Treatment for neural tube defects
Neural Tube Defects | MedlinePlus
On this page
Basics
- Summary
- Start Here
- Diagnosis and Tests
- Prevention and Risk Factors
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
- Genetics
See, Play and Learn
- No links available
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
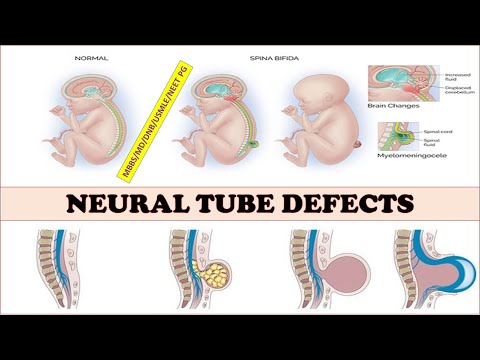
Neural tube defects are birth defects of the brain, spine, or spinal cord. They happen in the first month of pregnancy, often before a woman even knows that she is pregnant. The two most common neural tube defects are spina bifida and anencephaly. In spina bifida, the fetal spinal column doesn't close completely. There is usually nerve damage that causes at least some paralysis of the legs. In anencephaly, most of the brain and skull do not develop. Babies with anencephaly are usually either stillborn or die shortly after birth. Another type of defect, Chiari malformation, causes the brain tissue to extend into the spinal canal.
The exact causes of neural tube defects aren't known. You're at greater risk of having an infant with a neural tube defect if you:
- Have obesity
- Have poorly controlled diabetes
- Take certain antiseizure medicines
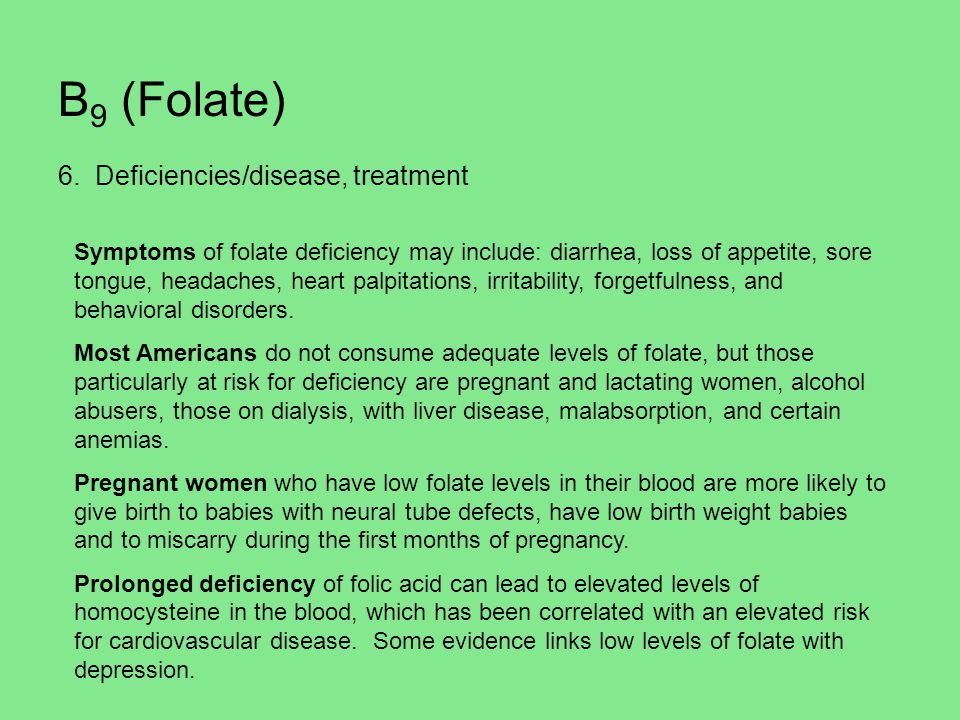
Getting enough folic acid, a type of B vitamin, before and during pregnancy prevents most neural tube defects.
Neural tube defects are usually diagnosed before the infant is born, through lab or imaging tests.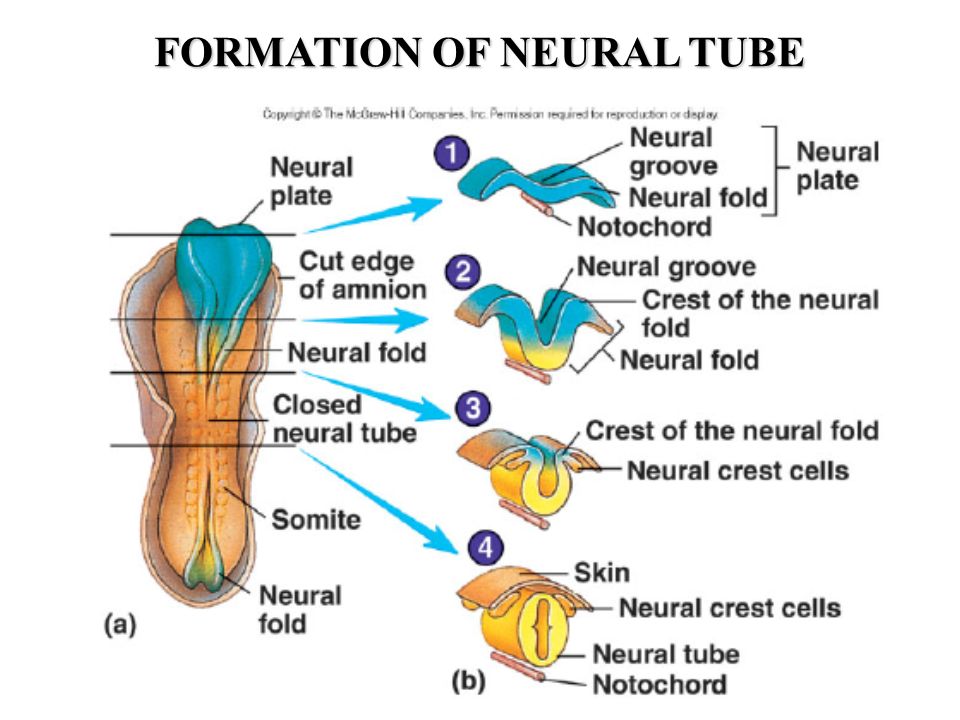 There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
NIH: National Institute of Child Health and Human Development
- About Neural Tube Defects (NTDs) (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Neural Tube Defects (March of Dimes Birth Defects Foundation)
- Alpha-fetoprotein (AFP) Test (National Library of Medicine) Also in Spanish
- How Do Health Care Providers Diagnose Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Treatments for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Are There Disorders or Conditions Associated with Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Anencephaly (National Institute of Neurological Disorders and Stroke)
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) Also in Spanish
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) - Short Summary
- Encephaloceles (National Institute of Neurological Disorders and Stroke)
- Facts about Anencephaly (Centers for Disease Control and Prevention) Also in Spanish
- Facts about Encephalocele (Centers for Disease Control and Prevention) Also in Spanish
- Hydranencephaly (National Institute of Neurological Disorders and Stroke)
- Iniencephaly (National Institute of Neurological Disorders and Stroke)
- Tethered Spinal Cord Syndrome (National Institute of Neurological Disorders and Stroke)
- How Many People Are at Risk for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- ClinicalTrials.
 gov: Anencephaly (National Institutes of Health)
gov: Anencephaly (National Institutes of Health) - ClinicalTrials.gov: Arnold-Chiari Malformation (National Institutes of Health)
- ClinicalTrials.
 gov: Neural Tube Defects (National Institutes of Health)
gov: Neural Tube Defects (National Institutes of Health)
- Article: Prenatal assessment and pregnancy outcomes of foetal low-lying conus medullaris using.
 ..
.. - Article: Aetiology and diagnostics of paediatric hydrocephalus across Africa: a systematic review...
- Article: Analysis of DNMT1 gene variants in progression of neural tube defects-an.
 ..
