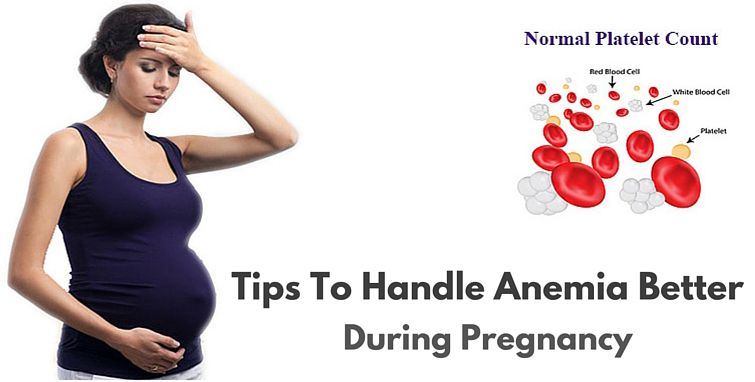
What causes low iron in pregnancy
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
When you're pregnant, you may develop anemia. When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia. This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.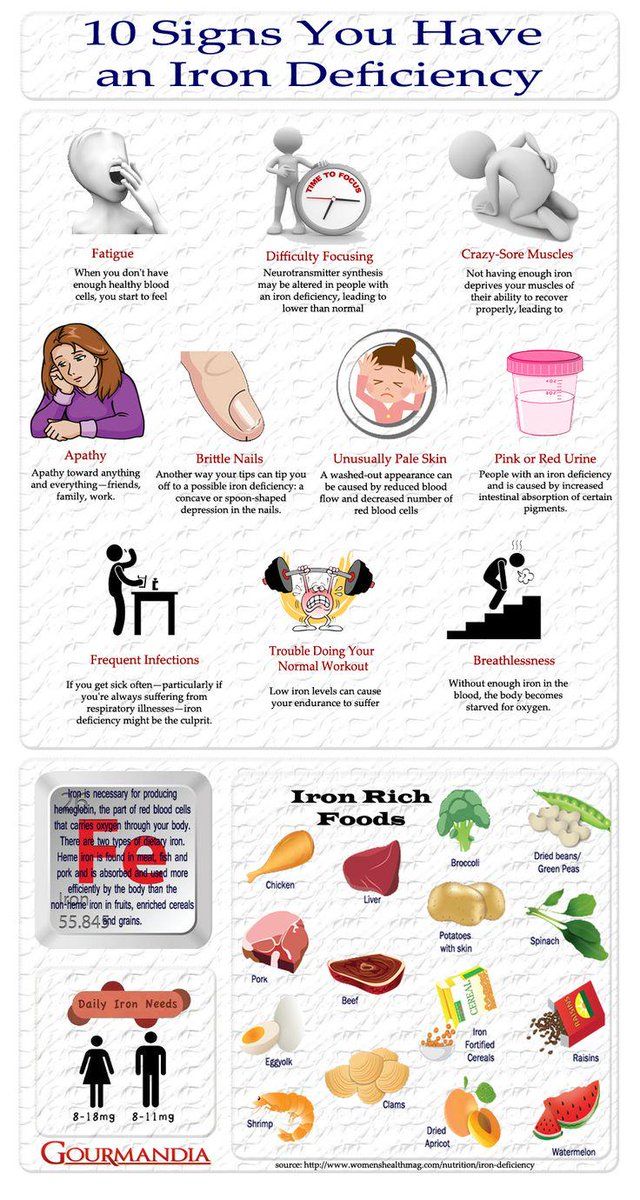
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic. That's because they need more iron and folic acid than usual. But the risk is higher if you:
That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms. And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.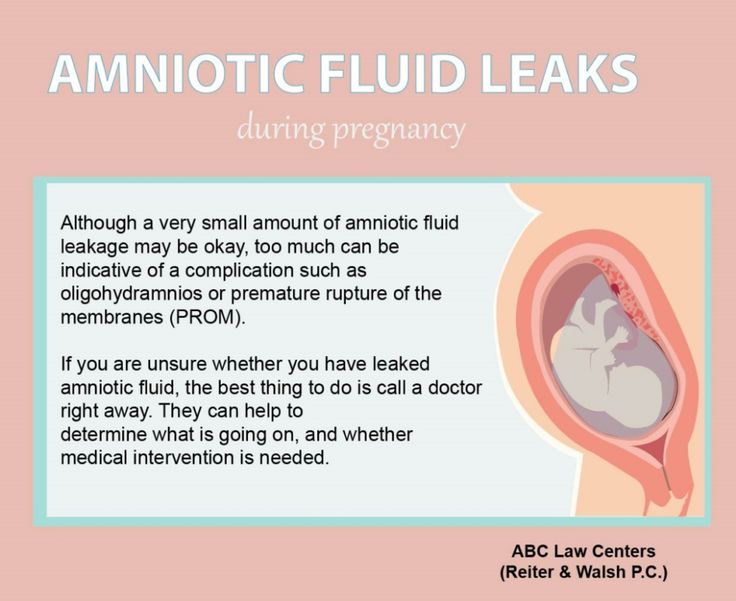
Tests for Anemia
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia. Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron. These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
When you're pregnant, you may develop anemia. When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia.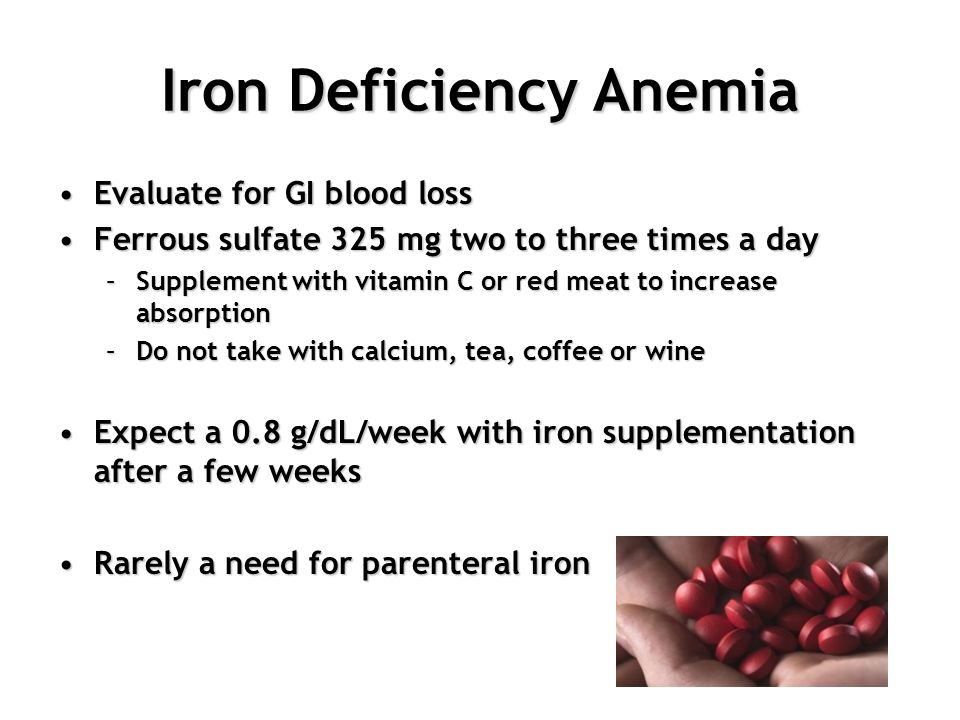 This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.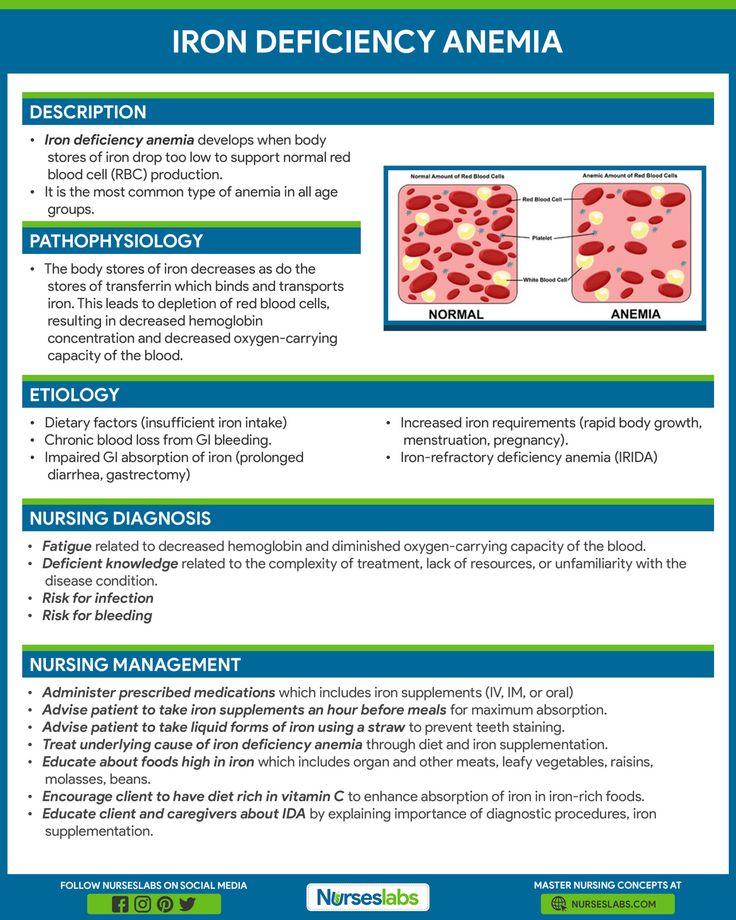
