Test for miscarriage
Miscarriage - Diagnosis and treatment
Diagnosis
Your health care provider might do a variety of tests:
- Pelvic exam. Your health care provider might check to see if your cervix has begun to dilate.
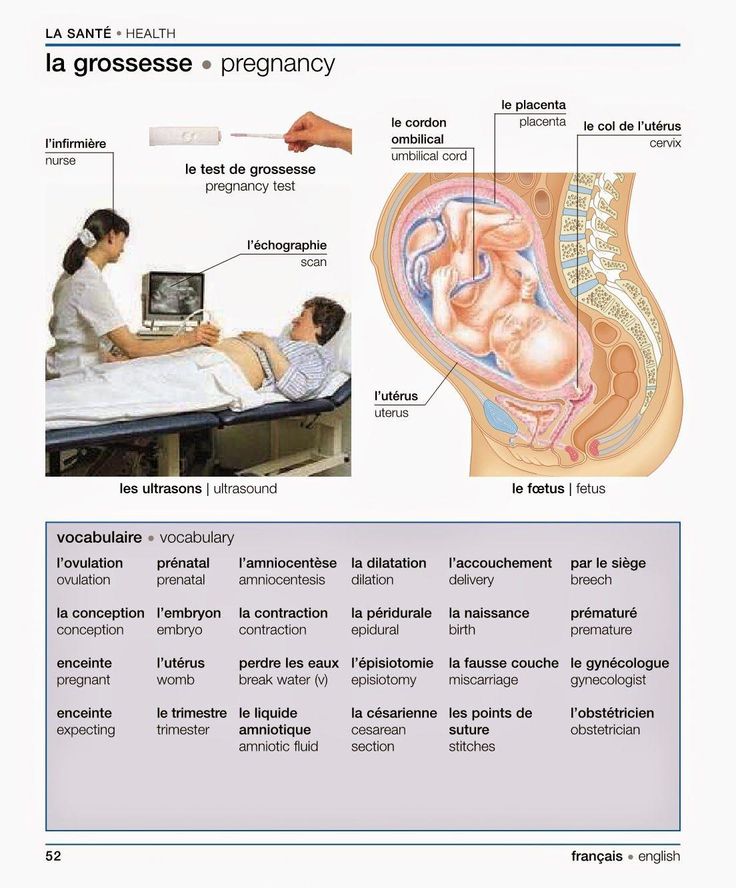
- Ultrasound. During an ultrasound, your health care provider will check for a fetal heartbeat and determine if the embryo is developing as it should be. If a diagnosis can't be made, you might need to have another ultrasound in about a week.
- Blood tests. Your health care provider might check the level of the pregnancy hormone, human chorionic gonadotropin (HCG), in your blood and compare it to previous measurements. If the pattern of changes in your HCG level is abnormal, it could indicate a problem. Your health care provider might check to see if you're anemic — which could happen if you've experienced significant bleeding — and may also check your blood type.
- Tissue tests. If you have passed tissue, it can be sent to a lab to confirm that a miscarriage has occurred — and that your symptoms aren't related to another cause.
- Chromosomal tests. If you've had two or more previous miscarriages, your health care provider may order blood tests for both you and your partner to determine if your chromosomes are a factor.
Possible diagnoses include:
- Threatened miscarriage. If you're bleeding but your cervix hasn't begun to dilate, there is a threat of miscarriage. Such pregnancies often proceed without any further problems.
- Inevitable miscarriage. If you're bleeding, cramping and your cervix is dilated, a miscarriage is considered inevitable.
- Incomplete miscarriage. If you pass fetal or placental material but some remains in your uterus, it's considered an incomplete miscarriage.
- Missed miscarriage.
 In a missed miscarriage, the placental and embryonic tissues remain in the uterus, but the embryo has died or was never formed.
In a missed miscarriage, the placental and embryonic tissues remain in the uterus, but the embryo has died or was never formed. - Complete miscarriage. If you have passed all the pregnancy tissues, it's considered a complete miscarriage. This is common for miscarriages occurring before 12 weeks.
- Septic miscarriage. If you develop an infection in your uterus, it's known as a septic miscarriage. This can be a severe infection and demands immediate care.