.. - Neural Tube Defects -- see more articles
- Eunice Kennedy Shriver National Institute of Child Health and Human Development Also in Spanish
- Find a Genetic Counselor (National Society of Genetic Counselors)
- Find a Pediatrician or Pediatric Specialist (American Academy of Pediatrics) Also in Spanish
- March of Dimes Birth Defects Foundation Also in Spanish
- National Institute of Neurological Disorders and Stroke Also in Spanish
Neural Tube Defects | Johns Hopkins Medicine
Neural tube defects, also known as spinal dysraphisms, are a category of neurological disorders related to malformations of the spinal cord, such as spina bifida, anencephaly, meningocele, myelomeningocele and tethered spinal cord syndrome.
What You Need to Know
- Neural tube defects can affect bones of the spine, the spinal cord or the nerve roots that extend from the spine into the body.
- The cause is not clear but may be related to genetics, maternal nutrition (including folic acid deficiency) during pregnancy or other factors.
- Spina bifida is the most common neural tube defect, affecting approximately one out of every 1,000 newborns.
- In some situations, surgery may address these defects and their symptoms.
How Neural Tube Defects Occur
Neural tube defects result from the beginnings of the embryo’s nervous system (the neural tube) failing to close completely before birth.
The neural tube forms very early in embryonic development — just one month after conception, sometimes before the mother knows she is pregnant. It starts as a flat, ribbon-like structure that rolls together, lengthwise, to form the tube that will normally grow into the brain and spinal cord.
It starts as a flat, ribbon-like structure that rolls together, lengthwise, to form the tube that will normally grow into the brain and spinal cord.
If the seam of the neural tube does not close correctly, portions of the spine, the covering of the spinal cord (meninges) or the cord itself can push outside of the back as the fetus grows.
Types of Neural Tube Defects
Two of the most common neural tube defects are spina bifida and tethered cord syndrome.
What is spina bifida?
Each year, one in 1,000 babies is born with spina bifida (meningomyelocele), a malformation of the bones (vertebrae) and skin surrounding the spine that can lead to serious infections, problems with bladder and bowel function, hydrocephalus, and paralysis. In most cases, surgical correction of the neural tube defect is necessary soon after birth.
Many problems associated with spina bifida can be managed well with the right treatment, and infants born with spinal neural tube defects can lead full lives.
What is tethered spinal cord syndrome?
Tethered spinal cord syndrome occurs when the spinal cord is abnormally attached to surrounding tissue. Failure to detect a tethered spinal cord can lead to a sudden, catastrophic injury during childhood or adolescence, such as paralysis.
Tethered spinal cord syndrome can be diagnosed through the detection of certain skin abnormalities along the midline of the back. Diagnosis may be confirmed by MRI scans and surgery is usually indicated to prevent any future neurological damage.
Spinal Subtraction Surgery | When Less Offers More
How are neural tube defects diagnosed?
If a child is born with a neural tube defect, such as spina bifida, a thorough evaluation by a pediatric neurosurgeon can help determine the best treatment option.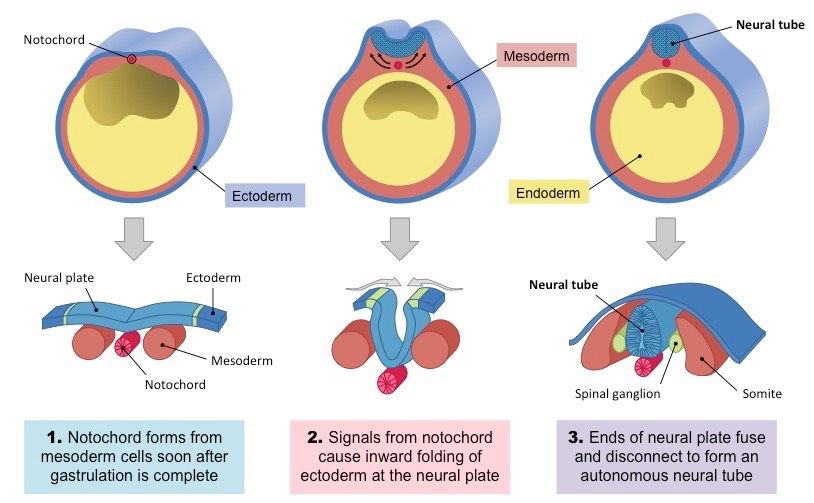
Your child’s doctor will conduct a thorough physical, ask for a detailed family and patient history and may order imaging of the spine using an MRI or ultrasound scan.
Treatment for Neural Tube Defects
The ideal treatment approach involves multiple specialties in reviewing the cases of children with neural tube defects, including pediatric neurosurgeons, pediatric neurologists, and pediatric urologists, among others.
Surgery for Neural Tube Defects
The purpose of surgery is to correct the physical malformation. If the child’s spinal cord is exposed to the skin, early surgical repair is essential to prevent infection and neurological deficits.
In the case of tethered spinal cord syndrome, a pediatric neurosurgeon will perform surgery to release the tether. If there are areas of fat intertwined within the nerves, the pediatric neurosurgeon will remove these as well during surgery.
After surgery, follow-up care is extremely important to monitor the child’s recovery.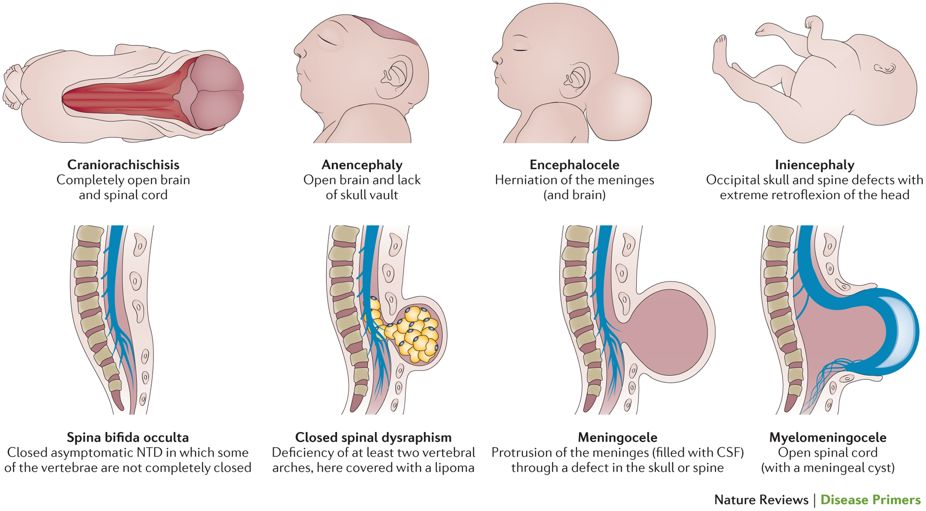 Your pediatric neurosurgeon will schedule follow-up appointments to make sure your child is making progress, and seeing the other specialists is important to your child’s overall well-being.
Your pediatric neurosurgeon will schedule follow-up appointments to make sure your child is making progress, and seeing the other specialists is important to your child’s overall well-being.
