Uti in babies treatment
Urinary Tract Infections (UTIs) in Infants & Children
What Are Urinary Tract Infections (UTIs)?
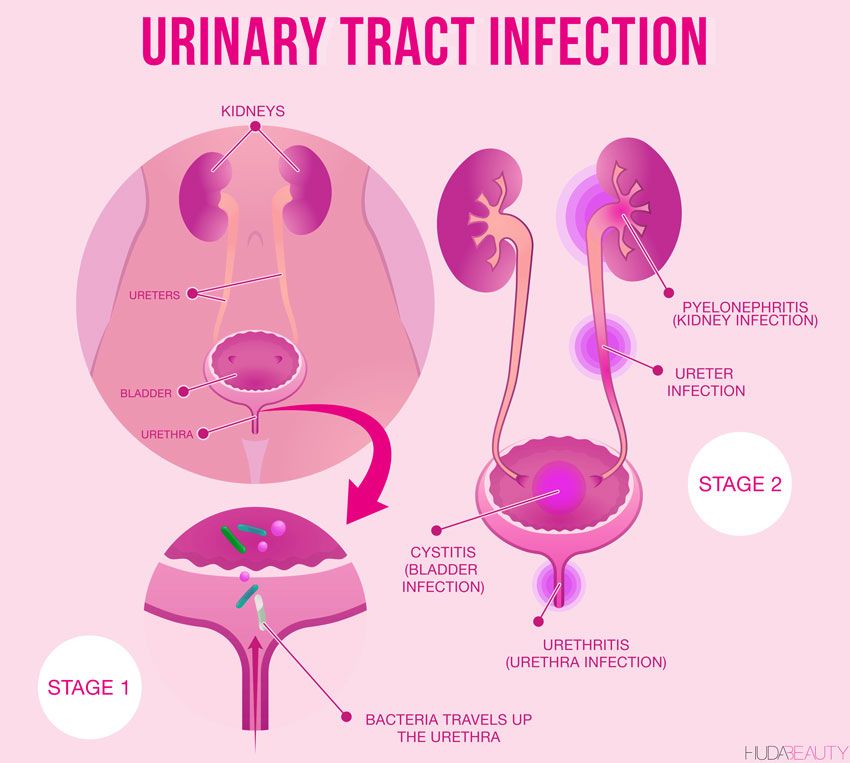
A urinary tract infection (UTI) happens when bacteria (germs) gets into the urinary tract. The most common place for a UTI to occur is in the bladder, but infections also occur in the urethra, ureters or kidneys. UTIs are easily treated but can cause problems if left alone.
What is the urinary tract and how do infections occur?
The urinary tract is the body’s drainage system for getting rid of urine (liquid waste). It includes the two kidneys, bladder (the organ where urine is stored), and two ureters and one urethra (tubes).
The blood in the body passes through the kidneys. The kidneys filter the liquid waste products (urine) out of the blood. This urine passes through the ureters and into the bladder. The urine leaves the bladder through the urethra, and passes out of the body through the opening (meatus).
Most UTIs in children occur because bacteria that are normally found in the bowel cause an infection in the urinary tract.
What causes UTIs?
These factors can increase your child’s chance of getting a UTI:
- Poor bathroom habits, such as not changing out of wet underwear or not wiping properly
- “Holding it,” instead of urinating frequently (in toilet trained kids)
- Frequent constipation or diarrhea
- Having some kind of blockage in the urinary tract that limits or stops urine flow
- Irritation in the “perineal” area (where urine comes out of the body). This can be caused by things such as bubble bath, bath soap or tight clothing.
- A condition called vesicoureteral reflux (VUR), in which urine flows backward from the bladder and toward the kidneys
Learn about how to prevent a UTI.
Are UTIs common in children?
UTIs are the second most common type of infection in children (ear infections are the most common). They are more common in girls, although uncircumcised boys are at slightly higher risk than other male babies or older boys.
What are the signs and symptoms of a UTI?
There are two different kinds of UTIs. The most common is called cystitis. It occurs when the infection is in the urethra or bladder. A child who has cystitis may:
- Have a fever (this may be the only symptom in babies)
- Be fussy (common in babies)
- Vomit (common in babies or older children)
- Feel the need to use the bathroom often, yet only pass a very small amount of urine (more common in older children)
- Wet themselves, even after being successfully potty trained
- Have pain or burning with urination (more common in older children)
- Have lower belly or back pain
- Have blood in the urine
The less common type of UTI is called pyelonephritis, which is an infection that occurs in the kidneys. Pyelonephritis can sometimes be treated at home, but in some cases it can become serious and even life threatening. A child who has pyelonephritis may have:
- A fever greater than 101 degrees
- Flu-like symptoms such as shaking, chills, nausea, vomiting or achiness
- Pain in the belly, back, side or groin
- Pain or a burning feeling when urinating
- Urine that is cloudy, red, foul smelling or changes to a dark cola color
- Pus or blood in the urine
- Urgent or frequent urination
If your child experiences symptoms of cystitis or pyelonephritis, call your pediatrician.
How is a child diagnosed with a UTI?
If the pediatrician thinks your child may have a UTI, they will:
- Ask about your child’s symptoms and health history
- Do a physical exam
- Run tests, including a urinalysis (a simple study of a urine sample) and/or urine culture (which detects specific bacteria in urine)
How do you treat UTIs?
The most common treatment for a UTI is antibiotics, which kill the germs that are causing the infection. The pediatrician also may recommend that your child take pain relief medicine as needed, and drink plenty of fluids.
UTIs can cause irritation and raw skin on your child’s private parts. If these symptoms do not improve after exposing the skin to air and creating a moisture barrier with petroleum jelly or, zinc oxide or lanolin, let your pediatrician know.