More Information
- Pelvic exam
- Ultrasound
Treatment
Threatened miscarriage
For a threatened miscarriage, your health care provider might recommend resting until the bleeding or pain subsides. Bed rest hasn't been proved to prevent miscarriage, but it's sometimes prescribed as a safeguard. You might be asked to avoid exercise and sex, too. Although these steps haven't been proved to reduce the risk of miscarriage, they might improve your comfort.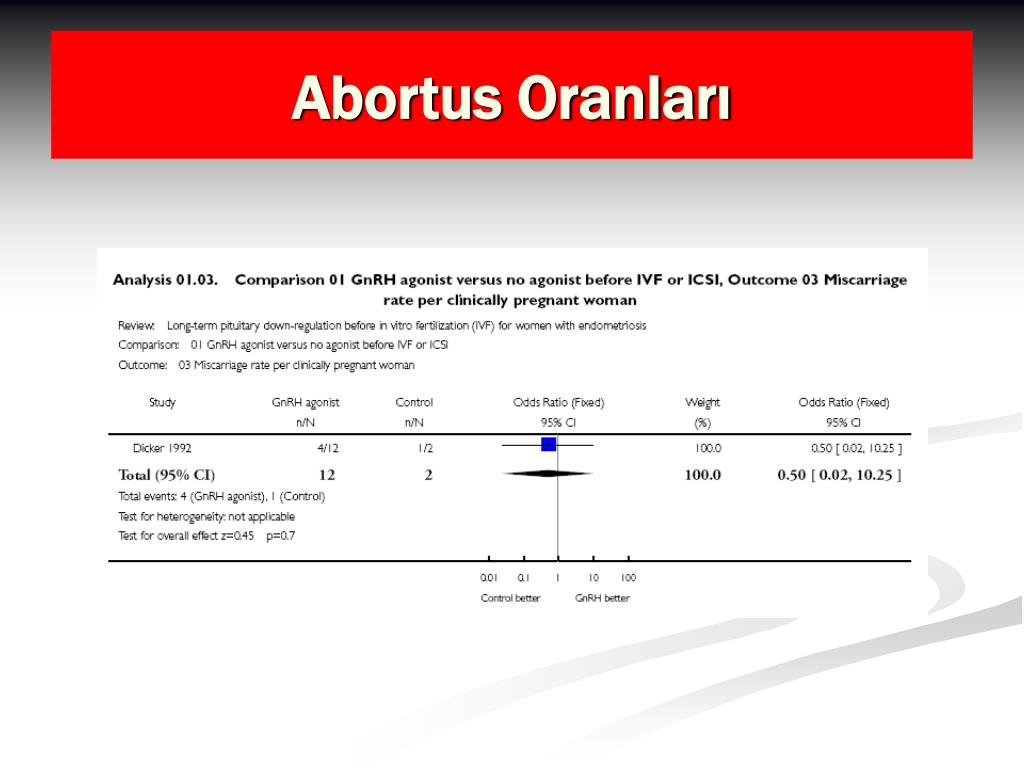
In some cases, it's also a good idea to postpone traveling — especially to areas where it would be difficult to receive prompt medical care. Ask your health care provider if it would be wise to delay any upcoming trips you've planned.
Miscarriage
With ultrasound, it's now much easier to determine whether an embryo has died or was never formed. Either finding means that a miscarriage will definitely occur. In this situation, you might have several choices:
- Expectant management. If you have no signs of infection, you might choose to let the miscarriage progress naturally. Usually this happens within a couple of weeks of determining that the embryo has died. Unfortunately, it might take up to three or four weeks. This can be an emotionally difficult time. If expulsion doesn't happen on its own, medical or surgical treatment will be needed.
- Medical treatment. If, after a diagnosis of certain pregnancy loss, you'd prefer to speed the process, medication can cause your body to expel the pregnancy tissue and placenta.
 The medication can be taken by mouth or by insertion in the vagina. Your health care provider might recommend inserting the medication vaginally to increase its effectiveness and minimize side effects such as nausea and diarrhea. For about 70 to 90 percent of women, this treatment works within 24 hours.
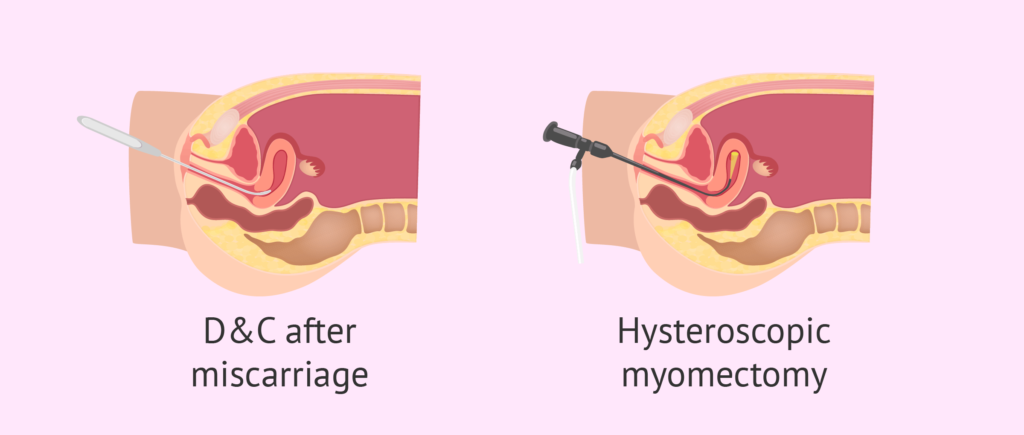
The medication can be taken by mouth or by insertion in the vagina. Your health care provider might recommend inserting the medication vaginally to increase its effectiveness and minimize side effects such as nausea and diarrhea. For about 70 to 90 percent of women, this treatment works within 24 hours. - Surgical treatment. Another option is a minor surgical procedure called suction dilation and curettage (D&C). During this procedure, your health care provider dilates your cervix and removes tissue from the inside of your uterus. Complications are rare, but they might include damage to the connective tissue of your cervix or the uterine wall. Surgical treatment is needed if you have a miscarriage accompanied by heavy bleeding or signs of an infection.