Principles for the prevention of fetal neural tube defects
03/27/2015
Despite significant advances in modern prenatal diagnosis, neural tube defects (NTD) of the fetus are still one of the most common congenital malformations. Annually in the USA, 1 case of NTD is registered per 1000 pregnancies, while 4000 pregnancies per year are terminated, including spontaneous miscarriage and induced abortion, due to fetal CNS developmental disorders. The annual incidence of fetal NTD in Russia is 0.45%; mortality due to NTD - 300 newborns (2% of total infant mortality). nine0006
NTD, or spina bifida, is a significant factor in disability, although some forms of this pathology are currently amenable to surgical correction.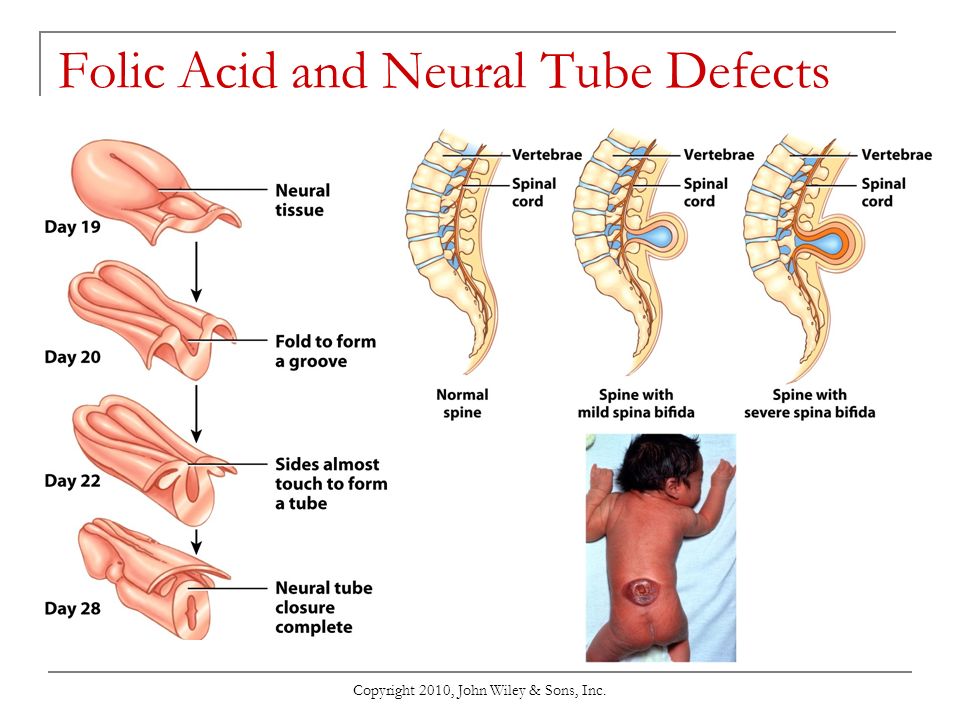
In most cases, NTDs result from failure of the ends of the neural tube to close or reopen. In humans, the neural tube is formed from the ectoderm, its closure occurs on the 21-28th day after conception. If the formation of the neural tube is disturbed, depending on the location of the defect, either anencephaly or spina bifida is formed, which is clinically manifested by paralysis of the lower extremities, bladder, rectum, etc.
The occurrence of NTD is due to both hereditary factors and the influence of the external environment. Among hereditary features, one can single out gender and ethnic differences, an increased degree of concordance in monozygotic twins, gene mutations and chromosomal abnormalities (a small number of NTDs). It is necessary to take into account the fact of the birth of children with NTD in history and hereditary history. Drugs that interfere with folate metabolism (trimethoprim, sulfasalazine, carbamazepine, phenytoin, valproic acid and other anticonvulsants, etc.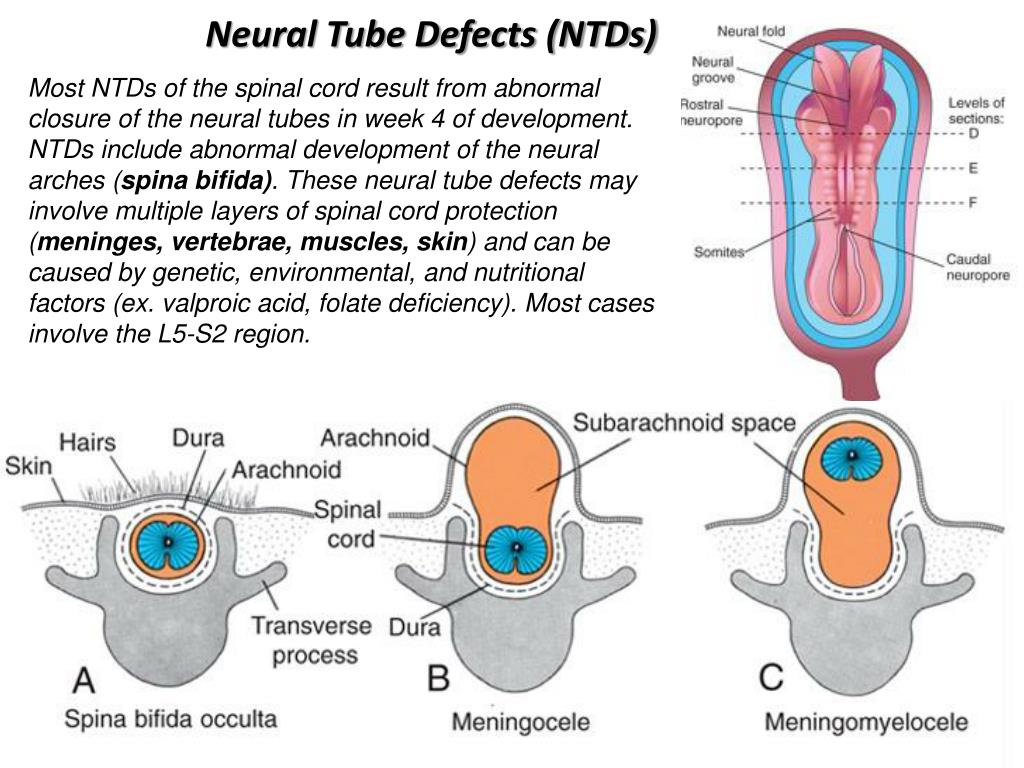 ), alcohol abuse, methanol can increase the risk of NTD. Acquired factors that can lead to the occurrence of NTD include diabetes mellitus, hyperthermia, smoking, etc. Factors such as place of residence, time of year at which conception occurred, mother's age, socio-economic conditions, as well as the nutritional factor. nine0009 The incidence of NTD varies from 2 (Mexico and Ireland) to 0.2 (Finland and Japan) per 1000 births, and the recurrence rate in subsequent pregnancies is 2%. Despite its low prevalence, spina bifida is the most common birth defect and results in disability.
), alcohol abuse, methanol can increase the risk of NTD. Acquired factors that can lead to the occurrence of NTD include diabetes mellitus, hyperthermia, smoking, etc. Factors such as place of residence, time of year at which conception occurred, mother's age, socio-economic conditions, as well as the nutritional factor. nine0009 The incidence of NTD varies from 2 (Mexico and Ireland) to 0.2 (Finland and Japan) per 1000 births, and the recurrence rate in subsequent pregnancies is 2%. Despite its low prevalence, spina bifida is the most common birth defect and results in disability.
