Tested positive for strep b
Group B strep disease - Symptoms and causes
Overview
Group B strep (streptococcus) is a common bacterium often carried in the intestines or lower genital tract. The bacterium is usually harmless in healthy adults. In newborns, however, it can cause a serious illness known as group B strep disease.
Group B strep can also cause dangerous infections in adults with certain chronic medical conditions, such as diabetes or liver disease. Older adults are at increased risk of illness due to group B strep, too.
If you're a healthy adult, there's nothing you need to do about group B strep. If you're pregnant, get a group B strep screening test during your third trimester. If you have group B strep, antibiotic treatment during labor can protect your baby.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Infants
Most babies born to women carrying group B strep are healthy. But the few who are infected by group B strep during labor can become critically ill.
In infants, illness caused by group B strep can be within six hours of birth (early onset) — or weeks or months after birth (late onset).
Signs and symptoms might include:
- Fever
- Low body temperature
- Difficulty feeding
- Sluggishness, limpness or weak muscle tone
- Difficulty breathing
- Irritability
- Jitteriness
- Seizures
- Rash
- Jaundice
Adults
Many adults carry group B strep in their bodies — usually in the bowel, vagina, rectum, bladder or throat — and have no signs or symptoms.
In some cases, however, group B strep can cause a urinary tract infection or other more-serious infections. Signs and symptoms of infections that may be caused by group B strep include the following.
Urinary tract infection
- A strong, persistent urge to urinate
- A burning sensation or pain when urinating
- Passing frequent, small amounts of urine
- Urine that appears red, bright pink or cola colored — a sign of blood in the urine
- Pelvic pain
Blood infection (bacteremia)
- Fever
- Chills
- Confusion or lack of alertness
Pneumonia
- Fever
- Chills
- Cough
- Shortness of breath
- Chest pain when you breathe or cough
Skin or soft-tissue infection
- Swelling, warmth or redness in the area of the infection
- Pain in the area of the infection
- Lesions with pus or drainage
Bone or joint infection
- Fever
- Chills
- Swelling, warmth or redness over the area of the infection
- Pain in the area of the infection
- Stiffness or inability to use a limb or joint
When to see a doctor
If you have signs or symptoms of group B strep infection — particularly if you're pregnant, you have a chronic medical condition or you're older than 65 — contact your doctor right away.
If you notice your infant has signs or symptoms of group B strep disease, contact your baby's doctor immediately.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Many healthy people carry group B strep bacteria in their bodies. You might carry the bacteria in your body for a short time — it can come and go — or you might always have it. Group B strep bacteria aren't sexually transmitted, and they're not spread through food or water. How the bacteria are spread to anyone other than newborns isn't known.
Group B strep can spread to a baby during a vaginal delivery if the baby is exposed to — or swallows — fluids containing group B strep.
Risk factors
Infants
An infant is at increased risk of developing group B strep disease if:
- The mother carries group B strep in her body
- The baby is born prematurely (earlier than 37 weeks)
- The mother's water breaks 18 hours or more before delivery
- The mother has an infection of the placental tissues and amniotic fluid (chorioamnionitis)
- The mother has a urinary tract infection during the pregnancy
- The mother's temperature is greater than 100.
 4 F (38 C) during labor
4 F (38 C) during labor - The mother previously delivered an infant with group B strep disease
Adults
Adults age 65 and older are at increased risk of group B strep. You're also at increased risk of if you have a condition that impairs your immune system or other serious diseases, including the following:
- Diabetes
- HIV infection
- Liver disease
- Heart disease
- Cancer or history of cancer
Complications
Group B strep infection can lead to life-threatening disease in infants, including:
- Pneumonia
- Inflammation of the membranes and fluid surrounding the brain and spinal cord (meningitis)
- Infection in the bloodstream (bacteremia)
If you're pregnant, group B strep can cause the following:
- Urinary tract infection
- Infection of the placenta and amniotic fluid (chorioamnionitis)
- Infection of the membrane lining the uterus (endometritis)
- Bacteremia
If you're an older adult or you have a chronic health condition, group B strep bacteria can lead to any of the following conditions:
- Skin infection
- Bacteremia
- Urinary tract infection
- Pneumonia
- Bone and joint infections
- Infection of the heart valves (endocarditis)
- Meningitis
Prevention
If you're pregnant, the American College of Obstetricians and Gynecologists recommends a group B strep screening during weeks 36 to 37 of pregnancy. Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
A positive test indicates that you carry group B strep. It doesn't mean that you're ill or that your baby will be affected, but that you're at increased risk of passing the bacteria to your baby.
