How to relieve pelvic pain while pregnant
What’s Causing It and How You Can Treat It
Message from our CEO Leighton McDonald
March 29, 2022
To Our Clients, Families and Caregivers,
It has been a long two years while we have all worked so hard together to manage the impact of COVID-19 in our own lives and in our communities. Throughout this time, CTG has been committed to continuing to safely deliver high quality care. I am happy to share that 99% of all CTG team members are fully vaccinated against COVID. A very small number of team members have been granted a vaccine exemption and these individuals test themselves for COVID on a regular basis.
As we enter this new phase of the COVID-19 pandemic in Canada, some public health requirements in public settings are changing. Changes such as no longer needing to provide proof of vaccination to dine in a restaurant or no longer being required to wear a mask when we go for groceries.
While these may be welcome changes in public settings, in home care we work in close proximity to people for periods of time and throughout the day we are often providing service to individuals who are vulnerable to becoming very sick due to a COVID-19 infection. As such, we must continue to work together to keep you, other clients and their families, and our CTG team members safe.
Our number one priority will always be the safety and well-being of our clients and CTG team members, every day and at every community, school, or clinic visit. CTG team members follow best practices in infection prevention and control, and we need you to be part of the safety team. Here’s what we can do together to keep everyone safe.
Before your visit
• A CTG team member will be asking you a series of screening questions the day before your visit and again at the time of your visit or appointment.
• It is critical that you answer all the questions honestly as it will help us keep everyone safe. Be assured that regardless of the screening results, you will receive the care you need but we may need to take additional precautions for your safety and the safety of others.
During your visit
• Your CTG health care provider will be wearing both a mask and a face shield or goggles. This is for both their protection and yours.
This is for both their protection and yours.
• You are asked to wear a mask when the CTG provider is in your home; if you do not have a mask, one will be provided to you. All nursing and physiotherapy clients will be provided a new mask when they arrive at a CTG clinic.
• Younger clients are also asked to wear a mask when receiving services in home or at school.
• If caregivers must be present and close by during a visit, they will be asked to wear a mask or face covering.
• Individuals in the home will be asked to maintain a 2 metre (6 feet) physical distance from the CTG provider unless they are an essential part of the care.
• Now that winter is easing, when possible, kindly open doors and windows in your home to take advantage of natural ventilation when a CTG team member is in your home.
• CTG team members will clean their hands frequently for your safety and we ask you do the same.
CTG prides itself on being a Team Made for Caring and our team includes you. Together we can continue to ensure you safely receive the high-quality care you deserve, and our team members remain safe.
Together we can continue to ensure you safely receive the high-quality care you deserve, and our team members remain safe.
If you have any questions or would like more information, please feel free to reach out to us. You can also find current information at www.ontario.ca/coronavirus or www.novascotia.ca/coronavirus
Sincerely,
Leighton McDonald
President & Chief Executive Officer
Closing the Gap Healthcare
How To Relieve Pelvic Pain During Pregnancy, 1st Through 3rd Trimester
by arizonapain
If you’re expecting, you know by now that pregnancy can be both exciting and exhausting. While you’re dreaming of the moment you’ll finally hold your little one in your arms, you’re also probably looking forward to relief from the common side effects of pregnancy. Of the many ailments expectant mothers experience, pelvic pain during pregnancy is one of the most common complaints.
Of the many ailments expectant mothers experience, pelvic pain during pregnancy is one of the most common complaints.
