What are ways to induce labor
7 Natural Ways to Induce Labor
Anecdotal evidence suggests that exercise, sex, and eating certain foods may help move labor along. But it’s best to talk with a healthcare professional before attempting to induce labor.
Your due date is an educated guess for when your baby might make its arrival.
While many women deliver perfectly healthy babies 2 weeks before or after this presumed due date, it’s recommended that women wait until at least 39 weeks for delivery.
It’s best to let mother nature decide when your baby comes.
In a 2011 study, 201 women who had recently delivered babies were surveyed about inducing labor at home. Of these women, 50 percent had tried a natural method of getting labor started.
If you’re 40 weeks in, here are seven natural ways to get things moving along.
Most of these methods are anecdotal and don’t have solid evidence that they work, so you should always talk to your healthcare provider before attempting any of these methods.
Your midwife or doctor may not be able to confirm that they work, but they can let you know if it’s safe to try with your pregnancy.
Exercise can be anything that gets the heart rate up, such as a long walk. Even if this method doesn’t work, it’s a great way to relieve stress and keep your body strong for the task ahead.
Theoretically, there are multiple reasons why having sex could induce labor.
For example, sexual activity, especially having an orgasm, can release oxytocin, which may help jumpstart uterine contractions.
Also, for pregnant people who have sex with men, there are prostaglandin hormones in semen that might help ripen the cervix.
Having sex is safe during the final weeks of pregnancy, but you shouldn’t have sex after your water has broken. Doing so can increase your risk for infection.
Stimulating your nipples can cause your uterus to contract and may bring about labor.
Nipple stimulations stimulate oxytocin production. Oxytocin is the hormone that causes the uterus to contract and the breast to eject milk.
In fact, if you choose to breastfeed your baby right after delivery, this same stimulation is what will help your uterus shrink back to its original size.
You or your partner may manually stimulate your nipples, or you can try using a breast pump.
Solidresearch shows that breast stimulation can be an effective way to:
- induce and augment labor
- avoid a medical induction
- reduce rates of postpartum hemorrhage
Acupuncture has been used for thousands of years. The exact way that acupuncture works is unclear.
In Chinese Medicine, it’s believed that it balances the chi or vital energy within the body. It might also stimulate changes in hormones or in the nervous system.
Acupuncture should be administered only by a licensed acupuncturist.
In a 2013 randomized trial in Denmark, more than 400 women were given acupuncture, membrane stripping, or both procedures before labor.
Study results showed that acupuncture didn’t decrease the need for induction, but sweeping membranes did.
According to research, the main benefit of acupuncture is increased cervical ripening.
Some practitioners believe that acupressure can help start labor. Prior to applying acupressure to yourself, make sure you get proper instruction from a trained acupressure professional.
If acupressure doesn’t get your labor going, it can still be an excellent way to alleviate pain and discomfort during labor.
Drinking a little bit, like only 1–2 ounces (29.57–59.14 mL) of castor oil stimulates prostaglandin release, which can help ripen the cervix and get labor started.
It’s recommended that this be done under the supervision of a midwife or doctor. People should be careful not to drink too much.
Someresearch shows that eating dates in the final weeks of pregnancy
- increases cervical ripening and cervical dilation at the start of labor
- decreases the need for Pitocin use during labor
Most pregnant people at 40 weeks are likely ready to have their babies out of their bellies as soon as possible and in their arms.
However, there are plenty of perks to waiting until your body naturally decides to go into labor — including recovery.
Women who weren’t induced typically recover more quickly than those who were. More time in the womb can mean both you and your new baby get to go home from the hospital sooner.
Infants who are born after a full-term pregnancy also experience other benefits. More time in the womb typically means:
- more time to build muscle and strength
- reduced risk of low blood sugar, infection, and jaundice
- improved breathing as infants born even as little as two weeks early can experience twice the number of complications
- better feeding once born
- increased brain development, with the brain growing a third of its size between weeks 35 and 40
Let your body do the work for a few more days and take the time to get as much rest as you possibly can.
