,” says Babettli, mother-of-two from Italy. - On the advice of experts, I tried nipple formers and nursing pads, but everything was unsuccessful. In the end, pumping with the Medela Symphony*** Double Electronic Clinical Breast Pump proved to be the best solution for us. I fed exclusively on expressed milk for up to four months.”
Care for different types of nipples
Flat or inverted nipples may require extra care as the baby may squeeze them harder and they may become inflamed at first. Tips on how to care for sore nipples can be found in Nursing Nipple Care.
Tips on how to care for sore nipples can be found in Nursing Nipple Care.
If your nipples become inverted after a feed, any moisture can lead to inflammation and increase the risk of infections, including thrush. Blot your nipples dry after each feed before they have time to hide inside.
With swelling of the mammary glands, when even protruding nipples can become flat, flat or inverted nipples can be difficult. Read the helpful tips in the article on breast swelling.
The good news is that continuous breastfeeding or pumping can change the shape of your nipples and breastfeeding will become easier over time. With the arrival of the next child, you may not have to face this problem at all, as happened with Leanne, a mother of two from the UK.
“The second feeding was like a fairy tale,” she says. “After almost four months of pumping for my first son, my flat nipples were so extended that with my second son I no longer had to use breast pads - he was able to suck directly from the breast. The youngest is now nine months old and I still breastfeed him.”
The youngest is now nine months old and I still breastfeed him.”
Literature
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing ; 2015. - Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast . 1997;6(2):72-78. — Alexander JM, Campbell MJ, "Prevalence of inverted and intractable nipples in pregnant women who intend to breastfeed." Ze Brest (Chest). 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature.Breastfeeding Medicine. 2010;5(6):309-314. — McKechnie A.S., Eglash A., "Nipple Covers: A Review of the Literature". Brestfeeding Medicine (Breastfeeding Medicine). 2010;5(6):309-314.
2010;5(6):309-314.
4 Garbin CP0106 , Rowan MK , Hartmann PE , Geddes DT . Association of nipple piercing with abnormal milk production and breastfeeding. JAMA, Journal of the American Medical Association. 2009;301(24):2550-2551. - Garbin S.P., Deacon J.P., Rowan M.C., Hartmann P.I., Geddes D.T., "Nipple piercing and its impact on abnormal milk production and breastfeeding", JAMA (Journal of the American medical association). 2009;301(24):2550-2551.
Read instructions before use. Consult a specialist about possible contraindications.
* RC No. FSZ 2010/07352 dated 07/19/10
** RC No. FSZ 2010/07353 dated 07/19/10
*** RC No. FSZ 2010/06525 dated 17/03/2021 nursing mothers | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples.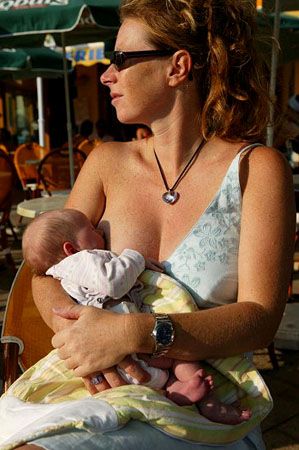 Check out our tips and tricks to help reduce the pain.
Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
A mother of three, Sioned Hilton has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.
In most women during pregnancy, the nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. 1 This sucking, pressure and saliva of the baby can cause sore nipples.
1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible. 2
Prevention is better than cure, so check out our tips.
Check your baby's latch on
Correct latch is the key to pain-free breastfeeding. When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby.
Check tongue frenulum
Tongue frenulum (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin that attaches the tongue to the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum. A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding tips for nipples
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples. Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6
- Pat the nipples gently with a soft towel or simply let them air dry.
 In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past!
In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past! - Do not wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's intestinal microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.
- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain. 9
Healthy teat care products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool.
 It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding.
It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding. - Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit inside a bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.
- Nursing Bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples.
- Nursing pads* are special silicone pads that are worn over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer. Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.

When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review. Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al., "Bacterial communities in breast milk and their association with the occurrence and development of the neonatal gut microbiome.