How to treat hip dysplasia in babies
Developmental Dysplasia of the Hip (for Parents)
What Is Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip (DDH) is a problem with the way a baby's hip joint forms. Sometimes the condition starts before the baby is born, and sometimes it happens after birth, as the child grows. It can affect one hip or both.
Most infants treated for DDH develop into active, healthy kids and have no hip problems.
What Happens in a Hip With Developmental Dysplasia?
The hip joint is a ball and socket joint. The top part of the thighbone (the ball part of the hip) sits inside a socket that's part of the pelvic bone. The ball moves around in different directions, but always stays inside the socket. This lets us move our hips front, back, and side to side. It also supports our body weight for walking and running.
In DDH, the hip does not form well. The ball part of the joint may be completely, or partly, out of the socket. Sometimes the ball part may slide in and out of the socket. Often, the socket is shallow. If this is not fixed, the hip joint will not grow well. This can lead to pain with walking and hip arthritis at a young age.
What Are the Signs & Symptoms of Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip doesn't cause pain in babies, so can be hard to notice. Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Parents could notice:
- The baby's hips make a popping or clicking that is heard or felt.
- The baby's legs are not the same length.
- One hip or leg doesn't move the same as the other side.
- The skin folds under the buttocks or on the thighs don't line up.
- The child has a limp when starting to walk.
Babies with any of these signs should see a doctor to have their hips checked. Finding and treating DDH early usually means there's a better chance for a baby's hips to develop normally.
What Is Hip Laxity?
Many babies are born with hips that feel loose when moved around. This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
A baby's whose hip ligaments are still loose after 6 weeks might need treatment. So follow-up doctor visits for babies with hip laxity are important.
Who Gets Developmental Dysplasia of the Hip?
Any baby can have DDH. But there's a higher chance of being born with it in babies who:
- are girls
- are first-born
- were breech babies (in the womb buttocks-down instead of head-down), especially during the third trimester of pregnancy
- have a family member with the condition, such as parent or sibling
Rarely, a baby isn't born with DDH, but develops it after birth. To prevent DDH in babies who aren't born with it, don't swaddle a newborn's hips or legs tightly together. Always make sure a baby's legs have plenty of wiggle room.
Always make sure a baby's legs have plenty of wiggle room.
How Is Developmental Dysplasia of the Hip Diagnosed?
Doctors find most cases of DDH during well-child exams. If a baby has signs of DDH or has a higher risk for it, the doctor will order tests.
Two tests help doctors check for DDH:
- An ultrasound uses sound waves to make pictures of the baby's hip joint. This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray.
- An X-ray works best in babies older than 4–6 months. At that age, their bones have formed enough to see them on an X-ray.
How Is Developmental Dysplasia of the Hip Treated?
A pediatric orthopedic surgeon (a specialist in children's bone conditions) cares for babies and kids with DDH. The goal of care is to get the ball of the hip in the socket and keep it there, so the joint can grow normally.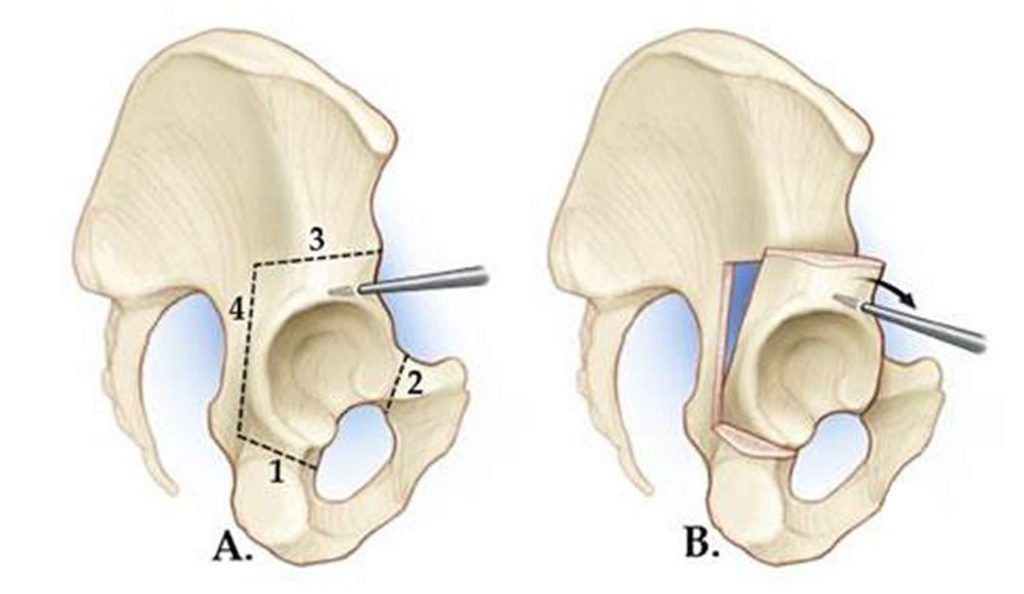
The orthopedic surgeon chooses the treatment based on the child's age. Options include:
- bracing
- a closed reduction and casting
- an open reduction (surgery) and casting
A brace or cast will hold the hip in place and will be on both sides, even if only one hip is affected.
Bracing
Treatment for babies younger than 6 months old usually is a brace. The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
Treatment with the Pavlik harness often lasts about 6–12 weeks. While wearing the harness, the baby has a checkup every 1–3 weeks with hip ultrasounds and exams. During the visit, the medical team can adjust the harness if needed.
The harness (brace) usually works well to keep the hips in position. Most babies won't need other treatment.
Rarely, the harness isn't able to keep the ball of the hip in the socket. Then, doctors might do either:
Then, doctors might do either:
- a closed reduction (manually moving the ball back into the socket) and casting
- an open reduction (surgery) and casting
Closed Reduction and Casting
A child might need a closed reduction if:
- The harness was not successful at keeping the ball of the hip in the socket.
- A baby starts care after age 6 months.
For a closed reduction, the baby gets medicine (general anesthesia) to sleep through the procedure and not feel pain. The surgeon:
- Injects contrast dye into the joint to see the cartilagepart of the ball.
- Moves the baby's thighbone so that the ball of the joint goes back into place in the socket.
- Puts on a hip spica cast to hold the hip in place. The baby wears the cast for 2–4 months.
Sometimes, the orthopedic surgeon also loosens the tight muscle in the groin during the closed reduction.
Open Reduction (Surgery) and Casting
A child might need surgery (an open reduction) if:
- The closed reduction was not successful at keeping the ball of the hip in the socket.

- The child is older than 18 months when starting treatment.
During an open reduction, the child is asleep under anesthesia. The surgeon:
- Makes a cut through the skin.
