Types of abortions procedures
Abortion Types and Costs
An abortion is a medical procedure to end a pregnancy growing in the womb (uterus).
Surgical procedures to induce an abortion are done in clinics or hospitals. A medical abortion can end an early pregnancy at home with prescription medicine – usually mifepristone (RU-486) followed by misoprostol. The type of abortion you get will probably depend almost entirely on how far you are along in your pregnancy.
If you’re in your first trimester, you’ll likely have a vacuum aspiration. If you’re in your second trimester (meaning that it’s been more than 13 weeks since your last menstrual period), you’ll likely have a dilation and evacuation, or D&E. If you’re further along than that, you might have a dilation and extraction, or D&X.
Almost all abortion procedures are outpatient, which means you won’t have to stay overnight in the doctor’s office, clinic, or hospital.
Is Abortion Common?
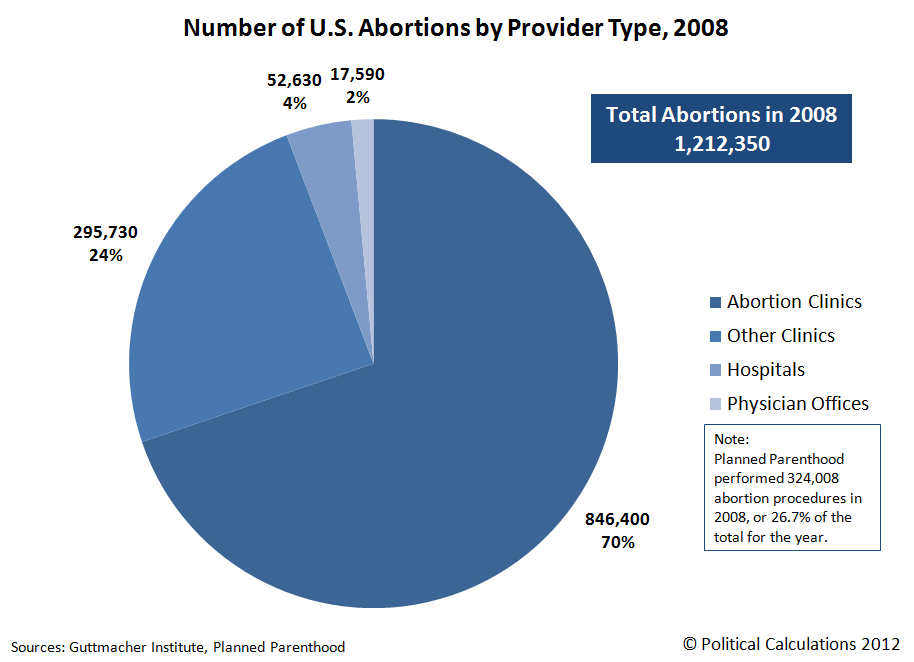
It’s reportedly been common. In 2017, the Guttmacher Institute estimated that close to 1 in 4 women in the U. S. would have an abortion by the age of 45.
In 2019, the CDC received reports of over 625,000 legal induced abortions. That year, the abortion rate was 11.4 abortions per 1,000 women 15 to 44 years old. More than half of the women who got these abortions were in their 20s, usually during or before their 13th week of pregnancy.
Is Abortion Safe?
In general, abortion is very safe. It comes with small risks, like any medical procedure does.
If you want a surgical abortion, you need to go to a doctor or a nurse with special training in a clinic or hospital. It can be very dangerous to try and end a pregnancy on your own.
If you want to have a medication abortion at home, it’s important to have access to accurate information, reliable abortion medications, and safe, nonjudgmental, and supportive care within the formal medical system in case you need it.
Where Can You Get a Legal Abortion?
It mainly depends on where you live. Restrictions on surgical and medication abortions vary by state. Doctors who provide abortions are required to follow the laws of the states where they’re licensed to practice medicine. If they don’t, they could risk losing their license or facing criminal or civil penalties.
Doctors who provide abortions are required to follow the laws of the states where they’re licensed to practice medicine. If they don’t, they could risk losing their license or facing criminal or civil penalties.
If you’re not sure what your state’s abortion laws are, you could consider using the state-by-state guide on AbortionFinder.org, which has other helpful resources, too.
Before the Procedure
When you schedule your appointment, your health care provider will probably give you some instructions over the phone. Because in-clinic abortions are considered surgeries, you may have to fast starting around midnight the night before your procedure.
When you arrive at the clinic, you’ll fill out some paperwork and answer questions about your medical history. You’ll then get a pre-abortion workup, which includes a physical examination, pregnancy test, blood test, screening for sexually transmitted infections, and possibly additional testing, if your case warrants it.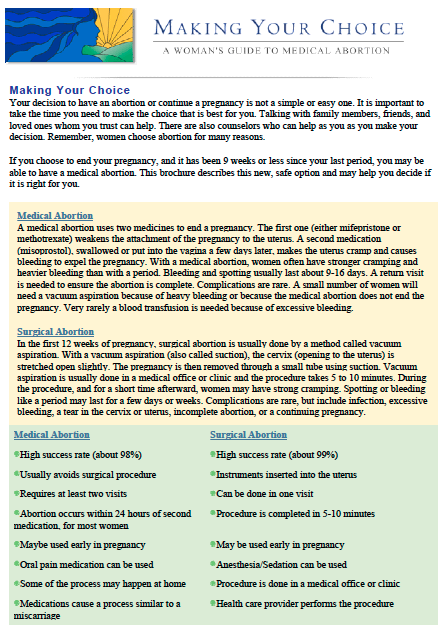 Many providers will also use an ultrasound to confirm how far along you are in your pregnancy and check for uterine, fetal, or placental abnormalities.
Many providers will also use an ultrasound to confirm how far along you are in your pregnancy and check for uterine, fetal, or placental abnormalities.
All of this information, which your doctor will discuss with you during a short counseling session, will help them determine which procedure is right for you.
Some states require you to get this counseling in person instead of over the phone or a video call. And lots of states require you to wait a certain amount of time after the counseling session until you get your abortion, although there’s no medical reason for this. Depending on the state, this waiting period could be from 18 to 72 hours. If you’re having a medical emergency or your life or health is in danger, states waive the waiting period requirements.
Pain Management
Your doctor will also talk to you about different types of pain management available to you during the procedure.
For an in-clinic abortion, you’ll probably get local anesthesia, meaning that your cervix will be numbed but you’ll be awake. While 600 to 800 milligrams of ibuprofen usually provides enough pain relief, your doctor might also offer you an oral medication to calm you down or mildly sedate you, so you’re awake but relaxed. If you prefer heavy sedation, meaning you’re in a light sleep throughout the procedure, you can ask if a sedative medication can be given to you through an IV.
While 600 to 800 milligrams of ibuprofen usually provides enough pain relief, your doctor might also offer you an oral medication to calm you down or mildly sedate you, so you’re awake but relaxed. If you prefer heavy sedation, meaning you’re in a light sleep throughout the procedure, you can ask if a sedative medication can be given to you through an IV.
Vacuum Aspiration (Suction Abortion)
Most abortions done in the U.S. take place in the first 12 to 13 weeks of pregnancy. If you opt for an in-clinic abortion in your first trimester, you’ll have a vacuum aspiration, which you may also hear called a “suction abortion.”
In most cases, your cervix doesn’t need to be prepped or dilated for this procedure. But if you’re more than about 10 to 12 weeks pregnant, your health care provider may take steps to open your cervix a bit before getting started so that the medical tools can access your uterus. They’ll likely insert little sticks made of sterilized seaweed that absorb moisture and expand, called laminaria.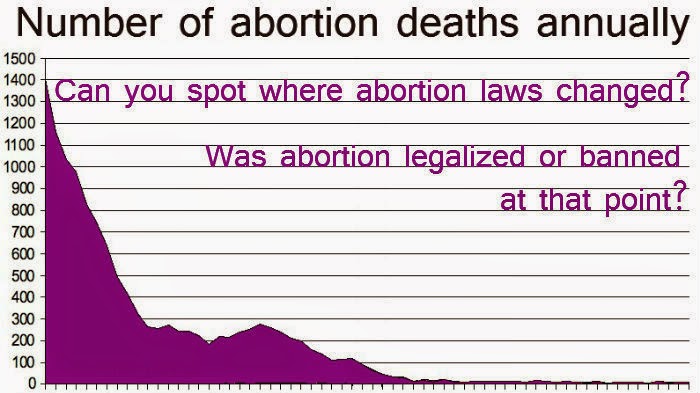
Once you’re ready for the procedure, your health care provider will have you lie on an exam table with your feet in stirrups, like you’re having a pelvic exam.
When you’re comfortable and sedated, if you so choose, your health care provider will insert a medical tool called a speculum into your vagina to keep it open, and swab your vagina and cervix with an antiseptic solution called Betadine.
They’ll inject an anesthetic into the cervix to numb it, holding your cervix in place with a grasping instrument. They’ll then insert a small tube attached to either a hand-held syringe or a suction machine into your uterus, and clear out its contents. From start to finish, the procedure takes several minutes.
Afterward, your doctor will check to make sure that the procedure was successful, and then let you rest for about 30 minutes under observation.
Second Trimester: Dilation and Evacuation
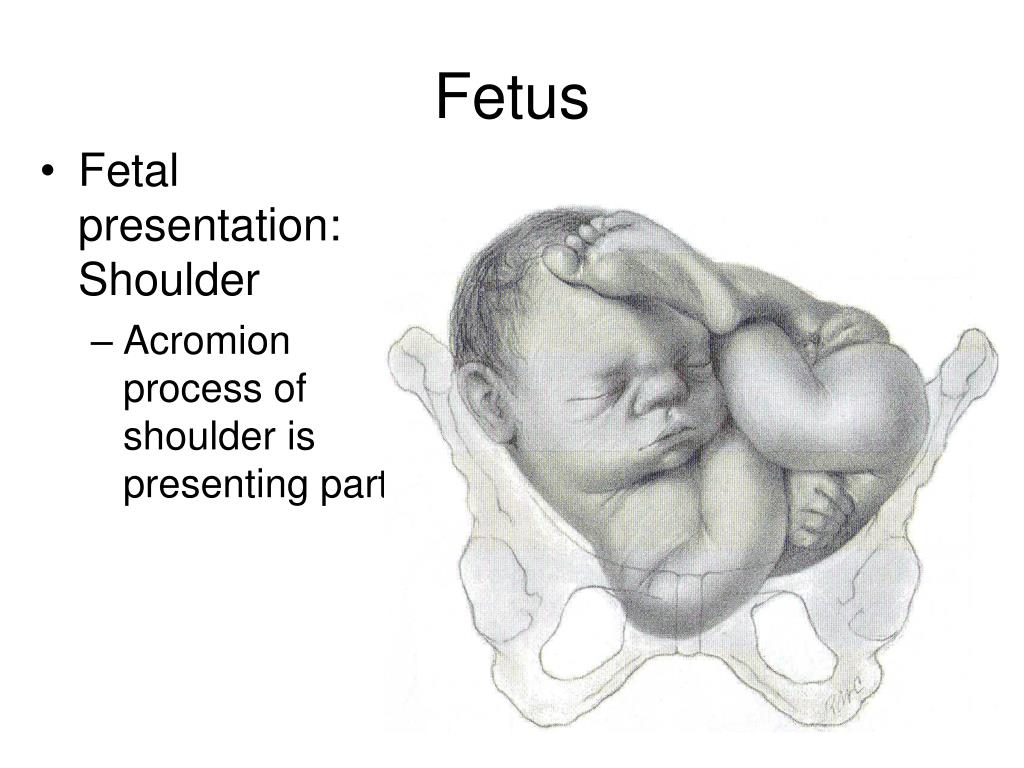
If you’re more than 12 weeks pregnant, your provider will use an ultrasound to date your pregnancy. The farther along you are, the more prep work you may have to undergo to prepare your body for the procedure.
