What causes braxton hicks contractions
Braxton Hicks Contractions: Causes & Relief
Toward the end of your pregnancy, you might start wondering how you'll know when you're in labor. It can be especially confusing if you experience contractions in the second or third trimester that go away without leading to labor. These are called Braxton Hicks contractions, and they're one of the ways your body gets ready for labor.
What Are Braxton Hicks Contractions?
Also known as "false" or "practice" contractions, Braxton Hicks contractions (named after the doctor who first identified them) are not actual labor contractions, but they are caused by the muscles of the uterus tightening, just as real labor contractions are. Braxton Hicks contractions help your body prepare for birth by tightening and relaxing the uterine muscles, although they're not actually opening the cervix. This will happen when true labor contractions start. Knowing how long your contractions last and how frequently they occur can help you determine whether you're experiencing real labor contractions or not. To help keep on top of this, download our guide to tracking your contractions.
What Do Braxton Hicks Contractions Feel Like?
Braxton Hicks contractions can be mild — you may detect sensations of tightening and relaxing of the uterus — but they can also be a bit more painful. These contractions may start out feeling something like familiar menstrual cramps, but can grow more intense in the final few weeks of pregnancy.
Luckily, there are a few ways to help ease the discomfort of these contractions, while also confirming that labor hasn't started yet. Try to change positions if you're seated or lying down, or go for a brief walk if possible. Movement can help these contractions subside. False contractions are also more likely to strike when you're dehydrated, so be sure to drink plenty of water, especially as your due date approaches.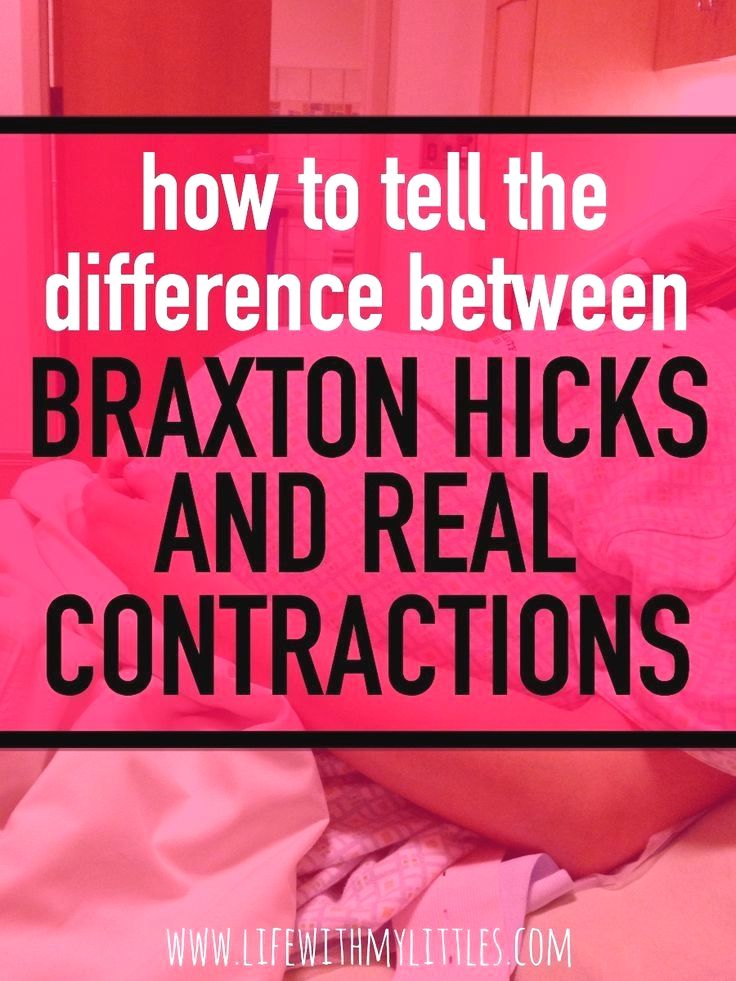
When Can Braxton Hicks Contractions Start?
Braxton Hicks contractions usually start in the third trimester, although you might notice them in the second trimester as well. They may begin a little earlier if this is not your first pregnancy.
When these contractions begin in the second trimester, they are generally mild, and they're more likely to strike after physical activity, like exercise or sex. They'll usually pass quickly, but if they become painful or regular, let your healthcare provider know right away.
Braxton Hicks vs. True Labor Contractions
If you notice contractions before your 37th week of pregnancy, you might worry you're going into preterm labor at the first sign of a contraction. And, if your pregnancy is full term, you might be wondering whether the contraction you're feeling is another Braxton Hicks or if it's finally the real deal.
To help sort this out, familiarize yourself with the symptoms of labor. It also helps to know what Braxton Hicks contractions feel like, and to keep in mind the following differences between Braxton Hicks and true labor contractions:
If you're not sure whether you're experiencing Braxton Hicks or true labor contractions, consult your healthcare provider. And if you notice any of the following signs of labor, contact your provider right away:
Abdominal cramps or pressure
Changes in vaginal discharge (discharge that is clear, pink, or slightly bloody or brownish could mean the mucus plug has come out)
Dull lower backache
Your water breaking.
If you're stocking up your baby's room or your hospital bag with diapers and wipes for your newborn, don't miss out on the rewards you could be getting. Download the Pampers Rewards App today.
Braxton Hicks contractions can cause a little discomfort, but they're a completely normal part of pregnancy. They play a key role in helping your body prepare for the big day when you actually go into labor.
They play a key role in helping your body prepare for the big day when you actually go into labor.
How we wrote this article The information in this article is based on the expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
Braxton Hicks Contractions - StatPearls
Deborah A. Raines; Danielle B. Cooper.
Author Information
Last Update: August 8, 2022.