DNT were described by the ancient Egyptians, and in 1641 N. Tulp first depicted spina bifida. The alimentary factor was one of the first to be recognized as a risk factor for the development of spina bifida. Stein et al. noted a high incidence of NTDs in 18-year-old boys entering the military who were born during the famine at the end of World War II. Hibbard and Smithells further showed that women who gave birth to children with NTDs experienced vitamin deficiencies during pregnancy.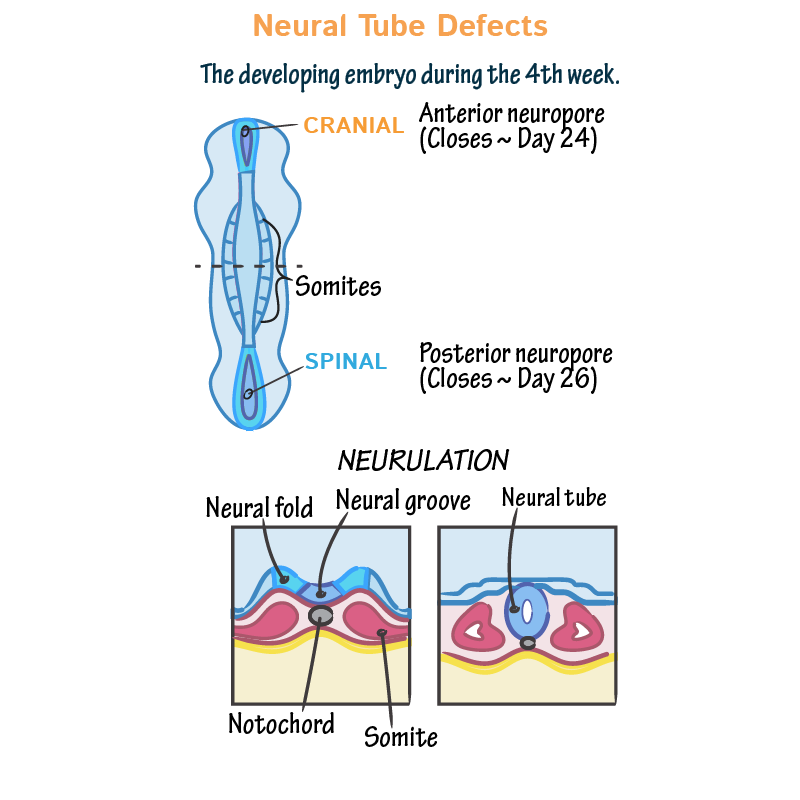 According to their observations, as a result of taking multivitamin complexes, the frequency of recurrence of this pathology in subsequent pregnancies was sharply reduced. nine0009 R.P. Steegers-Theunissen et al. for the first time suggested the existence of a link between the violation of folate-dependent processes of homocysteine (HC) metabolism and the development of NTD. Subsequently, they showed that the risk of spina bifida formation increases with an increase in the concentration of HC in the blood, and folic acid intake, in turn, reduces the content of HC in the blood plasma of pregnant women. The concentration of HC in the amniotic fluid in newborns born with NTD was higher than in the control group. When studying the metabolism of methionine in the extraembryonic and amniotic fluids, it was shown that the concentration of total HC in the embryonic fluid is significantly lower than in the mother's blood plasma, and the concentration of methionine is four times higher in the extraembryonic coelomic fluid and two times higher in the amniotic fluid compared to maternal plasma.
According to their observations, as a result of taking multivitamin complexes, the frequency of recurrence of this pathology in subsequent pregnancies was sharply reduced. nine0009 R.P. Steegers-Theunissen et al. for the first time suggested the existence of a link between the violation of folate-dependent processes of homocysteine (HC) metabolism and the development of NTD. Subsequently, they showed that the risk of spina bifida formation increases with an increase in the concentration of HC in the blood, and folic acid intake, in turn, reduces the content of HC in the blood plasma of pregnant women. The concentration of HC in the amniotic fluid in newborns born with NTD was higher than in the control group. When studying the metabolism of methionine in the extraembryonic and amniotic fluids, it was shown that the concentration of total HC in the embryonic fluid is significantly lower than in the mother's blood plasma, and the concentration of methionine is four times higher in the extraembryonic coelomic fluid and two times higher in the amniotic fluid compared to maternal plasma.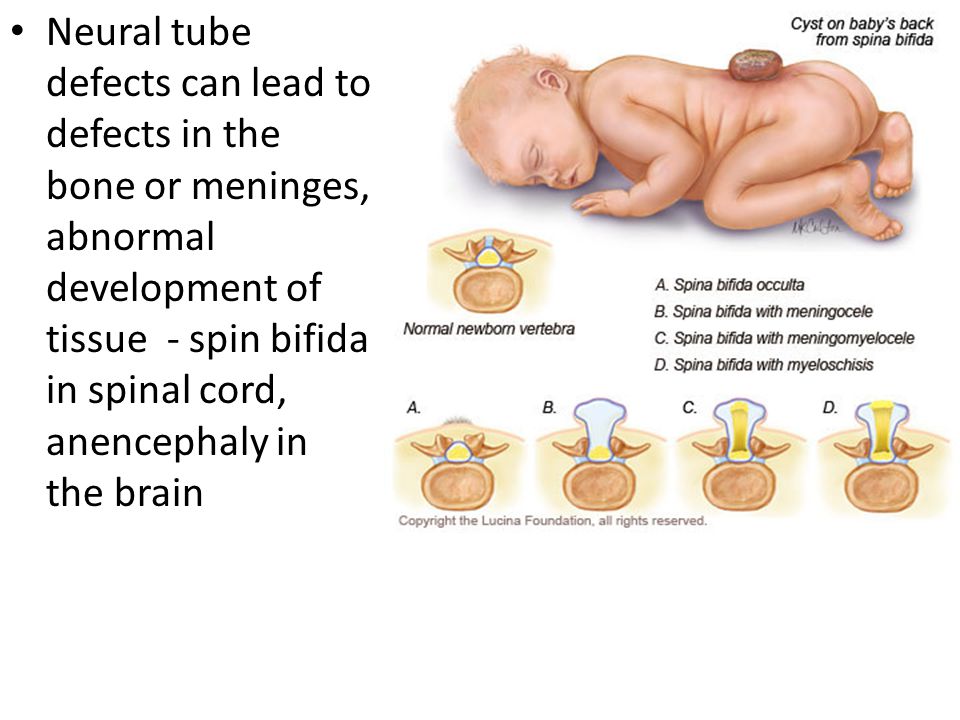 nine0009 In Denmark N.M. van der Put et al. revealed an increased frequency of C677T polymorphism of the gene encoding the enzyme methylenetetrahydrofolate reductase (MTHFR) in members of families in which children with NTD were born. The gene mutation was detected in 16% of mothers, 10% of fathers and 13% of newborns with spina bifida compared to 5% in the control group. Similar results have been obtained in other countries. This study shows that the risk of developing spina bifida increases seven-fold when a homozygous mutation in the mother and fetus is combined. This proves the influence of HC metabolism disorders in the fetus on the development of NTD. nine0009 The severity of spina bifida can be different - from erased forms to gross defects with spina bifida in combination with myeloschisis.
nine0009 In Denmark N.M. van der Put et al. revealed an increased frequency of C677T polymorphism of the gene encoding the enzyme methylenetetrahydrofolate reductase (MTHFR) in members of families in which children with NTD were born. The gene mutation was detected in 16% of mothers, 10% of fathers and 13% of newborns with spina bifida compared to 5% in the control group. Similar results have been obtained in other countries. This study shows that the risk of developing spina bifida increases seven-fold when a homozygous mutation in the mother and fetus is combined. This proves the influence of HC metabolism disorders in the fetus on the development of NTD. nine0009 The severity of spina bifida can be different - from erased forms to gross defects with spina bifida in combination with myeloschisis.
The severity of spina bifida is distinguished:
Vertebral dermal sinus
Hidden cleft of the vertebral arch;
cystic cleft of the arch;
Spina bifida associated with myeloschisis.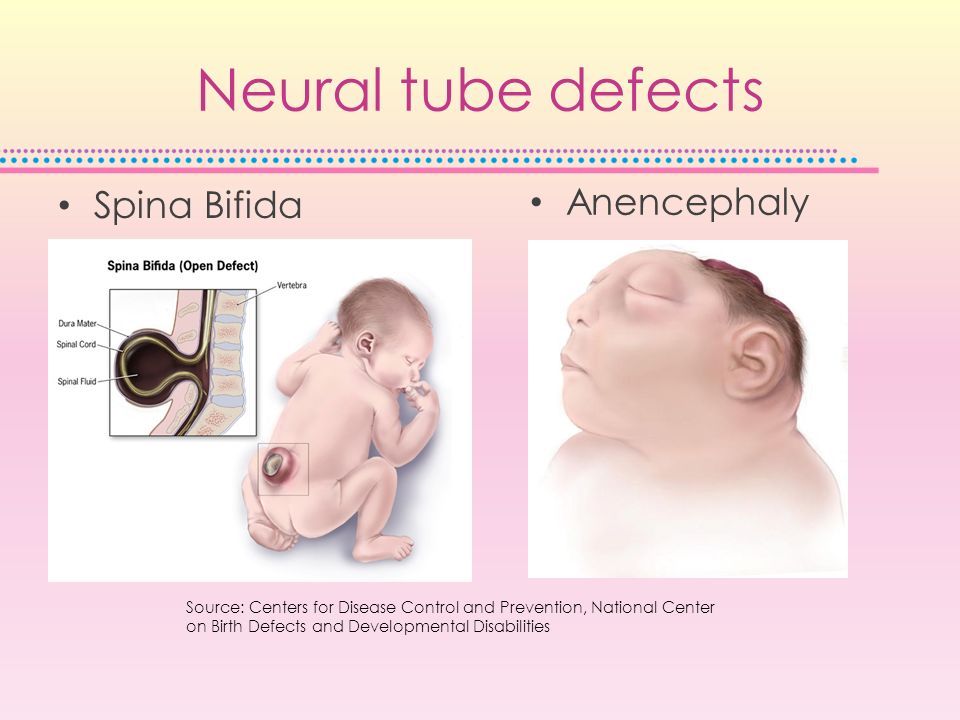
Despite the fact that NTDs have been known to man since ancient times, all the mechanisms for the development of this defect are still unclear, although there is no doubt that genetic factors, unbalanced nutrition (deficiency of folates and B vitamins), hyperhomocysteinemia (HHC), factors environment (radioactive radiation, etc.). nine0009 Most studies in recent years demonstrate the impact of disturbances in the metabolism of folate in the methionine cycle on the pathogenesis of NTD. Since these processes are inextricably linked with each other, deficiency or defects of any cofactor (B vitamins, folates) and enzymes, which can be either acquired or genetically determined, lead either to HHC or to erased or pronounced forms of folate deficiency states.