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic. That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms.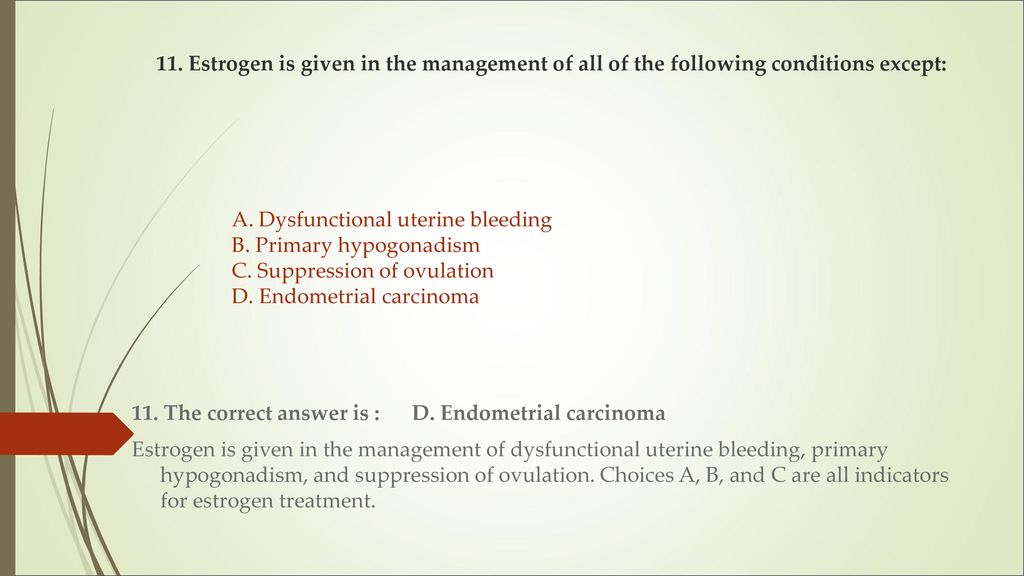 And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.
Tests for Anemia
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia.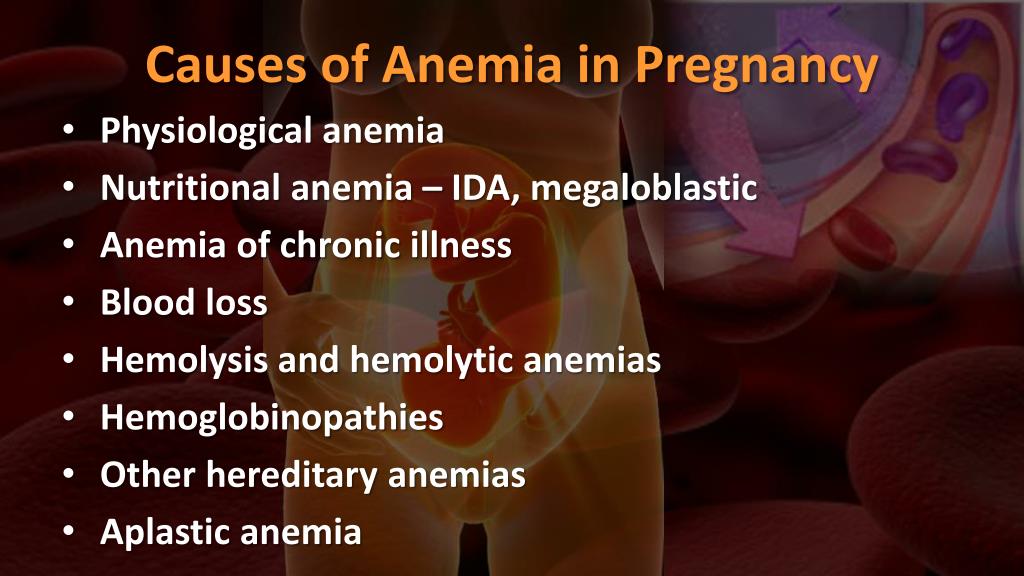 Blood tests typically include:
Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.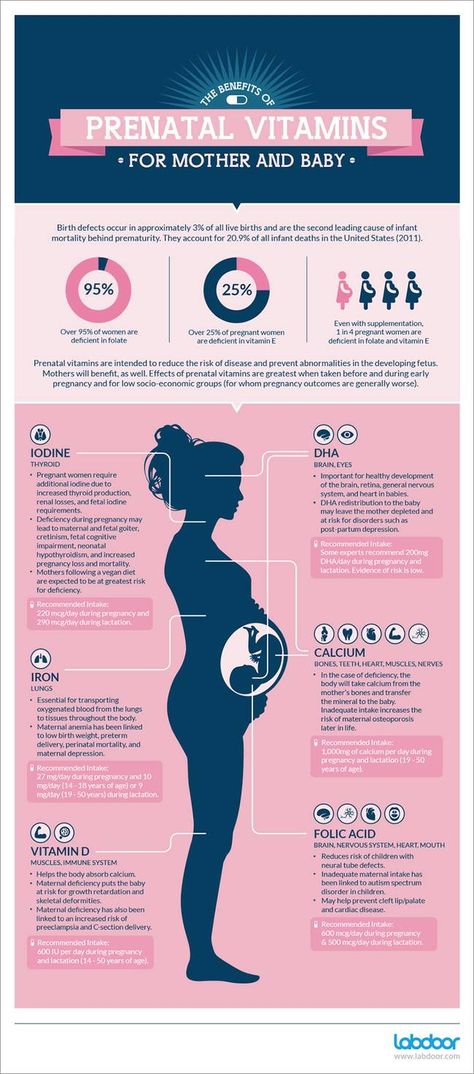
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron. These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Anemia during pregnancy - iron arguments and dispelling myths
Anemia is one of the most common complications that occur during pregnancy.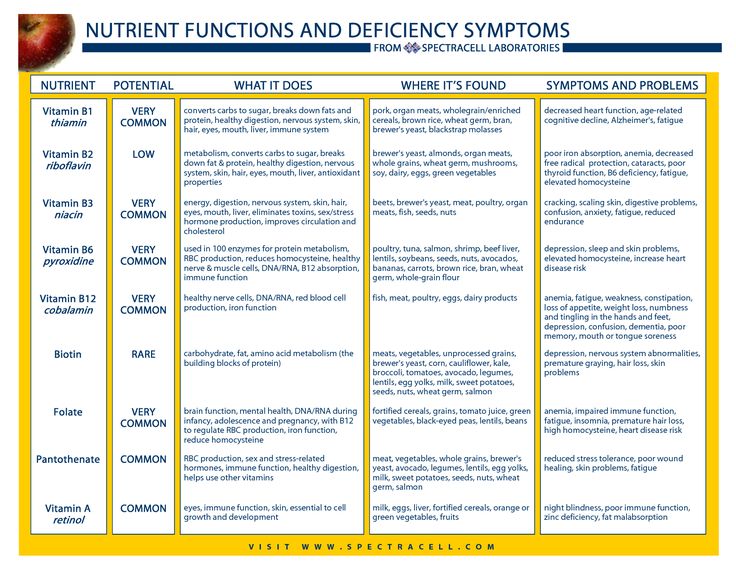 In Russia, this diagnosis is made to every third pregnant woman. However, not everyone, faced with this diagnosis, understands what is at stake and what needs to be done in order for the treatment to be as effective as possible.
In Russia, this diagnosis is made to every third pregnant woman. However, not everyone, faced with this diagnosis, understands what is at stake and what needs to be done in order for the treatment to be as effective as possible.