The farther along you are, the more prep work you may have to undergo to prepare your body for the procedure.
While doctors can do vacuum aspirations until about 14 weeks, the most common type of second-trimester abortion is called dilation and evacuation, or D&E.
The first step a provider will take before this procedure is to prepare and dilate your cervix so that it’s not injured in the procedure. They will likely use laminaria sticks, which might be left in overnight. They might also give you a dose of a medication such as misoprostol, either by mouth or through your vagina, to soften your uterus. They may also use tools to help dilate your cervix.
Like a first-trimester abortion, you’ll lie on an exam table with your feet in stirrups, and your health care provider will swab your vagina and cervix with Betadine, inject anesthesia into your cervix, and then use a gripping tool to hold your cervix in place.
The main difference is that in addition to using a vacuum suction in your uterus, they’ll also use forceps and other medical tools, including one called a curette to scrape the inside of your uterus.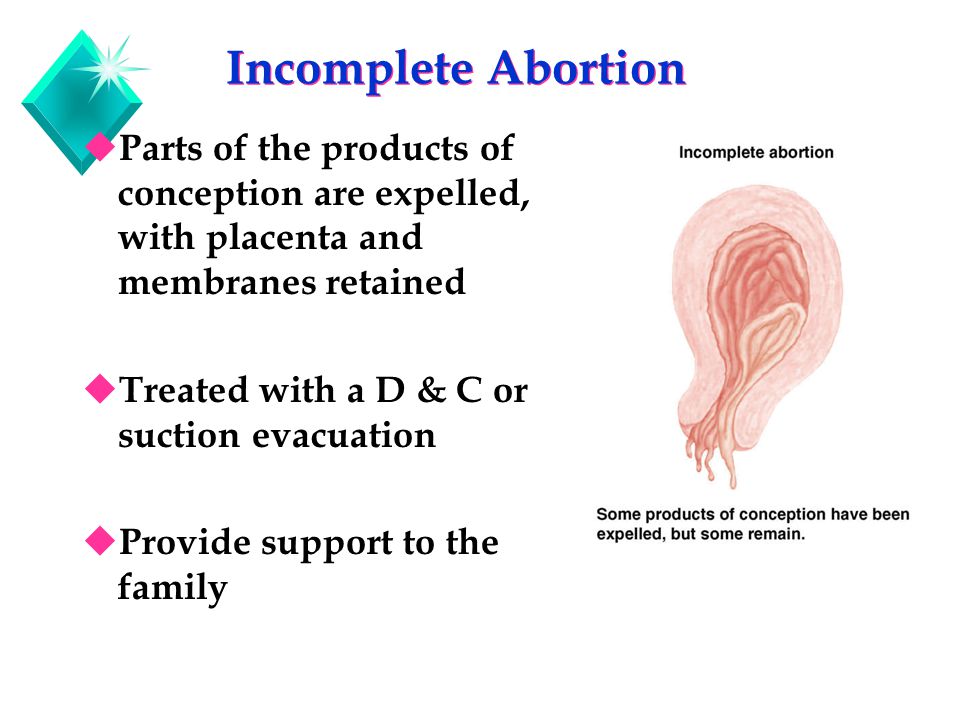 Your doctor may use ultrasound to guide them, and will likely use a suction or vacuum to make sure everything is cleared out. Some providers may use a medication, which you would get as a shot into your abdomen, to stop the fetal heartbeat before the procedure. Afterward, your provider may give you a medication to contract your uterus and reduce bleeding.
Your doctor may use ultrasound to guide them, and will likely use a suction or vacuum to make sure everything is cleared out. Some providers may use a medication, which you would get as a shot into your abdomen, to stop the fetal heartbeat before the procedure. Afterward, your provider may give you a medication to contract your uterus and reduce bleeding.
This procedure takes 10 to 20 minutes. You’ll rest for 30 minutes to an hour while your health care providers make sure you’re well.
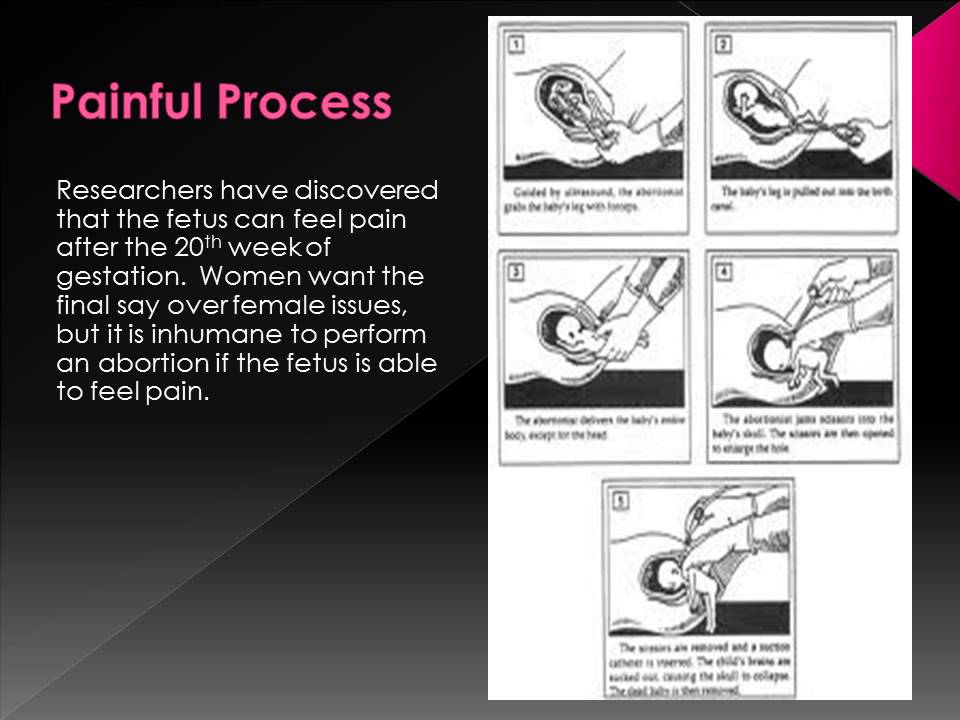
Late-Term Abortion: Dilation and Extraction
If you’re having an abortion further along in your pregnancy, you may have to find a specialized, experienced provider to do a dilation and extraction procedure, or D&X. This is a procedure that doctors usually reserve for when there is a serious problem with the fetus or medical complications related to the mother.
All the steps leading up to the procedure and steps taken after the procedure are the same as for a D&E, including the ultrasound to date your pregnancy and prep work to soften and dilate your cervix.
For sedation, you might be offered a general IV anesthesia, especially if the procedure is done in a hospital.
There are a few other options, like labor induction, hysterotomy and hysterectomy. But because they are riskier, doctors only do them if medically necessary.
How Much Does an Abortion Cost?
The amount may depend on how many weeks pregnant you are, if you get anesthesia or sedation for pain or discomfort, your financial situation, and where you get the procedure. Many clinics offer free or sliding-scale payment options based on how much money you make. To explore these options, look into your local Planned Parenthood or other women’s health clinics.
Generally, without other help, you can expect to pay anywhere from:
- $430 to $600 if you’re 4 to 12 weeks from your last menstrual period (LMP)
- $540 to $1,100 if you’re 13 to 16 weeks from your LMP
- $900 to $1,850 if you’re 17 to 21 weeks from your LMP
Suction termination (also called suction curettage or vacuum aspiration abortion) may range around $500 to $700. Dilation and evacuation abortions, which are usually for later-stage pregnancies, range from $800 to $2,500. But in some areas, these prices could be as little as $300. In other cases, they may be more expensive depending on your medical needs.
Dilation and evacuation abortions, which are usually for later-stage pregnancies, range from $800 to $2,500. But in some areas, these prices could be as little as $300. In other cases, they may be more expensive depending on your medical needs.
If you get conscious sedation as opposed to local anesthetic, your cost may be on the higher end.
If you’re 5-10 weeks pregnant, you can use the abortion pill to end a pregnancy. It usually costs about $500 to $1,500.
Paying for Abortions
In some states, you may only be able to get an abortion if you get pregnant because of rape, incest, or if the pregnancy threatens your life. In these situations, you may be able to receive financial help from the government. The facility that does your abortion will need to apply for government funds in these cases. Ask your provider to complete an application if you need financial help.
If you have Medicaid, you can get financial help for an abortion. Some states, including California, Colorado, Connecticut, Delaware, and New Jersey, also choose to use their funds to help people with abortion costs.
If you have insurance, abortions might be covered, depending on the rules of the state you’re insured in. Some states have stricter rules than others. If your insurance covers your abortion, it may be free. In some situations, you may have to pay a copay, just like with other medical procedures.
For example, Texas only allows abortion coverage if the pregnancy could severely threaten your health or life.
If you need a low-cost or free abortion, there are organizations that can help. You can find more information at:
- The National Abortion Federation: Visit prochoice.org or call 800-772-9100.
- Planned Parenthood: Visit plannedparenthood.org or call 800-230-7526.
- National Network of Abortion Funds: Visit abortionfunds.org to find local organizations that can offer financial help.
What Happens Next?
Once your procedure is done, you’ll rest at the clinic under supervision for about 30 minutes. You can then continue to relax in a recovery area until you’re ready to head home. If you’ve had any sedation, you’ll need someone to drive you. You’ll get a prescription for an antibiotic, too.