We know, that’s easier said than done when you’re 9 months pregnant. You and your baby will need all your energy soon enough!
You and your baby will need all your energy soon enough!
Before trying anything that might induce labor, speak with your healthcare provider to go over any risks or possible complications.
Though some of these methods are popular folklore among pregnant women, little scientific evidence supports their efficacy.
In most cases, it’s best to let baby set their own birth date, even if it means waiting another week or two.
7 Natural Ways to Induce Labor
Anecdotal evidence suggests that exercise, sex, and eating certain foods may help move labor along. But it’s best to talk with a healthcare professional before attempting to induce labor.
Your due date is an educated guess for when your baby might make its arrival.
While many women deliver perfectly healthy babies 2 weeks before or after this presumed due date, it’s recommended that women wait until at least 39 weeks for delivery.
It’s best to let mother nature decide when your baby comes.
In a 2011 study, 201 women who had recently delivered babies were surveyed about inducing labor at home. Of these women, 50 percent had tried a natural method of getting labor started.
Of these women, 50 percent had tried a natural method of getting labor started.
If you’re 40 weeks in, here are seven natural ways to get things moving along.
Most of these methods are anecdotal and don’t have solid evidence that they work, so you should always talk to your healthcare provider before attempting any of these methods.
Your midwife or doctor may not be able to confirm that they work, but they can let you know if it’s safe to try with your pregnancy.
Exercise can be anything that gets the heart rate up, such as a long walk. Even if this method doesn’t work, it’s a great way to relieve stress and keep your body strong for the task ahead.
Theoretically, there are multiple reasons why having sex could induce labor.
For example, sexual activity, especially having an orgasm, can release oxytocin, which may help jumpstart uterine contractions.
Also, for pregnant people who have sex with men, there are prostaglandin hormones in semen that might help ripen the cervix.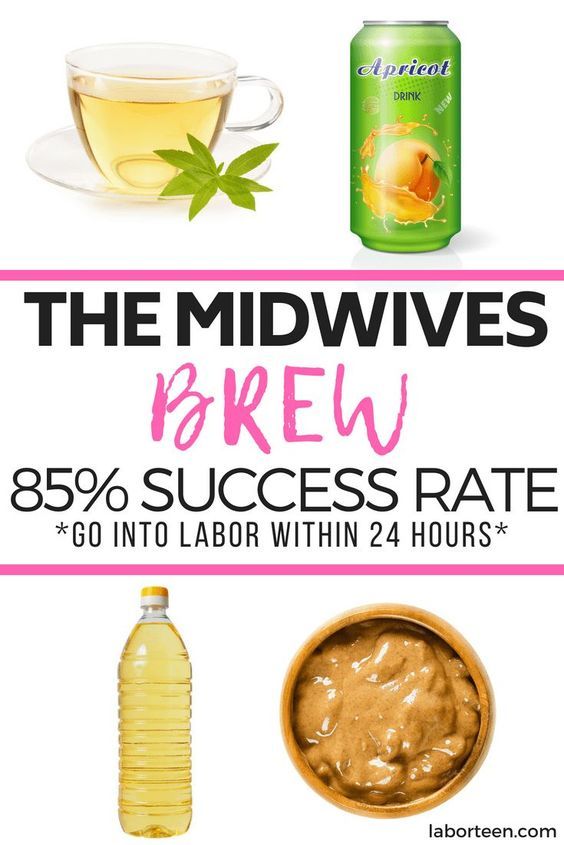
Having sex is safe during the final weeks of pregnancy, but you shouldn’t have sex after your water has broken. Doing so can increase your risk for infection.
Stimulating your nipples can cause your uterus to contract and may bring about labor.
Nipple stimulations stimulate oxytocin production. Oxytocin is the hormone that causes the uterus to contract and the breast to eject milk.
In fact, if you choose to breastfeed your baby right after delivery, this same stimulation is what will help your uterus shrink back to its original size.
You or your partner may manually stimulate your nipples, or you can try using a breast pump.