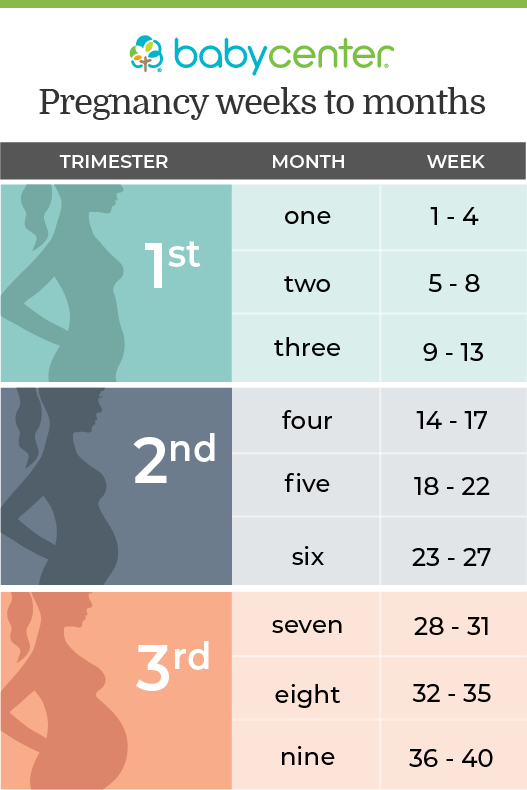
In fact, approximately 72% of pregnant women experience pelvic pain at some point. It’s commonly characterized by pain across the front of your pubic bone, level with your hips or across one or both sides of your lower back. While pelvic pain isn’t harmful to your baby, it can make your pregnancy uncomfortable. This post will cover why pelvic pain tends to occur at each stage of pregnancy, how to ease the discomfort you feel, and symptoms that could be an indication of something more serious.
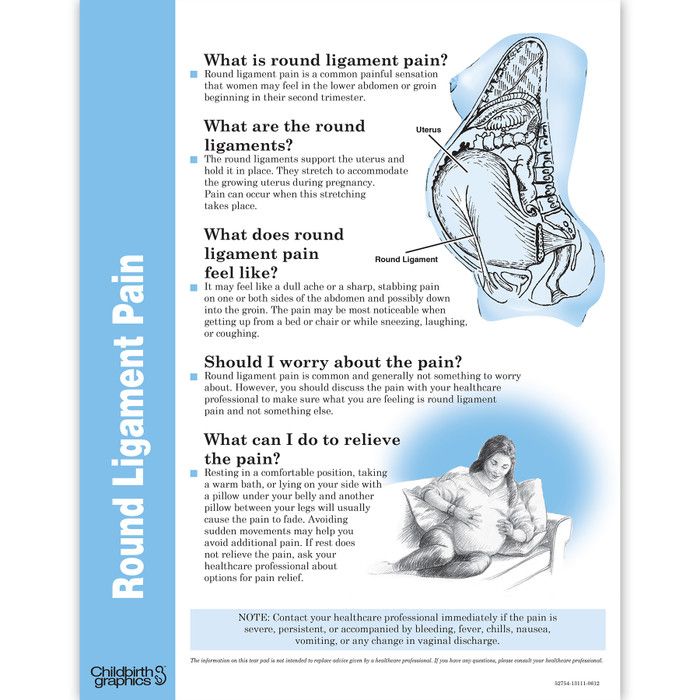
Why does pelvic pain during early pregnancy occur?Most women are surprised by the occurrence of pelvic pain in early pregnancy, but hormones are typically responsible for this sudden change. When you become pregnant, your body immediately starts to produce a hormone called relaxin. This hormone allows tendons and ligaments to stretch to allow the pelvis to open for birth.
While relaxin itself is not the cause of pelvic pain, the relaxed ligaments and tendons may lead your weight distribution to change, especially towards the end of your first trimester. This can cause both hip pain and pelvic pain during early pregnancy.
Unfortunately, this hormone will continue to release throughout your pregnancy. This means your pelvic pain may worsen as the months go on.
How can I relieve pelvic pain during early pregnancy naturally?While treatment options are often limited during pregnancy in order to protect your growing baby, there are some ways to relieve pelvic pain naturally.
However, always discuss your pain level and symptoms with your doctor before trying anything new. Be open and honest about how you’re feeling and how much pain you can tolerate.
Prenatal massageGetting a specialized prenatal massage can help to reduce stress hormones, relax your muscles, and increase blood flow. The boost in circulation after a massage will not only ease your discomfort, but may also help you sleep better (a welcome benefit for women suffering from aches and pains associated with pregnancy).
