Tingling feet during pregnancy
REASONS FOR TINGLING IN PREGNANCY - Healthcare Wellness Blogs
As if being pregnant wasn’t taxing and overwhelming enough, expectant mothers might also endure some unusual symptoms, particularly in the latter months. Consider the sensations of numbness and tingling. Toward the conclusion of their pregnancy, some pregnant women may have “pins and needles” or numbing sensations in their hands, fingers, legs, back, or buttocks.
Not only may these sensations be annoying and even painful, but they can also leave you wondering, “What precisely is going on here?“
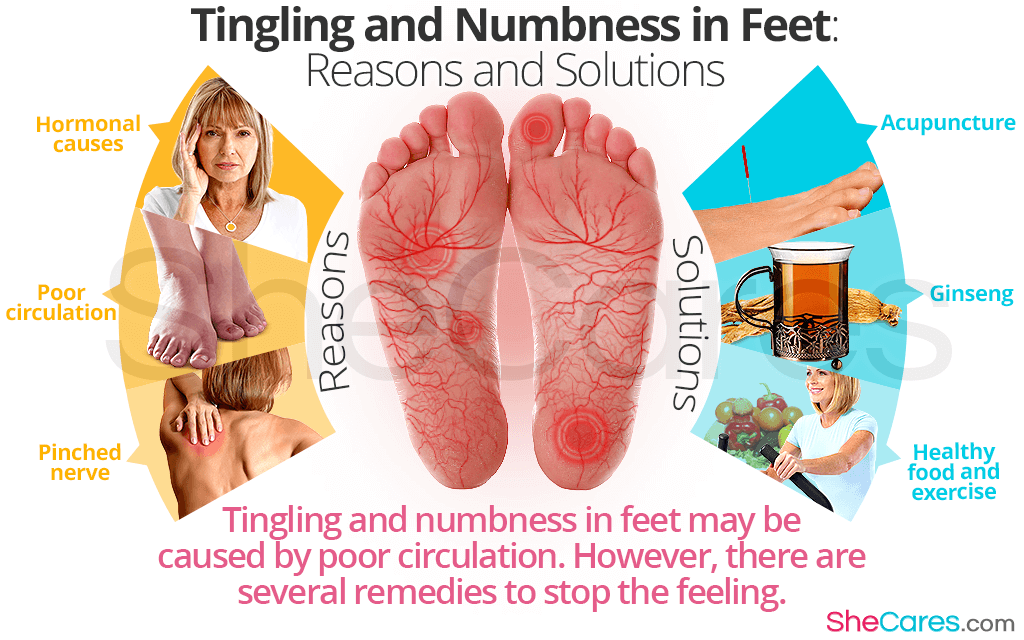
Lack of sleep is the most common cause of tingling in the second trimester. The feelings of numbness become more severe during the third trimester when blood vessels are constricted by the larger uterus and the changes women make to their sleeping positions. There are no definite remedies for tingling or numb tongue, numb stomach or tummy, or numb legs and feet during this period, but there are suggested measures or techniques to treat them.
Symptoms
The following are the most prevalent numbness and tingling sensations in pregnancy:
- Symptoms worsen when you wake up, in the middle of the night, or when you move your body in specific ways.
- It may feel like “pins and needles,” numbness, or a radiating burning or tingling feeling followed by pain.
- As weight growth and fluid retention rise near the middle or end of pregnancy, this symptom appears.
Causes
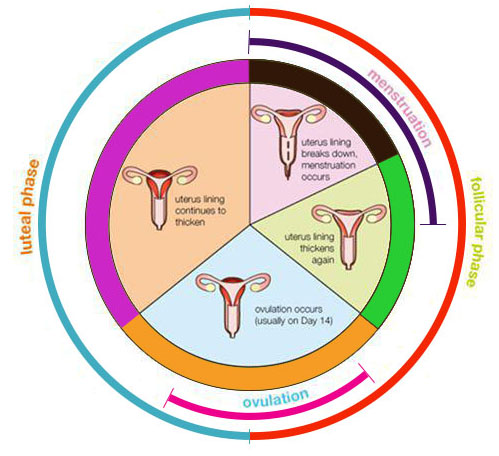
Hormones, as well as the usual biological changes you’re going through, are responsible for the numbness and tingling you’re feeling. Your body creates more relaxin as your pregnancy continues, allowing your ligaments to extend during pregnancy and labor.
However, your posture and center of gravity alter as a result of more relaxin. Your nerves may be squeezed as a result, resulting in shooting pain and tingling down your legs, thighs, back, and buttocks.
Similarly, when your uterus becomes larger and fuller, it places an unusual amount of strain on your muscles, ligaments, and nerves, which can cause numbness and tingling.