- Moves muscles out of the way to see the hip joint directly.
- Puts the ball back into place.
- Closes the surgical cut with stitches placed under the skin. These won't need to be removed.
- Puts on a hip spica cast to hold the hip in place. The child wears the cast for 6–12 weeks.
Sometimes, the orthopedic surgeon also does a surgery on the pelvic bone to deepen a very shallow hip socket, especially for a child older than 18 months.
What Else Should I Know?
Kids will have regular checkups with their orthopedic specialist until they're 16–18 years old and done growing. These help make sure the hip develops well.
Treatment for Developmental Dysplasia of the Hip or DDH
By
; John S.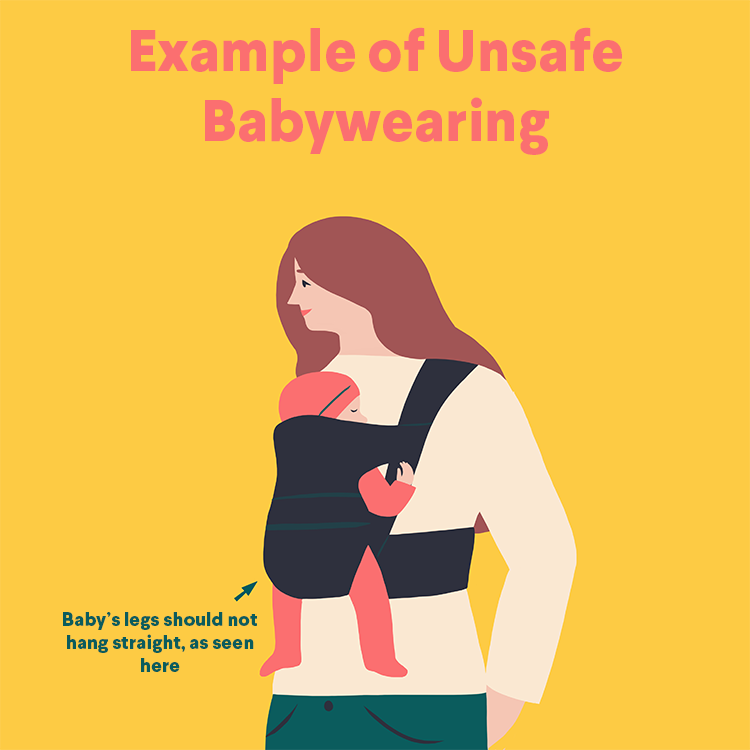 Blanco, MD; Emily R. Dodwell, MD, MPH, FRCSC; Shevaun Mackie Doyle, MD; David M. Scher, MD; Ernest L. Sink, MD; Roger F. Widmann, MD
Blanco, MD; Emily R. Dodwell, MD, MPH, FRCSC; Shevaun Mackie Doyle, MD; David M. Scher, MD; Ernest L. Sink, MD; Roger F. Widmann, MD
What is developmental dysplasia of the hip?
Developmental dysplasia of the hip (DDH), also known as developmental pediatric dysplasia of the hip or hip dysplasia, describes a spectrum of hip joint abnormalities that vary in severity from a complete dislocation of the hip joint to mild irregularities of the located hip joint.
Hip dysplasia may develop in a baby around the time of birth or during early childhood. Although it is commonly diagnosed in babies and young children, DDH also affects adolescents and adults. This can usually be attributed, however, to milder cases of DDH that are difficult in diagnose and may be untreated as a child.
Illustration of the femur and acetabulum.
meeting in a healthy hip joint
In the healthy hip joint, the upper end of the femur (thighbone) meets the acetabulum to fit together like a ball and socket, in which the ball rotates freely in the socket. Cartilage, a smooth protective tissue, lines the bones and reduces friction between the surfaces during movement.
In DDH, however, there is an abnormal relationship between the components of the hip, and often the hip socket is underdeveloped and does not support the femoral head (ball).
The conditions encompassed by the term hip dysplasia include:
- dislocated hip: where there is no contact between the cartilage on the ball and the cartilage on the socket
- dislocatable hip: where the ball easily pops in and out of the socket
- subluxatable hip: where the cartilage of the ball and the socket are touching, but the ball is not properly seated in the socket
- dysplastic hip: where the hip socket or acetabulum is underdeveloped or deficient to support the ball (more common in older adolescents and adults than in pediatrict patients)
Anterior-to-posterior (front-to-back) preoperative X-ray of a dislocated right hip in toddler (shown at left).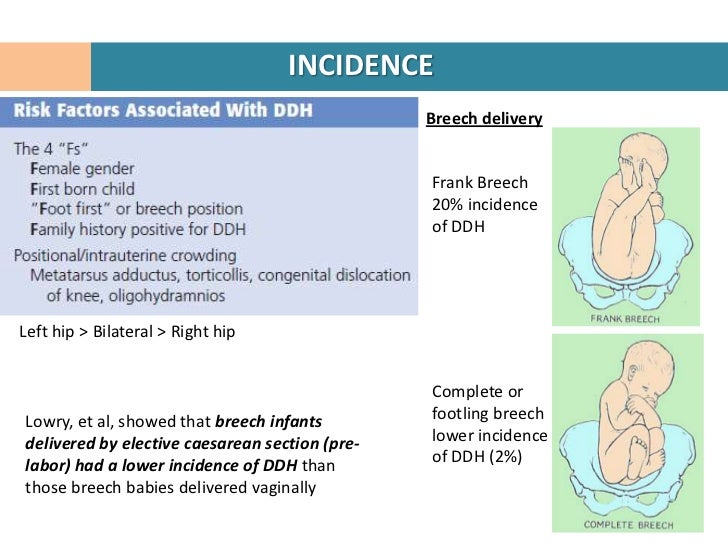
In children, hip dysplasia more frequently affects the left hip than the right. About 80% of cases follow this pattern. The condition can, however, be present in both hips.
Can hip dysplasia correct itself?
Some mild forms of developmental hip dysplasia in children – particularly those in infants – can correct on their own with time.
Who is at risk for hip dysplasia?
Hip dysplasia is much more common in girls than in boys, and it tends to run in families. Even among children who have no hereditary link, there is a greater risk in all first-born children.
What causes hip dysplasia?
Genetics plays a strong role, but other influences during pregnancy and birth – such as congenital conditions caused by the fetus being in a uterus that is too small – and cases of breech birth can also lead to developmental hip dysplasia.