To prevent group B bacteria from spreading to your baby during labor or delivery, your doctor can give you an IV antibiotic — usually penicillin or a related drug — when labor begins.
If you're allergic to penicillin or related drugs, you might receive clindamycin or vancomycin as an alternative. Because the effectiveness of these alternatives is not well understood, your baby will be monitored for up to 48 hours.
Taking oral antibiotics ahead of time won't help because the bacteria can return before labor begins.
Antibiotic treatment during labor is also recommended if you:
- Have a urinary tract infection
- Delivered a previous baby with group B strep disease
- Develop a fever during labor
- Haven't delivered your baby within 18 hours of your water breaking
- Go into labor before 37 weeks and haven't been tested for group B strep
Vaccine in development
Although it's not available yet, researchers are working on a group B strep vaccine that could help prevent group B strep infections in the future.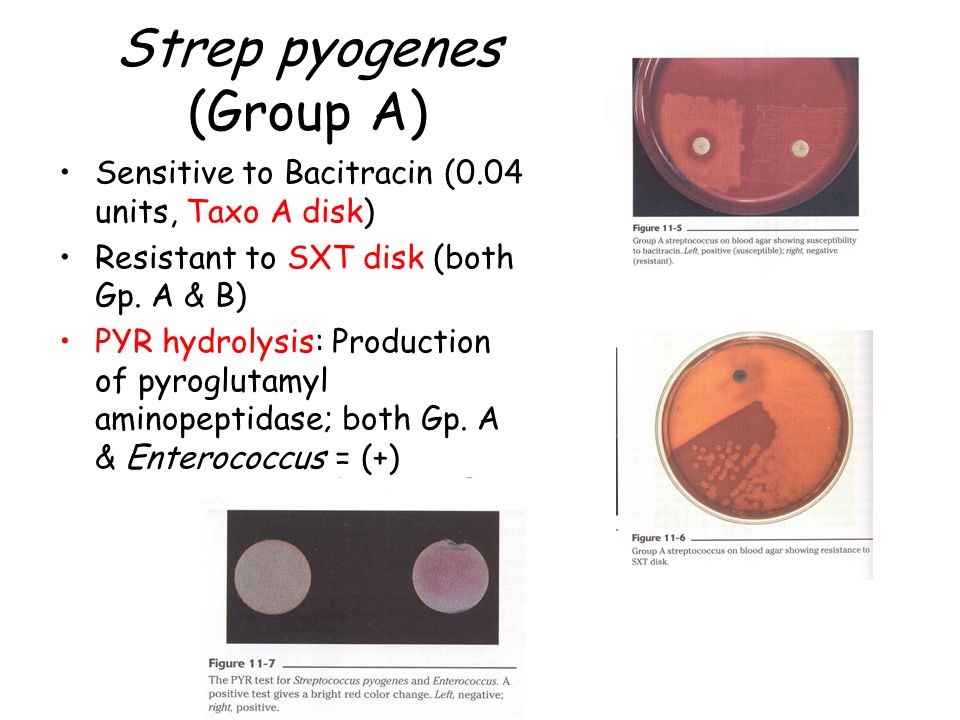
By Mayo Clinic Staff
Related
Products & Services
Group B Strep and Pregnancy (for Parents)
What Is Group B Strep?
Group B Streptococcus (group B strep, GBS) is a type of
bacteriaoften found in the urinary tract, digestive system, and reproductive tracts. The bacteria come and go from our bodies, so most people who have it don't know that they do. GBS usually doesn't cause health problems.
What Problems Can Group B Strep Cause?
Health problems from GBS are not common. But it can cause illness in some people, such as the elderly and those with some medical conditions. GBS can cause infections in such areas of the body as the blood, lungs, skin, or bones.
About 1 out of every 4 women have GBS. In pregnant women, GBS can cause infection of the urinary tract, placenta, womb, and amniotic fluid.
Even if they haven't had any symptoms of infection, pregnant women can pass the infection to their babies during labor and delivery.
How Does Group B Strep Affect Babies?
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
The two types of GBS disease in babies are:
- Early-onset infections, which happen during the first week of life. Babies often have symptoms within 24 hours of birth.