If my child is being treated for a UTI, what can I do to help?
- Give your child all the medicine the doctor prescribed for the infection.
 Do not stop the medicine, even if your child is feeling and acting better.
Do not stop the medicine, even if your child is feeling and acting better. - Give your child lots of fluids to drink so they continue to urinate regularly, every two to three hours for toilet trained children.
- Tell your doctor if your child’s fever, pain or other symptoms continue after taking the medicine for two days.
- If your child is in pain or has a fever, give medicine only as directed by the doctor. Do not give aspirin to children.
- Keep all follow-up appointments.
- Do not allow your child to sit in bathwater that contains bubble bath, shampoo or soap, as this can cause irritation. If your child takes a bath, have them sit in clear water until you’re ready to use these products. Once you are finished, rinse your child off and remove the products from the tub.
What if my child gets frequent UTIs?
Some children get UTIs more often than others. Be sure to tell your pediatrician if symptoms happen again after treatment, or if your child has three or more UTIs in a six-month period.
The pediatrician may recommend taking your child to a pediatric urology practice for an evaluation. Physicians and nurse practitioners at this type of practice specialize in treating children who have problems with their urinary system. These specialists may run additional tests to learn about the cause, and recommend a new treatment plan.
These additional tests may include:
- An ultrasound to view the kidneys, bladder and the tubes connecting them
- A voiding cystourethrogram (sis-toe-u-reeth-ro-gram), or VCUG. This X-ray shows how the bladder is working while the person is urinating.
Last Updated 07/2021
Reviewed By Nicole Inman, CNP
The Division of Urology treats a complete range of disorders affecting the urinary and genital tracts, from common concerns to rare and complex abnormalities.
Learn More
For more information or to request an appointment, contact the Division of Urology.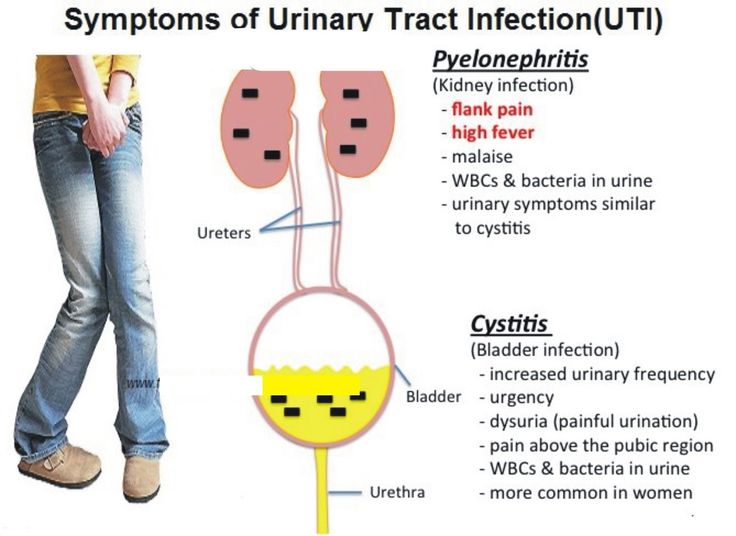
Contact Us
Diagnosis and Treatment of Urinary Tract Infections in Children
BRETT WHITE, MD
Acute urinary tract infections are relatively common in children, with 8 percent of girls and 2 percent of boys having at least one episode by seven years of age. The most common pathogen is Escherichia coli, accounting for approximately 85 percent of urinary tract infections in children. Renal parenchymal defects are present in 3 to 15 percent of children within one to two years of their first diagnosed urinary tract infection. Clinical signs and symptoms of a urinary tract infection depend on the age of the child, but all febrile children two to 24 months of age with no obvious cause of infection should be evaluated for urinary tract infection (with the exception of circumcised boys older than 12 months). Evaluation of older children may depend on the clinical presentation and symptoms that point toward a urinary source (e.g., leukocyte esterase or nitrite present on dipstick testing; pyuria of at least 10 white blood cells per high-power field and bacteriuria on microscopy). Increased rates of E. coli resistance have made amoxicillin a less acceptable choice for treatment, and studies have found higher cure rates with trimethoprim/sulfamethoxazole. Other treatment options include amoxicillin/clavulanate and cephalosporins. Prophylactic antibiotics do not reduce the risk of subsequent urinary tract infections, even in children with mild to moderate vesicoureteral reflux. Constipation should be avoided to help prevent urinary tract infections.
Clinical signs and symptoms of a urinary tract infection depend on the age of the child, but all febrile children two to 24 months of age with no obvious cause of infection should be evaluated for urinary tract infection (with the exception of circumcised boys older than 12 months). Evaluation of older children may depend on the clinical presentation and symptoms that point toward a urinary source (e.g., leukocyte esterase or nitrite present on dipstick testing; pyuria of at least 10 white blood cells per high-power field and bacteriuria on microscopy). Increased rates of E. coli resistance have made amoxicillin a less acceptable choice for treatment, and studies have found higher cure rates with trimethoprim/sulfamethoxazole. Other treatment options include amoxicillin/clavulanate and cephalosporins. Prophylactic antibiotics do not reduce the risk of subsequent urinary tract infections, even in children with mild to moderate vesicoureteral reflux. Constipation should be avoided to help prevent urinary tract infections. Ultrasonography, cystography, and a renal cortical scan should be considered in children with urinary tract infections.
Ultrasonography, cystography, and a renal cortical scan should be considered in children with urinary tract infections.
Guidelines regarding the diagnosis, treatment, and follow-up of urinary tract infections (UTIs) in children continue to evolve. Although a somewhat less aggressive approach to evaluation is now recommended, it is important for primary care physicians to appropriately diagnose and treat UTIs in children. Some underlying etiologies, including renal scarring and renal disease, can lead to considerable morbidity later in life.