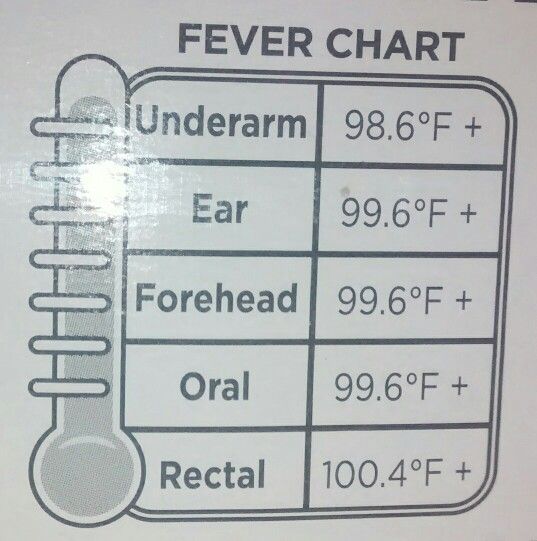
Physical recovery
In most cases, physical recovery from miscarriage takes only a few hours to a couple of days. In the meantime, call your health care provider if you experience heavy bleeding, fever or abdominal pain.
You may ovulate as soon as two weeks after a miscarriage. Expect your period to return within four to six weeks. You can start using any type of contraception immediately after a miscarriage. However, avoid having sex or putting anything in your vagina — such as a tampon — for two weeks after a miscarriage.
Future pregnancies
It's possible to become pregnant during the menstrual cycle immediately after a miscarriage. But if you and your partner decide to attempt another pregnancy, make sure you're physically and emotionally ready. Ask your health care provider for guidance about when you might try to conceive.
Miscarriage is usually a one-time occurrence. Most women who miscarry go on to have a healthy pregnancy after miscarriage. Less than 5 percent of women have two consecutive miscarriages, and only 1 percent have three or more consecutive miscarriages.
If you experience multiple miscarriages, generally two or three in a row, consider testing to identify any underlying causes. Such causes could include problems with the uterus, blood clotting or chromosomes. If the cause of your miscarriages can't be identified, don't lose hope. About 60 to 80 percent of women with unexplained repeated miscarriages go on to have healthy pregnancies.
Such causes could include problems with the uterus, blood clotting or chromosomes. If the cause of your miscarriages can't be identified, don't lose hope. About 60 to 80 percent of women with unexplained repeated miscarriages go on to have healthy pregnancies.
More Information
- Dilation and curettage (D&C)
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Emotional healing can take much longer than physical healing. Miscarriage can be a heart-wrenching loss that others around you might not fully understand. Your emotions might range from anger and guilt to despair. Give yourself time to grieve the loss of your pregnancy, and seek help from loved ones.
You'll likely never forget your hopes and dreams surrounding this pregnancy, but in time acceptance might ease your pain. Talk to your health care provider if you're feeling profound sadness or depression.
Talk to your health care provider if you're feeling profound sadness or depression.
Preparing for your appointment
If you have signs or symptoms of miscarriage, contact your health care provider right away. Depending on the circumstances, you might need immediate medical care.
Here's some information to help you get ready for your appointment, and what to expect from your health care provider.
What you can do
Before your appointment, you might want to:
- Ask about pre-appointment restrictions. In most cases you'll be seen immediately. If that's not the case, ask whether you should restrict your activities while you wait for your appointment.
- Find a loved one or friend who can join you for your appointment. Fear and anxiety might make it difficult to focus on what your health care provider says. Take someone along who can help remember all the information.
- Write down questions to ask your health care provider.
 That way, you won't forget anything important that you want to ask, and you can make the most of your time with your health care provider.
That way, you won't forget anything important that you want to ask, and you can make the most of your time with your health care provider.
Below are some basic questions to ask your health care provider about miscarriage:
- What are the treatment options?
- What kinds of tests do I need?
- Can I continue to do my usual activities?
- What signs or symptoms should prompt me to call you or go to the hospital?