If you’ve had any sedation, you’ll need someone to drive you. You’ll get a prescription for an antibiotic, too.
You’ll probably have some cramping for a few days and light bleeding for up to 2 weeks. Most pain and cramping is effectively treated with an over the counter or prescription painkiller like acetaminophen, ibuprofen, or codeine.
Plan to rest on the day of your procedure. You may need a few more days of rest if you had a D&E or D&X. You shouldn’t lift anything heavy for a few days. Ask your doctor when it would be OK to have sex or use a tampon again -- it may be up to a month before you can have anything in your vagina.
If you have severe pain, a fever over 100 F, or soak through more than two pads per hour, you should call your provider or the emergency contact they gave you right away.
Most providers will have you come back for a follow-up appointment in 1 to 4 weeks to make sure that you’ve physically recovered and are no longer pregnant.
Does Abortion Affect Your Fertility?
If a trained health care provider safely gives you a surgical abortion, it shouldn’t cause you to have trouble getting pregnant in the future if you decide to have a baby. There’s an exception to this that’s linked to getting more than one surgical abortion in which the doctor uses an instrument called a curette. This could raise the chances for scarring of the inner lining of your womb, a condition called Asherman syndrome. That condition is tied to having a harder time getting pregnant later.
There’s an exception to this that’s linked to getting more than one surgical abortion in which the doctor uses an instrument called a curette. This could raise the chances for scarring of the inner lining of your womb, a condition called Asherman syndrome. That condition is tied to having a harder time getting pregnant later.
What Is a Spontaneous Abortion?
It’s a medical term for miscarriage. It’s not a procedure like a surgical or a medical abortion.
Doctors also use a term called “missed abortion” to mean that there is a fetus in the womb but it no longer has a heartbeat.
Why Do People Get Abortions?
You might want or need an abortion for any number of reasons. For example, you might:
- Get pregnant by accident and decide you don’t want to have a baby
- Not have enough money or time to raise a child
- Not have the support of a partner or relative and decide you don’t want to raise a child by yourself
- Have personal problems with your partner
- Learn the unborn baby has a serious health problem
- Have a health problem of your own that makes pregnancy unsafe
By Trimester, What to Expect, and Resources
If you’re considering an abortion, it’s a good idea to familiarize yourself with the various methods to determine the best and most accessible choice for you.
The two main types of abortion are medical and surgical. Both are extremely safe and effective.
However, one might be preferable depending on how long you’ve been pregnant, where you live, your budget, and a few other factors.
Since the Supreme Court of the United States voted to overturn Roe v. Wade, which guaranteed the legal right to abortion nationwide, some states have already passed laws restricting access to abortion. Others are poised to follow suit.
That means not everyone has equal access to all methods of abortion, and you might face some challenges accessing one, depending on where you live.
Stay informed
The information in this article was accurate and up to date at the time of publication, but it’s possible the information has changed since. To learn more about your legal rights, you can message the Repro Legal Helpline via a secure online form or call 844-868-2812.
According to reproductive health research, more than half of all abortions in the United States are medical abortions.
Medical abortion involves taking pills that terminate a pregnancy. You’ll most likely take a mifepristone pill followed by another medication called misoprostol, though some people will only take misoprostol.
These medications stop the pregnancy from continuing to develop and cause the uterus to empty itself, ending the pregnancy.
Abortion pills are FDA-approved for ending a pregnancy up to 10 weeks, but they’re also used off-label later than this in some states.
In most states, you can legally obtain abortion pills from a provider in person or through a provider-staffed telehealth platform. This is what’s known as “clinician-supported” medication abortion.
Most people can also order abortion pills online and take them at home without working with a provider. This is called a “self-managed” abortion, and it’s just as safe and effective as clinician-supported abortion.
Learn more about medical abortion here.
Safety, side effects, and risks
Most medical experts agree that abortion — whether medical or surgical — is safe.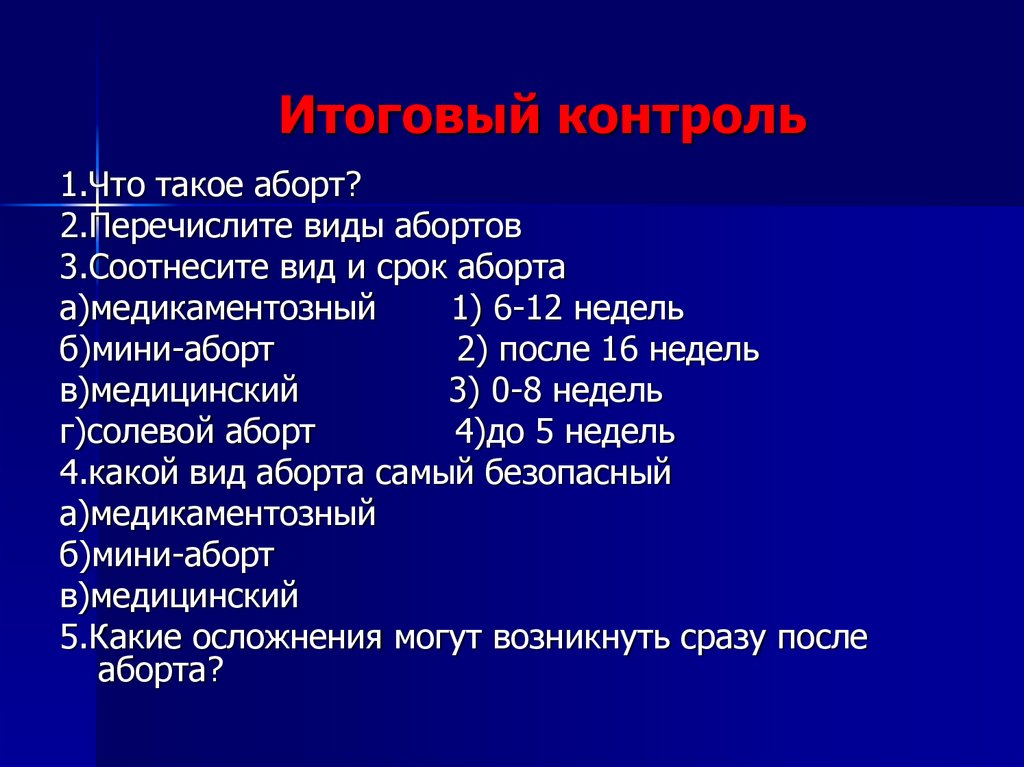 No more than 2% of people report complications, and most complications that do occur are easily treated with follow-up care.
No more than 2% of people report complications, and most complications that do occur are easily treated with follow-up care.
There are some side effects that many or even most people will experience, though. The most common side effect of medical abortion is heavy bleeding that lasts for a few days.
You can also expect cramping that may be more painful than menstrual cramps. It shouldn’t be severe, though — anything that feels concerning or unbearable is a good reason to call a healthcare professional.
Cramping and bleeding are natural parts of the process because abortion pills cause your uterus to contract and expel the pregnancy tissue. Moderate pain, while uncomfortable, is usually a sign that your medication is working.
The worst of the pain and bleeding will happen within the first few hours, but lesser cramps and spotting can linger for several weeks.
Some people also experience symptoms like nausea, diarrhea, vomiting, breast tenderness, and fatigue.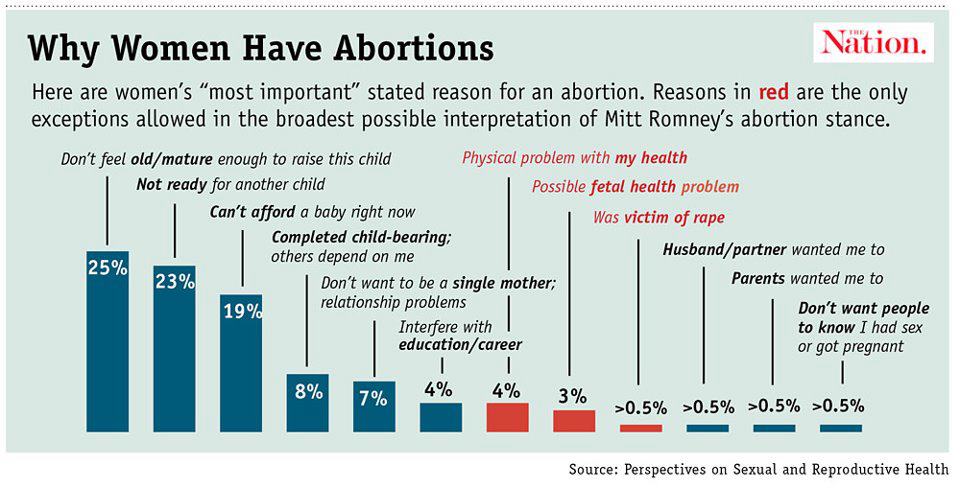 Most of these should resolve within 24 hours to a few days.
Most of these should resolve within 24 hours to a few days.
Infection and incomplete abortion (when some pregnancy tissue remains in the uterus after taking medication) are the main complications to watch for, but they’re rare.
Eligibility
While medical abortion is generally safe for most people, it’s not recommended for everyone. You may not be eligible if you:
- are experiencing an ectopic pregnancy (a non-viable pregnancy that is attempting to develop outside of the uterus)
- live with blood clotting disorders or anemia
- live with chronic adrenal failure
- have used steroid medicines over a long period of time
- live with inherited porphyrias (rare blood disorders)
- have an intolerance or allergy to mifepristone or misoprostol
You also shouldn’t use abortion pills if you have an intrauterine device (IUD). You’ll need to have it removed before taking the pills.