Anemia is a disease in which the level of hemoglobin in the blood decreases, often with a simultaneous decrease in the number of red blood cells. The main reason for the development of anemia is the discrepancy between the intake of iron in the body and its costs. nine0003
During pregnancy, the cost of the growing fetus causes a significant increase in iron requirements. In addition, a less common but possible cause of anemia may be insufficient intake of folic acid or vitamin B12.
Risk factors for developing iron deficiency anemia during pregnancy include:
- history of heavy menses;
- diseases of the gastrointestinal tract;
- infectious and inflammatory diseases; nine0014
- anemia in the past;
- short interval between pregnancies, including conception during lactation;
- multiple pregnancy.

Since the main task of hemoglobin is to deliver oxygen - a vital element - to all tissues and cells of a woman and fetus, it is easy to imagine the harm caused by its decrease during pregnancy. However, even after childbirth, the issue cannot be considered closed. It has been proven that a low level of hemoglobin is associated with a decrease in lactation, as well as with the development of anemia in a child. nine0003
Iron deficiency anemia is manifested by weakness, dizziness, pathological fatigue, perverted perception of tastes and smells, heart palpitations, shortness of breath, headache, fainting. The skin becomes dry and pale, and the hair and nails brittle.
The diagnosis of anemia is made based on the assessment of hemoglobin levels in the complete blood count. The lower limit of the hemoglobin norm during pregnancy is 110 g / l. However, before hemoglobin decreases, iron stores are depleted, which is manifested by a decrease in serum ferritin levels. This condition is called latent iron deficiency and also requires correction. nine0003
This condition is called latent iron deficiency and also requires correction. nine0003
Treatment of anemia and latent iron deficiency is with iron supplements, most commonly given as tablets or oral solution, but sometimes intravenous solutions are used. This need arises when the hemoglobin level is very low or in case of impaired absorption of iron from the gastrointestinal tract.