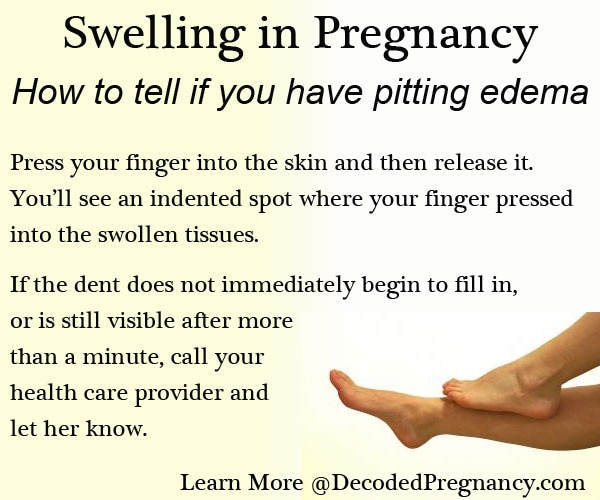
Swelling of the hands and feet is typical in the second and third trimesters of pregnancy owing to water retention. This swelling can cause numbness and tingling in your fingers and toes, as well as place strain on nerves in your wrists, back, legs, thighs, and buttocks.
Fingers and Hands
Numbness and tingling feelings in your hands and fingers are not uncommon, especially as your pregnancy continues. This extra fluid exerts pressure on the median nerve in the wrist, producing carpal tunnel syndrome in certain women.
Carpal Tunnel Syndrome during pregnancy –
Carpal tunnel syndrome is very common during pregnancy, with up to 62 percent of pregnant women suffering from it.
Fluid retention, increased weight gain, and hormonal shifts are all causes of carpal tunnel syndrome during pregnancy.
The majority of cases of carpal tunnel syndrome occur in the last few months of pregnancy, however if you’ve had carpal tunnel syndrome before or outside of pregnancy, your symptoms may appear sooner. Symptoms may appear in one or both hands, however symptoms in your dominant hand are generally more severe.
Symptoms may appear in one or both hands, however symptoms in your dominant hand are generally more severe.
You may encounter the following symptoms if you have carpal tunnel syndrome:
1. Feelings of burning in the hand, wrist, and arm
2. Having trouble gripping items
3. Hand, wrist, and finger numbness
4. In the fingers and hands, there are “pins and needles.”
5. Finger numbness, particularly in the thumb, index, and middle fingers
6. Shoulder, neck, and arm discomfort that radiates
7. Swelling of the fingers and hands
Swelling — all over – is one of the most prevalent pregnant symptoms. Puffiness in the cheeks, legs, and feet is common among patients. However, swelling inside the wrist might cause carpal tunnel syndrome in certain women (CTS).
Carpal tunnel syndrome affects about 4% of individuals in the general population, while it affects 31% to 62 percent of pregnant patients. After 30 weeks of pregnancy, many individuals begin to experience symptoms.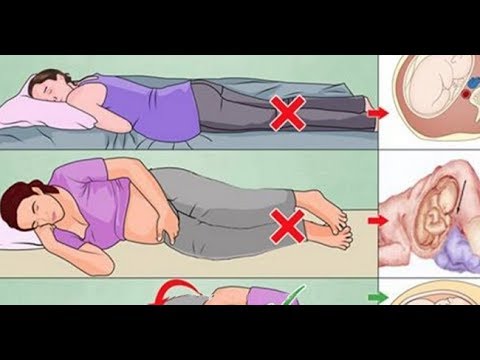
Your blood volume doubles during pregnancy. The additional fluid causes swelling and pressure in your blood vessels all over your body. Swelling can compress the median nerve, which runs to the hand, in tiny areas like the carpal tunnel region of the wrist, through which nine tendons and one nerve travel.
The palm-side surfaces of the thumb, index, and middle fingers, as well as part of the ring finger, are all supplied by the median nerve. It’s also in charge of moving the muscles in your hand that bend your fingers. Nerve compression in the wrist and hand can produce discomfort, tingling, and numbness, which might get worse when you’re attempting to sleep. Pregnancy may be the first time a woman has CTS symptoms, or it may be the final straw that prompts her to seek medical help for her problems.
Buttocks, back, and legs
Lower back discomfort is typical during pregnancy, and it can occasionally spread down your legs and buttocks, especially if pressure is placed on your nerves.
During pregnancy, numbness and tingling in the legs, back, and buttocks are most commonly caused by:
- Retention of fluid
- Relaxin is a hormone that causes your ligaments to loosen.
- Your uterus is developing, and your organs are being crushed.
- Gaining weight
All of this strain, ligament loosening, weight gain, and fluid retention can take a toll on your health. Your muscles may become tight or weak, and your posture may shift as a result.
When you lean forward or backward more frequently, your back muscles have to work harder, resulting in tightness and suffering. When you’re pregnant, you’re also more susceptible to back problems caused by activity.
