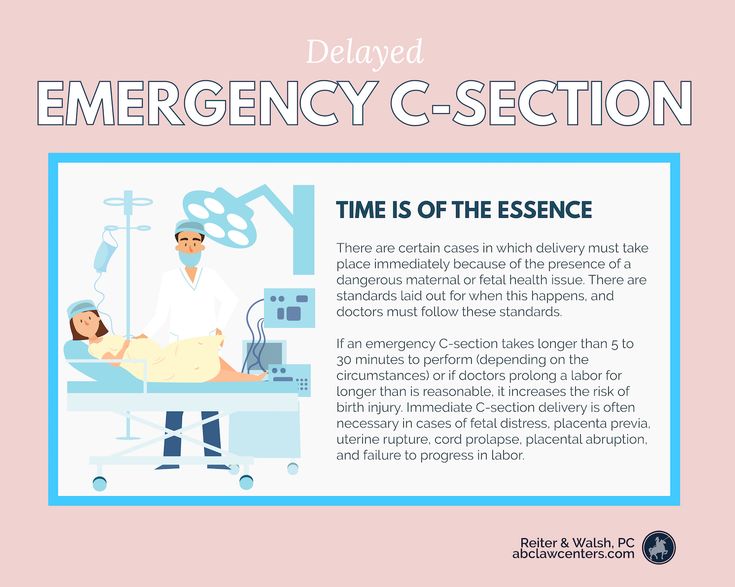
Recovering from emergency c section
C-Section Recovery - What to Expect: Walking, Blood Clots, & Pain
Series Cesarean Section (C-Section)
Written by Hallie Levine
About 1 of every 3 newborns in the United States are delivered by cesarean section, or C-section. That’s when the baby comes out through a cut in the mother’s belly and uterus rather than going through the birth canal and coming out through the vagina.
Afterward, you can expect to spend 2-3 days in the hospital with your new little one as you recover.
After C-Section Surgery
Most women are awake for the C-section, and you should be able to hold your baby right away. You’ll be taken to a recovery room, where nurses will check your blood pressure, heartbeat, and breathing and keep an eye on you.
You may feel sick to your stomach, groggy, or itchy from the drugs used to numb you during the surgery. You may be given a pump so you can change the amount of pain medication that’s going through a thin tube into your veins.
In the days after surgery, you can expect:
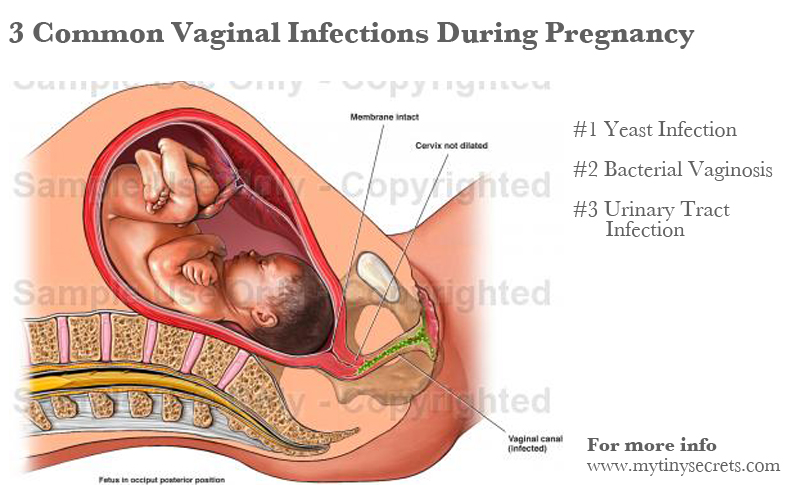
- Vaginal discharge: You’ll likely have vaginal bleeding for several weeks after delivery. This is how your body gets rid of the extra tissue and blood in your uterus that kept your baby healthy during pregnancy. The first few days, you’ll see bright red blood that will gradually get lighter -- turning pink, then brown, to yellow or clear before it stops.
- Afterpains: It’s normal to have things that feel like menstrual cramps for a few days after delivery. They narrow the blood vessels in your uterus to help keep you from bleeding too much. Ask your doctor if you can take an over-the-counter pain medication.