It is also important to be aware of the potential of a protein diet in correcting iron deficiency. Since hemoglobin is a bond between two subunits - metal-containing heme and globin protein - then with insufficient protein intake, even an adequate amount of iron in the body has nothing to contact. nine0003
When diagnosing anemia, it is important for the patient to remember that the consumption of foods high in iron will only help maintain the existing hemoglobin level, but will not be able to increase its level and saturate iron stores to a sufficient extent.
Separately, I would like to dwell on what kind of products the iron content is really high.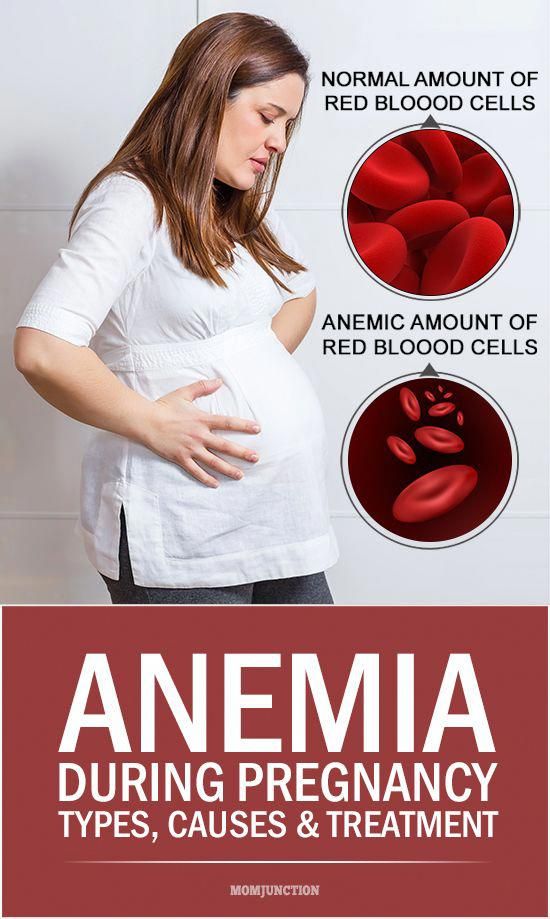 A common misconception is that people with anemia should eat apples, beets, and pomegranates, as well as drink pomegranate juice. 100 grams of apples contain 0.5 - 2.2 mg of iron; 100 grams of beets - 1.0 - 1.4 mg of iron; 100 grams of pomegranates - 0.78 mg of iron. Cucumbers, strawberries, pumpkins and other fruits and vegetables contain approximately the same amount of iron. For comparison, buckwheat contains 8 mg of iron per 100 g of product, dried fruits (dried apricots, prunes, dried apples) - from 12 to 15 mg of iron. The leader in iron content is pork liver. In addition, the content of this microelement is high in beef liver, cocoa, lentils, egg yolk, heart. nine0003
A common misconception is that people with anemia should eat apples, beets, and pomegranates, as well as drink pomegranate juice. 100 grams of apples contain 0.5 - 2.2 mg of iron; 100 grams of beets - 1.0 - 1.4 mg of iron; 100 grams of pomegranates - 0.78 mg of iron. Cucumbers, strawberries, pumpkins and other fruits and vegetables contain approximately the same amount of iron. For comparison, buckwheat contains 8 mg of iron per 100 g of product, dried fruits (dried apricots, prunes, dried apples) - from 12 to 15 mg of iron. The leader in iron content is pork liver. In addition, the content of this microelement is high in beef liver, cocoa, lentils, egg yolk, heart. nine0003
Prevention of iron deficiency anemia in pregnant women is a study of iron stores and hemoglobin levels at the stage of pregnancy planning, and if deviations from the norm are detected, their timely correction, consumption of foods high in iron, intake of vitamin and mineral complexes containing prophylactic doses of iron.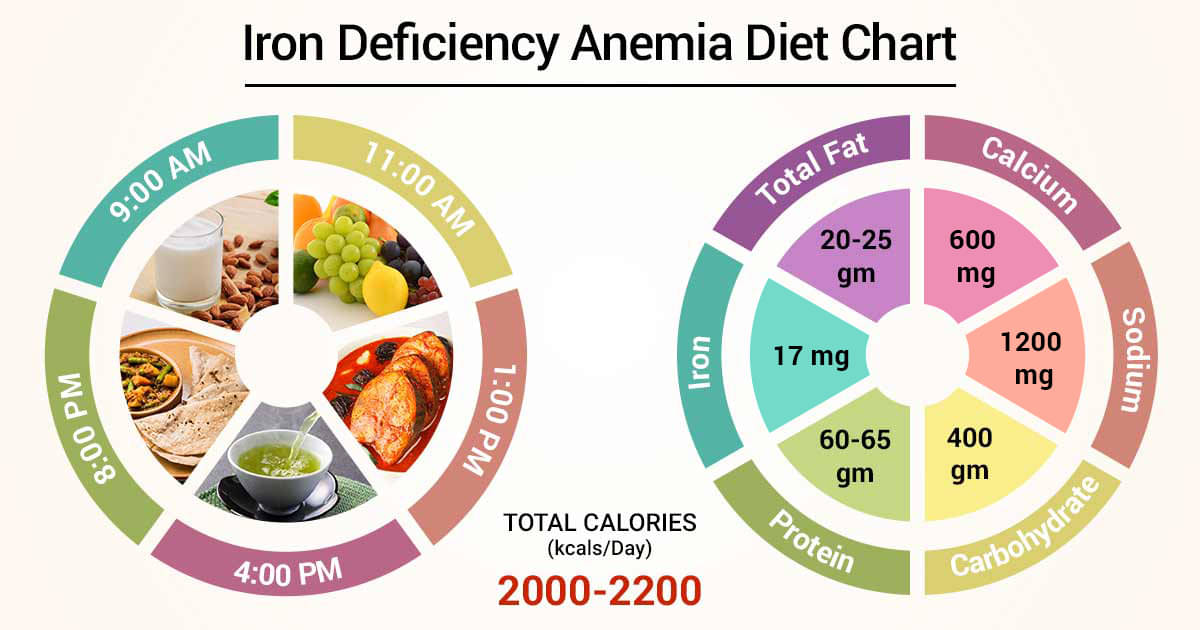
