Red spots on bottom of baby feet
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.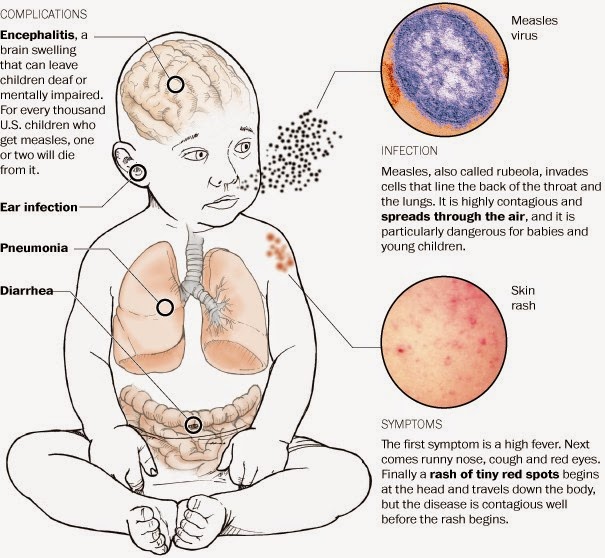
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
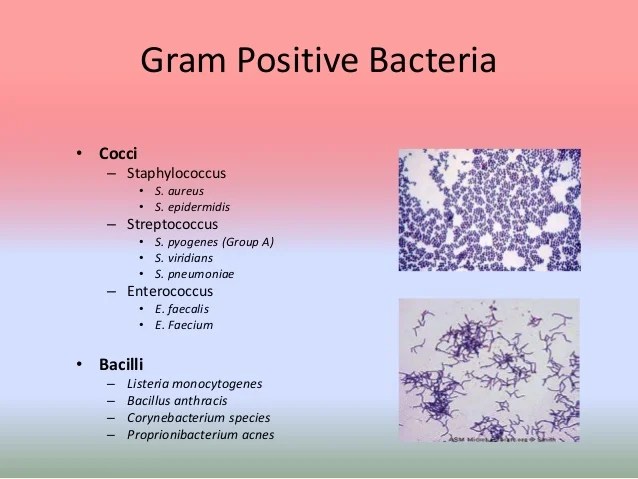
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.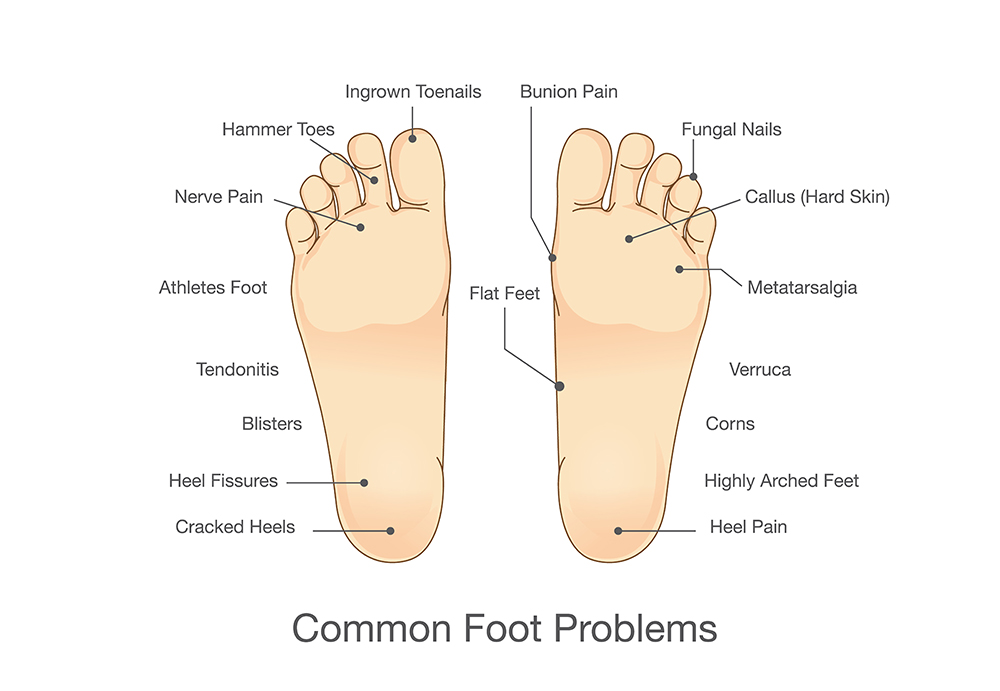
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Hand, Foot, and Mouth Disease (for Parents)
What Is Hand, Foot, and Mouth Disease (HFM)?