Acute UTIs are relatively common in children. By seven years of age, 8 percent of girls and 2 percent of boys will have at least one episode.1 In a study of infants presenting to pediatric emergency departments, the prevalence of UTI in infants younger than 60 days with a temperature greater than 100. 4°F (38°C) was 9 percent.2 The reference standard for the diagnosis of UTI is a single organism cultured from a specimen obtained at the following concentrations: suprapubic aspiration specimen, greater than 1,000 colony-forming units per mL; catheter specimen, greater than 10,000 colony-forming units per mL; or clean-catch, midstream specimen, 100,000 colony-forming units per mL or greater.3–5 Use of lower colony counts in symptomatic patients has been advocated, 6 although this has not been included in established guidelines.
4°F (38°C) was 9 percent.2 The reference standard for the diagnosis of UTI is a single organism cultured from a specimen obtained at the following concentrations: suprapubic aspiration specimen, greater than 1,000 colony-forming units per mL; catheter specimen, greater than 10,000 colony-forming units per mL; or clean-catch, midstream specimen, 100,000 colony-forming units per mL or greater.3–5 Use of lower colony counts in symptomatic patients has been advocated, 6 although this has not been included in established guidelines.
Common uropathogens include Escherichia coli (accounting for approximately 85 percent of UTIs in children), Klebsiella, Proteus, Enterobacter, Citrobacter, Staphylococcus saprophyticus, and Enterococcus.7 A systematic review found that renal parenchymal defects are identified in 3 to 15 percent of children within one to two years of their first diagnosed UTI.8 Long-term complications of UTI associated with renal scarring include hypertension, chronic renal failure, and toxemia in pregnancy. Long-term follow-up data are limited, although one Swedish study found that among patients who had renal scarring from pyelonephritis during childhood, 23 percent developed hypertension and 10 percent developed end-stage renal disease.9 However, more recent studies question the association between pyelonephritis and end-stage renal disease.10 Baseline abnormalities of the urogenital tract have been reported in up to 3.2 percent of healthy, screened infants.11 Additionally, obstructive anomalies are found in up to 4 percent and vesicoureteral reflux in 8 to 40 percent of children being evaluated for their first UTI. Children younger than two years may be at greater risk of parenchymal defects than older children.12
Long-term follow-up data are limited, although one Swedish study found that among patients who had renal scarring from pyelonephritis during childhood, 23 percent developed hypertension and 10 percent developed end-stage renal disease.9 However, more recent studies question the association between pyelonephritis and end-stage renal disease.10 Baseline abnormalities of the urogenital tract have been reported in up to 3.2 percent of healthy, screened infants.11 Additionally, obstructive anomalies are found in up to 4 percent and vesicoureteral reflux in 8 to 40 percent of children being evaluated for their first UTI. Children younger than two years may be at greater risk of parenchymal defects than older children.12
| Clinical recommendation | Evidence rating | References |
|---|---|---|
UTI should be suspected in patients with leukocyte esterase and nitrite present on dipstick testing, or with pyuria of at least 10 white blood cells per high-power field and bacteriuria on microscopy. | C | 13, 16 |
| In young children, urine samples collected with a bag are unreliable in the evaluation of UTI. | C | 17 |
| The recommended initial antibiotic for most children with UTI is trimethoprim/sulfamethoxazole (Bactrim, Septra). Alternative antibiotics include amoxicillin/clavulanate (Augmentin) or cephalosporins, such as cefixime (Suprax), cefpodoxime, cefprozil (Cefzil), or cephalexin (Keflex). | C | 10 |
| A two- to four-day course of oral antibiotics is as effective as a seven- to 14-day course in children with a lower UTI. A single-dose or single-day course is not recommended. | A | 19–21 |
Children with acute pyelonephritis can be treated effectively with oral antibiotics (e.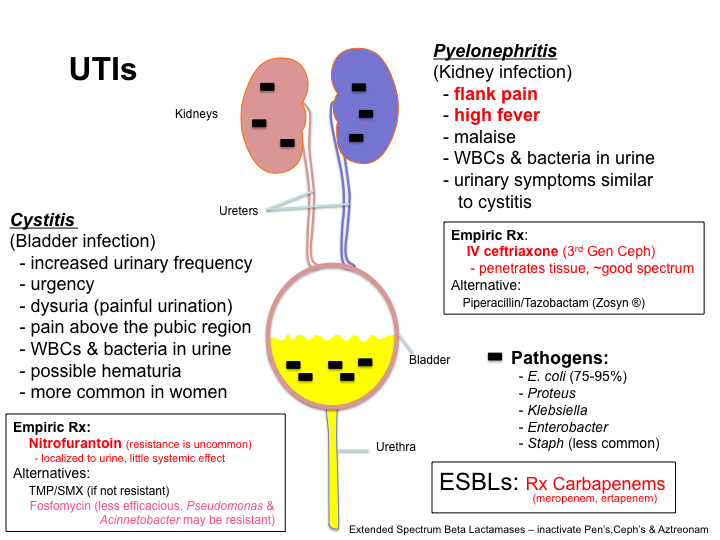 g., amoxicillin/clavulanate, cefixime, ceftibuten [Cedax]) for 10 to 14 days or with short courses (two to four days) of intravenous therapy followed by oral therapy. g., amoxicillin/clavulanate, cefixime, ceftibuten [Cedax]) for 10 to 14 days or with short courses (two to four days) of intravenous therapy followed by oral therapy. | A | 24 |
| Prophylactic antibiotics do not reduce the risk of recurrent UTIs, even in children with mild to moderate vesicoureteral reflux. | B | 25–27 |
| Routine circumcision in boys does not reduce the risk of UTI enough to justify the risk of surgical complications. | B | 32 |
Diagnosis
HISTORY AND PHYSICAL EXAMINATION
Clinical signs and symptoms of a UTI depend on the age of the child. Newborns with UTI may present with jaundice, sepsis, failure to thrive, vomiting, or fever. In infants and young children, typical signs and symptoms include fever, strong-smelling urine, hematuria, abdominal or flank pain, and new-onset urinary incontinence. School-aged children may have symptoms similar to adults, including dysuria, frequency, or urgency. Boys are at increased risk of UTI if younger than six months, or if younger than 12 months and uncircumcised. Girls are generally at an increased risk of UTI, particularly if younger than one year.3 Physical examination findings can be nonspecific but may include suprapubic tenderness or costovertebral angle tenderness.