- Do you know what caused my miscarriage?
- What are my chances for a successful future pregnancy?
In addition to the questions you've prepared, don't hesitate to ask other questions during your appointment — especially if you need clarification or you don't understand something.
What to expect from your health care provider
Your health care provider is likely to ask you a number of questions, too. For example:
- When was your last menstrual period?
- Were you using any contraceptive methods at the time you likely conceived?
- When did you first notice your signs or symptoms?
- Have your symptoms been continuous or occasional?
- Compared with your heaviest days of menstrual flow, is your bleeding more, less or about the same?
- Have you had a miscarriage before?
- Have you had any complications during a previous pregnancy?
- Do you have any other health conditions?
- Do you know your blood type?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Miscarriage - Diagnosis - NHS
If you see your GP or midwife because of vaginal bleeding or other symptoms of miscarriage, you may be referred to an early pregnancy unit at a hospital for tests.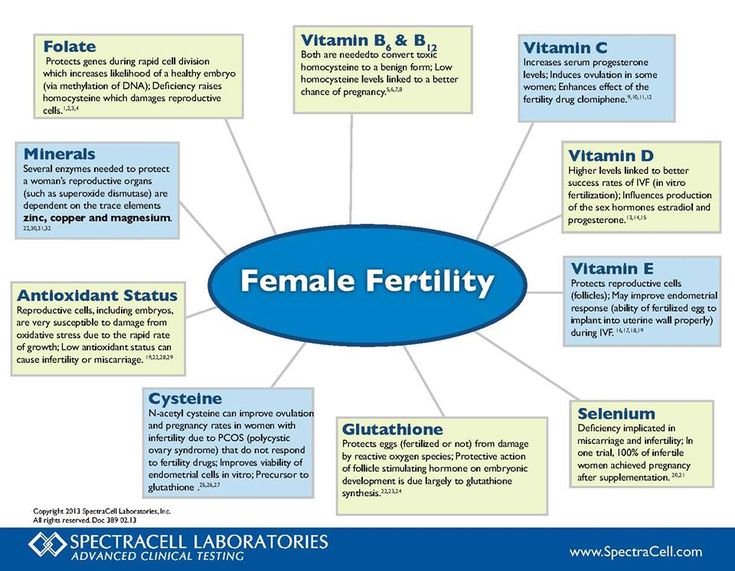
If you're more than 18 weeks pregnant, you'll usually be referred to the maternity unit at the hospital.
If you're less than 6 weeks pregnant, you may not be referred for tests straight away. This is because it's very hard to confirm a miscarriage this early on.
Tests
The hospital can carry out tests to confirm whether you're having a miscarriage. The tests can also confirm whether there's still some pregnancy tissue left in your womb (an incomplete or delayed miscarriage) or if all the pregnancy tissue has been passed out of your womb (a complete miscarriage).
The first test used is usually an ultrasound scan to check the development of your baby and look for a heartbeat. In most cases, this is usually carried out using a small probe inserted into the vagina (transvaginal ultrasound). This can feel a little uncomfortable but is not painful.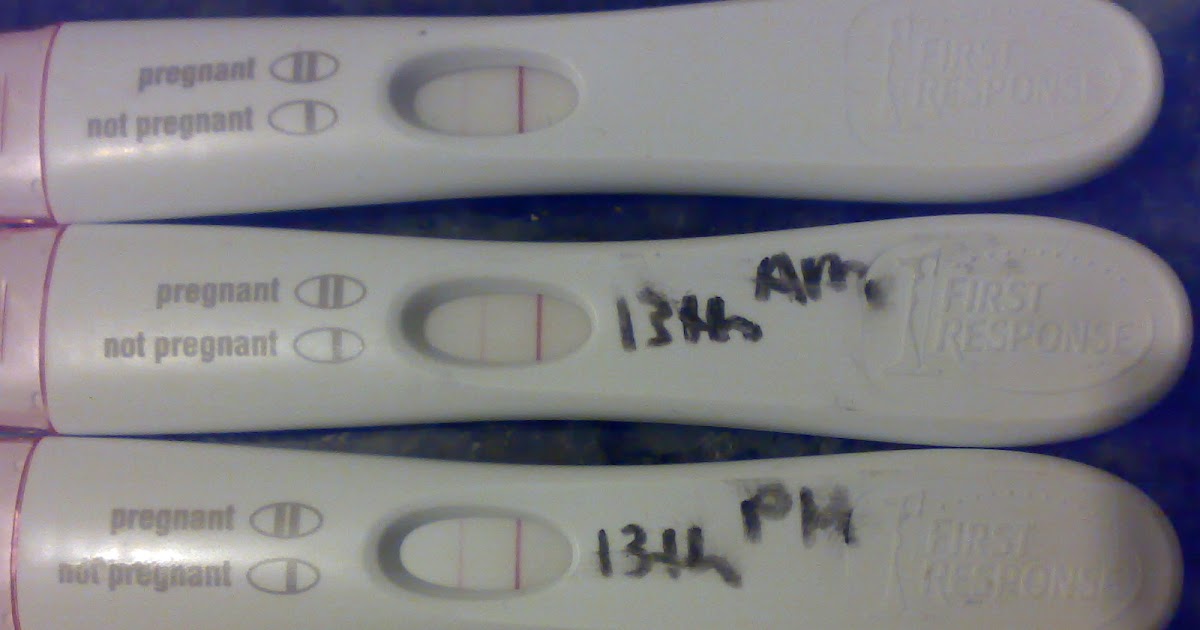
You may be able to have an external scan of your tummy if you prefer, although this method reduces the accuracy of the scan. Neither type of scan is dangerous to the baby and they do not increase your risk of miscarriage.