Efficacy
Medical abortion is an extremely effective way to end a pregnancy, especially when used at or before 12 weeks gestation.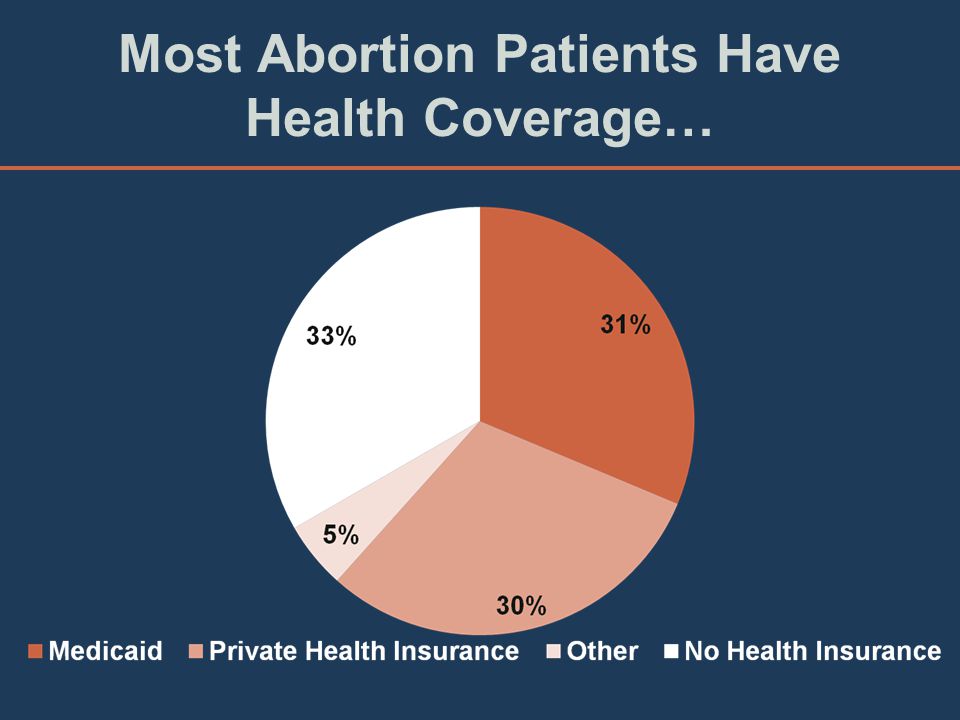
Research shows that the combination of mifepristone and misoprostol — the most common way to end an abortion via pills — fully ends pregnancy in 95–99% of cases.
Some people, especially people outside of the U.S., may only take misoprostol without mifepristone. This is also an effective abortion method, fully ending pregnancies in about 78% of people who take it.
More research is needed into the effectiveness of misoprostol alone. Some newer research suggests an even higher success rate, so the data is somewhat unclear for now.
Overall, both the combination of mifepristone with misoprostol and misoprostol alone are effective ways to have an abortion with pills.
Cost
One study found that the average price of mifepristone and misoprostol ordered online ranged from $110–$360, including shipping and fees. The cost of misoprostol by itself was lower.
According to Planned Parenthood, abortion pills obtained in a clinic can cost up to $750, though costs may vary by state.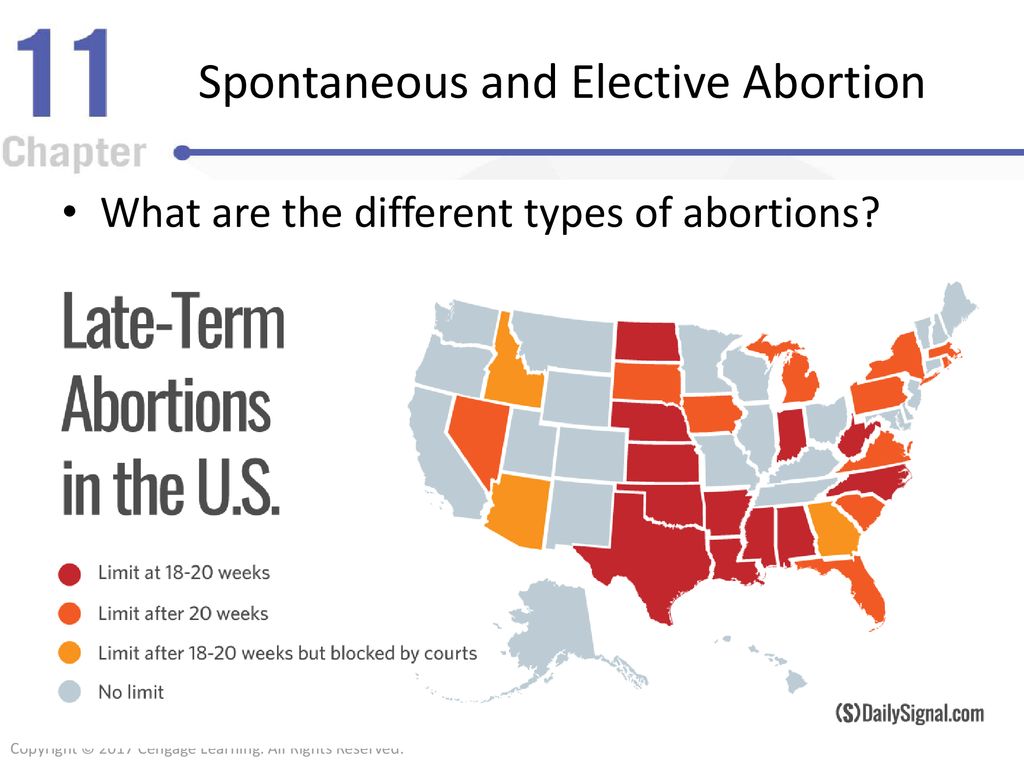
Access and legality
Many states have rushed to restrict or ban surgical abortion procedures since the fall of Roe v. Wade in June 2022. Limiting access to abortion medication is up next for plenty of states, and some have already moved to ban it.
In some areas, abortion providers and doctors cannot prescribe the medication for you in their clinic, especially if you have reached a certain point in pregnancy. You may have to order online.
Here’s what you need to know about telemedicine abortion in a post-Roe United States.
Resources for accessing medication abortion by mail include:
- AidAccess
- Plan C
- Hey Jane
- Abortion On Our Own Terms
- Carafem
- Just the Pill
Looking forward, states may not have much ability to limit access to abortion medication in the long term.
Attorney General Merrick Garland has said that states can’t ban abortion pills that are approved by the FDA.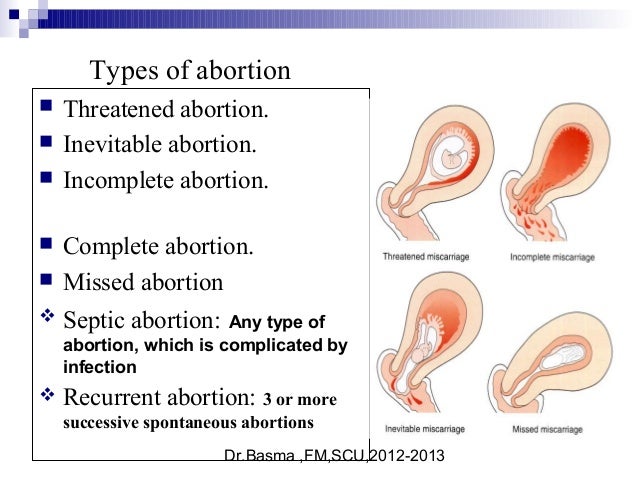 That means misoprostol, at least, could remain or become legally accessible in most states.
That means misoprostol, at least, could remain or become legally accessible in most states.
Plus, President Joe Biden directed the Department of Health and Human Services (HHS) to expand and protect access to abortion medication on the federal level.
It’s still unclear what that will look like, though, and you can expect many states to challenge any ruling that protects abortion access. It’s important to stay up-to-date on your state’s laws if you’re considering abortion.
Prioritize your privacy
There are legal risks to self-managed at-home medication abortion. Some states restrict access to telehealth abortion or receiving abortion pills by mail.
This means discretion and privacy are absolutely paramount.
If at all possible, tell as few people as you deem necessary about your pregnancy and your decision to terminate the pregnancy.
Clear any internet search, private message, or phone call history that might connect this to you.
Trying to make sense of the limitations in your state? Our state-by-state guide to abortion restrictions can help.
A surgical abortion is a procedure done by a trained medical professional in a clinical setting like an abortion clinic or, sometimes, a hospital.
There are two main types of surgical abortion: vacuum aspiration and dilation and evacuation (D&E). Vacuum aspiration is most often used up to 16 weeks after your last period, while D&E is used up to 24 weeks.
Vacuum aspiration
Vacuum aspiration is the most common type of in-clinic abortion, according to provider Planned Parenthood.
This procedure uses gentle suction to empty your uterus. It isn’t typically painful, but you may feel some cramping because your uterus will contract as the tissue is removed.
The procedure lasts about 5–10 minutes. You may need to stay at the clinic for up to a few hours afterward to ensure the abortion is complete.
Safety, side effects, and risks
Like other forms of abortion, vacuum aspiration is extremely safe. A large body of evidence suggests that fewer than 1% of people who have a vacuum aspiration procedure experience major complications.
Side effects after a vacuum aspiration procedure can include:
- bleeding or spotting
- cramps
- nausea
- sweating
- dizziness
As with any surgery or procedure, vacuum aspiration abortion has a small risk of infection. The chance of experiencing an infection from a vacuum aspiration abortion is likely a bit higher than it is from medical abortion.
Your provider may prescribe you an antibiotic to help reduce infection risk.
Despite myths and misinformation, there is no evidence that having any kind of abortion affects your fertility, prevents you from becoming pregnant in the future, raises your risk of breast cancer or miscarriage, or affects your mental health in the long term.
Dilation and evacuation (D&E)
D&E is often used a bit later on in pregnancy. It uses a combination of vacuum aspiration, forceps, and dilation and curettage (D&C).
To start, the provider dilates (or widens) your cervix to make it easier to remove the pregnancy tissue.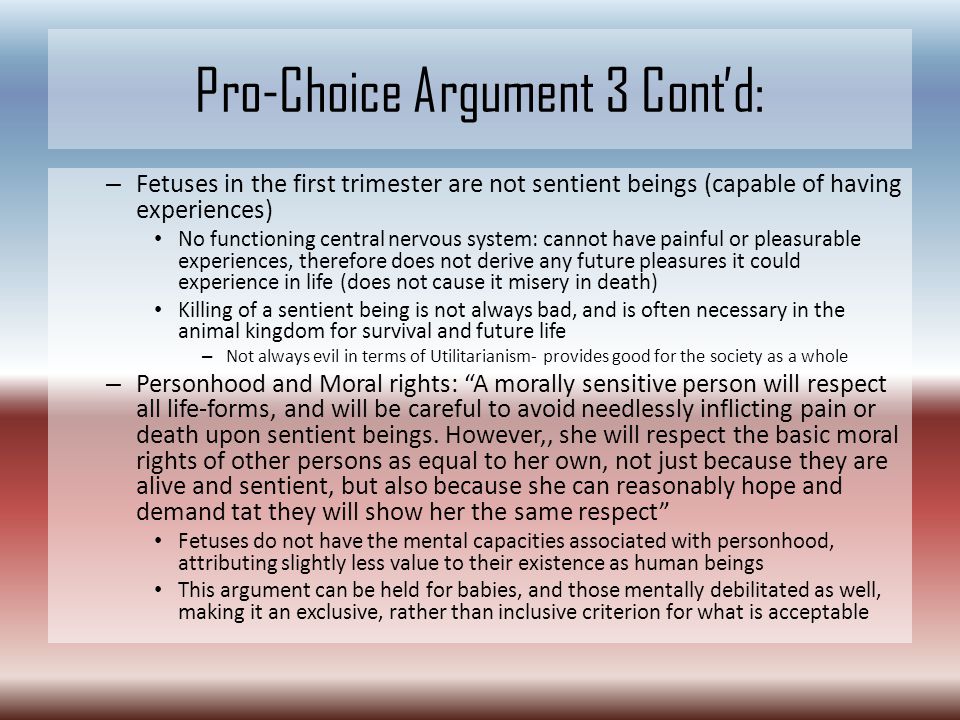 They may have you take misoprostol and/or mifepristone, medications that help soften the uterus and cause it to contract, to help with that.