- Late-onset infections, which develop weeks to months after birth. This type of GBS disease is not well understood.
What Are the Signs & Symptoms of GBS Disease?
Newborns and infants with GBS disease might show these signs:
- a fever
- feeding problems
- breathing problems
- irritability or fussiness
- inactivity or limpness
- trouble keeping a healthy body temperature
Babies with GBS disease can develop serious problems, such as:
- pneumonia
- sepsis
- meningitis (infection of the fluid and lining around the brain).
 Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
How Is Group B Strep Diagnosed?
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be "GBS-positive." This means only that she has the bacteria in her body — not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
How Is Group B Strep Treated?
Doctors will test a pregnant woman to see if she has GBS. If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
It's best for a woman to get antibiotics for at least 4 hours before delivery. This simple step greatly helps to prevent the spread of GBS to the baby.
Doctors also might give antibiotics during labor to a pregnant woman if she:
- goes into labor prematurely, before being tested for GBS
- hasn't been tested for GBS and her water breaks 18 or more hours before delivery
- hasn't been tested for GBS and has a fever during labor
- had a GBS bladder infection during the pregnancy
- had a baby before with GBS disease
Giving antibiotics during labor helps to prevent early-onset GBS disease only. The cause of late-onset disease isn't known, so no method has yet been found to prevent it. Researchers are working to develop a vaccine to prevent GBS infection.
Babies who get GBS disease are treated with antibiotics. These are started as soon as possible to help prevent problems. These babies also may need other treatments, like breathing help and IV fluids.
How Can I Help Prevent Group B Strep Infection?
Because GBS comes and goes from the body, a woman should be tested for it during each pregnancy. Women who are GBS-positive and get antibiotics at the right time during labor do well, and most don't pass the infection to their babies.
If you are GBS-positive and begin to go into labor, go to the hospital rather than laboring at home. By getting IV antibiotics for at least 4 hours before delivery, you can help protect your baby against early-onset GBS disease.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
Streptococcus agalactiae (group B haemolytic streptococcus), antigen
Test to detect and confirm infection with group B hemolytic streptococcus (Streptococcus agalactiae).
Synonyms Russian
Group B streptococcus, B-hemolytic streptococcus group B, GBS.
English synonyms
GBS, Streptococcus agalactiae.
Research method
Immunochromatography.
What biomaterial can be used for research?
Urogenital swab, swab from the inner surface of the cervix (from the cervical canal).
How to properly prepare for an examination?
- For women, it is recommended to test before menstruation or 2-3 days after it ends.
- Men do not urinate for 3 hours prior to examination.
General information about the study :
Streptococcus agalactiae (Group B Streptococcus, GBS) Gram-positive facultative anaerobes that do not form spores. It is an important pathogen that colonizes the urogenital and lower gastrointestinal tracts. It is believed that about 40% of healthy women of reproductive age are infected with Streptococcus agalactiae. Streptococcus agalactiae is the main cause of sepsis and meningitis in newborns. In addition, group B B-hemolytic streptococcus can infect the elderly and immunocompromised adults. GBS can form biofilms that enhance its colonizing properties and contribute to the persistence of the pathogen in the host organism.
Streptococcus agalactiae is the main cause of sepsis and meningitis in newborns. In addition, group B B-hemolytic streptococcus can infect the elderly and immunocompromised adults. GBS can form biofilms that enhance its colonizing properties and contribute to the persistence of the pathogen in the host organism.