You may also be offered blood tests to measure hormones associated with pregnancy. You usually need to have 2 blood tests 48 hours apart to see if your hormone levels go up or down.
Sometimes a miscarriage cannot be confirmed immediately using ultrasound or blood testing. If this is the case, you may be advised to have the tests again in 1 or 2 weeks.
Recurrent miscarriages
If you've had 3 or more miscarriages in a row (recurrent miscarriages), further tests are often used to check for any underlying cause. However, no cause is found in about half of cases.
If you become pregnant, most units offer an early ultrasound scan and follow-up in the early stages to reassure and support parents.
Karyotyping
If you've had a third miscarriage, it's recommended that the foetus is tested for abnormalities in the chromosomes (blocks of DNA).
If a genetic abnormality is found, you and your partner can also be tested for abnormalities with your chromosomes that could be causing the problem. This type of testing is known as karyotyping.
If karyotyping detects problems with your or your partner's chromosomes, you can be referred to a clinical geneticist (gene expert).
They'll be able to explain your chances of a successful pregnancy in the future and whether there are any fertility treatments, such as IVF, that you could try. This type of advice is known as genetic counselling.
Read more about genetic and genomic testing.
Ultrasound scans
A transvaginal ultrasound can be used to check the structure of your womb for any abnormalities.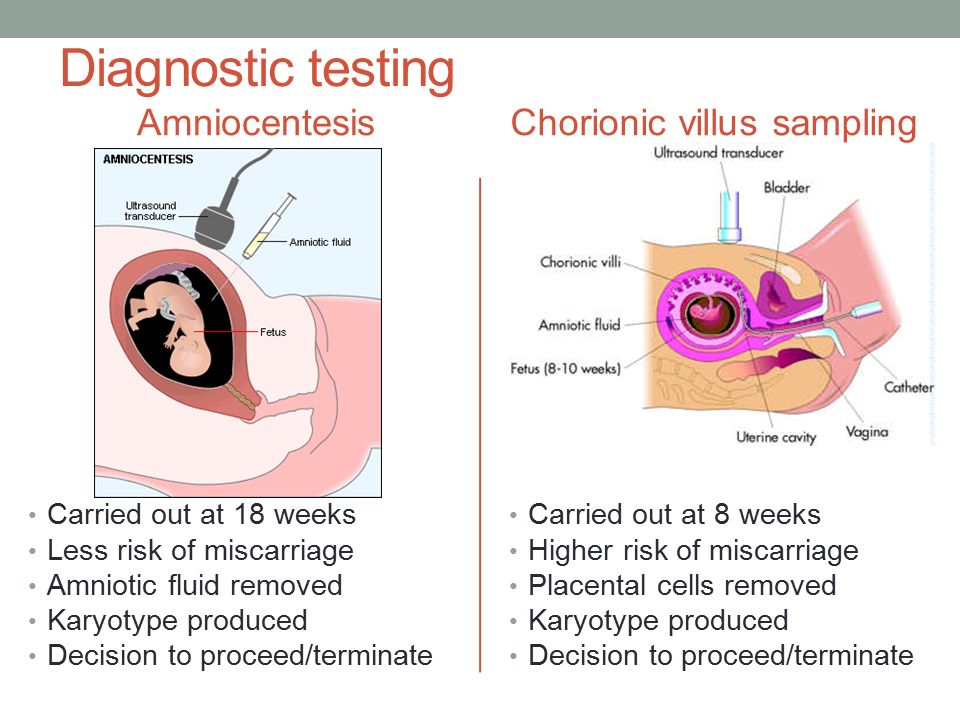 A second procedure may be used with a 3D ultrasound scanner to study your lower tummy and pelvis to provide a more accurate diagnosis.
A second procedure may be used with a 3D ultrasound scanner to study your lower tummy and pelvis to provide a more accurate diagnosis.