The boost in circulation after a massage will not only ease your discomfort, but may also help you sleep better (a welcome benefit for women suffering from aches and pains associated with pregnancy).
While any masseuse can perform a prenatal massage, it is best to go to someone who specializes in maternal care and has extensive experience working on pregnant women. They will know what positions to avoid and what level of pressure is acceptable. This will guarantee the safety of you and your baby.
Chiropractic careChiropractic care is generally considered safe during pregnancy. In fact, all chiropractors go through training designed specifically for the care of pregnant patients.
Through spinal manipulation and adjustments, a visit to the chiropractor may help relieve some of your pelvic pain. Achieving proper alignment for both standing and sitting can help you maintain a posture that won’t put added pressure on your body. This is crucial as your weight distribution will continue to shift as your baby grows.
As always, check with your doctor for a referral before seeking chiropractic care during pregnancy.
Exercise and stretchingIf your doctor has cleared you for exercise, staying active within your pain limits is one of the best ways to prevent and ease pelvic pain during pregnancy. Your doctor may even recommend at-home exercises and stretches for your pelvic floor, stomach, back, and hip muscles. Pelvic tilt exercises in particular can help strengthen your muscles and improve your posture to provide relief from pelvic pain.
If you’re considering workout classes, prenatal yoga, water aerobics, and swimming are all great options for low-impact exercise. Gyms and fitness studios across the country offer classes that are specifically created for pregnant women. Talk to your doctor about any local ones they recommend.
Maintaining an exercise routine can help alleviate pain by keeping you limber, but most women enjoy many other additional benefits. Exercising will help you sleep better and can even improve the overall ease of your labor and delivery. Staying active during pregnancy may also make it easier to get back in shape after your baby is born.
Exercising will help you sleep better and can even improve the overall ease of your labor and delivery. Staying active during pregnancy may also make it easier to get back in shape after your baby is born.
Pregnancy pillows (also known as body pillows) have become popular for pregnant women, and for good reason. Sleep is crucial for maintaining a healthy lifestyle and pregnancy, but it can become increasingly difficult as you continue to grow and gain weight.
There are a variety of shapes and sizes when it comes to pregnancy pillows, but one that is specifically designed to be placed between your knees is best for relieving pelvic pain. This position will ensure that your hips are aligned, stable, and at the correct height at night to minimize pressure in the pelvic and hip region.
Another type of pregnancy pillow is in the shape of a wedge. It simply lifts your growing belly off the mattress to relieve the pressure and weight you’re feeling in that region, especially while lying down.
Belly bands and compression pantyhose are a great option for everyday wear as you continue to grow throughout your pregnancy.
Belly bands or maternity belts are designed to lift your belly, giving your back and pelvic area extra support and relief from the weight of your growing baby. Many of them can be heated in the microwave to provide soothing heat therapy for tight and sore muscles.
Compression pantyhose offer the benefit of lifting your belly and giving it support while also adding compression around your legs. This can be helpful if you’re suffering from excessive swelling in the legs and feet.
What causes pelvic pain during pregnancy in later trimesters?Pelvic pain during the second and third trimesters can still be attributed in part to relaxin. This hormone will continue to surge through your body, especially in the final weeks before you give birth. It will continue to loosen your ligaments and open your pelvis for labor.
In addition to the relaxin hormone loosening and stretching your tendons and ligaments, your growing belly also creates a shift in the way your weight is distributed. This can affect everything from your stance to the way you walk. This is why it can often be painful no matter what position you’re in. For this reason, it’s best not to stay standing or sitting for too long.
It’s important to note that pelvic pain can also get much worse about two to four weeks before delivery once lightening occurs. Lightening is when your baby drops into the pelvic area in preparation for labor. Once this happens, your baby’s head puts stress on the bones, joints, and muscles in your pelvis and back. The good news? This is another indication that labor is near and the end is in sight!
pregnancy, medicine, healthcare and people concept – gynecologist doctor with laptop computer and pregnant african american woman meeting at hospitalHow can I relieve pelvic pain during pregnancy in the second and third trimester?The previously mentioned treatment options for relieving pelvic pain during early pregnancy are still great options in your second and third trimesters, but with a few modifications.