Family history
The risk of hip dislocation at birth is approximately one in 1,000. If a parent experienced hip dysplasia during childhood, the risk of his or her own child developing this risk increases by 12% compared to a parent with no history of the condition.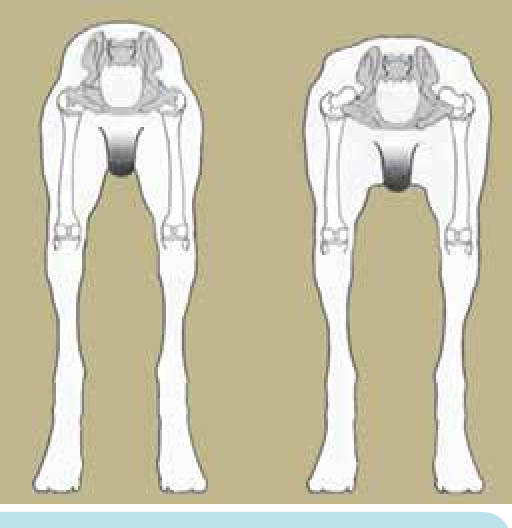 A child whose sibling has hip dysplasia will have a 6% higher chance of developing the condition.
A child whose sibling has hip dysplasia will have a 6% higher chance of developing the condition.
Molding abnormalities in the uterus
Head tilt (torticollis) and the turning in of the front of the foot (metatarsus adductus) are congenital conditions that often the result of being constrained in a uterus that is too small. These conditions alert medical professionals to be on the lookout for the presence of hip dysplasia, which can also be caused by such constraint.
Breech birth
This is when the baby emerges from the birth canal buttocks-first instead of headfirst. A breech-birth child is 10 times more likely to develop hip dysplasia than a child born headfirst.
What are the signs and symptoms of developmental hip dysplasia in children?
When present at birth, the abnormality may be detected during a routine physical examination of the newborn baby. Other signs include a leg length discrepancy, restricted range of motion in the hip, or a limp or waddle in walking in toddlers.
During a routine examination of a newborn, the physician gently flexes the child's hips in different directions. If the hip is dislocated or can be easily dislocated or subluxated (partially dislocated), the doctor may feel a "clunk" as the hip moves out of alignment. In a smaller percentage of cases, the problem does not become apparent until later in infancy or early childhood. Later diagnosis of hip dysplasia may be detected during routine examinations of hip stability in the pediatrician's office.
Additional signs that may bring undiagnosed developmental hip dysplasia to the attention of parent and physician include:
- a limb length discrepancy (one leg shorter than the other) on the affected side
- a limp
- a waddling gait (indicating both legs are affected)
- restricted range of motion of the hip joint (that initially may be detected by the caregiver when changing a diaper)
To confirm a diagnosis of developmental hip dysplasia in children up to four to six months of age, an orthopedist uses ultrasound imaging.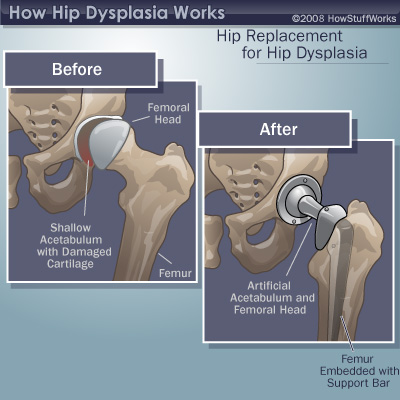 This technology offers a significant advantage over conventional a X-ray because images may be taken while the hip is in motion. "This is a very accurate and safe diagnostic tool since there is no radiation," according to Roger F. Widmann, MD, Chief of Pediatric Orthopaedic Surgery at HSS. In children older than six months, X-rays, which show bone detail better, are used to confirm the diagnosis.
This technology offers a significant advantage over conventional a X-ray because images may be taken while the hip is in motion. "This is a very accurate and safe diagnostic tool since there is no radiation," according to Roger F. Widmann, MD, Chief of Pediatric Orthopaedic Surgery at HSS. In children older than six months, X-rays, which show bone detail better, are used to confirm the diagnosis.
How is hip dysplasia treated?
Early intervention is essential to ensure the bones that make up the hip joint develop properly. Incorrect growth in either the ball or socket can cause formation problems in the other. The goal is to achieve and maintain joint congruity. "The acetabulum and the femoral head are dependent on one another for normal growth and development," explains Dr. Widmann. "If the ball does not fit tightly into the socket, providing a specific growth stimulus, the socket may become too flat and unable to accommodate a sphere. In turn, without proper contact with the acetabulum, the femoral head and neck will not grow normally. "
"
Does hip dysplasia always require surgery?
When treatment is required, the first choice for children under six months old is nonsurgical, using a Pavlik harness. In the minority of cases where this does not work, and in children not diagnosed until after six months of age, surgery may be required.
Pavlik harness
The Pavlik harness is a soft brace that gently redirects the head of the femur into the depth of the socket or acetabulum, which stimulates normal development of the joint.
Usually, the harness generally is used for three months. Initially, the child will wear the harness full-time and, as the hip position improves and stability is achieved, this can be reduced to part-time use. Treatment with the Pavlik harness is successful in about 85% of dislocated hips in children under six months of age.
Photo of an infant in a Pavlik harness.
Unfortunately, the Pavlik harness is not a good treatment option for older children because the hip has become more fixed in the dislocated position and is more difficult to realign.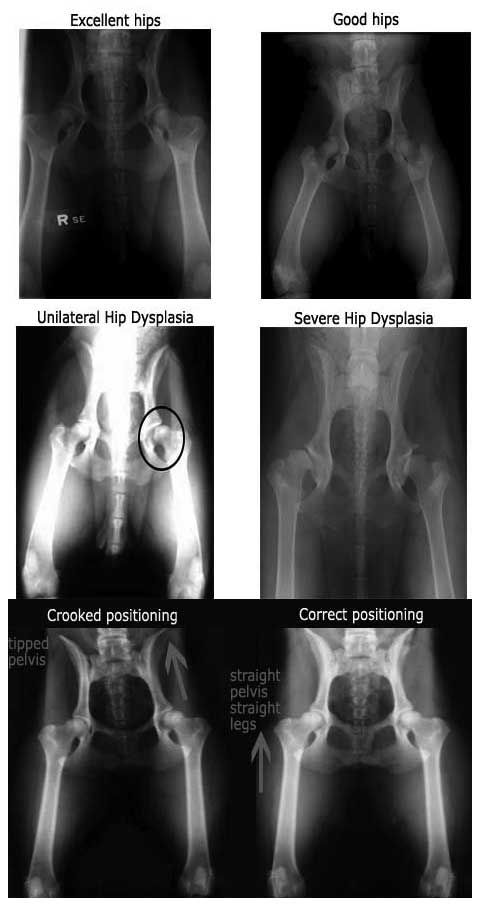
Reduction
For the small number of patients in whom treatment with the Pavlik harness is not successful, and for children in whom the diagnosis is not made until after they are six months old, the orthopedist may recommend either a closed reduction or open reduction surgery. Reduction is a procedure in which the bones are realigned or put back into place to optimize hip joint congruity. Reduction procedures are performed by pediatric orthopedists with specialized experience in the treatment of hip dysplasia. There are two types of reduction:
- Closed reduction: Although no incisions are made in this procedure, it does require the child to be placed under general anesthesia. During a closed reduction procedure, the physician uses radiography to observe the hip and then gently manipulates it into proper alignment, without making any incisions. A cast is then applied to hold the hip in place for up to three months.
