Sick in first trimester
Vomiting and morning sickness - NHS
Nausea and vomiting in pregnancy, often known as morning sickness, is very common in early pregnancy.
It can affect you at any time of the day or night or you may feel sick all day long.
Morning sickness is unpleasant, and can significantly affect your day-to-day life. But it usually clears up by weeks 16 to 20 of your pregnancy and does not put your baby at any increased risk.
There is a chance of developing a severe form of pregnancy sickness called hyperemesis gravidarum. This can be serious, and there's a chance you may not get enough fluids in your body (dehydration) or not get enough nutrients from your diet (malnourishment). You may need specialist treatment, sometimes in hospital.
Sometimes urinary tract infections (UTIs) can also cause nausea and vomiting. A UTI usually affects the bladder, but can spread to the kidneys.
Non-urgent advice: Call your midwife, GP or 111 if:
you're vomiting and:
- have very dark-coloured urine or have not had a pee in more than 8 hours
- are unable to keep food or fluids down for 24 hours
- feel severely weak, dizzy or faint when standing up
- have tummy (abdominal) pain
- have a high temperature
- vomit blood
- have lost weight
Treatments for morning sickness
Unfortunately, there's no hard and fast treatment that will work for everyone’s morning sickness. Every pregnancy will be different.
But there are some changes you can make to your diet and daily life to try to ease the symptoms.
If these do not work for you or you're having more severe symptoms, your doctor or midwife might recommend medicine.
Things you can try yourself
If your morning sickness is not too bad, your GP or midwife will initially recommend you try some lifestyle changes:
- get plenty of rest (tiredness can make nausea worse)
- avoid foods or smells that make you feel sick
- eat something like dry toast or a plain biscuit before you get out of bed
- eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta)
- eat cold foods rather than hot ones if the smell of hot meals makes you feel sick
- drink plenty of fluids, such as water (sipping them little and often may help prevent vomiting)
- eat foods or drinks containing ginger – there's some evidence ginger may help reduce nausea and vomiting (check with your pharmacist before taking ginger supplements during pregnancy)
- try acupressure – there's some evidence that putting pressure on your wrist, using a special band or bracelet on your forearm, may help relieve the symptoms
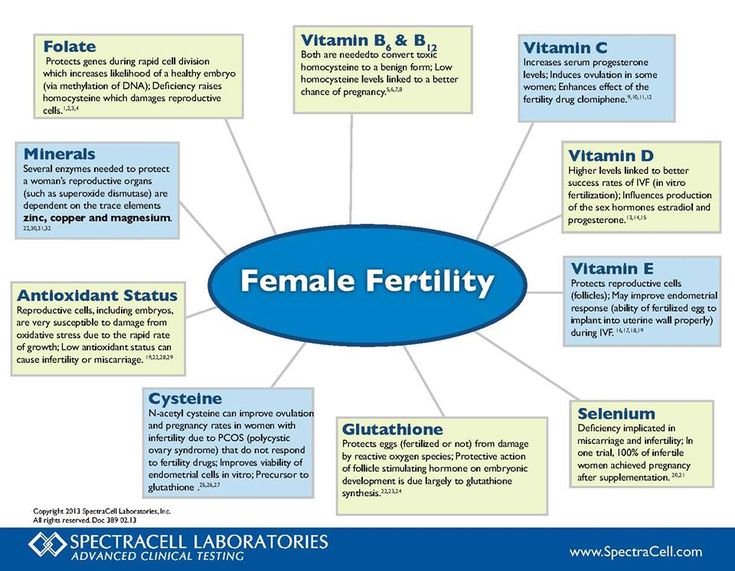
Find out more about vitamins and supplements in pregnancy
Anti-sickness medicine
If your nausea and vomiting is severe and does not improve after trying the above lifestyle changes, your GP may recommend a short-term course of an anti-sickness medicine, called an antiemetic, that's safe to use in pregnancy.