Due to the hormone relaxin, many women will suffer hypermobility in their joints during pregnancy. The trouble is that all of this flexibility and opening up can cause your body to become unstable, resulting in shooting pain, discomfort, numbness, and tingling in your lower back or legs.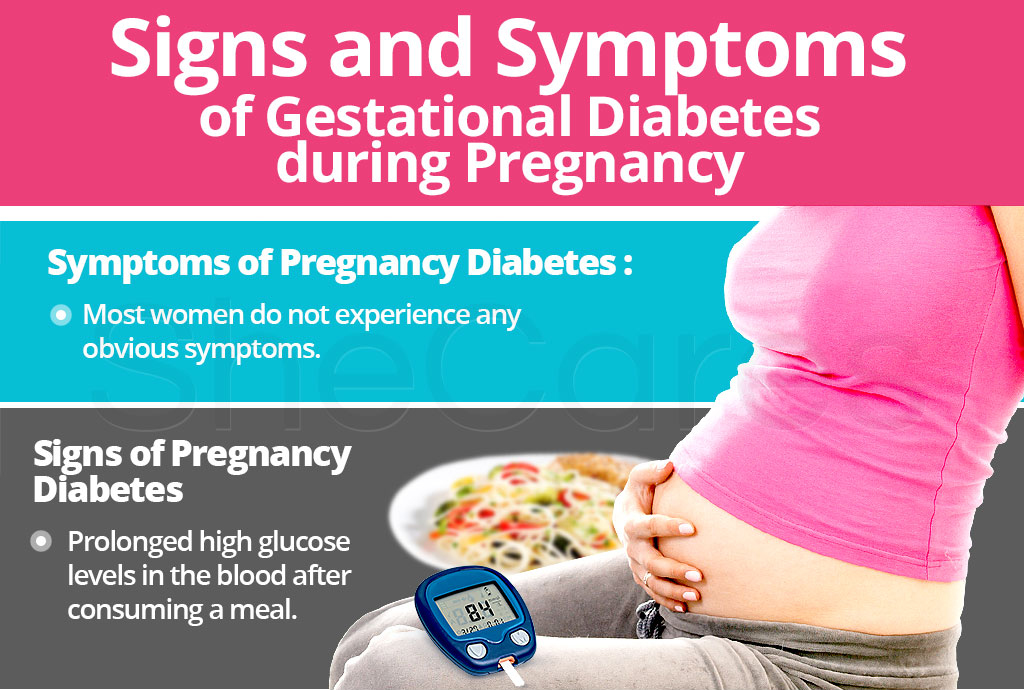
Pregnancy Sciatica
Sciatica, which is caused by a pinched sciatic nerve, is probably the most prevalent cause of tingling and numbness in the back, legs, and buttocks during pregnancy.
This ailment normally appears in the third trimester of pregnancy and is usually moderate, but for some women it can be devastating.
Pain, burning, and aching are some of the symptoms.
Sensations on one side of the body, although sometimes both sides are affected
Symptoms that start in the lower back and spread to the hips, buttocks, and down the leg
Muscle weakness, tingling feelings, and numbness
Pregnancy Meralgia Paresthetica
While sciatica is a frequent pregnant ailment that causes numbness and tingling in the back, legs, and buttocks, a disease known as meralgia paresthetica can also occur. Pressure on the lateral femoral cutaneous nerve (LFCN), which runs along the front and side of your thigh, causes meralgia paresthetica.
Among the signs and symptoms are:
- Aching and discomfort in the thigh that may spread to the outside of the knee
- It’s also possible to have numbness and burning feelings.

- Symptoms include as a “stabbing” sensation in the thigh
- Symptoms that generally affect only one leg (though sometimes the buttocks area is involved as well)
Treatment
A gentle massage, making sure to change your sleep positions (using a pregnancy body pillow helps a lot), soothing baths, and stretching can all assist with general numbness and tingling of the hands, fingers, back, legs, and buttocks during pregnancy.
Additionally, once your problem has been diagnosed, your doctor may propose therapy.
Carpal Tunnel Syndrome Treatments
- Ice packs are used to alleviate edema.
- Hands and wrists should be elevated.
- Pain relievers that are safe to use during pregnancy
Treatment for Meralgia and Sciatica Paresthetica
- Pads for heating
- Massage therapy is a type of treatment that involves mass
- Physical therapy is a type of treatment that is used
- Pain relievers that are safe to use during pregnancy
- Sleep on the non-affected side of your body.

- Showers or baths that are warm to keep your wrist in a neutral posture, use a wrist brace or splint
How Do You Deal With Tingling During Pregnancy?
During pregnancy, these solutions may assist with numbness or tingling in the hands, fingers, legs, back, or buttocks.
- Numbness can be relieved by soaking your hands in warm water or applying a hot compress.
- While sleeping, avoid resting on your hands to avoid exacerbating the numbness and pain.
- Consult your doctor before using a wrist brace. It may be used to keep your wrist in a neutral position, especially when sleeping.
- Continuously stretch your hands and wrists while conducting any task. Tingling and soreness may be relieved by repetitive activities such as shaking or rubbing.
- To the side that is not affected by numbness or discomfort, sleep easily.
- Numbness can be caused by swelling, which can be reduced by using an ice compress.

- Acupuncture and massage treatment are examples of alternative therapies that can help with numbness-related discomfort.
- Do not stand for long periods of time as this may cause numbness or tingling in the legs and toes.
- You can sleep on one side, with both knees raised up and a cushion between them. This may help to prevent numbness.
- You can slightly stretch your knees while sitting so that they are at or above the level of your hips.
- If you have trouble balancing your body, use a walker or cane to get around.
- Consult your doctor and attempt some gentle workouts to help strengthen your muscles.
Is it possible to avoid tingling?