Many of the pathological effects of folate deficiency are associated with increased plasma levels of HC. The role of folates in the development of NTDs has been known for over 40 years, and the role of vitamins B 12 and B 6 were installed much later.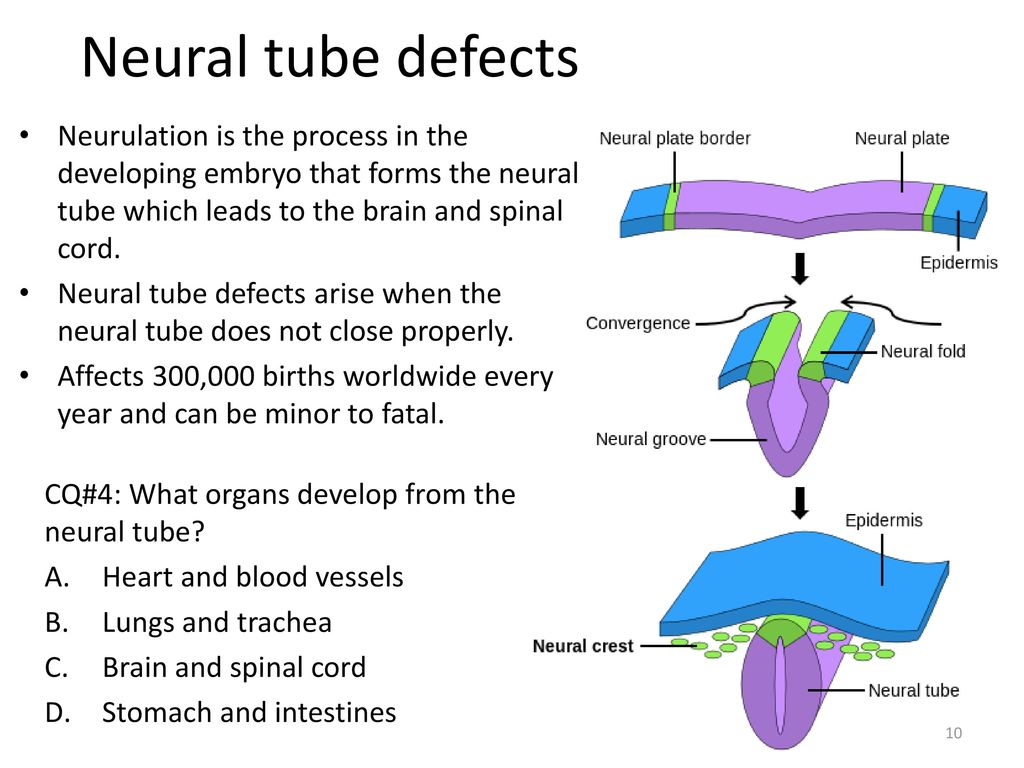 Intracellular vitamin B 12 acts as a factor in the remethylation of HC to methionine with the participation of the enzyme methionine synthetase (MS). Vitamin B deficiency 12 can thus cause HHC, although blood folate levels may be normal or even elevated. This phenomenon is known as the "methylfolate trap".
Intracellular vitamin B 12 acts as a factor in the remethylation of HC to methionine with the participation of the enzyme methionine synthetase (MS). Vitamin B deficiency 12 can thus cause HHC, although blood folate levels may be normal or even elevated. This phenomenon is known as the "methylfolate trap".
It should be emphasized that the combination of HHC and folate deficiency, including with a lack of B vitamins, especially vitamin B 6 , is a powerful risk factor for the development of not only NTD, but also vascular complications: venous and arterial thrombosis, preeclampsia, premature detachment of a normally located placenta, fetoplacental insufficiency and fetal growth retardation syndrome, antenatal fetal death, early and late miscarriages. Vitamin B 6 in the form of pyridoxol-5-phosphate, it participates in the transsulfation of HC to cysteine with the help of the enzyme cystathionine-beta-synthetase (CBS).
The metabolism of HC is inextricably linked to the methionine cycle.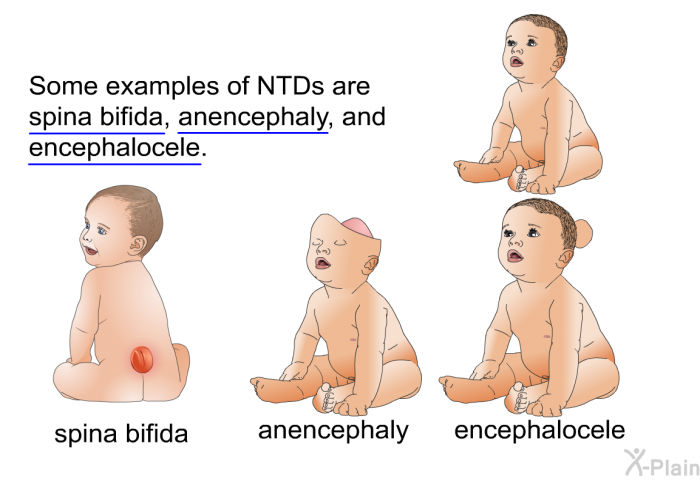 The synthesis of HC (in high concentrations - a cytotoxic amino acid) is the result of the formation of labile methyl groups due to the chemical processes of the methionine cycle. The formation of HC occurs in all cells, but the ways of its utilization differ. Most cells and tissues are able to remethylate HC (with the participation of folates, vitamin B 12 ), and only a few can carry out transsulfation processes. This, apparently, can explain the high efficiency of folic acid and B vitamins in reducing the level of HC in blood plasma.
The synthesis of HC (in high concentrations - a cytotoxic amino acid) is the result of the formation of labile methyl groups due to the chemical processes of the methionine cycle. The formation of HC occurs in all cells, but the ways of its utilization differ. Most cells and tissues are able to remethylate HC (with the participation of folates, vitamin B 12 ), and only a few can carry out transsulfation processes. This, apparently, can explain the high efficiency of folic acid and B vitamins in reducing the level of HC in blood plasma.
