Very itchy during pregnancy
Itching and intrahepatic cholestasis of pregnancy
Itching is common in pregnancy. Usually it's thought to be caused by raised levels of certain chemicals in the blood, such as hormones.
Later, as your bump grows, the skin of your tummy (abdomen) is stretched and this may also feel itchy.
However, itching can be a symptom of a liver condition called intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC).
ICP needs medical attention. It affects around 1 in 140 pregnant women in the UK.
Symptoms of ICP
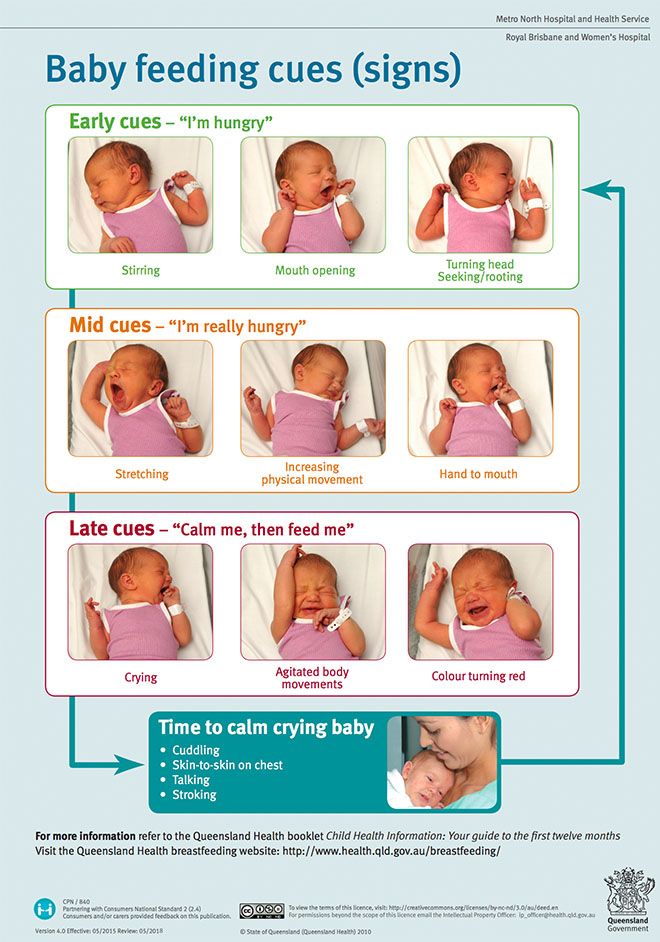
The main symptom is itching, usually without a rash. For many women with ICP, the itching is often:
- more noticeable on the hands and feet, but can be all over the body
- worse at night
Other symptoms can include:
- dark urine
- pale poo
- yellowing of the skin and whites of the eyes (jaundice), but this is less common
Symptoms of ICP typically start from around 28 weeks of pregnancy, but it's possible to develop the condition earlier.
Non-urgent advice: Call your midwife or GP if you have itching that's:
- mild or distressing, possibly worse at night
- anywhere on your body, but may be worse on the palms of your hands and soles of your feet
Feeling itchy like this can be a sign of ICP and needs to be checked.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation.
You may also want to avoid synthetic materials and opt for natural ones, such as cotton, instead. These are "breathable" and allow the air to circulate close to your skin.
You may find having a cool bath or applying lotion or moisturiser can help soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using unperfumed lotion or soap.
Mild itching is not usually harmful to you or your baby, but it can sometimes be a sign of a more serious condition, particularly if you notice it more in the evenings or at night.
Let your midwife or doctor know if you are experiencing itching so they can decide whether you need to have any further investigations.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy (ICP) is a potentially serious liver disorder that can develop in pregnancy.
Normally, bile acids flow from your liver to your gut to help you digest food.
In ICP, the bile acids do not flow properly and build up in your body instead. There's no cure for ICP, but it should go once you've had your baby.
ICP seems to run in families, but it can happen even if there is no family history. It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
If you have had ICP in a previous pregnancy, you have a high chance of developing it again in another pregnancy.
Some studies have found that babies whose mothers have ICP have a higher chance of being born prematurely or stillborn.