They may have you take misoprostol and/or mifepristone, medications that help soften the uterus and cause it to contract, to help with that.
Then, they will use forceps to remove the fetus and placenta, a tube to suction out the uterus, and a scoop-like instrument called a curette to scrape out the uterine lining.
You’ll have this procedure in a hospital or a clinic. A D&E can be somewhat painful, but your provider can give you numbing medicines or local anesthesia to prevent discomfort and will likely send you home with prescription pain medication.
The procedure generally takes less than 30 minutes. You can go home the same day, but as with many surgeries, you may need to wait at the clinic for a while to ensure you’re doing OK.
Safety, side effects, and risks
D&E is a safe and common abortion method, and it’s the preferred choice for ending a pregnancy that has progressed to the second trimester.
That’s because it’s associated with the lowest risk of complications, including incomplete abortion, compared with other methods of ending pregnancies in the second trimester.
Side effects from a D&E may include:
- bleeding
- cramping
- breast engorgement or lactation
- nausea, diarrhea, or vomiting
- chills
Some complications are possible but unlikely. These include infection, perforation, and excessive bleeding or hemorrhage.
Eligibility
There are no conditions that prevent you from having a surgical abortion, but people with certain health conditions may need to have theirs in a hospital setting instead of a clinic to ensure their safety.
These include bleeding diathesis or the use of anticoagulant medication. And if you have a pelvic infection, your provider will likely delay or reschedule your procedure if possible.
Efficacy
Vacuum aspiration and D&E are extremely effective for ending your pregnancy.
These abortions are successful about 98% of the time, with just 2% of people needing to return to a clinic for an additional procedure or a pill to complete the abortion.
Some sources suggest that surgical aspiration is somewhat more likely to be successful than medical abortion, but more research is needed to confirm whether and why that’s the case.
Cost
Surgical abortion may cost between $500–$2,000, depending on several factors, including your location.
The further along you are in your pregnancy, the more the procedure will cost.
Access and legality
The legality of abortion varies from state to state, especially since many states have rushed to restrict or ban surgical abortion procedures following the fall of Roe v. Wade in June 2022.
Limitations on surgical abortion are very common — especially after you’ve reached a point of pregnancy at which the fetus could be considered “viable,” or able to live outside of the uterus.
Other states impose unnecessary and harmful restrictions like mandatory counseling before receiving an abortion. Some even require providers to share false information about abortion safety before allowing you to have an abortion.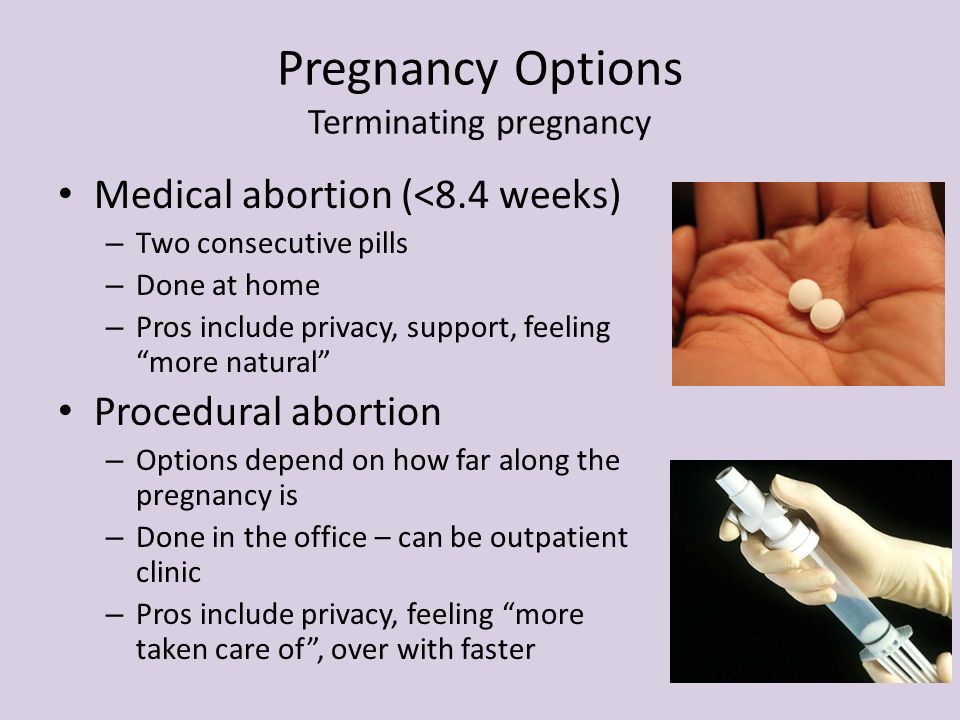
These restrictions are attempts to discourage you from making your own decisions about your reproductive health. They’re not based on evidence and contribute to anti-abortion stigma.
Experiencing stigma or judgment is associated with poorer mental and emotional health outcomes for those seeking an abortion.
One way to avoid some of these hurdles is to self-manage a medical abortion at home, so you may want to consider these factors when deciding what type of abortion is best for you.
Learn about the legality of surgical abortion in each state.
Watch out for crisis pregnancy centers (CPCs)
While some CPCs offer limited healthcare services like pregnancy tests or ultrasounds, they do not provide abortions or support accessing abortions.
CPC workers are known to shame and mislead people into believing that abortion is unsafe or harmful.
The Crisis Pregnancy Center Map can help you steer clear of these predatory groups. You can also check ReproAction’s Fake Clinic Database and the #ExposeFakeClinics resource hub.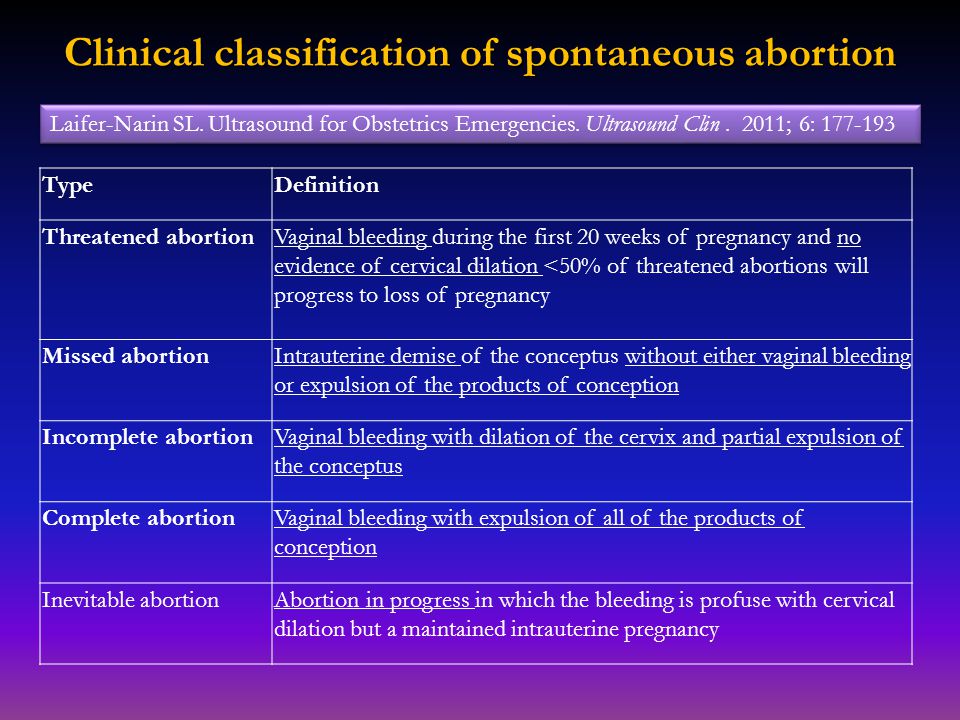
Learn more about identifying, avoiding, and leaving CPCs.
Later-term abortions are uncommon in the U.S.
According to the Centers for Disease Control and Prevention (CDC), just 6.2% of abortions in 2019 happened at 14–20 weeks’ gestation. Fewer than 1% of all U.S. abortions were performed at 21 weeks or later.
People most commonly opt for abortions later in pregnancy if they’ve learned of severe health complications affecting the fetus, developed severe health complications themselves, or were denied an abortion earlier on.
If you need an abortion later in pregnancy, you’ll likely have a D&E procedure. It may take place over 2 days and require multiple visits to a provider. You will probably receive general anesthesia.
Complications are still rare, and later-term abortions are considered safe and effective with no risk of affecting your future fertility.
Learn more about later-term abortions here.
Complications are extremely rare for all types of abortion, but they can happen. The major concerns are infection, excessive bleeding or hemorrhage, organ perforation during surgery, or an incomplete abortion.
The major concerns are infection, excessive bleeding or hemorrhage, organ perforation during surgery, or an incomplete abortion.