In most cases colonization of the urogenital tract and rectum is considered as asymptomatic carriage. Manifestations of infection in adults include bacteremia, skin and soft tissue infections, pneumonia, osteomyelitis, urinary tract infections, necrotizing fasciitis, myositis, sepsis, arthritis, prostatitis. However, group B streptococcus is most dangerous for newborns. Until now, Streptococcus agalactiae occupies one of the leading places in the structure of pathogens of perinatal infections. Most often, a child becomes infected with GBS during childbirth, its transmission from mother to child occurs in 37-75% of cases. Intrauterine transmission of GBS is possible, which can cause miscarriages, miscarriages, and stillbirths.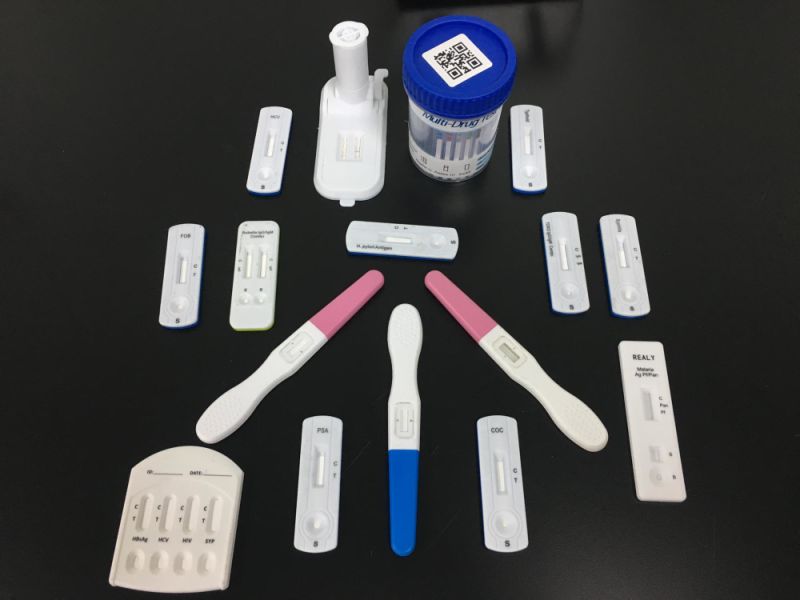 Risk factors for infection in a child born to a mother with GBS include age of pregnancy (less than 20 years), history of miscarriage or medical abortion, amnionitis, preterm birth (before 37 weeks), fever during labor, prolonged anhydrous period, intrauterine growth retardation etc. The more massive the GBS colonization of the skin and mucous membranes of newborns, the greater the likelihood of developing an infectious process. Streptococcal infection can occur in two forms: 1) in the first 48 hours of a newborn's life and manifest itself as septicemia or pneumonia; 2) and with a later onset and proceed in the form of meningitis. With a fulminant form of the disease, mortality among newborns reaches 60%. To prevent transmission of infection from mother to fetus, antibiotic prophylaxis with penicillin is recommended at 35-37 weeks of gestation in women diagnosed with GBS in swabs from the urogenital tract and / or rectum.
Risk factors for infection in a child born to a mother with GBS include age of pregnancy (less than 20 years), history of miscarriage or medical abortion, amnionitis, preterm birth (before 37 weeks), fever during labor, prolonged anhydrous period, intrauterine growth retardation etc. The more massive the GBS colonization of the skin and mucous membranes of newborns, the greater the likelihood of developing an infectious process. Streptococcal infection can occur in two forms: 1) in the first 48 hours of a newborn's life and manifest itself as septicemia or pneumonia; 2) and with a later onset and proceed in the form of meningitis. With a fulminant form of the disease, mortality among newborns reaches 60%. To prevent transmission of infection from mother to fetus, antibiotic prophylaxis with penicillin is recommended at 35-37 weeks of gestation in women diagnosed with GBS in swabs from the urogenital tract and / or rectum.
There is currently no widespread screening for Streptococcus agalactiae in Russia.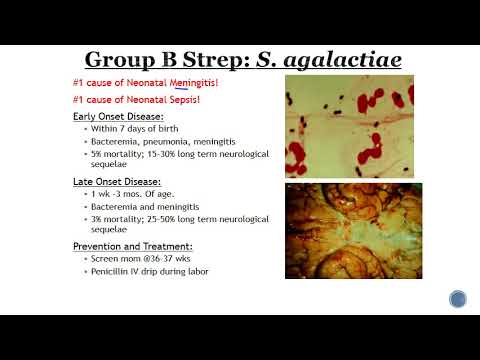 Due to the low specificity of the manifestations of infection, laboratory diagnostic methods are of particular importance in verifying the diagnosis. For this test, an immunochromatographic method is used using Vedalab test cassettes (France). Test sensitivity - 10 3 -10 4 bacterial cells per 0.1 ml of sample. This is a rapid screening test for β-hemolytic streptococcus.
Due to the low specificity of the manifestations of infection, laboratory diagnostic methods are of particular importance in verifying the diagnosis. For this test, an immunochromatographic method is used using Vedalab test cassettes (France). Test sensitivity - 10 3 -10 4 bacterial cells per 0.1 ml of sample. This is a rapid screening test for β-hemolytic streptococcus.
What is research used for?
- For the early detection of Streptococcus agalactiae in order to prevent infection of the fetus.