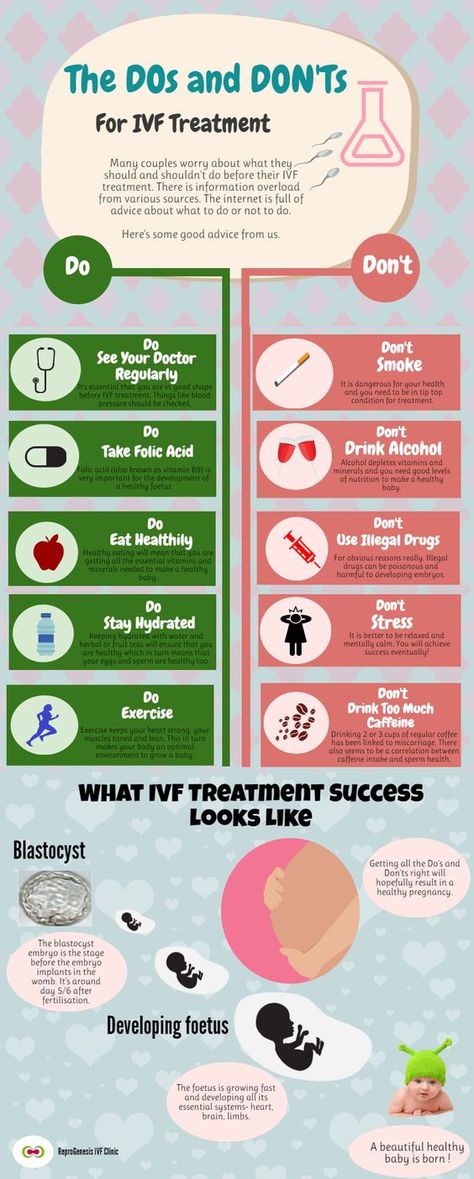
You may not be able to prevent tingling, but you may minimize your risks by making dietary and lifestyle adjustments.
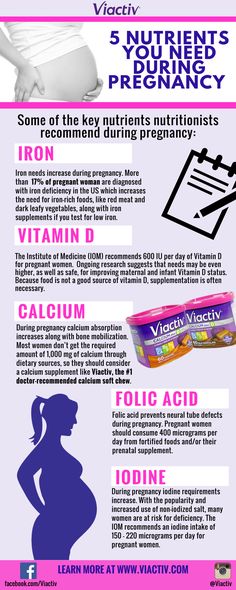
- To gain a healthy pregnancy weight, eat a nutritious and balanced diet.
- Reduce your intake of salt, sugar, and fats, and drink plenty of water. Check with your doctor before taking any supplements.
- Avoid alcohol because the chemicals in it might induce nerve damage and numbness.
- Reduce the amount of time you spend doing things like typing, crocheting, or sewing, especially if you’re prone to carpal tunnel syndrome.
- Get a supportive maternity bra to relieve the strain on your median nerve caused by the weight of your breastbone and rib cage.
- When sitting, standing, or sleeping, it is critical to maintain proper posture.
- Wear shoes with soft soles that are well-fitting and non-skid.
When Should You Visit Your Doctor?
The majority of incidences of numbness and tingling during pregnancy are frequent and normal. Any new symptoms, on the other hand, should be shared with your healthcare physician. If you have any symptoms in addition to the numbness and tingling, such as vaginal bleeding, severe stomach discomfort, contractions, severe headaches, hazy vision, or significant swelling, contact your healthcare professional immediately.
Weight increase, fluid retention, and hormones are the most common causes of numbness and tingling during pregnancy. In some circumstances, such as pregnancy-induced carpal tunnel syndrome, sciatica, or meralgia paresthetica, a pinched nerve may be implicated. In some circumstances, all that is necessary for relief is at-home remedies, physical therapy, or doctor-approved pain medication.
Although most cases of numbness and tingling during pregnancy are harmless, numbness and tingling are indicators of certain more dangerous diseases. If you suspect any of the illnesses listed below, go to your doctor right away because they can lead to grave issues during pregnancy.
Anemia
Iron-deficiency causing anemia can produce “restless leg syndrome” during pregnancy, which can be accompanied by tingling or a “creepy-crawly” sensation in the legs.
Nerve damage from a B12 shortage during pregnancy can cause numbness and tingling in the hands, as well as overall muscular weakness, difficulty walking, memory loss, and mental health issues.
Preeclampsia
Preeclampsia is a dangerous pregnancy syndrome that can cause significant swelling and numbness and tingling. Call your doctor right away if your tingling and numbness feelings are followed by visual problems, severe headaches, decreased urine output, severe stomach pain, vomiting, nausea, or seizures.
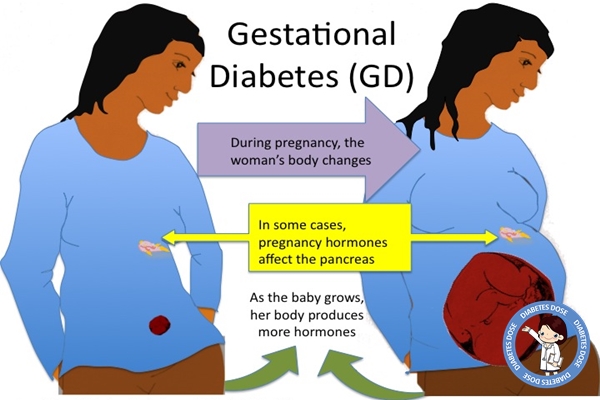
Diabetes during Pregnancy
Tingling and numbness in the hands and feet are common signs of gestational diabetes. If you’ve already been diagnosed with gestational diabetes, these symptoms might indicate that your condition isn’t being effectively controlled.