Continuing Education Activity
Braxton-Hicks contractions, also known as prodromal or false labor pains, are contractions of the uterus that typically are not felt until the second or third trimester of the pregnancy. Braxton-Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun.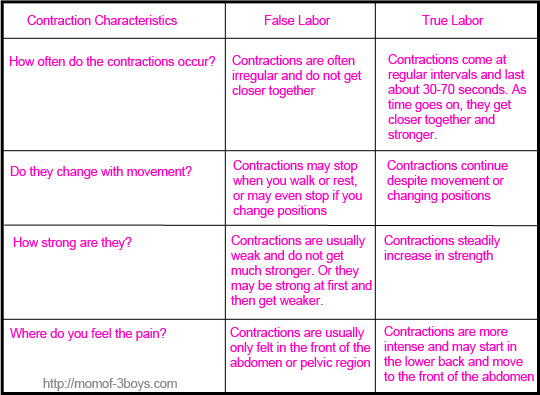 Because many pregnant patients have not been educated about Braxton-Hicks contractions, they often seek care and undergo unnecessary evaluation for these contractions. This activity reviews the evaluation and management of patients with Braxton-Hicks contractions and highlights the role of the interprofessional team in educating the patient about the condition.
Because many pregnant patients have not been educated about Braxton-Hicks contractions, they often seek care and undergo unnecessary evaluation for these contractions. This activity reviews the evaluation and management of patients with Braxton-Hicks contractions and highlights the role of the interprofessional team in educating the patient about the condition.
Objectives:
Describe the etiology of Braxton-Hicks contractions.
Review the presentation of a patient with Braxton-Hicks contractions.
Explain how to evaluate a patient with Braxton-Hicks contractions.
Employ strategies to improve interprofessional communication, which will improve outcomes in patients with Braxton-Hicks contractions.
Access free multiple choice questions on this topic.
Introduction
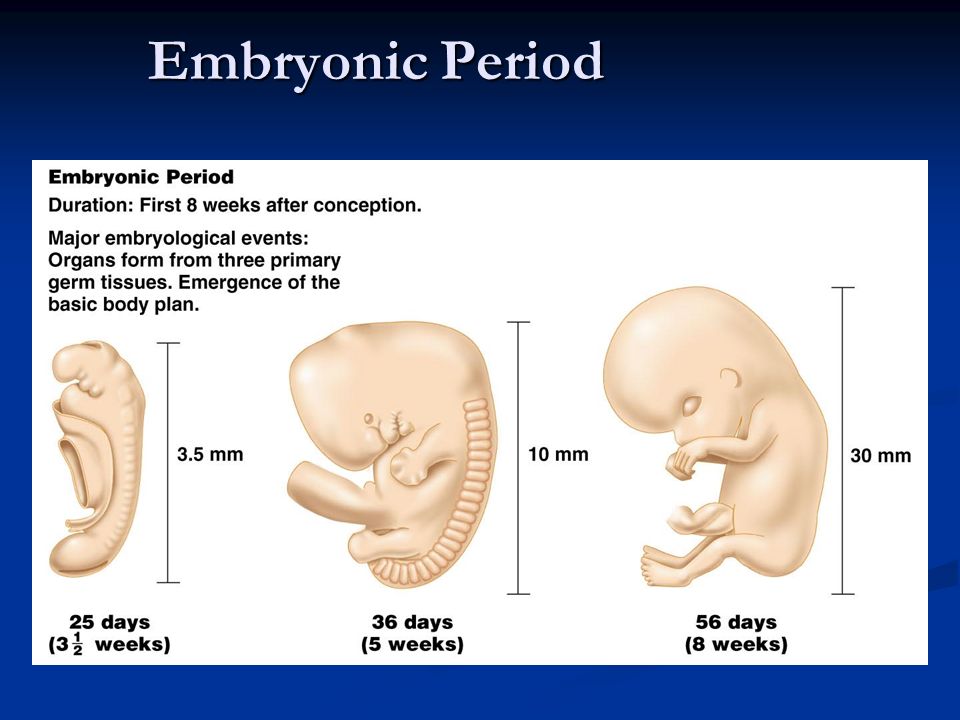
Braxton Hicks contractions are sporadic contractions and relaxation of the uterine muscle. Sometimes, they are referred to as prodromal or “false labor" pains. It is believed they start around 6 weeks gestation but usually are not felt until the second or third trimester of the pregnancy. Braxton Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun or is going to start.
It is believed they start around 6 weeks gestation but usually are not felt until the second or third trimester of the pregnancy. Braxton Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun or is going to start.