The nervous tissue uses the following mechanisms to maintain the concentration of HC at the proper level:
remethylation with the participation of methionine synthetase with a normal content of vitamin B 12 and folates;
the transition of HC under the action of the enzyme cystathionine-beta-synthetase into cystathionine, which is a less toxic product for the brain and is subsequently used for the synthesis of cysteine; nine0009 export of HC to the blood.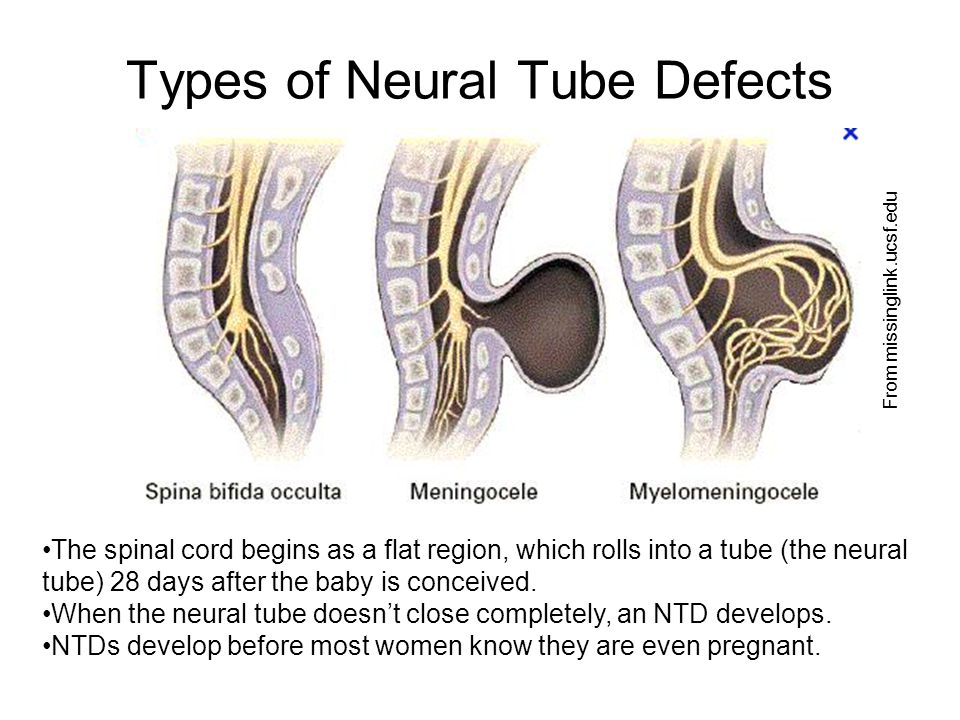
In the nervous system, as in other organs, HC metabolism disorders can occur as a result of genetic disorders, after taking various drugs and under the influence of other acquired factors.
The concentration of HC in the blood of pregnant women is 50-60% lower than outside pregnancy. Pregnancy is characterized by a change in the hormonal profile, an increase in circulating blood volume, cardiac output, peripheral vasodilation, changes in kidney function, and an increase in body weight. Possible reasons for the decrease in the concentration of HC are hemodilution, increased synthesis of steroids, as well as the consumption of methionine and HC by the growing fetus. nine0009 A number of studies have shown that oral contraceptives (OCs), containing even less than 50 micrograms of estrogen (in modern preparations - no more than 35 micrograms), disrupt the kinetics of folates, and in the blood of women using OCs, the content of vitamin A is increased and the concentration of vitamin B is reduced 12 and folic acid. Thus, the risk of developing NTD is higher in patients who became pregnant immediately after long-term use of OCs, especially in the presence of genetic mutations in enzymes (MTHFR, MS, etc.), and who did not additionally take folic acid and B vitamins.
Thus, the risk of developing NTD is higher in patients who became pregnant immediately after long-term use of OCs, especially in the presence of genetic mutations in enzymes (MTHFR, MS, etc.), and who did not additionally take folic acid and B vitamins.
Studies on the role of vitamin B 12 in the process of HC remethylation and in the genesis of the development of NTDs, have been carried out in the last 5-10 years. It is proved that the participation of vitamin B 12 as a cofactor provides a more complete and rapid absorption of folic acid by cells. Study by M. Paskal et al. on vitamin B content 12 in the blood plasma of mothers who gave birth to children with spina bifida, showed that a decrease in the concentration of vitamin B 12 in maternal serum levels below 185 mmol / l correlates with a 3.5-fold increase in the risk of having a child with spina bifida. Average concentrations of vitamin B 12 in mothers of the spina bifida group were 21% less compared to the control group, while the differences between the concentrations of folate, vitamin B 6 and HC in blood serum and erythrocytes was not observed.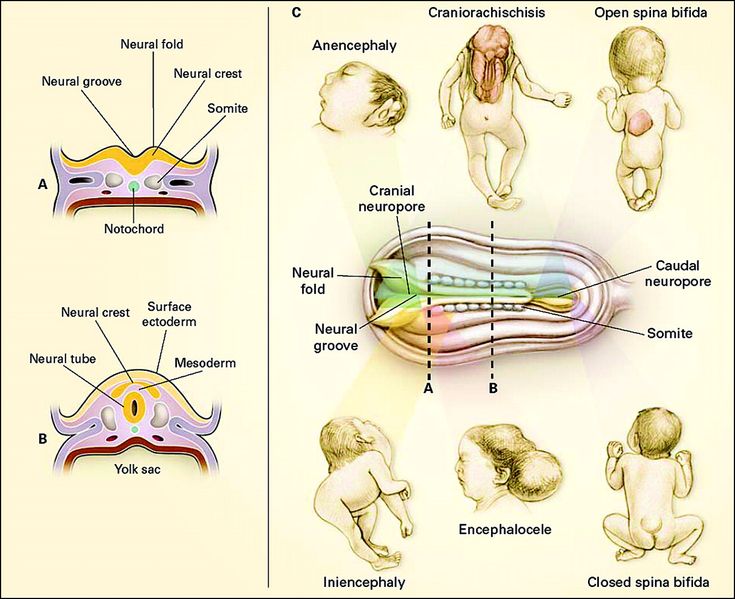 These data confirm the multifactorial nature of the origin of NTDs and the need to include vitamin B 12 along with folate in the prevention of fetal NTDs.
These data confirm the multifactorial nature of the origin of NTDs and the need to include vitamin B 12 along with folate in the prevention of fetal NTDs.
A special risk group for deficiency of folates and vitamins of group B are patients who have received hormonal contraception for a long time, as well as smokers, coffee abusers (more than 5 cups a day) and, of course, patients with genetic factors (mutation MTHFR, CBS, transcobalamin), malabsorption , unbalanced nutrition, diagnosed with HHC and fetal NTD in history. It should also be taken into account that up to 80% of women aged 18 to 40 have suboptimal blood folate concentrations. nine0009 Prophylactic administration of folates and B vitamins, as well as dietary adjustments, significantly reduce the incidence of neural tube defects in the fetus. Thus, in Dublin, cereals (grain fortification), which are an important part of the Irish diet, were enriched with vitamin B 12 (1981) and folic acid (1987), which led to a decrease in the frequency of birth of children with NTD from 4.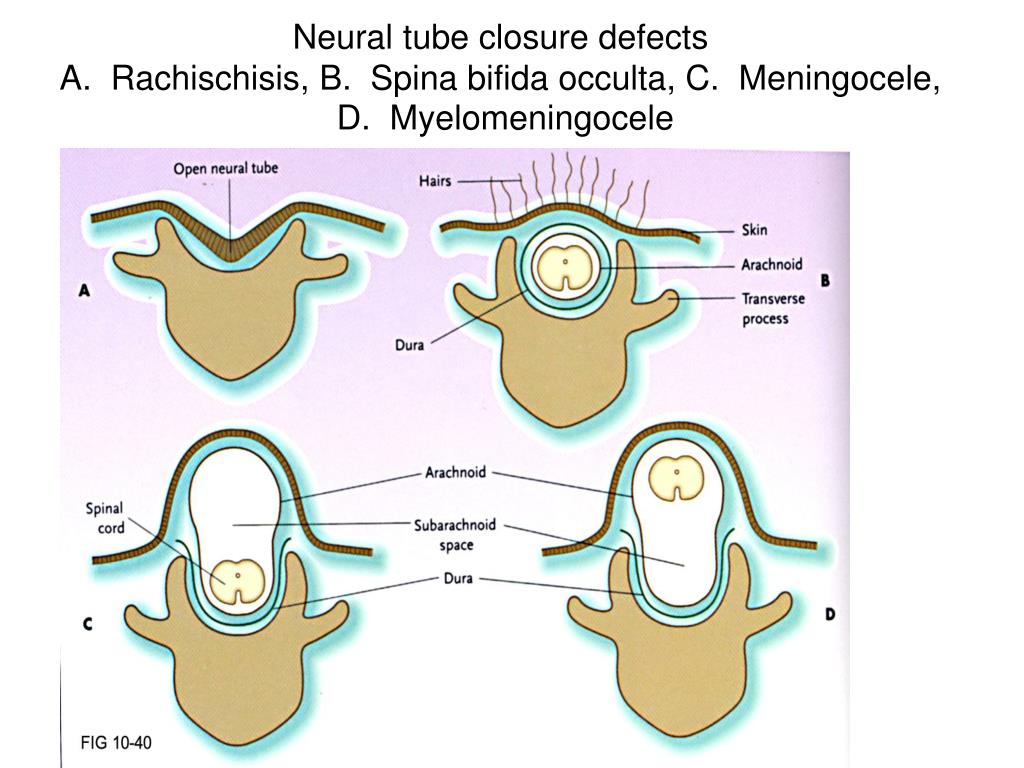 7 to 1.3 per 1000 newborns. NTD prevention has become a National Health Program in many developed countries. For example, the United States and Canada introduced a program to fortify grains with folates to reduce the risk of having children with NTDs, which resulted in a decrease in the number of newborns with NTDs by 19% (M.A. Honein et al., 2001). In a number of countries, there is a preference for programs aimed at the preventive use of folate-containing drugs by women of childbearing age. Thus, according to a multicenter study conducted in 33 clinical centers in England (1817 women examined), more than 75% of cases of NTD can be prevented by prescribing folic acid and vitamin B 12 .