- Breast swelling and soreness: The first 3-4 days after delivery, your breasts make something called colostrum, a nutrient-rich substance that helps boost your baby’s immune system.
 After that, your breasts will swell as they fill up with milk. You can help ease tenderness by nursing or pumping, and putting cold washcloths on your breasts between feedings. If you’re not breast-feeding, wear a firm, supportive bra. Don’t rub your breasts -- that will cause them to make more milk.
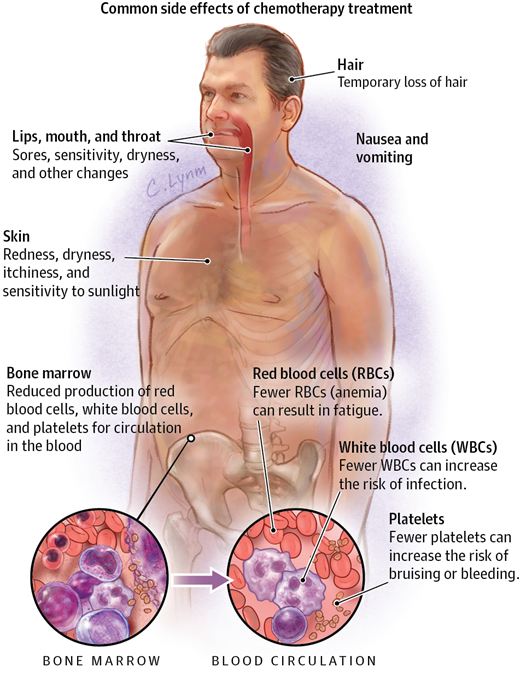
After that, your breasts will swell as they fill up with milk. You can help ease tenderness by nursing or pumping, and putting cold washcloths on your breasts between feedings. If you’re not breast-feeding, wear a firm, supportive bra. Don’t rub your breasts -- that will cause them to make more milk. - Hair and skin changes: You may notice your hair thinning in the first 3-4 months. This is normal. It’s caused by changing hormone levels. (When you were pregnant, high levels of hormones made your hair grow faster and fall out less.) You may also see red or purple stretch marks on your belly and breasts. They won’t go away, but they will fade to silver or white.
- Feeling blue: After you bring your baby home, you may find yourself going through a roller coaster of emotions. You might feel worried, anxious, or very tired during the first few weeks of motherhood.
 Called the “baby blues,” this comes from hormone changes. If you feel this way beyond a couple of weeks, though, call your doctor. You may have postpartum depression or anxiety, a more serious condition that happens in about 15% of all new moms. Talk therapy or antidepressants can usually help.
Called the “baby blues,” this comes from hormone changes. If you feel this way beyond a couple of weeks, though, call your doctor. You may have postpartum depression or anxiety, a more serious condition that happens in about 15% of all new moms. Talk therapy or antidepressants can usually help.
C-Section Incision Care
Your doctor will send you home with detailed instructions -- for instance, how long to keep your cut bandaged, how often to change bandages.
Here are some tips for taking care of your C-section incision:
- If the cut is closed with stitches, staples or glue, you should be able to remove the bandage and take showers, but check with your doctor first. Letting the water run down over the wound should also help with cleaning.
- When you’re washing, use mild soap and water and clean it lightly (don’t scrub, particularly if your incision is closed with steristrips or glue). Pat dry.
- Don’t soak in a bath or hot tub or go swimming until your doctor says you can.
- Try over-the-counter pain relievers such as ibuprofen or acetaminophen to manage incision pain. Ask your doctor what they recommend.
- A heating pad set on low or a warm washcloth can help with pain around your belly.
- Keep an eye out for any signs of infection. Let your doctor know if:
- Your incision is red, swollen or hot to the touch.
- It’s leaking discharge
- You develop a fever.
- Your pain is getting worse not better.
- You are having heavy bleeding
Tips for Healing After a C-Section
The area around the stitches, staples, or tape on your belly will be sore for the first few days. Keep it clean to prevent infections. You can do a few other things to speed your recovery:
- Take it easy. A C-section is a major surgery. Don’t lift anything heavier than your baby for the first couple of weeks, and keep everything you might need within reach.
- Support your stomach.