The scan can also check if you have a weakened cervix. This test can usually only be carried out when you become pregnant again, in which case you'll usually be asked to come for a scan when you are between 10 and 12 weeks pregnant.
Blood testing
Your blood can be checked for high levels of the antiphospholipid (aPL) antibody and lupus anticoagulant. This test should be done twice, a few weeks apart, when you're not pregnant.
These aPL antibodies are known to increase the chance of blood clots and change the way the placenta attaches. These blood clots and changes can reduce the blood supply to the foetus, which can cause a miscarriage.
Missed or delayed miscarriage
Sometimes a miscarriage is diagnosed during a routine scan carried out as part of your antenatal care. A scan may reveal your baby has no heartbeat or that your baby is too small for the date of your pregnancy. This is called a missed or delayed miscarriage.
A scan may reveal your baby has no heartbeat or that your baby is too small for the date of your pregnancy. This is called a missed or delayed miscarriage.
Page last reviewed: 09 March 2022
Next review due: 09 March 2025
5 Causes of a False Positive Pregnancy Test
If a woman is trying to conceive or suspects pregnancy, a pregnancy test, available from pharmacies or personal care stores, can help confirm these suspicions. Although many home pregnancy tests are 99% accurate, they are not perfect. A false positive result of a pregnancy test is one that indicates the presence of pregnancy in its absence.
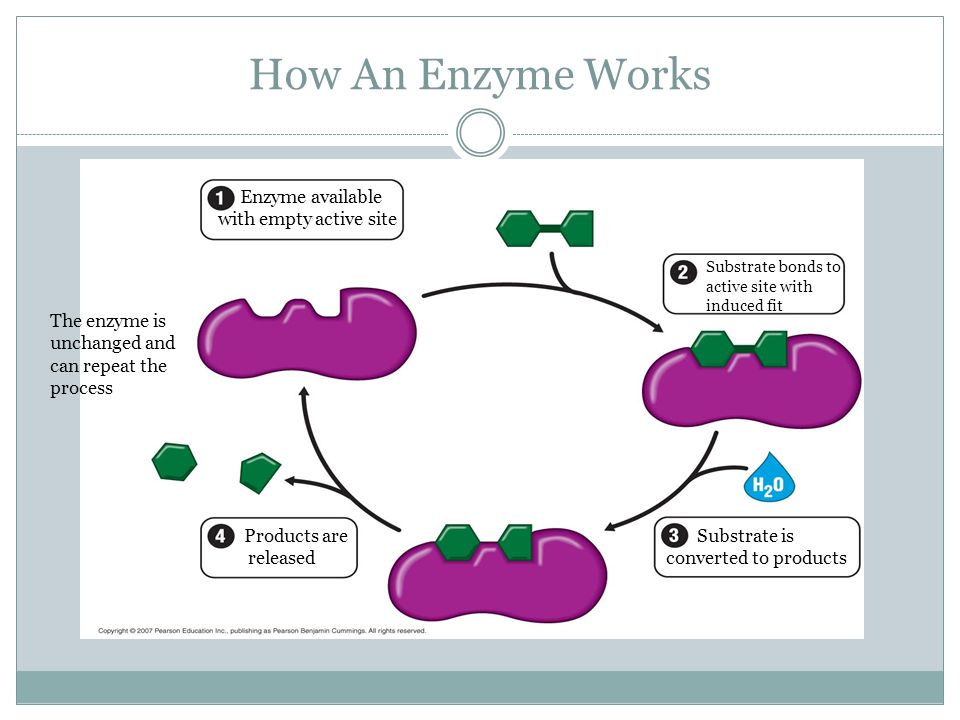
Pregnancy tests detect the presence of human chorionic gonadotropin (hCG) in the urine, a pregnancy hormone that is excreted in the urine and in the blood during pregnancy. It is important to note that when taking a pregnancy test, a woman should know that even a weak plus sign or a second line indicates a positive result.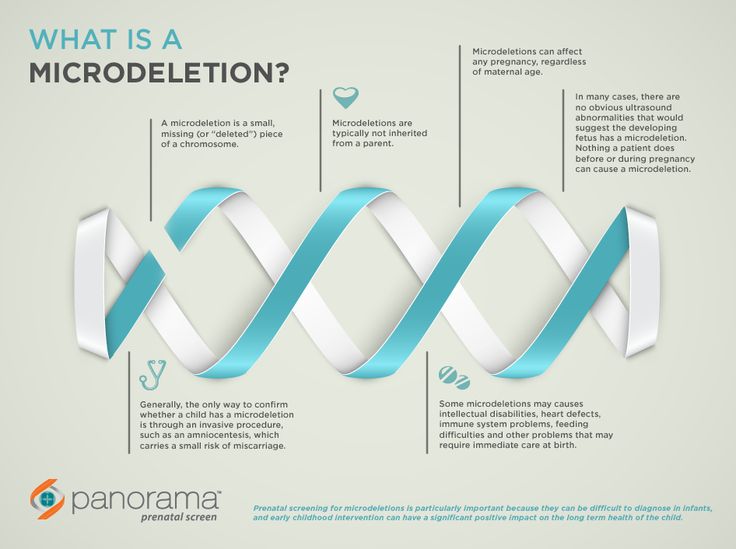
However, not all positive pregnancy tests mean that a woman is pregnant. There are some cases where a pregnancy test can give a false positive result:
Incorrect use of the test. When performing a home pregnancy test, it is important to follow the instructions carefully. Each brand has specific instructions, so it's important to read them carefully. For most tests, the result should be evaluated within 4-5 minutes after the test and no more than 10-30 minutes after that. If the pregnancy test is read after the recommended time, this may cause a weak second line to appear on the test - as a rule, this line appears after the urine has evaporated.