Hand, foot, and mouth disease (HFM) is a common viral infection that causes painful red blisters in the mouth and throat, and on the hands, feet, and diaper area. The coxsackievirus causes most HFM infections.
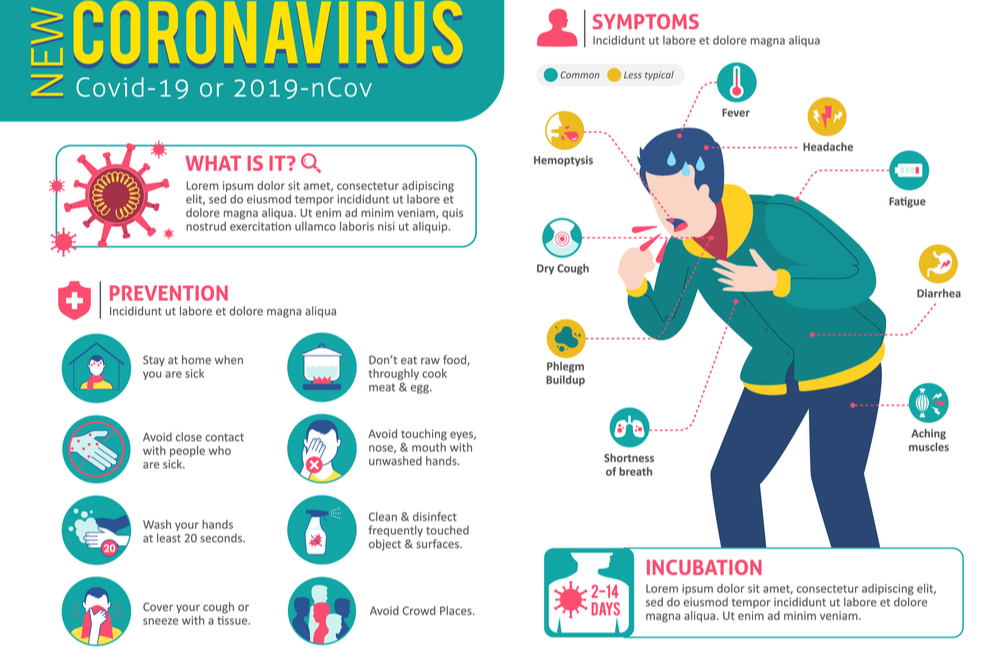
HFM is contagious and easily spreads through contact with unwashed hands, feces (poop), saliva (spit), mucus from the nose, or fluid from the blisters. Kids under age 7 are most at risk for HFM. Infections are common in childcare centers, preschools, schools, summer camps, and other places where kids are close together.
Kids under age 7 are most at risk for HFM. Infections are common in childcare centers, preschools, schools, summer camps, and other places where kids are close together.
Besides the blisters, kids often have a fever for a few days and can get dehydrated because it hurts to swallow liquids. Symptoms usually clear up within a week to 10 days, and kids recover completely.
There's no cure for HFM and no vaccine to prevent it, but your doctor can recommend home care to make your child more comfortable during recovery.
What Are the Signs & Symptoms of Hand, Foot, and Mouth Disease?
The blisters caused by HFM are red with a small bubble of fluid on top. They often peel, leaving an ulcer, which is a sore with a reddish base. The soles of the feet and the palms of the hands may have a rash that can look like flat red spots or red blisters.
Occasionally, there might be a pink, non-itchy rash on other parts of the body, such as the buttocks and thighs. However, some kids will have no problems other than sores in the back of the throat (called herpangina).
It can be hard for parents to tell if a child (especially a very young one) has HFM if sores are only inside the mouth or throat. Very young kids might not be able to communicate that they have a sore throat. But if a child stops eating or drinking, or wants to eat or drink less often, it's a sign that something is wrong.
A child with HFM also might:
- have a fever, muscle aches, or other flu-like symptoms
- become irritable, fussy, or sleep more than usual
- begin drooling (due to painful swallowing)
- only want to drink cold fluids
- have belly pain, vomiting, or diarrhea
How Is HFM Treated?
You can give acetaminophen or ibuprofen if your child is achy or irritable. Never give aspirin to children or teens, as it may cause a rare but serious illness called Reye syndrome.
Cold foods like ice cream, smoothies, and popsicles also help by numbing the area, and will be a welcome treat for kids who have trouble swallowing (and even those who don't!). Avoid hot drinks, sodas, and acidic food (citrus juice, tomato sauce, etc.) because they can make the pain worse.