 Hold your belly when you sneeze, cough, or laugh to keep it still.
Hold your belly when you sneeze, cough, or laugh to keep it still. - Ease your pain. A heating pad (set on low) or a warm washcloth can help with pain around your belly. You may also need acetaminophen, ibuprofen (Advil, Motrin), or other pain relievers. Most are safe to take if you’re breastfeeding.
- Drink fluids. You’ll need to replace the water you lost during delivery as well as what you lose if you nurse your baby.
Eat fiber-rich foods and smaller, more frequent meals. Try a fiber supplement if you are having constipation.
Breastfeeding After a C-Section
You can start nursing almost right away. Your body will make milk about as quickly as after a vaginal delivery. Here’s what you need to know:
Medications: You probably got pain-numbing medicine, such as an epidural, during your C-section, but it isn’t likely to affect the baby much. Your baby may be sleepy, but that should pass and they should be eager to nurse. You may be tempted to ask your doctor to cut back on your pain medicine, but it’s important that you stay comfortable. Pain can mess with the hormone that helps you make milk. If you have any questions about how the drugs you’re given can affect breastfeeding, ask to speak to the hospital’s breastfeeding specialist.
Your baby may be sleepy, but that should pass and they should be eager to nurse. You may be tempted to ask your doctor to cut back on your pain medicine, but it’s important that you stay comfortable. Pain can mess with the hormone that helps you make milk. If you have any questions about how the drugs you’re given can affect breastfeeding, ask to speak to the hospital’s breastfeeding specialist.
Nursing positions: The site of the surgery may make it hard to find a comfortable position to nurse your baby. You can put a pillow over your stomach to ease the baby’s weight, or try these:
- Football hold. Cradle your baby’s neck in your palm, and rest their back on your forearm. Tuck the feet and legs under your arm and then lift your baby to your breast.
- Side-lying hold. Lie down facing your baby, and use your hand to bring your nipple to their lips. You can place a pillow behind their back to keep them from rolling.

Returning to Physical Activities After a C-Section
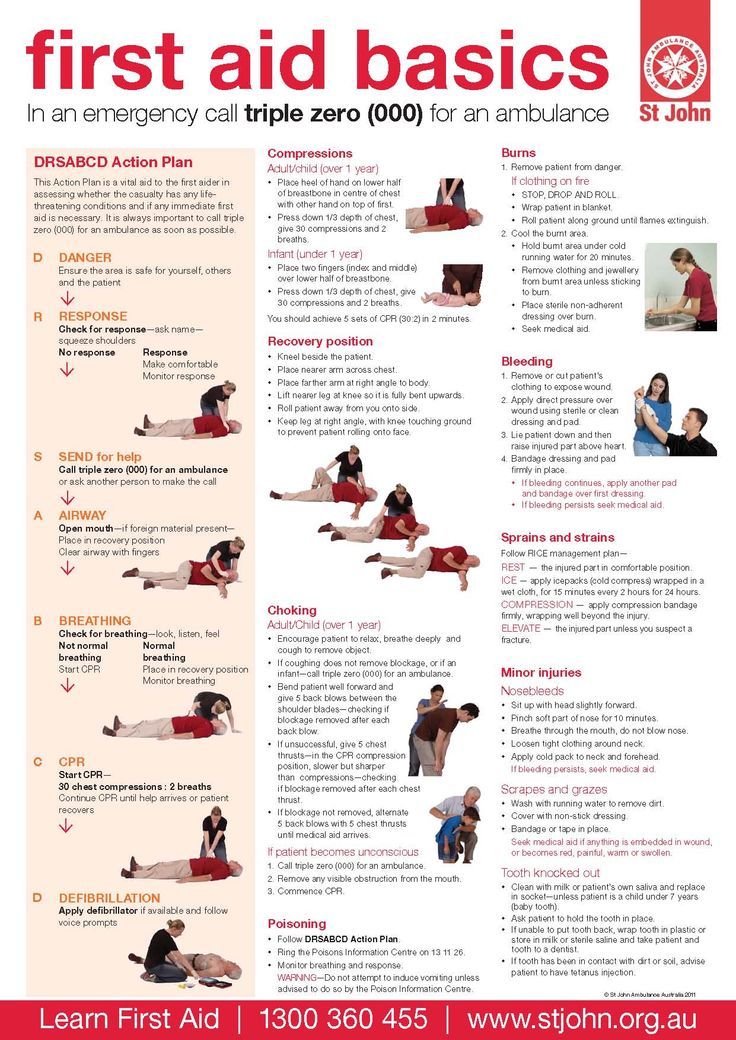
It’s important to get out of bed and walk around within 24 hours after surgery. This can help ease gas pains, help you have a bowel movement, and prevent blood clots.