School-aged children may have symptoms similar to adults, including dysuria, frequency, or urgency. Boys are at increased risk of UTI if younger than six months, or if younger than 12 months and uncircumcised. Girls are generally at an increased risk of UTI, particularly if younger than one year.3 Physical examination findings can be nonspecific but may include suprapubic tenderness or costovertebral angle tenderness.
DIAGNOSTIC TESTS
Dipstick tests for UTI include leukocyte esterase, nitrite, blood, and protein. Leukocyte esterase is the most sensitive single test in children with a suspected UTI. The test for nitrite is more specific but less sensitive. A negative leukocyte esterase result greatly reduces the likelihood of UTI, whereas a positive nitrite result makes it much more likely; the converse is not true, however. Dipstick tests for blood and protein have poor sensitivity and specificity in the detection of UTI and may be misleading. Accuracy of positive findings is as follows (assumes a 10 percent pretest probability)13:
Nitrite: 53 percent sensitivity, 98 percent specificity, 75 percent probability of UTI
Bacteria on microscopy: 81 percent sensitivity, 83 percent specificity, 35 percent probability of UTI
Leukocytes on microscopy: 73 percent sensitivity, 81 percent specificity, 30 percent probability of UTI
Leukocyte esterase: 83 percent sensitivity, 78 percent specificity, 30 percent probability of UTI
Leukocyte esterase or nitrite: 93 percent sensitivity, 72 percent specificity, 27 percent probability of UTI
Blood: 47 percent sensitivity, 78 percent specificity, 19 percent probability of UTI
Protein: 50 percent sensitivity, 76 percent specificity, 19 percent probability of UTI
All febrile children between two and 24 months of age with no obvious cause of infection should be evaluated for UTI, with the exception of circumcised boys older than 12 months..jpg) 14 Older children should be evaluated if the clinical presentation points toward a urinary source. The National Institute for Health and Clinical Excellence in the United Kingdom endorses incorporating specific strategies for urine testing based on the child's age (Figure 1).15 In this model, microscopy and urine culture should be performed in children younger than three years instead of dipstick testing. The presence of pyuria of at least 10 white blood cells per high-power field and bacteriuria are recommended as the criteria for diagnosing UTI with microscopy.16 In young children, urine samples collected with a bag are unreliable compared with samples collected with a catheter.17 Therefore, in a child who is unable to provide a clean-catch specimen, catheterization should be considered. If urine cannot be cultured within four hours of collection, the sample should be refrigerated.
14 Older children should be evaluated if the clinical presentation points toward a urinary source. The National Institute for Health and Clinical Excellence in the United Kingdom endorses incorporating specific strategies for urine testing based on the child's age (Figure 1).15 In this model, microscopy and urine culture should be performed in children younger than three years instead of dipstick testing. The presence of pyuria of at least 10 white blood cells per high-power field and bacteriuria are recommended as the criteria for diagnosing UTI with microscopy.16 In young children, urine samples collected with a bag are unreliable compared with samples collected with a catheter.17 Therefore, in a child who is unable to provide a clean-catch specimen, catheterization should be considered. If urine cannot be cultured within four hours of collection, the sample should be refrigerated.
Imaging procedures with the highest ratings from the American College of Radiology Appropriateness Criteria for further evaluation of select children with UTIs are renal and bladder ultrasonography, radionuclide cystography or voiding cystourethrography, and renal cortical scan. 18 Renal and bladder ultrasonography is effective for evaluating anatomy, but is unreliable for detecting vesicoureteral reflux. Radionuclide cystography or voiding cystourethrography is effective for screening and grading vesicoureteral reflux, but involves radiation exposure and catheterization. Although voiding cystourethrography is suggested for either girls or boys, radionuclide cystography is suggested only for girls because voiding cystourethrography is needed for adequate anatomic imaging of the urethra and bladder in boys. A renal cortical scan (also called scintigraphy or DMSA scan) uses technetium and is effective for assessing renal scarring, but requires intravenous injection of radioisotope.
18 Renal and bladder ultrasonography is effective for evaluating anatomy, but is unreliable for detecting vesicoureteral reflux. Radionuclide cystography or voiding cystourethrography is effective for screening and grading vesicoureteral reflux, but involves radiation exposure and catheterization. Although voiding cystourethrography is suggested for either girls or boys, radionuclide cystography is suggested only for girls because voiding cystourethrography is needed for adequate anatomic imaging of the urethra and bladder in boys. A renal cortical scan (also called scintigraphy or DMSA scan) uses technetium and is effective for assessing renal scarring, but requires intravenous injection of radioisotope.