Because of the link with stillbirth, you may be offered induction of labour. This could be any time from 35 weeks, depending on the level of bile acids in your blood.
If you have ICP, you will probably be advised to give birth in hospital under a consultant-led maternity team.
Diagnosis and treatment of ICPICP is diagnosed by excluding other causes of the itch. Your doctor will probably talk to you about your medical and family history and advise you to have some blood tests.
These will include tests to check your liver function (LFT) and measure your bile acid levels (BA).
If you are diagnosed with ICP, you will have regular liver blood tests (LFTs) and bile acid measurement tests so your doctor can monitor your condition.
Initially, you may be given these tests every week. You may then be given more, or less, frequent tests depending on the results and your symptoms.
Creams and medicines for ICPCreams, such as aqueous cream with menthol, are safe to use in pregnancy and can provide some relief from itching.
A medicine called ursodeoxycholic acid (UDCA) can be prescribed to try to relive itching. But recent evidence suggests it may not be effective in reducing bile acids and easing itching.
UDCA is considered safe to take in pregnancy, although it is prescribed on what is known as an "informed consent" basis as it has not been properly tested in pregnancy.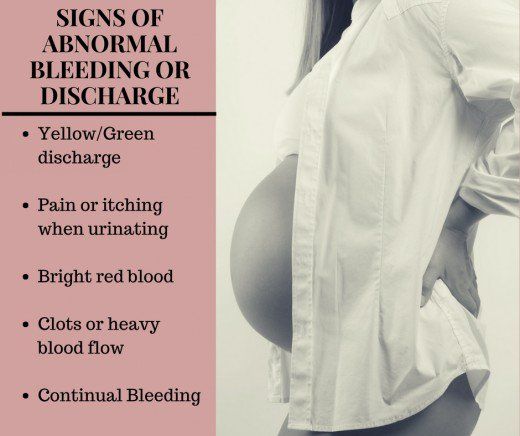 It is usually only prescribed by a hospital doctor.
It is usually only prescribed by a hospital doctor.
A possible alternative, which can be helpful if itchiness is keeping you awake at night, is antihistamine medicine, such as chlorphenamine. Chlorphenamine tends to cause drowsiness so it can also help with sleep problems as well as itchiness. If you do feel drowsy do not drive or operate machinery.
You may also be offered a vitamin K supplement. This is because ICP can affect your absorption of vitamin K, which is important for healthy blood clotting.
Most experts on ICP only prescribe vitamin K if the mother-to-be reports pale poo, has a known blood clotting problem, or has very severe ICP from early in pregnancy.
If you are diagnosed with ICP, your midwife and doctor will discuss your health and your options with you.
Further information
There is information about obstetric cholestasis on the Royal College of Obstetricians & Gynaecologists (RCOG) website, including what it means for you and your baby, and the treatment that's available.
You can also get information about intrahepatic cholestasis of pregnancy (ICP) on the British Liver Trust website.
The charity ICP Support provides information about ICP. You can also watch a video about living with intrahepatic cholestasis of pregnancy (ICP) on the ICP support website featuring mums and clinical experts.
Community content from HealthUnlockedItching during pregnancy | Pregnancy Birth and Baby
beginning of content3-minute read
Listen
Mild itching is common in pregnancy because of the increased blood supply to the skin. As your pregnancy progresses and as your baby grows, the skin of your abdomen is stretched and this may also feel itchy.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg)
Mild itching is usually nothing to worry about, but if the itching becomes severe it can be a sign of a serious liver condition called obstetric cholestasis. This affects fewer than 1 in 100 pregnant women, but needs medical attention.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation. You may also want to avoid synthetic materials and choose natural fabrics such as cotton that allow the air to circulate close to your skin. You may find that having a cool bath or applying lotion or moisturiser can help to soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using plain lotion or soap.
Serious itching: obstetric cholestasis
If you’re worried about your itching, or if you have severe itching, it’s important to see your midwife or doctor.
Obstetric cholestasis (OC), also called intrahepatic cholestasis of pregnancy, is a serious liver disorder that affects a small number of pregnant women, usually in the last 3 months of pregnancy.