You can try gentle exercises a few days after the C-section:
- Deep breathing: Take 2 or 3 slow, deep breaths every half-hour. This can help prevent lung congestion from sitting in bed so much.
- Shoulder circles: Sit upright and roll your shoulders 20 times in both directions every hour to help with stiffness.
- Gentle stretching: Stand against a wall and raise both arms slowly above your head until you feel the muscles in your belly stretch. Hold for 5 seconds, and then relax. You can do this up to 10 times a day to boost flexibility around your stitches.
Try not to do too much housework or other activities for the first couple of weeks. Check with your doctor before returning to any of these activities, but in general you will have to wait:
Check with your doctor before returning to any of these activities, but in general you will have to wait:
- 4-6 weeks before doing heavy exercises that involve your belly or lifting anything larger than your infant
- 2 weeks before you can drive a car
- 3 weeks (once you have a healed incision) to take a bath or go swimming
Get your doctor’s OK before having sex again.
When to Call a Doctor
Once you get home, check the site of your surgery regularly for signs of infection. Here are some things you would need to let your doctor know:
- Your incision is red, swollen, hot to the touch, or leaking discharge
- You have a fever higher than 100.4 F.
- You have a lot of vaginal bleeding, it smells bad or has unusually large clots.
- Your pain is getting worse, not better.
- You have swelling, bumps, pain or heat in your calves (which can be signs of a blood clot)
- You have pain, redness or warmth, which are signs of infection
- You get a very bad headache that does not go away.
- You notice swelling in your hands, arms, or feet.
- You notice vision changes or have difficulty seeing.
- You have a cough, shortness or breath or pain in your chest, which could be a sign of a blood clot.
You’ll probably see your doctor about 6 weeks after delivery. They’ll check your vagina, cervix, and uterus as well as your weight and blood pressure.
How to recover from a c-section at home
How long does it take to recover after a c-section?
It usually takes about 6 weeks to recover from your c-section but this will depend on your individual situation. If you had any problems during or after your c-section, or if you’re looking after other children at home, you may feel you need more time to recover.
Speak to your GP if you are still having pain or you don’t feel you have recovered after 6 weeks.
“I was busy at home looking after my older children. I felt tired and uncomfortable for nearly three months.
”
Sarah
Gentle exercise, such as walking, will help you recover from your c-section. But avoid anything more active until you have no pain and you feel ready. For example, avoid driving, carrying anything heavy, having sex or doing heavy housework, such as vacuuming, until you feel able to. You will need help with carrying your baby in their car seat and with lifting their pram. Check with your insurance company when you will be covered for driving after a c-section.
Read more about when to exercise after a c-section.