Long-term outcome studies have not been performed to determine the best initial imaging study in children diagnosed with UTI. Guidelines based on observational studies and expert opinion recommend that all boys, girls younger than three years, and girls three to seven years of age with a temperature of 101. 3°F (38.5°C) or greater receive cystography and ultrasonography with a first-time UTI.3 An optional imaging strategy for febrile children with UTI, especially those older than three years, is to first perform ultrasonography and a renal cortical scan. This strategy avoids bladder catheterization with cystography and minimizes radiation exposure if the results of the scan are normal. However, if pyelonephritis or cortical scarring is found on the renal cortical scan, cystography is indicated.3
3°F (38.5°C) or greater receive cystography and ultrasonography with a first-time UTI.3 An optional imaging strategy for febrile children with UTI, especially those older than three years, is to first perform ultrasonography and a renal cortical scan. This strategy avoids bladder catheterization with cystography and minimizes radiation exposure if the results of the scan are normal. However, if pyelonephritis or cortical scarring is found on the renal cortical scan, cystography is indicated.3
Observation without imaging should be considered in girls three years or older with a temperature less than 101.3° F and in all girls older than seven years.3 The family should share in the decision to perform imaging with the first UTI or delay imaging until the second UTI, if it occurs. Figure 2 is an algorithm for imaging strategies in children with UTI.3
DIFFERENTIAL DIAGNOSIS
Although fever may be the sole presenting symptom in children younger than 24 months, physical examination findings may point toward an alternative diagnosis, including otitis media, gastroenteritis, or upper respiratory tract infection.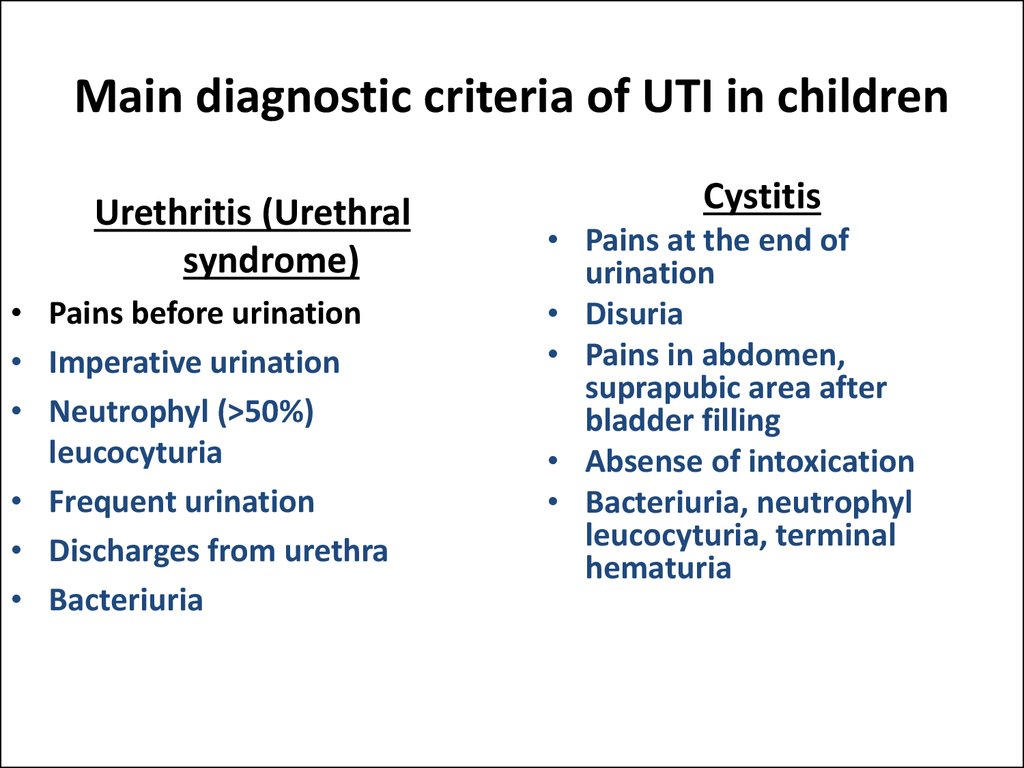 Occult bacteremia should always be considered, although the probability of this diagnosis is much lower than UTI (less than 1 versus 7 percent) in fully immunized children with no other identifiable potential source for fever on physical examination.4 Urinary calculi, urethritis (including a sexually transmitted infection), dysfunctional elimination, and diabetes mellitus must be considered in verbal children with urinary tract problems.
Occult bacteremia should always be considered, although the probability of this diagnosis is much lower than UTI (less than 1 versus 7 percent) in fully immunized children with no other identifiable potential source for fever on physical examination.4 Urinary calculi, urethritis (including a sexually transmitted infection), dysfunctional elimination, and diabetes mellitus must be considered in verbal children with urinary tract problems.
Treatment
Although amoxicillin has traditionally been a first-line antibiotic for UTI, increased rates of E. coli resistance have made it a less acceptable choice, and studies have found higher cure rates with trimethoprim/sulfamethoxazole (Bactrim, Septra). Other choices include amoxicillin/clavulanate (Augmentin) or cephalosporins, such as cefixime (Suprax), cefpodoxime, cefprozil (Cefzil), or cephalexin (Keflex).10Table 1 lists commonly used antibiotics, with dosing information and adverse effects. Physicians should be aware of local bacterial resistance patterns that might affect antibiotic choices.