7 to 1.3 per 1000 newborns. NTD prevention has become a National Health Program in many developed countries. For example, the United States and Canada introduced a program to fortify grains with folates to reduce the risk of having children with NTDs, which resulted in a decrease in the number of newborns with NTDs by 19% (M.A. Honein et al., 2001). In a number of countries, there is a preference for programs aimed at the preventive use of folate-containing drugs by women of childbearing age. Thus, according to a multicenter study conducted in 33 clinical centers in England (1817 women examined), more than 75% of cases of NTD can be prevented by prescribing folic acid and vitamin B 12 .
Current issues of optimal prevention of fetal NTDs are the duration of use and the dose of folic acid. According to the recommendations of various international organizations (including the Food and Drug Administration, USA; March of Dimes CDC-Alanta - Spina Bifida Assotiation Public Health Service; Reino Unido Junta de Sanidad y Consumo de Espana, 2001, etc.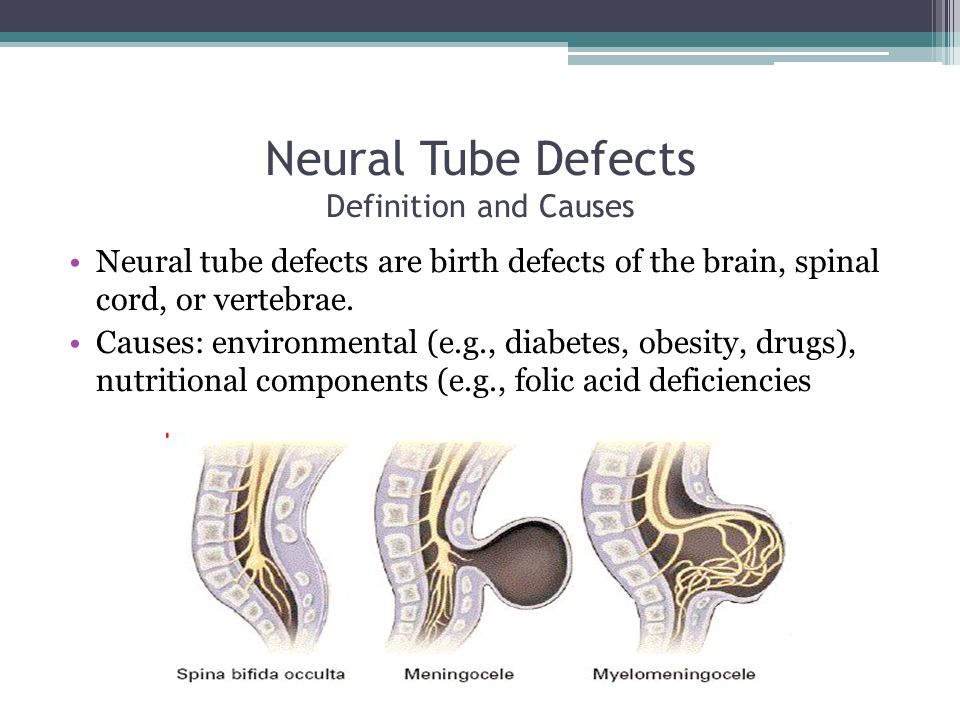 ), women with an uncomplicated history of NTD should receive 400 micrograms of folic acid per day in combination with vitamin B 12 at a dose of 2 mcg / day at least a month before conception and during the first trimester of pregnancy. In Italy, since 2005, the need for a daily intake of 400 micrograms of folic acid by women planning a pregnancy has been legally approved.
), women with an uncomplicated history of NTD should receive 400 micrograms of folic acid per day in combination with vitamin B 12 at a dose of 2 mcg / day at least a month before conception and during the first trimester of pregnancy. In Italy, since 2005, the need for a daily intake of 400 micrograms of folic acid by women planning a pregnancy has been legally approved.
In light of recent scientific evidence, it is important that, in addition to folic acid, drugs intended for the prevention of fetal NTD include vitamin B 12 .
Printed in abbreviated form.
nine0004 Published in the magazine "Pharmateka" No. 1 (136), 2007- Number:
- № 4/1 March - Pediatrics
01/06/2023 CardiologyTherapy and family medicine Post-covid syndrome: rational pharmacotherapy in patients with symptoms from the side of the cardiovascular system
More patients will be treated after being infected with the SARS-CoV‑2 coronavirus.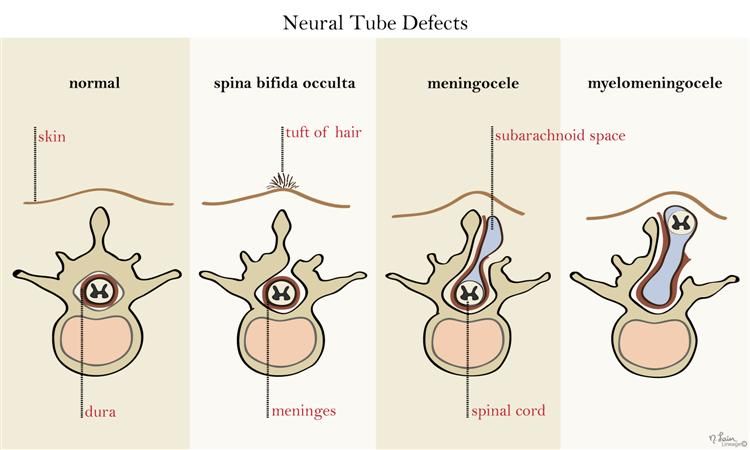 However, close to 10% of cases report self-perceived filth and unacceptable symptoms after three or more common ailments. Patients with high cardiovascular (CV) risk and verification of cardiovascular pathologies occupy a special place in the structure of illness for post-covid syndrome. ...
However, close to 10% of cases report self-perceived filth and unacceptable symptoms after three or more common ailments. Patients with high cardiovascular (CV) risk and verification of cardiovascular pathologies occupy a special place in the structure of illness for post-covid syndrome. ...