Often this will be a type of antihistamine, which are usually used to treat allergies but also work as medicines to stop sickness (antiemetic).
Antiemetics will usually be given as tablets for you to swallow.
But if you cannot keep these down, your doctor may suggest an injection or a type of medicine that's inserted into your bottom (suppository).
See your GP if you'd like to talk about getting anti-sickness medication.
Risk factors for morning sickness
It's thought hormonal changes in the first 12 weeks of pregnancy are probably one of the causes of morning sickness.
But you may be more at risk of it if:
- you're having twins or more
- you had severe sickness and vomiting in a previous pregnancy
- you tend to get motion sickness (for example, car sick)
- you have a history of migraine headaches
- morning sickness runs in the family
- you used to feel sick when taking contraceptives containing oestrogen
- it's your first pregnancy
- you're obese (your BMI is 30 or more)
- you're experiencing stress
Visit the pregnancy sickness support site for tips for you and your partner on dealing with morning sickness.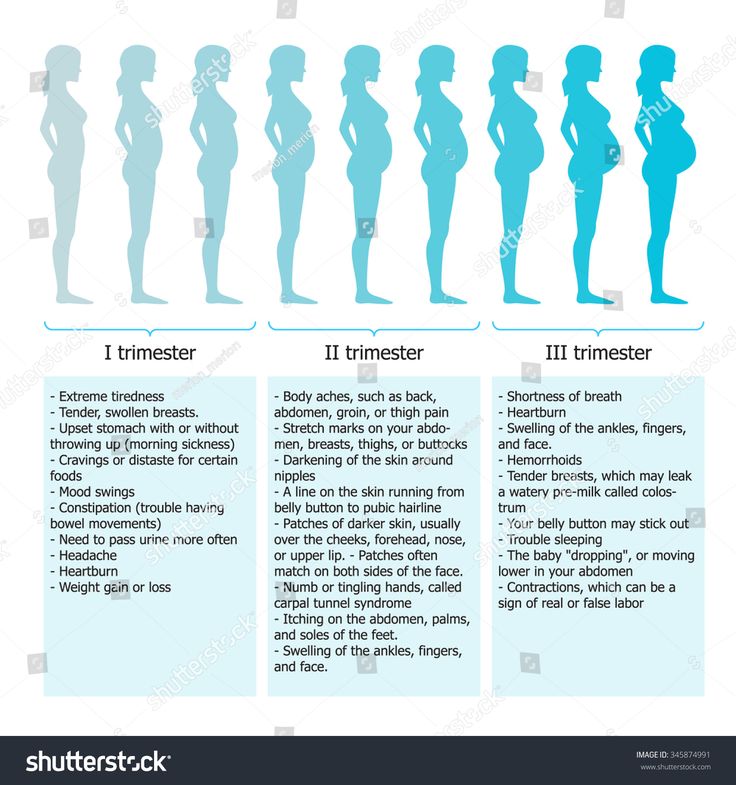
Find maternity services near you
Sign up for pregnancy emails
Sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Video: how can I cope with morning sickness?
In this video, a midwife gives advice on how to deal with morning sickness during your pregnancy.
Media last reviewed: 27 February 2017
Media review due: 27 March 2020
Page last reviewed: 13 April 2021
Next review due: 13 April 2024
Severe Morning Sickness (Hyperemesis Gravidarum) (for Parents)
What's Morning Sickness?
During the first trimester of pregnancy, many women have the bouts of nausea and vomiting known as morning sickness.
Despite its name, morning sickness can happen day or night. It usually starts around the 6th week of pregnancy, is at its worst around week 9, and stops by weeks 16 to 18. Although unpleasant, morning sickness is considered a normal part of a healthy pregnancy.
It usually starts around the 6th week of pregnancy, is at its worst around week 9, and stops by weeks 16 to 18. Although unpleasant, morning sickness is considered a normal part of a healthy pregnancy.
What’s Severe Morning Sickness?