- Open reduction: In an open reduction, also performed under general anesthesia, a surgical incision is needed to remove any tissue that is keeping the femoral head from proper alignment in the socket.
 A cast is then applied as well.
A cast is then applied as well.
Arthrogram image of dislocated hip in the operating room.
MRI image of relocated (anatomically aligned) hip.
Closed reduction and spica cast
Following closed reduction of the hip, the patient is placed into a spica body cast for 12 weeks to maintain proper alignment of the hip ball and socket. At HSS, we use cross-sectional, 3D MRI imaging of the hip after closed reduction in order to confirm appropriate location of the hip and confirm hip joint congruency. HSS prefers to use MRI maging, rather than X-rays or CT scans, since radiation is not involved.
Photo of an infant in a spica cast.
Open reduction surgery for hip dysplasia
Treatment by open reduction is generally reserved for children greater than 10 months of age who have new diagnosis of a dysplastic hip, or in cases in which a prior, closed reduction of the hip was unsuccessful.
In this procedure, the surgeon makes an incision, removes any obstacles to anatomic realignment of the hip (such as adjusting tight muscles or other soft tissue) and relocates the femoral head into the acetabulum. The surgeon may also need to restore normal anatomy by performing a hip osteotomy, a procedure in which cuts are made to the femur and/or the acetabulum in order to adjust the angles at which the bones meet and optimize joint congruity. The need for a femoral or acetabular osteotomy increases with the age at which diagnosis is made. It is usually required to correct abnormal development of the bones in any child over age three or four.
Preoperative view of a right hip dislocation, where
the right leg appears shorter than the left.
Anterior-to-posterior (front-to-back) X-ray image, six
months after open reduction with a realigned right hip.
All reduction procedures, including those that involve an osteotomy, are done on an inpatient basis and require the use of general anesthesia.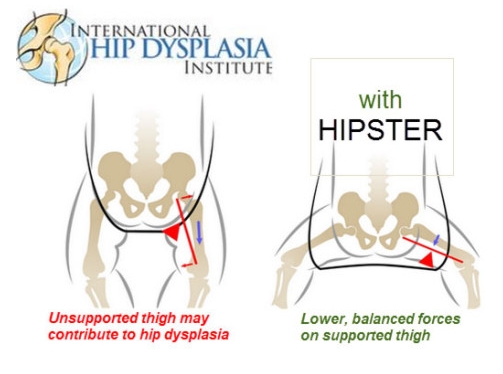 Children who undergo open reduction wear a cast for a period of six to eight weeks. Once the cast is removed, he or she usually continues to wear a brace at night until the orthopedic surgeon determines that the hip joint is developing normally.
Children who undergo open reduction wear a cast for a period of six to eight weeks. Once the cast is removed, he or she usually continues to wear a brace at night until the orthopedic surgeon determines that the hip joint is developing normally.
In some patients who have an open or closed reduction and/or a femoral osteotomy, an osteotomy of the pelvis may also be required to adjust the angle of the acetabulum. In younger patients, the procedure often used is the Pemberton or Dega osteotomy, in which the bony and cartilage roof of the hip is reoriented into normal alignment.
Anterior-to-posterior (front-to-back) X-ray showing residual
acetabular dysplasia on the right hip (shown at left).
Immediate postoperative X-ray after Dega pelvic osteotomy.
X-ray: Pelvis and hip 18 months after Dega pelvic osteotomy.
What are the risks of DDH treatments?
The risks associated with surgery – bleeding, infection and those associated with anesthesia – are minimal. Pediatric orthopedists take special care to avoid a condition called avascular necrosis (also known as AVN or osteonecrosis), in which the bones of the hip joint do not receive enough blood. This can be caused if the femoral head (the ball of the hip joint) is put back into the acetabulum (socket) with unnecessary pressure, and so minimal pressure is used. Avascular necrosis can result in abnormal growth of the bone.
Pediatric orthopedists take special care to avoid a condition called avascular necrosis (also known as AVN or osteonecrosis), in which the bones of the hip joint do not receive enough blood. This can be caused if the femoral head (the ball of the hip joint) is put back into the acetabulum (socket) with unnecessary pressure, and so minimal pressure is used. Avascular necrosis can result in abnormal growth of the bone.
Regarding the safety of these procedures, Dr. Widmann says, "What I usually tell parents is that the primary risk with a diagnosis of developmental hip dysplasia is not doing anything at all. Untreated, these children face a high risk of developing osteoarthritis as adults, with the associated degenerative changes that cause chronic and progressive pain and stiffness."
Although the numbers are difficult to define, some members of the medical community believe that up to 50% of adults who eventually require hip replacement due to osteoarthritis, have developed the disease as a result of a pediatric hip problem. The majority of those cases are thought to be hip dysplasia.
The majority of those cases are thought to be hip dysplasia.
What kind of outcome can a child with DDH expect?
The earlier the condition is treated, the better the chance of a successful outcome, meaning a hip that appears anatomically normal both during physical examination and on X-ray. Children who are treated for hip dysplasia are examined on regular intervals until they are skeletally mature (when growth is completed), to ensure that normal development continues. In some cases, a dislocated hip that was successfully reduced may still develop dysplasia in later years, requiring additional treatment.