Your doctor will advise you to sleep on your side after your first trimester. This is because your growing uterus can put pressure on blood vessels, restricting the blood flow to both your heart and your baby’s heart. This same rule applies during exercise or any other activity that requires you to lie down, such as a prenatal massage. It’s always best to seek out instructors and practitioners who are specifically trained to work with pregnant women so that they’re aware of these guidelines.
Basic lifestyle changes should also be made during your second and third trimesters. Wear comfortable shoes with little to no heel and plenty of support, especially if you plan to be walking or exercising. You may also want to consider adding a warm bath to your nightly routine, as this can often help relieve pain and relax your muscles before bedtime.
When should I see my doctor for pelvic pain during pregnancy?As always, it’s important to contact your doctor if you feel like something isn’t right.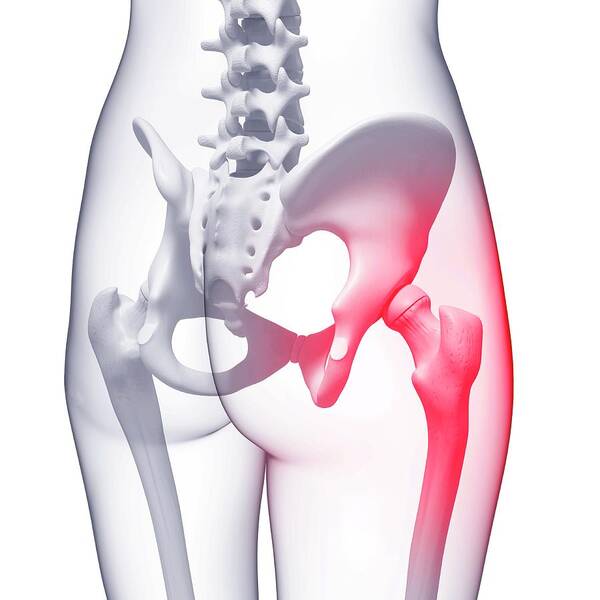 While it’s normal to feel aches and pains as your pregnancy progresses, there are times when pain can be a sign of a more serious problem.
While it’s normal to feel aches and pains as your pregnancy progresses, there are times when pain can be a sign of a more serious problem.
Be open and honest about the level of pain you’re experiencing during appointments. Call your doctor immediately if you have any of the following symptoms:
- Pain that you can’t walk or talk through
- Bleeding
- Fever
- Chills
- Severe headache
- Dizziness
- Sudden swelling of the hands, feet, or face
- Persistent nausea and vomiting
In rare, but serious cases, pelvic pain can be a sign of complications or miscarriage, especially if it is paired with other symptoms. These are some of the serious causes of pelvic pain that you should be aware of.
Ectopic pregnancyWhile it is considered rare, one in 50 pregnancies are classified as an ectopic or tubal pregnancy. This is when the egg implants outside of the uterus, most often in the fallopian tube. Symptoms include intense pain and bleeding. This happens most commonly between the sixth and tenth week of pregnancy.
This happens most commonly between the sixth and tenth week of pregnancy.
Unfortunately, ectopic pregnancies can’t continue and must be treated immediately. If you have taken a positive at-home pregnancy test and are experiencing these types of symptoms, you should contact a doctor immediately. A medical team will use an ultrasound to confirm whether the egg has implanted in the uterus.
Preterm laborIf you have persistent back and pelvic pain that comes and goes (with no relief after resting and lying down), you could be experiencing preterm labor.
Be sure to contact your doctor immediately if you think you could be feeling contractions, rather than basic pelvic pressure and pain.
PreeclampsiaAccording to the Preeclampsia Foundation of America, 5-8% of all pregnant women experience preeclampsia. The condition, characterized by high blood pressure and protein in your urine, can develop at any time after 20 weeks.