Previous miscarriage or abortion. After an abortion or miscarriage, a home pregnancy test may result in a false positive because the hCG levels in the woman's body may still be relatively high. As soon as a fertilized egg implants in the uterine wall, the body begins to secrete the hCG hormone.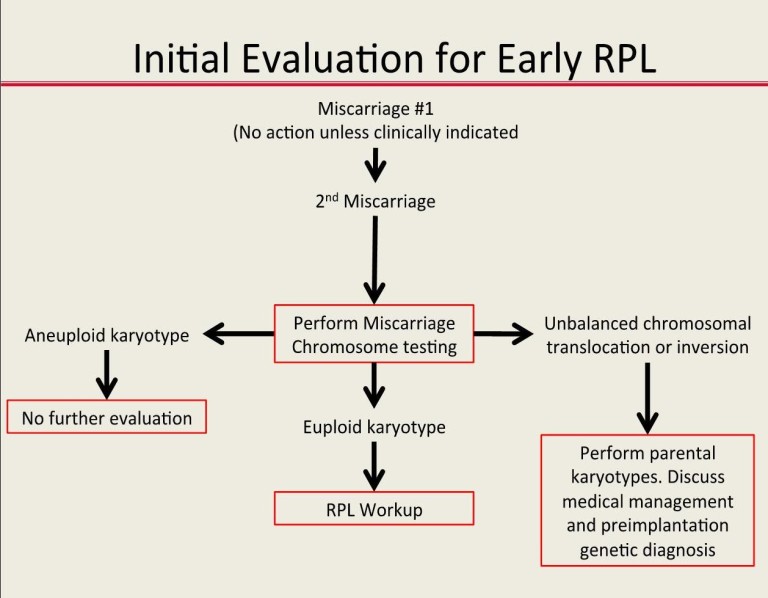 After a miscarriage or abortion, hCG levels begin to drop, but this happens slowly. As a rule, hCG decreases over a period of 9 to 35 days. The average time interval is about 19days. Taking a pregnancy test during this period may result in a false positive result.
After a miscarriage or abortion, hCG levels begin to drop, but this happens slowly. As a rule, hCG decreases over a period of 9 to 35 days. The average time interval is about 19days. Taking a pregnancy test during this period may result in a false positive result.
In some cases, a miscarriage may not occur completely, as a result, tissue remains in the uterus that provokes the release of hCG. In this situation, surgery may be required to remove any retained products of conception.