Medical checks
Your midwife and health visitor will visit you at home for the first few weeks to check how you and your baby are getting on. After that, you can see your health visitor at a local clinic if you’d like your baby to be weighed or if you want to talk about any problems you’re having. You will need to make an appointment with your GP for your post-natal check 6–8 weeks after your c-section. This is to check how you are recovering.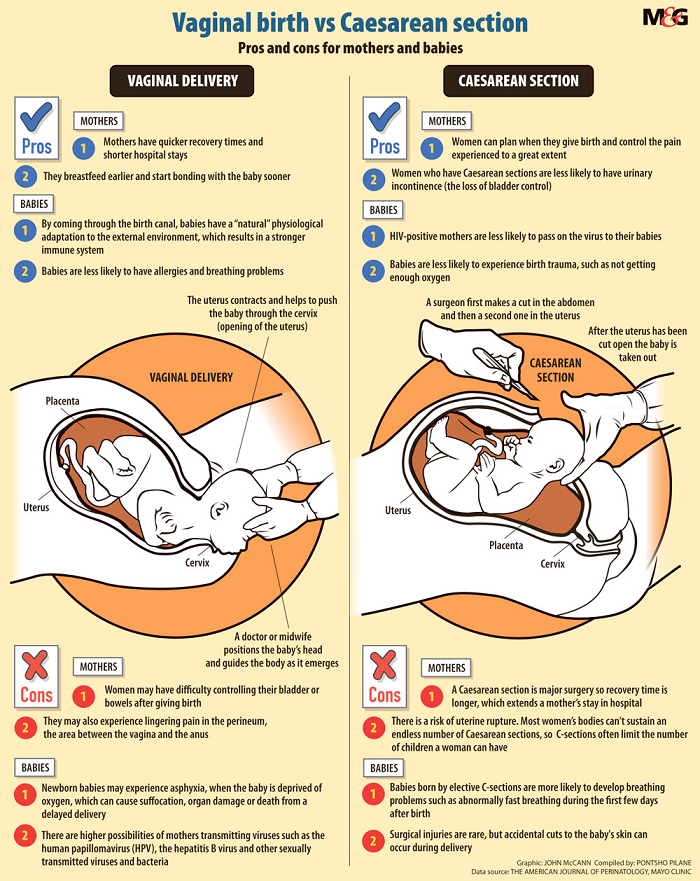
Read about coping emotionally after a c-section.
Looking after your c-section wound
Your midwife will visit you at home to check your wound and remove your dressing, if you still have one. They will also remove the stitches or staples after 5–7 days, unless you have dissolvable stitches. This does not hurt but it may feel uncomfortable.
Once your dressing is off, clean and dry your wound carefully every day. You may find it more comfortable to wear cotton high-waisted pants and loose clothes.
Tell your midwife or GP straight away if you have any signs of infection, such as:
- you have a high temperature
- you feel generally unwell - for example, an upset stomach
- your wound becomes red, swollen, painful or has a discharge.
“I got an infection in my wound a week after surgery and I felt a bit of a failure because of it. I had been bathing and keeping it clean as well as I could, but it’s in an awkward place and with the extra baby weight, it’s hard to see the wound.
”
Laura
Pain relief
Your wound will feel sore and bruised for a few weeks. You will need to take pain relief for at least 7–10 days after your c-section.
Your midwife or doctor will tell you what pain relief you can take. Small amounts of any medicine you take may pass into your breastmilk but they’re unlikely to harm your baby if you take them as instructed. Do not take codeine or co-codamol (which contains codeine) if you’re breastfeeding, as they may harm your baby.
Always check with your doctor, midwife or pharmacist before taking any medicines. Your midwife may give you painkillers, such as paracetamol, to take at home.
It’s important to take your pain relief regularly and on time, even if you don’t have pain at the moment. If you are still having pain with the painkillers, speak to your midwife, pharmacist or GP.
Getting in and out of bed
Getting in and out of bed can be difficult or uncomfortable while you’re recovering from your c-section.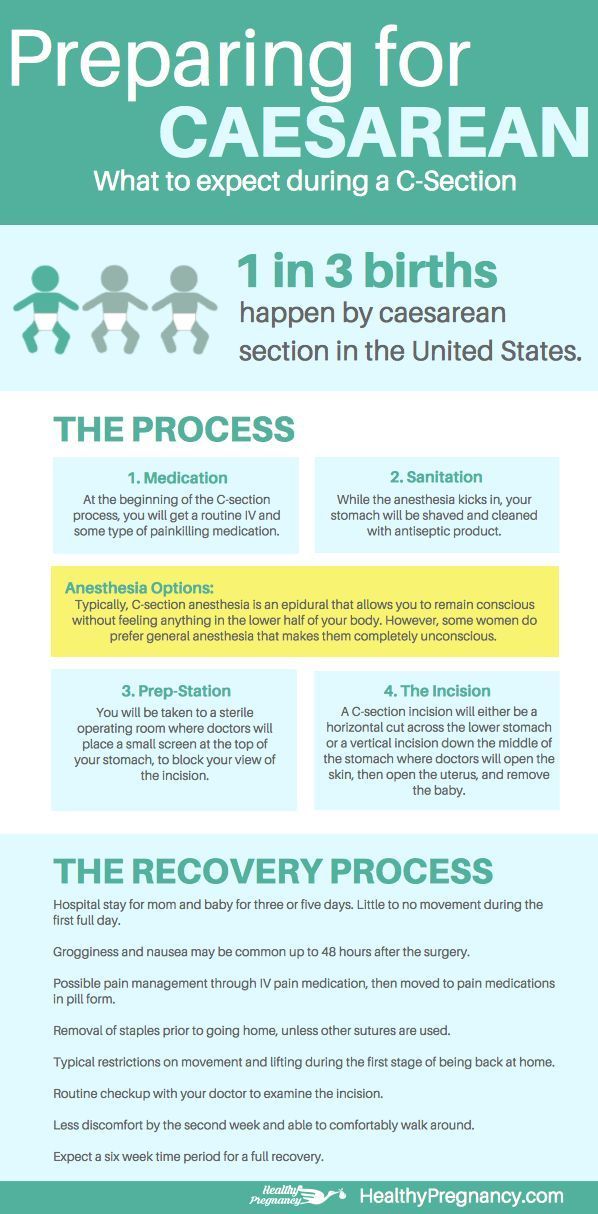 To make it easier to get out of bed, you could try:
To make it easier to get out of bed, you could try:
- rolling on to your side
- dropping both legs over the side of the bed