This condition is dangerous because blood pressure can constrict the blood vessels in your uterus that supply oxygen and nutrients to your baby. In severe cases, symptoms of preeclampsia can include abdominal pain.
Placental abruptionYour placenta typically implants high on the uterine wall and doesn’t detach until after your baby is born.
In rare cases, though, the placenta can separate from the uterine wall, causing constant and worsening pain in the lower abdominal region. Depending on the case, you may go into labor naturally. If not, your doctor will opt to either induce labor or perform an emergency cesarean section.
Uterine fibroidsMost common during childbearing years, noncancerous growths on the uterus are known as fibroids.
Pregnancy will often cause them to get larger and increasingly painful. Most doctors will simply keep an eye on them during your pregnancy. Only in rare cases is it necessary to remove them in order for the pregnancy to progress.
This is a special time in any woman’s life. Don’t let pelvic pain during pregnancy overshadow the anticipation and joy of welcoming a baby to your family. Talk to your doctor about what treatment options are right for you.
If you live in Arizona, get in touch with our pain specialists at Arizona Pain today. We have skilled physicians with extensive experience in pain management. We will tailor your treatment plan to ensure safe and successful pain relief during your pregnancy, coordinating with your other care providers.
Methods for the prevention and treatment of pain in the lumbar region and pelvic region during pregnancy
Review question
We were looking for evidence of the effect of any treatment used to prevent or treat low back pain, pelvic pain, or both during pregnancy. We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
Relevance
Pain in the lumbar region, pelvic region, or both is a common complaint during pregnancy, often progressing as the pregnancy progresses. This pain can interfere with the daily activities, work, and sleep of pregnant women. We wanted to find out which treatment or combination of treatment options would be better than conventional prenatal care for pregnant women with these complaints.
Study profile
This evidence is current to 19 January 2015. We included 34 randomized trials with 5,121 pregnant women aged 16 to 45 in this updated review. The women were between 12 and 38 weeks pregnant. Studies have looked at various treatments for pregnant women with low back pain, pelvic pain, or both types of pain. All treatments were added to routine antenatal care and only compared to routine antenatal care in 23 studies. Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Main results
Pain in the lumbar region
When we combined the results of seven studies (645 women) that compared any form of physical exercise with routine prenatal care, exercise (lasting five to 20 weeks), we found that women with low back pain improved and disability rates decreased .
Pelvic pain
Less evidence is available for the treatment of pelvic pain. Two studies showed that women who participated in group exercise and received training in pain management reported no difference in pelvic pain compared to women who received routine prenatal care.
Pain in the lumbar region and pelvis
Results from four studies (1,176 women) when combined showed that an 8 to 12 week exercise program reduced the number of women who complained of low back and pelvic pain. In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
However, two other studies (374 women) found that group exercise and education was no better in preventing pain, both in the pelvic region and in the lumbar region, compared with conventional prenatal care.
There have been a number of separate studies that have evaluated different treatment options. These results confirm that craniosacral therapy, osteomanipulation therapy, or multimodal intervention (manual therapy, exercise, and education) may be beneficial.
When side effects were reported, there were no long-term side effects in any of the studies.
Quality of evidence and conclusions
There is low-quality evidence that exercise reduces pain and disability in women with low back pain, and moderate-quality evidence for the effect of exercise on reducing sick leave and reducing the number of women with both lower back and pelvic pain complaints. The quality of the evidence depends on problems with study design, small numbers of women, and variable results. Ultimately, we believe that future research is likely to change our findings. There is not enough good quality evidence to make confident decisions about the treatment of these complaints.
The quality of the evidence depends on problems with study design, small numbers of women, and variable results. Ultimately, we believe that future research is likely to change our findings. There is not enough good quality evidence to make confident decisions about the treatment of these complaints.