Updated: 3/17/2021
Summary Prepared by Nancy Novick • Diagnostic imaging examinations provided by HSS Radiologists
Authors
John S. Blanco, MD
Associate Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Clinical Orthopedic Surgery, Weill Cornell Medical College
Emily R. Dodwell, MD, MPH, FRCSC
Dodwell, MD, MPH, FRCSC
Associate Attending Pediatric Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Orthopedic Surgery, Weill Cornell Medical College
Shevaun Mackie Doyle, MD
Associate Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Orthopedic Surgery, Weill Cornell Medical College
David M. Scher, MD
Attending Orthopedic Surgeon, Hospital for Special Surgery
Professor, Clinical Orthopedic Surgery, Weill Cornell Medical College
Ernest L. Sink, MD
Chief, Hip Preservation Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Roger F.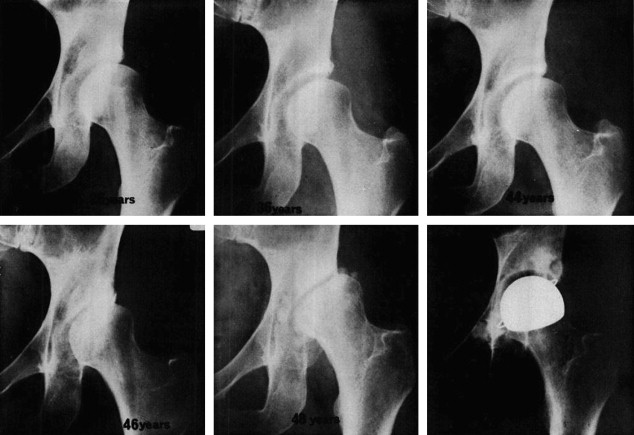 Widmann, MD
Widmann, MD
Chief, Pediatric Orthopedic Surgery, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Related articles
Dysplasia in a child: the main thing is to start treatment on time
Young parents often meet with such a diagnosis in a baby as hip dysplasia. This is a congenital inferiority of the joint, which is due to its underdevelopment and can lead to subluxation or dislocation of the hip.
Traumatologist-orthopedist of the first qualification category of the Chelyabinsk Regional Children's Clinical Hospital Alexander Semenov tells about the signs of dysplasia, methods of treatment and the main mistakes of parents.
- Alexander Vladimirovich, why does dysplasia occur?
- One of the reasons leading to disruption of the normal development of the joint is its abnormal development already in utero. The disease begins to develop at 5-6 weeks of gestation.
Genetic and hormonal factors influence. Hip dysplasia is 10 times more common in children whose parents had signs of congenital hip dislocation. It is worth noting that in girls, hip dysplasia occurs twice as often and is especially difficult.
- Can a woman learn about the disease during pregnancy through ultrasound and avoid its development?
- During ultrasound, as a rule, this diagnosis is not revealed. In this case, nothing depends on the woman. Here the main thing is timely diagnosis in a child and proper treatment.
- What should parents pay attention to first of all?
- For the asymmetry of the folds on the legs and buttocks, during gymnastics - restriction of movement in the joint. Parents often complain that one leg is shorter than the other in a child, but most often this symptom is misinterpreted. Factors such as breech presentation of the fetus, large fetus, pregnancy toxemia should alert a pregnant woman in terms of possible congenital joint pathology in a child. The risk in these cases increases tenfold.
The risk in these cases increases tenfold.
- Is there an asymptomatic course of dysplasia?
- It happens. Sometimes parents cannot suspect dysplasia on their own when there is no restriction of movement in the hip joint. In this case, only a doctor detects the disease. Therefore, in one month, the child must be examined by an orthopedist.
- But orthopedists are not available in all areas of the Chelyabinsk region. What about families from the outback?
- Currently, about 18 orthopedists are being treated in the Chelyabinsk region, two of them are in the regional hospital, three in the region - in Kopeysk, Miass and Zlatoust, about 13 - in the city of Chelyabinsk. The orthopedist must necessarily examine the child within the decreed terms (1 month, 6 months, 12 months), so if there is no doctor in the area, you need to take a referral to our children's regional clinic. We are ready to accept all children from the Chelyabinsk region.
In addition, in some maternity hospitals in the region, a screening ultrasound of the hip joints is performed on the 5-7th day of the newborn to exclude dysplasia. If the disease is detected, then the baby is discharged already with recommendations and a referral to an orthopedist.
- What are the treatments for dysplasia?
- The main principles of treatment are early onset, the use of orthopedic devices for long-term retention of the legs in the position of abduction and flexion, active movements in the hip joint.
The main thing in treatment is gymnastics, which parents should perform with their children. The task of exercise therapy is to strengthen the muscles of the hip joint and organize the child's motor activity, sufficient for full physical development. Usually it includes five types of exercises. In addition, complex treatment should include massage and physiotherapy. In more severe cases (severe dysplasia, subluxation, dislocation of the hip), we use various orthopedic aids - Pavlik's stirrups at an earlier age, spacer splints for older children.
- Where is the child being treated?
- We send patients for treatment at their place of residence. The main responsibility in this case lies with the parents, they must perform a set of exercises daily. And massage and physiotherapy can be obtained in polyclinics at the place of residence.
- Who can massage a child?
- Massage can only be done by a specially trained massage therapist, certified and preferably specialized in baby massage.
- How does swaddling a baby affect treatment?
- Previously, tight swaddling was used, now it has already been abandoned, because in this case the joint is in a non-physiological position. Now experts recommend either wide swaddling or a free position for the legs.
- If a child is prescribed orthopedic products, then his movements are limited for a long time. How will this affect his future development?
- Nothing. The fact is that there is no particular restriction on movement. If parents follow the orthopedic regimen, then in 80% of cases we cancel Pavlikama's stirrups after 3 months. Even if a child wears a spacer splint for six months, this only has a positive effect on the formation of his joints. In the future, this will not affect the overall development of the child.
The fact is that there is no particular restriction on movement. If parents follow the orthopedic regimen, then in 80% of cases we cancel Pavlikama's stirrups after 3 months. Even if a child wears a spacer splint for six months, this only has a positive effect on the formation of his joints. In the future, this will not affect the overall development of the child.
- Is it possible to completely get rid of dysplasia?
- The leading role is played by early recognition of this defect and timely treatment. With timely treatment and compliance with the orthopedic regimen by parents, about 70% of children recover completely, but 30% develop gait disturbance at an older age.
If we talk about congenital dislocation of the hip, then there is a high probability of developing arthrosis of the hip joint in a few years. But still, in most children, the disease goes away without a trace if it is detected in time and treated.
- How many children in the Chelyabinsk region suffer from dysplasia?
- Every day 4-5 people from all over the region come to our regional polyclinic with this diagnosis. Congenital dislocation occurs once or twice a month. Luckily, there are not so many cases. Basically, this happens in remote areas of the Chelyabinsk region, where it is not possible to show the child to an orthopedist in a timely manner.
Congenital dislocation occurs once or twice a month. Luckily, there are not so many cases. Basically, this happens in remote areas of the Chelyabinsk region, where it is not possible to show the child to an orthopedist in a timely manner.
Hip Dysplasia - Family Doctor Clinic.
“Your child has hip dysplasia” - very often this phrase from the mouth of an orthopedic doctor causes a state close to emotional shock in the parents of the baby. But is everything so gloomy and scary, and what kind of pathology is this?
Dysplasia - this term means a violation of the formation of any organ or body system. In this material we will talk about hip dysplasia.