Braxton Hicks contractions are a normal part of pregnancy. They may be uncomfortable, but they are not painful. Women describe Braxton Hicks contractions as feeling like mild menstrual cramps or a tightening in a specific area of the abdomen that comes and goes.[1][2][3]
Braxton Hicks contractions can be differentiated from the contractions of true labor. Braxton Hicks contractions are irregular in duration and intensity, occur infrequently, are unpredictable and non-rhythmic, and are more uncomfortable than painful. Unlike true labor contractions, Braxton Hicks contractions do not increase in frequency, duration, or intensity. Also, they lessen and then disappear, only to reappear at some time in the future.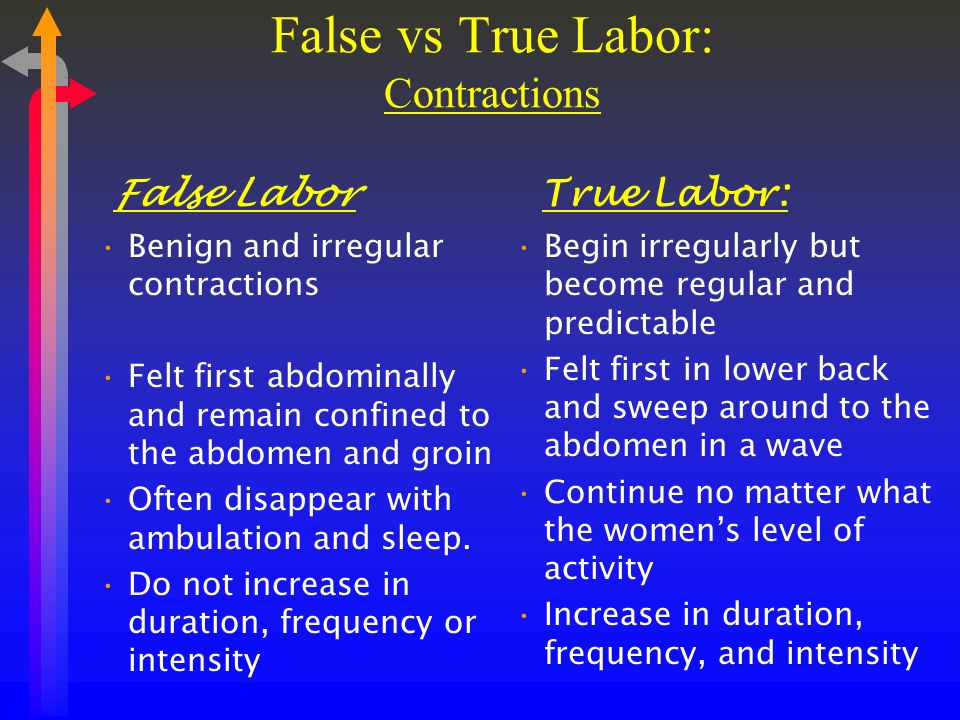 Braxton Hicks contractions tend to increase in frequency and intensity near the end of the pregnancy. Women often mistake Braxton Hicks contractions for true labor. However, unlike true labor contractions, Braxton Hicks contractions do not cause dilatation of the cervix and do not culminate in birth.
Braxton Hicks contractions tend to increase in frequency and intensity near the end of the pregnancy. Women often mistake Braxton Hicks contractions for true labor. However, unlike true labor contractions, Braxton Hicks contractions do not cause dilatation of the cervix and do not culminate in birth.
Etiology
Braxton Hicks contractions are caused when the muscle fibers in the uterus tighten and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are known circumstances that trigger Braxton Hicks contractions including when the woman is very active, when the bladder is full, following sexual activity, and when the woman is dehydrated. A commonality among all these triggers is the potential for stress to the fetus, and the need for increased blood flow to the placenta to provide fetal oxygenation.[4][5][6]
Epidemiology
Braxton Hicks contractions are present in all pregnancies. However, each woman's experience is different. Most women become aware of Braxton Hicks contractions in the third trimester, and some women are aware of them as early as the second trimester. Sometimes Braxton Hick contractions occurring near the end of the third trimester of pregnancy are mistaken as the onset of true labor. It is not unusual, especially in a first pregnancy, for a woman to think she is in labor only to be told it is Braxton Hicks contractions and not true labor.
Sometimes Braxton Hick contractions occurring near the end of the third trimester of pregnancy are mistaken as the onset of true labor. It is not unusual, especially in a first pregnancy, for a woman to think she is in labor only to be told it is Braxton Hicks contractions and not true labor.
Pathophysiology
Braxton Hicks contractions are thought to play a role in toning the uterine muscle in preparation for the birth process. Sometimes Braxton Hicks contractions are referred to as "practice for labor." Braxton Hicks contractions do not result in dilation of the cervix but may have a role in cervical softening.
The intermittent contraction of the uterine muscle may also play a role in promoting blood flow to the placenta. Oxygen-rich blood fills the intervillous spaces of the uterus where the pressure is relatively low. The presence of Braxton Hicks contractions causes the blood to flow up to the chorionic plate on the fetal side of the placenta. From there the oxygen-rich blood enters the fetal circulation.
History and Physical
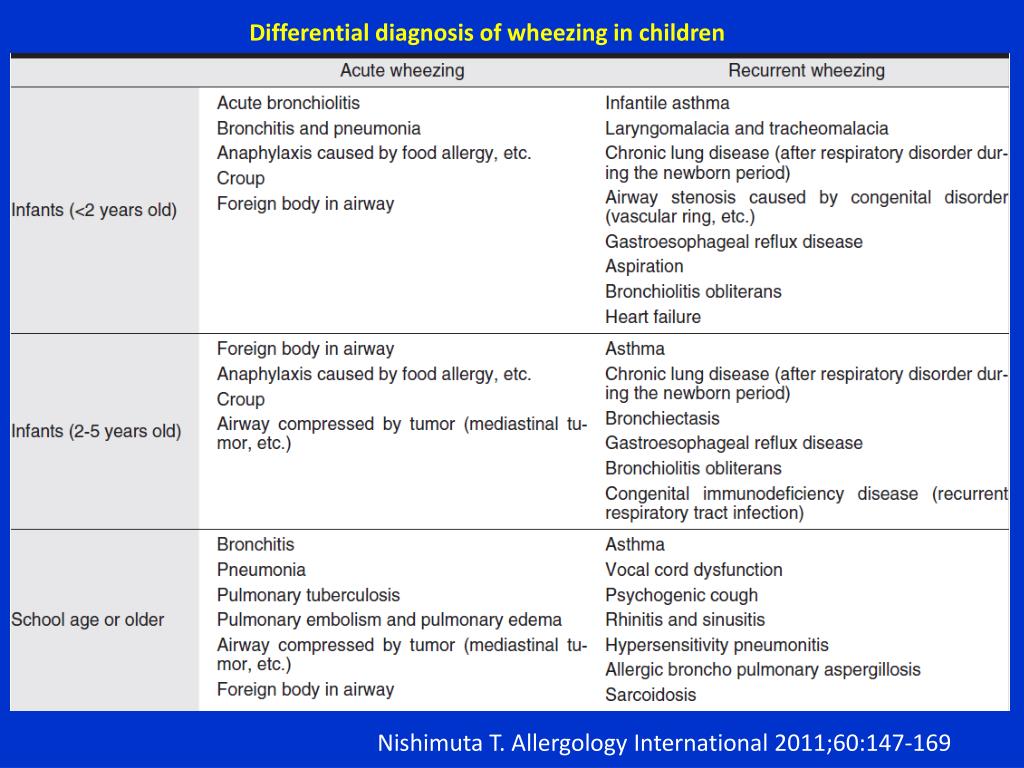
When assessing a woman for the presence of Braxton Hicks contractions, there are some key questions to ask. Her response to these questions will assist the healthcare provider to differentiate Braxton Hicks contractions and true labor contractions.[7][8][9]
How often are the contractions? Braxton Hicks contractions are irregular and do not get closer together over time. True labor contractions come at regular intervals, and as time goes on, they get closer together and stronger.