Severe morning sickness is when nausea and vomiting get so serious that a pregnant woman vomits several times a day, loses weight, and gets dehydrated or is at risk for dehydration.
If this rare pregnancy-related condition isn’t treated, it can affect a woman's health and her baby's ability to thrive.
The medical term for severe morning sickness is "hyperemesis gravidarum" (hi-per-EM-eh-sis grav-ih-DARE-um), which means "excessive vomiting during pregnancy." It usually follows a similar timeline to normal morning sickness. But it can go longer, sometimes lasting for the whole pregnancy. Often, the symptoms get less severe as the pregnancy continues.
Most cases of hyperemesis gravidarum affect a woman's first pregnancy. But women who have it in one pregnancy are more likely to have it in future pregnancies.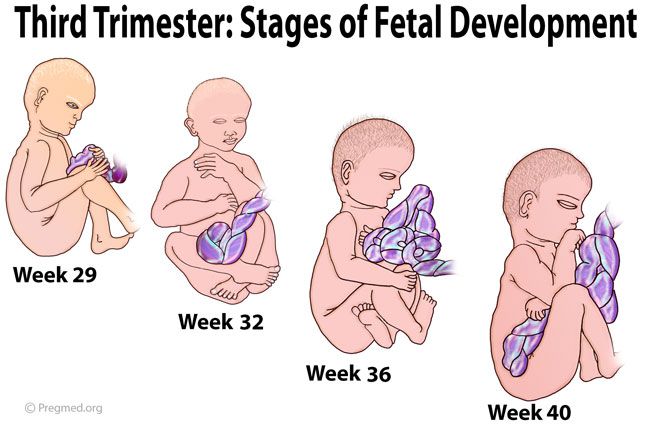
What Causes Severe Morning Sickness?
The cause of severe morning sickness isn’t known. But it might be related to the hormone changes of pregnancy. A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
Severe morning sickness also might run in families. It’s more common in women whose close family members (such as mothers and sisters) have had it.
Other things that can increase a woman's chances of having severe morning sickness include:
- carrying multiples (twins, triplets, etc.)
- history of motion sickness
- migraine headaches with nausea or vomiting
What Problems Can Happen?
The nausea and vomiting that happen in severe morning sickness are so extreme that they can harm the mother and the baby. Not being able to keep down food makes it hard for the mom to meet her nutritional needs. So she might lose weight. And a loss of fluids, combined with the loss of stomach acid from vomiting, can cause dehydration and electrolyte imbalances.
So she might lose weight. And a loss of fluids, combined with the loss of stomach acid from vomiting, can cause dehydration and electrolyte imbalances.
If severe morning sickness isn’t treated, it can cause many problems, including organ failure and the early birth of her baby.
When Should I Call the Doctor?
Call the doctor right away if you’re pregnant and have any of these symptoms:
- nausea that lasts throughout the day, making it impossible to eat or drink
- vomiting three to four times per day or not being to keep anything in the stomach
- brownish vomit or vomit with blood or streaks of blood in it
- weight loss
- fainting or dizziness
- peeing less than usual
- a fast heart rate
- a lot of headaches
- unpleasant, fruity mouth or body odor
- extreme tiredness
- confusion
How Is Severe Morning Sickness Treated?
Treatments used for morning sickness, such as eating dry crackers in the morning or a bland diet, may be recommended for women with extreme morning sickness. But these might not help with severe symptoms.
But these might not help with severe symptoms.
Medical treatment can include:
- a short period of not eating to rest the gastrointestinal system
- intravenous (IV) fluids
- vitamin and nutritional supplements
Some women might get medicine to stop the vomiting, either by mouth or through an IV. The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
- Eat a bland diet.
- Eat frequent small meals.
- Drink plenty of liquids when not feeling nauseated.
- Avoid spicy and fatty foods.
- Eat high-protein snacks.
- Avoid sensory stimuli that can act as triggers (like specific smells or noises).
If a woman feels anxious or depressed about her condition, talking to a therapist or counselor might help her cope with her feelings.