- pushing yourself up sideways into a sitting position.
Try to stand up as straight as you can. You can do the opposite to get back into bed.
“I was not prepared for how difficult I would find getting out of bed after my second c-section. The first few days are the worst so if you can sleep sitting up, it’s probably worth trying!”
Stacey
C-section scar recovery
Your wound will take about 6 weeks to heal. You will have a scar but this will fade over time. Your scar will be 10–20cm long and is usually just below your bikini line. It will be red at first but will fade over time. On darker skin, it may fade to a brown or white line. You may lose feeling in the area of your wound, which may come back over time.
“I had no feeling around my wound for nearly 5 months.
I just had a strange feeling of pins and needles when I touched the area.”
Sarah
Your midwife may advise you to massage your scar after it has fully healed. This can break up the scar tissue and stop any itching. There isn’t much evidence to show how well this works, but some people find it helpful. To massage your scar:
- lie on your back
- using a non-perfumed cream or lotion, make 20–30 small circular motions with your fingertips over your scar
- repeat 2–3 times a day.
Read more about what to expect after a c-section.
Preventing blood clots
Keeping as active as possible and drinking plenty of fluids will help to lower your risk of a blood clot.
Your midwife may have given you a blood-thinning medicine. While you’re in hospital, they will show you how to inject yourself daily.
Tell your GP, midwife or health visitor straight away if you have signs of a blood clot, such as:
- a cough
- shortness of breath
- swollen or painful lower legs.

Sex after a c-section
You may not feel ready to have sex again until you have fully recovered from your c-section. This may take about 6 weeks. How long you wait will depend on how you feel physically and emotionally.
Your GP will talk to you about your contraception options at your 6-week check. But you can speak to your midwife, health visitor or GP at any time about contraception.
Read more about sex after pregnancy.
Driving after a c-section
You can start driving again once your GP has told you that it’s safe for you to do so. This may be about 6 weeks after your c-section.
You should be insured to drive once your GP has said you can. Have a look at your insurance company’s website to check their policy on driving after a c-section.
If you have ongoing complications from your c-section that affect your driving, you may need to tell the DVLA and your insurance company.