Hip dysplasia is understood as a violation of the formation of the hip joint, which captures all the elements that make up the joint: the bone and cartilage base, the ligamentous-capsular apparatus and the muscle component. This definition is quite broad and includes the physiological immaturity of the hip joint, preluxation, subluxation and dislocation of the hip.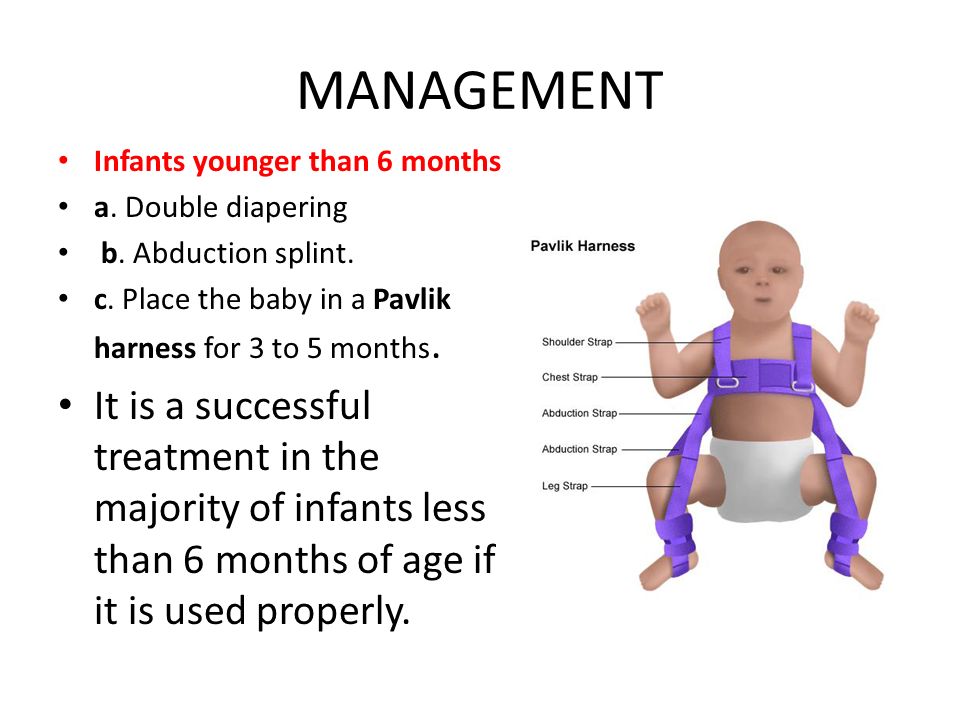
Physiological immaturity consists in the incomplete formation of the joint components without violating the congruence (correct matching) of the articular surfaces of the bones and, as a rule, requires minimal treatment or only dynamic observation, and it is this form of hip joint pathology that is mainly assigned the diagnosis of "dysplasia", although this is not entirely correct. terminologically. With pronounced immaturity of the hip joint, treatment is necessary to create favorable conditions for the proper maturation of the joint components.
Predislocation of the hip is already a pathology of the joint associated with the lack of stability of the femoral head in another component of the hip joint - the acetabulum and already requires close attention. In the absence of adequate treatment, hip predislocation can lead to the development of joint deformity (arthrosis), which leads to pain and impaired joint mobility, and can also lead to hip dislocation after the start of walking.
Dislocation of the hip is the most severe form of the pathology of the development of the hip joint, which consists in the almost complete discrepancy between the articular surfaces of the femoral head and the acetabulum. Such a malformation of the joint requires maximum efforts for a thorough diagnosis and active and prompt treatment. Late diagnosis or inadequate treatment leads to gross impairment of the hip joint mobility and, ultimately, leads to disability.
Now we understand why so much attention is paid to hip dysplasia by pediatricians and orthopedists. Why is it the hip joint that is most susceptible to these misfortunes?
The fact is that the hip joint, due to its anatomical and physiological characteristics, is the most loaded joint in our body, and a failure in one of its constituent components leads to dysfunction of the joint and, ultimately, to a deterioration in the quality of life of the patient. That is why the diagnosis of hip dysplasia can so often be heard from the lips of an orthopedist, although one cannot but recognize the fact of some overdiagnosis of this pathology, but given the severity of the consequences in the absence of treatment, this is still justified.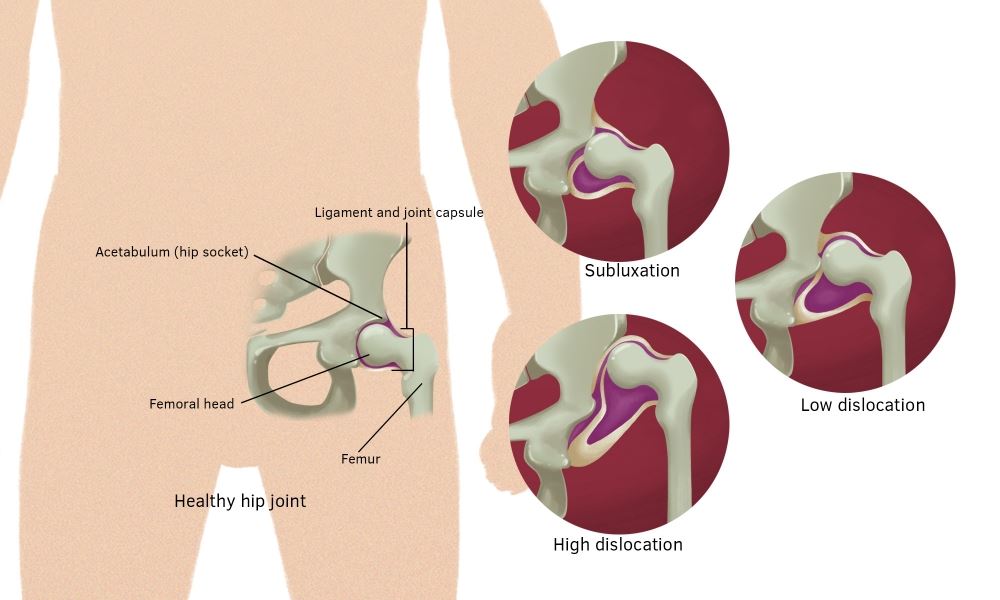
According to statistics, the incidence of hip dysplasia is 4-6 cases per 1000 newborns, in girls it occurs 6-7 times more often. Unilateral lesion predominates over bilateral (more often the left hip joint is affected). There is inheritance from mother to daughter. Quite a lot of factors leading to impaired intrauterine joint formation have been noted, among them are breech presentation of the fetus, narrowness of the uterus, oligohydramnios, toxic and biological (primarily viral diseases of the mother during pregnancy) factors and much more.