What Else Should I Know?
With treatment, women with severe morning sickness can feel better and get the nourishment they need so they and their babies thrive. And lifestyle changes can help ease nausea and vomiting and make the pregnancy more enjoyable.
And lifestyle changes can help ease nausea and vomiting and make the pregnancy more enjoyable.
With time, symptoms usually do improve. And, of course, they stop by the time a woman's next journey starts: parenthood.
Why pulls the stomach in the early stages of pregnancy?
Why does the stomach pull in the early stages of pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of having an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.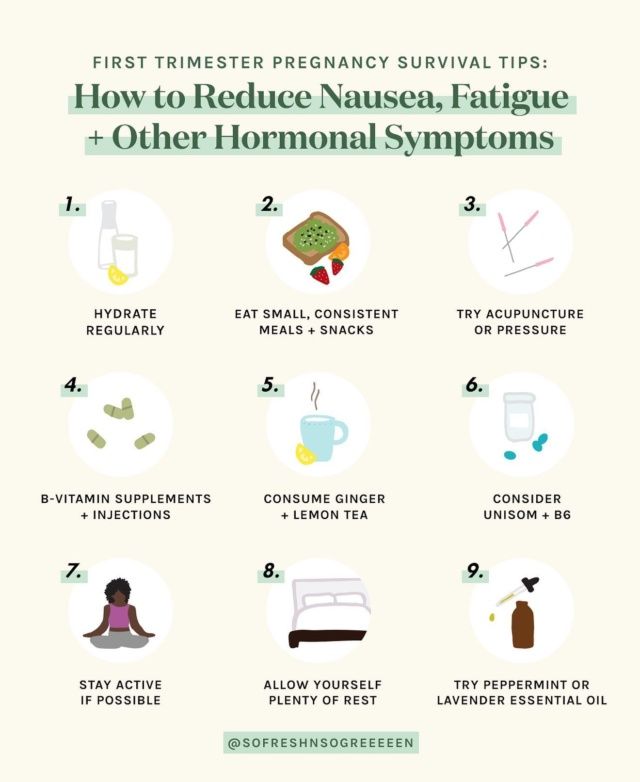 nine0003
nine0003
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas. nine0003
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment. nine0003
However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment. nine0003
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy may be:
- obstetric;
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- missed pregnancy;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.

Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- stretching of the ligaments and muscles associated with the growth of the uterus. nine0034
Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good when menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like. nine0003
nine0003
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual. nine0003
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes.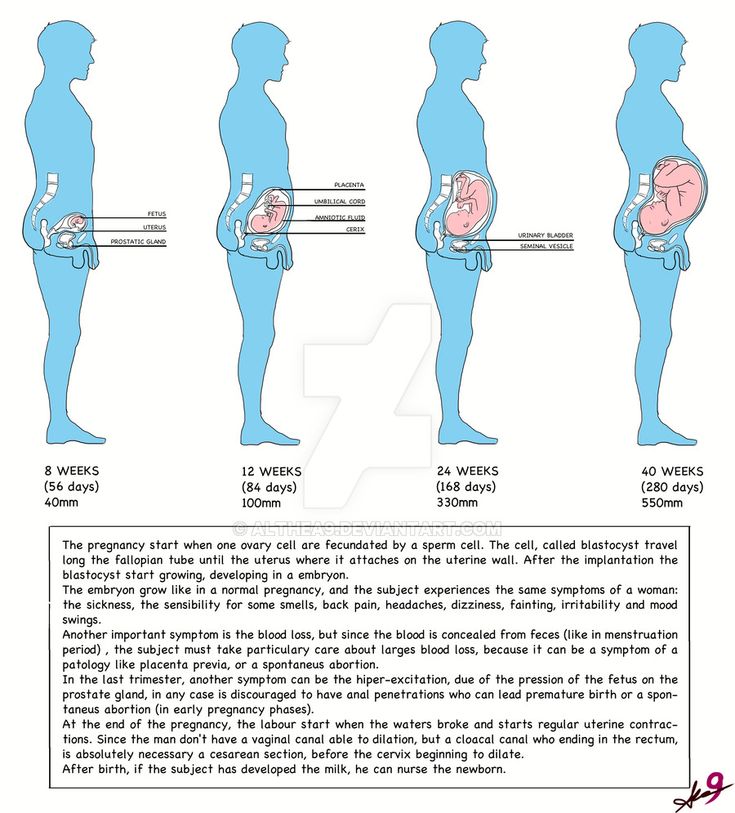 The uterine endometrium is a loose mass where a fertilized egg is implanted. nine0003
The uterine endometrium is a loose mass where a fertilized egg is implanted. nine0003
The process of implantation is the insertion of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child. nine0003
Among the reasons that may cause a miscarriage may be:
- severe physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss. nine0008
Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss. nine0008
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- aching or drawing pains in the small of the back or sacrum.