Tingling and numbness, as well as any other new symptoms that may be related to your gestational diabetes diagnosis and management, should be discussed with your healthcare practitioner.
Pregnancy is full of unexpected twists and turns. Most of us aren’t aware of the wide range of uncommon pregnancy symptoms, but now you can add numbness and tingling in the fingers, hands, legs, back, and buttocks to that list.
However, you should be assured that, while these symptoms might be annoying at times, they are typically not significant and will diminish once your baby comes. Although any new pregnancy symptom should be taken carefully, numbness and tingling by themselves seldom suggest a more serious issue.
Aches and pains during pregnancy: MedlinePlus Medical Encyclopedia
During pregnancy, your body will go through a lot of changes as your baby grows and your hormones change. Along with the other common symptoms during pregnancy, you will often notice new aches and pains.
Headaches are common during pregnancy. Before you take medicine, ask your health care provider if it is safe to take. Other than medicine, relaxation techniques may help.
Headaches can be a sign of preeclampsia (high blood pressure during pregnancy). If your headaches get worse, and they do not go away easily when you rest and take acetaminophen (Tylenol), especially toward the end of your pregnancy, tell your provider.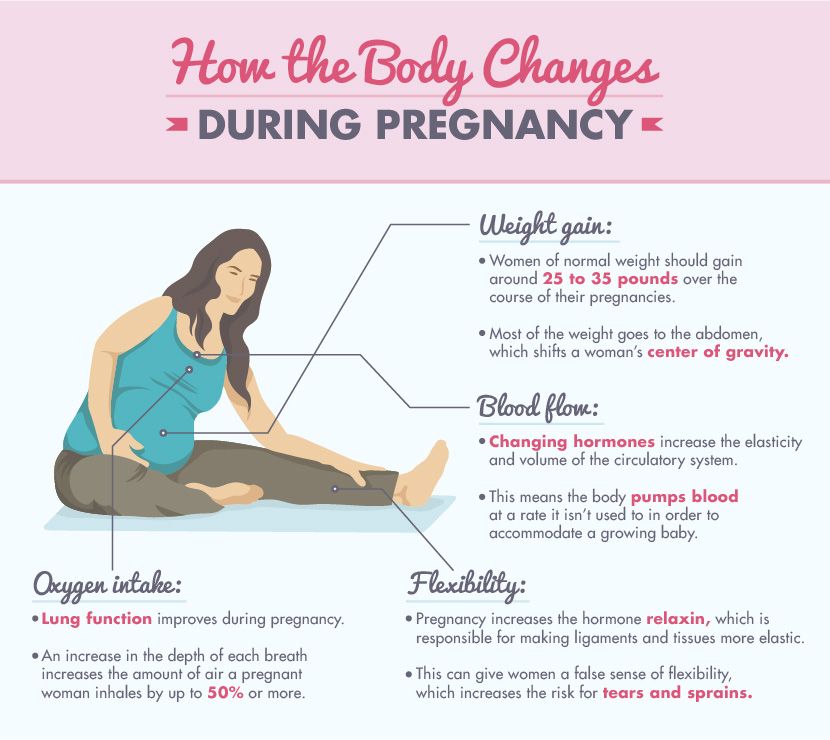
Most often, this happens between 18 and 24 weeks. When you feel stretching or pain, move slowly or change positions.
Mild aches and pains lasting for short periods of time are normal. But see your provider right away if you have constant, severe abdominal pain, possible contractions, or you have pain and are bleeding or have fever. These are symptoms that can indicate more severe problems, such as:
- Placental abruption (the placenta separates from the uterus)
- Preterm labor
- Gallbladder disease
- Appendicitis
As your uterus grows, it may press on the nerves in your legs. This may cause some numbness and tingling (feeling of pins and needles) in your legs and toes. This is normal and will go away after you give birth (it may take a few weeks to months).
You may also have numbness or tingling in your fingers and hands. You may notice it more often when you wake up in the morning. This also goes away after you give birth, though, again, not always right away.
If it is uncomfortable, you can wear a brace at night. Ask your provider where to get one.
Have your provider check any persistent numbness, tingling, or weakness in any extremity to ensure there is not a more serious problem.
Pregnancy strains your back and posture. To avoid or reduce backaches, you can:
- Stay physically fit, walk, and stretch regularly.
- Wear low-heeled shoes.
- Sleep on your side with a pillow between your legs.
- Sit in a chair with good back support.
- Avoid standing for too long.
- Bend your knees when picking things up. Do not bend at the waist.
- Avoid lifting heavy objects.
- Avoid gaining too much weight.
- Use heat or cold on the sore part of your back.
- Have someone massage or rub the sore part of your back. If you go to a professional massage therapist, let them know you are pregnant.
- Do back exercises that your provider suggests to relieve back stress and maintain a healthy posture.
The extra weight you carry when you are pregnant can make your legs and back hurt.
Your body will also make a hormone that loosens ligaments throughout your body to prepare you for childbirth. However, these looser ligaments are more easily injured, most often in your back, so be careful when you lift and exercise.
Leg cramps are common in the last months of pregnancy. Sometimes stretching your legs before bed will reduce the cramps. Your provider can show you how to safely stretch.