- To reduce morbidity and mortality from perinatal S. agalactiae infection.
- To detect infection in elderly and immunocompromised individuals.
When is the examination scheduled?
- In preparation for pregnancy.
- At 35-37 weeks of pregnancy.
- For symptoms of skin and soft tissue infection, pneumonia, osteomyelitis, urinary tract infections, necrotizing fasciitis, myositis, sepsis, arthritis, prostatitis in the elderly and immunocompromised.

What do the results mean?
Reference values: not found.
A positive indicates infection with B-hemolytic streptococcus group B.
A negative result means no Streptococcus agalactiae infection.
Who orders the examination?
Obstetrician-gynecologist, urologist, general practitioner, pediatrician.
Literature
- Rosini R, Margarit I. Biofilm formation by Streptococcus agalactiae: influence of environmental conditions and implicated virulence factors. Front Cell Infect Microbiol. 2015;5:6. Published 2015 Feb 4. doi:10.3389/fcimb.2015.00006.
- Zatsiorskaya S.L., Krysanova A.A., Khvan V.O., Martikainen Z.M., Savicheva A.M. Diagnosis and prevention of infections caused by Streptococcus agalactiae in pregnant women and newborns // Pediatrician. 2014. No. 3.
Culture for group B beta-hemolytic streptococcus
Group B beta-hemolytic streptococcus belongs to the normal intestinal microflora, in particular, it lives in the rectum. In titers that do not exceed the norm, it does not cause disruption of the intestines, and also does not colonize neighboring departments and organs. But in the presence of provoking factors, such as decreased immunity, chronic inflammation of the genitourinary tract, vaginal dysbiosis with a change in the acidity of the environment and a decrease in the amount of beneficial flora, streptococcus can affect the cells of the urethra, vagina, cervical canal, and even move upward to the uterus and appendages.
In titers that do not exceed the norm, it does not cause disruption of the intestines, and also does not colonize neighboring departments and organs. But in the presence of provoking factors, such as decreased immunity, chronic inflammation of the genitourinary tract, vaginal dysbiosis with a change in the acidity of the environment and a decrease in the amount of beneficial flora, streptococcus can affect the cells of the urethra, vagina, cervical canal, and even move upward to the uterus and appendages.
This type of streptococcus got its name because of the ability to hemolysis, but its severity depends on a number of factors and may differ until the disappearance of hemolysis. In such cases, streptococcus acquires qualities that are atypical for itself and makes it difficult to diagnose.
Diagnosis of group B β-hemolytic streptococcus is essential. During pregnancy, the carriage of this bacterium can lead to severe complications, damage to the organs of the fetus.