How long are the contractions? Braxton Hicks contractions are unpredictable. They may last less than 30 seconds or up to 2 minutes. True labor contractions last between 30 to less than 90 seconds and become longer over time.
How strong are the contractions? Braxton Hicks contractions are usually weak and either stay the same or become weaker and then disappear. True labor contractions get stronger over time.
Where are the contractions felt? Braxton Hicks contractions are often only felt in the front of the abdomen or one specific area.
 True labor contractions start in the midback and wrap around the abdomen towards the midline.
True labor contractions start in the midback and wrap around the abdomen towards the midline.Do the contractions change with movement? Braxton Hicks contractions may stop with a change in activity level or as the woman changes position. If she can sleep through the contraction, it is a Braxton Hicks contraction. True labor contractions continue and may even become stronger with movement or position change.
During the physical assessment, the provider may palpate an area of tightening or a "spasm" of the uterine muscle, but the presence of a uterine contraction in the uterine fundus is not palpable. The woman will be assessed for the presence of uterine bleeding or rupture of the amniotic membrane. An examination of the cervix reveals no change in effacement or dilatation as a result of the Braxton Hicks contractions.
Evaluation
There are no laboratory or radiographic tests to diagnose Braxton Hicks contractions. Evaluation of the presence of Braxton Hicks contractions is based on an assessment of the pregnant woman's abdomen, specifically palpating the contractions.
Treatment / Management
By the midpoint of pregnancy, the woman and provider should discuss what the woman may experience during the remainder of the pregnancy. Braxton Hicks contractions are one of the normal events a woman may experience. Teaching her about Braxton Hicks contractions will help her to be informed and to decrease her anxiety if they occur.[10][11][12]
There is no medical treatment for Braxton Hicks contractions. However, taking action to change the situation that triggered the Braxton Hicks contractions is warranted. Some actions to ease Braxton Hicks contractions include:
Changing position or activity level: if the woman has been very active, lie down; if the woman has been sitting for an extended time, go for a walk.
Relaxing: take a warm bath, get a massage, read a book, listen to music, or take a nap.
Drinking water to rehydrate.
If these actions do not lessen the Braxton Hicks contractions or if the contractions continue and are becoming more frequent or more intense, the patient's healthcare provider should be contacted.
Also, if any of the following are present the healthcare provider should be contacted immediately:
Vaginal bleeding
Leaking of fluid from the vagina
Strong contractions every 5-minutes for an hour
Contractions that the woman is unable to "walk through"
A noticeable change in fetal movement, or if there are less than ten movements every 2 hours.
Differential Diagnosis
Amenorrhea
Ascites
Full bladder
Hematometra
Nausea
Ovarian cysts
Pseudocyesis
Uterine fibroids
Vomiting
Pearls and Other Issues
In addition to Braxton Hicks contractions, there are other causes of abdominal pain during pregnancy. Some normal reasons for abdominal pain during pregnancy, in addition to Braxton Hicks contractions and true labor contractions, include:
Round ligament pain or a sharp, jabbing feeling felt in the lower abdomen or groin area on one or both sides.

Higher levels of progesterone can cause excess gas during pregnancy.
Constipation may be a source of abdominal pain.
Circumstances in which abdominal pain is a sign of a serious condition that requires immediate medical attention include:
Ectopic pregnancy.
Placental abruption. A key symptom of placental abruption is intense and constant pain that causes the uterus to become hard for an extended period without relief.
Urinary tract infection symptoms include pain and discomfort in the lower abdomen as well as burning with urination.
Preeclampsia is a condition of pregnancy occurring after 20-weeks gestation and characterized by high blood pressure and protein in the urine. Upper abdominal pain, usually under the ribs on the right side, can be present in preeclampsia.