Contact a medical professional — ideally an abortion provider in your local community — if you:
- experience no bleeding at all within 24 hours of taking misoprostol
- have extremely heavy bleeding, which is defined as 1) bleeding through 2 or more regular maxi pads in an hour for 2 or more hours in a row or 2) soaking through 1 or more regular pads in an hour for 3 or more hours in a row
- pass foul-smelling vaginal discharge
- pass blood clots larger than a lemon
- run a fever of 100.4ºF (38ºC) or higher
- have pain that doesn’t decrease after taking over-the-counter or prescription pain medication
- experience nausea, vomiting, or diarrhea for more than a day or so after taking misoprostol
- see, feel, or experience any unusual or concerning symptoms like shortness of breath or chest pain
Listen to your body.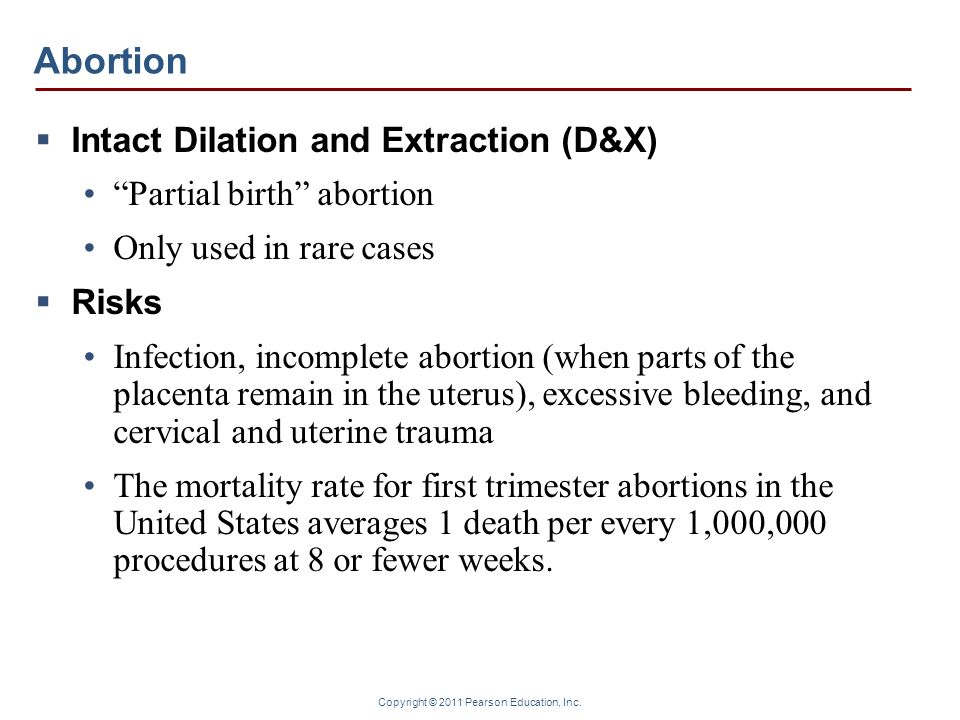 If something doesn’t feel right, even if it’s not on the above list, reach out to a healthcare professional.
If something doesn’t feel right, even if it’s not on the above list, reach out to a healthcare professional.
Seek care
If you think you’re experiencing complications and live in an abortion-hostile state, you should still seek medical care.
Healthcare professionals can’t distinguish a medication abortion from an unintentional miscarriage, and you don’t have to disclose that you induced the abortion using pills.
You can say that you’re experiencing heavy menstrual bleeding or suspect that you’re having a miscarriage. These conditions are treated the same way.
If you have the freedom to choose which type of abortion you’d feel most comfortable with, there are many factors to consider:
- How long you’ve been pregnant: Some forms of abortion are safer and more effective earlier in pregnancy and should be avoided later on. Medication abortions are often reserved for earlier abortions, while surgeries are needed later. The duration of your pregnancy may also affect which method(s) of abortion you can legally access where you live.
- Accessibility: Many states restrict or outlaw some forms of abortion or impose unnecessary and stressful hurdles — especially now, following the end of Roe v. Wade. Be sure to know the laws in your area and prioritize your privacy if you live somewhere that is hostile toward abortion.
- Costs: Abortion pills generally cost less than in-clinic surgical abortions, though prices can vary based on where you live. You may want or need to opt for a more affordable abortion method. Or, if you have insurance, your plan may only cover some abortion methods.
- Privacy: Many people prefer to use abortion pills in the privacy of their own homes or among their personal support systems. But if you don’t live with people who support your abortion choice, you might prefer to have the procedure in a clinic to better protect your privacy.
- Trust in the medical system: For many people, especially members of marginalized communities, ordering pills and self-managing an abortion at home may be more appealing than engaging with the medical system.
 Other people may not feel confident self-managing a procedure and would feel better in a sterile clinical setting with experienced professionals around, and that’s OK, too.
Other people may not feel confident self-managing a procedure and would feel better in a sterile clinical setting with experienced professionals around, and that’s OK, too.
While it’s important to consider the risks of any procedure, the risk of complications is low for any method of abortion and doesn’t vary much by type. The risk mostly increases based on how long you’ve been pregnant.
However, surgical abortions are likely associated with a higher risk of infection, while medical abortions may cause more bleeding over a longer period of time.
The chart below summarizes some of the main differences between the types of abortion.
| Mifepristone and misoprostol | Misoprostol only | Vacuum aspiration | Dilation and evacuation | |
| Type | Medical (2 medications) | Medical (1 medication) | Surgical (5–10 minutes plus waiting periods) | Surgical (30 minutes plus waiting periods and medications) |
| Timeline | Up to 10–12 weeks of pregnancy | Up to 10–12 weeks of pregnancy | Up to 16 weeks of pregnancy | Up to 24 weeks of pregnancy |
| Effectiveness | 95–99% | About 78% | About 98% | About 98% |
| Accessibility and legality | Available in-clinic or online without a provider’s prescription; may be legally challenging in some states | Available in-clinic or online without a provider’s prescription; more likely to be legally protected in the long term | Restricted or banned in many states, with more likely to follow | Restricted or banned in many states, with more likely to follow |
| Medical limitations | Not safe for people with IUDs or certain medical conditions | Not safe for people with IUDs or certain medical conditions | No medical limitations | No medical limitations |
| Privacy | Can be done safely and effectively at home without the aid of a clinician | Can be done safely and effectively at home without the aid of a clinician | Must be done in person at a clinic or hospital | Must be done in person at a clinic or hospital |
Wading through the sea of abortion information — and misinformation — online can be overwhelming.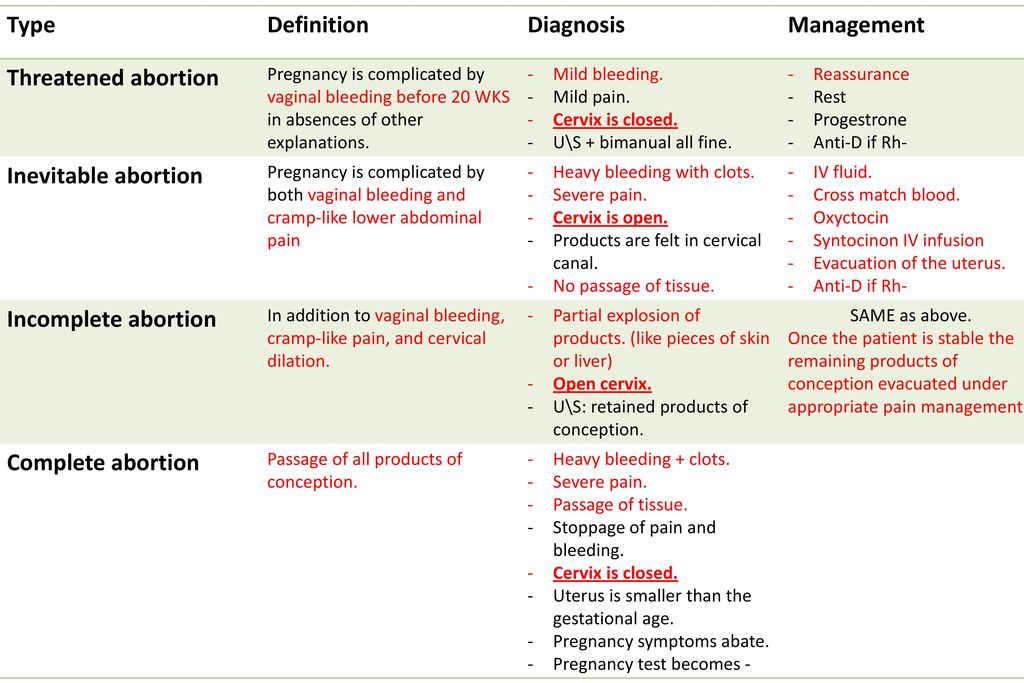 So can navigating costs, legality, and travel. And of course, deciding whether an abortion is right for you in the first place can be tough.
So can navigating costs, legality, and travel. And of course, deciding whether an abortion is right for you in the first place can be tough.
Remember that support is available for every step of your abortion process.
Several U.S. organizations can offer guidance on your options, help you find a provider, and assist with covering the costs of an abortion.
Finding an abortion provider
If you’re unsure where to start, consider reaching out to the nearest Planned Parenthood clinic, which you can find here.
Clinic staff can counsel you on your options and help you weigh the pros and cons of each.
If you decide to pursue an abortion, they can provide you with discreet, lower-cost services, including medical and surgical abortions.
Other options include INeedAnA.com and the National Abortion Federation’s U.S. Abortion Clinic Locator. These sites can help you find a local or independent abortion clinic.
The National Abortion Federation also operates a hotline that can help you find an abortion provider or financial support for your abortion.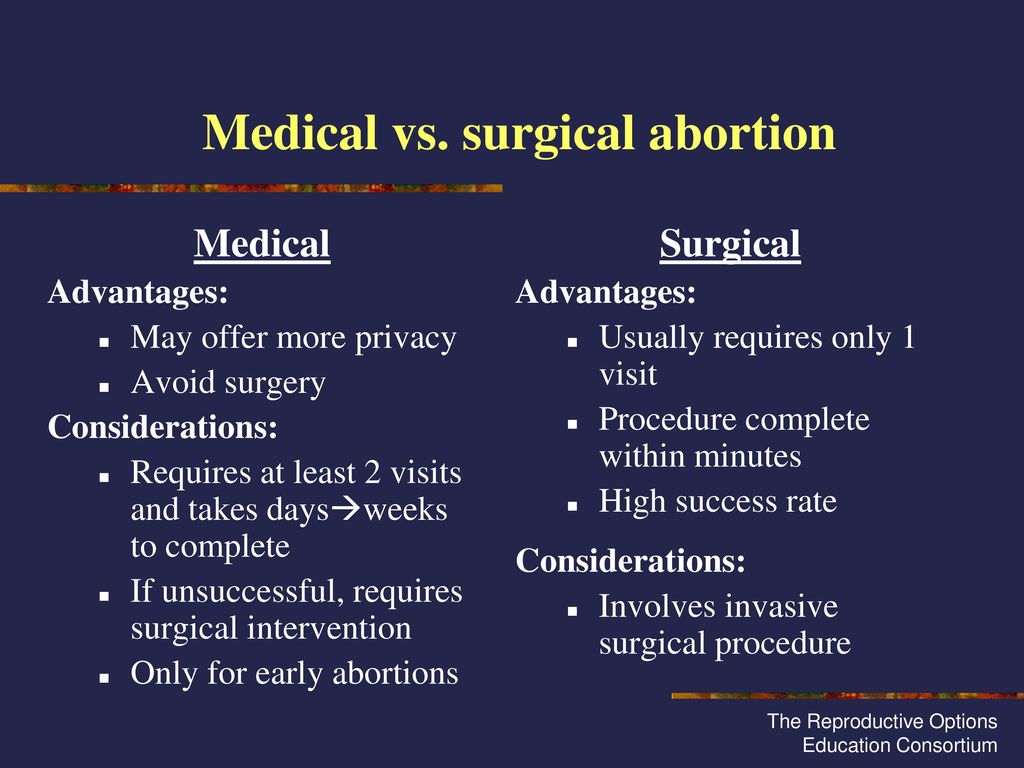
Paying for an abortion
Some insurance plans will cover the cost of abortion, whether medical or surgical, so check in with your insurance provider if you have one and feel safe asking them about abortion.