Translation notes:
Translation: Kong Hong Han. Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center based at Kazan Federal University). For questions related to this translation, please contact us at: [email protected]
How to avoid or manage pelvic pain during pregnancy
06 Aug 2018
My name is Fedaka Anna, I am a yoga teacher for pregnant women , I have been teaching Perinatal Yoga teachers since 2012, a rehabilitation therapist. I have three children and at the time of writing I was pregnant with my fourth.
It was a case from my life and practice that caused me to develop a new complex for pregnant women and write this article.
Many pregnant women experience discomfort in the pelvis, hip joints, lower abdomen and perineum. Degree Pain varies from slight tingling at the beginning of movement to severe pain that can interfere with walking. The longer the pregnancy and the less general physical activity, the earlier these symptoms appear. Sometimes a pregnant woman walks to childbirth with difficulty, gets up from a chair, rolls over in bed.
There is a type of woman who is more prone to this condition than others. These are women of the gynecoid type - with an apple-shaped figure: with wide hips and narrow shoulders. It is easier for such women to give birth due to the mobility of the pelvic bones and the general structure of the body, the nervous and hormonal systems. But it is they who experience discomfort and expressed pelvic pain long before delivery.
This phenomenon is sometimes called symphysitis , but of course this is not yet it, it is the mobility of the pelvic bones that increases during pregnancy, the preparation of the body for childbirth.
Symphysitis - inflammation of the tissues of the pubic joint during pregnancy and divergence of the pubic bones. Manifested by pain over the pubis of varying severity. Pain is aggravated by walking, climbing stairs, turning over in bed, and other physical exertion. Pain causes changes in gait, sometimes it becomes impossible to perform some movements. For treatment, calcium preparations, anti-inflammatory and analgesic agents are used. In severe cases, caesarean section is chosen as the most preferred method of delivery.
A special hormone, relaxin, appears in the body from the first days of pregnancy, its content during this period is 10 times higher than the non-pregnant norm. It helps to soften all joints: it mainly affects the sacroiliac and pubic joints, the hip and joints of the spine. Because of it, the size of the foot increases in pregnant women. To a certain extent, discomfort is normal, but you want to minimize it and keep it under control.
Because of it, the size of the foot increases in pregnant women. To a certain extent, discomfort is normal, but you want to minimize it and keep it under control.
I myself go through this every pregnancy. At different times, the first three times, depending on the number of kilograms gained and physical activity, there were unpleasant sensations in the hip joints and pelvic joints, as well as in the pelvic diaphragm. My personal statistics: the first pregnancy sensations appeared at 38 weeks (increased until the end of 42), in the second - at 35-36, in the third - two weeks earlier, and now in the fourth pregnancy - at 29 weeks. This is understandable, the older the woman and the more pregnancies there were, the more pronounced all the symptoms. But how early this time - at least 3 more months before the birth. The prospect of crawling instead of walking, and turning over in bed in four stages with rest, did not suit me at all. And there was no way out, something had to be done: the pain was severe, and mobility was significantly limited.

Rapid weight gain and insufficient or, conversely, excessive physical activity can provoke such a condition.
This time I had a long and heavy domestic load. I gathered my family for departure to the sea for the whole summer, prepared the house for our absence, swapped winter and summer things, sorted, shifted, drove a lot, and the housekeeper also went on an unplanned vacation. So almost two weeks. Already at the end, just before departure, I began to feel heaviness in the pelvic floor and slight pain in the pubic joint, but decided not to pay attention to it. I tied up with a sling and continued my activity. The trigger was a long trip, in a sitting position, I spent more than 8 hours. The next day after the flight, she could no longer move without a rather hard tie-up, rested every 20 minutes, and could barely walk. The pains increased, the difficulty of movement too. But on the other hand, such a mockery of myself allowed me to understand what to do in such a state and what to avoid.
I have compiled a set of rules for life and a set of exercises that will help to cope with pain or significantly alleviate it.
Rules for life in the acute period:
- Do not sit. Neither soft nor hard, in any case, do not drive a car while sitting. Sitting instantly exacerbates the situation, makes the pelvic bones diverge more, exacerbates the pain. But you can stand, walk or lie down.