If a woman is unsure if she is experiencing Braxton Hicks contractions or another condition, a discussion with a healthcare provider is needed.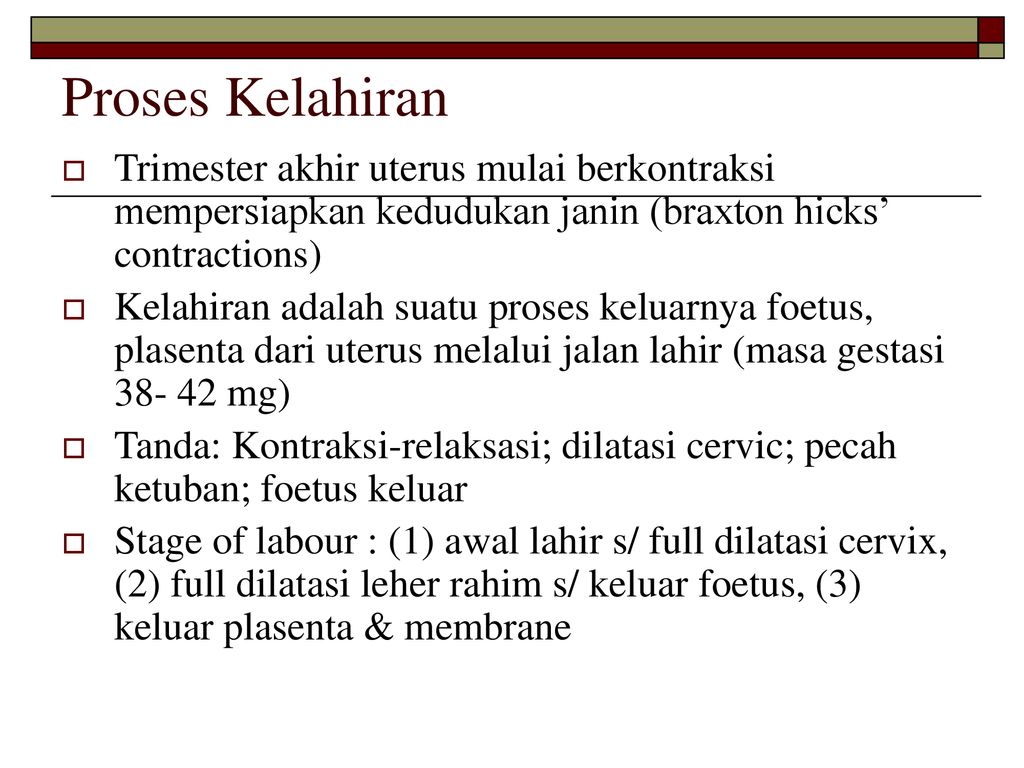 The healthcare provider may recommend a visit to the office setting or labor and delivery for an examination by a healthcare professional to determine the cause of the abdominal pain.
The healthcare provider may recommend a visit to the office setting or labor and delivery for an examination by a healthcare professional to determine the cause of the abdominal pain.
Enhancing Healthcare Team Outcomes
Braxton hicks contractions are fairly common and it is important for the emergency department physician labor & delivery nurse and nurse practitioner to be aware that this is not true labor. If there is any doubt, the obstetrician should be consulted. However, at the same time, the onus is on the healthcare workers to rule out true labor. Other organic disorders like appendicitis, urinary tract infection or cholecystitis must also be ruled out. With the right education, patients with braxton hicks contraction will not needlessly rush to the ED every time they sense a contraction.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Hanghøj S.
 When it hurts I think: Now the baby dies. Risk perceptions of physical activity during pregnancy. Women Birth. 2013 Sep;26(3):190-4. [PubMed: 23711581]
When it hurts I think: Now the baby dies. Risk perceptions of physical activity during pregnancy. Women Birth. 2013 Sep;26(3):190-4. [PubMed: 23711581]- 2.
MacKinnon K, McIntyre M. From Braxton Hicks to preterm labour: the constitution of risk in pregnancy. Can J Nurs Res. 2006 Jun;38(2):56-72. [PubMed: 16871850]
- 3.
Dunn PM. John Braxton Hicks (1823-97) and painless uterine contractions. Arch Dis Child Fetal Neonatal Ed. 1999 Sep;81(2):F157-8. [PMC free article: PMC1720982] [PubMed: 10448189]
- 4.
Lockwood CJ. The diagnosis of preterm labor and the prediction of preterm delivery. Clin Obstet Gynecol. 1995 Dec;38(4):675-87. [PubMed: 8616965]
- 5.
Arduini D, Rizzo G, Rinaldo D, Capponi A, Fittipaldi G, Giannini F, Romanini C. Effects of Braxton-Hicks contractions on fetal heart rate variations in normal and growth-retarded fetuses. Gynecol Obstet Invest. 1994;38(3):177-82. [PubMed: 8001871]
- 6.

Kofinas AD, Simon NV, Clay D, King K. Functional asymmetry of the human myometrium documented by color and pulsed-wave Doppler ultrasonographic evaluation of uterine arcuate arteries during Braxton Hicks contractions. Am J Obstet Gynecol. 1993 Jan;168(1 Pt 1):184-8. [PubMed: 8420324]
- 7.
Lockwood CJ, Dudenhausen JW. New approaches to the prediction of preterm delivery. J Perinat Med. 1993;21(6):441-52. [PubMed: 8006770]
- 8.
Rhoads GG, McNellis DC, Kessel SS. Home monitoring of uterine contractility. Summary of a workshop sponsored by the National Institute of Child Health and Human Development and the Bureau of Maternal and Child Health and Resources Development, Bethesda, Maryland, March 29 and 30, 1989. Am J Obstet Gynecol. 1991 Jul;165(1):2-6. [PubMed: 1677235]
- 9.
Oosterhof H, Dijkstra K, Aarnoudse JG. Fetal Doppler velocimetry in the internal carotid and umbilical artery during Braxton Hicks' contractions.
 Early Hum Dev. 1992 Aug;30(1):33-40. [PubMed: 1396288]
Early Hum Dev. 1992 Aug;30(1):33-40. [PubMed: 1396288]- 10.
Oosterhof H, Dijkstra K, Aarnoudse JG. Uteroplacental Doppler velocimetry during Braxton Hicks' contractions. Gynecol Obstet Invest. 1992;34(3):155-8. [PubMed: 1427416]
- 11.
Bower S, Campbell S, Vyas S, McGirr C. Braxton-Hicks contractions can alter uteroplacental perfusion. Ultrasound Obstet Gynecol. 1991 Jan 01;1(1):46-9. [PubMed: 12797102]
- 12.
Hill WC, Lambertz EL. Let's get rid of the term "Braxton Hicks contractions". Obstet Gynecol. 1990 Apr;75(4):709-10. [PubMed: 2314790]
Braxton-Hicks contractions or false labor contractions are irregular contractions and relaxation of the muscles of the uterus as a way of preparing for true labor. They are thought to start around 6 weeks of gestation but are not usually felt until the 2nd or 3rd trimester.
False contractions are a normal part of pregnancy. They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves.
They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves.
They are also irregular in duration and intensity, occur infrequently, are unpredictable and not rhythmic, and are more uncomfortable than painful.