Solidresearch shows that breast stimulation can be an effective way to:
- induce and augment labor
- avoid a medical induction
- reduce rates of postpartum hemorrhage
Acupuncture has been used for thousands of years. The exact way that acupuncture works is unclear.
In Chinese Medicine, it’s believed that it balances the chi or vital energy within the body. It might also stimulate changes in hormones or in the nervous system.
It might also stimulate changes in hormones or in the nervous system.
Acupuncture should be administered only by a licensed acupuncturist.
In a 2013 randomized trial in Denmark, more than 400 women were given acupuncture, membrane stripping, or both procedures before labor.
Study results showed that acupuncture didn’t decrease the need for induction, but sweeping membranes did.
According to research, the main benefit of acupuncture is increased cervical ripening.
Some practitioners believe that acupressure can help start labor. Prior to applying acupressure to yourself, make sure you get proper instruction from a trained acupressure professional.
If acupressure doesn’t get your labor going, it can still be an excellent way to alleviate pain and discomfort during labor.
Drinking a little bit, like only 1–2 ounces (29.57–59.14 mL) of castor oil stimulates prostaglandin release, which can help ripen the cervix and get labor started.
It’s recommended that this be done under the supervision of a midwife or doctor. People should be careful not to drink too much.
People should be careful not to drink too much.
Someresearch shows that eating dates in the final weeks of pregnancy
- increases cervical ripening and cervical dilation at the start of labor
- decreases the need for Pitocin use during labor
Most pregnant people at 40 weeks are likely ready to have their babies out of their bellies as soon as possible and in their arms.
However, there are plenty of perks to waiting until your body naturally decides to go into labor — including recovery.
Women who weren’t induced typically recover more quickly than those who were. More time in the womb can mean both you and your new baby get to go home from the hospital sooner.
Infants who are born after a full-term pregnancy also experience other benefits. More time in the womb typically means:
- more time to build muscle and strength
- reduced risk of low blood sugar, infection, and jaundice
- improved breathing as infants born even as little as two weeks early can experience twice the number of complications
- better feeding once born
- increased brain development, with the brain growing a third of its size between weeks 35 and 40
Let your body do the work for a few more days and take the time to get as much rest as you possibly can.
We know, that’s easier said than done when you’re 9 months pregnant. You and your baby will need all your energy soon enough!
Before trying anything that might induce labor, speak with your healthcare provider to go over any risks or possible complications.
Though some of these methods are popular folklore among pregnant women, little scientific evidence supports their efficacy.
In most cases, it’s best to let baby set their own birth date, even if it means waiting another week or two.
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.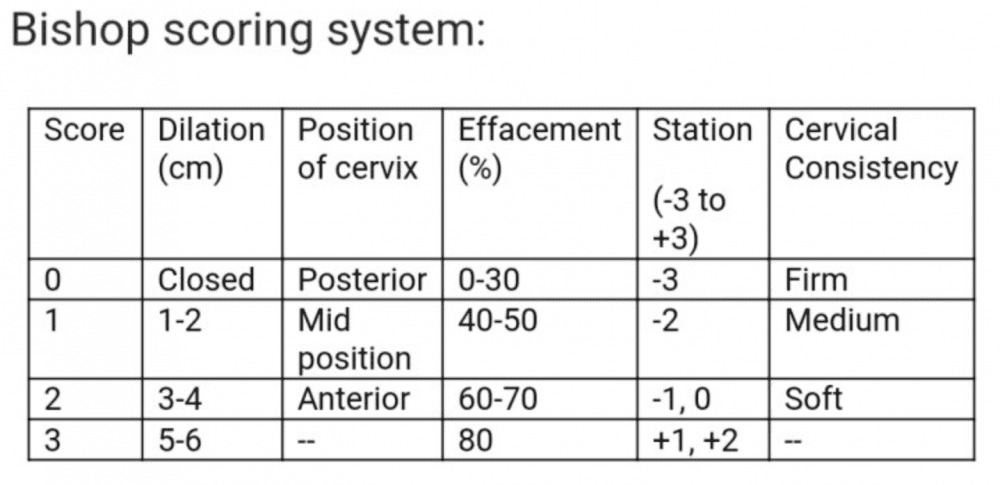
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix of the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body.