| Antibiotic | Dosing | Common adverse effects |
|---|---|---|
| Amoxicillin/clavulanate (Augmentin) | 25 to 45 mg per kg per day, divided every 12 hours | Diarrhea, nausea/vomiting, rash |
| Cefixime (Suprax) | 8 mg per kg every 24 hours or divided every 12 hours | Abdominal pain, diarrhea, flatulence, rash |
| Cefpodoxime | 10 mg per kg per day, divided every 12 hours | Abdominal pain, diarrhea, nausea, rash |
| Cefprozil (Cefzil) | 30 mg per kg per day, divided every 12 hours | Abdominal pain, diarrhea, elevated results on liver function tests, nausea |
| Cephalexin (Keflex) | 25 to 50 mg per kg per day, divided every 6 to 12 hours | Diarrhea, headache, nausea/vomiting, rash |
| Trimethoprim/sulfamethoxazole (Bactrim, Septra) | 8 to 10 mg per kg per day, divided every 12 hours | Diarrhea, nausea/vomiting, photosensitivity, rash |
A Cochrane review analyzing short-duration (two to four days) versus standard-duration (seven to 14 days) oral antibiotics in 652 children with lower UTIs found no significant difference in positive urine cultures between the therapies immediately after treatment (eight studies: relative risk = 1. 06; 95% confidence interval, 0.64 to 1.76) or 15 months after treatment (10 studies: relative risk = 0.95; 95% confidence interval, 0.70 to 1.29). There was also no significant difference between short- and standard-duration therapies in the development of resistant organisms at the end of treatment.19 Thus, a two- to four-day course of oral antibiotics appears to be as effective as a seven- to 14-day course in children with lower UTIs.19 A single-dose or single-day course may be less effective than longer courses of oral antibiotics and is not recommended.20,21
06; 95% confidence interval, 0.64 to 1.76) or 15 months after treatment (10 studies: relative risk = 0.95; 95% confidence interval, 0.70 to 1.29). There was also no significant difference between short- and standard-duration therapies in the development of resistant organisms at the end of treatment.19 Thus, a two- to four-day course of oral antibiotics appears to be as effective as a seven- to 14-day course in children with lower UTIs.19 A single-dose or single-day course may be less effective than longer courses of oral antibiotics and is not recommended.20,21
When the presenting symptoms are nonspecific for a UTI or the urine dipstick test is nondiagnostic, there may be a delay in treatment while culture results are pending. Parents can be reassured that antibiotics initiated 24 hours after the onset of fever are not associated with a higher risk of parenchymal defects than immediate antibiotics in children younger than two years.22 However, delaying antibiotics by four days or more may increase the risk of renal scarring. 8
8
Fluoroquinolones are not usually used in children because of potential concerns about sustained injury to developing joints, although there is no compelling evidence supporting the occurrence of this phenomenon. Fluoroquinolones may be useful when infection is caused by multidrug-resistant pathogens for which there is no safe and effective alternative, parenteral therapy is not feasible, and no other effective oral agent is available. Guidelines from the American Academy of Pediatrics recommend limiting fluoroquinolone therapy to patients with UTIs caused by Pseudomonas aeruginosa or other multidrug-resistant, gram-negative bacteria.23 Ciprofloxacin (Cipro) is approved by the U.S. Food and Drug Administration for complicated UTIs and pyelonephritis attributable to E. coli in patients one to 17 years of age.23
A Cochrane review concluded that children with acute pyelonephritis can be treated effectively with oral antibiotics (e. g., amoxicillin/clavulanate, cefixime, ceftibuten [Cedax]) for 10 to 14 days or with short-courses (two to four days) of intravenous therapy followed by oral therapy. If intravenous therapy is used, single daily dosing with aminoglycosides is safe and effective. Studies are needed to determine the optimal duration of intravenous therapy in children with acute pyelonephritis, but 10 to 14 days is typical.24 Hospitalization should be considered for any child that is unable to tolerate oral intake or when the diagnosis is uncertain in a markedly ill child.
g., amoxicillin/clavulanate, cefixime, ceftibuten [Cedax]) for 10 to 14 days or with short-courses (two to four days) of intravenous therapy followed by oral therapy. If intravenous therapy is used, single daily dosing with aminoglycosides is safe and effective. Studies are needed to determine the optimal duration of intravenous therapy in children with acute pyelonephritis, but 10 to 14 days is typical.24 Hospitalization should be considered for any child that is unable to tolerate oral intake or when the diagnosis is uncertain in a markedly ill child.
Follow-up assessment to confirm an appropriate clinical response should be performed 48 to 72 hours after initiating antimicrobial therapy in all children with UTI. Culture and susceptibility results may indicate that a change of antibiotic is necessary. If expected clinical improvement does not occur, consider further evaluation (e.g., laboratory studies, imaging, consultation with subspecialists). Referral to a subspecialist is indicated if vesicoureteral reflux, renal scarring, anatomic abnormalities, or renal calculi are discovered, or if invasive imaging procedures are considered.
Prevention
In an observational study of otherwise healthy children with a first UTI, antibiotic prophylaxis was not associated with a reduced risk of recurrent UTI and increased the risk of treatment-resistant pathogens.25 A randomized controlled trial of children two months to seven years of age found that prophylactic antibiotics for 12 months following a febrile UTI did not reduce the risk of subsequent UTI, even in children with mild to moderate vesicoureteral reflux.26 Another randomized controlled trial of children and adolescents with pyelonephritis found that antibiotic prophylaxis did not prevent subsequent UTIs in patients with no documented vesicoureteral reflux or with mild to moderate vesicoureteral reflux.27 Antibiotic prophylaxis may be more beneficial in children with more severe vesicoureteral reflux, however.28 The most recent Cochrane review on the subject concluded that large, properly randomized, double-blind studies are needed to determine the effectiveness of long-term antibiotics for the prevention of UTI in susceptible children. 1 Additionally, continuous antibiotic prophylaxis in children younger than two and a half years with vesicoureteral reflux may not decrease the risk of pyelonephritis or renal damage.29
1 Additionally, continuous antibiotic prophylaxis in children younger than two and a half years with vesicoureteral reflux may not decrease the risk of pyelonephritis or renal damage.29
Constipation should be addressed in infants and children who have had a UTI to help prevent subsequent infections.30 There is some evidence that cranberry juice decreases symptomatic UTIs over 12-months, particularly in women with recurrent UTIs.31 The effectiveness of cranberry juice in children is less certain, and the high dropout rate in studies indicates that cranberry juice may not be acceptable for long-term prevention. A systematic review concluded that routine circumcision in boys does not reduce the risk of UTI enough to justify the risk of surgical complications.32
Medical advice for doctors | Remedium.ru
11/17/2022
Protracted bacterial bronchitis: new aspects of the problem based on clinical recommendations of the Ministry of Health of the Russian Federation
IU Taranushenko 1 , S. O. Falaleeva 1 , T.A. Gerasimova 2 ; 1 Krasnoyarsk State Medical University named after Professor V.F. Voino-Yasenetsky, 2 Research Institute of Medical Problems of the North
O. Falaleeva 1 , T.A. Gerasimova 2 ; 1 Krasnoyarsk State Medical University named after Professor V.F. Voino-Yasenetsky, 2 Research Institute of Medical Problems of the North
In world pediatric practice, prolonged bacterial...