Braxton Hicks contractions tend to increase in frequency and intensity towards the end of pregnancy. Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Braxton Hicks contractions occur when the muscle fibers of the uterus contract and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are circumstances that can cause them:
- when the woman is very active,
- when the bladder is full,
- after sexual activity,
- when the woman is dehydrated.
Common among all these circumstances is the potential stress on the fetus and the need for increased blood flow to the placenta to provide oxygen to the fetus.
- Change position or activity level: if you were very active, lie down; if you have been sitting for a long time, go for a walk.
- Relax: take a warm bath, massage, read a book, listen to music or take a nap.
If you have Braxton Hicks contractions or if they continue and become more frequent and intense, you should see your doctor.
When assessing for Braxton Hicks contractions, there are a few key questions to ask yourself. We have prepared a table for you with questions, the answers to which will help you understand what kind of contractions you have:
| Braxton Higgs contractions | Real labor pains | |
|---|---|---|
| How often do contractions occur? | Irregular and do not increase over time. | Occurs at regular intervals and gets stronger over time. |
| How long do contractions last? | Unpredictable. They can last less than 30 seconds or up to 2 minutes. | Lasts 30 to 90 seconds and gets longer over time. |
| How strong are the contractions? | Usually weak and either stay the same or get weaker and then disappear. | Increase over time. |
| Where do contractions feel? | Often only felt in the front of the abdomen or in one specific area. | Begin in the middle of the back and wrap around the belly towards the midline. |
| Do abbreviations change with movement? | May stop if activity level changes or if woman's position changes. | Continue and may even get worse with movement or change of position. |
Back to the list of articles
false or real / “Waiting for a baby”
February
How to distinguish them from real contractions, and why they are needed, we will try to find out.
The phenomenon of temporary contractions was first described by the English doctor John Braxton Hicks. That is why they are called - Braxton Hicks contractions or false, training contractions, precursor contractions. In his scientific work of 1872, he argued that these contractions are short-term (from half a minute to 2 minutes) contractions of the muscles of the uterus, which are felt by a pregnant woman as an increase in the tone of the uterus. They appear after the 20th week of pregnancy. And during the day they happen often, but the expectant mother in the daytime may not even notice them. However, as time goes on, they intensify, becoming more and more obvious.
That is why they are called - Braxton Hicks contractions or false, training contractions, precursor contractions. In his scientific work of 1872, he argued that these contractions are short-term (from half a minute to 2 minutes) contractions of the muscles of the uterus, which are felt by a pregnant woman as an increase in the tone of the uterus. They appear after the 20th week of pregnancy. And during the day they happen often, but the expectant mother in the daytime may not even notice them. However, as time goes on, they intensify, becoming more and more obvious.
WHAT DO YOU NEED FALSE BROUGHT
The uterus is a muscular organ. And like any muscle that has to perform the work allotted to it in the body, it needs training. After all, if she hangs for all forty weeks like a bag, she will not cope with the load in childbirth. Thus, the purpose of training or false contractions is to prepare the uterus and cervix for childbirth. That is why one of the names of training bouts is contractions harbingers - harbingers of an approaching birth.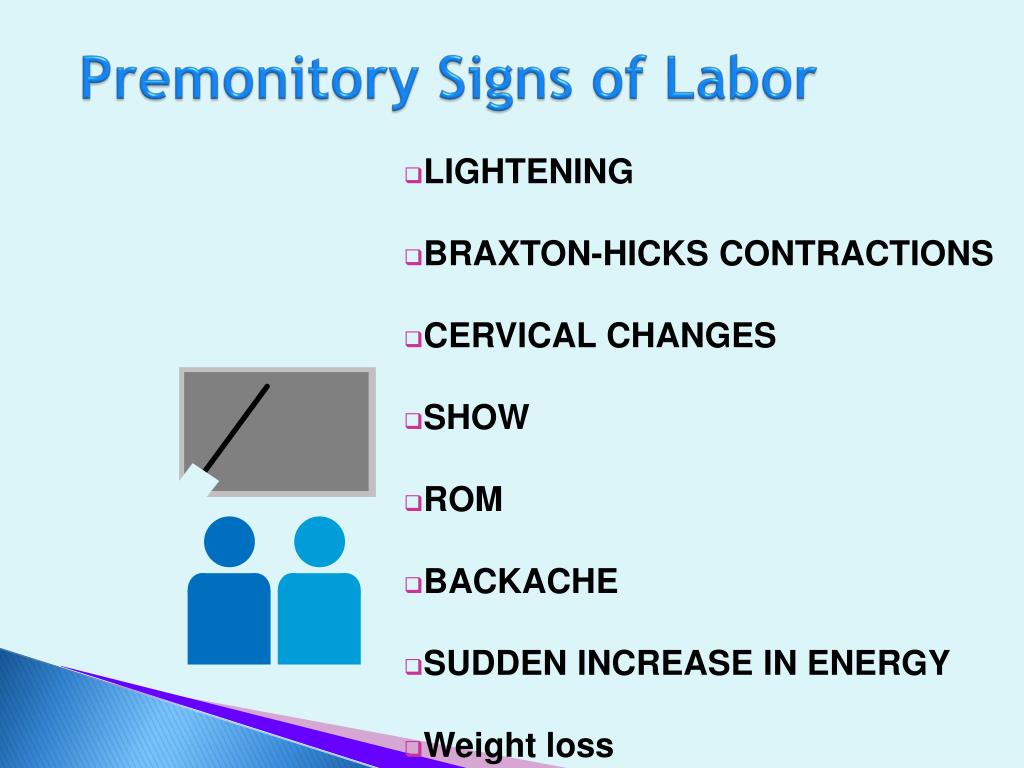
ARE FALSE PARTS PAINFUL?