- bloody discharge from the genital tract.
If you have pain in the lower abdomen, you need to see a doctor, because a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless. nine0003
An ambulance should be called if:
- pain in the lower abdomen gets worse;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.

Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition. nine0003
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen. nine0003
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun. nine0003
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy. nine0003
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Miscarriage
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death.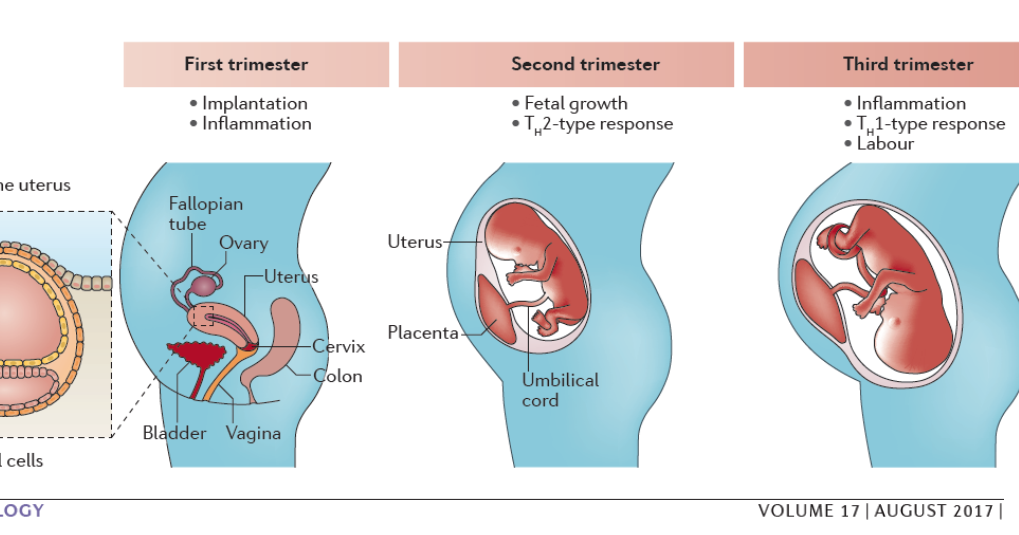 Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks. nine0003
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible. nine0003
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character. nine0003
nine0003
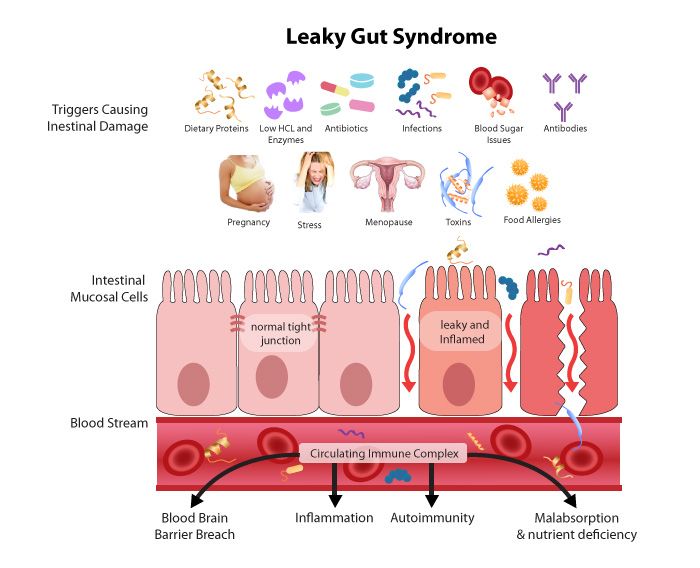
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken. nine0003
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins.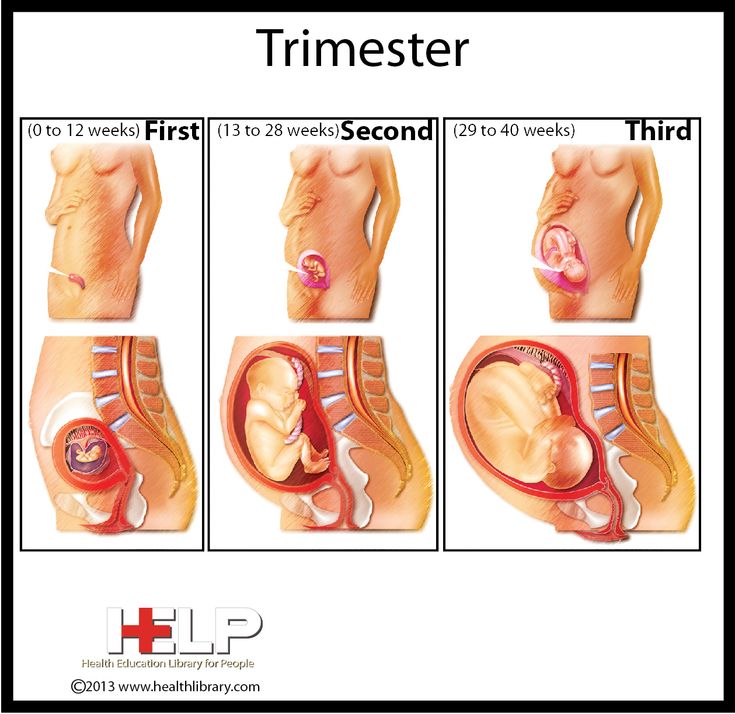 The only treatment is surgery. In this case, the pregnancy is preserved. nine0003
The only treatment is surgery. In this case, the pregnancy is preserved. nine0003
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Due to the anatomical features of a woman, cystitis can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women. nine0003
The bladder, located in the lower third of the abdomen, may give false symptoms of threatened miscarriage.
Cystitis, in addition to pulling or aching pains in the lower abdomen, is accompanied by pain during urination, pain at the end of the act of urination. In addition, with cystitis, the urine may be stained with blood, and it is difficult to distinguish this from bloody discharge during a miscarriage.
In any case, it is necessary to consult an obstetrician-gynecologist, pass a general urine test, and then consult a urologist and treat the infection. Any infection can adversely affect the condition of the fetus, so timely treatment is the key to the normal development of your child. nine0003
Any infection can adversely affect the condition of the fetus, so timely treatment is the key to the normal development of your child. nine0003
Make an appointment with a gynecologist
For more details, consult a qualified specialist at the Semeynaya clinic.
To find out prices for a gynecologist's appointment or other questions, follow the link below:
Pain in the first trimester in pregnant women
General information
The first trimester of pregnancy is the period from conception to the end of the 12th week of pregnancy. During the 1st trimester of pregnancy, the fertilized egg becomes an embryo, and embryo fetus.
The first trimester is an important time, the expectant mother needs to be especially careful and attentive to herself. After all, the health of the child will depend on the nutrition of the mother, her emotional and physical condition.