Molar pregnancy. It is caused by genetic abnormalities at conception and leads to abnormal pregnancy. In a complete molar pregnancy, the embryo does not develop, but the placental tissue grows rapidly. Typically, this happens because the woman's eggs lack the maternal chromosome, and the egg is fertilized by one or two sperm. In a partial molar pregnancy, the egg is fertilized by 2 spermatozoa. This results in an embryo containing 1 set of chromosomes from the mother and 2 sets of chromosomes from the father - 69chromosomes instead of the normal set of 46 chromosomes.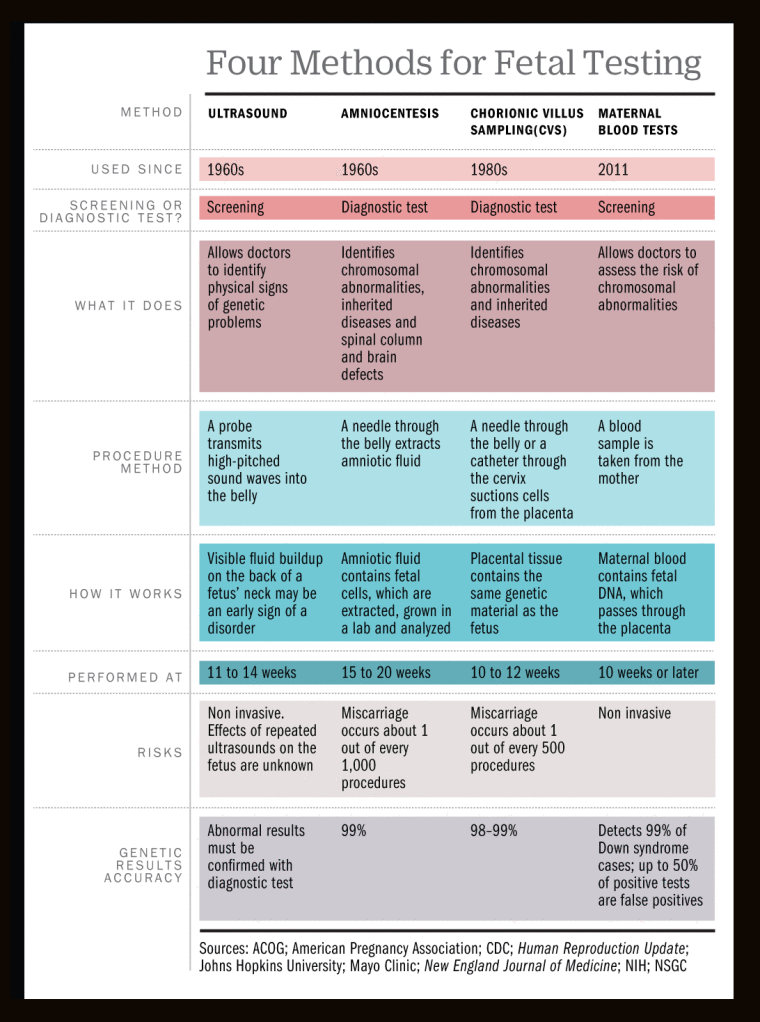
Instead of a normal placenta and embryo, placental tissue in molar pregnancy develops in a way that resembles a bunch of grapes. To eliminate such a pregnancy, an operation is required with careful monitoring of the level of hCG in a woman after the intervention. Sometimes a condition called persistent gestational trophoblastic disease can occur, which is associated with the continued growth of molar pregnancy products in the uterus. In this situation, surgery is required to remove the uterus or chemotherapy.
Medicines. Certain medications may cause a false positive pregnancy test result. These medicines include preparations with hCG as the active ingredient, which are often used to treat infertility. Yet most medications do not affect the results of home pregnancy tests.
Pathologies. Certain diseases and conditions can cause a woman's hCG levels to rise even if she is not pregnant. They include:
- disorders affecting pituitary hormone levels, especially in perimenopausal or menopausal women;
- gestational trophoblastic disease;
- cancer of the ovary, bladder, kidney, liver, lung, colon, breast and stomach;
- phantom hCG, when certain body proteins bind to molecules in a pregnancy test kit, resulting in a false positive result;
- ovarian cysts;
- kidney disease or urinary tract infection.
If a pregnancy test indicates a positive result, it is important to notify your physician as further evaluation and testing will be required to confirm and monitor pregnancy.
Based on www.medicalnewstoday.com
Early miscarriage - symptoms and how to prevent it
The term "early miscarriage" refers to a spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body.
In addition, a curious pattern was revealed: more often than a natural one, a pregnancy induced artificially ends in a miscarriage. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
Why can an early miscarriage occur?
Here are the most common causes, each of which significantly increases the risk of miscarriage:
- the future mother has certain infectious diseases, as well as STDs;
- intoxication of a woman's body for various reasons, including as a result of her living in an ecologically unfavorable region;
- all kinds of metabolic disorders in the body;
- hormonal disruptions, including those caused by a malfunction of the thyroid gland;
- various neoplasms in the uterus and others, as well as the cervix, pathologies;
- maintenance by the future mother of a life far from a healthy lifestyle. May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition;
- obesity;
- immune status disorders;
- cardiac diseases;
- diabetes mellitus;
- too early for pregnancy or, conversely, the patient's overly mature age at times increases the risk of miscarriage;
- all kinds of pathologies of chromosomes and genes;
- prolonged exposure to stress or severe psycho-emotional trauma in a woman.
The timing of a miscarriage may depend, among other things, on the patient's genetic predisposition to miscarriage. Finally, often its specific cause remains unexplained to the end.
Symptoms of miscarriage
A pregnant woman should urgently seek medical help if she has the following warning signs:
- bleeding from the vagina;
- spotting discharge from the genital tract. They can have both light pink and intense red or brownish tint;
- convulsions;
- severe pain in the lumbar region;
- abdominal pain, etc.
All of the above signs can be symptoms of a miscarriage. Timely provision of qualified medical care is the key to maintaining pregnancy.
Life after miscarriage
If a woman could not bear the pregnancy - an early miscarriage crossed out all her plans - then she needs to calm down and take all measures to prevent such complications in the future.