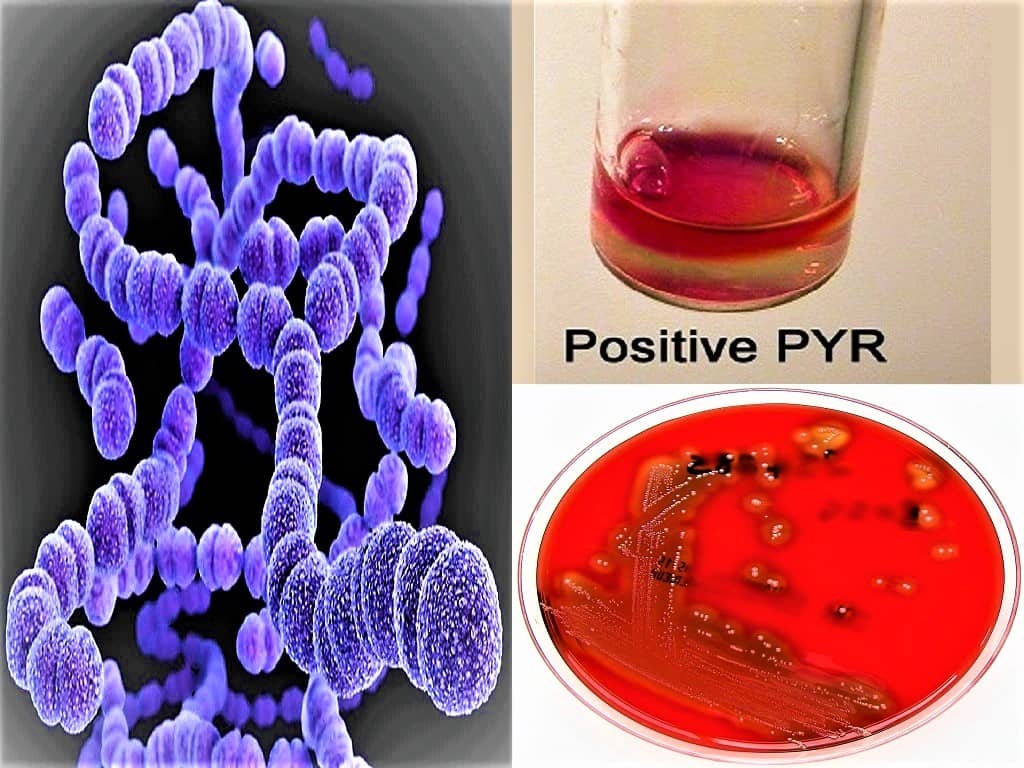 The most common pneumonia, meningitis, pyelonephritis, neonatal sepsis. Most often, the child becomes infected from the mother during childbirth, and a high probability of infection is noted during childbirth through the natural birth canal. Less risk for caesarean section. The statistics of the possibility of infection depending on the term of delivery deserves special attention. Thus, in full-term pregnancy, only 2% of newborns have a pronounced clinical picture of GBS infection. The shorter the period, the more cases of infection and the development of complications. So, in premature babies born at a period of more than 28 weeks, the probability of developing an infection is 15-20%, while in very premature newborns (delivery less than 28 weeks), the probability is almost 100%. Neonatologists of all countries are still working on the issue of early prevention and treatment of such children. A separate issue is the delayed complications and manifestations of GBS infection, which is also being investigated by researchers.
The most common pneumonia, meningitis, pyelonephritis, neonatal sepsis. Most often, the child becomes infected from the mother during childbirth, and a high probability of infection is noted during childbirth through the natural birth canal. Less risk for caesarean section. The statistics of the possibility of infection depending on the term of delivery deserves special attention. Thus, in full-term pregnancy, only 2% of newborns have a pronounced clinical picture of GBS infection. The shorter the period, the more cases of infection and the development of complications. So, in premature babies born at a period of more than 28 weeks, the probability of developing an infection is 15-20%, while in very premature newborns (delivery less than 28 weeks), the probability is almost 100%. Neonatologists of all countries are still working on the issue of early prevention and treatment of such children. A separate issue is the delayed complications and manifestations of GBS infection, which is also being investigated by researchers.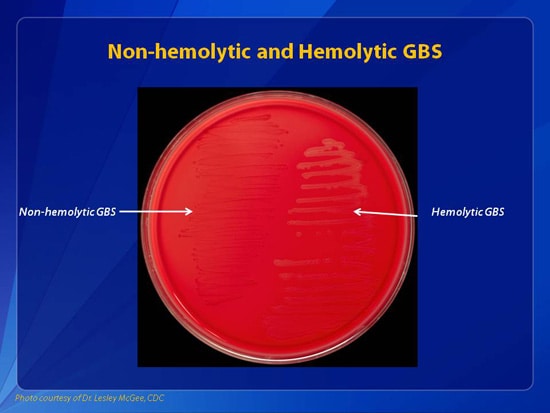 We should not forget that under certain conditions, group B β-hemolytic streptococcus can cause the development of bacteremia, infections of the urinary and reproductive systems, cause premature rupture of amniotic fluid, inflammation of the placenta and membranes.
We should not forget that under certain conditions, group B β-hemolytic streptococcus can cause the development of bacteremia, infections of the urinary and reproductive systems, cause premature rupture of amniotic fluid, inflammation of the placenta and membranes.
Diagnosis of streptococcal infection in non-pregnant women is also important, especially if there are complaints of pathological discharge from the genital tract, the clinical picture of inflammation, as well as in cases of infertility against the background of endometritis, salpingo-oophoritis. Of course, in the future, when pregnancy occurs, the study is repeated, and more than once, be sure to re-sow on the eve of childbirth.
Sowing of the discharged genital organs on the flora is carried out to assess the presence of β-hemolytic streptococcus of group B. At the same time, the titer of the bacterium is determined during the study, if it is present. A small amount of bacteria is isolated, usually less than 10 to the 3rd degree, in which case laboratory diagnostic systems do not assess the sensitivity of this type of bacteria to antibiotics, since the titer is normal, treatment is not required.