Causes of obstetric cholestasis
The cause of OC is unclear, but it’s thought the rise of pregnancy hormones later in pregnancy may slow the normal flow of bile — the digestive fluid made in the liver that helps your digestive system break down fats. In OC, bile salts build up rather than leaving the liver, eventually entering the bloodstream, which can make you feel itchy.
OC seems to run in families, although it can occur with no family history. It is also more common in women of Indian and Pakistani origin. If you have had OC in a previous pregnancy, you're more likely to develop it again in a subsequent pregnancy.
Babies of women with OC are more likely to be born prematurely or to be stillborn, or to have lung problems from breathing in meconium. Because of these complications, your doctor may consider inducing labour before you are due.
Symptoms of obstetric cholestasis
The classic symptom of OC is itching without rash, usually on the palms and soles of the feet, but it may be more widespread. The itching can be non-stop or unbearable, and worse at night.
The itching can be non-stop or unbearable, and worse at night.
Other symptoms include dark urine, jaundice (yellowing of the skin and whites of the eyes), and pale bowel movements (poo).
The itchiness usually goes away within a few days after giving birth.
Treatment of obstetric cholestasis
OC is diagnosed through taking a medical and family history, and blood tests that check your liver function (liver functions tests — LFTs). Once OC is diagnosed, you will have regular LFTs until your baby is born, so that your doctor can monitor your condition.
Creams, such as calamine lotion, are safe to use in pregnancy and can provide some relief from itching. Your doctor may prescribe a medication to reduce bile salts and ease itching.
OC can affect your absorption of vitamin K, which is important for healthy blood clotting so you may be offered a vitamin K supplement.
If you are diagnosed with OC, your midwife and doctor will discuss your health and your options with you.
Sources:
Mayo Clinic (Cholestasis of pregnancy), NSW Health (Having a baby), Royal Women’s Hospital (Common concerns in early pregnancy), SA Health Department (Clinical guideline obstetric cholestasis), Women's and Children's Health Network (Itching in pregnancy), King Edward Memorial Hospital (Cholestasis in pregnancy - clinical guidelines)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Some features, tools or interaction may not work correctly.
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from? nine0005
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood. This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus. nine0003
Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus. nine0003
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women. nine0003
If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women. nine0003
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers. nine0003
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Itchy skin during pregnancy: causes and remedies
Itching of the skin during pregnancy can be psychogenic. In this case, itching is a consequence of stress, an early symptom of multiple sclerosis. nine0003
In the early stages, itching occurs due to loss of skin elasticity caused by hormonal changes and excessive dryness of the skin. In the second and third trimester, the reasons may be the rapid weight gain of the expectant mother, the developing stretching of the skin of the abdomen as it increases.
Some expectant mothers experience intimate itching. It is provoked by genital infections, urological and proctological diseases.
The causes of skin itching also include dermatoses of pregnant women (atopic dermatitis, cholestasis of pregnancy). They are provoked by hereditary predisposition, decreased immunity, physiological changes (stretching of the skin with damage to the connective tissue).
Atopic dermatitis is the most common cause of itching during pregnancy. A specific condition is caused by hormonal immune restructuring of the whole organism. In 80% of cases, the disease manifests itself exclusively during pregnancy, and all signs disappear after childbirth without specific treatment. nine0003
Atopic dermatitis is more common in nulliparous women in the early stages and in the second trimester. Itching is caused by papular and exametic rashes localized on the face, neck, limbs, elbows, palms.