- Walk in small steps, trying to roll the entire foot on the floor surface, engage the gluteal muscles in walking. There are also special MBT sneakers, in which it immediately becomes clear which muscles should work when walking.
- When you are standing, you need to work with your foot, extend your thumbs, distribute the load between the outer edge of the entire foot, the inner edge of the heel and the ball under the thumb, lift the inside ankle, do not collapse the arch of the foot. In general, it is preferable to stand in Tadasana, working hard with the muscles of the feet and thighs.
- If there is something that you can lean on with your hands or chest - you have to lean - then you will get Ardha Uttanasana, and here you also need to work with your feet.
- When it's really hard, during any movement you need to tie up with a sling. The sling should go over the shoulders.
Another very important point when tying up is not so much to remove the heaviness of the abdomen, but to tighten the pelvis between the ilium and hip joints.
By the way, in Japan this is routine support during pregnancy. It differs from the bandage, which is most often used in Russia. That is, at first the lower part of the sling passes in this place, supports the stomach and rests on the shoulders with straps. When the acute period has passed and the pain has decreased, you can tie up only in the pelvic region with a wide soft belt or scarf.
- Take homeopathic Calcarea Phosphorica 30 3 times a day for 3 peas for 3 days or as long as there is pain.
Complex in the acute period:
- Vajrasana with support on the shins, 3 times for 20 seconds.
- Tadasana with emphasis on foot and leg muscles, 1 min.
- Ardha Uttanasana with the same accent, 3 min.
- Adho Mukha Svanasana on ropes, with heels on the floor, 3 min.
- Dynamic setu bandha sarvangasana, 8-10 reps.
- Sarvangasana with chair, 5 min.
- Viparita karani on a bolster against the wall, 6 min.
It is advisable to do this complex 2 times a day. During the day, you need to practice Tadasana whenever you stand, Ardha Uttanasana whenever you stand and have something to lean on. And a pose for relaxation within 2-3 minutes after each episode of activity. Significant relief should come within 2-3 days.
After relief comes, there are still some rules.
- Do yoga at least 3 times a week for 90 minutes, always including asanas from the complex. If you don’t know how, go to a teacher for women’s practice or practice for pregnant women, I recommend Iyengar yoga. Any other yoga, which may be useful in a normal situation, will now loosen the joints even more.
- Practice Pelvic Floor Relief Pose periodically for about 10 minutes a day.
- Perform Viparita karani before going to bed every day for at least 5 minutes.
- Increase physical activity, gradually bring it up to 10 thousand steps a day. During an increase in the duration of walking, monitor sensations, prevent fatigue, split periods of walking, and rest in a prone position. Tie up if the pain intensifies.
- Walk over rough terrain so that the muscles of the legs and buttocks work while walking, up a small hill, up stairs with low steps.
 After such a walk, there should be relief from pain. If they are not, then it means they started early, we still have to wait. You can walk in MBT shoes.
After such a walk, there should be relief from pain. If they are not, then it means they started early, we still have to wait. You can walk in MBT shoes. - Avoid prolonged sitting until the end of pregnancy, sit for no more than 20 minutes. It is better to lie down, reclining or standing.
- Swim in the pool crawl, with hands on the board, work with legs. Breaststroke swim slowly and symmetrically. Just spend a lot of time in the water.
- Always sleep with a pillow between your legs. Or on the back, if there are no symptoms from the inferior vena cava.
- Avoid asymmetrical pelvic position when standing, sitting or lying down. Do not stand with a load on one leg, do not sit cross-legged, do not lie on your side without a pillow between your thighs.
- Eat enough protein (at least 1.2 g per 1 kg of weight), include in food or drink separately omega-3, 6, 9, eat enough saturated fats (about 1 g per 1 kg of body weight) and bone broth. Exclude simple carbohydrates, do not go beyond your caloric intake, for most pregnant women this is 2500-3000 kcal per day.