Watch for pain and swelling in one leg, but not the other. This can be a sign of a blood clot. Let your provider know if this happens.
Cline M, Young N. Antepartum care. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier; 2021:1209-1216..
Gregory KD, Ramos DE, Jauniaux ERM. Preconception and prenatal care. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 5.
Philadelphia, PA: Elsevier; 2021:chap 5.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
Restless legs syndrome
- Home
- Restless legs syndrome
Restless legs syndrome (RLS) is a neurological disease manifested by paresthesias in the lower extremities and their excessive motor activity, mainly at rest or during sleep.
Restless legs syndrome was first described by Thomas Willis in 1672: “In some people, when they are going to sleep and lie down in bed, immediately after this there is a movement of the tendons, arms and legs, accompanied by colic and such restlessness that the patient cannot sleep like he's under torture." The modern definition of this syndrome was proposed by the Swedish scientist K. Ekbom in 1945:
Ekbom in 1945:
Restless legs syndrome can be primary (idiopathic) and secondary.
One of the most likely causes of the development of primary restless legs syndrome is considered to be the insufficiency of dopaminergic systems in the subcortical structures of the brain involved in inhibitory processes.
Secondary restless legs syndrome can develop during pregnancy and various pathological conditions.
The main causes of secondary restless leg syndrome are:
- Iron deficiency. Iron deficiency disrupts the production of dopamine in the brain, which in turn provokes the development of secondary RLS. A patient's iron stores may be depleted even without clinically significant anemia. Studies have shown that a decrease in iron stores, defined as a decrease in ferritin levels below 50 µg/L, can cause or exacerbate the symptoms of RLS.
- Neurological disorders. Secondary RLS is often observed in injuries of the spinal cord and peripheral nervous system, as well as peripheral neuropathies of various origins (diabetic, alcoholic, toxic).
 nine0004
nine0004 - Pregnancy. RLS occurs in 15-20% of women during pregnancy. Symptoms can be quite severe, but usually disappear completely within a few weeks after delivery. Iron deficiency anemia, folic acid deficiency, hormonal changes, and venous congestion in the lower extremities are thought to be the causes of RLS during pregnancy.
- Uremia. Up to 50% of patients with ESRD have RLS. The frequency of RLS was shown to correlate with blood urea levels, anemia, peripheral neuropathy, and a decrease in parathyroid hormone levels in this category of patients. Especially severe symptoms are noted directly during dialysis, when the patient is forced to lie motionless for several hours. Reduction or disappearance of RLS symptoms has been shown after kidney transplantation. nine0004
- Use of medicines. Symptoms of RLS may develop or worsen with the use of various medications, such as tricyclic antidepressants (amitriptyline, azafen, etc.), selective serotonin reuptake inhibitors (trazodone, Prozac), lithium preparations, metoclopramide (raglan), calcium channel blockers (corinfar, finoptin).
 Caffeine also worsens the symptoms of RLS.
Caffeine also worsens the symptoms of RLS.
Clinical manifestations of RLS can be grouped into several main symptom complexes:
Discomfort in the legs. They are usually described as crawling, trembling, tingling, burning, twitching, electric shock, wiggling under the skin, etc. About 30% of patients characterize these sensations as pain. Sometimes patients cannot accurately describe the nature of the sensations, but they are always extremely unpleasant. These sensations are localized in the thighs, shins, feet and undulate every 5-30 seconds. There are significant fluctuations in the severity of these symptoms. In some patients, symptoms may occur only at the beginning of the night, in others - continuously disturb throughout the day. nine0009
Symptoms worse at rest. The most characteristic and unusual manifestation of RLS is an increase in sensory or motor symptoms at rest. Patients usually report worsening while sitting or lying down and especially when falling asleep. Usually, before the onset of symptoms, it takes from several minutes to an hour when you are in a calm state.
Usually, before the onset of symptoms, it takes from several minutes to an hour when you are in a calm state.
Symptoms are relieved by movement. Symptoms are greatly relieved or disappear on movement. The best effect most often has a simple walk. In some cases, sipping, bending over, exercising on a stationary bike, or just standing up helps. nine0009
Symptoms are circadian. Symptoms are significantly worse in the evening and in the first half of the night (between 6 pm and 4 am). Before dawn, the symptoms weaken and may disappear altogether in the first half of the day.
However, it should be noted that diagnostic difficulties can sometimes arise in the differential diagnosis of primary and secondary restless leg syndrome. Since there are no exact biochemical markers of primary RLS, it is not possible to say with certainty whether the above condition is the cause that caused secondary RLS, or whether it only provoked the clinical manifestations of primary RLS. nine0009
nine0009
Valuable diagnostic information to confirm the presence of restless legs syndrome can be obtained by performing polysomnography, a method of long-term recording of various physiological parameters during sleep.
If you or your relatives want to fully relax while sleeping, we are waiting for you at the Department of Somnology of the Medical and Diagnostic Center of the International Institute of Biological Systems named after S.M. Berezina.
Treat yourself to a healthy sleep! nine0009
Leg pain during pregnancy: causes and how to get rid of it
Feet in pregnant women hurt for various reasons. Since there is a considerable load on the legs during pregnancy, this is not surprising. Just don't ignore the pain. Sometimes, if a woman feels pain in her legs, we can talk about pathology.