Avoid hot drinks, sodas, and acidic food (citrus juice, tomato sauce, etc.) because they can make the pain worse.
Kids with blisters on their hands or feet should keep the areas clean and uncovered. Wash the skin with lukewarm soap and water, and pat dry. If a blister pops, dab on a bit of antibiotic ointment to help prevent infection and cover it with a small bandage.
Make sure your child drinks plenty of fluids to stay hydrated.
When Should I Call the Doctor?
Call your doctor if your child remains very irritable, can't be comforted, is sluggish, or seems to be getting worse. Also call if you see signs of dehydration, like a dry or sticky mouth, sunken eyes, and peeing less than usual or fewer wet diapers.
Can Hand, Foot, and Mouth Disease (HFM) Be Prevented?
To prevent the spread of HFM, keep kids home from school and childcare while they have a fever or open blisters on the skin and in the mouth.
Hand washing is the best protection. Remind everyone in your family to wash their hands well and often, especially after using the toilet or changing a diaper, and before preparing or eating food. Shared surfaces and toys in childcare centers should be cleaned often with a disinfectant because many viruses can live on objects for a few days.
Remind everyone in your family to wash their hands well and often, especially after using the toilet or changing a diaper, and before preparing or eating food. Shared surfaces and toys in childcare centers should be cleaned often with a disinfectant because many viruses can live on objects for a few days.
Spots on the foot of a child
The appearance of spots on the foot of a child often worries parents. They come in different colors, sizes, cause itching or do not bother at all. If you encounter such a problem, you should immediately consult a doctor to find out what caused them and how to deal with them. Remember that an independent search for answers on the Internet and self-treatment is unsafe for health. After all, the reasons are not always obvious.
White
White spots on the foot of a child cause vitiligo. This is a skin disease in which the production of the melanin pigment responsible for coloring stops in some areas. As a result, the skin in this place becomes milky white.
As a result, the skin in this place becomes milky white.
Spots can appear anywhere on the skin, including the feet. At first they are small. If you do not start treatment, they will gradually increase. Causes of vitiligo include genetic predisposition, weakened immunity, autoimmune disorders.
See below for a photo of what the spots on the foot of a child with vitiligo look like:
Features of spots with vitiligo:
- feel like healthy skin;
- do not cause discomfort;
- hairs growing in the affected area also become discolored;
- do not sunbathe in the sun, do not get goosebumps.
Red
Red spots on the foot of a child are the most common. The color varies from pale pink to deep dark red. The main causes of occurrence: allergic reactions, infections, mechanical factors.
Allergy
Allergic skin changes usually manifest as urticaria or contact dermatitis. With urticaria, the spots are red, slightly raised above the surface of the skin, tend to merge with each other. With contact dermatitis, they are pink, cause severe itching, get wet, peel off. In allergic children, rashes on the feet are provoked by the use of highly allergenic foods, sweets, skin treatment with inappropriate baby cream, wearing shoes or socks made of non-natural materials, insect bites and other factors.
With urticaria, the spots are red, slightly raised above the surface of the skin, tend to merge with each other. With contact dermatitis, they are pink, cause severe itching, get wet, peel off. In allergic children, rashes on the feet are provoked by the use of highly allergenic foods, sweets, skin treatment with inappropriate baby cream, wearing shoes or socks made of non-natural materials, insect bites and other factors.
Foot fungus
Usually occurs in children under 10 years of age. Contributes to the development of the disease unformed defense mechanisms and the thinness of the skin, through which the infection easily penetrates. At risk are children who visit the pool, who like to walk barefoot.
Fungal infection causes small cracks, pink, red or yellowish spots on the skin, with an unpleasant odor, burning and severe itching. The skin in the affected area becomes very dry and begins to peel off. For treatment, local antifungal agents are used, which the doctor should prescribe.
Infectious diseases
Red spots or a rash on the feet of a child can be symptoms of childhood viral infections: chickenpox, rubella, measles, infectious erythema, etc. Depending on the type of pathogen, the rash looks different, spreads throughout the body or to individual plots.
For example, when infected with Coxsackie enterovirus, the rash spreads only to the palms, feet and mouth. In infectious diseases in children, the temperature rises, there is weakness, lethargy, loss of appetite, headache. They go by themselves. For treatment, only symptomatic agents are prescribed to reduce temperature, relieve itching, and prevent bacterial complications.