As a rule, false contractions are painless, but with increasing duration they become more noticeable and bring more discomfort. However, in all women, they manifest themselves in different ways, someone does not feel them at all, and someone does not sleep at night, tossing and turning and trying to find a comfortable position for sleeping. It all depends on the pain threshold. The main thing in this situation is to stop being nervous about this and calm yourself with the thought that such training is necessary for the most important upcoming event - the birth of your crumbs. And to calm down a little and sleep better, ask your doctor to prescribe a sedative for you and get a special pillow for expectant and nursing mothers. With her, falling asleep and experiencing the discomfort of the last weeks of pregnancy will be much easier!
HOW TO LIVE WITH FREQUENT PARTS
Some expectant mothers complain that their Braxton Hicks contractions are frequent and cause significant discomfort, even when they are doing housework or other light physical activity.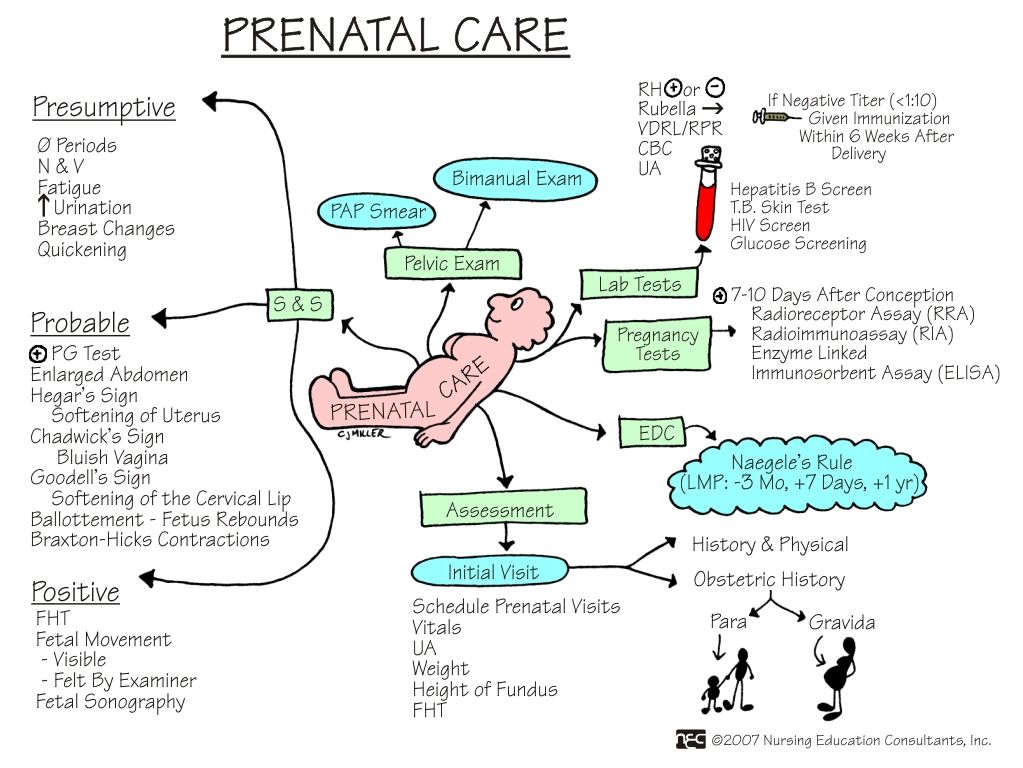 In such a situation, obstetricians are advised to lie down or vice versa, take an easy walk, in any case, change the type of activity. If training contractions bother you a lot, it is recommended to drink a glass of water, juice or herbal tea, calm down and get some rest. Ask someone close to give you a massage. Lie in silence. And to also benefit from training fights, try doing breathing exercises: practice breathing techniques in childbirth in practice.
In such a situation, obstetricians are advised to lie down or vice versa, take an easy walk, in any case, change the type of activity. If training contractions bother you a lot, it is recommended to drink a glass of water, juice or herbal tea, calm down and get some rest. Ask someone close to give you a massage. Lie in silence. And to also benefit from training fights, try doing breathing exercises: practice breathing techniques in childbirth in practice.
HOW TO DIFFERENTIATE TRAINING FROM LIVING
The most important thing to understand is that real contractions are much more painful than Braxton Hicks contractions. You will understand it right away. In addition, the contractions that bring you closer to childbirth are more regular. The contractions start in the lower back, spread to the front of the abdomen, and occur every 10 minutes (or more than 5 contractions per hour). Then they occur with an interval of about 30-70 seconds and over time the intervals between them are reduced. Some women describe the sensations of labor pains as severe menstrual cramps, or sensations during diarrhea, when the pain rolls in waves in the abdomen. These contractions, unlike false ones, continue even after a change of position and when walking, constantly intensifying. As soon as you feel all these symptoms, call your obstetrician-gynecologist - hour X has arrived. If in doubt, also do not be afraid to disturb the doctor. The doctor will ask you a few questions that will help him determine the type of contractions and eliminate all your doubts and worries. After all, it is always better to consult a doctor and trust his professional experience.
Some women describe the sensations of labor pains as severe menstrual cramps, or sensations during diarrhea, when the pain rolls in waves in the abdomen. These contractions, unlike false ones, continue even after a change of position and when walking, constantly intensifying. As soon as you feel all these symptoms, call your obstetrician-gynecologist - hour X has arrived. If in doubt, also do not be afraid to disturb the doctor. The doctor will ask you a few questions that will help him determine the type of contractions and eliminate all your doubts and worries. After all, it is always better to consult a doctor and trust his professional experience.