Additionally, many communities are home to abortion funds. These organizations can help you pay for your abortion or any associated costs like transportation, lodging, medication and recovery management, and child care.
Some abortion funds you can contact for help include:
- Indigenous Women Rising
- Access Reproductive Care Southeast
- Yellowhammer Fund
- Lilith Fund
- Northwest Abortion Access Fund
- Access Reproductive Justice
- Utah Abortion Fund
- Florida Access Network
- Holler Health Justice
- Kentucky Health Justice Network
- Midwest Access Coalition
- Apiary
The above list is far from complete, as many local and regional communities have abortion funds. The National Network of Abortion Funds can connect you with organizations serving your area.
Where to get help outside the United States
Abortion access varies widely by country.
The Center for Reproductive Rights offers more information on abortion laws worldwide, along with a map you can use to check the abortion laws in your country.
If you live in Canada, you can call the National Abortion Federation hotline at 877-257-0012 for a referral to a nearby clinic.
British Pregnancy Advisory Services can offer more information about your abortion options if you live in the United Kingdom. They also provide abortion services and support to international patients.
Abortion isn’t associated with poor mental health outcomes long term. In fact, people who have had abortions are no more likely to experience mental health challenges than people who have not had abortions.
Still, it’s natural to feel intense and possibly mixed emotions.
If you’re struggling with your emotional health, feel empowered to speak with an abortion-informed mental health professional or consider joining a support group.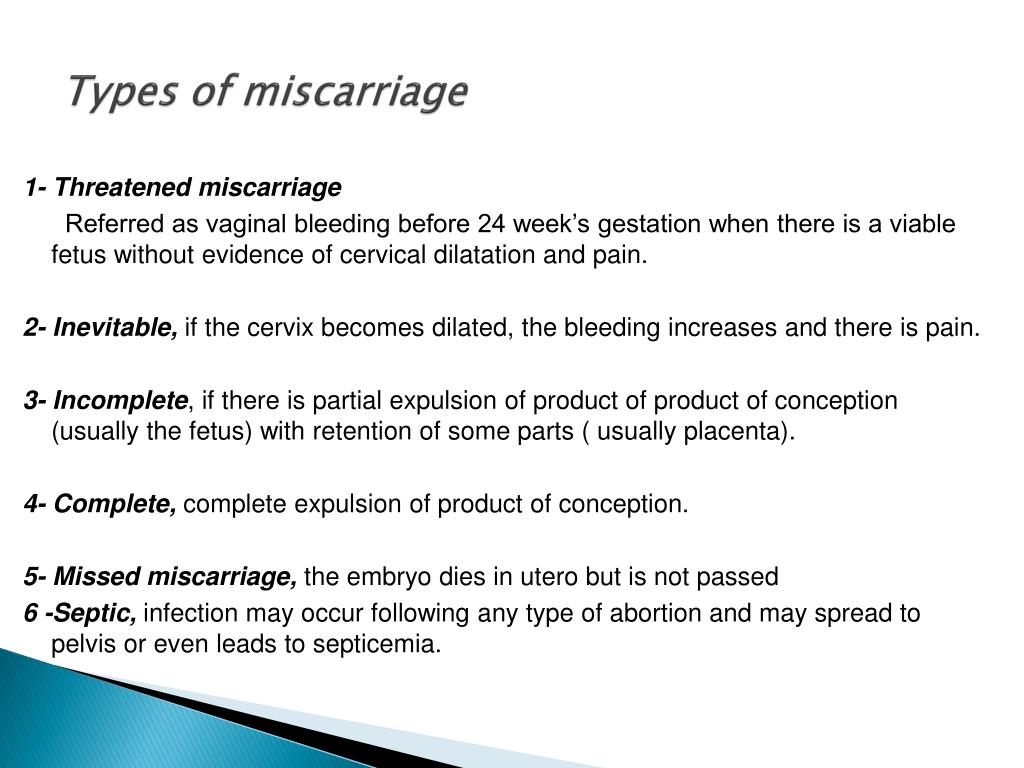
Other resources that can help include Exhale and All-Options, which can connect you with unbiased, nonjudgmental post-abortion emotional support.
Finding support for mental and emotional healthIf you need to talk with someone right away, help is available:
- Call the National Suicide Prevention Lifeline at 988.
- Text “HOME” to the Crisis Text Line at 741741.
- If you’re a young person of color, text STEVE to 741741.
- Call the Trans Lifeline Hotline at 877-565-8860 (US) or 877-330-6366 (Canada).
The types of abortion are medical and surgical.
A medical abortion involves taking one or two pills that cause your uterus to empty itself. You can order these yourself and take them at home, or you can receive and take them in a clinic.
Medical abortion is approved up to 10–12 weeks of pregnancy.
There are two main types of surgical abortion: vacuum aspiration and dilation and evacuation (D&E). These will be performed by trained professionals in a clinic or hospital.
These will be performed by trained professionals in a clinic or hospital.
Vacuum aspiration is quicker and can be accessed up to 16 weeks of pregnancy, while D&E is used up to 24 weeks.
It can be difficult to determine which abortion method is best for you. Legal restrictions that vary by state can make it even tougher to know what’s accessible in your area.
You’ll need to consider how long you have been pregnant, what abortion laws exist, your budget, and your personal preferences regarding medical care.
Resources are available to help you if you’re struggling to find a provider, pay for an abortion, or manage your emotional health during the abortion process.
Rose Thorne is an associate editor at Healthline Nutrition. A 2021 graduate of Mercer University with a degree in journalism and women’s & gender studies, Rose has bylines for Business Insider, The Washington Post, The Lily, Georgia Public Broadcasting, and more. Rose’s proudest professional accomplishments include being a college newspaper editor-in-chief and working at Fair Fight Action, the national voting rights organization. Rose covers the intersections of gender, sexuality, and health, and is a member of The Association of LGBTQ+ Journalists and the Trans Journalists Association. You can find Rose on Twitter.
Rose covers the intersections of gender, sexuality, and health, and is a member of The Association of LGBTQ+ Journalists and the Trans Journalists Association. You can find Rose on Twitter.
Abortion and its consequences
Abortion and its consequences.
The issue of termination of pregnancy at the request of a woman remains relevant for modern Russia. In the Komi Republic, only 60% of pregnancies end in childbirth, while the birth rate in the republic is declining.
Unwanted pregnancy is always a high risk of unsafe abortion and maternal death. Unfortunately, pregnancy does not always occur at the moment when it is realized and desired.
In some cases, the measure of abortion is forced. For example, if the health of the mother does not allow a healthy fetus to be born; there are fetal malformations that are incompatible with life; had a spontaneous abortion ("miscarriage").
According to the Federal Law of the Russian Federation No.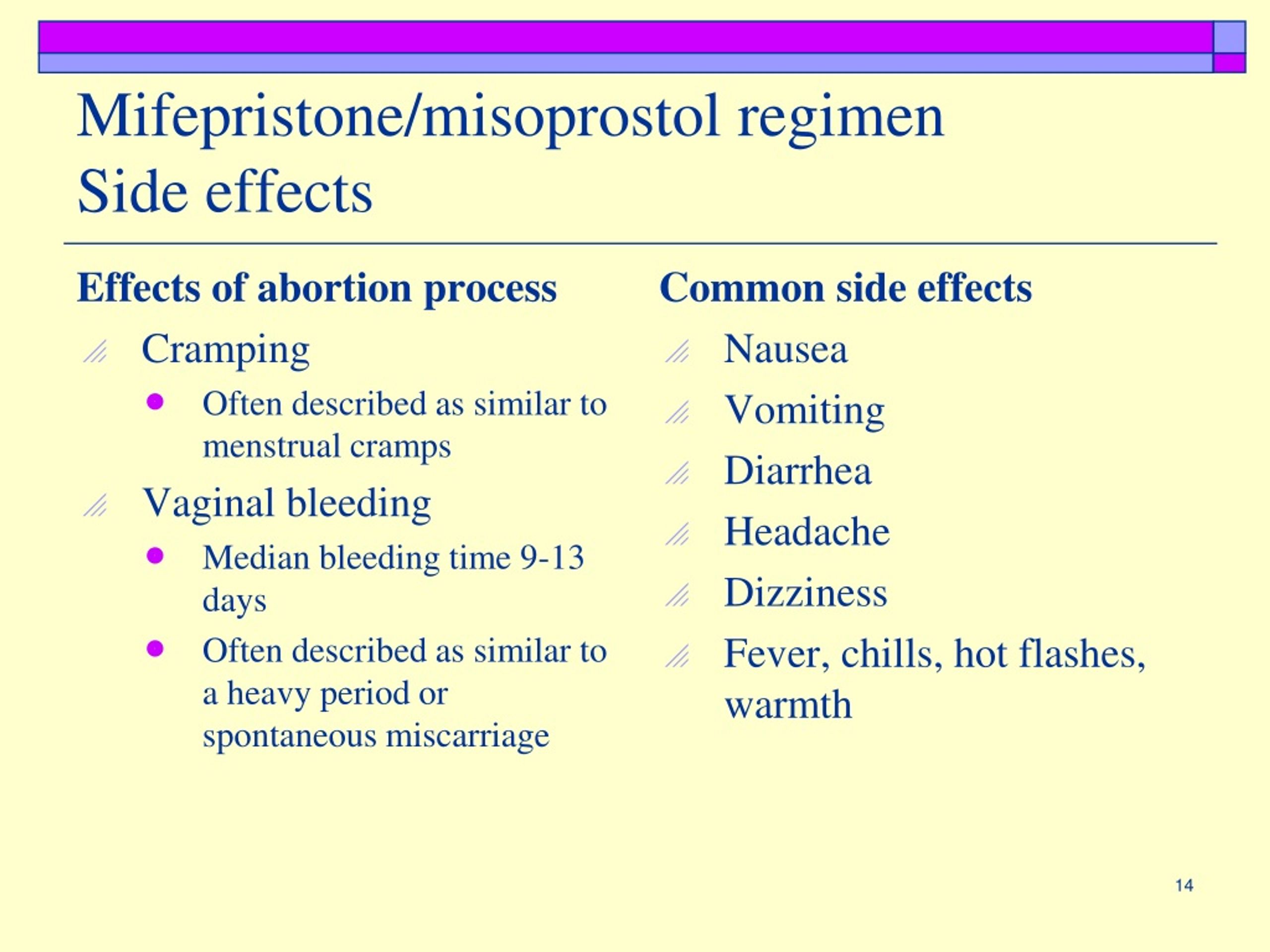 323 - FZ "On the Basics of Protecting the Health of Citizens in the Russian Federation", a woman is given a waiting time for making a decision to terminate a pregnancy:
323 - FZ "On the Basics of Protecting the Health of Citizens in the Russian Federation", a woman is given a waiting time for making a decision to terminate a pregnancy:
weeks, but no later than the end of the twelfth week of pregnancy;
2) not earlier than 7 days from the date of application for a period of 8-10 weeks of pregnancy.