Obstetrician-gynecologist
antenatal clinic No. 14
Khivrich E.B.
ANEMIA and PREGNANCY, OUTPATIENT
Anemia of pregnancy is a series of anemic conditions that occur during pregnancy, complicate its course and usually disappear soon after childbirth or after its termination. Since the prevalence of anemia in pregnant women is much higher than in non-pregnant women, it is logical to assume that most of these anemias are related to the pregnancy itself. Isolation in the ICD-10 anemia of pregnant women (this code is O 99.0) in a separate heading emphasizes the peculiarity of this group of anemia, which consists in the existence of physiological and pathophysiological changes characteristic of pregnancy that contribute to the development of anemia. nine0003
The most common consequences of anemia in pregnancy are miscarriage, premature birth, intrauterine growth retardation and an increased risk of low birth weight babies. The development of anemia in the 1st and 2nd trimesters of pregnancy is associated with a two-fold increase in the risk of preterm birth.
Most researchers believe that iron stores in the fetus do not depend on the iron content in the mother's body. The transfer of iron from the mother through the placenta is regulated by the needs of the fetus, even against the concentration gradient, and mainly occurs in the 3rd trimester of pregnancy. That is why the development of iron deficiency is possible only in premature babies. nine0003
These adverse effects of anemia in pregnancy are generally associated with hemoglobin levels < 90 g/l. With a hemoglobin level of 90-110 g / l in the second half of pregnancy, the prognosis for a woman and a child is favorable. At the same time, an increase in the concentration of Hb above 120 g / l in this period of gestation is fraught with a high risk of complications (in particular, preeclampsia).
Any pregnancy results in an increase in plasma volume, which averages 1250 ml. This is approximately 1.5 times the plasma volume in non-pregnant women. This condition is one of the main reasons for the relative decrease in Hb levels in pregnant women.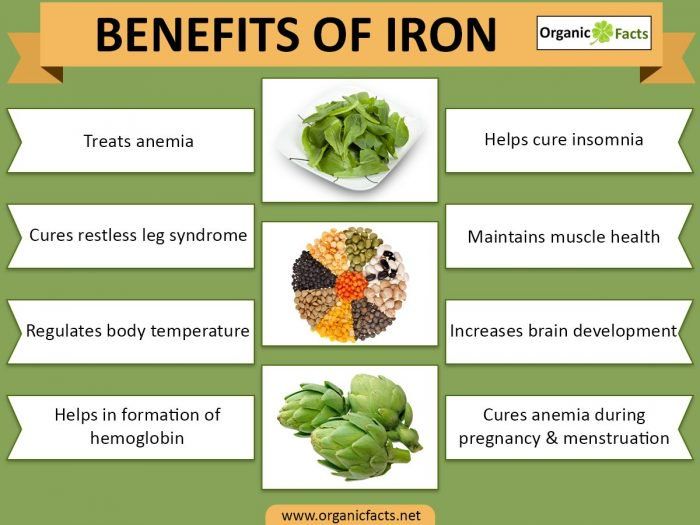 nine0003
nine0003
Today, the lower limit of the normal concentration of Hb in pregnant women is 110 g / l, Hb from 90 to 110 g / l is anemia of 1 degree, from 70 to 90 g / l - anemia of 2 degrees, < 70 g / l - anemia 3 tbsp.