When to seek help after a c-section
If you have any of the following symptoms contact your GP or call 111 straight away:
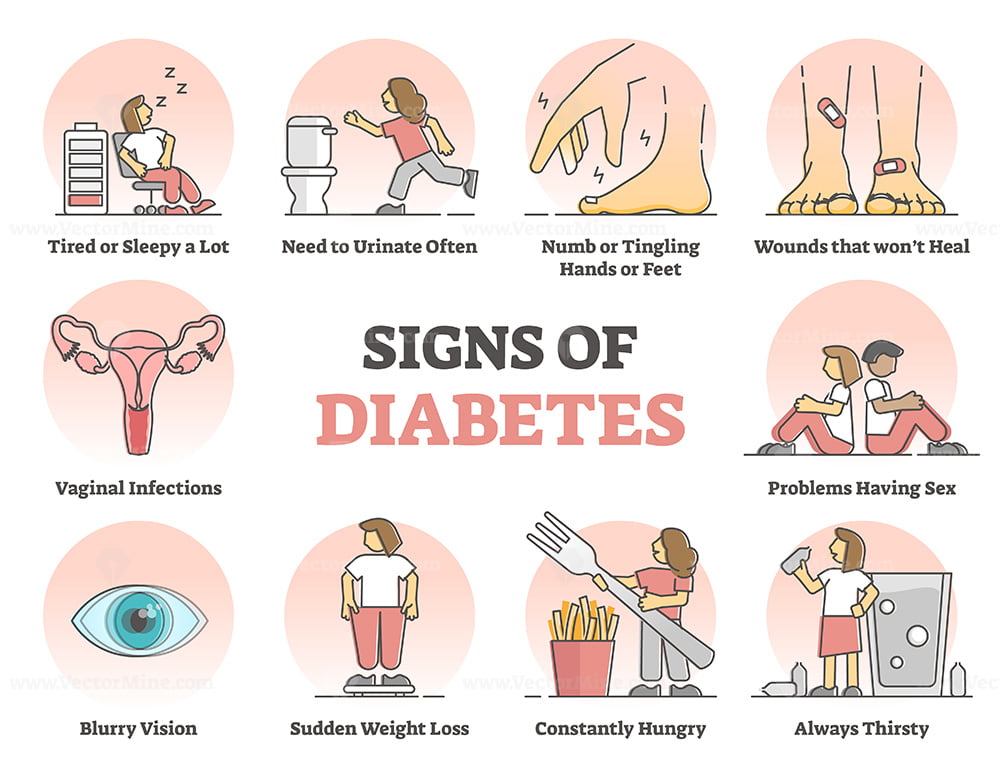
- difficulty or pain passing urine or leaking urine when you don’t mean to
- your pain relief is not keeping your pain under control or your pain is getting worse
- sore or tender abdomen (tummy area)
- red, swollen or painful wound
- discharge from your wound or you’re worried your wound is not healing properly
- a high temperature
- vaginal bleeding that is still heavy after a week or gets heavier – get help straight away if you also feel faint or dizzy, or your heartbeat is fast or ‘pounding’
- unpleasant smelling vaginal blood or discharge
- cough, chest pain or shortness of breath
- a persistent or severe headache
- pain, redness or swelling in the lower leg (calf muscle)
- breast redness and swelling for more than 24 hours and is getting worse
- problems with your baby’s breathing – call 999 if you’re worried about your baby’s breathing.
Always call 999 if you or your baby needs emergency medical help.
Read more about vaginal bleeding after a c-section.
Your next pregnancy
When you’re ready, you may start thinking about having another baby. Read more about your health in pregnancy and options for giving birth if you've had a previous c-section.
Recovery after caesarean section
The birth of a baby is an exciting event for the family. However, sometimes, for various reasons, a child cannot be born naturally. And then, in order to save the mother and baby, they perform a caesarean section (CS). As a result, a scar remains on the uterus - "the smile of life, with the help of which the baby was born." After this operation, mothers need special support and care: how and what exactly - about this midwife Alla Yevtushenko.
nine0005CS is performed as follows: under spinal anesthesia, doctors cut the abdominal wall and uterus, and then remove the baby and placenta.
In addition to the standard procedure, there is a soft CS. It can be done, both planned and in childbirth, if mom and baby feel good. Mom is conscious, helps the baby to be born, pushing, and sometimes takes it herself. Doctors wait for the umbilical cord to pulsate, then remove the placenta, suture the uterus, and apply cosmetic sutures to the skin.
There is still a difference in recovery after natural childbirth (ER) and CS. After ER, a woman, as a rule, feels well within a day. And after the CS, you need a few more days, weeks or months to recover. The body heals the fastest, the psyche recovers more slowly, especially if the woman was very determined to give birth naturally.