01/06/2023 CardiologyTherapy and family medicineTreatment of arterial hypertension in patients with metabolic diseases
on the Central Congorian Congress Cardiologi Kholesyan, Yaky Vid, 20-23 Veresnya, INOMANI TOITHYSHYSYYYYA MALIS OF THE STARTIONS OF THE STRARICHIA TO KNOW IMDICHICHICHICHICHICHICHICHICHICHICHICHICA Victorious digital technologies, participants in the largest trend in cardiology, zokrema, shared the rest of their achievements in science and clinical practice with colleagues from all over the world.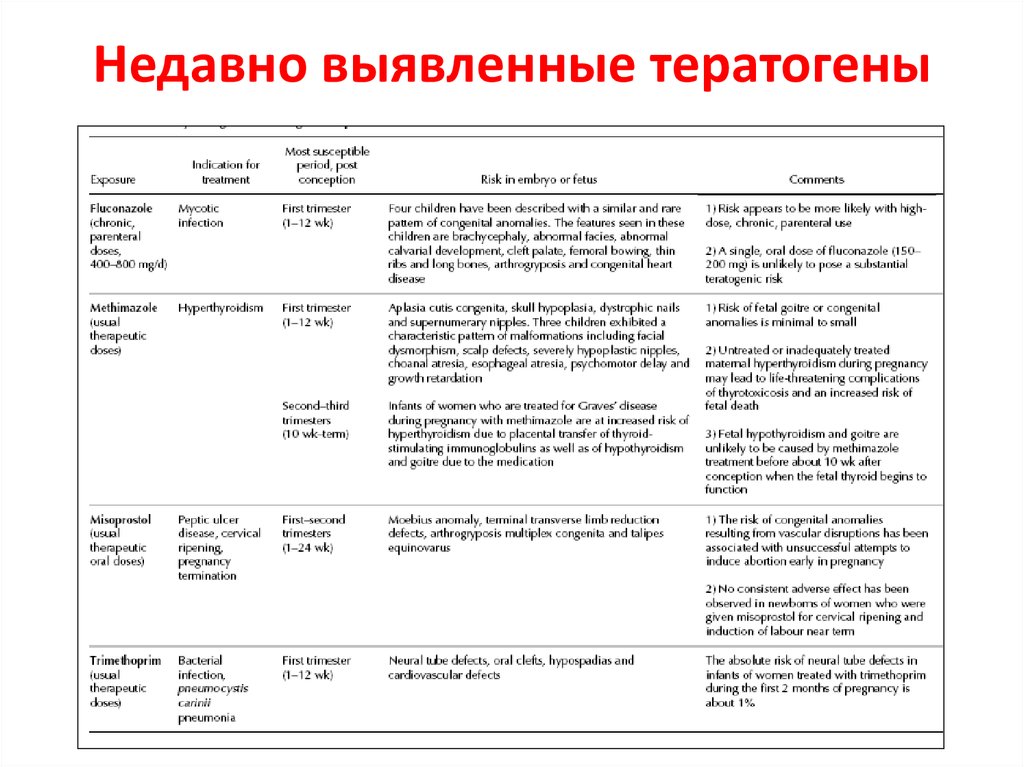 ...
...
01/06/2023 Cardiology "Happiness in the gut": current possibilities of antiarrhythmic therapy
to Vashiy respect, the recommendation of the recommendation of the Cardiologiiv (ESS, 2022) Shto Ottsiyunnnya of the Sudyno systems is the Vedennya Patzyntiv, the Yaki, they transferred the non-reeds (NKV). Indicate to establish and evaluate the evidence of evidence to help medical practitioners to promote the best treatment strategies for a patient with severe illnesses, and also to make it easier to make decisions in practical practice. ... nine0003
Fomina Clinic — a network of multidisciplinary clinics
We have already found out that when planning a pregnancy, the lifestyle of the expectant mother plays an important role, namely the rejection of bad habits, proper nutrition, hygiene and sports.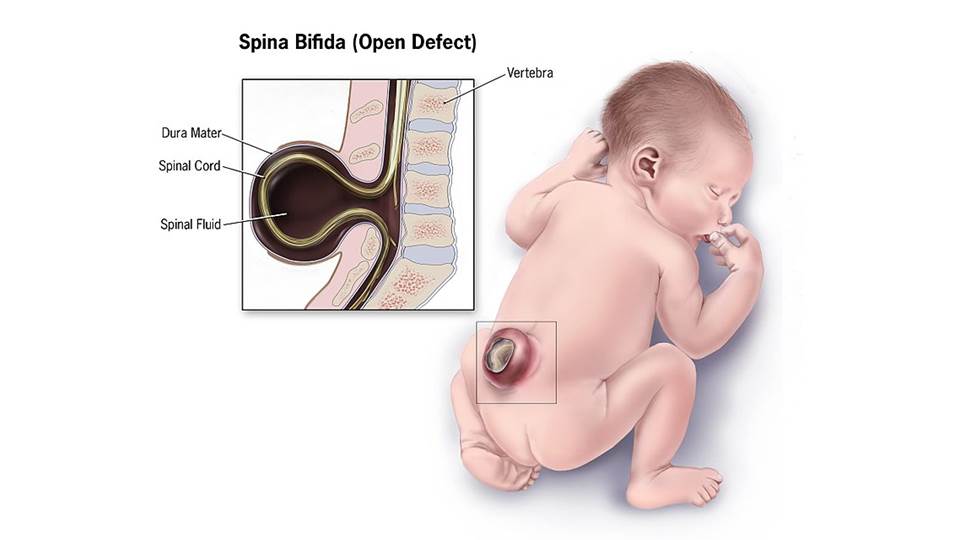 Vitamins play an important role in this, namely folic acid, which is advised to start taking 1-3 months before the expected pregnancy. It is its use that prevents possible malformations that can lead to the death of the child. nine0003
Vitamins play an important role in this, namely folic acid, which is advised to start taking 1-3 months before the expected pregnancy. It is its use that prevents possible malformations that can lead to the death of the child. nine0003
This is a B vitamin that prevents neural tube defects in the fetus. Moreover, it is important to understand that such an effect is possible only if folic acid begins to enter the mother's body before pregnancy and continues to be taken during pregnancy. Thus, from the first days after conception, the child begins to develop in the right conditions, because by this time folic acid has time to get into your bloodstream in sufficient quantities.
Unfortunately not. The fact is that violations of the laying of the neural tube usually occur on the 18th - 30th day after conception, when a woman may still not know about her pregnancy. nine0003
Let's start with the statistics: neural tube defects (yes, there are several!) are found in about 7 out of 10,000 newborns, and it is believed that in half of these cases they are caused by a lack of folic acid in the mother's diet.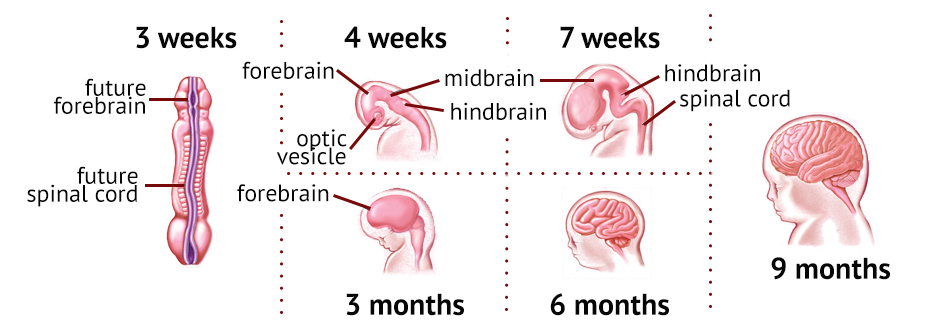
The two most common neural tube defects are:
- Spina bifida damages the spinal cord: with this defect, most children survive and reach adulthood, but they may be accompanied by central nervous system disorders throughout life, such as paralysis or inability to control urination and defecation; nine0089
- with anencephaly, the entire brain or a significant part of it is missing, in which case most children die shortly after birth.
Recommended foods include: Green vegetables, legumes (beans, peas, lentils), lettuce, berries, citrus fruits (fruits and juices), breakfast cereal, whole grain bread/bread.
This, of course, is not enough, because in most of these products the content of folic acid is less than 20% (or even 10%) of the recommended daily amount by doctors. The only exception is lentils, one glass of which contains 90%. Therefore, additionally every day when planning pregnancy and throughout its duration, you need to take vitamins that contain 400 mcg of folic acid.