Atopic dermatitis is the most benign form of dermatosis of pregnancy and usually does not adversely affect the fetus. However, children born to mothers who suffered from this disease at the stage of gestation are also prone to allergic skin diseases. nine0003
Itching of the skin, as a symptom of cholestasis, is provoked by intrahepatic stagnation of bile as a reaction to increased estrogen production. The disease occurs at the end of the second - beginning of the third trimester, closer to the date of birth.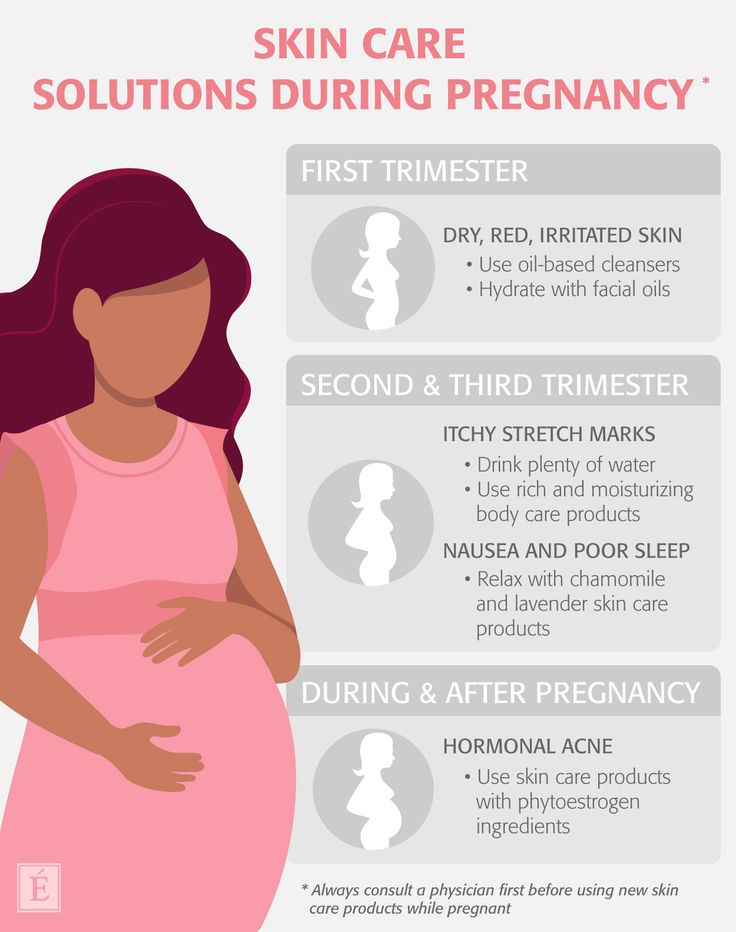 A pregnant woman experiences severe itching in the abdomen, back, palms, legs.
A pregnant woman experiences severe itching in the abdomen, back, palms, legs.
Cholestasis is dangerous for the health of the mother and unborn child in severe cases of the disease. There is a risk of fetal hypoxia, delayed development and even premature birth. nine0003
Symptoms
The main sign of pathological changes is the appearance of irritating-itchy sensations in different parts of the body. Locally, a woman may also feel a tingling and burning sensation.
Other symptoms include:
- blistering or eruption of blistering character;
- peeling, irritation and redness of the skin;
- formation of scaly spots;
- sores and sores caused by scratching; nine0057
- deterioration in general condition caused by sleep disorders and emotional depression.
In most cases, itching of the skin during pregnancy does not pose a real danger to the intrauterine development of the fetus, but significantly worsens the quality of life of the expectant mother, acts depressingly on the state of her nervous system and general well-being.
Diagnostics
In order to successfully deal with itching, it is necessary to establish the cause that causes it. The choice of diagnostic methods is determined based on the degree of intensity and localization of itching, the presence of concomitant symptoms and chronic diseases, the duration of pregnancy, and the individual characteristics of the health of the expectant mother. nine0003
Treatment is prescribed only after the exact cause of the itching is established.
At the initial examination, the doctor listens to the patient's complaints, examines the condition of the skin, paying attention to the appearance of rashes or spots. This allows you to draw a preliminary conclusion and determine what laboratory tests and instrumental studies will be needed.
The main diagnostic measures for itchy skin in pregnant women include: nine0003
- general urine and blood tests;
- biochemical blood test;
- studies of hormone levels - if endocrine pathologies are suspected;
- analysis of vaginal smear for microflora;
- skin scraping examination;
- allergy testing;
- Ultrasound of the digestive tract, liver and kidneys;
- histological examination;
- analysis of feces for the detection of helminth eggs.
 nine0057
nine0057
The choice of research methods is determined individually. In some cases, a pregnant woman is shown a consultation with an endocrinologist, urologist, gastroenterologist, venereologist.