We tell you what pain in the legs during pregnancy can be associated with and what to do to alleviate the symptoms.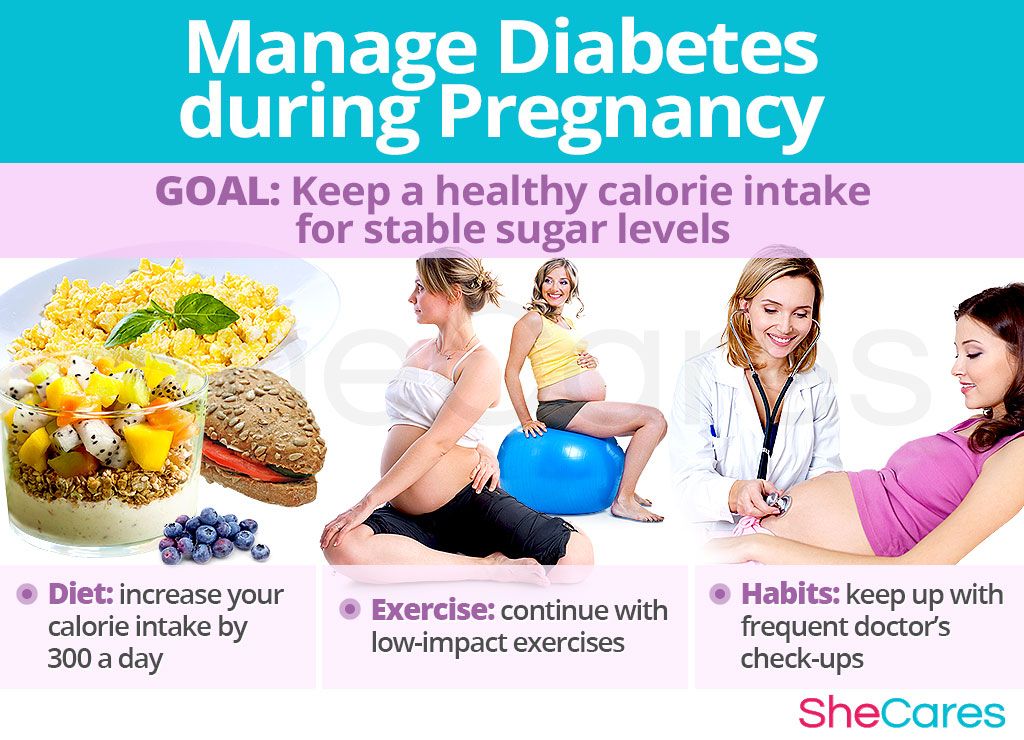 nine0009
nine0009
Why my feet hurt during pregnancy
During pregnancy, the center of gravity usually shifts, which creates an excessive load on the legs. Therefore, many women who are carrying a child experience pain in their feet. In general, during pregnancy, a woman's body is rebuilt, so pain can also occur for other reasons that are also not associated with the development of diseases.
Causes of leg pain in pregnant women
The most common causes of foot pain in pregnant women include: nine0009
-
Natural increase in body weight;
-
The shift in the center of gravity, which increases the load on the feet;
-
Excessive accumulation of fluid in the body can cause swelling and, as a result, throbbing pain;
-
Aching pain, swelling after walking or standing for a long time - these symptoms appear in women prone to varicose veins; nine0009
-
Cramping that cramps the legs or only the feet can occur due to an increased concentration of progesterone in the blood, as well as due to iron and calcium deficiency.

Consider the cases when the feet hurt during pregnancy due to existing diseases.
Flat feet
If flat feet have already been, then during pregnancy, if the disease is not treated, it only gets worse. There are cases when a woman had the first stage of flat feet, and in the last trimester - already the third. Usually, transverse flat feet are more acutely tolerated. Its symptoms: nine0009
-
Burning in the feet;
-
By the end of the day, the legs are very tired, they may swell;
-
In the evening there are cramps in the area of calves and shins, which are accompanied by pain in the feet;
-
Pain in the area of the kneecaps, pelvis and back - these symptoms appear when flat feet are neglected; nine0009
-
Calluses and growth that affects the base of the thumb;
-
Hammer toe deformity.
It is important to diagnose the transverse flatfoot of the foot in time. Usually orthopedic traumatologists deal with this issue. To diagnose the disease, the doctor sends an x-ray. Pregnancy is not an absolute contraindication for x-rays. Radiation should be avoided only in the first three months of pregnancy. Before the procedure, be sure to warn the doctor about your situation. nine0009
Usually orthopedic traumatologists deal with this issue. To diagnose the disease, the doctor sends an x-ray. Pregnancy is not an absolute contraindication for x-rays. Radiation should be avoided only in the first three months of pregnancy. Before the procedure, be sure to warn the doctor about your situation. nine0009
Only after studying the radiographs, the doctor can confirm the diagnosis. Further steps will depend entirely on the stage of the disease. At the initial stages, the disease is cured by conservative methods, in advanced cases, surgical intervention is required.
Conservative treatments include:
-
treatment with medications if there is inflammation;
- nine0008 wearing orthopedic insoles and other devices;
-
physiotherapy;
-
massage;
-
exercise therapy.