You should seek help if:
• you have more than four contractions an hour and they happen regularly
• contractions are accompanied by pain in the lower spine
• contractions are accompanied by watery or bloody vaginal discharge
• the contractions are so strong that it is very difficult for you to endure them
• there is a marked change in the child's movement, or less than 10 movements every 2 hours
• you think your waters have started to break
Alla Misyutina, Consultant Physician, Independent Laboratory INVITRO
Dear women, during labor, the body needs a lot of oxygen, so proper breathing is very important. A large influx of oxygen into the blood of mother and baby alleviates the condition of the crumbs, which during childbirth experiences oxygen starvation. Special breathing techniques help to properly open the birth canal and make contractions and attempts as effective as possible.
A large influx of oxygen into the blood of mother and baby alleviates the condition of the crumbs, which during childbirth experiences oxygen starvation. Special breathing techniques help to properly open the birth canal and make contractions and attempts as effective as possible.
Different types of breathing should be used at different stages of labor.
• During "false" contractions, breathing should be deep and slow. During the period when the contractions become more intense, it is necessary to use "pain-relieving breathing". This breathing is slow, deep, the inhalation is done through the nose, it should be longer than the exhalation through the mouth. More details: inhale is done at the expense of 1-2-3-4, and exhale - at the expense of 1-2-3-4-5-6. With the help of such breathing: mom relaxes, distracts from pain, focuses on the score; the baby receives as much as possible, so he needs oxygen.
• In breaks from contractions, you need to rest and breathe evenly without any effort, so that you can then easily follow the doctor's recommendations.
• During attempts, you need to exhale all the air from the lungs, then take a deep breath and push for up to 6-9 seconds. Quickly exhale all the air, quickly take a deep breath and again hold your breath for 6-9 seconds, and so on - about three times per attempt.
• In breaks from attempts to rest and breathe deeply, evenly and relaxed.
• It is very important to only push on the perineum and never push on the head. In this case, all efforts are wasted and will appear in the form of burst vessels in the eyes and on the face.
• In the period after the birth of the head, it is necessary to stop pushing and breathing shallowly, some call this breathing “dog-like”, deep breathing can harm both mom and baby. Then everything goes on as usual, the main thing is to obey the doctor.
• After the baby was born, within half an hour the last stage of labor begins - the birth of the placenta. Special breathing is no longer required, at the doctor's command, push a little into the perineum and EVERYTHING! Dear women, pain during childbirth is good, it means that your baby will be born soon. There is no need to resist the pain, this is a mistake that brings a woman and a child nothing but fatigue. On the contrary, it is necessary to concentrate and help in every possible way to give birth to a healthy baby.
There is no need to resist the pain, this is a mistake that brings a woman and a child nothing but fatigue. On the contrary, it is necessary to concentrate and help in every possible way to give birth to a healthy baby.
BIRTH AGAIN
So, you have decided that this is no longer a “teaching”, but the beginning of childbirth. In addition to contractions, the onset of labor can be indicated by the outflow of amniotic fluid and the passage of a mucous plug that closes the lumen of the cervix. The mucous plug can also come off 2-3 days before delivery. However, her departure does not always mean that it is time to go to the hospital. During pregnancy, the cervix is tightly closed. With the onset of labor pains, its opening begins: the cervix of the uterus gradually expands to 10-12 cm in diameter (full disclosure). The birth canal is preparing to "release" the child from the womb. Intrauterine pressure increases during contractions as the uterus shrinks. And in the end, this leads to rupture of the fetal bladder and the outflow of part of the amniotic fluid.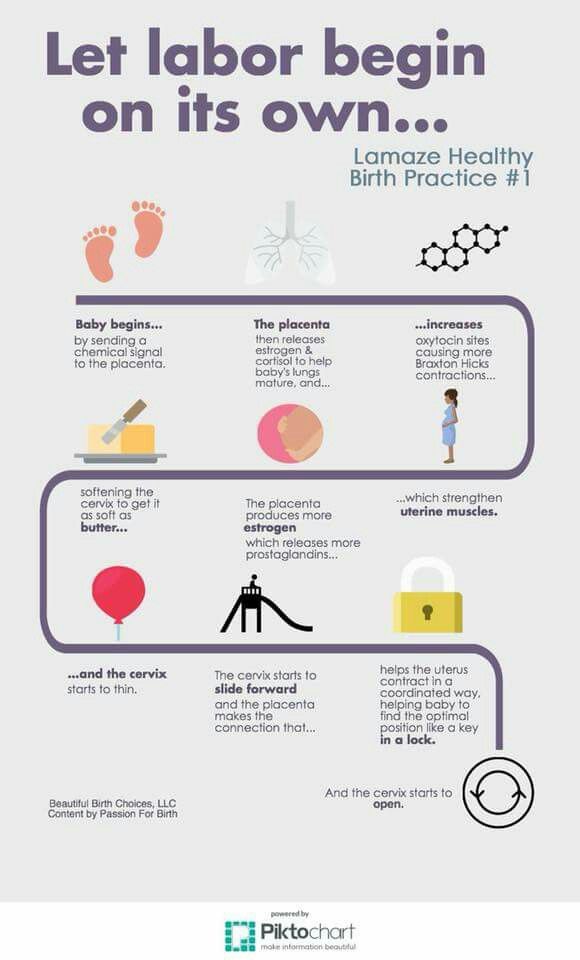
The first, preparatory, period of labor for women giving birth for the first time takes an average of 12 hours, and 2-4 hours less for those who have second births. At the beginning of the second stage of labor, contractions join the contractions - contractions of the muscles of the abdominal wall and diaphragm. In addition to the fact that different muscle groups are involved in contractions and attempts, they have one more important difference: contractions are an involuntary and uncontrollable phenomenon, neither their strength nor frequency depend on the woman in labor, while attempts to a certain extent obey her will , it can delay or strengthen them. Therefore, at this stage of childbirth, a lot depends on the expectant mother and her ability to quickly and correctly follow the commands of the obstetrician taking delivery. And most importantly - to tune in correctly and not allow panic and thoughts about something bad. Obstetricians and gynecologists recommend that mothers perceive childbirth as a holiday, a baby's birthday.