According to WHO, 35-75% of pregnant women in the world are anaemic every year. In domestic obstetric practice, the prevalence of iron deficiency in pregnant women is considered to be high.
Pregnancy anemia is multifactorial, and iron deficiency is an important, but by no means the only, cause of anemia during pregnancy. nine0003
FORMS OF ANEMIA.
| Acquired | Hereditary |
| 1. iron deficiency 2. Post -hemorrhagic 3. Folic -deck 4. Anemia of inflammation 5.molytic 9000. | 1. Thalassemias 2. Sickle cell diseases 3. Anemias in other hemoglobinopathies 4. Hemolytic anemias outside of hemoglobinopathies |
The most common types of anemia in pregnancy include iron deficiency anemia (IDA) and folic deficiency anemia, and less frequent are aplastic, megaloblastic, hemolytic anemias.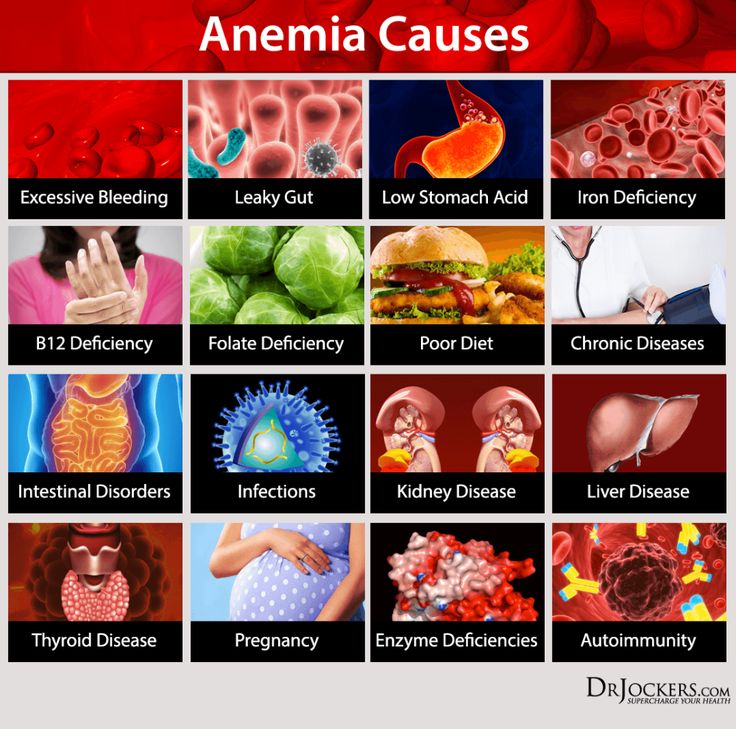
Factors that predispose to the development of IDA in pregnant women include frequent bleeding with placenta previa; anemia that existed in the patient's mother during pregnancy and prematurity of the patient, as well as seasonality and related changes in the composition of food (vitamin deficiency in the winter-spring period). nine0003
Anemia of inflammation - in recent years, there has been an increase in the number of women with urogenital infections (colpitis, cervicitis, bacterial vaginosis, pyelonephritis, etc.), which often occur latently. At the same time, about 30% of pregnant women with urogenital infections approach childbirth in a state of anemia, despite the repeated correction with iron preparations. This anemia is defined as "hypochromic anemia without iron deficiency" with normal or elevated iron stores in the body.