- After the operation, the CS-mother may feel weakness in the muscles around the suture, numbness and decreased sensitivity in this area. Pain at the incision site may persist for up to 1-2 weeks. Sometimes painkillers are needed to deal with it. nine0017
- Immediately after CS, women are encouraged to drink more and go to the toilet (pee).
The body needs to replenish the volume of circulating blood, because blood loss with CS is always greater than with EP. While the CS-mother is in the intensive care unit (within 6-24 hours, depending on the maternity hospital), she has a urinary catheter. This allows you to evaluate how the kidneys are working.
- In the early days, it is better to eat liquid and semi-liquid food - it is absorbed faster and does not overload the body. nine0017
- When a woman returns home from the hospital, you need to take care of the seam - ventilate more often, treat with disinfectants (miramistin or an alcohol solution of chlorophyllipt). Remember - the scar can not be rubbed and scratched. Itching indicates that the wound is healing.
- After the operation, you can wear a bandage - an elastic belt that supports the front wall of the abdomen. Rules: you need to put on a bandage lying down and wear it no more than 5-6 hours a day and no longer than a month so that the muscles do not lose their tone.
You need to wear a bandage over linen made from natural fabrics. A good alternative is to tie up with a sling or rebozo. nine0017
- After 6 weeks, you can already start doing exercises. Ideally - special complexes for postpartum recovery. For example, postnatal gymnastics from Birthlight.
- It is very good if there are helpers at home who will take care of everyday life, and the woman will only take care of the baby. These may be relatives, friends, or professionals (such as postnatal doulas, whose services are now available in many major cities).
nine0016 Feed the baby on demand. Breast milk, as a rule, comes at the same time as during normal childbirth, but sometimes a little later. If the mother is having difficulty latching on, the nurses in the postpartum ward or breastfeeding consultants can help feed her. It is better if the baby is breastfed as soon as possible. This will help the formation of the correct microflora in the baby's intestines, and the mother's uterus will contract better.

- Baby, of course, you can wear. You need to feed the baby on demand and try to sleep when he sleeps. If the baby does not sleep well or this time is not enough for mom to rest, you can entrust a walk in the first months to dad or "walk" in a stroller on the balcony. nine0017
And most importantly: share your feelings and emotions with those around you. If you do not find support among your inner circle, look for like-minded people and support in thematic groups on social networks. And remember, you are not alone!
Recovery after caesarean section - Arnika Family Clinic, Krasnoyarsk
Services
Virtual tour. Clinic "ARNIKA"
Doctors' advice
The rate of births by caesarean section is increasing worldwide. It can be carried out both in the interests of the mother and in the interests of the child. Today we will talk about the rehabilitation of my mother after this operation.
Immediately from the operating room, the patient is transferred to the intensive care unit, where the medical staff monitors her condition. Depending on the maternity hospital, a child may be brought to the intensive care unit, or the mother will see him already in the postpartum ward. A few hours after the operation, the patient is offered to get out of bed - this is necessary for the prevention of thrombosis. After about 8 hours, the mother is transported to the postpartum ward. For the first day, a sparing diet is prescribed - cereals, broths, steam cutlets. nine0004
Breastfeeding is possible without restrictions - drugs for epidural anesthesia do not get into milk, and stimulation of the nipple promotes uterine contraction and prevents blood clots from stagnation in its cavity. That is why during feeding, many women notice cramping uterine contractions and increased blood secretions.
The skin may be sutured or stapled. And with that, and with the other you can go to the shower.
Pain in the area of the incision can be relieved with pain medication or epidural anesthesia. As a rule, there is no need for anesthesia already for 2-3 days after the operation. nine0009 Many doctors recommend wearing a bandage after a caesarean section. It can also speed up recovery.
In most maternity hospitals, patients spend 5 days after a caesarean section. Discharge may be delayed due to the condition of the mother or child.
Once at home, you can lead your usual way of life, however, do not overwork yourself with household chores. We recommend not to lift anything heavier than a baby.
You need to pay attention to the nature of the discharge. Normally, they should be bloody, gradually becoming transparent. The appearance of bloody discharge, as well as discharge with an unpleasant odor, is an indication for a visit to the doctor. nine0009 In addition, an increase in body temperature should be alarming (remember that nursing mothers measure the temperature in the elbow bend).