When and by what methods can and should hip dysplasia be diagnosed? Can a mother herself suspect the presence of hip dysplasia in a child and, if so, with what methods? The answer to this question depends on the severity of the joint injury. Let's try to answer this question by tying the timing and methods of diagnosis to the age of the baby.
When conducting ultrasound diagnostics during pregnancy, it is possible to diagnose only gross violations - subluxation and dislocation of the hip, that is, those changes in which the articular surface of the femoral head does not correspond to the surface of the acetabulum of the child's pelvis.
In the first 7-10 days of a child's life, an examination can reveal a “click symptom” or “slipping symptom” - dislocation and reduction of the hip in the joint. These symptoms are revealed in a child as follows: in the supine position, the legs are bent at the knee and hip joints at an angle of 90 degrees. The thumbs are located on the inner surface of the child's thighs, the index and middle fingers on the outer. With careful abduction and traction of the hips, the femoral head is set into the acetabulum with a characteristic click.
After the 2nd - 3rd week of a child's life, limitation of hip abduction comes to the fore in the diagnosis of hip dysplasia. To identify it, the legs of the child bent at the knee and hip joints in the supine position are bred without violence. Normally, it is possible to spread the hips to an angle of 85-90 degrees to the surface. With increased muscle tone and spasm of the muscles adducting the thigh, abduction can be limited to an angle of about 70 degrees, but such a restriction of hip abduction can also be caused by impaired joint formation. Limitation of hip abduction on one side in most cases is a sign of pathology from the hip joint.
Limitation of hip abduction on one side in most cases is a sign of pathology from the hip joint.
In favor of the pathology of the hip joint, symptoms such as shortening of one limb, turn of the foot on the side of the lesion outward from the middle position (external rotation of the foot) also speak.
The most widely known in parents (so to speak, "mommy symptom") - the asymmetry of the subgluteal folds - is not absolute and can be caused by many factors, but its importance in the diagnosis of hip dysplasia should not be underestimated, since this is the most common question that is addressed to orthopedic doctor.
To confirm the diagnosis of hip dysplasia and control the dynamics of treatment, ultrasound diagnostics are currently widely used. The positive aspects of this method of examination include painlessness, non-invasiveness, relative safety and a sharp increase in recent availability. Also, with the help of an ultrasound examination of the joint, minimal changes in the structure of the hip joint can be detected.:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/22248886/HipSublux.jpg) But, unfortunately, this examination method does not always give accurate results (its reliability is about 85-90%. Nevertheless, to date, ultrasound diagnostics is the main method of screening for the diagnosis of hip dysplasia.
But, unfortunately, this examination method does not always give accurate results (its reliability is about 85-90%. Nevertheless, to date, ultrasound diagnostics is the main method of screening for the diagnosis of hip dysplasia.
In the case when the clinical picture differs from the data of the ultrasound examination or in case of late diagnosis of the pathology of the hip joint, the X-ray method is used. With a correctly performed radiograph, the picture of the structure of the joint and the position of the femoral head in the joint become completely clear. But due to the rather large radiation exposure during radiography, this examination method is used as rarely as possible.
In children older than a year, the main symptom is lameness on the affected side when walking or a "duck" gait with a bilateral process. Diagnosis at this age is belated. The clinical picture in this case almost always requires confirmation by x-ray, since it is necessary to accurately determine the relative position of the joint components.
And so, the child was diagnosed with hip dysplasia, what to do next and how to help the baby?
Treatment of hip dysplasia should be started as early as possible. The goal of the treatment is to center the femoral head in the joint and create conditions for the formation of the entire acetabulum. Early, most gentle, but systematic treatment allows you to completely restore the anatomy and function of the underdeveloped hip joint.
The centering of the hip in the joint in the early stages of treatment is achieved by wide swaddling - two diapers are placed between the divorced hips of the child and fixed with a third. In severe degrees of hip dysplasia, special splints are used to center the femoral head (Pavlik's stirrups, Freik's pillow, etc.). When using these tires, parents may have questions and difficulties in caring for their baby, here are some tips to help you and your baby adjust during this period:
1. Only a baby diaper (disposable or gauze) should be under the stirrups or pillow.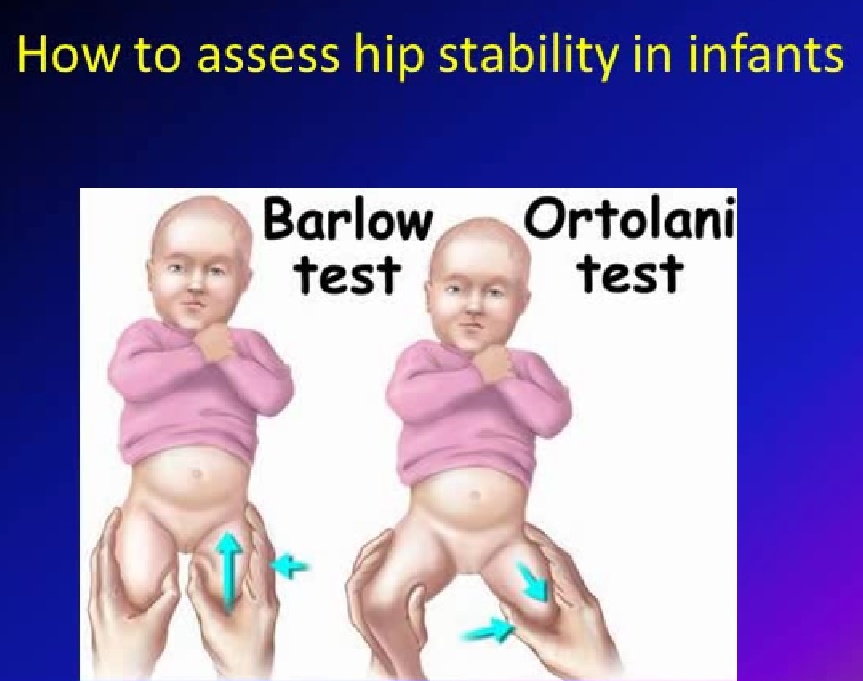 If you prefer to use gauze diapers, wear oilcloth panties that have zippers on the sides.
If you prefer to use gauze diapers, wear oilcloth panties that have zippers on the sides.
2. When changing a diaper, do not lift the child by the legs, but put your hand under the buttocks.
3. The vests can be changed without removing the stirrups: unfasten the shoulder straps from the chest strap and remove the vest over your head.
Over the tires you can wear loose pants, suits, dresses.