Identification of atopic dermatitis is usually not difficult. In addition to the general examination, such types of diagnostics as dermatoscopy and examination under the Voodoo lamp are carried out.
If itching in a pregnant woman is allergic in nature, a mandatory diagnostic measure is the determination of the allergen (pathogen). nine0003
Treatment of itching
Although itching during pregnancy is not dangerous in many cases, it should not be tolerated either. You need to tell the gynecologist about unpleasant sensations, who will determine the diagnostic methods and, if necessary, give a referral to other specialists. Treatment of itching during pregnancy is carried out by the attending gynecologist together with a dermatologist.
You can not self-medicate and use medicines without the approval of a doctor.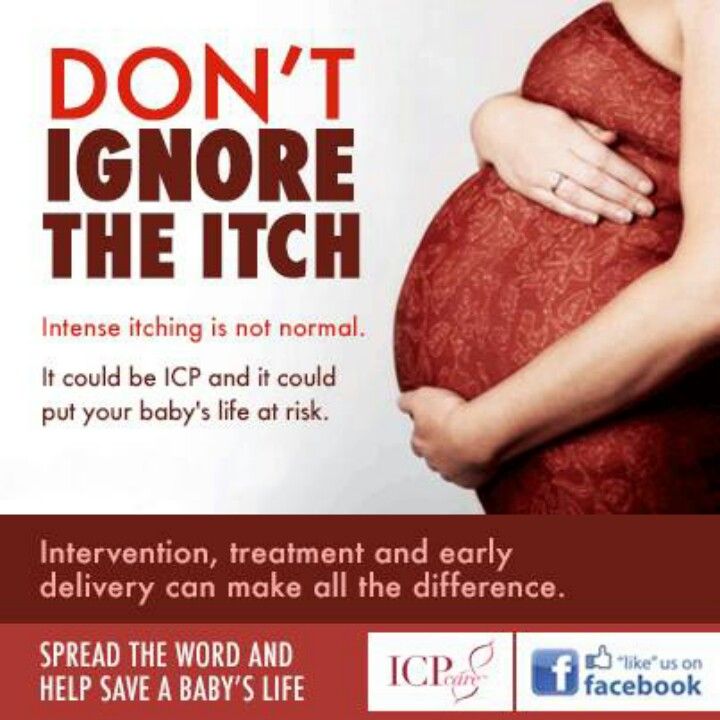 Many of them have contraindications and can cause severe side effects. A pregnant woman should remember the prohibition of scratching itchy places. This leads to a violation of the integrity of the skin, the appearance of wounds and abrasions, which will become sites of infection. nine0003
Many of them have contraindications and can cause severe side effects. A pregnant woman should remember the prohibition of scratching itchy places. This leads to a violation of the integrity of the skin, the appearance of wounds and abrasions, which will become sites of infection. nine0003
The treatment regimen depends on the disease that causes itching. When choosing drug therapy, the risks of negative effects on the fetus are taken into account. This is especially true in the case of the appointment of antibiotics, hormonal and antifungal drugs. Self-medication is unacceptable!
In the treatment of itching during pregnancy, the following types of drugs can be prescribed:
- antihistamines - to eliminate itching caused by dermatitis, urticaria; nine0057
- glucocorticoids - used to treat dermatitis;
- emollients - have a moisturizing and regenerating effect in case of excessive dryness and dehydration of the skin;
- adsorbents and hepatoprotectors - to normalize the liver;
- choleretic preparations - for the correction of the state of the digestive tract;
- sedatives - to normalize the state of the nervous system, if a pregnant woman has signs of increased anxiety and sleep disturbances.
 nine0057
nine0057
With moderate itching, a pregnant woman is shown taking baths with a decoction of a string or oatmeal. An oatmeal bath is effective for itching caused by stretch marks, eczema, or psoriasis. To prepare it, crushed oatmeal is mixed with baking soda and a little milk is added, the mixture is poured into a warm bath.