During the first twelve weeks, almost all vital organs are formed in the unborn child, and the body of the future mother gets used to her pregnancy and begins to work for the child.
First trimester pain in pregnancy
Physiological pain and symptoms in the first trimester that do not require treatment:
- Presumably due to hormonal changes observed during pregnancy, many women (especially at 1-2 weeks) experience a metallic taste in the mouth.
- There is swelling and pain in the breasts.
- Accumulation of blood in the pelvic organs makes the color of the vulva bluish or purple and may also cause frequent urination. nine0034
- A pregnant woman feels that she has begun to tire more quickly than usual; she may experience dizziness, nausea, vomiting (especially in the morning, but it happens throughout the day).
- Sense of smell becomes very acute; for example, some strong or pungent odors (tobacco, fried foods, alcohol) can cause nausea.
Pregnancy by week
At 6 weeks, many pregnant women begin to suffer from constipation and occasional abdominal pain. This is easy to fix if you drink enough water (up to 2 liters per day), and also include foods rich in fiber and fiber, lots of vegetables and fruits in the diet. nine0003
This is easy to fix if you drink enough water (up to 2 liters per day), and also include foods rich in fiber and fiber, lots of vegetables and fruits in the diet. nine0003
At 7 weeks, the uterus is about 8-10 cm in diameter. The breast continues to swell, the nipples may change color to a darker one. The growing uterus creates constant pressure on the bladder, squeezing it, which leads to pain in the lower abdomen and frequent urination.
At 12 weeks, a woman may feel a slight pain in the lower abdomen , which is due to tension in the ligaments that support the growing uterus.
In the first trimester of pregnancy, women usually suffer from pain in the lumbar region. However, this pain can absolutely disappear after the twentieth week of pregnancy.
Most women suffer from lower back pain in the first trimester due to softening of the supporting ligaments and discs and due to an increase in the hormone progesterone. If during pregnancy a woman gets sick with any infectious disease of the bladder, then this can also be the cause of lower back pain. Constant back pain in pregnant women is due to the fact that the center of gravity of the abdomen is changing, in which the child grows and develops. nine0003
Constant back pain in pregnant women is due to the fact that the center of gravity of the abdomen is changing, in which the child grows and develops. nine0003
If something goes wrong during the first trimester, there are two main scenarios: miscarriage or ectopic pregnancy. If you find yourself experiencing one of the symptoms discussed below, call your gynecologist immediately, or better yet, call an ambulance.
Threat of miscarriage
Miscarriage can be caused by different reasons. Some studies suggest that about 60% of all miscarriages during the first trimester are due to genetic abnormalities. Over 90% of women who have had a single miscarriage go on to give birth safely. However, it is worth waiting three to six months before trying again.
The risk of miscarriage increases with age. In women under 30, it is 10%, after 45 it rises to 50%. After two miscarriages, it's best to stop trying to conceive and have diagnostic tests done to understand what's causing the miscarriage.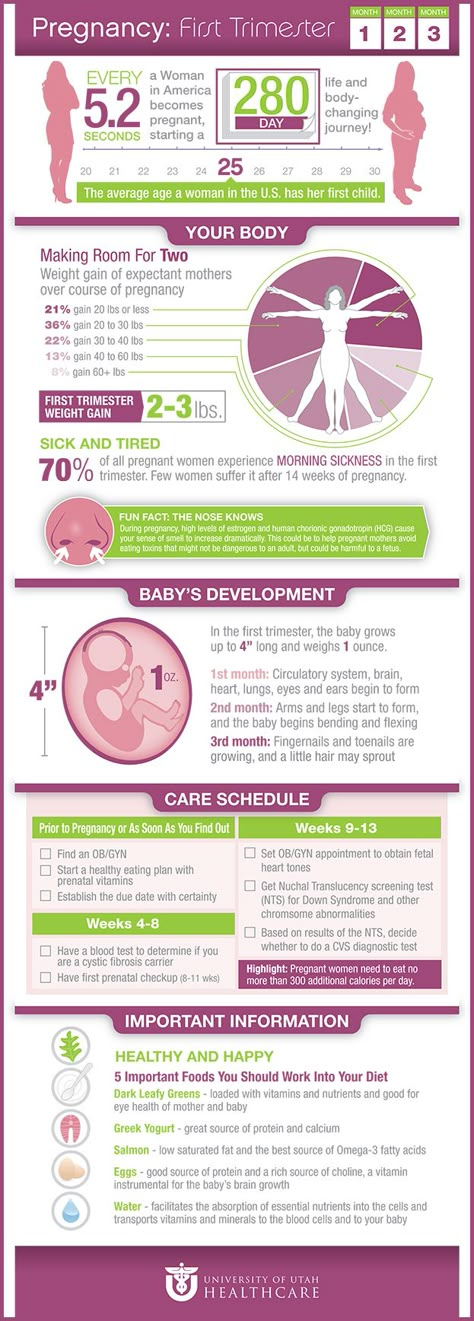 Among the possible causes of miscarriage at this stage:
Among the possible causes of miscarriage at this stage:
- hormonal deficiency preventing fetal development;
- anomalies in the structure of the uterus;
- genetic failures;
- Rhesus conflict.
However, the reasons often remain unknown, and the woman safely bears her third pregnancy. After two miscarriages, there is a 70% chance that the third pregnancy will pass without pathologies.
It is very important that women know that the chances of miscarriage are quite high in the first trimester of pregnancy were ready for it and did not panic. Miscarriages recur only in a small number of women; if you have had one miscarriage, the chances that the next pregnancy will be successful is very high.
The main symptom of threatened interruption is bleeding . However, it is important to remember that not all bleeding indicates a threatened miscarriage. However, although some spotting in early pregnancy is quite common, it is still not normal. Severe bleeding requiring frequent pad changes for heavy flow should be reported to the doctor immediately. Bleeding is usually accompanied by other symptoms: colic, pain in the lower abdomen, fever, weakness, and sometimes vomiting. There may be clots in the blood. You may also notice an unusual smell. Others are possible types of bleeding :
Severe bleeding requiring frequent pad changes for heavy flow should be reported to the doctor immediately. Bleeding is usually accompanied by other symptoms: colic, pain in the lower abdomen, fever, weakness, and sometimes vomiting. There may be clots in the blood. You may also notice an unusual smell. Others are possible types of bleeding :
- brown simultaneous or continuous discharge from the vagina;
- minor bleeding accompanied by severe pain in the abdomen or shoulders.
If minor bleeding does not stop for more than three days, this is a bad symptom.
Severe bleeding and colic between the end of the second and the end of the third month: classic symptoms threatened miscarriage. A sharp pain in the lower abdomen, not accompanied by bleeding, is also an alarm signal. Bleeding can reach such intensity that you have to change several pads within an hour, or it can be "bearable" - as during heavy menstrual bleeding. A thick discharge may appear: dark red clots that look like small pieces of raw beef liver. nine0003
A thick discharge may appear: dark red clots that look like small pieces of raw beef liver. nine0003
Sometimes gray or pink discharge. In the first trimester, the threat of miscarriage may also be indicated by persistent minor bleeding or not very severe pain in the abdomen. In the hospital, the doctor will be able to tell if it is really a threat of miscarriage, and if so, how far the process has gone. He will perform a careful examination of the abdominal organs, may prescribe an ultrasound.
Ectopic pregnancy
An ectopic pregnancy occurs when the fetus does not implant in the uterine cavity, but begins to develop in the fallopian tube. It is very dangerous. In the event of a pipe rupture, there may be a threat to life. Classic symptoms ectopic pregnancy : severe pain in the abdomen or side.
The pain may start as a dull ache and get worse. Pain in the neck and shoulders is also common. Along with pain, you may also have menstrual-type bleeding, but pain is the main symptom.