More
11/14/2022
Personalized targeted therapy of severe bronchial asthma in combination with polypous rhinosinusitis
I.V. Demko 1.2 , E.A. Sobko 1.2 , N.A. Shestakova 1.2 , A.Yu. Kraposhina 1.2 ; 1 Krasnoyarsk State Medical University im. prof. V.F. Voyno-Yasenetsky, 2 Regional Clinical Hospital (Krasnoyarsk)
Bronchial asthma (BA) is an urgent public health problem due to the high prevalence and heterogeneity of the disease. Development and implementation in clinical...
Development and implementation in clinical...
More
11/10/2022
Cervical caries - symptoms and treatment
Dental caries is a biofilm-mediated multifactorial dynamic disease leading to phasic demineralization and remineralization of dental hard tissues. Caries can occur throughout life, both in milk and permanent teeth, can damage the crown of the tooth, ...
More
09.11.2022
Mannitol inhalation for children with cystic fibrosis: efficacy and safety
O.I. Simonova 1,2,3 * , Yu.V. Gorinova 1 , O.V. Vysokolova 3 , M.A. Mukhina 3 , E.E. Yakushina 3 ; 1 National Medical Research Center for Children's Health Sechenov (Sechenov University), . ..
..
More
07.11.2022
Multifaceted properties of erdosteine and its place in the treatment of diseases of the respiratory tract
VV Salukhov, A.V. Nikolaev, V.V. Ivanov, M.A. Zhurkin, A.A. Chugunov, D.A. Marchenko; Military Medical Academy named after S.M. Kirova
Mucoactive drugs are commonly used in the treatment of respiratory diseases such as chronic bronchitis (CB) or chronic obstructive pulmonary disease (COPD),...
More
03.11.2022
New principles for the treatment of chronic heart failure: the phenomenon of sodium-glucose cotransporter type 2 inhibitors
S. G. Kanorsky ; Kuban State Medical University
Chronic heart failure (CHF) is one of the most important problems in clinical cardiology due to high morbidity, frequent hospitalizations and poor prognosis of patients. Quite unexpected...
Quite unexpected...
More
01.11.2022
Clinical and allergological characteristics of chronic inflammatory diseases of the nose in patients with severe bronchial asthma receiving immunobiological therapy in the Sverdlovsk region
A.V. Kiseleva, E.K. Beltyukov, V.V. Naumova ; Ural State Medical University
Introduction . Allergic rhinitis, chronic rhinosinusitis (with/without polyps) are chronic inflammatory diseases of the nose and often accompany bronchial asthma, exacerbating...
More
31.10.2022
Sudden cardiac death due to complicated peripartum cardiomyopathy in combination with long QT syndrome and a mutation in the FLNC gene
E. V. Reznik 1.2 , A.A. Yasnovskaya 1 , E.M. Yadrov 1 , S.V. Borisovskaya 3 ; 1 Russian National Research Medical University im. N.I. Pirogova, 2 GKB No. 31 (Moscow), 3 GKB im. V.M. Buyanova
V. Reznik 1.2 , A.A. Yasnovskaya 1 , E.M. Yadrov 1 , S.V. Borisovskaya 3 ; 1 Russian National Research Medical University im. N.I. Pirogova, 2 GKB No. 31 (Moscow), 3 GKB im. V.M. Buyanova
Peripartum cardiomyopathy "diagnosis of exclusion" in women with systolic heart failure of unknown etiology that developed at the end of pregnancy or ...
More
28.10.2022
The use of resveratrol and indole-3-carbinol as an antiproliferative method for the prevention of HPV-associated diseases
K.I. Gusakov 1 * , N.M. Nazarova 1 , P.R. Abakarova 1 A.A. Tararykova 2 , I. A. Ivanov 1 ; 1 Academician National Medical Research Center for Obstetrics, Gynecology and Perinatology, 2 N.N. More
A. Ivanov 1 ; 1 Academician National Medical Research Center for Obstetrics, Gynecology and Perinatology, 2 N.N. More
21.10.2022
Some aspects of adherence to combined hormonal contraception in young women
I.G. Zhukovskaya, L.F. Khuzin; IGMA
Introduction. In addition to protecting against unwanted pregnancies, combined hormonal contraceptives (CHCs) can improve women's health and quality of life. The awareness of Russian women about CHC is 85%, however, only 13% of women in Russia have experience of a long...
More
Load more
Pediatric Urinary Tract Infections - Symptoms, Diagnosis and Treatment
Sign In or Subscribe to Full Access to BMJ Best Practice
Last Viewed: 17 October 2022
Last updated: 10 August 2021
Urinary tract infections (UTIs) are common in children. Symptoms and signs may be non-specific, especially in neonates and infants. Older children may have dysuria, urinary urgency or frequent urination with lower urinary tract infection, as well as fever, lower back or back pain, and vomiting in pyelonephritis.