In the fight against flat feet, orthopedic insoles, which are designed for pregnant women, have proven themselves well.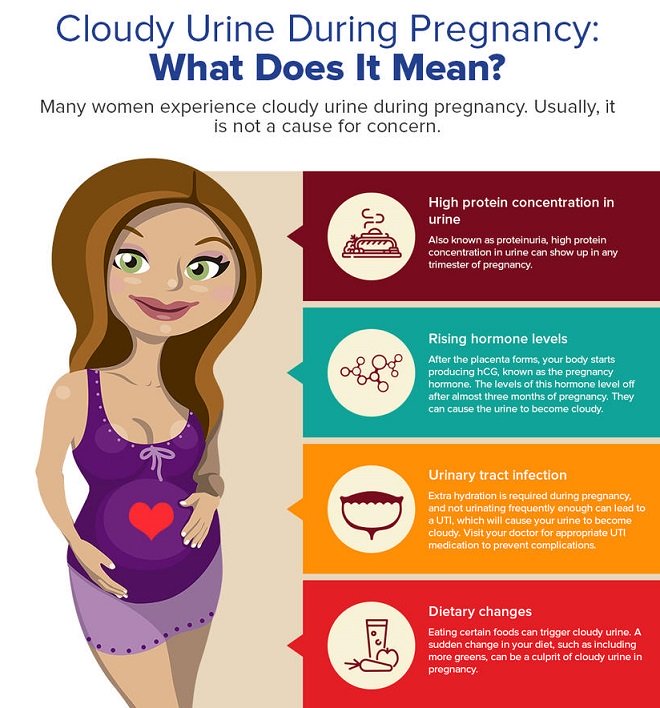 They help to evenly distribute the load on the legs of women. nine0009
They help to evenly distribute the load on the legs of women. nine0009
Varicose veins
Even if a woman has never suffered from this disease, there is a risk that pregnancy will worsen the condition of the vessels.
Since mother and baby have a common circulatory system, varicose veins can provoke oxygen starvation in the fetus. The fact is that it is with the mother's blood that the child receives all the necessary substances to maintain his life.
It is not difficult to recognize varicose veins on your own. The most obvious signs that can be seen with the naked eye are pronounced vascular networks. It is worth making an appointment with a doctor if you have symptoms such as: nine0009
-
Aching pain in the legs, especially after exercise;
-
Fatigue and heaviness in the legs at the end of the day;
-
tingling, itching and burning;
-
Numbness of limbs or cramps.

The treatment of the disease is carried out by a phlebologist (vascular surgeon). nine0009
Is it possible to do foot massage during pregnancy?
If the attending specialist does not see any contraindications for massage, then the procedure will only benefit. Foot massage during pregnancy will help not only alleviate the condition of the legs, but also improve the mood of the expectant mother. Massage has a positive effect on the emotional state of the mother, and therefore on the unborn child.
How to get rid of foot pain
Often, with pain in the legs, a woman can help herself. These recommendations will help get rid of leg pain or at least reduce it: nine0009
-
During pregnancy, aching and tired feet come to the rescue in the evening foot baths. Water should be at room temperature. It is also useful to rinse the feet with cold water;
-
It is advisable to sleep on the left side - on the right is the inferior vena cava, which carries the bulk of the blood, so it is better to remove the load from it;
-
A contrast shower helps to get rid of pain in the legs - this procedure will also strengthen the walls of blood vessels; nine0009
To avoid unpleasant pain in the legs, it is also important to follow preventive measures:
-
Drink enough water.
 Edema appears when the body is dehydrated, and not vice versa;
Edema appears when the body is dehydrated, and not vice versa; -
Movement. To improve blood flow, it is useful to move and do light exercise. Walking is the best activity for pregnant women. When driving, it is important to take regular breaks to stretch your legs; nine0009
-
Leg lift. If you have to sit for a long time, it is advisable to raise your legs more often. To do this, you can put a stand or a small bench near you;
-
Balanced diet. This applies mainly to the consumption of salt, since it is it that retains water in the body. In general, the diet should be varied, with sufficient protein;
nine0003 -
Avoidance of heavy workloads. Long stay on your feet, lifting weights and any physical labor - all this negatively affects the health of blood vessels during pregnancy.
 You should also pay attention to the position of the body. For example, a pose in which the legs are crossed harms the vessels; nine0009
You should also pay attention to the position of the body. For example, a pose in which the legs are crossed harms the vessels; nine0009 -
Correct posture. With proper posture, the load on the legs is distributed evenly. It is important to ensure that the lower back does not bend too much or the body does not lean back too much;
-
Comfortable shoes and clothes. Clothing or shoes that are tight on the body can block blood flow. Therefore, it is not recommended to wear socks with tight elastic bands that leave marks on the body, and shoes that are too narrow and short; nine0009
-
Be careful with sunburn. If there is a tendency to varicose veins, you should not stay under the sun for a long time - ultraviolet rays weaken blood vessels.
Weight control. Almost all women gain weight during pregnancy. It is only important to ensure that the “increase” fits into the norm, since excess weight provokes swelling;
If you follow these simple recommendations, you can minimize the pain in the legs during pregnancy. If you suspect flat feet, you can always contact our orthopedic center.