Lotions on herbal decoctions can be applied to itchy areas of the skin. Chamomile, succession or St. John's wort is poured with boiling water and insisted. After a few hours, the decoction for lotions is ready for use. nine0003
To eliminate itching of the genital organs, medicinal suppositories with local action are prescribed. Of great benefit are sitz baths of decoctions of sage or chamomile.
Itching in the abdomen, caused by skin tension, can cause stretch marks. To prevent aesthetic imperfections, it is necessary to moisturize the skin with special means.
To reduce itching, a pregnant woman should only wear clothes made from natural fabrics, preferably cotton. Natural fabrics allow the skin to breathe freely. It is useful for future mothers to take a cool shower without the use of soaps or bathing gels. The skin needs to be effectively protected from external aggressive factors: sun, frost and wind. nine0003
Natural fabrics allow the skin to breathe freely. It is useful for future mothers to take a cool shower without the use of soaps or bathing gels. The skin needs to be effectively protected from external aggressive factors: sun, frost and wind. nine0003
When itching of the skin appears, it is better to refuse the use of perfumes, take the choice of cosmetics very responsibly.
Prophylaxis
Itching during pregnancy can be prevented if you follow the doctor's recommendations and preventive measures. Tips for expectant mothers:
- meticulously observe body hygiene, take regular showers or baths without the use of perfumed substances;
- refuse underwear and clothes made of synthetic fabrics; nine0057
- after taking a shower or bath, moisturize the skin of the body with special products, with a neutral pH level, creams, lotions, emulsions are suitable for this;
- use phosphate-free laundry detergents;
- wear loose clothing that does not restrict movement;
- avoid stuffy rooms or open places under the scorching summer sun;
- exclude intense physical activity that provokes increased sweating; nine0057
- provide the expectant mother with a plentiful drinking regimen that prevents dehydration of the body;
- avoid stressful situations, get positive impressions.

Proper nutrition plays an important role in the prevention of itching of the skin. This is especially important if itching is provoked by various foods. The woman is recommended a hypoallergenic diet, with the exception of fast food, smoked, salty and pickled foods, as well as foods with preservatives, emulsifiers and artificial flavors. The diet of the future mother should be rich in vitamins, minerals, fatty acids, antioxidants. To do this, the menu includes sour-milk products, meat and fish of low-fat varieties, vegetable dishes, fruits. nine0003
Itching during pregnancy when following medical recommendations has a favorable prognosis and is not an obstacle to natural childbirth.
If a woman had signs of atopic dermatitis during her first pregnancy, the likelihood of a recurrence of the disease during subsequent pregnancies is high. At the stage of planning a child, it is necessary to visit a dermatologist.
Itching
A series of products "Emolium" effectively eliminates the symptoms of skin diseases, including itching, peeling, irritability.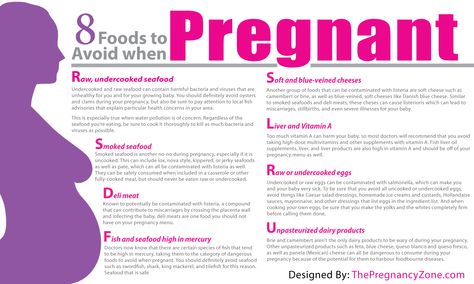 They are prescribed to moisturize the skin, eliminate dryness and tightness in atopic dermatitis, psoriasis, eczema, and allergies. Means of the Emolium series are used in the complex treatment of these and other diseases that provoke itching. nine0003
They are prescribed to moisturize the skin, eliminate dryness and tightness in atopic dermatitis, psoriasis, eczema, and allergies. Means of the Emolium series are used in the complex treatment of these and other diseases that provoke itching. nine0003
The main advantages of the series:
- have a mild anti-inflammatory effect;
- ensure the normal functioning of the skin;
- restore skin structure;
- retain moisture in cells and intercellular space;
- restore the water-lipid layer;
- relieve irritation and itching.
The delicate and delicate consistency of the products makes it easy to apply and distribute them over the entire surface of the affected areas. nine0003
With severe itching of pregnant women, a triactive series is recommended, taking care of atopic and damaged skin. Triactive cream enriched with rapeseed oil and sodium hyaluronate has anti-inflammatory, antibacterial and antipruritic effects.