Complaints with anemia during pregnancy are usually rare, usually in the presence of concomitant pathology. The most characteristic are complaints of weakness, dizziness, fatigue, in more severe cases, shortness of breath, anxiety and impaired consciousness.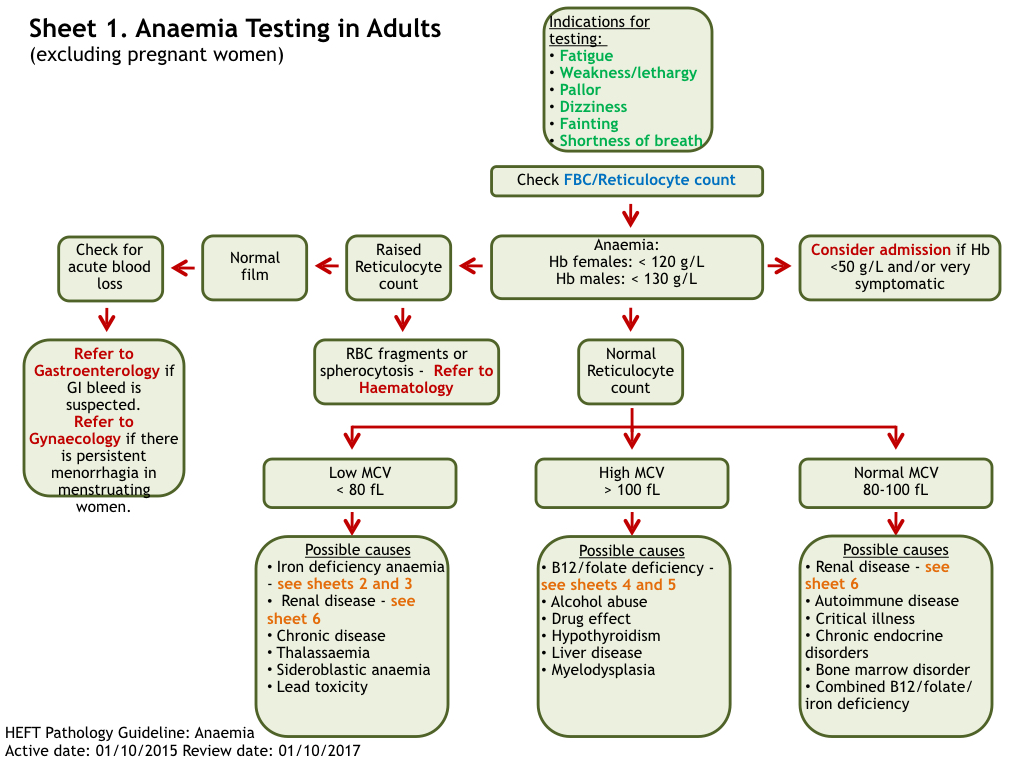
Examination and treatment at the outpatient stage of patients with anemia in pregnancy is carried out in accordance with the Order of the Ministry of Health of the Russian Federation dated 01.11.2012. No. 572n.
Examination at the outpatient stage:
1) Completed general clinical blood test once a month with leukocyte count, count of reticulocytes and platelets. nine0003
2) ECG in each trimester.
3) Biochemical blood test (total protein, serum iron, ferritin, transferrin, total and direct bilirubin).
4) Consultation with a general practitioner (hematologist) and further follow-up (1-2 times a month).
5) Clarification of the diagnosis and resolution of the issue of the possibility of continuing the pregnancy up to 10 weeks.
6) Bone marrow puncture (as prescribed by a hematologist).
7) CTG and dopplerometry in dynamics. nine0003
Outpatient treatment:
1) Diet rich in proteins, iron, vitamins and folates.
2) Preparations containing iron (in accordance with the Decree of the Government of the Russian Federation of December 26, 2015 N 2724-r, which contains a list of vital and essential drugs for medical use for 2016) - these are oral preparations of 3-valent iron - iron 3 hydroxide polymaltose (maltofer, fenyuls, ferrum lek). It is not recommended to stop taking iron supplements after normalization of hemoglobin levels. nine0044
3) Treatment of underlying and concomitant diseases.
Indications for hospitalization:
1) Deterioration of the pregnant woman's condition, lack of effect from outpatient treatment of pregnancy complications.
2) Planned hospitalization for delivery at 38-39 weeks.
Prevention of anemia in pregnancy.
To maintain a normal iron balance during pregnancy, it is necessary that:
1. iron stores in the woman's body by the beginning of pregnancy are adequate; nine0003
2. The pregnant woman's diet contained sufficient bioavailable iron to ensure high levels of intestinal absorption in the 2nd half of pregnancy.
The daily iron requirement of a pregnant woman is estimated at 27 mg. Lower intake in women with inadequate iron stores may lead to anemia. Iron absorption is greatly increased in the presence of ascorbic acid. Therefore, it is most beneficial to consume foods containing iron in combination with foods fortified with vitamin C.
WHO recommends 60 mg iron per day for all pregnant women in areas where the prevalence of IDA is less than 20% and 120 mg where it is above this value.
Prevention of iron deficiency during pregnancy planning is an ideal form of prevention of IDA in pregnant women.
Primary prevention of IDA in pregnant women aims to reduce the prevalence of iron deficiency during pregnancy and prevent the adverse effects it can cause on the woman and fetus. nine0079
2014
1803
382
21,2
2015
1782
462
26
Statistical data on the incidence of anemia for 6 months. 2015 and 6 months 2016
2015 and 6 months 2016
| Finished pregnancy | Anemia of pregnancy | % | |
| 6 months 2015 | 845 | 155 | 18% |
| 6 mon. 2016 | 1118 | 250 | 22.3% |
If you analyze the above incidence of anemia in pregnant women over the past 3 years, then we can say the following, which in 2013. and in 2015 % of this pathology among pregnant women remained approximately at the same level, in 2014 there was a slight decrease in this indicator to 21.2%. nine0003
Management of patients with anemia of pregnancy in the w/c No. 2.
No. 572n.
2. When the diagnosis of anemia of pregnancy is established, the patient is referred for a consultation with a general practitioner f/c.
3. With anemia 2-3 tbsp. and not amenable to correction of anemia 1 tbsp.