4. During the splint period, bathing the child is less frequent, so it is necessary to examine the skin under the straps, under the knees and around the neck 2-3 times a day to make sure there are no signs of inflammation (redness) of the skin. During this period, it is necessary to wipe the baby's skin with a soft cloth soaked in warm water. When carrying out water procedures, you can unfasten one foot part of the stirrup, but do not remove it, and keep the leg in a bent and retracted position.
5. It is also necessary to monitor the hygienic condition of the tire itself, it must always remain dry, avoid getting powders and lotions under the belts, this can cause inflammation on the baby's skin.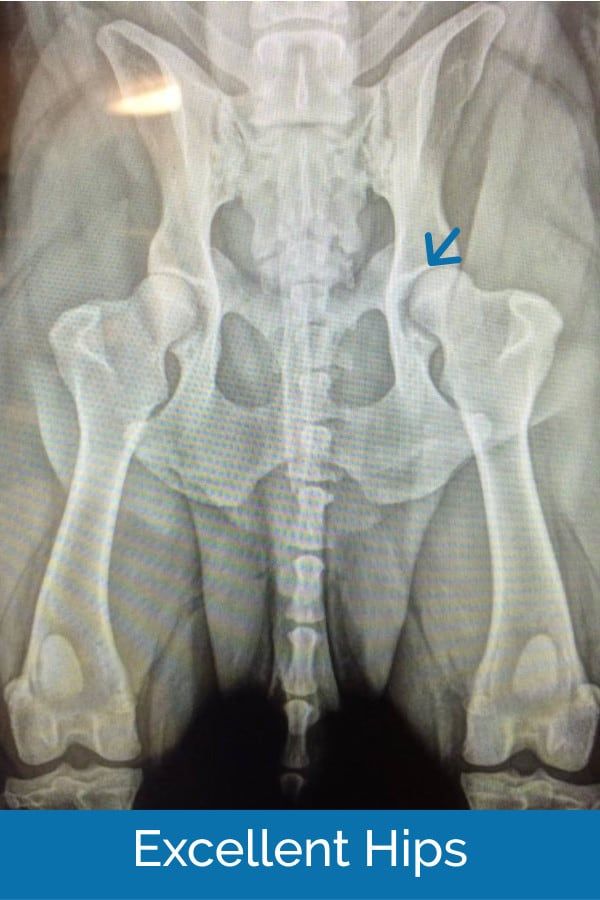
6. When feeding, be especially careful to ensure that the baby's hips do not come together.
The wearing of these devices (orthoses) is long-term - from 3 months to a year, and it is extremely important for the parents of a child who has been diagnosed with hip dysplasia to be patient and not be cowardly during the treatment period and meticulously follow the doctor's prescriptions.
After centering the femoral head, they begin massage and therapeutic exercises aimed at creating the correct ratio of the articular surfaces. We can recommend some exercises that are easy to do at home.
1. In the position of the child lying on his back, we bend the child's legs at the knee and hip joints as much as possible, and then fully straighten them.
2. In the previous starting position, we bend the child's legs at the knee and hip joints at a right angle, moderately spread the hips and, giving a moderate load along the axis of the hips, perform rotational movements with the hips.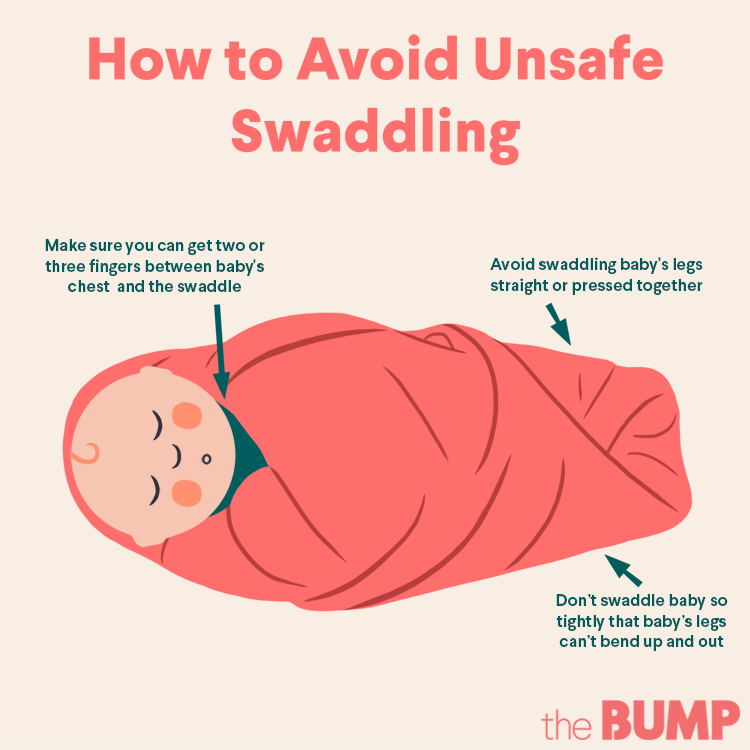
3. In the position of the child lying on his back, we breed the legs of the child bent at the knee and hip joints as much as possible to the surface of the table.
All exercises are performed 8-10 times 3-4 times a day.
Also during this period, physiotherapy (paraffin baths, electrophoresis with calcium and phosphorus preparations) is used to improve the nutrition of the joint components and complex orthopedic massage.
In cases of late diagnosis of hip dysplasia or in the absence of adequate treatment in the early stages, treatment is carried out by long-term staged plastering, as well as surgical treatment, but in these cases there are no standard treatment regimens and patient care tactics are developed individually.
After treatment of hip dysplasia, the child should be kept in the dispensary with an orthopedist for a long time - from 3 to 5 years until the end of growth. If necessary, control radiographs are performed once every 2 years to monitor the correct development of the joint. Also, restrictions on the load on the joint are often imposed. For children treated for hip dysplasia, it is desirable to visit specialized orthopedic groups in preschool institutions.
Also, restrictions on the load on the joint are often imposed. For children treated for hip dysplasia, it is desirable to visit specialized orthopedic groups in preschool institutions.
In severe degrees of hip dysplasia, functional disorders are, as a rule, lifelong in nature, even with timely and properly conducted treatment.
So what do the parents of the baby need to do in order to recognize hip dysplasia in time and, if this diagnosis was made to the child, to prevent serious complications?
First of all, it is necessary to show the child to the orthopedist in time. The recommended terms of examination by an orthopedist are 1 month, 3 months, 6 months and 1 year.
If the orthopedist nevertheless made a diagnosis of hip dysplasia, then the effectiveness of treatment by 50 percent depends on the correct and timely fulfillment by the child's parents of the doctor's prescriptions. It is important to remember that the sooner treatment is started, the better the results and the less chance of severe complications.