Uncomfortable shoes
Red spots on the feet are often associated with ill-fitting shoes. If certain areas experience pressure, friction or increased stress, then the skin in this area will turn red. Also, the reason may be in violation of thermoregulation. For example, if the feet are too hot in shoes and they constantly sweat.
Particular attention should be paid to the choice of shoes if the child has flat feet or other types of foot deformity. In this case, special, orthopedic shoes are needed. Which one is suitable for the child, the orthopedist decides after the examination.
Brown
Such spots on the legs and feet of a child are associated with the accumulation of melanin pigment in the skin. Areas where there is a lot of it become dark in color. We call them moles or birthmarks. They are quite small, up to 1.5 mm in size, or large, more than 1 cm in diameter. They begin to appear in the first years of life and during puberty.
Moles and birthmarks are generally harmless and do not require removal. However, they need to be monitored.
Warning signs include:
- size increase;
- asymmetry;
- uneven jagged edges;
- discoloration;
- spotting.
If you notice that such changes occur with a mole, you need to urgently consult a doctor, because this is how skin cancer, melanoma, manifests itself.
To keep your child's feet in good condition, visit a pediatric podiatrist regularly. The doctor will tell you how to care for the skin of the feet, how to choose shoes, how to prevent diseases.
Red feet in a child, what causes?
Red feet and a rash on the legs is a sign that parents should not ignore. Such changes do not always indicate problems with the feet; they can be a symptom of an allergic reaction, injury, infection, or internal disease.
Allergy
Allergy occurs in response to direct contact with certain irritants. Each child will have their own, depending on the characteristics of the immune system. Allergy manifests itself in the form of urticaria or contact dermatitis.
When a child has urticaria, red spots and circles of different sizes and shapes appear on the child's feet. They rise slightly above the skin and sometimes merge with each other. With contact dermatitis in children, red dots form on the feet, irritation, itching and peeling of the skin are observed.
Socks or shoes made of artificial materials, new baby cream, soap, washing powder can cause allergies. Some children have this reaction to changes in temperature, cold or heat.
Antihistamines help to cope with the manifestations of allergies. For children, they are produced in the form of syrups, drops. A specific medicine is prescribed by a doctor. To prevent repetitions of allergies, it is important to identify the irritant and try to avoid contact with it in the future.
Injuries
Injuries are often accompanied by redness, swelling, pain, inflammation. These include bruises, sprains, tendons, joint dislocation and others.
Red spots on the feet of a child cause deformities of the foot and improper distribution of the load. In this case, the places experiencing the greatest pressure are injured and inflamed. To fix the problem, you need to contact an orthopedist. Pick up orthopedic insoles, shoes, liners that contribute to the anatomically correct position of the foot, correction of deformity.
Injury to delicate skin is often caused by ill-fitting or tight shoes. She will squeeze the leg, rub in certain places, which will also cause redness. Especially if the baby spends a lot of time in uncomfortable shoes, walks or runs for a long time.
Infections
Redness and rash on the feet of a child are provoked by viral, bacterial and fungal infections.
For example, one of the manifestations of an enterovirus infection caused by the Coxsackie virus will be a rash in the form of sores and watery red pimples on the palms and feet of a child. They do not require special treatment, they go away on their own within 3-5 days as they recover. In the first days, the rash is very itchy. But it is important to ensure that the child does not comb, as there is a risk of introducing a bacterial infection.
Chickenpox and measles cause red spots on the feet and hands of a child. In this case, the rash spreads throughout the body. You can recognize a viral infection by a sudden high temperature (up to 39 - 40 ° C), lethargy, capriciousness, loss of appetite, headache. The rash appears 1 to 2 days after the temperature rises.
The rash appears 1 to 2 days after the temperature rises.
Red spots on the feet of a child, burning, itching, peeling, cracks are signs of a fungal infection of the skin and nails. If these symptoms appear, consult a podiatrist. Fungal infection often occurs in children who visit the pool. It is necessary to ensure that in the showers and changing rooms, children do not walk barefoot on the floor. The fungus is treated with antifungal ointments, creams.
Bacterial infections develop when the integrity of the skin is violated, if the sites of damage are not treated in time with an antiseptic (brilliant green, chlorhexidine, iodine). Pathogenic bacteria easily penetrate the skin through wounds, scratches, abrasions. Diabetic children are most vulnerable because high blood sugar levels interfere with rapid healing. Most often, bacterial infections occur in the summer, when the baby walks with bare legs, wears open sandals, slippers.
What to do?
If you find red spots, rashes or pimples on your child's feet, see a dermatologist or surgeon if there has been an injury.