There are currently three types of artificial termination of pregnancy.
1. Medical abortion.
Medical abortion is the safest abortion technology available today. It does not imply surgical intervention, which women are so afraid of. With medical abortion, patients take drugs orally according to a certain scheme.
Termination of pregnancy with medical abortion up to 9 weeks of pregnancy.
2. Vacuum abortion.
This type of abortion is often referred to as a "mini-abortion". It is believed that after a vacuum abortion, the female body recovers faster than after a surgical one. With a “mini-abortion”, medical intervention is carried out in the uterine cavity using special equipment (vacuum aspirator).
With a “mini-abortion”, medical intervention is carried out in the uterine cavity using special equipment (vacuum aspirator).
Dates - up to 20 days of delayed menstruation (5-6 weeks).
3. Surgical abortion.
Is the so-called "classic" abortion, which is also popularly called "curettage". It is considered the most dangerous of all, as it can lead to catastrophic consequences. This type of abortion is especially dangerous for primigravida, young girls - there is a risk that after such an abortion they will not be able to have children in the future.
Possible complications during abortion:
- Heavy bleeding requiring surgery.
- Massive haemorrhage requiring a blood transfusion.
- Damage to the cervix.
- Uterine perforation.
If these complications occur, surgical treatment may be suggested.
Possible complications after abortion:
- Infection.
 Taking antibiotics can reduce the risk of this complication. If left untreated, women at risk may develop a severe infection (acute pelvic inflammatory disease).
Taking antibiotics can reduce the risk of this complication. If left untreated, women at risk may develop a severe infection (acute pelvic inflammatory disease). - Having a chlamydial infection before an abortion increases the risk of salpingitis (“inflammation of the uterus”).
- Secondary infertility.
- Incomplete abortion requiring additional emptying of the uterine cavity by vacuum aspiration.
- Increased future risk of preterm birth.
Any abortion leads to a change in the hormonal background in the female body. This leads to the development of gynecological diseases, weight gain, metabolic disorders.
Finally, one cannot ignore the psychological consequences of abortion. This is especially true for young girls, for whom an abortion can be a real shock. In this case, psychologists talk about the "post-abortion syndrome", which is characterized by severe depression and stress.
Timing of initiation of contraceptive use after an abortion.
Ovulation can occur as early as 8-10 days after an induced abortion. It is noted that more than 50% of women resume sexual activity within two weeks after an abortion, and 6% of them have a new pregnancy in the next cycle. Therefore, it is necessary to start using contraception immediately after an abortion. Modern contraception is effective and safe enough to completely protect a woman from unwanted pregnancy.
A child is a great happiness. However, each person is free in his choice. We sincerely hope that you will choose not to have an abortion, choose to have a child and not regret it in the future.
Medical abortion: types, risks, complications
Unfortunately, for one reason or another, you have decided to terminate the pregnancy. We do not touch on the circumstances that led to this. Let's touch on the correct approach to this procedure. At the request of a woman or medical indicators, one of several methods for terminating a pregnancy is selected.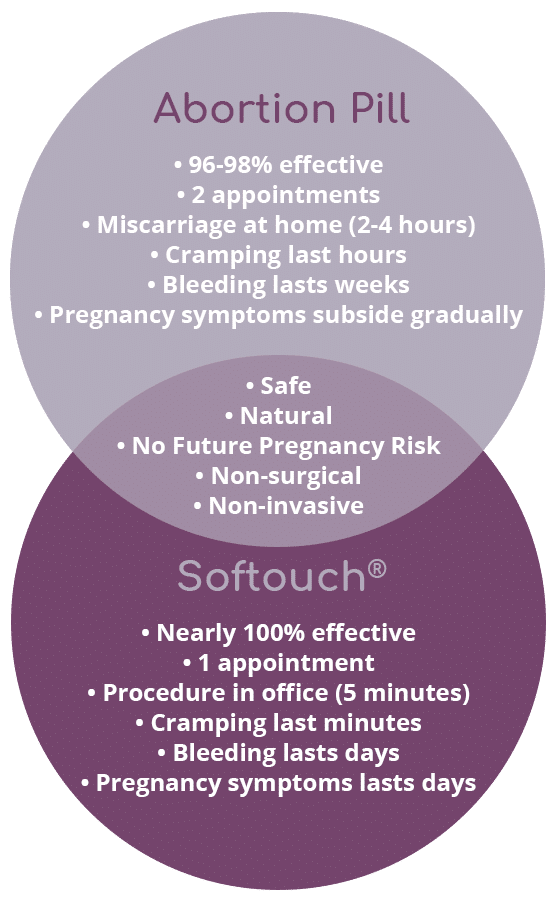
1. Medical abortion up to 5 weeks of pregnancy or 21 days of delay.
Currently, there is a widespread opinion among patients that medical abortion is safe and easy. Many people think that medical abortion does not cause any harm to health. We want to say that any abortion is bad and dangerous! Moreover, more and more often women are frivolous about both the medical method of terminating a pregnancy and the consequences of this procedure.
Our clinic receives inquiries from patients asking them to sell them a drug used to terminate a pregnancy, or write a prescription to buy it in the pharmacies of the city in order to take it on their own at home, and thereby save themselves from having to visit a doctor. It is unacceptable! Medical abortion must be carried out in a medical institution in the presence of a gynecologist, after the necessary examination and determination of the gestational age. A woman should understand that a medical abortion, carried out under the supervision of a specialist, will not save her from the risk of complications, but will minimize the consequences of a medical method of abortion. What can not be said about the consequences that may arise from self-administered medical abortion.
What can not be said about the consequences that may arise from self-administered medical abortion.
2. Mini abortion or vacuum aspiration.
This method is also carried out in the early stages of pregnancy: from 5 to 10 weeks. A vacuum abortion is performed on an outpatient basis under anesthesia under ultrasound guidance using individual disposable instruments and materials. The fetal egg during a vacuum abortion is removed from the uterine cavity through a disposable catheter attached to a vacuum device. The doctor explains to the patient that such an abortion in the early stages, although it is considered more gentle than a surgical abortion, nevertheless, it can cause hormonal failure, inflammation of the reproductive organs, and menstrual irregularities.
3. Surgical abortion: 10 to 12 weeks.
The operation is performed under intravenous anesthesia. At this time, the fetus reaches a weight of several grams, it is already firmly attached to the wall of the uterus by the placenta, and can only be removed from the woman's body with a sharp knife with a loop-shaped end - a curette.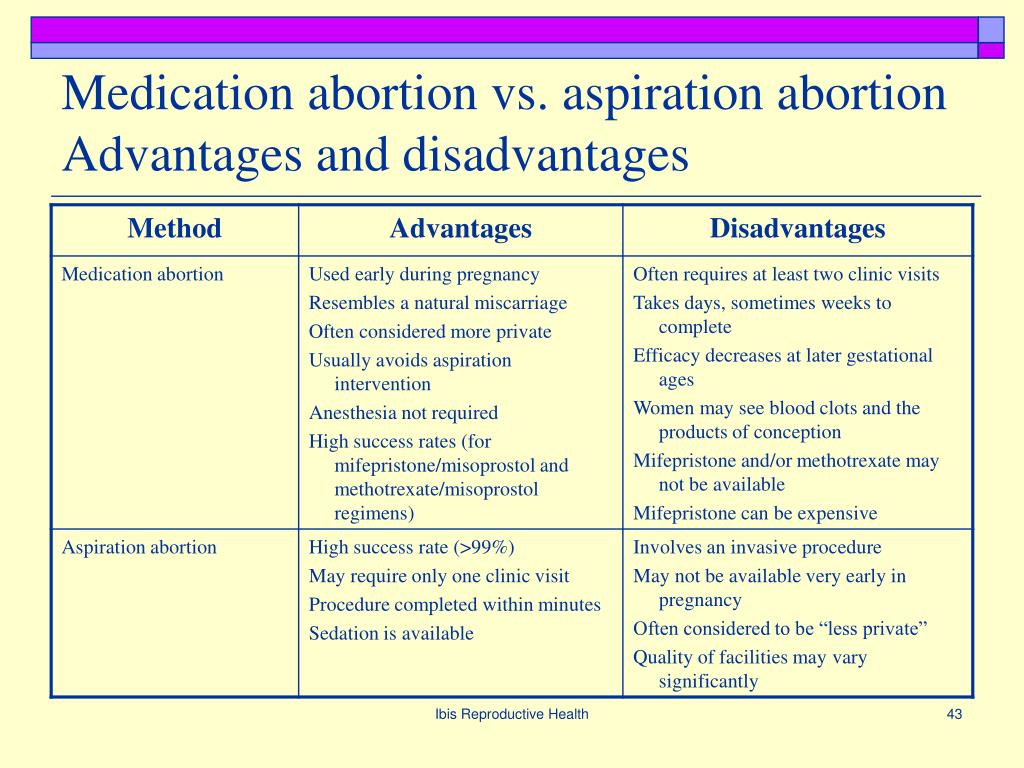 Surgical abortion can also cause various complications. The endometrium, the innermost layer of the uterus, suffers the most.
Surgical abortion can also cause various complications. The endometrium, the innermost layer of the uterus, suffers the most.
After any medical abortion, the patient must undergo a special rehabilitation (rehabilitation) course of treatment aimed at the speedy "recovery" of the uterus and the whole body after the operation to terminate the pregnancy. This treatment makes it possible to significantly reduce the number of complications of abortion and the woman in the future to safely endure the already desired pregnancy. And in order to get rid of the need to have medical abortions in the future, it is imperative to choose a method of contraception.
If you want to terminate an unwanted pregnancy, make an appointment at our medical center. Our doctors will advise you and, depending on the duration of pregnancy, recommend and perform a medical, vacuum or surgical abortion, having previously examined for contraindications.
Also, our staff will tell you in detail about the possible consequences of an abortion and help you choose the most suitable contraceptive for you, which will avoid the need for abortions in the future.