 It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
It prepares the body for childbirth, under its action the cervix becomes softer and begins to open. - Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already dilated sufficiently, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions).
 The dose of the drug can be increased as needed to achieve regular uterine contractions.
The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.

- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.
Induction of labor, compared with spontaneous labor, increases the risk of prolonged labor, the need for instrumentation
(use of vacuum or forceps), postpartum hemorrhage, uterine rupture, the onset of too frequent uterine contractions and the associated deterioration of the fetus, prolapse umbilical cord, as well as premature detachment of the placenta.
If induction of labor is not successful
The time frame for induction of labor varies from patient to patient, on average labor begins within 24-72 hours. Sometimes more than one method is required.
The methods used do not always work equally quickly and in the same way on different patients. If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
ITK833
This informational material was approved by the Women's Clinic on 01/01/2022.
Labor induction at home and in hospital
What is the problem?
Based on the results of randomized controlled trials (RCTs), we wanted to find out whether women preferred to return home or stay in the facility while waiting for labor after induction of labor in a medical facility. In addition, it needs to be established whether this has an impact on clinical outcomes for both women and their infants.
Why is this important?
Induction of labor at the end of pregnancy involves the artificial induction of labor to initiate the process of labor. There are maternal and infant health risks associated with labor induction, but sometimes the risks of prolonged pregnancy far outweigh them.
However, induction of labor can be a very difficult challenge for women, as they may feel they are deprived of comfort, support, and control over the process. The use of home induction of labor can improve the conditions of labor for women, reduce length of hospital stay, and reduce overall costs. The safety of both mother and child is a critical factor to consider. Only certain forms of induction are suitable for home induction (stimulation) of labor, such as vaginal prostaglandins or balloon/Foley catheters.
The safety of both mother and child is a critical factor to consider. Only certain forms of induction are suitable for home induction (stimulation) of labor, such as vaginal prostaglandins or balloon/Foley catheters.
What evidence did we find?
We searched for evidence on 31 January 2020 and found seven RCTs, six of which provided data on 1610 women and their infants. All of these studies were conducted in high-income countries. The certainty of the evidence was generally very low, mainly due to the limited number of trials, some of which were small, and the lack of clarity on study design.
Labor induction was performed in all trial participants at initial hospital follow-up. Women in the home labor induction group could then go home to wait for active labor to begin, or for a set period of time. Women belonging to the group giving birth in a medical facility remained in the hospital.
Two trials were found involving 1022 women and their infants who were given vaginal prostaglandin (PGE2) to induce labor. The difference in women's satisfaction with waiting to give birth at home or in hospital may be minimal or non-existent, although women were generally more satisfied with waiting at home. Outcomes for women: There may not be clear differences in the number of women with spontaneous vaginal delivery, or with uterine hyperstimulation, or in the number of deliveries by caesarean section. Infant outcomes: There may be similar rates of infection and admission to the neonatal intensive care unit (NICU). At home, costs may be less.
The difference in women's satisfaction with waiting to give birth at home or in hospital may be minimal or non-existent, although women were generally more satisfied with waiting at home. Outcomes for women: There may not be clear differences in the number of women with spontaneous vaginal delivery, or with uterine hyperstimulation, or in the number of deliveries by caesarean section. Infant outcomes: There may be similar rates of infection and admission to the neonatal intensive care unit (NICU). At home, costs may be less.
For labor induction with controlled vaginal release prostaglandin (PGE2), we found only one study involving 299 women and their infants, but the results probably indicate little or no difference.
On the use of a balloon catheter or Foley catheter for induction, we found three studies providing data on 289 women and their infants. Two studies reported on women's satisfaction and showed a tendency to prefer home environments, but the mode of data collection was unclear.