Symptoms and signs may be non-specific, especially in neonates and infants. Older children may have dysuria, urinary urgency or frequent urination with lower urinary tract infection, as well as fever, lower back or back pain, and vomiting in pyelonephritis.
A correctly collected urinalysis confirms the diagnosis and identifies the pathogen; an antibiotic suitable for treatment is selected according to bacteriological examination of urine with antimicrobial sensitivity.
Anatomical and functional disorders of the urinary tract and intestines may predispose children to recurrent UTIs. Further evaluation of children with recurrent UTIs is required to identify a treatable underlying cause. Recurrent UTIs can lead to scarring of the kidney tissue and kidney failure.
Definition
A urinary tract infection in children (UTI) is a disease caused by an infection in the lower urinary tract (cystitis), upper urinary tract (pyelonephritis), or both. The presence of pyuria and symptoms distinguishes UTI from asymptomatic bacteriuria.[1]American Academy of Pediatrics. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011 Sep;128(3):595-610. http://pediatrics.aapplications.org/content/128/3/595.long http://www.ncbi.nlm.nih.gov/pubmed/21873693?tool=bestpractice.com
The presence of pyuria and symptoms distinguishes UTI from asymptomatic bacteriuria.[1]American Academy of Pediatrics. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011 Sep;128(3):595-610. http://pediatrics.aapplications.org/content/128/3/595.long http://www.ncbi.nlm.nih.gov/pubmed/21873693?tool=bestpractice.com
Asymptomatic bacteriuria is the presence of bacteria in the urine collected from children without clinical symptoms at routine screening or incidentally detected during other studies. The prevalence of asymptomatic bacteriuria is 0.37% in boys and 0.47% in girls, with the highest rates in uncircumcised boys under 1 year of age and girls over 2 years of age.[2]Shaikh N, Osio VA, Wessel CB, et al. Prevalence of asymptomatic bacteriuria in children: a meta-analysis. J Pediatr. 2020 Feb;217:110-7. http://www.ncbi.nlm.nih.gov/pubmed/31787323?tool=bestpractice. com Asymptomatic bacteriuria does not require treatment.[3] Fitzgerald A, Mori R, Lakhanpaul M. Interventions for covert bacteriuria in children. Cochrane Database Syst Rev. 2012 Feb 15;(2):CD006943. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006943.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/22336827?tool=bestpractice.com
com Asymptomatic bacteriuria does not require treatment.[3] Fitzgerald A, Mori R, Lakhanpaul M. Interventions for covert bacteriuria in children. Cochrane Database Syst Rev. 2012 Feb 15;(2):CD006943. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006943.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/22336827?tool=bestpractice.com
Uncomplicated UTI: UTI in a patient older than 2 months with a structurally and functionally normal urinary tract, normal renal function, and an uncompromised immune system.[4]European Association of Urology. Guidelines on pediatric urology. 2021 [internet publication]. https://uroweb.org/guideline/pediatric-urology
Complicated UTI: A UTI in a child who is: ≤2 months of age; or has a structural or functional abnormality of the urinary tract; or has impaired renal function; or systemically unwell (appears toxic, haemodynamically unstable, immunocompromised, cannot tolerate oral medications, or does not respond to oral medications).[4]European Association of Urology. Guidelines on pediatric urology. 2021 [internet publication]. https://uroweb.org/guideline/pediatric-urology [5] National Institute for Health and Care Excellence. Urinary tract infection in under 16s: diagnosis and management. October 2018 [internet publication]. https://www.nice.org.uk/guidance/cg54 [6] Leung AKC, Wong AHC, Leung AAM, et al. Urinary tract infection in children. Recent Pat Inflamm Allergy Drug Discov. 2019;13(1):2-18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6751349 http://www.ncbi.nlm.nih.gov/pubmed/30592257?tool=bestpractice.com
Guidelines on pediatric urology. 2021 [internet publication]. https://uroweb.org/guideline/pediatric-urology [5] National Institute for Health and Care Excellence. Urinary tract infection in under 16s: diagnosis and management. October 2018 [internet publication]. https://www.nice.org.uk/guidance/cg54 [6] Leung AKC, Wong AHC, Leung AAM, et al. Urinary tract infection in children. Recent Pat Inflamm Allergy Drug Discov. 2019;13(1):2-18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6751349 http://www.ncbi.nlm.nih.gov/pubmed/30592257?tool=bestpractice.com
History and examination
Key diagnostic factors
- presence of risk factors
- fever >39°C (>102.2°F)
- moodiness (newborns and infants) newborns and infants age)
- suprapubic tenderness
- costovertebral angle tenderness
More key diagnostic factors
Other diagnostic factors
- urine malodor (infants, older children and adolescents)
- dysuria (preschool age, older children13)
- urinary frequency (older children and adolescents)
- abdominal/flank pain (infants, older children and adolescents)
- vomiting
- Painful appearance (newborns)
- Gross hematuria (older children and adolescents)
- Newly diagnosed urinary incontinence (infants, older children and adolescents)
Other diagnostic factors
Risk factors age
- <
- female
- children of Caucasian ethnicity
- uncircumcised boys in the first year of life
- previous UTIs
- bladder dysfunction
Tests that are a priority
- test strips for urine tests
- microscopy of urine
- culture of urine
More tests that are recommended first
tests that need to be considered
- culture
- bacteriological examination of urine for fungi
- Serum creatinine, urea and electrolytes
- Explanes of the kidneys
- Scyinticgraphy with dimercaptosucinic acid (DMSK)
- Cystooretrogram with natural urination
- KT of the abdominal organs (with contrasting) of the abdominal organs (with contrasting) 9000 9000 9000 9000.